Abstract
Introduction
Uddanam is an agricultural area with a high burden of chronic kidney disease of unknown etiology (CKDu). Despite reports of many deaths due to CKD in the lay press, the exact contribution of CKD to deaths remains uncertain because most deaths occur outside medical care.
Methods
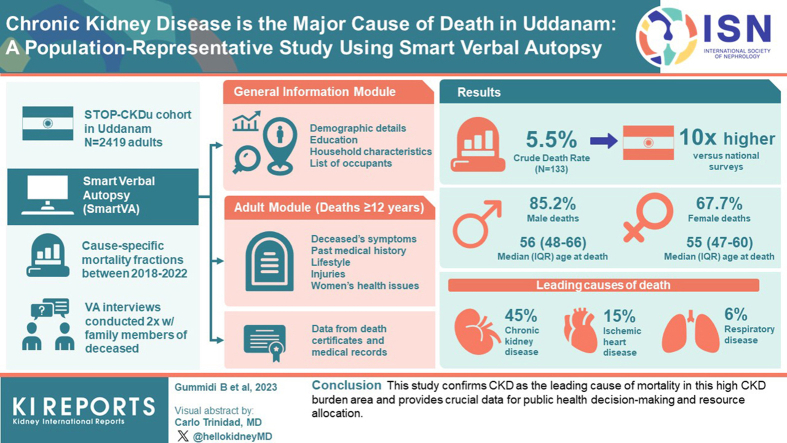
We used SmartVA automated verbal autopsy tool to ascertain the cause-specific mortality fractions among a 2419 subject-strong general population cohort of adult subjects in Uddanam between 2018 and 2022. Verbal autopsy interviews were conducted twice with the family members of the deceased.
Results
A total of 133 deaths were recorded, giving a crude death rate of 5.5%, 10 times higher than that recorded in national surveys. CKD was responsible for 45% of all deaths, followed by ischemic heart disease (15%) and respiratory disease (6%).
Conclusion
This study confirms CKD as the leading cause of mortality in this high CKD burden area and provides crucial data for public health decision-making and resource allocation.
Keywords: cause of death, chronic kidney disease, CKD of unknown etiology, SmartVA, uddanam nephropathy, verbal autopsy
Graphical abstract
See Commentary on Page 10
CKD is the third fastest growing cause of death (COD) worldwide and is projected to rise in the rank of CODs from 16th in 2016 to 5th by 2040 .1 The greatest increases in CKD deaths are forecast in low and lower-middle-income countries. In India, from 2001–2003 to 2011–2013, there was a 50% increase in the contribution of CKD to all deaths among persons aged 15 to 69 year.2 COD reporting is problematic in many jurisdictions, including India, and the Global Burden of Disease study has admitted to having a high proportion of garbage codes (codes that are not useful for public health analysis) in ascertaining a CKD diagnosis.3 Many deaths occur at home for which the COD is either not reported at all or reported by untrained persons.4 Only 22.3% of the total registered deaths in 2020 were medically certified.4 Therefore, the true contribution of various conditions to deaths remains uncertain. Tools such as verbal autopsy have been used to reduce this uncertainty.5
Population clusters with higher than usual prevalence of CKD not associated with traditional risk factors such as diabetes, hypertension, and other known etiological categories have been reported in many parts of the world. This CKDu is mostly encountered among rural agricultural communities.6 One such region is in the coastal district of Srikakulam in Andhra Pradesh, India, known as Uddanam (population 5.5 million).7 The age-adjusted and sex-adjusted prevalence of CKD in this area is estimated at 18% to 22%,8,9 2.5 to 3.3 times higher than the population prevalence of CKD reported from other regions of India.10
More than 4500 deaths due to kidney disease were reported in Uddanam in the lay press in 2015.9 However, there has been no formal ascertainment of the COD in this population, which is critical for gaining actionable insights. We conducted this study to ascertain the cause-specific mortality fractions to overcome the key data gap in COD estimates using the SmartVA automated verbal autopsy tool11 in a population-based cohort of adults in Uddanam.
Methods
This population-representative study was conducted in Uddanam as part of an ongoing research program, the Study to Test and Operationalize Preventive Approaches for Chronic Kidney Disease of Undetermined Etiology (STOP-CKDu), the details of which are published elsewhere.8,12 The study established a general population-based cohort of adult subjects in July 2018 using a cluster sample technique, and the participants are being followed-up with to determine the incidence and risk factors for kidney disease progression.
All households included in the study were surveyed between 2018 and 2022 to create a mortality list through active community surveillance. After obtaining verbal consent from the family members, health workers scheduled an appointment for a verbal autopsy interview. The primary informants for the interviews were the deceased's closest relatives. The George Institute Ethics Committee approved the study.
We used SmartVA, a computerized algorithm validated by Population Health Metrics and Research Consortium in various settings and included in World Health Organization 2022 questionnaire. The tool has been developed to interpret data from interviews conducted with family members or caregivers of a deceased individual using a set of standardized questions to collect information about the signs, symptoms, and circumstances of the individual's death and applies an automated algorithm to assign a probable COD based on the collected data.13,14 There are 3 age-specific modules and a general information module in the SmartVA questionnaire: neonatal fatalities (from birth to 28 days), child deaths (from 29 days up to 11 years), and adult deaths (from 12 years and older). We used the adult deaths module for this study. The general information module collects data about the decedent's demographic details, education, household characteristics, and a list of their occupants. The adult module gathers information on the deceased's symptoms, past medical history, lifestyle (smoking and alcohol intake), injuries, and women's health issues if the deceased were a female. In addition, it transcribes data from death certificates and available medical records. We used modified Kuppuswamy scale to assess the socioeconomic status of the participants (Supplementary Material). This scale considers 3 key parameters: the education and occupation of the participant, as well as the total income derived from all sources within the family.
Verbal Autopsy Interview and Quality Maintenance
A trained interviewer collected data on android phones using a questionnaire developed by the Population Health Metrics and Research Consortium, translated into local language (Telugu) and implemented with the Open Data Kit software suite.15
Household members (aged 18 and older) who had cared for the deceased or were familiar with the illness were interviewed in-person. If medical records were accessible, the interviewee was asked to provide a transcription of the medical record’s most recent summary. If a death certificate was provided, the interviewer was asked to note the reason for death as listed on the certificate.
Interviews lasted an average of 25 to 30 minutes, with a further 3 to 5 minutes required for the open narrative section. The completed questionnaires were saved on the tablets and transmitted to a central database following verification. To ensure the highest quality data were collected, this questionnaire was administered twice over 3 months by 2 independent, trained interviewers.
Data Analysis
The data were exported from Open Data Kit Collect using the Open Data Kit Briefcase tool as comma separated value files and uploaded into the SmartVA program, which assigns individual COD by using the Tariff Method 2.0 method,15,16 which uses an additive algorithm that assigns weights or scores to symptoms and signs reported during a verbal autopsy interview. These scores are based on their associations with different causes of death. The cumulative score for a particular set of symptoms and signs helps determine the most likely COD for the individual. In the few instances where symptoms were vague, contradictory, or mutually inconsistent, SmartVA could not determine the COD, and as a result, these deaths were deemed undetermined. Cohen’s kappa statistic (κ) was used to compare the agreement proportions between interviews.
COD Assignment
If the SmartVA-generated COD assignment matched between the 2 interviewers, it was considered the final COD. All unmatched results were reviewed by a trained, unbiased physician who had access to the decedent’s verbal autopsy narratives and medical records. Assessment of the physician was considered the final COD in the case of unmatched records (Figure S1).
Results
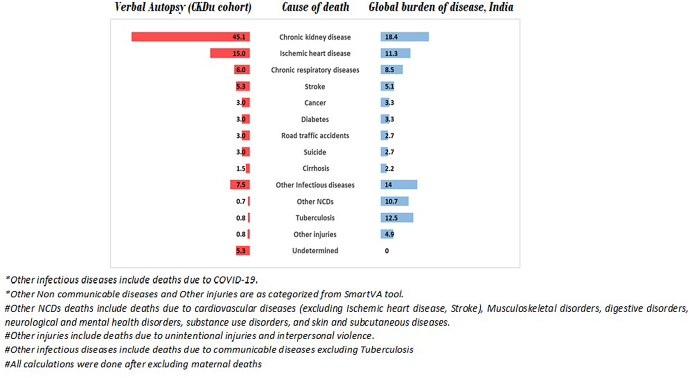
The STOP-CKDu cohort consisted of 2419 adult participants (Table 1). During a median follow-up of 3.9 years, there were 133 deaths (crude death rate 5.5%). A total of 100 (85.2%) were males, and 90 (67.7%) belonged to the lower-middle socioeconomic group. The median (interquartile range) age at death in the sample was 56 (48–66) and 55 (47–60) years for males and females, respectively. A total of 106 deaths were reported at home; the number was higher among females (87.9%) than males (77%). Cause specific mortality fraction from the STOP-CKDu cohort and global burden of disease estimates are depicted in Figure 1. CKD and chronic respiratory diseases were more prevalent in the study population, whereas burden of deaths due to neoplasm and TB was higher at the national level. Age-specific death rates from the STOP-CKDu cohort compared with vital statistics death rate of Andhra Pradesh are summarized in Supplementary Table S1. There was a high level of agreement between the COD determined in the 2 independent interviews (86.5%), with a Cohen’s kappa (κ) statistic score of 0.85.
Table 1.
Sociodemographic characteristics of the entire cohort and the deceased population
| Characteristics |
Entire Cohort |
Deceased Population |
||
|---|---|---|---|---|
| Variables | Male | Female | Male | Female |
| Number of cases | 1193 | 1226 | 100 | 33 |
| Age (yrs) | ||||
| 18–30 | 156 (13.1) | 169 (13.8) | 2 (2) | 0 |
| 31–40 | 242 (20.3) | 326 (26.6) | 3 (3) | 3 (9.1) |
| 41–50 | 318 (26.7) | 343 (28.0) | 19 (19) | 8 (24.2) |
| 51–60 | 267 (22.4) | 244 (19.9) | 25 (25) | 11 (33.3) |
| >60 | 210 (17.6) | 144 (11.8) | 51 (51) | 11 (33.3) |
| Level of education | ||||
| College | 400 (33.5) | 194 (15.8) | 15 (15) | 2 (6.1) |
| Attended school | 487 (40.8) | 411 (33.5) | 43 (43) | 9 (27.3) |
| No formal education | 306 (25.7) | 621 (50.7) | 42 (42) | 22 (66.7) |
| Occupation | ||||
| Not working | 80 (6.7) | 342 (27.9) | 7 (7) | 6 (18.2) |
| Sedentary workers | 116 (9.7) | 53 (4.3) | 4 (4) | 5 (15.2) |
| Manual workers/farmers | 997 (83.6) | 831 (67.8) | 89 (89) | 22 (66.7) |
| Socio-economic status | ||||
| Lower middle | 515 (43.2) | 856 (69.8) | 64 (64) | 26 (78.8) |
| Upper lower | 677 (56.8) | 370 (30.2) | 36 (36) | 36 (21.2) |
| Medical history (yes) | ||||
| Diabetes | 186 (7.7) | 131 (5.4) | 28 (21.1) | 2 (1.5) |
| Hypertension | 408 (16.8) | 312 (12.9) | 60 (45.1) | 22 (16.5) |
| Longstanding hypertension (≥5 yrs) | 95 (3.9) | 66 (2.7) | 22 (16.5) | 6 (4.5) |
| Heart disease | 138 (5.7) | 111 (4.6) | 24 (18.1) | 2 (1.5) |
| CKD | 299 (12.4) | 209 (8.7) | 59 (44.4) | 19 (14.3) |
| Place of death | ||||
| Home | 77 (77) | 29 (87.9) | ||
| Hospital | 23 (23) | 4 (12.1) | ||
Figure 1.
Cause-specific mortality fractions for leading causes of death from verbal autopsy data in the STOP-CKDu cohort, Uddanam region (N = 133) compared with Global Burden of Disease estimates for India (age >20 years).
The 15 leading COD by sex, before and after redistribution of undetermined causes are reported in Table 2. Tariff assigned a specific COD for 94.7% of deaths, with the COD being undetermined in approximately 5.3% of cases. The leading COD was CKD in 60 (45.1%), followed by ischemic heart disease (20, 15%), respiratory disease (8, 6%), and stroke (7, 5.3%). The COD distribution was similar between males and females. Table 3 shows the characteristics of the persons who died of CKD and those due to other causes among the cohort.
Table 2.
Leading cause-specific mortality fractions for all verbal autopsy deaths
| Cause of death | Males | Females | Total |
|---|---|---|---|
| Chronic kidney disease | 43 (43) | 17 (51.5) | 60 (45.1) |
| Ischemic heart disease | 14 (14) | 6 (18.2) | 20 (15) |
| Chronic respiratory disorders | 7 (7) | 1 (3.0) | 8 (6.0) |
| COVID-19 | 8 (8) | 0 | 8 (6) |
| Stroke | 4 (4) | 3 (9.0) | 7 (5.3) |
| Undetermined | 4 (4) | 4 (12.1) | 7 (5.3) |
| Neoplasm | 4 (4) | 0 | 4 (3) |
| Diabetes | 4 (4) | 0 | 4 (3) |
| Transport accidents | 4 (4) | 0 | 4 (3) |
| Suicide | 3 (3) | 1 (9.0) | 4 (3) |
| Cirrhosis | 2 (2) | 0 | 2 (1.5) |
| Other infectious diseases | 1 (1) | 1 (3.0) | 2 (1.5) |
| Other injuries | 1 (1) | 0 | 1 (0.8) |
| Other NCDs | 0 | 1 (3.0) | 1 (0.8) |
| TB | 1 (1) | 0 | 1 (0.8) |
| Total | 100 (75.2) | 33 (24.8) | 133 (100) |
NCDs, non-communicable diseases; TB, tuberculosis.
Table 3.
Characteristics of the persons who died of CKD versus non-CKD among the cohort
| Variables | CKD death (n = 60) | Non-CKD deaths (n = 73) |
|---|---|---|
| Gender | ||
| Male | 43 (71.7) | 57 (78.1) |
| Female | 17 (28.3) | 16 (21.9) |
| Age (yrs) | ||
| 18–30 | 0 (0) | 2 (2.7) |
| 31–40 | 5 (8.3) | 6 (6.8) |
| 41–50 | 11 (18.3) | 18 (24.6) |
| 51–60 | 18 (30) | 21 (28.7) |
| >60 | 26 (43.3) | 37 (36.9) |
| Level of education | ||
| College | 3 (5) | 14 (19.2) |
| Attended school | 37 (61.7) | 27 (37) |
| No formal education | 20 (33.3) | 32 (43.8) |
| Occupation | ||
| Not working | 52 (86.7) | 59 (80.8) |
| Sedentary workers | 5 (8.3) | 8 (11) |
| Manual workers/farmers | 3 (5) | 6 (8.2) |
| Socio-economic status | ||
| Lower middle | 46 (76.7) | 44 (60.3) |
| Upper lower | 14 (23.3) | 29 (39.7) |
| Medical history (yes) | ||
| Diabetes | 7 (5.3) | 15 (11.3) |
| Hypertension | 37 (61.7) | 41 (56.7) |
| Longstanding hypertension (≥5 yrs) | 11(18.3) | 17 (23.3) |
| Heart disease | 12 (20) | 14 (19.2) |
| CKD | 35 (58.3) | 11 (15.1) |
| Place of death | ||
| Home | 53 (88.3) | 53 (72.6) |
| Hospital | 7 (11.7) | 20 (27.4) |
CKD, chronic kidney disease.
Discussion
This first-of-its-kind study confirms CKD as the dominant COD in this rural agricultural population, long identified as a high CKD prevalence area. The proportion of individuals with CKD as the COD was significantly greater than that reported from the global burden of disease estimates for the state. In addition, the annual all-cause and sex-specific mortality rates were nearly 10 times higher than that documented in the sample registration survey report for Andhra Pradesh17 among adults of age 20 years and older. The COD ascertainment was made with high confidence because the data were collected twice by independent interviewers, and any disagreements resolved by an independent physician.
Our study showed an alarmingly high proportion of CKD deaths in this community. The burden of CKD mortality is more than the national and state average (2.37% and 2.08% of total deaths, respectively), and the neighboring states that report CKDu clusters, such as Tamil Nadu (5.16%), Kerala (4.89%), Goa (3.66%), and West Bengal (2.97%). The high burden of CKD deaths could be related to poor access to care pathways.18
High mortality burden among communities with high CKDu burden is also reported from Central America (60–70/100,000 population)19,20 and Sri Lanka (67.6% of total deaths).21 This high burden of CKD cases and associated mortality underscore the need for systematic efforts to establish the cause of CKDu and generate evidence on locally acceptable and scalable primary and secondary preventative strategies.
We used an automated tool for COD assessment, SmartVA. High reliability scores for COD ascertainment were observed from existing studies using similar tools in community settings of Uganda,22 Indonesia,23 China,24 and Philippines.25 Our finding of favorable agreement scores, the minimal proportion of undermined deaths, and low disagreement rate between the 2 interviewers indicate SmartVA can generate high-quality verbal autopsy data in rural settings and has the potential to be used as a tool for medical certification of deaths in community settings.26 These findings have implications for improving the quality of death reporting from rural communities which is vital for developing meaningful policies.
Working collaboratively with trained staff and supplementing the COD results with adjudication from an independent physician are the principal strengths of our work. The proportion of undetermined deaths was minimal, indicating a high quality of verbal autopsy narratives, which was achieved by adequately training the investigators, utilizing medical records, and using an automated verbal autopsy method. The limitations include the lack of a comparator for verbal autopsy records collected solely by the SmartVA tool. The delay between the time of death and verbal autopsy interviews might have introduced a recall bias, especially where the interval was relatively long. In addition, given that CKD is endemic in the region, the families could have inappropriately attributed the deaths to CKD. The latter was minimized by collecting comprehensive medical information, verifying the informant’s narratives with medical records, and conducting the interviews twice by independent interviewers. Furthermore, our study was not powered enough to estimate any association or generate a hypothesis of no causal inference; therefore, these findings should be confirmed in larger studies. Lastly, factors associated with lower mortality rates for deaths attributable to tuberculosis and neoplasm in STOP-CKDu cohorts need to be explored further.
In conclusion, using a validated automated verbal autopsy tool, this population-based study provides accurate information on cause-specific mortality rates for the adult population of the Uddanam region. The burden of mortality attributable to CKD is high, which indicates that policymakers need to address this concern and develop region-specific policies to prevent and manage CKD through prompt and accurate screening and diagnosis of CKD cases. Equally important would be to act on improving community awareness of the significance of early diagnosis and management.
Disclosure
VJ has received grant funding from GSK, Baxter Healthcare, and Biocon and honoraria from Bayer, AstraZeneca, Boehringer Ingelheim, NephroPlus, and Zydus Cadilla, under the policy of all honoraria being paid to the organization. All the other authors have declared no competing interest.
Acknowledgments
The Open Access Fees was paid from the Imperial College London Open Access Funds.
Footnotes
Figure S1. Data collection flow.
Table S1. Age and sex disaggregated mortality data of Andhra Pradesh and STOP-CKDu study.
Population Health Metrics and Research Consortium General module.
Population Health Metrics and Research Consortium shortened verbal autopsy questionnaire adult verbal autopsy module.
Modified Kuppuswamy classification, socio economic status scale.
Supplementary Material
Figure S1. Data collection flow.
Table S1. Age and sex disaggregated mortality data of Andhra Pradesh and STOP-CKDu study.
Population Health Metrics and Research Consortium General module.
Population Health Metrics and Research Consortium shortened verbal autopsy questionnaire adult verbal autopsy module.
Modified Kuppuswamy classification, socio economic status scale.
References
- 1.Bikbov B., Purcell C.A., Levey A.S. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–733. doi: 10.1016/S0140-6736(20)30045-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dare A.J., Fu S.H., Patra J., et al. Renal failure deaths and their risk factors in India 2001-13: nationally representative estimates from the Million Death Study. Lancet Glob Health. 2017;5:e89–e95. doi: 10.1016/S2214-109X(16)30308-4. [DOI] [PubMed] [Google Scholar]
- 3.Johnson S.C., Cunningham M., Dippenaar I.N., et al. Public health utility of cause of death data: applying empirical algorithms to improve data quality. BMC Med Inform Decis Mak. 2021;21:175. doi: 10.1186/s12911-021-01501-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Annual report on medical certification of cause of death, 2020. Office of the Registrar General & Census Commissioner India. Published 2020. https://censusindia.gov.in/nada/index.php/catalog/42681
- 5.WHO. Verbal autopsy standards: the 2016 WHO verbal autopsy instrument. Published 2016. https://score.tools.who.int/tools/count-births-deaths-and-causes-of-death/tool/verbal-autopsy-standards-the-2016-who-verbal-autopsy-instrument-23/
- 6.John O., Gummudi B., Jha A., et al. Chronic kidney disease of unknown etiology in India: what do we know and where do we need to go. Kidney Int Rep. 2021;6:2743–2751. doi: 10.1016/j.ekir.2021.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tatapudi R.R., Rentala S., Gullipalli P., et al. High prevalence of CKD of unknown etiology in Uddanam, India. Kidney Int Rep. 2019;4:380–389. doi: 10.1016/j.ekir.2018.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gummidi B., John O., Ghosh A., et al. A systematic study of the prevalence and risk factors of CKD in Uddanam, India. Kidney Int Rep. 2020;5:2246–2255. doi: 10.1016/j.ekir.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.No end to agony of kidney patients in Uddanam region. Hindu. Published 2015. https://www.thehindu.com/news/national/andhra-pradesh/no-end-to-agony-of-kidney-patients-in-uddanam-region/article6992310.ece
- 10.Anand S., Shivashankar R., Ali M.K., et al. Prevalence of chronic kidney disease in two major Indian cities and projections for associated cardiovascular disease. Kidney Int. 2015;88:178–185. doi: 10.1038/ki.2015.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Serina P., Riley I., Stewart A., et al. Improving performance of the Tariff Method for assigning causes of death to verbal autopsies. BMC Med. 2015;13:291. doi: 10.1186/s12916-015-0527-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.John O., Gummidi B., Tewari A., et al. Study to Test and operationalize preventive approaches for CKD of undetermined etiology in Andhra Pradesh, India. Kidney Int Rep. 2019;4:1412–1419. doi: 10.1016/j.ekir.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murray C.J., Lopez A.D., Black R., et al. Population Health Metrics Research Consortium gold standard verbal autopsy validation study: design, implementation, and development of analysis datasets. Popul Health Metr. 2011;9:27. doi: 10.1186/1478-7954-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart J.D., de André P.A., de André C.D.S., et al. Validation of SmartVA using conventional autopsy: a study of adult deaths in Brazil. Lancet Reg Health Am. 2022;5 doi: 10.1016/j.lana.2021.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.IHME. Verbal autopsy tool. https://www.healthdata.org/data-tools-practices/verbal-autopsy
- 16.James S.L., Flaxman A.D., Murray C.J., Population Health Metrics Research Consortium (PHMRC) Performance of the Tariff Method: validation of a simple additive algorithm for analysis of verbal autopsies. Popul Health Metr. 2011;9:31. doi: 10.1186/1478-7954-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sample Registration System Statistical Report 2020. Office of the Registrar General & Census Commissioner, India. Published 2020. https://censusindia.gov.in/nada/index.php/catalog/44376
- 18.Bharati J., Jha V. Global dialysis perspective: India. Kidney360. 2020;1:1143–1147. doi: 10.34067/KID.0003982020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ordunez P., Martinez R., Reveiz L., et al. Chronic kidney disease epidemic in Central America: urgent public health action is needed amid causal uncertainty. PLoS Negl Trop Dis. 2014;8 doi: 10.1371/journal.pntd.0003019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ordunez P., Nieto F.J., Martinez R., et al. Chronic kidney disease mortality trends in selected Central America countries, 1997-2013: clues to an epidemic of chronic interstitial nephritis of agricultural communities. J Epidemiol Community Health. 2018;72:280–286. doi: 10.1136/jech-2017-210023. [DOI] [PubMed] [Google Scholar]
- 21.Ranasinghe A.V., Kumara G.W.G.P., Karunarathna R.H., et al. The incidence, prevalence and trends of Chronic Kidney Disease and Chronic Kidney Disease of uncertain aetiology (CKDu) in the North Central Province of Sri Lanka: an analysis of 30,566 patients. BMC Nephrol. 2019;20:338. doi: 10.1186/s12882-019-1501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nabukalu D., Ntaro M., Seviiri M., et al. Community health workers trained to conduct verbal autopsies provide better mortality measures than existing surveillance: results from a cross-sectional study in rural western Uganda. PLoS One. 2019;14 doi: 10.1371/journal.pone.0211482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siregar K.N., Kurniawan R., Nuridzin D.Z., et al. Strengthening causes of death identification through community-based verbal autopsy during the COVID-19 pandemic. BMC Public Health. 2022;22:1607. doi: 10.1186/s12889-022-14014-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang J., Joshi R., Sun J., et al. A feasibility study on using smartphones to conduct short-version verbal autopsies in rural China. Popul Health Metr. 2016;14:31. doi: 10.1186/s12963-016-0100-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joshi R., Hazard R.H., Mahesh P.K.B., et al. Improving cause of death certification in the Philippines: implementation of an electronic verbal autopsy decision support tool (SmartVA auto-analyse) to aid physician diagnoses of out-of-facility deaths. BMC Public Health. 2021;21:563. doi: 10.1186/s12889-021-10542-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Firth S.M., Hart J.D., Reeve M., et al. Integrating community-based verbal autopsy into civil registration and vital statistics: lessons learnt from five countries. BMJ Glob Health. 2021;6 doi: 10.1136/bmjgh-2021-006760. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.