Abstract
Lifestyle Medicine (LM) is a rapidly growing discipline that focuses on the role of lifestyle factors in preventing, managing, and reversing chronic disease. At this point in the field’s evolution, there is strong evidence that the 6 pillars of LM—a whole-food, plant-predominant eating pattern, physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connections—are central in the creation and maintenance of health. Previous publications, many of them randomized controlled studies and meta-analyses, have solidified the evidence base for the use of the 6 pillars within the field of LM. As data emerged, so did its governing body, the American College of Lifestyle Medicine (ACLM), and with it a rich history began to unfold. Several articles have been written on the early history of the ACLM and the growth of the field; however, this review article explores the history and foundation of LM, aiming to provide a comprehensive understanding of its relevance and impact on health care. It underscores landmark studies that have defined the field and provides a road map detailing national and global barriers and areas of potential future growth.
Article Highlights.
-
•
Lifestyle Medicine (LM) is a rapidly growing discipline that focuses on the role of lifestyle factors in preventing, managing, and reversing chronic disease.
-
•
Lifestyle medicine (LM) in the United States began as a medical specialty in 2004 and now boasts more than 9000 active members in 2022 in over 30 member groups and communities.
-
•
With its focus on evidence-based lifestyle applications for the prevention, management, and reversal of chronic diseases, LM has become one of the fastest growing medical specialties in America while fostering growth internationally as well.
Lifestyle Medicine: An Operational Definition
The American college of lifestyle medicine (ACLM) defines lifestyle medicine (LM) as “a medical specialty that uses therapeutic lifestyle interventions as a primary modality to treat chronic conditions including, but not limited to, cardiovascular diseases, type 2 diabetes, and obesity. Lifestyle medicine certified clinicians are trained to apply evidence-based, whole-person, prescriptive lifestyle change to treat and, when used intensively, often reverse such conditions. Applying the 6 pillars of LM also provides effective prevention for these conditions.”1
In summary, LM works to treat the whole person by employing lifestyle changes as its foundation for health. The origins of the field are traced to an inaugural textbook explicitly devoted to the topic of LM,2 and to the influential research and writing of several early luminaries.3, 4, 5 In 2004, the ACLM was founded as a professional medical association, and in 2007 the American Journal of Lifestyle Medicine was first published. Since this time, LM has become one of the fastest growing medical specialties.6
Lifestyle medicine uses the 6 pillars to help treat and prevent the root causes of many conditions. It places the patient, not medications or procedural treatments, at the center. Thus, it borrows and develops skills from multiple disciplines, such as nutrition science, positive psychology, behavior change, health and wellness coaching, exercise physiology, addiction medicine, and sleep medicine, with an ultimate focus on the health of both the patient and the LM clinician. The goal is to establish LM as a bedrock and foundation of primary care, exposing medical students and health care professionals to the education and tools necessary to improve the well-being of themselves and their patients. Fortunately, the American board of family practice has been a strong proponent, and the journal of the American board of family medicine has recently solicited papers on the intersection of LM and family medicine.7
Lifestyle medicine is distinct from other aspects of medicine, particularly conventional medicine, in that the core principles are to use daily healthy habits to prevent, treat, and even reverse chronic diseases. Contrary to conventional medicine, where the emphasis is on medications whose benefits are condition-specific, the benefits of lifestyle are not. Lifestyle practices directed at any given disease, whether prevention or treatment, are apt to confer comparable benefits across the expanse of all others.8 On a larger scale, LM, particularly the shift in dietary patterns to a whole-food plant-predominant eating pattern, can positively impact more than just the people but also the planet. There have been recent calls for health professionals to embrace planetary health as part of their professional purview and obligation and given the urgency of the situation and the potential for LM to contribute to a timely solution.9
With its focus on education and behavioral change, admittedly it can be a time-intensive field for both the patient and clinician. That being said, in addition to family practice physicians, many medical specialists, such as cardiologists, endocrinologists, and even orthopedic surgeons, became certified in LM because they see its value for patients, themselves, and the health care system.
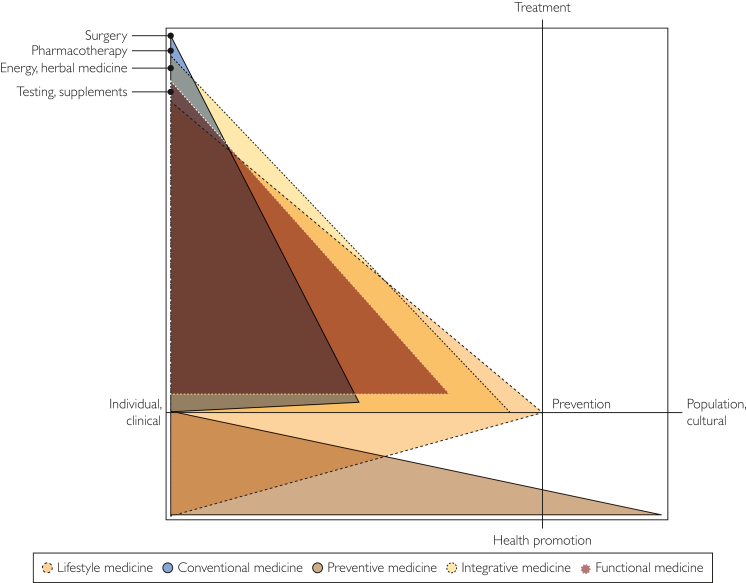
Lifestyle medicine is distinctly different from integrative or functional medicine. Integrative medicine focuses on integrating evidence-based complementary therapies, such as acupuncture, yoga, massage, and chiropractic into a conventional treatment plan to optimize patient healing. Functional medicine often also incorporates specific supplementation and often a wide variety of laboratory testing that is not in the core of LM. With more of a recent focus on wellness in the lay press, there is often confusion and misconception regarding the various fields that intersect between wellness and preventive medicine. Lifestyle medicine is the foundation on which other fields such as integrative medicine and functional medicine build their therapies as one cannot conceive of creating a holistic treatment plan for a patient without first establishing healthy habits within the 6 pillars of nutrition, exercise, stress reduction, avoidance of risky substances, and positive social connection (Figure).
Figure.
The domain of lifestyle medicine is compared with the most closely related fields of medicine. An array of related and to some extent overlapping medical fields, such as lifestyle medicine, conventional medicine, preventive medicine, integrative medicine, and functional medicine with each discipline color-coded. The horizontal axis represents progression from the individual to society and the vertical axis a progression from health promotion to treatment. Disciplines are characterized by (1) the modalities they include, exclude, and emphasize; (2) their focus on treatment vs prevention and health promotion; and (3) their focus on individual clinical care vs population health. This figure was developed through an iterative methodology and represents consensus by the authors. Lifestyle medicine, represented in light green, is unique in its exclusive emphasis on nutrition, exercise, sleep, stress management, social connections, and substance use cessation or modification for clinical benefit. Lifestyle medicine encompasses both treatment and prevention, with a preferential emphasis on individual patient care rather than population health. Conventional medicine, represented in gray, uses the modalities of lifestyle medicine but relies preferentially on pharmacotherapy, technology, and surgery to treat patients. The emphasis is on treatment over prevention, and individuals over population health. Preventive medicine, represented in light blue, uses the modalities of lifestyle medicine and conventional medicine to treat individual patients, but with a primary focus on prevention and health promotion. Preventive medicine is also the only discipline in this group with a major emphasis on population health. Integrative medicine, represented in purple, uses the modalities of lifestyle and conventional medicine to treat individual patients, and extends to other modalities as well, including but not limited to supplements, herbs, and energy medicine. The discipline extends to prevention, but the primary focus is on the treatment of the individual patient. Functional medicine, represented in brown/orange, uses the modalities of lifestyle and conventional medicine. The preferential focus is on identifying biochemical imbalances through blood, stool, and skin testing and then correcting those imbalances with targeted supplements. The discipline is primarily devoted to treatment rather than prevention, and to individual patient care rather than population health.
(Source: Used with permission from Maxcy-Rosenau-Last, Public Health and Preventive Medicine: 16th ed)
Lifestyle medicine often tries to anchor its treatments on the studies of healthy societies and incorporate such healthy lifestyles in the treatment of the patient and the health care professional. For example, imagine a female patient who is post-menopausal. The LM approach may be to focus on healthy foods rich in phytoestrogens such as legumes, flaxseeds, and soy, while emphasizing the importance of exercise to reduce central adiposity, stress management, and healthy body composition, the functional medicine provider may also consider treatment with bioidentical hormones, and the integrative clinician may recommend acupuncture and natural supplements to help with hot flashes.
One critical element for the ACLM is that the treatment prescribed is evidence-based. The college bases its recommendations often on randomized controlled trials showing reversal of many of the most common and costly chronic diseases or epidemiological-based trials, such as the Global Burden of Disease and Framingham Heart Study, which will be discussed in further detail later in this paper.
Ancient Foundations of Lifestyle Medicine
Although LM may be thought of as a newer medical specialty, its principles have roots that extend back for centuries. Hippocrates, an ancient Greek philosopher, and physician often thought of as the father of medicine, famously stated “in order to keep well, one should simply avoid too much food, too little toil.”10 Hippocrates devoted his time to figuring out the cause of disease, rather than simply describing the progression of pathology. He encouraged physicians to consider not only the disease process but also the patient context—whether they eat excessive amounts of food, if they get exercise and adequate sleep, what wine they drink and how much of it.11 It is with this lens he was able to distinguish lifestyle patterns that predisposed patients to specific diseases and conditions.
Around the same time, but several thousand miles to the East, the Chinese philosopher Confucius was also recognizing the impact that moderation in diet and alcohol, along with persistent practices of mindfulness and meditation, had on the quality of life. During the Han Dynasty, nurturing life techniques like diet and meditation became center stage for the well-being of the people.12
The wisdom of these ancient philosophers has been reiterated through time, a constant thread throughout humanity’s journey. However, as the burden of disease shifts from acute mortality caused by infectious disease in the 19th century to a more insidious killer—that of chronic disease—in the 21st, their words are more applicable now than they have ever been. In fact, it has been asserted that the Hippocratic prescription now needs to be expanded,13 perhaps to encompass the tenets of eating plants, keeping moving, sleeping well, being present, staying calm, avoiding risky substances, and loving people—a group of pillars collectively referred to as LM.
Modern Foundations of Lifestyle Medicine
The past several decades has shown mounting evidence that reports the impact that lifestyle practices can have on health, with a focus on physical activity, nutritious diet, not smoking, maintaining a healthy body weight, and healthy body composition. In 1993, in a landmark study in the Journal of the American Medical Association (JAMA), authors estimated that ∼80% of premature death in the United States was because of poor lifestyle.14 Before these studies, it was known that unhealthy behaviors were linked to morbidity and mortality, but the concept that healthy lifestyle habits could actually prevent disease was a paradigm change. This concept coincided with a shift in mortality rates over the past several generations moving from infectious to chronic diseases.15 At the turn of the 21st century, with heart disease and cancer being leading causes of mortality and morbidity, the emphasis shifted to needing to understand the root causes of chronic disease. Given the rates of heart disease deaths and a growing number of patients with type 2 diabetes and associated complications, a growing body of research has focused on understanding how particular foods influence endothelial cell function,16 glucose control, and insulin sensitivity.17
With the rise in these conditions in the United States, it became increasingly important to investigate areas of the world where chronic diseases were less common and how lifestyle choices impacted the incidence of chronic diseases experienced in those populations. This concept is clearly evident in T. Colin Campbell’s book, The China Study, which found that the Chinese counties that ate the most plant-based foods had the least or no chronic diseases and those who had adopted more of a westernized diet of animal protein had the most heart disease, cancer, and diabetes.18 Evidence that adhering to LM principles promotes longevity was also revealed in the Blue Zones research: lessons from the world’s longest lived populations,19 which examines different cultures around the world with the highest number of centenarians, such as Okinawa (Japan), Sardinia (Italy), Nicoya (Costa Rica), Icaria (Greece), and Loma Linda (California, USA). As this data shows, cumulative adherence to the LM principles, namely strong social and family connection, positive community building, moving naturally, eating wisely, and having a purpose in life, can positively impact not only the years of life but life in the years.
As type 2 diabetes and obesity continue to rise among adults and exceedingly so among children and adolescents in the United States, it has become a national priority to focus on adaptive lifestyle strategies to target this growing public health concern. Through a call to help educate physicians on methods and strategies not formally focused on through traditional medical training, physician core competencies for prescribing lifestyle medicine emerged in 2010 through a collaboration of ACLM and American College of Preventive Medicine.20 These competencies help guide physicians in the clinical practice of LM through improving leadership, knowledge, assessment skills, management skills, and the use of office and community support to improve the practice of patient care and chronic disease management. With the initiation of a board certification in LM in 2017 through the American Board of Lifestyle Medicine (ABLM), physicians and allied health care providers can be certified in lifestyle medicine. Physicians can be certified as LM physicians or LM intensivists and those with PhDs master’s degrees or allied health care providers can be certified as LM professionals. Given the interest in LM is international, there is a lifestyle medicine global alliance in collaboration with ACLM.21 Over the past decade the number of board-certified physicians and professionals in LM has grown exponentially. This has also been reflected in the growing number of lifestyle medicine interest groups (LMIG)s in medical school and the number of academic initiatives in medical schools and residency programs across the country to incorporate LM within curricula.22,23
Validating Evidence
Lifestyle medicine is built on evidence-based medicine and strong evidence supports its intervention and positive impact on health. In this section, we will explore several of the landmark studies that have shaped the field of lifestyle medicine.
The diabetes prevention program is a 27-center randomized clinical trial that reported LM intervention is more effective than metformin at preventing the progression of prediabetes to type 2 diabetes. In the trial, patients were randomized to 1 of 3 arms: metformin, lifestyle intervention, and placebo. Patients in the lifestyle intervention arm engaged in self-monitoring of caloric intake and exercise and received a 16-session core curriculum that covered information about nutrition, exercise, and stress management. After 3 years, the lifestyle intervention group had decreased their incidence of type 2 diabetes by 58%, compared with just 31% in the metformin-treated group.24 This trial was one of the first to report the power of lifestyle intervention over pharmacotherapy to prevent the progression of prediabetes to diabetes.
One of the earliest landmark studies reporting the power of lifestyle not just to prevent, but actually reverse chronic disease was The Lifestyle Heart Trial, published in The Lancet in 199025 and JAMA in 1995 and 1998. A secondary prevention trial, reported for the first time at 1-year and 5-year follow-ups that intensive therapeutic lifestyle change including a 10%-15% fat whole-food vegetarian diet, stress management training, smoking cessation, aerobic exercise, and group psychosocial support reversed the progression of coronary artery disease (CAD) as measured by quantitative coronary angiography. At 5 years, patients in the lifestyle intervention group had a relative reduction in their average coronary artery stenosis by 7.9%, compared with the placebo group, which had a worsening in stenosis by 27.7%.26 This study found that patients with pre-existing CAD who use lifestyle modalities can often reverse coronary artery stenosis. There were 2.5 times fewer cardiac events in the lifestyle intervention group, and cardiac positron emission tomography scans found a 400% increase in blood flow to the heart after 5 years when compared with the randomized control group.27
Nutritional science strongly supports a predominantly plant-based diet. The Health Effects of Dietary Risks in 195 Countries, 1990-2017: a systematic analysis estimated that in 2017, 11 million deaths were attributable to dietary risk factors. The 3 primary dietary risk factors were: (1) High intake of sodium (accounting for 3 million deaths); (2) low intake of whole grains (3 million deaths); and (3) low intake of fruits (2 million deaths). The study concluded, “Our findings show that suboptimal diet is responsible for more deaths than any other risks globally, including tobacco smoking, highlighting the urgent need for improving human diet across nations.” In addition to mortality, this global analysis concluded that suboptimal diet was responsible for 255 million daily adjusted life years lost because of disability.28
The PREDIMED Study (primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts) was originally published in the New England Journal of Medicine in 2013. There was some controversy, but the study was republished in 2018 with the initial findings still intact. It evaluated 7447 patients aged 55-80 years at a risk for heart disease and randomized them to 3 diets: mediterranean supplemented with olive oil, mediterranean supplemented with nuts, or the control who were advised to follow a low-fat diet. The study was stopped early because after 4.8 years of randomization, the study groups reported ∼30% reduction in the primary end points (myocardial infarction, stroke, or death from cardiovascular causes).29 However, there was no reduction in myocardial infarction when examined separately.
Another important study showing the benefits of the Mediterranean diet is the Lyon Heart Study, a study of over 600 individuals who suffered a myocardial infarction. A 27-month intermediate analysis found a 50%-70 % reduction in secondary prevention of heart attacks and associated outcomes with a mediterranean diet.30 The final report on the study lasting 46 months confirmed the earlier studies.31 A 50% reduction in secondary prevention of myocardial infarction is comparable to statin therapy. In a study of over 32,000 individuals with coronary artery calcification, statin therapy reduced the risk of myocardial infarction by ∼50%.32 In the JUPITER trial, which looked at individuals with high risk on the basis of elevated C-reactive protein, the reduction in myocardial infarction was ∼50%.33 After the final report on the Lyon Heart Study, an American Heart Association (AHA) Advisory statement stated “the AHA and its partners should take advantage of the remarkable opportunity to dramatically lower cardiovascular disease risk in the population by funding further nutrition-based research.”34 Both high-dose statin therapy and a heart healthy diet are recommended by the AHA for secondary prevention of myocardial infarctions.35
Physical activity is also incredibly important for longevity and health span. In a study of over 4800 individuals that lasted 10 years, step count was significantly associated with decreased mortality. There was nearly a 70% decrease in death rate for individuals who walked 10,000 steps or more compared with those who walked 2,000 steps or less. The findings were even more pronounced for those over 65 years. In that subset of patients, the death rate decreased by ∼80%. It did not matter how fast the individuals walked, simply that they got the steps.36 This points to the power of lifestyle. This decrease in death is orders of magnitude greater than nearly any available pharmaceutical treatment.
Restorative sleep has profound impacts on health over the course of the lifespan. Sleep is related to the repair and clearance processes needed to correct and prevent neuronal damage in addition to assisting in learning and synaptic homeostasis.37 Accumulated effects of disordered sleep include cognitive impairment but also span much broader to include cardiovascular disease, hypertension, metabolic syndrome, impaired glucose tolerance, immunosuppression, inflammation, anxiety and depression and premature mortality.38 Lifestyle medicine focuses on a behavior-centered approach to insomnia that highlights sleep hygiene and CBT-I, which has been reported by clinical trials as the most effective treatment for long-term insomnia.39
Similar to sleep, stress levels have diverse and extensive impacts on health and well-being. There are direct physiologic consequences secondary to activation of the sympathetic nervous system and elevated levels of cortisol including alterations of gut function, cardiovascular changes, and downregulation of immune function.40 However, from a broader perspective, stress also adversely affects health behaviors resulting in disordered sleep, inactivity, and poorer dietary choices.41,42 The ACLM encourages stress reduction through a variety of modalities43 including for example time in nature and evidence-based mind-body techniques including biofeedback, meditation, and mindful movement such as yoga or tai chi.44
Although there has been a significant decrease since 1960, cigarette smoking is still a leading cause of mortality estimated to be responsible for 1 in 5 of all deaths and claiming an estimated 480,000 lives in America alone.45 Alcohol is estimated to claim ∼140,000 deaths46 and there has been an explosion in deaths from illicit drug use, primarily illegally manufactured fentanyl. Illicit drug use is estimated to claim ∼100,000 lives in America annually47 and unintentional injuries, such as overdose from illegally manufactured fentanyl is now the leading cause of death for all individuals aged 18-44 years old.48 In short, the use of risky substances considerably affects lifespan and morbidity across our country and curbing their use is a top priority for our nation and health care system. Avoidance of risky substances clearly improves health and lifespan and serves as 1 of the 6 core pillars of LM.
Social Connectivity is a pillar of LM that has recently been highlighted given the COVID-19 pandemic. On reviewing the data of the Harvard Study of Adult Development which began in 1938, the current Director and the Associate Director of the study wrote “Through all the years of studying these lives, one crucial factor stands out for the consistency and power of its ties to physical health, mental health and longevity…Good relationships. In fact, good relationships are significant enough that if we had to take all 84 years of the Harvard Study and boil it down to a single principle for living, one life investment that is supported by similar findings across a wide variety of study, it would be this: Good relationships keep us healthier and happier. Period.”49 This is a powerful statement and reinforces the importance of positive social relationships. Furthermore, the impact of social isolation on poor health outcomes led the National Academy of Sciences (NAS) to create a 2020 report titled Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System.50 The NAS notes that social isolation has been associated with ∼50 percent increased risk of developing dementia and that loneliness among heart failure patients has been associated with a nearly 400% increased risk of death, whereas poor social relationships have been associated with a 29% increased risk of incident coronary heart disease and a 32% increased risk of stroke. In short, social connectivity is vital to human health.
The ineffectiveness of pharmacological treatment in many chronic conditions compared with the power of lifestyle is also evident in the cognitive science field. Acknowledging this, a press release for the 2019 Alzheimer’s Association International Conference emphasized the focus on lifestyle with the conclusion that adopting 4 or 5 healthy lifestyle factors reduced risk of Alzheimer’s dementia by 60% compared with adopting none or only 1 factor.51 Scientific American’s summary of the conference was titled, “Alzheimer’s Meeting: Lifestyle Factors Are the Best—and Only—Bet Now for Reducing Dementia Risk.”52 Such findings reinforce studies such as the Mediterranean-Dash Diet Intervention for Neurodegenerative Delay (MIND), which found, the difference in decline rates for being in the top tertile of MIND diet scores vs the lowest was equivalent to being 7.5 years younger in age, and concluded, the study findings suggest that the MIND diet substantially slows cognitive decline with age.53
Furthermore, through the perspective of LM, one may uncover potential unconscious bias that can arise from perceiving the clinician as the prime mover in health care rather than the patient. For instance, consider one of the greatest epidemiological studies ever performed and which is still continuing—the Framingham Heart Study (FHS) which has over 3 generations of health research. The FHS began in 1948 with 5209 participants aged 30-62 years old from Framingham, Massachusetts. The National Institute of Health itself stated, “One of the first long-term cohort studies of its kind, the Framingham Heart Study is considered the crown jewel of epidemiology. Thanks to Framingham, we now know that most cardiovascular disease is caused by modifiable risk factors like smoking, high blood pressure, obesity, high cholesterol levels, and physical inactivity.”54
The modifiable risk factors are nearly all lifestyle related. Focusing on physical activity, how many health care providers really ask about and encourage increased physical activity? Rather, in a medical situation, high blood pressure and cholesterol are often treated with pharmacological therapy, and the patient is counseled to stop smoking. In fact, there is often a desire to find pharmacological treatments for conditions rather than to encourage effective behavioral change.
For instance, early research on the FHS found that low high-density lipoprotein (HDL) was seen as a significant risk factor for heart disease. In 1977, the study found an association between low HDL levels and increased cardiovascular mortality.55 In 1988, an article titled “Cholesterol and lipids in the risk of coronary artery disease--the Framingham Heart Study” was published stating, “Data from 35 years of the Framingham Heart Study have shown that factors other than total or low-density lipoprotein (LDL) cholesterol must be considered when evaluating CAD risk. In fact, low levels of high-density lipoprotein (HDL) cholesterol are as much a risk factor for CAD as high LDL cholesterol. The best simple test for predicting CAD is the ratio of total:HDL cholesterol and using this criterion, approximately half the population of North America is at risk for heart attack.”56 It was from the FHS that the HDL/total cholesterol risk calculation was created and it is still in use today. Epidemiological studies have shown that for every 1 mg/dL rise in HDL cholesterol, the risk of developing cardiovascular diseases decreases by 2%.57
Great lengths have been taken by pharmacological companies to develop medications that increase HDL; however, 1 large review of a total of 12 randomized control trials including 26,858 patients with follow-up period ranging from 1-6.2 years concluded “Increasing HDL levels via pharmacological manipulation beyond optimal lipid lowering therapy for secondary prevention is not beneficial.”58 One pharmaceutical company spent over $800 million on torcetrapib, a drug which increased HDL by over 72%.59 However, it was pulled off the market after a study of over 15,000 participants concluded “Torcetrapib therapy resulted in an increased risk of mortality and morbidity of unknown mechanism.” Pharmacological manipulation of HDL actually INCREASED death rates.60 Another pharmaceutical company spent $500 million on anacetrapib but never released the drug, stating the data simply is not strong enough.61
From a LM perspective, could the data be viewed differently? There are few things that increase HDL, primarily aerobic exercise. Is it possible that the higher levels of HDL, and its association with decreased cardiovascular disease, were really a marker of the increased aerobic capacity of such participants and it was this that was primarily responsible for the health benefit? Would it be more efficacious to work on increasing an individual’s HDL through lifestyle measures such as walking, jogging, playing tennis, weight loss etc, rather than searching for a drug to artificially increase the HDL molecule itself?
Indeed, by focusing on the HDL molecule itself, did we lose focus on a possibly much larger risk factor of physical inactivity in relation to heart disease? In a 2022 study of over 750,000 veterans that lasted for 10 years, the conclusion was “Being unfit carried a greater risk than any of the cardiac risk factors examined.” Those at the highest metabolic equivalentcapacity of 14 reported ∼75% reduced risk of death.62 The magnitude of decreased risk by cardiovascular fitness is indicative of this essential aspect of lifestyle intervention.
If the medical community focused on physical activity as a risk factor with the same intensity as we focused on discrete variables such as blood pressure and cholesterol, would we have arrived at this conclusion decades earlier? Would not that be truly evidence based?
Determinants of Health
Determinants of health can be divided into 5 groups: genetics, behavior, environmental and physical influences, medical care, and social factors. Although individual choice and behavior greatly influence LM and health care outcomes, it is important to consider the wide range of social factors that impact health on a population level. Individual behavioral factors that are paramount in LM, are inextricably intertwined with social factors and barriers. For example, the likelihood of a person to start smoking is impacted by age, gender, education, peer network, and geographic location. Thus, although smoking is a key modifiable behavioral risk factor for disease, the risk of smoking changes on the basis of social determinants the individual has experienced.
The Centers for Disease Control and Prevention (CDC) identifies addressing Social Determinants of Healthcare (SDOH) as the primary approach to achieving health equity.63 Health equality calls for sameness of treatment but ignores the fact that some people have been historically and intentionally excluded from certain resources. Conversely, health equity involves redistributing resources so that individuals with the greatest needs can have those needs addressed.64 One of the most effective ways of addressing SDOH and achieving health equity is through LM. The ACLM actively works to address public health and health equity through several modalities including the (HEAL) Health Equity for Lifestyle Medicine Initiative, which aims to educate clinicians about health equity, expand services using community-based participatory research, build partnerships with community groups, empowers patients with tools for self-efficacy, addresses the reality of underrepresentation in medicine, and advocates for public policy change.64 For the first time in many decades, there are governmental/national efforts to support this movement. In September 2022, President Biden hosted the first White House Conference on Hunger, Nutrition, and Health in over 50 years to bring Americans together to achieve the goal of ending hunger and increasing healthy eating and physical activity by 2030 so that fewer Americans experience diet-related diseases (diabetes, obesity, and hypertension). The Administration also released a national strategy with actions the federal government plans to enact detailing new commitments as part of the conference’s call to action.65
Evolution of the Field
United States
Lifestyle medicine in the United States began as a medical specialty in 2004, when the ACLM had their first general meeting.66 The novel premise of LM was that healthy lifestyle behaviors not only prevented chronic diseases, but, when sufficiently intensive, could also treat, and even reverse, these conditions. A corollary was that lifestyle treatment programs required a special skill set not prevalent in conventional medicine to successfully change lifestyle behaviors. The ACLM membership approached 4000 by 2019, swelling to more than 9000 active members in 2022 in over 30 member groups and communities.
Physician competencies for prescribing LM were published in 201020 and updated in 2022,67 emphasizing leadership, knowledge, assessment skills, management skills, and using office and community support. These standards facilitated board certification as an integral, and logical, corollary to the rapid growth of LM as a specialty and as a foundation for mainstream medicine.68 The ABLM first certified 221 US physicians (diplomates) in 2017, rising to 2445 total diplomates by 2022. These diplomates view certification as a source of personal pride that could help market clinical services while fostering credibility among consumers, the public, payers, and health systems.68,69 Concurrently, the ACLM has certified 729 professionals with a masters or doctorate degree in a health or allied health discipline.
Perhaps the most exciting aspects of LM in the United States are advances in education, training, and quality. The ACLM has produced an annual education conference since 2011, had over 11,250 individuals enrolled in continuing education courses in 2022, and oversees medical-student-run LMIGs at 104 US medical schools (about 60% of all schools). The LM residency curriculum, initiated in 2018 at 8 training sites and 13 residency programs, grew by 2022 to 130 sites and 207 programs. The ABLM is working with the Accreditation Council on Graduate Medical Education to incorporate LM formally into family medicine residency training.70 Diverse quality initiatives from ACLM include creating the Health Systems Council for value-based LM care,71 publishing their first multidisciplinary expert consensus statement,72 and initiating their first multidisciplinary clinical practice guideline, for treating and preventing prediabetes and type 2 diabetes.
The dramatic growth of LM in the United States has posed challenges that include recognition as a distinct medical specialty, integration into mainstream medicine, and reimbursement. Recognition should increase as new LMIGs are created, the LM residency curriculum is adopted by more training programs, the ACGME initiative comes to fruition, and the LM fellowship programs increase. Integration into mainstream medicine, especially primary care settings, will increase as LM continues to gain prominence as the foundation of all health care and optimal practice models are identified, which is the subject of an upcoming expert consensus statement from ACLM. Reimbursement issues are also addressed in the new consensus statement, but important advances are occurring through the ACLM Health Systems Council, increasing the prevalence of group medical visits, and the appeal of value-based care to payers. Despite challenges, the future of LM in the United States is bright and approaching a tipping point in the health care paradigm.
International
Although LM as a formal medical movement is recent, it has spread around the globe quickly. With the ACLM’s support, the international board of LM was established to help countries develop their own LM societies and run the international board of LM certification exam. These societies are key to spreading the LM message in the scientific community and making national movements stronger. Regular gatherings with a variety of countries at the LM global alliance are important to discuss lessons learned and challenges faced, and to create a sense of global community. In addition, the exam is important to set and maintain standards of competencies achieved by health professionals internationally.73
The principles of LM are necessary in every country to prevent, treat, reverse, and lower costs related to noncommunicable diseases, including mental health. According to the Global Burden of Diseases published in The Lancet in 2019, “highly preventable risk factors are rising at alarming rates, and creating huge burdens on global social, economic, and health systems.”74
To educate health professionals, there are an increasing number of LM programs for undergraduates, postgraduates, residents, and fellows.75, 76, 77, 78 These programs bring evidence of the impact of the pillars of lifestyle medicine in noncommunicable disease management and tools on the basis of neuroscience, behavior science, and health and wellness coaching to help patients adopt and maintain healthy behaviors. Many programs include physicians and other health professionals, as transdisciplinarity is essential for better results. Physicians are being trained on intensive LM interventions to manage a deeper approach, bringing a better treatment and, when possible, deprescribe drugs and reverse disease conditions.79,80
For patients, there are programs structured to educate and promote behavior change in a welcoming environment that respects individualities. PAVING the Path to Wellness81 and Pivio82 are good examples. Individual programs in clinics and corporate programs for employees are available in many countries, and intensive LM programs.
For the general public, we find LM programs at schools, community centers and important related initiatives. In Mexico, Peru, Uruguay, and Chile there are modifications of food labels with warnings for excess salt, sugar, fat, and calories.83 In Brazil, the Health Ministry published the acclaimed Dietary Guidelines for the Brazilian Population84 that includes Dr. Carlos Monteiro’s team NOVA classification on processed foods. Initiatives related to physical activity, mental well-being, healthy sleep, and social connection are supported by the World Health Organization and United Nations and are important to achieve the Sustainable Development Goal 3 (health and wellness).85 Lifestyle medicine professionals understand and support these environmental and comprehensive interventions to create healthier communities around the globe.
Key Challenges
In regard to the evolution of the field, LM can be transformational not only for the patient and clinician, but also for society in general. However, to truly harness the power of LM, its potential must be seen, challenges of implementation must be faced, and strategic action must be taken to use the principles of LM to increase both longevity and vitality (adding years to life and life to years) for both individuals and communities. In short, rate limiting steps in the catalyst for LM adoption as a society and medical community must be identified and overcome. There are multiple obstacles. They include the following:
Limited Awareness and Education
The medical mindset continues to prioritize pharmacological and surgical therapies, starting from the undergraduate level, while overlooking the importance of lifestyle modification. This approach disregards the evidence-based foundations of lifestyle medicine—including behavioral science and health and wellness coaching techniques—to prevent, treat, and reverse diseases.86 Furthermore, although guidelines for many conditions such as diabetes and CAD focus several pages on LM changes, there is often not enough emphasis on implementing such changes in the treatment plan for the patient, and clinicians frequently fall into clinical inertia in regard to promoting lifestyle change. Furthermore, the physicians themselves often exhibit poor lifestyle habits. This complicates adoption of LM because evidence shows that overweight, inactive, poorly nourished physicians who neglect self-care themselves are less likely to inquire about or provide effective guidance regarding these crucial lifestyle factors.87 One of the challenges is the limited awareness and education about LM among health care professionals,88 policymakers,88 and the general public. Many health care providers may not be familiar with the principles and evidence supporting lifestyle interventions. Similarly, policymakers may not prioritize the integration of LM into health care policies and guidelines. Increasing awareness and providing comprehensive education about LM are crucial to overcome this challenge.89
Institutional Resistance and Lack of Integration
The traditional health care system is often resistant to change and may not readily embrace LM.90 The integration of lifestyle interventions into existing medical practices requires overcoming institutional barriers, including resistance from some medical professionals, as it requires training, time, and communication skills.
For instance, one of the primary difficulties in implementing LM in the United States is related to the fee-for-service practice model. Under such a system, the clinician is paid for a procedure or service, but not reimbursed for preventing disease. To practice LM in such a system, the clinician must become an expert in current procedural terminology (CPT) codes, focusing on ones associated with screening (such as alcohol, tobacco cessation, or depression), or the use of modifier 33 code, which can be associated with Grade A or B recommendations from the United States Preventive Service Task Force. They also may use shared medical appointments, also known as group visits, in order to generate more revenue in a classroom-like environment.91
However, acknowledging the difficulty of working within the CPT system, some LM clinicians choose a direct practice model, also known as direct primary care, in which the clinician is paid a direct monthly fee retainer to see a patient and work to largely bypass the fee-for-service model entirely.92 Others may work directly with insurance companies through a growing model of value-based care in an effort to provide higher value care at lower cost for the patients and thus reap financial benefits from savings associated with healthier patients.93 There have been calls for changing the entire CPT reimbursement methodology to pay providers on the basis of healthier outcomes.94 Regardless, with the high cost of overhead for a primary care practice and the high cost of insurance for patients, it can be challenging for clinicians and patients to benefit from all LM has to offer in the current medical system.
Inadequate Time and Resources
Health care professionals often have limited time available for patient consultations, which may hinder their ability to adequately address lifestyle factors. Insufficient resources, such as training programs, support systems, and reimbursement models, also challenge the effective integration of LM into health care delivery73 for both private and public health services.
Cultural and Socioeconomic Factors
Cultural and socioeconomic factors can influence the adoption and implementation of LM practices. Behavior modification is challenging in every culture. It requires accountability, resiliency, compassion, and professional skills, and it depends on individual, collective and environmental variables. Societal norms, beliefs, and economic disparities can either facilitate or impede lifestyle behavior change. Tailoring lifestyle interventions to diverse cultural contexts and addressing socioeconomic barriers, such as access to healthy food options and safe environments for physical activity, is crucial for successful implementation worldwide. In addition, using community health workers and patient advocates can help LM clinicians better understand how to best reach the community in need in a culturally sensitive way and develop programming that fits their needs.
Despite the perceived current obstacles, we must not lose the vision of the bright future that LM can help create. We have to measure quality metrics that matter. Often quality metrics focus on the prescription of certain medications. Yes, renin angiotensin aldosterone agents are important for diabetics with microalbuminuria, and statins are important for individuals with CAD, but so are smoking cessation, step count, and healthy diet, and these LM changes may offer orders of magnitude greater health benefit to the patient than simple pharmacological treatment. As US health care reimbursement continues to lean toward value-based rather than fee-for-service care, the importance of holistic health and patient outcomes will be even more critical for clinician sustainability.
Implementing LM on a community level can help not only the individual being treated, but also the entire community itself. This is evidenced by the North Karelia Project. North Karelia, Finland, was associated with one of the highest cardiovascular mortality rates in the world. Massive social and educational programs were instituted, focusing on modifiable risk factors, and cardiovascular disease was reduced by 84% from 1972 to 2014. It was felt that 2/3 of the reduction in death was related to LM changes.95 This is the power of LM, not just for the individual, whether they be a patient or clinician, but for the community, society, and global world which we all inhabit. By tackling these challenges, health care systems can harness the potential of lifestyle interventions to improve population health outcomes and reduce the burden of chronic diseases worldwide. Clearly, LM can work powerfully and synergistically with value-based care, which focuses on providing the highest quality care while controlling costs. Harnessing the power of positive behavioral change, LM offers the ability to improve outcomes, improve quality measures, and improve population health.
Discussion
Lifestyle medicine is an exciting new medical specialty founded in 2004 that works to treat the whole person by employing lifestyle interventions—a whole-food, plant-predominant eating pattern, physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection—as its foundation for health. It is distinct from conventional medicine in that it encourages lifestyle behaviors to not only prevent chronic diseases, but, when sufficiently intensive, also treat, and even reverse, these conditions.
Over the past several decades, LM has amassed a critical body of evidence reporting the significant impact the 6 pillars have on health. Publications including the Diabetes Prevention Program, The Lifestyle Heart Trial, The PREDIMED Study, The Lyon Heart Study, and the Framingham Heart Study establishes the field on the cutting edge of modern-day medicine. As we find ourselves in a chronic disease pandemic and in more of a sick care system than a health care system, the discipline of LM, devoted to the application of prevention and reversal of chronic disease with the goal of addressing health disparities and achieving health equity through cost effective methods, is of paramount importance.
Barriers to continued growth in the field include limited awareness and education, institutional resistance and lack of integration, inadequate time and resources, and cultural and socioeconomic factors. Despite these challenges, the field continues to grow rapidly—not only throughout the United States, but also globally. From annual education conferences, medical-student-run LMIGs, the LM residency curriculum, and the lifestyle medicine global alliance, the importance of LM at all levels of training across a broad range of specialties is clear.
The future of LM is bright as more and more clinicians, patients, and health care systems worldwide have concluded that by addressing the underlying root of chronic disease we are able to impact health and wellness on a global scale. As data shows, cumulative adherence to the principles of LM can positively impact not only the years of life but life in the years. Lifestyle medicine is poised strategically, in a critical chasm and a unique point in time, able not only to help us rethink and redesign the way our global health care systems operate, but also to reconsider our impact on this world, its inhabitants, and our sustainability. It is imperative, at this moment, that the health care community rallies behind the principles of LM- for the well-being and health of the individual, the global community, and the planet.
Potential Competing Interests
John Kelly, founding president of ACLM; Sley Tanigawa Guimaraes, Hospital Israelita Albert Einstein, International Board of Lifestyle Medicine at the Mexican Lifestyle Medicine Conference 2022, President of the Brazilian College of Lifestyle Medicine; David Lippman, board member on the American Board of Lifestyle Medicine; Dean Ornish, directs PMRI institute has received grants from Ballantine Books, Sharecare, The Preventive Medicine Research Institute, United Airlines, Beyond Meat, Founder, Ornish Lifestyle Medicine; Richard Rosenfeld, director for guidelines and quality ACLM, Treasurer and Board Member ABLM. Mariah Stump, University of Arizona Center for Integrative Medicine lecturer, ACP National meeting speaker, Chair of PCP Advisory Committee to Rhode Island Department of Health; Erica Veazey, no disclosures; David Katz,-no disclosures. The authors report no competing interests.
References
- 1.American College of Lifestyle Medicine https://lifestylemedicine.org/
- 2.Rippe J.M. CRC Press; 1999. Lifestyle Medicine. [Google Scholar]
- 3.Ornish D., Ornish A. Random House; 2019. UnDo It! How Simple Lifestyle Changes Can Reverse Most Chronic Diseases. [Google Scholar]
- 4.Campbell T.C., Campbell T.M. BenBella Books; 2005. The China Study. [Google Scholar]
- 5.Esselstyn C.B., Jr. Resolving the coronary artery disease epidemic through plant-based nutrition. Prev Cardiol. 2001;4(4):171–177. doi: 10.1111/j.1520-037x.2001.00538.x. [DOI] [PubMed] [Google Scholar]
- 6.American College of Lifestyle Medicine. https://lifestylemedicine.org/clinician/
- 7.J Am Board Fam Med. https://www.jabfm.org/content/lifestyle-medicine
- 8.Ford E.S., Bergmann M.M., Kröger J., Schienkiewitz A., Weikert C., Boeing H. Healthy living is the best revenge: findings from the European prospective investigation into cancer and nutrition-potsdam study. Arch Intern Med. 2009;169(15):1355–1362. doi: 10.1001/archinternmed.2009.237. [DOI] [PubMed] [Google Scholar]
- 9.Redvers N. Patient-planetary health co-benefit prescribing: emerging considerations for health policy and health professional practice. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.678545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hippocrates . Encyclopedia Britannica; Chicago, IL: 1955. Hippocratic Writings. [Google Scholar]
- 11.Ippokratous P.G. Papyros; 1938. Ta apanda [Hyppocrates: the Collection] (in Greek) [Google Scholar]
- 12.Ngo V. Presses Universitaires de France; 1976. Divination Magie et Politique dans la Chine Ancienne. [Google Scholar]
- 13.Battersby M., Egger G., Litt J. In: Lifestyle Medicine: Managing Disease of Lifestyle in the 21st Century. 2nd ed. Egger G., Binns A., Rossner S., editors. McGraw-Hill Australia Pty Ltd; 2011. Introduction to lifestyle medicine; p. 5. [Google Scholar]
- 14.McGinnis J.M., Foege W.H. Actual causes of death in the United States. JAMA. 1993;270(18):2207–2212. [PubMed] [Google Scholar]
- 15.Mokdad A.H., Marks J.S., Stroup D.F., Gerberding J.L. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 16.Tuso P., Stoll S.R., Li W.W. A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm J. 2015;19(1):62–67. doi: 10.7812/TPP/14-036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ujvari D., Hulchiy M., Calaby A., Nybacka Å., Byström B., Hirschberg A.L. Lifestyle intervention up-regulates gene and protein levels of molecules involved in insulin signaling in the endometrium of overweight/obese women with polycystic ovary syndrome. Hum Reprod. 2014;29(7):1526–1535. doi: 10.1093/humrep/deu114. [DOI] [PubMed] [Google Scholar]
- 18.Campbell T., Campbell T., II . Rodale Books; 2016. The China Study Solution: the Simple Way to Lose Weight and Reverse Illness, Using a Whole-Food, Plant-Based Diet. [Google Scholar]
- 19.Buettner D., Skemp S.S. Blue Zones: Lessons from the world’s longest lived. Am J Lifestyle Med. 2016;10(5):318–321. doi: 10.1177/1559827616637066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lianov L., Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010;304(2):202–203. doi: 10.1001/jama.2010.903. [DOI] [PubMed] [Google Scholar]
- 21.Lifestyle Medicine Global Alliance. https://lifestylemedicineglobal.org/
- 22.Pojednic R., Frates E. A parallel curriculum in lifestyle medicine. Clin Teach. 2017;14(1):27–31. doi: 10.1111/tct.12475. [DOI] [PubMed] [Google Scholar]
- 23.Pojednic R.M., Trilk J., Phillips E.M. Lifestyle medicine curricula: an Initiative to Include Lifestyle Medicine in Our Nation’s Medical Schools. Acad Med. 2015;90(7):840–841. doi: 10.1097/ACM.0000000000000744. [DOI] [PubMed] [Google Scholar]
- 24.Knowler W.C., Barrett-Connor E., Fowler S.E., et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ornish D.M., Brown S.E., Scherwitz L.W., et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336(8708):129–133. doi: 10.1016/0140-6736(90)91656-u. [DOI] [PubMed] [Google Scholar]
- 26.Ornish D., Scherwitz L.W., Billings J.H., et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280(23):2001–2007. doi: 10.1001/jama.280.23.2001. [DOI] [PubMed] [Google Scholar]
- 27.Gould K.L., Ornish D., Scherwitz L., et al. Changes in myocardial perfusion abnormalities by positron emission tomography after long-term, intense risk factor modification. JAMA. 1995;274(11):894–901. doi: 10.1001/jama.1995.03530110056036. [DOI] [PubMed] [Google Scholar]
- 28.GBD 2017 Diet Collaborators Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Estruch R., Ros E., Salas-Salvadó J., et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378(25):e34. doi: 10.1056/NEJMoa1800389. [DOI] [PubMed] [Google Scholar]
- 30.de Lorgeril M., Renaud S., Mamelle N., et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343(8911):1454–1459. doi: 10.1016/s0140-6736(94)92580-1. Published correction appears in Lancet. 1995;345(8951):738. [DOI] [PubMed] [Google Scholar]
- 31.de Lorgeril M., Salen P., Martin J.L., Monjaud I., Delaye J., Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–785. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- 32.Øvrehus K.A., Diederichsen A., Grove E.L., et al. Reduction of myocardial infarction and all-cause mortality associated to statins in patients without obstructive CAD. JACC Cardiovasc Imaging. 2021;14(12):2400–2410. doi: 10.1016/j.jcmg.2021.05.022. [DOI] [PubMed] [Google Scholar]
- 33.Ridker P.M., Danielson E., Fonseca F.A., et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- 34.Kris-Etherton P., Eckel R.H., Howard B.V., St Jeor S., Bazzarre T.L., Nutrition Committee Population Science Committee and Clinical Science Committee of the American Heart Association AHA Science Advisory: Lyon Diet Heart Study. Benefits of a Mediterranean-style, National Cholesterol Education Program/American Heart Association Step I dietary pattern on cardiovascular disease. Circulation. 2001;103(13):1823–1825. doi: 10.1161/01.cir.103.13.1823. [DOI] [PubMed] [Google Scholar]
- 35.Virani S.S., Smith S.C., Jr., Stone N.J., Grundy S.M. Secondary prevention for atherosclerotic cardiovascular disease: comparing recent US and European guidelines on dyslipidemia. Circulation. 2020;141(14):1121–1123. doi: 10.1161/CIRCULATIONAHA.119.044282. [DOI] [PubMed] [Google Scholar]
- 36.Saint-Maurice P.F., Troiano R.P., Bassett D.R., et al. Association of Daily Step Count and Step Intensity With Mortality Among US Adults. JAMA. 2020;323(12):1151–1160. doi: 10.1001/jama.2020.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benca R.M., Teodorescu M. Sleep physiology and disorders in aging and dementia. Handb Clin Neurol. 2019;167:477–493. doi: 10.1016/B978-0-12-804766-8.00026-1. [DOI] [PubMed] [Google Scholar]
- 38.Institute of Medicine, Board on Health Sciences Policy, Committee on Sleep Medicine and Research . National Academies Press; 2006. Sleep Disorders and Sleep Deprivation: an Unmet Public Health Problem. [PubMed] [Google Scholar]
- 39.Mitchell M.D., Gehrman P., Perlis M., Umscheid C.A. Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Fam Pract. 2012;13:40. doi: 10.1186/1471-2296-13-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Daviu N., Bruchas M.R., Moghaddam B., Sandi C., Beyeler A. Neurobiological links between stress and anxiety. Neurobiol Stress. 2019;11 doi: 10.1016/j.ynstr.2019.100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stults-Kolehmainen M.A., Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44(1):81–121. doi: 10.1007/s40279-013-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kalmbach D.A., Anderson J.R., Drake C.L. The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J Sleep Res. 2018;27(6) doi: 10.1111/jsr.12710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baban K.A., Morton D.P. Lifestyle medicine and stress management. J Fam Pract. 2022;71(suppl 1 Lifestyle):S24–S29. doi: 10.12788/jfp.0285. [DOI] [PubMed] [Google Scholar]
- 44.Davidson R.J., Kabat-Zinn J., Schumacher J., et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65(4):564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- 45.Diseases and death. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/diseases-and-death.html#:∼:text=Smoking%20is%20the%20leading%20cause%20of%20preventable%20death.&text=Cigarette%20smoking%20is%20responsible%20for,or%201%2C300%20deaths%20every%20day
- 46.Spencer M.R., Curtin S.C., Garnett M.F. Alcohol-induced death rates in the United States, 2019-2020. NCHS Data Brief. October 21, 2022;(448):1–8. https://www.cdc.gov/nchs/products/databriefs/db448.htm [PubMed] [Google Scholar]
- 47.Drug overdose deaths in the U.S. top 100,000 annually. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm; November 17, 2021.
- 48.Injuries and violence are leading causes of death. Centers for Disease Control and Prevention. https://www.cdc.gov/injury/wisqars/animated-leading-causes.html#:∼:text=Unintentional%20injuries%20are%20the%20leading,aged %201%2D44%2b0years%20old
- 49.Waldinger R.J., Schulz M.S. Simon and Schuster; 2023. The Good Life: Lessons from the World’s Longest Scientific Study of Happiness. [Google Scholar]
- 50.National Academies of Sciences, Engineering, and Medicine. Division of Behavioral and Social Sciences and Education, Health and Medicine Division, Board on Behavioral, Cognitive, and Sensory Sciences, Board on Health Sciences Policy. Committee on the Health and Medical Dimensions of Social Isolation and Loneliness in Older Adults . National Academies Press; February 27, 2020. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. [PubMed] [Google Scholar]
- 51.Alzheimer’s Association press release: lifestyle interventions provide maximum memory benefit when combined, may offset elevated Alzheimer’s risk due to genetics, pollution. https://aaic.alz.org/releases_2019/sunLIFESTYLE-jul14.asp#: ∼:text=Five%20research%20studies %20reported%20at%20AAIC%202019%20suggest%3A,lifestyle%20may%20counteract%20genetic%20risk%20for%20Alzheimer%E2%80%99s%20disease
- 52.Weintraub K. 2018. The Means of Reproduction. Sci Am Alzheimer’s Meeting: Lifestyle Factors Are the Best—and Only—Bet Now for Reducing Dementia Risk.https://www.scientificamerican.com/article/alzheimers-meeting-lifestyle-factors-are-the-best-and-only-bet-now-for-reducing-dementia-risk/ [Google Scholar]
- 53.Morris M.C., Tangney C.C., Wang Y., et al. MIND diet slows cognitive decline with aging. Alzheimers Dement. 2015;11(9):1015–1022. doi: 10.1016/j.jalz.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.The Framingham heart study: laying the foundation for preventive health care. https://www.nih.gov/sites/default/files/about-nih/impact/framingham-heart-study.pdf National Institutes of Health.
- 55.Gordon T., Castelli W.P., Hjortland M.C., Kannel W.B., Dawber T.R. High density lipoprotein as a protective factor against coronary heart disease. The Framingham study. Am J Med. 1977;62(5):707–714. doi: 10.1016/0002-9343(77)90874-9. [DOI] [PubMed] [Google Scholar]
- 56.Castelli W.P. Cholesterol and lipids in the risk of coronary artery disease—the Framingham Heart Study. Can J Cardiol. 1988;4(suppl A):5A–10A. [PubMed] [Google Scholar]
- 57.Gordon D.J., Probstfield J.L., Garrison R.J., et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79(1):8–15. doi: 10.1161/01.cir.79.1.8. [DOI] [PubMed] [Google Scholar]
- 58.Kaur N., Pandey A., Negi H., et al. Effect of HDL-raising drugs on cardiovascular outcomes: a systematic review and meta-regression. PLOS ONE. 2014;9(4) doi: 10.1371/journal.pone.0094585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Learning lessons from Pfizer’s $800 million failure. Nat Rev Drug Discov. 2011;10(3):163–164. doi: 10.1038/nrd3401. [DOI] [PubMed] [Google Scholar]
- 60.Barter P.J., Caulfield M., Eriksson M., et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357(21):2109–2122. doi: 10.1056/NEJMoa0706628. [DOI] [PubMed] [Google Scholar]
- 61.CETP inhibitor class finally dies as Merck abandons anacetrapib. PMLiVE. https://www.pmlive.com/pharma_news/cetp_inhibitor_class_finally_dies_as_merck_abandons_anacetrapib_1208239#:∼:text=Despite%20positive%20results%20in%20a,simply%20isn%27t%20strong%20enough
- 62.Kokkinos P., Faselis C., Samuel I.B.H., et al. Cardiorespiratory fitness and mortality risk across the spectra of age, race, and sex. J Am Coll Cardiol. 2022;80(6):598–609. doi: 10.1016/j.jacc.2022.05.031. [DOI] [PubMed] [Google Scholar]
- 63.NCHHSTP social determinants of health. Centers for Disease Control and Prevention. https://www.cdc.gov/nchhstp/socialdeterminants/faq.html; December 19, 2019.
- 64.LMRC . 2022. Health Equity : 1. Lifestyle Medicine Residency Curriculum. Lifestyle Medicine, Public Health, and Health Equity.https://education.lifestylemedicine.org/d2l/le/lessons/6803/lessons/7743 [Google Scholar]
- 65.Ending hunger and reducing diet-related diseases and disparities. https://health.gov/our-work/nutrition-physical-activity/white-house-conference-hunger-nutrition-and-health ite House Conference on Hunger, Nutrition, and Health.
- 66.Benigas S. American College of Lifestyle Medicine: Vision, Tenacity, Transformation. Am J Lifestyle Med. 2020;14(1):57–60. doi: 10.1177/1559827619881094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lianov L.S., Adamson K., Kelly J.H., Matthews S., Palma M., Rea B.L. Lifestyle medicine core competencies: 2022 update. Am J Lifestyle Med. 2022;16(6):734–739. doi: 10.1177/15598276221121580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lianov L., Rosenfeld R. The Case for Physician Training and Certification in Lifestyle Medicine. Am J Lifestyle Med. 2023;17(2):326–330. doi: 10.1177/15598276221138087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rosenfeld R.M. Physician attitudes on the status, value, and future of board certification in lifestyle medicine. Am J Lifestyle Med. 2022 doi: 10.1177/15598276221131524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Accreditation Council for Graduate Medical Education (ACGME) Advancing innovation in residency education (AIRE) https://www.acgme.org/initiatives/advancing-innovation-in-residency-education-aire/
- 71.American College of Lifestyle Medicine Health Systems Council. https://lifestylemedicine.org/health-systems-council/
- 72.Rosenfeld R.M., Kelly J.H., Agarwal M., et al. Dietary interventions to treat Type 2 diabetes in adults with a goal of remission: an expert consensus statement from the American college of lifestyle medicine. Am J Lifestyle Med. 2022;16(3):342–362. doi: 10.1177/15598276221087624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.International Board of Lifestyle Medicine https://iblm.co/
- 74.Global Burden of disease 2019. The Lancet. https://www.thelancet.com/infographics-do/gbd-2019
- 75.Education: academic integration and continuing education. https://lifestylemedicine.org/education-courses/ American College of Lifestyle Medicine.
- 76.Events. https://lifestylemedicineglobal.org/events/ Lifestyle Medicine Global Alliance.
- 77.Lifestyle medicine: tools for promoting healthy change. Harvard Medical School. https://lifestylemedicine.hmscme.com/
- 78.Estilo de vida e coaching de Saúde. https://ensino.einstein.br/pos_estilo_vida_coaching_saude_p2788/p?sku=6247&cidade=sp Albert Einstein Instituto Israelita de Ensino E Pesquisa.
- 79.Medication deprescribing protocols for Type 2 diabetes. https://lifestylemedicine.org/articles/medication-deprescribing/ American College of Lifestyle Medicine.
- 80.Fields D., Arnold M., Karlsen M., Kelly J. A lifestyle medicine approach to medication deprescribing: an introduction. J Fam Pract. 2022;71(suppl 1 Lifestyle):eS100–eS104. doi: 10.12788/jfp.0259. [DOI] [PubMed] [Google Scholar]
- 81.Paving the Path to Wellness. https://www.pavingwellness.org/
- 82.Pivio. https://piviohealth.com/ Lifestyle Medicine Institute.
- 83.Front-of-packaging labeling advances in the Americas. https://www.paho.org/en/news/29-9-2020-front-package-labeling-advances-americas Pan-American Health Organization.
- 84.Dietary guidelines for the Brazilian population. Ministry of Health or brazil. https://bvsms.saude.gov.br/bvs/publicacoes/dietary_guidelines_brazilian_population.pdf
- 85.Ensure healthy lives and promote well-being for all at all ages. United Nations. https://sdgs.un.org/goals/goal3 Department of Economic and Social Affairs.
- 86.Rea B., Worthman S., Shetty P., Alexander M., Trilk J.L. Medical education transformation: lifestyle medicine in undergraduate and graduate medical education, fellowship, and continuing medical education. Am J Lifestyle Med. 2021;15(5):514–525. doi: 10.1177/15598276211006629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cepni A.B., Hatem C., Ledoux T.A., Johnston C.A. The importance of health values among health care providers. Am J Lifestyle Med. 2021;15(3):224–226. doi: 10.1177/1559827621992271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pronk N.P., Kottke T.E., Isham G.J. Leveraging lifestyle medicine and social policy to extend the triple aim from the clinic into the community. Am J Lifestyle Med. 2013;7(6):360–366. doi: 10.1177/1559827613483433. [DOI] [Google Scholar]
- 89.Elswick S., O’Donnell L., Dinon N., Stachnik A., Rippe J. Incorporating lifestyle medicine into a large health care system: the Orlando health experience. Am J Lifestyle Med. 2011;5(2):192–199. doi: 10.1177/1559827610389131. [DOI] [Google Scholar]
- 90.Guthrie G.E. Money talks. Am J Lifestyle Med. 2017;11(5):373–374. doi: 10.1177/1559827616689557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gobble J., Donohue D., Grega M. Reimbursement as a catalyst for advancing lifestyle medicine practices. J Fam Pract. 2022;71(suppl 1 Lifestyle):eS105–eS109. doi: 10.12788/jfp.0255. [DOI] [PubMed] [Google Scholar]
- 92.Carlasare L.E. Defining the place of direct primary care in a value-based care system. WMJ. 2018;117(3):106–110. [PubMed] [Google Scholar]
- 93.A new care model for medicare patients. Lore. published 2023 https://www.lorehealthcare.com/model; [Google Scholar]
- 94.Beckman K. A New Approach for Lifestyle Medicine Payment. Am J Lifestyle Med. 2019;13(1):36–39. doi: 10.1177/1559827618795410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Vartiainen E. The North Karelia Project: Cardiovascular disease prevention in Finland. Glob Cardiol Sci Pract. 2018;2018(2):13. doi: 10.21542/gcsp.2018.13. [DOI] [PMC free article] [PubMed] [Google Scholar]