Abstract
Background
Sudarshan Kriya Yoga (SKY – a rhythmic cyclic breathing) is known to produce several physiological changes in human body. Earlier it has been reported that SKY improves cardiovascular modulations, namely increase in heart rate variability.
Objective
To observe the synchronization in oscillatory modulations in cardiac autonomic tone and ventilatory exchange during Long Sudarshan Kriya Yoga (LSKY). LSKY is a sequential combination of pranayama in ujjayi breath, bhastrika, and cyclic rhythmic breathing followed by yog-nidra.
Methods
Regular LSKY practitioners from the Art of Living community with more than two years of experience participated in the study (n = 22; age 40.09 ± 12.68). The Electrocardiogram (ECG), respiration, oxygen saturation, and concentrations of oxygen and carbon-di-oxide from exhaled air were recorded before and during LSKY. The time domain parameters of heart rate variability (HRV) were calculated from ECG. All parameters were compared and correlated at each stage of LSKY.
Results
Highly significant reciprocal correlation was found between HRV parameters and respiration rate during LSKY. Both O2 consumption and CO2 production increased significantly during three stages of pranayama and decreased towards the end of cyclic breathing. We also saw increased SPO2 simultaneously.
Conclusion
The autonomic parameters exhibited reciprocal response to respiratory rate and correlated well to the ventilatory parameters. Further during LSKY we observed enhanced synchronization. In conclusion the LSKY has a potential to influence cardiorespiratory parameters for improving the performance of both systems. LSKY - enhances oscillations in HRV that resets the autonomic system, indicative of better cardiac health and prepares body for better metabolic response. Such changes are capable of inducing resilience along with physiological, psychological relaxation and emotional well-being.
1. Introduction
The respiratory modulations are known to affect hemodynamics and neuronal oscillations. Complex dynamic cardio-neuro-respiratory interdependence is responsible for maintaining homeostasis. This may be the probable cause of the synchronization between cerebral hemispheres and increased high-frequency brain rhythms during LSKY [1]. Cardio-respiratory coupling occurs via various neuronal and mechanical regulatory mechanisms [2]. In healthy humans, heart rate (HR) is influenced by physical, mental, and social activities; subsequently, variable beat-to-beat fluctuations are induced in HR, and these physiological oscillations represent heart rate variability (HRV). The complex regulatory system interaction between the autonomic nervous system and heart rate describes it. It is a known indicator of a healthy cardiovascular system and reflects the homeostasis in organisms influenced by physical and psychological variables in their environment [3]. Better emotion regulation is related to high HRV with sizable cognitive improvement, better health, and lower stress levels, as the brain regions involved in regulating both HRV and emotion regulation are the same [4]. Reduced HRV is witnessed in depression, cardiovascular diseases like congestive heart failure, hypertension, and autoimmune diseases [5]. The beneficial effects of yogic breathing on HRV are already established [6]. Cardio-respiratory integration may impact gas exchange positively at the level of the lung via effectual ventilation/perfusion matching [7]. Cardiorespiratory phase synchronization increased during meditation [8]. This synchronization at a breath rate of 6 BPM (breath per minute) is induced during meditative practices; even in inexperienced Zen meditators [9,10].
The breath and the mind are closely connected in a bidirectional fashion. Yogic breathing induces relaxation; its therapeutic benefits have been scientifically validated widely. Benefits include promoting overall physical and mental wellness, self-awareness, improved pulmonary and cognitive functions, and other psychosomatic patterns [11]. The physiological benefits of slow yogic breathing are scientifically proven as a homeostasis regulator that optimizes ventilation, gas exchange, arterial oxygenation, and cardio-respiratory reserves. It also maximizes vagal tone, initiates, and maintains parasympathetic–sympathetic balance. Slow breathing increases respiratory sinus arrhythmia (RSA); a naturally occurring biological phenomenon; whereas fast breathing decreases it. It is a marker of neuro-cardiac communication that can offer crucial insight into the pathways linked to mental and physical health [12].
Several homeostatic mechanisms which keep the arterial blood partial pressures of carbon dioxide and oxygen constant also control the depth and rate of breathing. Yogic practices profoundly impact oxygen consumption, inducing hyper or hypometabolic effects. The oxygen consumption measurements may bring forth an understanding of the stress reaction and overall homeostatic balance. Multiple pathways controlled by the hypothalamus and the autonomic nervous system mediate stress responses. The autonomic nervous system alterations are characterized by parasympathetic withdrawal and sympathetic activation during day-to-day activities and pathological conditions. The sympathetic nervous system via sympatho-adrenal-medullary pathways summons the vital systems of the body that in turn increases oxygen consumption. Whereas, the parasympathetic nervous system by activating the relaxation response induces enhanced vagal activity thereby a hypometabolic state mediated which reduces physiological arousal that finally reduces oxygen consumption. Thus, the metabolic rate indicates autonomic activation and vice-versa [13].
Recently a study reported that yoga and meditation increase cardiopulmonary health, symptoms of well-being, self-efficacy, fitness, enhanced cognitive function, working memory, and decrease anxiety, post-traumatic stress disorder, depression, and negative affect [14].
Long Sudarshan Kriya Yoga (LSKY) is a contemplative practice, a holistic approach to well-being. It is a combination of different pranayama in varying breathing rates, pauses, resistance, and cyclic rhythms. The Art of Living (AOL) foundation conducts workshops to introduce LSKY which has been practiced and experienced worldwide by many. It is known to modulate psycho-physiological dynamics and experientially produce profound harmony in physical, mental, and emotional health. Research suggests that SKY reduces depression, anxiety, PTSD, and stress [15]. It has many therapeutic effects and significantly increases feelings of well-being, optimism, state of restful alertness, mental focus and improves emotion regulation [16]. In addition, SKY is associated with enhanced antioxidative status, and better immune functions and has been proven as potential therapeutic self-help in COVID19 [17,18]. LSKY increases HRV and parasympathetic tone which initiates the appropriate autonomic balance and enhanced cardio-respiratory coupling [[19], [20], [21]].
To our best knowledge, the cardio-respiratory synchronization and its ventilatory correlates during LSKY in healthy participants are sparsely studied. A complex interplay of linear and nonlinear subsystems delineates the cardio-respiratory and vascular systems [22]. In the present study, we have explicitly observed the linear correlates of cardio-respiratory synchronization and its cardio-ventilatory correlates.
2. Methodology
Twenty-two healthy volunteers with an average age of 40.09 ± 12.68 years, M: F: 9:13, average height 164.04 ± 9.89 cms, and an average weight of 61.07 ± 10.72 Kgs from the Art of Living community participated in the study. All participants had learned Long SKY under the guidance of an expert teacher during the Happiness program organized by the AOL Foundation. They were regular Sudarshan Kriya Yoga practitioners with more than two years of experience and those who consented to perform the practice with mask-on were included in the study. The experimental protocol was explained, and informed consent was taken. The ethical clearance was obtained from the Ethical Committee of Ved Vignan Maha Vidya Peeth (SSIAR/IEC/05).
2.1. The experimental protocol
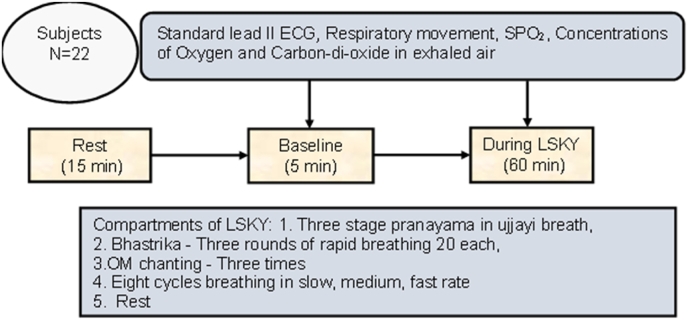
Participants were instructed to report after at least 2 h of light breakfast and before data acquisition they were made to rest for 15 min. The data was acquired for 65 min: 5 min before LSKY and 60 min during LSKY in a sitting position. The volunteers followed the recorded voice of HH Sri Sri Ravishankarji for instructions to perform LSKY, keeping their eyes closed. The study was conducted at Sri Sri Institute of Advanced Research (SSIAR), Ved Vignan Maha Vidhya Peeth (VVMVP), Bangalore. Fig. 1 describes the experimental protocol.
Fig. 1.
Details of the experimental protocol, recorded variables, and main compartments of LSKY.
2.2. Procedure for performing LSKY
LSKY is a combination of breathings with varying rates, resistance, and pauses, and it has six main sequential compartments: C1 - The three-stage pranayama; C2 - Rest after Pranayama; C3 - Bhastrika; C4 - Rest after Bhastrika; C5 - OM chanting & cyclic rhythmic breathing and C6 - Rest after cyclic breathing.
C1. Three stages of pranayama (P1, P2, & P3), sectional breathing at three different positions.
C2. Each stage is followed by 30 s of rest (P1 Rest, P2 Rest, & P3 Rest).
C3. Three rounds of Bhastrika pranayama (B1, B2, & B3), with 20 rapid exhalations in each round.
C4. Each round of Bhastrika is followed by 30 s rest (B1 Rest, B2 Rest, & B3 Rest).
C5. Three times Om chanting and eight cycles of cyclic rhythmic breathing in slow, medium, and fast pace (OM, SB1, MB1, FB1, SB2, MB2, FB2, SB3, MB3, FB3, SB4, MB4, FB4, SB5, MB5, FB5, SB6, MB6, FB6, SB7, MB7, FB7, SB8, MB8).
C6. Rest for 20 min (R1, R2, YN, and CR).
The intervention is 60 min in duration. The detailed procedure of LSKY has been described in earlier publications [1,20]. Refer to Table 1 for the description of the stages.
Table 1.
Shows details of stages of LSKY its description, respiration rate and duration of each stage
| S. No. | Stages of LSKY | Description | Respiration rate | Duration |
|---|---|---|---|---|
| 1 | Baseline | 5 min of data recording before the LSKY resting stage | Spontaneous | 300 s. |
| 2 | P1 | The first stage of Pranayama: Ujjayi breath: ratio of 4:4:6:2 (8 cycles). Abdominal breathing | 3-4 BPM | 180 s. |
| 3 | P1 Rest | Rest for 30 s keeping open palm on the knees | Spontaneous | 30 s |
| 4 | P2 | The second stage of Pranayama: Ujjayi breath: ratio of 4:4:6:2 (8 cycles) Thoracic breathing | 3-4 BPM | 180 s. |
| 5 | P2 Rest | Rest for 30 s keeping open palm on the knees | Spontaneous | 30 s |
| 6 | P3 | The third stage of Pranayama: Ujjayi breath: ratio of 4:4:6:2 (6 cycles) Clavicular breathing | 3-4 BPM | 150 s. |
| 7 | P3 Rest | Rest for 30 s keeping open palm on the knees | Spontaneous | 30 s |
| 7 | B1 | Bhastrika Round 1: 20 normal forceful exhalations, hands up & down | 20 BPM | 40 s |
| 8 | B1 Rest | Bhastrika Rest 1: Rest for 30 s keeping open palm on the knees | Spontaneous | 30 s |
| 9 | B2 | Bhastrika Round 2: 20 normal forceful exhalations, hands up & down | 20 BPM | 40 s |
| 10 | B2 Rest | Bhastrika Rest 2: Rest for 30 s keeping open palm on the knees | Spontaneous | 30 s |
| 11 | B3 | Bhastrika Round 3: 20 normal forceful exhalations, hands up & down | 20 BPM | 40 s |
| 12 | B3 Rest | Bhastrika Rest 3: Rest for 30 s keeping open palm on the knees | Spontaneous | 30 s |
| 13 | Om | Chanting Om three times | 5 BPM | 36 s |
| 14 | SB1 | Slow Breath cycle 1 | 14 BPM | 86 s |
| 15 | MB1 | Medium Breath cycle 1 | 37 BPM | 95 s |
| 16 | FB1 | Fast Breath Cycle 1 | 80 BPM | 53 s |
| 17 | SB2 | Slow Breath cycle 2 | 13 BPM | 51 s |
| 18 | MB2 | Medium Breath cycle 2 | 28 BPM | 128 s |
| 19 | FB2 | Fast Breath Cycle 2 | 83 BPM | 39 s |
| 20 | SB3 | Slow Breath cycle 3 | 14 BPM | 75 s |
| 21 | MB3 | Medium Breath cycle 3 | 39 BPM | 68 s |
| 22 | FB3 | Fast Breath Cycle 3 | 96 BPM | 20 s |
| 23 | SB4 | Slow Breath cycle 4 | 15 BPM | 74 s |
| 24 | MB4 | Medium Breath cycle 4 | 33 BPM | 81 s |
| 25 | FB4 | Fast Breath Cycle 4 | 86 BPM | 44 s |
| 26 | SB5 | Slow Breath cycle 5 | 16 BPM | 87 s |
| 27 | MB5 | Medium Breath cycle 5 | 38 BPM | 83 s |
| 28 | FB5 | Fast Breath Cycle 5 | 90 BPM | 32 s |
| 29 | SB6 | Slow Breath cycle 6 | 14 BPM | 66 s |
| 30 | MB6 | Medium Breath cycle 6 | 30 BPM | 85 s |
| 31 | FB6 | Fast Breath Cycle 6 | 95 BPM | 57 s |
| 32 | SB7 | Slow Breath cycle 7 | 11 BPM | 17 s |
| 33 | MB7 | Medium Breath cycle 7 with Hmmm Sound | 36 BPM | 31 s |
| 34 | FB7 | Fast Breath cycle 7 with Hmmm Sound | 109 BPM | 12 s |
| 35 | SB8 | Slow Breath cycle 8 | 13 BPM | 33 s |
| 36 | MB8 | Medium Breath Cycle 8 | 30 BPM | 32 s |
| 37 | Rest1 | Rest for 5 min | Spontaneous | 300 s |
| 38 | Rest2 | Rest for 5 min | Spontaneous | 300 s |
| 39 | YN | Yog nidra for 5 min | Spontaneous | 300 s |
| 40 | CR | Chanting of shloka and Rest for 5 min | Spontaneous | 300 s |
2.3. Data collection and analysis
Standard lead II ECG, respiratory movement, oxygen saturation, and concentrations of oxygen and carbon-di-oxide in exhaled air were recorded through PowerLab (AD Instruments, Australia) before and during LSKY. ECG signal was recorded with band-pass filters at the cut-off limits of 0.05–0 35 Hz frequencies at a sampling rate of 1 kHz Standard lead II ECG was recorded using disposable Ag-AgCl electrodes. A respiratory belt sensor was used to determine respiratory movements. The SpO2 finger clip with the appropriate oximeter pod was used to measure oxygen saturation. Gas analyzer ML206 was used to measure concentrations of oxygen and carbon-di-oxide in exhaled air. During data acquisition, 40 event markers were placed for every stage to observe dynamics in the oscillations of cardio-respiratory parameters and changes in the ventilatory exchange. A list of the markers for every stage is given in Table .1.
LabChart 8 was used to record and analyze the data. Time domain parameters of HRV (standard deviation of all NN intervals (SDNN), square root of the mean of the sum of the squares of differences between adjacent NN intervals (RMSSD), NN50 count divided by the total number of all NN intervals (pNN50), and difference between maximum & minimum heart rate (Delta HR)) were calculated from the HRV module of LabChart for every stage of LSKY. Frequency domain analysis of HRV was not attempted as the epoch size for each event was not adequate. Standard HRV parameters are well recognized for their physiological significance [3]. The SDNN reflects the overall short-term heart rate variability, influenced by both sympathetic and parasympathetic nervous activity. The RMSSD, pNN50, and Delta HR reflect short-term heart rate fluctuations, which represent parasympathetic activity and vagal tone [23]. Delta HR also represents respiratory sinus arrhythmia. Time domain parameters of HRV were calculated for 12 participants with noise-free ECG and no motion artifacts during all stages of LSKY. HRV was not calculated during Bhastrika due to motion artifacts.
Concentrations of oxygen consumed (%) and carbon-di-oxide produced (%) were calculated as follows in equations:
Oxygen consumed (%) = 21 (Atmospheric O2 in %) – observed oxygen (%) in exhaled air.
Carbon-di-oxide produced (%) = Observed CO2 (%) −0.04 (Atmospheric CO2 in %) in exhaled air. Oxygen saturation in % was calculated by LabChart as a direct value.
2.4. Statistical analysis
Three normality test namely Kolmogorov-Smirnov test, D'Agostino and Pearson Ombibus normality test, and Shapiro-Wilks normality Test were applied for the normality screening of data. Data was considered parametric if two tests were passed. Non-parametric data were transformed into parametric by log transformation. Repeated measures of ANOVA were applied, and post hoc analysis was done using Tukey's Multiple Comparison Test to compare 39 stages of LSKY with Baseline. For non-parametric data, Friedman's test was applied. A p-value of equal to or less than 0.05 levels was considered significant. GraphPad Prism 5.0 was used for statistical analyses.
3. Results
3.1. Time domain parameters of HRV
To observe cardio-respiratory synchronization, time domain parameters of HRV and breathing rate were plotted for all stages of LSKY with respiration rate as an independent parameter. High synchronization was observed between the HRV parameters and respiration rate (Fig. 2). To confirm this synchronization Correlation coefficient was calculated between time domain parameters and respiration rate for all stages of LSKY and compartments of LSKY (Table .2). A highly significant and reciprocal correlation between respiration rate and RMSSD, pNN50, SDNN, & delta HR was found during all stages, and C5 of LSKY and non-significant during C1, C2, C4, and C6 (Fig. 3). Correlation was direct during C1 and C4. The HRV parameters for C3 were not calculated due to motion artifacts. No significant change was found in all time domain parameters during all stages of LSKY.
Fig. 2.
Shows strong reciprocal synchronization between respiration rate (shaded area) and Average HR, SDNN, RMSSD, Delta HR and pNN50, where respiration event precedes changes in cardiac parameter. HR- Heart rate, SDNN-standard deviation of all NN intervals (ms), RMSSD-square root of the mean of the sum of the squares of differences between adjacent NN intervals in (ms), pNN50-NN50 count divided by the total number of all NN intervals in (%) and Delta HR- (maximum HR – minimum HR). Repeated measures of ANOVA were non-significant for all parameters during LSKY (n = 12).
Table 2.
Shows correlation coefficient values between respiration rate and time domain parameters of HRV. Correlation between SDNN and parasympathetic parameters RMSSD, pNN50 and Delta HR was significantly very high during all stages of LSKY and C5, P*** = <0.001
| S. No. | Correlation with respiration rate (RR) | All stages of LSKY | C1 (P1, P2, P3) | C2 (P1 Rest, P2 Rest, P3 Rest) | C4 (B1 Rest, B2 Rest, B3 Rest) | C5(Cyclic rhythmic breathing) | C6 (R1, R2, R3,R4) |
| 1 | RR & RMSSD | −0.81*** | 0.38 | −0.81 | 0.55 | −0.91*** | −0.67 |
| 2 | RR & SDNN | −0.69*** | 0.57 | −0.24 | 0.44 | −0.70*** | −0.35 |
| 3 | RR & pNN50 | −0.66*** | −0.41 | −0.77 | 0.39 | −0.89*** | 0.07 |
| 4 | RR & Delta HR | −0.71*** | 0.21 | −0.66 | 0.26 | −0.68*** | −0.46 |
| Correlation with SDNN | |||||||
| 6 | SDNN & RMSSD | 0.80*** | 0.97 | 0.99 | 0.99 | 0.84*** | 0.925 |
| 7 | SDNN & pNN50 | 0.62*** | 0.50 | 0.80 | 0.99 | 0.79*** | 0.75 |
| 8 | SDNN & Delta HR | 0.93*** | 0.92 | 0.88 | 0.98 | 0.94*** | 0.63 |
| Correlation with RMSSD | |||||||
| 10 | RMSSD & pNN50 | 0.88*** | 0.68 | 0.99*** | 0.98 | 0.96*** | 0.57 |
| 11 | RMSSD & Delta HR | 0.75*** | 0.98 | 0.97*** | 0.95 | 0.86*** | 0.67 |
| 12 | pNN50 & Delta HR | 0.56*** | 0.79 | 0.98 | 0.99 | 0.82*** | −0.00 |
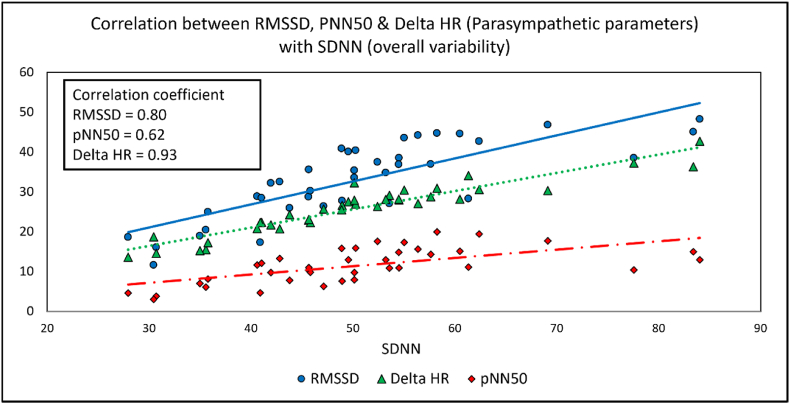
Fig. 3.
Shows high reciprocal correlation between respiration rate and RMSSD, SDNN, pNN50 & Delta HR during LSKY. The values of cardiac parameters are low during fast breathing, increased during medium breathing, and highest during slow and very slow breathing. (n = 12).
All parasympathetic parameters RMMSD, pNN50 and Delta HR were highly correlated with SDNN during all stages of LSKY, and C5 indicating that parasympathetic activity has contributed significantly to the variation of overall HRV (Fig. 4). The significant correlation between RMSSD, pNN50 and Delta HR further strengthen the parasympathetic dominance during all stages and C5 of LSKY. Interestingly, all parameters were within normal limits despite repeated activation and deactivation of overall HRV and parasympathetic activity with the change in breathing rate.
Fig. 4.
Shows a graphic relationship between SDNN (overall HRV) and RMSSD, pNN50 & Delta HR (parasympathetic parameters) indicating that change in HRV, and parasympathetic parameters were oscillating in synchronization with the modulations of respiration rate during LSKY (n = 12).
3.2. Oxygen consumption (O2), carbon-di-oxide production (CO2) and oxygen saturation (SPO2)
O2 consumption and CO2 production significantly altered during three stages of pranayama in slow ujjayi breath and during slow, medium, and fast rhythmic breathing in 7–8 cycles of LSKY. All the values of concentrations of oxygen consumption, carbon-di-oxide production and SPO2 were mainly found under normal physiological limits during LSKY. Absolute values of O2 consumption during three stages of pranayama were significantly increased, ranging from 2.55 to 3.15 % and decreased significantly during slow, medium, and fast rhythmic breathing in 7–8 cycles of LSKY ranging from 0.97 to 2.29 % as compared to Baseline 2.15 %. Absolute values of CO2 production during three stages of pranayama were significantly increased, ranging from 3.16 to 3.57 % and decreased significantly during slow, medium, and fast rhythmic breathing in 7–8 cycles of LSKY ranged from 1.82 to 3.05 % as compared to Baseline 2.82 %. SPO2 increased significantly in the last 4 phases of cyclic rhythmic breathing of LSKY (C5), i.e., SB7, MB7, FB7 and SB8, compared with Baseline. Overall, a trend of increase in SPO2 at all stages of LSKY is observed. Absolute values of SPO2 during LSKY ranged from 97.03 to 98.08 %. Refer to Table .3 presenting percentage change with respect to Baseline in O2, CO2 and SPO2 with significance and Fig. 5 demonstrating the change in parameters with change in the breathing rate. A highly significant correlation was observed between respiration rate and the ventilatory parameters: O2 consumption, CO2 production, their ratios and SPO2 during LSKY and C5. The correlation between HRV parameters SDNN & RMSSD with ventilatory parameters was also highly significant (Table .4).
Table 3.
Percentage change in oxygen consumption and carbon-di-oxide production and oxygen saturation with respect to Baseline during 40 stages of LSKY. P*<0.05, **<0.01, ***<0.001
| S. No | Stages of LSKY | % Change w.r.t. Baseline (SPO2) | % Change w.r.t. Baseline (O2) | % Change w.r.t. Baseline (CO2) | % Change w.r.t. Baseline (CO2/O2) |
|---|---|---|---|---|---|
| 1 | Baseline | ||||
| 2 | P1 | 0.05 | 18.69*** | 12.12*** | −2.80 |
| 3 | P1 Rest | 0.31 | 39.14*** | 23.11*** | −10.67 |
| 4 | P2 | 0.18 | 36.73*** | 23.04m*** | −9.49 |
| 5 | P2 REST | −0.11 | 46.72*** | 26.41*** | −13.83 |
| 6 | P3 | 0.14 | 40.03*** | 24.71*** | −11.41 |
| 7 | P3 REST | 0.12 | 45.61 | 26.69 | −14.13 |
| 8 | B1 | −0.04 | 7.48 | 11.66 | 4.56 |
| 9 | B1 REST | 0.60 | −20.27 | 1.13 | 28.33** |
| 10 | B2 | −0.56 | −10.27 | 2.34 | 13.76 |
| 11 | B2 REST | 0.40 | −19.43 | −0.60 | 29.87 |
| 12 | B3 | −0.29 | −8.23 | 1.63 | 10.30 |
| 13 | B3 REST | 0.35 | −13.48 | 0.04 | 16.63 |
| 14 | OM | −0.11 | 2.51 | 3.47 | 5.08 |
| 15 | SB1 | 0.69 | 6.79 | 8.26 | 1.40 |
| 16 | MB1 | 0.69 | −16.83*** | −6.52*** | 18.25 |
| 17 | FB1 | 0.61 | −38.17*** | −22.08*** | 39.29 |
| 18 | SB2 | 0.68 | −35.52 | −19.74 | 35.10*** |
| 19 | MB2 | 0.59 | −25.48*** | −13.51*** | 20.31 |
| 20 | FB2 | 0.66 | −36.40*** | −21.41*** | 30.68** |
| 21 | SB3 | 0.79 | −33.84* | −19.60* | 27.15* |
| 22 | MB3 | 0.52 | −28.41*** | −16.27*** | 19.43 |
| 23 | FB3 | 0.52 | −35.10 | −21.84 | 25.31 |
| 24 | SB4 | 0.73 | −32.08 | −19.32 | 23.18 |
| 25 | MB4 | 0.49 | −24.69*** | −15.28*** | 11.41 |
| 26 | FB4 | 0.26 | −38.59** | −26.23** | 22.22 |
| 27 | SB5 | 0.84 | −31.10* | −18.82** | 20.53 |
| 28 | MB5 | 0.59 | −30.08*** | −18.33*** | 18.18 |
| 29 | FB5 | 0.47 | −39.47*** | −24.46*** | 29.95** |
| 30 | SB6 | 0.75 | −36.54 | −21.59** | 25.90 |
| 31 | MB6 | 0.59 | −27.06 | −18.01 | 14.20* |
| 32 | FB6 | 0.42 | −44.82*** | −28.18*** | 29.95** |
| 33 | SB7 | 0.60*** | −54.57*** | −35.20*** | 57.91*** |
| 34 | MB7 | 1.19*** | −38.26*** | −23.22*** | 27.89*** |
| 35 | FB 7 | 1.29*** | −44.77*** | −25.20*** | 40.62*** |
| 36 | SB8 | 1.13* | −43.51 | −25.63 | 34.22*** |
| 37 | MB8 | 0.99 | −25.01 | −14.96* | 19.43 |
| 38 | Rest 1 | 0.22 | −20.36 | −16.06 | 11.33 |
| 39 | Rest 2 | −0.57 | 2.70 | −8.26 | −8.17 |
| 40 | YN | 0.20 | 6.79 | −2.38 | −6.40 |
| 41 | CR | 0.15 | 5.16 | −3.23 | −7.87 |
Fig. 5.
Showing Respiration rate (as shaded area), concentrations of oxygen and carbon-di-oxide in exhaled air (in percentage) and their ratio during all stages of LSKY. During pranayama in very slow ujjayi breathing O2 consumption and CO2 production increased significantly and decreased during cyclic rhythmic breathing. Ratio of CO2/O2 was also significantly increased during 7th and 8th cycles of rhythmic cyclic breathing. For significance refer Table .4.
Table 4.
Correlation between oxygen consumption, carbon-di-oxide production, and oxygen saturation with respiration rate, SDNN & RMSSD P*<0.05, **<0.01, ***<0.001
| S. No. | Correlation with respiration rate (RR) | All stages of LSKY | C1 (P1, P2, P3) | C2 (P1 Rest, P2 Rest, P3 Rest) | C4 (B1 Rest, B2 Rest, B3 Rest) | C5 (Cyclic rhythmic breathing) | C6(R1, R2,R3,R4) |
|---|---|---|---|---|---|---|---|
| 1 | O2 consumption | −0.53*** | −0.90 | −0.10 | 0.04 | −0.47* | −0.76 |
| 2 | CO2 production | −0.54*** | 1.00 | 0.03** | 1.00 | −0.44* | −0.91 |
| 3 | CO2/O2 | 0.56** | −1.00 | −0.26 | −0.45 | 0.46* | 0.64 |
| SPO2 | 0.34** | 0.10 | −0.53 | 0.86 | 0.07 | −0.24 | |
| Correlation within ventilatory parameters | |||||||
| 5 | O2 & CO2 | 0.98*** | 1.00** | 0.99 | 0.05 | 0.98*** | 0.93** |
| O2 & CO2/O2 | −0.92*** | −1.00 | −0.94 | −0.91 | −0.87*** | −0.94 | |
| CO2 & CO2/O2 | −0.86** | −1.00* | −0.97 | −0.46 | −0.82*** | −0.97 | |
| 4 | SPO2&O2 | −0.62 | 0.10 | 0.10 | −0.47 | −0.13 | −0.35 |
| Correlation with SDNN | |||||||
| 6 | O2 consumption | 0.54*** | −0.16 | 0.99 | 0.99 | 0.33 | 0.85 |
| 7 | CO2 production | 0.54*** | −0.19 | 0.96 | 0.96 | 0.28 | 0.60 |
| 8 | CO2/O2 | −0.49*** | 0.26 | −0.87 | −0.87 | −0.32 | −0.92 |
| 9 | SPO2 | −0.47*** | 0.96 | −0.69 | −0.69 | −0.42* | −0.79 |
| Correlation with RMSSD | |||||||
| 10 | O2 consumption | 0.43** | 0.06 | 0.66 | 0.66 | 0.35 | 0.97** |
| 11 | CO2 production | 0.42** | 0.03 | 0.56 | 0.56 | 0.32 | 0.83 |
| 12 | CO2/O2 | −0.42** | 0.03 | −0.35 | −0.35 | −0.34 | −0.98* |
| 13 | SPO2 | −0.30 | 1.00* | −0.06 | −0.06 | −0.18 | −0.53 |
Table 3 is showing that oxygen consumption and carbon-di-oxide production increased significantly during three stages pranyama (P1, P2 &P3) and reduced significantly during the eight cycles of cyclic rhythmic breathing in slow, medium, and fast pace. Simultanoeusly in 7th & 8th cycle of Sudarshan kriya SPO2 and ratio of CO2/O2 increased significantly.
Table 4 is showing Oxygen consumption, carbon-di-oxide production & their ratio, and Oxygen saturation increased significantly during all stages of LSKY. A highly significant correlation was observed between respiration rate and the ventilatory parameters: O2 consumption, CO2 production, their ratios and SPO2 during LSKY and C5. The correlation between HRV parameters SDNN & RMSSD with ventilatory parameters was also highly significant indicating cardiovascular and respiratory synchronization.
4. Discussion
Respiration entrains modulation in cardiac-vascular oscillations and ventilatory exchange as well. Cardio-respiratory synchronization reflects a reciprocal interaction between autonomic and respiratory control systems, and the ventilatory correlates are also modulated by the cardiovascular system [2]. Multiple complementary mechanisms mediate respiration's influence on cardiovascular function. The main findings of the study suggest that.
-
i.
A strong cardio-respiratory coupling was recognized with a highly significant reciprocal correlation coefficient between time domain parameters of HRV (SDNN, RMSSD, Delta HR and pNN50) and respiration rate during all stages and cyclic breathing of LSKY (C5). A highly significant direct correlation between overall variability and parasympathetic parameters indicates an increase in overall HRV and increased contribution of parasympathetic activity.
-
ii.
The concentrations of O2 and CO2 increased significantly during three-stage pranayama and decreased during cyclic breathing of LSKY in exhaled air. These values correlated significantly with the respiration rate during all stages of LSKY, this finding indicates ventilatory variability with respiration rate.
-
iii.
The significant correlation between overall HRV and parasympathetic parameters with the concentrations of O2 and CO2 during all stages of LSKY indicates real-time interaction between the two systems with the variation in the respiration rate.
The underlying mechanisms of the above findings can be understood considering the proposed model and hypothesis. The underlying neurophysiological mechanism of Sudarshan kriya was earlier postulated by Brown et al. based on the polyvagal theory and vagus nerve stimulation [24]. The neurovisceral integration model (NVM) proposes that the central autonomic network (CAN) operates through a series of feedback loops within the central nervous system, including autonomic nervous system. Different heart rates are associated with changes in the functional coupling between CAN [25]; it increases significantly at lower heart rate. This indicates a strong relationship between functional connectivity in the cortico-subcortical circuit and heart rate regulation [26]. The higher functional connectivity indicates that slow oscillations in heart rate strengthen the brain network connectivity and exert a positive effect on emotion regulation and self-control [27]. The cyclic rhythmic breathing during LSKY may probably induce high amplitude oscillations in HRV that generate concurrent high amplitude physiological oscillations and stimulate the oscillations in the same brain regions involved in emotion regulation [4]. Thus, increased modulations in HRV during LSKY may entrain the brain rhythms and strengthens the regulatory brain networks responsible for emotional well-being. Repeated brief episodes of synchronized activity can strengthen its internal pathways and lead to enhanced and coordinated functional connectivity in emotion regulation networks [28]. Improvement in physical and mental wellbeing with an increase in HRV, and parasympathetic dominance along with improved autonomic balance, high frequency cerebral activation, and appropriate coherence between the cerebral hemispheres following LSKY have already been established in our earlier studies [1,20].
Voluntary interventions in the form of sequential cyclic breathing with slow, medium, and fast respiration rates during LSKY induce mild challenges under normal physiological limits. This intervention is responsible for inducing perturbations in the HRV, reflected in RMSSD, pNN50, and Delta HR values changed with respiration rate. These autonomic perturbations will likely make the system resilient with daily and regular practice. The cardio-respiratory synchronization during LSKY may involve CAN as proposed in NVM; therefore, autonomic, and emotional control improves with the practice.
During slow deep breathing slowly adapting receptors (SARs) are supposed to be recruited preferentially due to stretch in lung tissues. These activated pathways project discrete areas in the brain stem within the nucleus of the solitary tract (NTS), that may lead to the modulation of the autonomic nervous system [29,30]. High breathing rate (close to the resting heart rate) induces direct neuronal communication between the respiration and heart centres in the brain. This cardio-respiratory synchronization at both low and high breathing rates is associated with a common underlying communication mechanism [31]. It is likely that, during LSKY repeated episodes of voluntarily induced transient high frequency breathing in the range of 80–109 breaths per minute altered with slow (3–11 breaths per minute) and medium breathing may also induce direct neuronal communication between the lung and heart.
Tyagi & Cohen have reported in their review that O2 consumption increases with various pranayama practices performed at both fast (232 breath/min) and slow (1 breath/min) rates [13], similarly, we found increased O2 consumption in both C1 (with slow breathing in ujjayi breath) and C3 (fast breathing in bhastrika). Whereas when the cyclic breathing was performed with alternate slow and fast breathing for less the 1-min duration each, the O2 consumption was varying with the breathing rate below the baseline value and significantly low during most of the cycles. O2 consumption was lowest at the 7th cycle of LSKY and SPO2 was also highest at this point, this suggests a hypometabolic state with normal circulation. So, during cyclic breathing the response to the system was better in terms of oxygen consumption that reduced to a lower level.
Respiration is the only system where involuntary commands are modulated by voluntary actions, yet the limits of volition cannot be impelled as central command overrides after a point, therefore respiratory intervention can never go to the level of coercion. Intervention through breathing manoeuvring in a specific sequence in LSKY may entrain the brain rhythms and synchronize with the heart. Enhancing parasympathetic action by pranayama in ujjayi breath followed by enhancement of sympathetic activity by bhastrika and then act of balance with Om chanting, these three steps make our autonomic nervous system up and running. Then, the next eight of cycles of slow, medium, and fast breathing activates CAN differentially and helps in ensuing perturbations in the system. Repeated activation and deactivation of both limbs of autonomic nervous system helps in the recruitment of many overlapping pathways of CAN. These multi-regulatory pathways activate limbic system, hypothalamus, prefrontal cortex along with tonic control of autonomic reflexes and respiration. Also, increased HRV oscillations with increased parasympathetic contribution during cyclic breathing add to this relaxed state. This helps in reduced mentation, improved attention, better emotional control and state of musculoskeletal quiescence or low metabolic state, thereby reaching to a relative parasympathetic dominance. This makes us believe that regular and long-term practice of LSKY will make the person more resilient for day-to-day stressors.
4.1. Limitations of the study
Linear approaches might be insufficient to quantify nonlinear structures and the complexity of physiological (sub)systems and lack of control group in the study. Therefore, in future studies approaches from nonlinear time-series analysis can be applied to capture complex interactions between time series by using Granger causality, nonlinear prediction, entropy, and phase synchronization. Assessment of Ventilatory parameters and metabolic equivalents along with HRV and oxygen consumption will make study comprehensive. Also, addition of control group will improve the strength of the study.
5. Conclusion
LSKY induces cardio-respiratory synchronization and ventilatory variability with slow, medium, and fast breathing. The autonomic parameters exhibited reciprocal response to respiratory rate and correlated well to the ventilatory parameters. Further during LSKY we observed enhanced synchronization. In conclusion the LSKY has a potential to influence cardiorespiratory parameters for improving the performance of both systems. Voluntarily induced transient episodes of high and low frequency breathing enhances oscillations in HRV that resets the autonomic system, indicative of better cardiac health and prepares body for better metabolic response. Such changes are capable of inducing resilience along with physiological, psychological relaxation and emotional well-being.
Author contributions statement
DC, CK, PS, KKD & VK were key persons in Conceptualization of the study. DC, CK and VK worked for the Methodology/Study design. Formal analysis was done by DC, CK, AP and OLB. Investigations were done by DC and AP. DC, CK, AP, PS, OLB, KKD, and VK were Resources for the study. Data curation was done by DC, AP and OLB. Original draft was written by CK and OLB. Reviewing and editing was done by CK, PS, OLB, KKD and VK. Visualization was done by CK, OLB, KKD & VK. The study was supervised by DC, CK, PS, and VK. Project administration was done by DC, AP and VK. Financial acquisition: None of the authors receive any financial support for this study. All authors validated and approved the final version of the manuscript. All persons designated as authors qualify for authorship, and all those who qualify for authorship are listed.
Sources of funding
No funding from any funding agency was utilized for the conduct of this study.
Data availability statement
The data used in this study will be available on request.
Declaration of generative AI in scientific writing statement
No generative AI is used in scientific writing statements.
Declaration of competing interest
The authors declare no competing or financial interests.
Acknowledgment
We gratefully acknowledge the help and support of Sri Sri Institute for Advanced Research (SSIAR), Ved Vignan Maha Vidhya Peeth (VVMVP) for allowing us to use the required facilities to carry this work. We are thankful to all volunteers who participated and successfully completed the study.
References
- 1.Bhaskar L., Tripathi V., Kharya C., Kotabagi V., Bhatia M., Kochupillai V. High-frequency cerebral activation and interhemispheric synchronization following sudarshan kriya yoga as global brain rhythms: the state effects. Int J Yoga. 2020;13(2):130. doi: 10.4103/IJOY.IJOY_25_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dick T.E., Hsieh Y.H., Dhingra R.R., et al. Cardiorespiratory coupling: common rhythms in cardiac, sympathetic, and respiratory activities. Prog Brain Res. 2014;209:191. doi: 10.1016/B978-0-444-63274-6.00010-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Merrick J., Grippo A.J., Bartlett G., Shaffer F., Ginsberg J.P. Article 258 1 citation: shaffer F and Ginsberg JP (2017) an overview of heart rate variability metrics and norms. Front Public Health. 2017;5:258. doi: 10.3389/fpubh.2017.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thayer J.F., Åhs F., Fredrikson M., Sollers J.J., Wager T.D. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. 2012;36(2):747–756. doi: 10.1016/j.neubiorev.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Westhoff-Bleck M., Lemke L.H., Bleck J.M.S., Bleck A.C., Bauersachs J., Kahl K.G. Depression associated with reduced heart rate variability predicts outcome in adult congenital heart disease. J Clin Med. 2021;10(8) doi: 10.3390/JCM10081554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tyagi A., Cohen M. Yoga and heart rate variability: a comprehensive review of the literature. Int J Yoga. 2016;9(2):97. doi: 10.4103/0973-6131.183712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yasuma F., Hayano J.I. Respiratory sinus arrhythmia: why does the heartbeat synchronize with respiratory rhythm? Chest. 2004;125(2):683–690. doi: 10.1378/chest.125.2.683. [DOI] [PubMed] [Google Scholar]
- 8.Wu S da, Lo P.C. Cardiorespiratory phase synchronization during normal rest and inward-attention meditation. Int J Cardiol. 2010;141(3):325–328. doi: 10.1016/J.IJCARD.2008.11.137. [DOI] [PubMed] [Google Scholar]
- 9.Peng C.K., Henry I.C., Mietus J.E., et al. Heart rate dynamics during three forms of meditation. Int J Cardiol. 2004;95(1):19–27. doi: 10.1016/J.IJCARD.2003.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Cysarz D., Büssing A. Cardiorespiratory synchronization during Zen meditation. Eur J Appl Physiol. 2005;95(1):88–95. doi: 10.1007/S00421-005-1379-3. [DOI] [PubMed] [Google Scholar]
- 11.Jayawardena R., Ranasinghe P., Ranawaka H., Gamage N., Dissanayake D., Misra A. Exploring the therapeutic benefits of pranayama (yogic breathing): a systematic review. Int J Yoga. 2020;13(2):99. doi: 10.4103/IJOY.IJOY_37_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tonhajzerova I., Mestanik M., Mestanikova A., Jurko A. Respiratory sinus arrhythmia as a non-invasive index of “brain-heart” interaction in stress. Indian J Med Res. 2016;144(6):815–822. doi: 10.4103/IJMR.IJMR_1447_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tyagi A., Cohen M. Oxygen consumption changes with yoga practices: a systematic review. J Evid Based Complementary Altern Med. 2013;18(4):290–308. doi: 10.1177/2156587213492770. [DOI] [Google Scholar]
- 14.Gerritsen R.J.S., Band G.P.H. Breath of life: the respiratory vagal stimulation model of contemplative activity. Front Hum Neurosci. 2018;12:9. doi: 10.3389/FNHUM.2018.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vasudev K., Ionson E., Inam S., et al. Sudarshan kriya yoga program in posttraumatic stress disorder: a feasibility study. Int J Yoga. 2020;13(3):239. doi: 10.4103/IJOY.IJOY_16_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zope S.A., Zope R.A. Sudarshan kriya yoga: breathing for health. Int J Yoga. 2013;6(1):4. doi: 10.4103/0973-6131.105935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma H., Sen S., Singh A., Bhardwaj N.K., Kochupillai V., Singh N. Sudarshan Kriya practitioners exhibit better antioxidant status and lower blood lactate levels. Biol Psychol. 2003;63(3):281–291. doi: 10.1016/S0301-0511(03)00071-1. [DOI] [PubMed] [Google Scholar]
- 18.Zope S.A., Zope R.A., Biri G.A., Zope C.S. Sudarshan kriya yoga: a breath of hope during COVID-19 pandemic. Int J Yoga. 2021;14(1):18. doi: 10.4103/IJOY.IJOY_102_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kharya C., Gupta V., Deepak K.K., et al. Effect of controlled breathing exercises on the psychological status and the cardiac autonomic tone: sudarshan Kriya and Prana-Yoga. Indian J Physiol Pharmacol. 2014;58(3) [PubMed] [Google Scholar]
- 20.Bhaskar L., Kharya C., Deepak K.K., Kochupillai V. Assessment of cardiac autonomic tone following long sudarshan kriya yoga in Art of living practitioners. J Alternative Compl Med. 2017;23(9) doi: 10.1089/acm.2016.0391. [DOI] [PubMed] [Google Scholar]
- 21.Toschi-Dias E., Tobaldini E., Solbiati M., et al. Sudarshan Kriya Yoga improves cardiac autonomic control in patients with anxiety-depression disorders. J Affect Disord. 2017;214:74–80. doi: 10.1016/J.JAD.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Schulz S., Adochiei F.-C., Edu I.-R., Schroeder R., Costin H., Bär K.-J., Voss A. Cardiovascular and cardiorespiratory coupling analyses: a review. Phil Trans R Soc A. 2013;371 doi: 10.1098/rsta.2012.0191. [DOI] [PubMed] [Google Scholar]
- 23.Laborde S., Mosley E., Thayer J.F. Heart rate variability and cardiac vagal tone in psychophysiological Research – recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017;8:213. doi: 10.3389/fpsyg.2017.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brown R.P., Gerbarg P.L. Sudarshan Kriya Yogic Breathing in the Treatment of Stress, Anxiety, and Depression: Part I—Neurophysiologic Model. 2005;11(1):189–201. doi: 10.1089/ACM.2005.11.189. https://home.liebertpub.com/acm [DOI] [PubMed] [Google Scholar]
- 25.Thayer J.F., Lane R.D. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61(3):201–216. doi: 10.1016/s0165-0327(00)00338-4. [DOI] [PubMed] [Google Scholar]
- 26.Mather M., Thayer J. How heart rate variability affects emotion regulation brain networks. Curr Opin Behav Sci. 2018;19:98–104. doi: 10.1016/j.cobeha.2017.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de la Cruz F., Schumann A., Köhler S., Reichenbach J.R., Wagner G., Bär K.J. The relationship between heart rate and functional connectivity of brain regions involved in autonomic control. Neuroimage. 2019;196:318–328. doi: 10.1016/j.neuroimage.2019.04.014. [DOI] [PubMed] [Google Scholar]
- 28.Ma L., Narayana S., Robin D.A., Fox P.T., Xiong J. Changes occur in resting state network of motor system during 4 Weeks of motor skill learning. Neuroimage. 2011;58(1):226. doi: 10.1016/J.NEUROIMAGE.2011.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noble D.J., Hochman S. Hypothesis: pulmonary afferent activity patterns during slow, deep breathing contribute to the neural induction of physiological relaxation. Front Physiol. 2019;10:1176. doi: 10.3389/FPHYS.2019.01176/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jerath R., Edry J.W., Barnes V.A., Jerath V. Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med Hypotheses. 2006;67(3):566–571. doi: 10.1016/J.MEHY.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 31.Perry S., Khovanova N.A., Khovanov I.A. Control of heart rate through guided high-rate breathing. Sci Rep. 2019;9(1) doi: 10.1038/s41598-018-38058-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in this study will be available on request.