Abstract
Age-related sarcopenia places a tremendous burden on healthcare providers and patients' families. Blood flow restriction (BFR) training may be a promising treatment to bring sarcopenia down, and it offers numerous advantages over traditional resistance training. The purpose of this review was to compare the effects of BFR training and conventional resistance training on clinically delayed sarcopenia in the elderly. Databases such as PubMed, Web of Science, Embase, and Science Direct were searched to identify eligible studies; blinded data extraction was performed to assess study quality, and conflicts were submitted to third parties. Someone made the decision. One author used Review Manager (RevMan) 5.4 and compared it with data obtained by another author for this purpose. A total of 14 studies met the inclusion criteria for this review. The funnel plots of the studies did not show any substantial publication bias. Low-load blood flow restriction (LL-BFR) had no significant effect on muscle mass compared with high-load resistance training (HL-RT) (p = 0.74, SMD = 0.07, 95% CI: 0.33 to 0. 46) and LL-BFR had a significant effect on muscle strength compared with HL-RT (p = 0.03, Z = 2.16, SMD = -0.34, 95% CI: 0.65 to -0.03). LL-BFR showed a slight effect on mass compared to LL-RT (p = 0.26, SMD = 0.25, 95% CI: 0.19 to 0.69). Sensitivity analysis produced a nonsignificant change, suggesting that the results of this study are reasonable. In conclusion, the data suggest the possibility that BFR training improves age-related sarcopenia.
Keywords: Blood flow restriction, LL-BFR, Resistance training, Sarcopenia, Older adults, Systematic review, Meta-analysis
Abbreviations
- BFR
blood flow restriction
- LL-BFR
low-load blood flow restriction
- HL-RT
high-load resistance training
- LL-RT
low-load resistance training
- RCT
randomized controlled trials
- CCS
clinical cohort studies
- M
Mean
- SD
Standard Deviation
- RevMan
Review Manager
- SMD
standard mean differences
- RM
repetition maximum
- EG
experimental group
- CG
controlled group
- ND
no description
- ASM
appendicular skeletal muscle
- GRADE
Grades of Recommendation, Assessment, Development, and Evaluation
1. Introduction
China is currently entering an aging phase. According to China's 7th census in 2021, people over the age of 60 account for 18.70% of the population.1 As people age, their skeletal muscle mass is expected to reduce because of limitations of physical activity, which has been referred to as sarcopenia.2 Sarcopenia is a generalized skeletal muscle disorder that emerges with aging, most often found in middle-aged and elderly people.3 According to the definition of the Asian Working Group on Sarcopenia (AWGS), sarcopenia is an age-related progressive age-related activity disorder syndrome characterized by a reduction in whole-body muscle mass, a decrease in muscle strength, and a decline in muscle physiology.45 The Asian Working Group on Sarcopenia (AWGS) defines sarcopenia as the presence of decreased muscle strength and decreased somatic function in conjunction with decreased muscle mass.46
Conventional resistance training has been confirmed to maintain muscle mass and improve muscle strength, however, the effect appears to be insignificant in elderly people because of the high load it requires.61 Since its establishment in Japan in the 1970s,4 Low-Load Blood Flow Restriction (LL-BFR) training has been evidenced to increase skeletal muscle growth and strength,5, 6, 7, 8 as well as reduce knee pain and fluid storage, therefore resulting in the prevention of atrophy and improvement of the overall body function.9 In recent years, LL-BFR has been identified as an effective protocol to improve sarcopenia in elderly people, which has evidenced the crucial improvement of LL-BFR training on skeletal muscle hypertrophy and strength increases. Centern et al. compared the LL-BFR with the protein group, the LL-BFR with the placebo group, and the control group without training but with protein, supplementation and found that the former two groups were significantly more effective than the control group in increasing muscle cross-sectional area.6 Moreover, Hughes, et al. and Lixandro et al. examined the effects of high-load resistance training (HL-RT) and LL-BFR on skeletal muscle strength and mass, further evidencing the important role of LL-BFR in increasing skeletal muscle strength and size.9,11
Currently, there are still some shortcomings in the research content and perspectives of relevant systematic reviews.10,11 For example, participants in the meta-analyses of Centner et al. and Lixandro et al. on the advantage of RCTs are healthy. In addition, there are fewer scientific studies reporting on BFR training in older adults at risk for sarcopenia. In recent years, prospective studies have been well carried out on the effects of LL-BFR on skeletal muscle in older adults, however, the effects of LL-BFR on sarcopenia still remain doubtful. This review is aiming at reformulating the inclusion and exclusion criteria of the meta-analysis to establish the effect of LL-BFR on sarcopenia and is expected to give clinical healthcare practitioners reference ideas for the treatment and rehabilitation of patients with degenerative disorders.
2. Methods
2.1. Protocol
This review, registered on PROSPERO (CRD42022331192), follows the PRISMA criteria for publishing systematic reviews and meta-analyses of healthcare interventions.12
2.2. Search strategy
We used databases including PubMed, Web of Science, Embase, and Science Direct to collect information using combinations of blood flow restriction, blood flow restriction training, BFR, LL-BFR, BFR occlusion, BFR therapy, sarcopenia, and sarcopenia. All synonyms are linked using "OR" and treated as the same component throughout the search. The conjunction "AND" is used to ensure that at least one search result contains the search term. This necessitates truncation and adjacency searches in order to discover alternative variants and sort results. Except for Scopus, all searches use "Title/Abstract, and Keywords." The publications' references were checked to ensure no missing results in our study.
2.3. Inclusion and exclusion criteria
All studies included in this review met the following criteria: (i) they were randomized controlled trials (RCT) or clinical cohort studies (CCS); and (ii) the experimental group completed an LL-BFR intervention while the control group did a conventional HL-RT or LL-RT intervention. (iii) the subjects were all older adults over 60 years of age at risk for sarcopenia, and there were no significant differences in their baseline characteristics; (iv) the outcome metrics included muscle strength and muscle mass, and the indicator data were expressed as mean ± standard deviation (M ± SD); and (v) the studies were all published in English-language scientific journals peer-reviewed by experts.
In addition, studies were excluded if (i) the blinded experimental designs were not used; (ii) the experimental groups used other drugs or nutritional interventions along with LL-BFR; (iii) the studies were conducted in relevant animal models; (iv) the studies included target populations that used drugs to improve muscle strength and mass; and (v) the full texts of the studies were not available, and the significance of indicators was not known.
2.4. Study selection and data extraction
We assigned two researchers to blind-screene independently the literature and exclude the non-inclusion studies. From the remaining eligible studies, we extracted (i) the first author's name, (ii) the year of publication, (iii) clinical population characteristics, (iv) type, frequency, load, and duration of the LL-BFR rehabilitation program, and (v) outcome measures: muscle strength and size, physical function, and pain. All data were counted in the tables, with a focus on muscle mass. The risk of bias was evaluated using the Cochrane Handbook.13 The Dispute Division is handled by a third party.
2.5. Sensitivity analysis
All studies included in this review were subjected to sensitivity analysis, which included alterations to the analysis model, effect size selection, and case-by-case literature exclusion, and the meta-analysis was re-run.
2.6. Meta-analysis
One of the coauthors managed the data using Review Manager (RevMan) 5.4 (Cochrane Collaboration, 2020). Each unit was evaluated because the literature uses continuous outcome variables. The research's effect scale signifies standard mean differences (SMD). The data display initial to final values. The data were examined for study suppression using a random-effects model and the I2 statistic. I2 = 0 shows no heterogeneity between studies; I2 > 50% suggests heterogeneity. When heterogeneity was minimal, a fixed effects model analysis was performed; when heterogeneity was present, subgroup analysis was employed. p < 0.05 was determined to be statistically significant using forest plots to evaluate mean differences, and funnel plots were employed to analyze publication bias.
3. Results
3.1. Study selection
A total of 4 103 studies were found in databases, in which 14 studies met our inclusion criteria, after excluding review articles and non-randomized controlled trials (Fig. 1).
Fig. 1.
Flow diagram of study selection process.
3.2. Study characteristics
Table 1 contains the concluding information and data statistics for all included studies including older persons. The comparison between groups was made by comparing LL-BFR with HL-RT or LL-RT, with muscle mass and strength serving as common outcome markers.
Table 1.
Characteristics of the included studies.
| Study | Subjects | Age (years) | n (EG vs. CG) | Protocol | Intervention |
Indicators | Conclusion | ||
|---|---|---|---|---|---|---|---|---|---|
| Strength (% 1RM) | Duration (weeks) | Frequency | |||||||
| Bigdeli et al., 202057 | Older men | 66.7± 5.8 | 10 & 10 | LL-BFR & HL-RT | 25 - 35 & 50 - 70 | 6 | 3/week | Muscle strength | BFR exercise led to greater improvements in muscle mass index and functional performance in older men. |
| Cook et al., 201714 | Older adults | ≥ 65 | 12 & 12 | LL-BFR & HL-RT | 30 - 50 & 70 | 12 | 2/week | Muscle mass & Muscle strength | LL-BFR and HL-RT both led to increases in muscular strength and CSA. |
| Cook et al., 201915 | Older adults | 67–90 | 10 & 11 | LL-BFR & HL-RT | 30 & 70 | 12 | 2/week | Muscle mass & Muscle strength | Both HL-RT and LL-BFR boosted the KE and KF muscle groups' bulk and strength. |
| Karabulat et al., 200916 | Older men | 50–64 | 13 & 13 | LL-BFR & HL-RT | 20 & 80 | 6 | 3/week | Muscle strength | LL-BFR can improve leg muscle strength. |
| Kargaran et al., 202158 | Older women | 62.9± 3.1 | 8 &8 | LL-BFR & LL-RT | 20 - 30 & 45 | 8 | 3/week | Muscle strength | BFR should be considered as a training method to counteract the undesired changes associated with advancing age. |
| Letieri et al., 201817 | Older women | > 60 | 11 & 10/11 & 12 | LL-BFR & HL-RT/LL-BFR & LL-RT | 20 - 30 & 70–80/20–30 & ND | 12 | 2/week | Muscle strength | LL-BFR has similar effects to high-intensity training in enhancing muscle strength in older women. |
| Libardi et al., 201518 | Older adults | > 60 | 8 & 10 | LL-BFR & HL-RT | 20 - 30 & 70 - 80 | 12 | 2/week | Muscle mass & Muscle strength | BRF training may be an effective alternative to current exercise prescription recommendations for older adults. |
| Park et al., 202259 | Older women | > 65 | 10 & 10 | LL-BFR & HL-RT | 6 | 3/week | Muscle mass | BFR exercise has beneficial effects on leg muscle thickness and balance in older women with skeletal sarcopenia. | |
| Patterson et al., 201119 | Older adults | 62–73 | 10 & 10 | LL-BFR & LL-RT | 25 & 25 | 4 | 3/week | Muscle strength | After four weeks of LL-BFR training, the strength of older adults can increase even further. |
| Shimizu et al., 201620 | Older adults | > 65 | 20 & 20 | LL-BFR & LL-RT | 20 & 20 | 8 | 3/week | Muscle strength | LL-BFR resistance training increases muscle strength in aging adults who are physically fit. |
| Silva et al., 201560 | Older adults | 61.8 ±6.01 | 15 & 15 | LL-BFR & HL-RT | 30 & 80 | 12 | 2/week | Muscle mass | BFR can effectively improve the physical condition of the elderly. |
| Thiebaud et al., 201321 | Older women | 61 ± 5 | 8 & 6 | LL-BFR & HL-RT | 10 - 30 & 70 - 90 | 8 | 3/week | Muscle mass & Muscle strength | Similar to moderate to vigorous stretch training, LL-BFR increases pectoralis major strength and muscle thickness. |
| Vechin et al., 201522 | Older adults | 59–71 | 8 & 8 | LL-BFR & HL-RT | 20 - 30 & 70 - 80 | 12 | 2/week | Muscle mass & Muscle strength | The LL-BFR program is effective for increasing quadriceps mass and strength. |
| Yasuda et al., 201423 | Older women | 61–86 | 10 & 10 | LL-BFR & HL-RT | 35–45 & 70- 90 | 12 | 2/week | Muscle strength | LL-BFR is capable of significantly enhancing muscle strength. |
LL-BFR: low-load blood flow restriction; HL-RT: high-load resistance training; LL-RT: low-load resistance training; RM: repetition maximum; EG: experimental group; CG: controlled group; ND: no description.
3.3. Risk of bias in individual studies
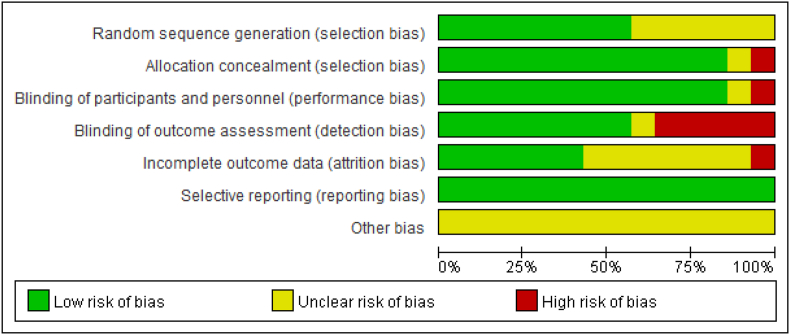
The bias risk graph (Fig. 2) and summary (Fig. 3) of this review: Random sequence generation posed 50% low risks, 50% unclear risks, and 0% high risk; allocation concealment posed 90% low risks, 1% unclear risks, and 0% high risks; blinding of participants and personnel posed 100% low risks, no unclear risks, and 0% high risks; and outcome assessment blinding posed 60% low risks, 40% unclear risks, and 0% high risks. (v) Forty percent of incomplete outcome data were low risks, sixty percent were unclear risks, and one was high risks; (vi) all selective reporting was low risks, there were no unclear risks, and there was no high risk; (vii) another bias was an unclear risk, there was no low risk, and there was no high risk.
Fig. 2.
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
Fig. 3.
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
3.4. Sensitivity analysis
The results of the sensitivity analysis did not change significantly, indicating the validity of this review.
3.5. Publication bias
Among the outcome indicators expressed in this review, there are only 10 studies on muscle strength in LL-BFR and HL-RT and therefore were made into a funnel plot (Fig. 4). We showed a symmetrical distribution of studies in the funnel plot, indicating that the studies included in this review had a low risk of bias and a high degree of confidence. However, the risk of bias could not be assessed because all other studies were less than 10.
Fig. 4.
Funnel plot of risk of bias analysis: Low-load blood flow restriction (LL-BFR) and (high-load resistance training) HL-RT for Muscle Strength.
3.6. Data analysis
3.6.1. LL-BFR versus HL-RT for muscle mass
Forest plot showed no heterogeneity between studies for comparison of LL-BFR to HL-RT in determining muscle mass (Fig. 5) (I2 = 0, p = 0.90, X2 = 1.58, df = 5), and combining effect sizes revealed that the results were not statistically significant (p = 0.74, Z = 0.34, SMD = 0.07, 95% CI: 0.33 to 0.46). A small number of combined studies prevented subgroup analysis.
Fig. 5.
Forest plot of comparison: Low-load blood flow restriction (LL-BRF) versus high-load resistance training (HL-RT) for Muscle Mass.
3.6.2. LL-BFR versus HL-RT for muscle strength
Forest plot demonstrated that muscle strength comparisons between LL-BFR and HL-RT reveal acceptable variability (I2 = 29%, p = 0.18, Chi2 = 12.63, df = 9), and the combined effect size showed a significant difference between the 2 groups (p = 0.03, Z = 2.16, SMD = -0.34, 95% CI: 0.65 to -0.03; Fig. 6). Fewer studies were pooled, preventing subgroup analysis.
Fig. 6.
Forest plot of comparison: Low-load blood flow restriction (LL-BFR) versus high-load resistance training (HL-RT) for Muscle Strength.
3.6.3. LL-BFR versus LL-RT for muscle strength
Uniform forest plots were produced to compare LL-BFR and LL-RT for determining muscle strength, (I2 = 0, p = 0.03, χ2 = 1.73) (Fig. 7), unlike LL-RT, LL-BFR showed no significant effect on muscle strength (p = 0.26, Z = 1.13, SMD = 0.25, 95% CI: 0.19 to 0.69). There was no subgroup analysis since fewer trials were merged.
Fig. 7.
Forest plot of comparison: Low-load blood flow restriction (LL-BFR) versus low-load resistance training (LL-RT) for Muscle Strength.
4. Discussion
This study investigated whether LL-BFR was as effective as HL-RT in increasing muscle mass and performance in an aged population. This review provided fundamental information about the included studies and assessed their literature quality, publication bias, and sensitivity. The conclusions of this review are dependable and valuable.
Although this review compared LL-BFR with HL-RT and LL-RT individually and examined it in terms of muscle mass and muscle strength, it did not compare LL-BFR with LL-RT to analyze muscle mass due to the limited number of included studies and the lack of data. Three further comparisons allow for the development of the ensuing debate.
4.1. LL-BFR versus HL-RT
The findings of this review are comparable to those of Centner et al. who reported a non-significant effect of LL-BFR compared to HL-RT on muscle mass, showing that the interventions had the same effects. This review differs from that of Centner et al. in collecting all trial data from beginning to end.6 All data were used for meta-analysis, which provides a comprehensive summary of the effects of LL-BFR and HL-RT on muscle mass and is advantageous for combining effect sizes. But they were unable to determine whether there was a publication bias analysis between the included studies, as a publication bias analysis must be reported by the funnel plot. Therefore, this would be uncritically more studies when producing the funnel plot for Revman 5.4, which prevents confounding. This systematic review extracted data for outcome markers exclusively for the endpoints, enhancing the credibility of the study and showing the publication bias of the funnel plot without altering the combined effect sizes.
Numerous studies have documented the effect of HL-RT on muscle growth. HL-RT is a practical, efficient, and safe training method for preventing sarcopenia in the elderly.24 An RCT in which senior participants were randomly assigned to groups revealed that an equivalent volume of moderate or high-intensity strength training increased muscle mass in the participants.25 In addition, a substantial amount of minimal dose resistance training for enhancing muscle mass, strength, and function was reviewed narratively through a review of the evidence and practical considerations, and the significant effects of HL-RT on muscle mass enhancement are summarized and reported here.26 In addition, a more comprehensive evaluation and meta-analysis have established the effect of HL-RT on muscle mass. For example, Schoenfeld et al. showed that heavy or high-intensity resistance training provides the greatest benefits for strength, whereas muscular hypertrophy can be obtained with a variety of loads.27 Based on the evidence presented here, a reasonable conclusion can be made that HL-RT can effectively increase muscle mass. This shows that both LL-BFR and HL-RT play an effective role in muscle mass in the elderly.
In contrast to the results described previously, this study found that LL-BFR significantly improved muscle strength compared to HL-RT. According to a randomized controlled trial,29 muscle strength does not decrease in the presence of other relevant exercise stimuli. LL-BFR may also contribute to rehabilitation efforts in adults over the age of 50, particularly in terms of improving muscle strength and function.30 All of the participants in the studies included in this review were older than 50 and yielded identical results.30 Therefore, this review's rigorous methodology lends credibility to its findings. In summary, both LL-BFR and HL-RT increased muscle mass, but LL-BFR significantly enhanced muscle strength.
4.2. LL-BFR versus LL-RT
On the basis of the data from the included studies, it was not possible to conduct a meta-analysis comparing the effect of LL-BFR and LL-RT on muscle mass. Nonetheless, this review showed that the difference between LL-BFR and LL-RT in terms of muscle strength was not statistically significant. Even though this review did not conduct a study in this area, it is easy to conclude that LL-BFR has a greater effect on muscle mass improvement than LL-RT based on the methodological analysis of the data included in the study based on this review and the conclusion that LL-BFR has a greater effect on muscle mass than HL-RT. And the difference between HH-LT and LL-RT in terms of muscle mass is also uncontroversial, as this finding has been reported in multiple studies. Lasevicius et al. and Ikezoe et al. both reported that HL-RT was more effective for increasing muscle mass. LL-BFR may have a greater impact on muscle mass than LL-RT.31,32
The forest plot demonstrates that LL-BFR and LL-RT have comparable effects on muscle strength. The results of current systematic reviews and meta-analyses are problematic. According to a systematic review, LL-BFR improved muscle strength more than LL-RT.10 However, the result is problematic according to the available systematic reviews and meta-analyses. In a systematic review, for instance, the superior effect of LL-BFR over LL-RT on muscle strength was reported, but the analysis of the results revealed relatively large heterogeneity between the included studies, which undermines the credibility of the meta-analysis. Although many sets of data were used for the analysis, they were all derived from only 2 RCTs, and these data were measured at different times between baseline and endpoint with the same subjects, preventing the included studies from being used for publication bias analysis and sensitivity analysis, indicating low confidence in the results.19,20 Although the above-mentioned two randomized controlled trials (RCTs) and one other study were included in this review and their endpoint results were extracted for the analysis, the results obtained in this review differed significantly from those of other systematic reviews. Differences in training time and frequency may have contributed to the contradictory results, so this aspect of the study requires further.
4.3. Mechanism of LL-BFR action on skeletal muscle
Understanding the effects of LL-BFR on increasing muscle strength is insufficient as one must also comprehend the mechanism of LL-action BFRs on muscle strength. According to a review, LL-BFR training improved muscle mass, appendicular skeletal muscle (ASM), grip strength, and isometric peak torque, particularly endothelial function, erythrocyte velocity, C-reactive protein concentration, and soluble intercellular adhesion molecule-1.28 In addition, endothelin-1 and oxidative stress increased after treatment of LI-BFR. These factors all encourage the development of muscle mass and muscular strength. The specific mechanisms are outlined below.
4.3.1. BFR stimulates growth hormone secretion
Growth hormone (GH) is stimulated to generate insulin-like growth factor (IGF-1), which regulates growth and metabolism and is a potent factor in skeletal muscle growth.47 It has been reported that GH levels were 290-fold higher after BFR compared to controls without flow restriction.48 LL-BFR with low-intensity resistance training promotes GH secretion.49 LL-BFR was effective in increasing GH, IGF-1, and testosterone levels in young men, which in turn increased muscle anabolic potential and increased cuff stress leading to higher levels of hormone secretion.50
4.3.2. BFR promotes muscle protein synthesis
The blood stasis caused by BFR training can lead to an increase in extracellular fluid and the accumulation of metabolites such as lactate, creating a pressure gradient that will drive fluid into muscle fibers, resulting in an increase in cell volume will alter cell structure and drive muscle protein synthesis - the mammalian rapamycin (mTOR) pathway.51 mTOR pathway is through S6 protein kinase (protein S6 kinase, S6K1) that stimulates muscle protein synthesis by phosphorylation.52 The fractional synthesis rate (FSR) of partial muscle protein synthesis increased by 46% 3 h after a round of BFR training. Thus, enhanced mTOR signaling may be an important cellular mechanism for BFR training-induced muscle hypertrophy.53
4.3.3. BFR increases fast muscle fiber recruitment
When the body is exercised, slow twitch fibers (ST) are recruited first and then fast twitch fibers (FT) are recruited as force increases.54 FT has a high anaerobic metabolic capacity and inorganic phosphate catabolism during BFRT, and FT recruitment is accompanied by a significant increase in mean peak amplitude and frequency of motor units and significant changes in surface muscle electrical power spectral parameters.55 It was reported that FT cross-sectional area increased by 27.6% in low-intensity BFRT, while ST increased by only 5.9% due to tissue hypoxia and susceptibility to fatigue.56
4.4. Practical significance
Physical function, muscle mass, and muscle strength all decline with age,33 and a rise in the incidence of sarcopenia can be ascribed to a decline in muscle mass and strength.2 China has unquestionably entered an aging society, resulting in a rise in the prevalence of sarcopenia in Chinese society.1 sarcopenia is capable of causing numerous diseases in the body,34 including an increased risk of falls and death,35,36 and the development and progression of cardiomyopathy diseases that may affect the elderly.37 For these potential conditions, specific interventions are necessary to mitigate the occurrences that may occur after sarcopenia. Physical activity has been suggested as a means of preventing sarcopenia, especially for patients with sarcopenia who need to develop resistance training under medical supervision.38 This review compares the high and low intensities of LL-BFR and resistance training, and the results can serve as a benchmark for the design of exercise prescriptions for patients with sarcopenia.
LL-BFR is superior to conventional resistance training. As was previously reported, LL-BFR is effective at reducing knee pain and preventing fluid storage, while having similar effects on skeletal muscle as HL-RT.9 This review also compared the effects of LL-BFR and resistance training on muscle mass and muscle strength using the obtained study results, which yielded benefits. In addition, LL-BFR has reportedly been applied to bone metabolism.39,40 In addition, if a patient is unable to perform traditional aerobic or resistance training due to weakness, athletic injury, or ongoing rehabilitation, BFR training has become an alternative intervention for these training modalities. BFR training can be used as a supplement to traditional training protocols to improve adaptation to training.41
To sum up the above, the findings of this meta-analysis may aid physicians in geriatrics and rehabilitation medicine in the treatment and prevention of sarcopenia, allowing patients to avoid the likelihood of adverse events associated with sarcopenia, which has an impact on clinical practice.
4.5. Strengths and limitations
This is the first systematic review and meta-analysis of the effects of BFR training on the skeletal muscles that references the requirements reported in AMSTAR 2 and PRISMA and is more standardized, and unlike other published systematic reviews, it included studies with less variation in baseline subject characteristics and conducted publication bias analysis and meta-analysis prior to sensitivity analyses.42,43 This review excluded studies that did not use blinding, which can increase the credibility of the results. Moreover, we excluded studies suspected to be from the same subject group, reducing the selection bias of subjects in the included studies. The data for each outcome indicator endpoint was chosen for analysis in this study based on the low variation in baseline subject characteristics, ensuring the dependability of the results. In addition, credible results were ensured by symmetric funnel plots and forest plots with low heterogeneity, in accordance with the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) entry.44
Nonetheless, this analysis has a couple of flaws. Few studies (n = 14) were retrieved for inclusion in this review, making it susceptible to publication bias, which is detrimental to the obtained results, it is also on this basis that funnel plots were abandoned to be drawn to test for publication bias between studies. In addition, the review was unable to perform subgroup analyses to determine the effects of LL-BFR versus LL-RT with different training durations and frequencies on muscle mass and muscle strength due to the limited number of included studies. In addition, the results of LL-BFR versus LL-RT for Muscle Mass were not obtained by this review analysis based on the obtained studies and data, which casts doubt on the veracity of the LL-BFR advantage. In addition, variability in the timing of training interventions included in the study may lead to bias.
5. Conclusion
In conclusion, both LL-BFR and traditional resistance training have some potential to improve sarcopenia in older adults, and they have similar improvements in muscle mass, but LL-BFR has greater improvements in muscle strength.
Submission statement
This article has not been published previously (except in abstract form or in published lectures or academic papers), is not being considered for publication elsewhere, has been approved by all authors, and is implicitly or explicitly the work of the responsible authorities; if accepted, it will not be published elsewhere, including electronically, in the same form, in English, or in any other language without the written permission of the copyright holder.
Authors’ contributions
In this systematic review, JK completed the registration, design, and primary draft for this systematic review, whereas LL and PZ were responsible for information retrieval, data extraction analysis, and discussion perspectives, and their disputes were arbitrated by ZL. Before submitting the article, SC and LZ determined the final results and data extraction to be included in the study and completed the final draft.
Conflict of interest
The authors claim that they have no competing interests.
Acknowledgements
We thank Dr. Xianfeng Yi for editing this manuscript language.
References
- 1.National Bureau of Statistics of China . National Bureau of Statistics of China; May 11, 2021. The Seventh National Population Census Main Data Situation.http://www.stats.gov.cn/tjsj/zxfb/202105/t20210510_1817176.html Accessed June 6, 2021. [Google Scholar]
- 2.Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50(5):889–896. doi: 10.1046/j.1532-5415.2002.50216.x. [DOI] [PubMed] [Google Scholar]
- 3.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019;393(10191):2636–2646. doi: 10.1016/S0140-6736(19)31138-9. [DOI] [PubMed] [Google Scholar]
- 4.Nascimento DDC, Rolnick N, Neto IVS, Severin R, Beal FLR. A useful blood flow restriction training risk stratification for exercise and rehabilitation. Front Physiol. 2022;13 doi: 10.3389/fphys.2022.808622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodrigues R, Ferraz RB, Kurimori CO, et al. Low-load resistance training with blood-flow restriction in relation to muscle function, mass, and functionality in women with rheumatoid arthritis. Arthritis Care Res. 2020;72(6):787–797. doi: 10.1002/acr.23911. [DOI] [PubMed] [Google Scholar]
- 6.Centner C, Zdzieblik D, Roberts L, Gollhofer A, König D. Effects of blood flow restriction training with protein supplementation on muscle mass and strength in older men. J Sports Sci Med. 2019;18(3):471–478. [PMC free article] [PubMed] [Google Scholar]
- 7.Lima-Soares F, Cholewa JM, de Araujo Pessôa K, et al. Blood flow restriction and blood flow restriction resistance training improves muscle mass, muscle strength and mobility in an older patient with osteoarthrosis carrying the ACTN3 endurance genotype: a case report. Geriatr Gerontol Int. 2019;19(5):458–459. doi: 10.1111/ggi.13634. [DOI] [PubMed] [Google Scholar]
- 8.Slysz JT, Boston M, King R, Pignanelli C, Power GA, Burr JF. Blood flow restriction combined with electrical stimulation attenuates thigh muscle disuse atrophy. Med Sci Sports Exerc. 2021;53(5):1033–1040. doi: 10.1249/MSS.0000000000002544. [DOI] [PubMed] [Google Scholar]
- 9.Hughes L, Rosenblatt B, Haddad F, et al. Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: a UK national health service randomised controlled trial. Sports Med. 2019;49(11):1787–1805. doi: 10.1007/s40279-019-01137-2. [DOI] [PubMed] [Google Scholar]
- 10.Centner C, Wiegel P, Gollhofer A, König D. Effects of blood flow restriction training on muscular strength and hypertrophy in older individuals: a systematic review and meta-analysis. Sports Med. 2019;49(1):95–108. doi: 10.1007/s40279-018-0994-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lixandrão ME, Ugrinowitsch C, Berton R, et al. Magnitude of muscle strength and mass adaptations between high-load resistance training versus low-load resistance training associated with blood-flow restriction: a systematic review and meta-analysis. Sports Med. 2018;48(2):361–378. doi: 10.1007/s40279-017-0795-y. [DOI] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339 doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10 doi: 10.1002/14651858.ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cook SB, LaRoche DP, Villa MR, Barile H, Manini TM. Blood flow restricted resistance training in older adults at risk of mobility limitations. Exp Gerontol. 2017;99:138–145. doi: 10.1016/j.exger.2017.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cook SB, Cleary CJ. Progression of blood flow restricted resistance training in older adults at risk of mobility limitations. Front Physiol. 2019;10:738. doi: 10.3389/fphys.2019.00738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karabulut M, Abe T, Sato Y, Bemben MG. The effects of low-intensity resistance training with vascular restriction on leg muscle strength in older men. Eur J Appl Physiol. 2010;108(1):147–155. doi: 10.1007/s00421-009-1204-5. [DOI] [PubMed] [Google Scholar]
- 17.Letieri RV, Teixeira AM, Furtado GE, Lamboglia CG, Rees JL, Gomes BB. Effect of 16 weeks of resistance exercise and detraining comparing two methods of blood flow restriction in muscle strength of healthy older women: a randomized controlled trial. Exp Gerontol. 2018;114:78–86. doi: 10.1016/j.exger.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 18.Libardi CA, Chacon-Mikahil MP, Cavaglieri CR, et al. Effect of concurrent training with blood flow restriction in the elderly. Int J Sports Med. 2015;36(5):395–399. doi: 10.1055/s-0034-1390496. [DOI] [PubMed] [Google Scholar]
- 19.Patterson SD, Ferguson RA. Enhancing strength and postocclusive calf blood flow in older people with training with blood-flow restriction. J Aging Phys Activ. 2011;19(3):201–213. doi: 10.1123/japa.19.3.201. [DOI] [PubMed] [Google Scholar]
- 20.Shimizu R, Hotta K, Yamamoto S, et al. Low-intensity resistance training with blood flow restriction improves vascular endothelial function and peripheral blood circulation in healthy elderly people. Eur J Appl Physiol. 2016;116(4):749–757. doi: 10.1007/s00421-016-3328-8. [DOI] [PubMed] [Google Scholar]
- 21.Thiebaud RS, Loenneke JP, Fahs CA, et al. The effects of elastic band resistance training combined with blood flow restriction on strength, total bone-free lean body mass and muscle thickness in postmenopausal women. Clin Physiol Funct Imag. 2013;33(5):344–352. doi: 10.1111/cpf.12033. [DOI] [PubMed] [Google Scholar]
- 22.Vechin FC, Libardi CA, Conceição MS, et al. Comparisons between low-intensity resistance training with blood flow restriction and high-intensity resistance training on quadriceps muscle mass and strength in elderly. J Strength Cond Res. 2015;29(4):1071–1076. doi: 10.1519/JSC.0000000000000703. [DOI] [PubMed] [Google Scholar]
- 23.Yasuda T, Fukumura K, Tomaru T, Nakajima T. Thigh muscle size and vascular function after blood flow-restricted elastic band training in older women. Oncotarget. 2016;7(23):33595–33607. doi: 10.18632/oncotarget.9564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lichtenberg T, von Stengel S, Sieber C, Kemmler W. The favorable effects of a high-intensity resistance training on sarcopenia in older community-dwelling men with osteosarcopenia: the randomized controlled FrOST study. Clin Interv Aging. 2019;14:2173–2186. doi: 10.2147/CIA.S225618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Létocart AJ, Mabesoone F, Charleux F, et al. Muscles adaptation to aging and training: architectural changes - a randomised trial. BMC Geriatr. 2021;21(1):48. doi: 10.1186/s12877-020-02000-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fyfe JJ, Hamilton DL, Daly RM. Minimal-dose resistance training for improving muscle mass, strength, and function: a narrative review of current evidence and practical considerations. Sports Med. 2022;52(3):463–479. doi: 10.1007/s40279-021-01605-8. [DOI] [PubMed] [Google Scholar]
- 27.Schoenfeld BJ, Grgic J, Ogborn D, Krieger JW. Strength and hypertrophy adaptations between low- vs. High-load resistance training: a systematic review and meta-analysis. J Strength Cond Res. 2017;31(12):3508–3523. doi: 10.1519/JSC.0000000000002200. [DOI] [PubMed] [Google Scholar]
- 28.Lopes KG, Bottino DA, Farinatti P, et al. Strength training with blood flow restriction - a novel therapeutic approach for older adults with sarcopenia? A case report. Clin Interv Aging. 2019;14:1461–1469. doi: 10.2147/CIA.S206522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teixeira EL, de Salles Painelli V, Silva-Batista C, et al. Blood flow restriction does not attenuate short-term detraining-induced muscle size and strength losses after resistance training with blood flow restriction. J Strength Cond Res. 2021;35(8):2082–2088. doi: 10.1519/JSC.0000000000003148. [DOI] [PubMed] [Google Scholar]
- 30.Baker BS, Stannard MS, Duren DL, Cook JL, Stannard JP. Does blood flow restriction therapy in patients older than age 50 result in muscle hypertrophy, increased strength, or greater physical function? A systematic review. Clin Orthop Relat Res. 2020;478(3):593–606. doi: 10.1097/CORR.0000000000001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lasevicius T, Ugrinowitsch C, Schoenfeld BJ, et al. Effects of different intensities of resistance training with equated volume load on muscle strength and hypertrophy. Eur J Sport Sci. 2018;18(6):772–780. doi: 10.1080/17461391.2018.1450898. [DOI] [PubMed] [Google Scholar]
- 32.Ikezoe T, Kobayashi T, Nakamura M, Ichihashi N. Effects of low-load, higher-repetition vs. High-load, lower-repetition resistance training not performed to failure on muscle strength, mass, and echo intensity in healthy young men: a time-course study. J Strength Cond Res. 2020;34(12):3439–3445. doi: 10.1519/JSC.0000000000002278. [DOI] [PubMed] [Google Scholar]
- 33.Shur NF, Creedon L, Skirrow S, et al. Age-related changes in muscle architecture and metabolism in humans: the likely contribution of physical inactivity to age-related functional decline. Ageing Res Rev. 2021;68 doi: 10.1016/j.arr.2021.101344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilburn D, Ismaeel A, Machek S, Fletcher E, Koutakis P. Shared and distinct mechanisms of skeletal muscle atrophy: a narrative review. Ageing Res Rev. 2021;71 doi: 10.1016/j.arr.2021.101463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52(7):1121–1129. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- 36.Cooper R, Kuh D, Hardy R. Mortality Review Group; FALCon and HALCyon Study Teams. Objectively measured physical capability levels and mortality: systematic review and meta-analysis. BMJ. 2010;341 doi: 10.1136/bmj.c4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yarasheski KE. Exercise, aging, and muscle protein metabolism. J Gerontol A Biol Sci Med Sci. 2003;58(10):M918–M922. doi: 10.1093/gerona/58.10.m918. [DOI] [PubMed] [Google Scholar]
- 38.Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS) Age Ageing. 2014;43(6):748–759. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bittar ST, Pfeiffer PS, Santos HH, Cirilo-Sousa MS. Effects of blood flow restriction exercises on bone metabolism: a systematic review. Clin Physiol Funct Imag. 2018 doi: 10.1111/cpf.12512. [published online ahead of print, 2018 Mar 2] [DOI] [PubMed] [Google Scholar]
- 40.Nascimento DDC., Petriz B, Oliveira SDC., et al. Effects of blood flow restriction exercise on hemostasis: a systematic review of randomized and non-randomized trials. Int J Gen Med. 2019;12:91–100. doi: 10.2147/IJGM.S194883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freitas EDS, Karabulut M, Bemben MG. The evolution of blood flow restricted exercise. Front Physiol. 2021;12 doi: 10.3389/fphys.2021.747759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358 doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339 doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr. 1997;127(5 Suppl):990S–991S. doi: 10.1093/jn/127.5.990S. [DOI] [PubMed] [Google Scholar]
- 46.Chen LK, Liu LK, Woo J, et al. Sarcopenia in asia: consensus report of the asian working group for sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101. doi: 10.1016/j.jamda.2013.11.025. [DOI] [PubMed] [Google Scholar]
- 47.Kim H, Barton E, Muja N, Yakar S, Pennisi P, Leroith D. Intact insulin and insulin-like growth factor-I receptor signaling is required for growth hormone effects on skeletal muscle growth and function in vivo. Endocrinology. 2005;146(4):1772–1779. doi: 10.1210/en.2004-0906. [DOI] [PubMed] [Google Scholar]
- 48.Takarada Y, Nakamura Y, Aruga S, Onda T, Miyazaki S, Ishii N. Rapid increase in plasma growth hormone after low-intensity resistance exercise with vascular occlusion. J Appl Physiol (1985) 2000;88(1):61–65. doi: 10.1152/jappl.2000.88.1.61. [DOI] [PubMed] [Google Scholar]
- 49.Sharifi S, Monazzami A, Nikousefat Z, Heyrani A, Yari K. The acute and chronic effects of resistance training with blood flow restriction on hormonal responses in untrained young men: a comparison of frequency. Cell Mol Biol (Noisy-le-grand) 2020;66(1):1–8. [PubMed] [Google Scholar]
- 50.Yinghao L, Jing Y, Yongqi W, et al. Effects of a blood flow restriction exercise under different pressures on testosterone, growth hormone, and insulin-like growth factor levels. J Int Med Res. 2021;49(9) doi: 10.1177/03000605211039564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fry CS, Glynn EL, Drummond MJ, et al. Blood flow restriction exercise stimulates mTORC1 signaling and muscle protein synthesis in older men. J Appl Physiol (1985) 2010;108(5):1199–1209. doi: 10.1152/japplphysiol.01266.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fujita S, Abe T, Drummond MJ, et al. Blood flow restriction during low-intensity resistance exercise increases S6K1 phosphorylation and muscle protein synthesis. J Appl Physiol (1985) 2007;103(3):903–910. doi: 10.1152/japplphysiol.00195.2007. [DOI] [PubMed] [Google Scholar]
- 53.Dreyer HC, Fujita S, Cadenas JG, Chinkes DL, Volpi E, Rasmussen BB. Resistance exercise increases AMPK activity and reduces 4E-BP1 phosphorylation and protein synthesis in human skeletal muscle. J Physiol. 2006;576(Pt 2):613–624. doi: 10.1113/jphysiol.2006.113175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Loenneke JP, Wilson GJ, Wilson JM. A mechanistic approach to blood flow occlusion. Int J Sports Med. 2010;31(1):1–4. doi: 10.1055/s-0029-1239499. [DOI] [PubMed] [Google Scholar]
- 55.Suga T, Okita K, Morita N, et al. Intramuscular metabolism during low-intensity resistance exercise with blood flow restriction. J Appl Physiol (1985) 2009;106(4):1119–1124. doi: 10.1152/japplphysiol.90368.2008. [DOI] [PubMed] [Google Scholar]
- 56.Abe T, Kearns CF, Sato Y. Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. J Appl Physiol (1985) 2006;100(5):1460–1466. doi: 10.1152/japplphysiol.01267.2005. [DOI] [PubMed] [Google Scholar]
- 57.Bigdeli S, Dehghaniyan MH, Amani-Shalamzari S, Rajabi H, Gahreman DE. Functional training with blood occlusion influences muscle quality indices in older adults. Arch Gerontol Geriatr. 2020;90 doi: 10.1016/j.archger.2020.104110. [DOI] [PubMed] [Google Scholar]
- 58.Kargaran A, Abedinpour A, Saadatmehr Z, Yaali R, Amani-Shalamzari S, Gahreman D. Effects of dual-task training with blood flow restriction on cognitive functions, muscle quality, and circulatory biomarkers in elderly women. Physiol Behav. 2021;239 doi: 10.1016/j.physbeh.2021.113500. [DOI] [PubMed] [Google Scholar]
- 59.Park JC, Mun D, Choi SJ. Effects of blood flow restriction exercise on leg muscle thickness and balance in elderly women with sarcopenia. PNF and Movement. 2022;20(1):1–8. doi: 10.21598/JKPNFA.2022.20.1.1. [DOI] [Google Scholar]
- 60.Silva J, Neto GR, Freitas E, et al. Chronic effect of strength training with blood flow restriction on muscular strength among women with osteoporosis. J Exerc Physiol Online. 2014;18(4):33–41. [Google Scholar]
- 61.Rodrigues F, Domingos C, Monteiro D, Morouço P. A review on aging, sarcopenia, falls, and resistance training in community-dwelling older adults. Int J Environ Res Publ Health. 2022;19(2):874. doi: 10.3390/ijerph19020874. [DOI] [PMC free article] [PubMed] [Google Scholar]