Abstract
Objectives:
Bowel preparation is burdensome because of long cleansing times and large dose volumes of conventional polyethylene glycol (PEG) lavage solution NiflecⓇ (Nif). MoviPrep (Mov)Ⓡ is a hyperosmolar preparation of PEG, electrolytes, and ascorbic acid; despite the smaller dose volume of 2 L, it can be challenging for many patients. We examined a more effective and acceptable bowel preparation method without compromising cleanliness and effectiveness, combining low-residue diet and laxative (Modified Brown Method) in Mov administered 1 day pre-colonoscopy.
Methods:
This multicenter, randomized, open-label, parallel-group comparative study, conducted at Hiroshima University Hospital and 7 affiliated hospitals in May 2015-March 2016, evaluated adherence to and effectiveness of Mov in bowel preparation. Participants (n=380) were allocated to receive 1 of 3 pre-colonoscopy regimens: Nif+Modified Brown Method (Group A), Mov+Modified Brown Method (Group B), or Mov+Laxative (Group C).
Results:
Total intake volume showed no significant difference among the groups. Bowel preparation time was significantly shorter in Group B (112.4±44.8 min, n=118) than in Groups A (131.3±59 min, n=105) and C (122.6±48.1 min, n=115). Sleep disturbance (37%) was significantly higher in Group B than Group A; distension (11%) was significantly lower in Group C than in Groups A and B (p<0.05, respectively). No severe adverse events occurred in any group.
Conclusions:
Mov+Modified Brown method provided significantly shorter bowel preparation time, with no significant difference in total intake volume among the regimens. Mov+Laxative yielded significantly less distension than the other groups, with bowel preparation equivalent to that of the Nif+Modified Brown method.
Keywords: colonoscopy, bowel preparation, MoviPrepⓇ, Modified Brown Method
Introduction
Colonoscopy is considered the most effective procedure for early detection and prevention of colorectal cancer[1-3]. Bowel preparation is one of the most important requirements to ensure complete colonoscopy. Inadequate bowel preparation can result in a colonoscopy of poor quality, a decreased possibility of missed lesions, and a decreased adenoma detection rate. Polyethylene glycol lavage solution (PEG-LS) is an isosmotic non-absorbable polymer commercially available as NiflecⓇ (Nif; Ajinomoto Co., Inc., Tokyo, Japan) and is generally used for bowel preparation. However, the main disadvantage of Nif is that a large volume, typically 4 L, is needed[4]. This 4-L volume of Nif is frequently used but is a burden to patients because of the long cleansing time and large dose volume. To address this, we previously reported that the required volume of Nif could be reduced to around 1 L with concomitant use of a low-residue diet and laxatives (Modified Brown Method; article in Japanese)[5].
MoviPrepⓇ (Mov; EA Pharma Co., Ltd., Tokyo, Japan), which was developed by adding ascorbic acid to the standard PEG-LS, has been marketed as a bowel-cleansing solution in Japan since 2013. Standard PEG-LS is an isotonic preparation containing a polymer of PEG and electrolytes, whereas MoviPrepⓇ is a hyperosmolar preparation of PEG, electrolytes, and ascorbic acid that provides comparable colonic irrigation with low dosage by hypertonic treatment[6,7]. Thus, when using Mov, a smaller dosage is required compared with Nif.
In Japan, a phase III trial was conducted to evaluate the efficacy, acceptability, tolerability, and safety of Mov compared with Nif without food restriction and laxatives. The study found that about 1.6 L Mov is required to achieve optimal preparation for colonoscopy (unpublished results of the phase III Japanese PEG-Asc clinical trial, provided by Ajinomoto Pharmaceutical Co.). This 1.6 L of Mov is still not an easy quantity to take, and further improvement is necessary to improve acceptability and reduce the total intake volume of Mov until irrigation is complete.
We therefore designed this study to determine a more effective method of bowel preparation with superior acceptability without compromising bowel cleanliness and effectiveness by combining a low-residue diet and laxatives in Mov on the day before total colonoscopy.
Methods
This multicenter, randomized, open-label, parallel-group comparative study to evaluate adherence to and effectiveness of Mov in bowel preparation for colonoscopy was conducted at Hiroshima University Hospital and 7 affiliated hospitals between May 2015 and March 2016. The study protocol was approved by the Institutional Review Board at our hospital, and the study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. Written informed consent was obtained from all participants after they were given detailed explanations of the study. The study was registered with the University Hospital Medical Information Network (UMIN) Clinical Trials Registry System http://www.umin.ac.jp/ctr/index.htm (UMIN 00017122).
Eligible patients were those who required total colonoscopy, were older than 20 years of age, and gave consent to participate in this study. The exclusion criteria were: (1) confirmed /or suspected gastrointestinal tract obstruction; (2) intestinal perforation; (3) gastric retention; (4) toxic megacolon; (5) active inflammatory bowel disease; (6) prior colectomy; (7) history of allergy to the drug; (8) no bowel movement until the procedure day; and (9) being deemed unfit to participate in the study by a physician.
Clinical characteristics and colonoscopic outcomes were analyzed by reviewing the following data in the medical records: age, sex, body mass index (BMI), mean procedure time, and cleansing level.
Patients were then randomized to receive 1 of the following 3 cleansing regimens (Figure 1) using a random number list.
Figure 1.
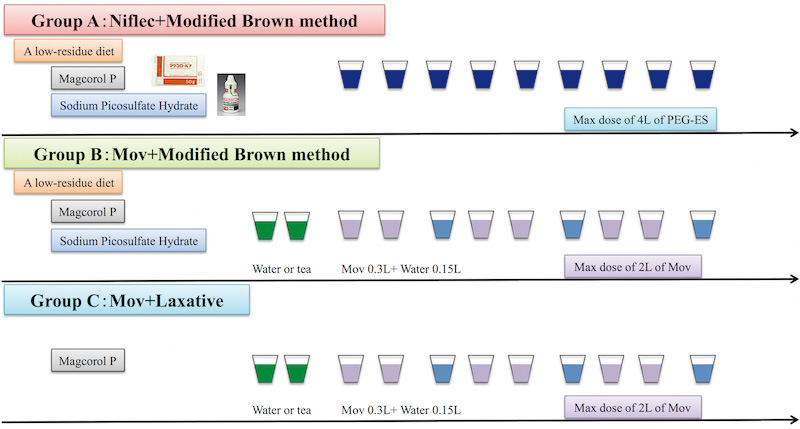
Dose intake schedules for the Nif+Modified Brown Method, Mov+Modified Brown Method, and Mov+Laxative.
1) Group A: Nif+Modified Brown Method
On the day before the procedure, patients consumed a low-residue diet and then drank a solution of isotonic Magcorol PⓇ 50 g and 1 bottle of 0.75% sodium picosulfate solution at 9 p.m. On the day of the procedure, they ingested the Nif at least until their stools became clear. They were then instructed to take the Nif preparation at a rate of no more than 1 L over 1 h. For cases with poor preparation before colonoscopy, additional Nif was used and this was noted in the records so that the maximum intake volume of Nif would be no less than 4 L in total.
2) Group B: Mov+Modified Brown Method
On the day before the procedure, patients consumed a low-residue diet and drank a solution of Magcorol PⓇ 50 g and 1 bottle of 0.75% sodium picosulfate solution at 9 p.m. On the morning of the procedure, they were allowed to drink 2 glasses of water or green tea. Next, they were to repeat a cycle of taking approximately 300 mL of Mov and 150 mL of water or green tea freely, until their stools became clear. Patients were instructed to take the Mov, water, or green tea at a rate of no more than 1 L over 1 h. For cases with poor preparation before colonoscopy, additional Mov was used and this was noted in the records so that the maximum intake volume of Mov would be no less than 2 L in total.
3) Group C: Mov + Laxative
On the day before the procedure, patients drank Magcorol PⓇ 50 g with no diet restriction at 9 p.m. On the morning of the procedure, they were allowed to drink 2 glasses of water or green tea. Then, they were to repeat a cycle of taking approximately 300 mL of Mov and 150 mL of water or green tea freely, until their stools became clear. Patients were instructed to take Mov, water, or green tea at a rate of no more than 1 L over 1 h. For cases of poor preparation before colonoscopy, additional Mov was used and this was noted in the records so that the maximum intake volume of Mov would be no more than 2 L in total.
For cases of poor preparation before colonoscopy, an enema was added in all regimens. The enema consisted of 60-120 mL of lukewarm water and was administered 1-5 times depending on the state of the feces.
The overall quality of colon preparation was determined based on assessments of individual segments (rectum, sigmoid colon, descending colon, transverse colon, ascending colon, and cecum) using the following 5 categories during colonoscopy (Figure 2).
Figure 2.
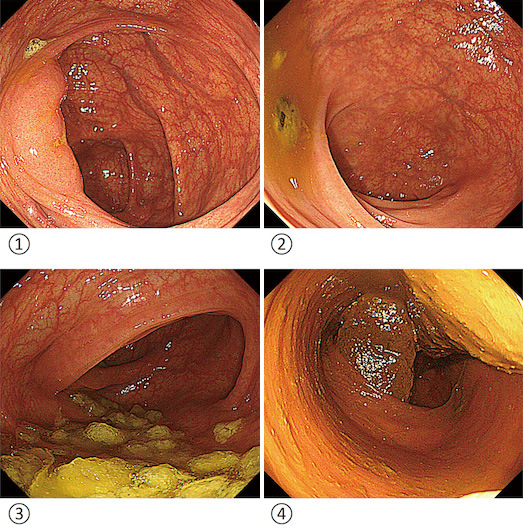
Representative images of bowel preparation for each cleansing score.
1) Entire mucosa of colonic segment clearly visualized with no residual staining, with small fragments of stool and/or opaque liquid.
2) Some semi-solid stool that could be suctioned or washed away and did not obscure visualization.
3) Semi-solid stool that could not be suctioned or washed away and obscured visualization.
4) Examination is impossible because of a considerable amount of solid stool obscuring visualization.
1) Entire mucosa of colon segment seen clearly with no residual staining, but with small fragments of stool and/or opaque liquid.
2) Some semi-solid stool that could be suctioned or washed away and would not obscure visualization.
3) Semi-solid stool that could not be suctioned or washed away and would obscure visualization.
4) Visualization not possible because of a considerable amount of solid stool.
5) Indeterminate (for example, assessment of bowel preparation in the cecum and ascending colon were both 5 when colonoscopy could only reach up to the transverse colon).
The final assessment of bowel preparation was divided into two categories, adequate (1 or 2) and inadequate (3-5). Tolerability, acceptability, preference, and adverse events were investigated by using questionnaires.
Patients graded discomfort subjectively on a scale of 1 to 10, with 1 being the most discomfort. The total score was categorized into two groups: 1-5 and 6-10; the range 6-10 was defined as acceptable and 1-5 as unacceptable.
Outcome measures
The primary outcome was intake dose (total intake volume, Nif/Mov intake volume, and water intake volume). Secondary outcomes were total time for colonic preparation, quality of cleansing, tolerability, and adverse events.
Sample size and statistical analysis
In setting the target number of subjects, the significance level and power were set at 1.67% and 90%, respectively, taking multiplicity into consideration because the study involved three groups. Based on the results (Mov; 1,521 ± 140 mL, Nif; 1,772 ± 354 mL) of a previous study conducted at an affiliated hospital but not published as a paper, we estimated the standard deviation of the difference between the two groups to be 381 mL. The clinically meaningful difference between the two groups was then estimated to be 200 mL. We calculated a sample size of 100 patients for each arm in order to demonstrate the equivalence between the regimens assuming a normal distribution. Therefore, we assumed a drop-out rate of 20% and aimed to enroll a total of 360 patients.
Categorical variables were compared using Fisher's exact test or the χ2 test, and continuous variables were compared using Student's t-test. A p value <0.05 was considered statistically significant. All statistical analysis was performed using JMP software version 9.02 (SAS Institute, Cary, NC).
Results
The study disposition is shown in Figure 3. A total of 360 patients were randomized to Group A (n=117), Group B (n=121), or Group C (n=122). After randomization, some patients withdrew their consent: 12 in Group A, 3 in Group B, and 7 in Group C. Therefore, a total of 338 patients were included in the final analysis (105 in Group A, 118 in Group B group, and 115 in Group C). Demographics and clinical characteristics of the patients are shown in Table 1. No significant differences were observed in age, sex, BMI, previous colonoscopy, previous abdominal or pelvic surgery, constipation, and medications for constipation.
Figure 3.
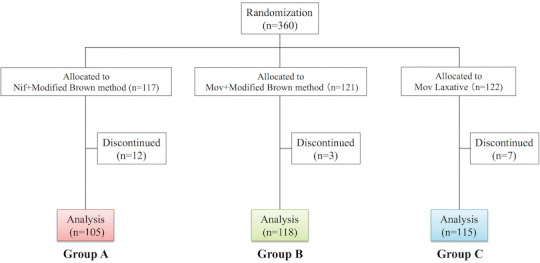
Flowchart for patient selection.
Table 1.
Demographic and Clinical Characteristics of Patients.
| Variables | Group A (n=105) | Group B (n=118) | Group C (n=115) |
|---|---|---|---|
| Age (years old) | |||
| Mean ± SD | 64.4 ± 13.4 | 62.2 ± 13.8 | 63.1 ± 13.2 |
| Sex | |||
| Male | 58 (55) | 58 (49) | 65 (57) |
| Female | 47 (45) | 60 (51) | 50 (43) |
| BMI (kg/m2) | 23 ± 2.7 | 23 ± 3.6 | 23 ± 4.0 |
| Previous colonoscopy | |||
| Yes | 67 (64) | 82 (69) | 76 (66) |
| Previous abdominal or pelvic surgery | |||
| Yes | 35 (33) | 37 (31) | 27 (23) |
| Constipation | |||
| Yes | 20 (19) | 28 (24) | 18 (16) |
| Medications for constipation | |||
| Yes | 14 (13) | 16 (14) | 10 (9) |
| No | 6 (6) | 12 (10) | 8 (7) |
(%)
The results of bowel preparation are shown in Table 2. Total intake volume until irrigation was completed was 1,630 mL in Group A, 1,685 mL in Group B, and 1,819 mL in Group C; there were no significant differences among the groups. Mov intake volume until irrigation was completed was 1,069 mL in Group B and 1,126 mL in Group C. Time for completion of dosing for bowel preparation was significantly shorter in Group B (112.4±44.8 min, n=118) than in Group A (131.3±59 min, n=105) and Group C (122.6±48.1 min, n=115). The distribution of overall cleaning quality determined as adequate (bowel cleansing scale score 1 or 2) or inadequate (score 3-5) for each group is shown in Table 3. Bowel preparation was adequate for 91%, 97%, and 96% of patients in Group A, Group B, and Group C, respectively, and did not significantly differ among the three groups.
Table 2.
Results of Preparation.
| Variables | Group A (n=105) | Group B (n=118) | Group C (n=115) |
P value A vs B |
P value B vs C |
P value A vs C |
|---|---|---|---|---|---|---|
| Total intake volume (ml) | ||||||
| Mean ± SD | 1,630 ± 371 | 1,685 ± 502 | 1,819 ± 584 | 0.88 | 0.87 | 0.74 |
| Nif/Mov intake volume (ml) | ||||||
| Mean ± SD | 1,630 ± 371 | 1,069 ± 314 | 1,126 ± 327 | 0.28 | 0.72 | 0.38 |
| Water intake volume (ml) | ||||||
| Mean ± SD | - | 617 ± 254 | 693 ± 356 | - | 0.59 | - |
| Time for bowel preparation (min) | ||||||
| Mean ± SD | 131.3 ± 59.0 | 112.4 ± 44.8 | 122.6 ± 48.1 | 0.02 | 0.03 | 0.15 |
(%)
Table 3.
Adequate Rate of Bowel Preparation.
| Variables | Group A (n=105) | Group B (n=118) | Group C (n=115) |
|---|---|---|---|
| Total | 91% (95/104) | 97% (115/118) | 96% (110/115) |
| Cecume | 94% (98/104) | 98% (116/118) | 97% (111/115) |
| Ascending colon | 91% (95/104) | 97% (115/118) | 96% (110/115) |
| Transverse colon | 97% (101/104) | 99% (117/118) | 99% (114/115) |
| Descending colon | 94% (98/104) | 99% (117/118) | 98% (113/115) |
| Sigmoid colon | 96% (101/105) | 98% (116/118) | 100% (115/115) |
| Rextum | 96% (101/105) | 100% (118/118) | 100% (115/115) |
The quality of colon preparation was investigated using a questionnaire, and this led to there being some missing values.
Regarding tolerability and acceptability, Group B showed significantly better responses regarding taste, but willingness to repeat the same preparation method was not different among the 3 groups (Table 4). The incidence of symptoms associated with bowel preparation, including sleep disturbance, nausea, abdominal pain, and distension in the 3 groups is shown in Table 5. Analysis of specific symptoms revealed that instances of sleep disturbance (37%) were significantly higher in Group B than Group A, and distension (11%) was significantly lower in Group C than in Group A and Group B (p<0.05, respectively). No severe adverse events occurred in any of the groups.
Table 4.
Patients’ Tolerance and Acceptance.
| Variables | Group A (n=105) | Group B (n=118) | Group C (n=115) |
P value A vs B |
P value B vs C |
P value A vs C |
|---|---|---|---|---|---|---|
| Taste | ||||||
| Acceptable | 22% (23/105) | 37% (44/118) | 33% (37/113) | 0.03 | 0.85 | 0.07 |
| Unacceptable | 78% (82/105) | 63% (74/118) | 67% (76/113) | |||
| Volume | ||||||
| Acceptable | 42% (44/104) | 44% (52/118) | 40% (46/114) | 0.84 | 0.79 | 0.75 |
| Unacceptable | 58% (60/104) | 56% (66/118) | 60% (68/114) | |||
| Willingness to repeat same regimen | ||||||
| Yes | 87% (90/104) | 84% (98/116) | 85% (98/115) | 0.85 | 0.84 | 0.98 |
| No | 13% (14/104) | 16% (18/116) | 13% (15/115) |
Tolerability, acceptability, and preference were investigated using a questionnaire, and this led to there being some missing values.
Table 5.
Adverse Events.
| Variables | Group A (n=105) | Group B (n=118) | Group C (n=115) |
P value A vs B |
P value B vs C |
P value A vs C |
|---|---|---|---|---|---|---|
| Sleep disturbance | 22% (20/92) | 37% (40/109) | 33% (35/106) | 0.03 | 0.87 | 0.08 |
| Nausea | 17% (16/96) | 12% (14/114) | 10% (11/106) | 0.88 | 0.49 | 0.12 |
| Abdominal pain | 16% (16/97) | 15% (15/99) | 11% (12/109) | 0.98 | 0.13 | 0.12 |
| Distension | 21% (19/92) | 24% (21/89) | 11% (11/101) | 0.78 | 0.02 | 0.03 |
Adverse events were investigated using a questionnaire, and this led to there being some missing values.
Discussion
In this study, three bowel cleansing regimens were explored: Nif+Modified Brown Method, Mov+Modified Brown Method, and Mov+Laxative. The rate of successful bowel preparation with each of these 3 regimens was more than 91%. Furthermore, a good cleansing effect was confirmed in all segments from the cecum to the rectum. We used Mov and water or green tea as 1 cycle or taking Mov alone for the following reasons: 1) to reduce the total intake volume of Mov until irrigation was completed; 2) to prevent dehydration resulting from high osmotic diarrhea due to ascorbic acid; and 3) to accurately measure the total intake volume of Mov. Also, we anticipated further benefits as the taste was refreshed by drinking water or green tea intermittently, and we expected that this would improve acceptability.
In this study, we demonstrated that the time to first defecation and time to completion of bowel preparation were significantly shorter with the Mov+Modified Brown Method than in the Nif+Modified Brown Method and Mov+Laxative. These shorter times may lead to improved patient acceptability. Furthermore, these results will also provide some benefit in saving time for medical staff. The Mov regimen with one-split dosing is recommended in Japan. That is, 2 L of Mov can be taken as 2 L on the day of the procedure (same-day dosing). The time necessary for completion of dosing with hypertonic Mov was significantly longer than that with isotonic Nif. This regimen combining a low-residue diet and laxative together in Mov with split dosing on the day before total colonoscopy overcame the inconvenience of the long time required with the conventional Mov regimen.
Xie et al. reported a meta-analysis of randomized controlled trials of low-volume Mov versus standard-volume Nif as bowel preparation modalities for colonoscopy[8]. The report identified 11 randomized controlled trials for analysis. The authors demonstrated that low-volume Mov achieved noninferior efficacy for bowel cleansing, was more acceptable to patients, and produced fewer side effects than standard-volume Nif.
There are several reports that have shown a decrease in Mov. For example, Yoshida et al. analyzed a total of 5,427 patients (mean age: 64.5 ±13.8) in terms of the cleaning level, using the rate of the Boston bowel preparation score (BBPS)[9]. Patients were required to consume a low residue diet and 10 mL of sodium picosulfate in the evening of the day before the colonoscopy. Then, patients consumed 1 L Mov and 0.5 L water 4 h before the examination, which must be completed 2 h before the procedure. The rate of BBPS ≥ 6 in the elderly (65-79 years old; 2,761 patients), special-elderly (≥80 years old; 565 patients), and non-elderly (18-64 years old, 2,101 patients) was 94.1%, 91.8%, and 94.6%, respectively. They concluded that a same-day 1-L Mov method was efficient for bowel preparation because the rates of good preparation (BBPS ≥ 6) were high. Furthermore, the safety of the same-day 1-L Mov method was confirmed when it was examined in the special-elderly (≥80 years old) cases in this report[9].
Maeda et al. analyzed a total of 344 patients who received 1-L or 2-L Mov regimens in terms of the cleaning level, using the rate of BBPS. They compared the 1-L Mov plus 24 mg senna and conventional 2-L Mov regimens in terms of colonoscopic bowel preparation (BP) quality and patient tolerability. The 1-L Mov group showed noninferior adequate BP rates compared with the 2-L Mov group (88% vs. 89%, P = 1.00); overall BBPS was 7.1±1.5 and 7.2±1.5, respectively (P = 0.39). Higher willingness to repeat the BP was observed in the 1-L Mov group (85% vs. 62%, P < 0.01). They concluded that the 1-L Mov regimen was comparable to the 2-L Mov regimen in terms of BP adequacy, required lower BP solution volumes, and had better patient tolerance[10].
In our study, we were able to reduce the intake volume medication of Mov to about 1 L with the concomitant use of a low-residue diet and laxative.
Yamano et al. recommended the four-split Mov regimen because of its shorter cleansing time without causing severe nausea[11]. Mov with four-split dosing had a significantly shorter preparation time (3.00±0.53 h) compared with Mov with one-split dosing[11]. In our study, the time for bowel preparation in the Mov+Modified Brown Method (112.4±44.8 min) was significantly shorter than in the Nif+Modified Brown Method (131.3±59 min). It was possible to shorten the time further with our regimen.
A low-residue diet showed efficacy in decreasing the required volume of Nif[12]. Also, 43% of patients in the 4-L Nif group showed good or excellent bowel preparation compared with 23% in the low-volume 2-L Nif plus sennoside group (p=0.03)[13]. However, the low-volume Nif plus sennoside was significantly better tolerated than standard Nif (p<0.001). Furthermore, we reported that the required intake volume of Nif could be reduced to around 1 L with the concomitant use of a low-residue diet and laxatives (article in Japanese)[5]. Based on these reports, taking a low-residue diet and laxatives on the evening before Nif or Mov is administered is a more effective method of bowel preparation.
Regarding patient tolerability and acceptability, the Mov+Modified Brown Method yielded better results; the reduced volume of Mov administered may have positively influenced the patients' responses, despite their being instructed to consume an additional liter of PEG-free liquid. However, contrary to our expectations, patient-reported acceptability below 50% for taste and volume, although willingness to repeat the same preparation method did not differ among the three groups.
Patients receiving the Mov+Modified Brown Method preparation showed similar results in the adverse events categories, including sleep disturbance and distension compared with the Nif+Modified Brown Method that offered no overt advantages. This finding could possibly be attributed to the fact that adherence was considered to be poor because patients had to eat a low-residue diet and take two different kinds of laxative preparations on the day before colonoscopy. In contrast, the Mov+Laxative group had significantly less distension than the other groups, and had bowel preparation that was equivalent to Nif+Modified Brown method. Even the regimen that had reduced laxative volume on the day before colonoscopy may have had both high cleansing effect and acceptability.
Poor bowel preparation was positively associated with some polyps going undetected. Adenomas and high-risk lesions were frequently detected on repeat colonoscopy in patients with inadequate bowel preparation, suggesting that these lesions were likely missed[14]. Recently, narrow band imaging (NBI) and blue laser imaging (BLI) were found to be efficient in improving polyp detection and polyp visibility[15,16]. However, views of NBI and BLI endoscopy are reddish with poor bowel preparation, and this reduces the merits of these modalities. Adequate bowel preparation with good tolerability is expected to increase polyp detection.
In Japan, colorectal cancer has become the leading cause of cancer mortality in women and the third-leading cause in men; however, the rate of colorectal cancer screening and colonoscopy has not exceeded 70%. Furthermore, in Hiroshima Prefecture, these rates remain stubbornly below 70%[17]. There is still inadequate public awareness of the importance of colonoscopy as a tool for the early detection of colorectal cancer, despite widespread acceptability of upper gastrointestinal endoscopy. One of the most important factors impeding widespread use of colonoscopy is that bowel preparation has been consistently cited as the main reason for poor acceptability to patients because the regimen is burdensome[18]. It is thus necessary to consistently examine regimens for bowel cleansing prior to colonoscopy to ensure both high cleansing effect and acceptability.
There are several limitations to consider in interpreting the results of this study. First, cleansing level was not evaluated using the standard BBPS[9] and the Ottawa Bowel Preparation Scale[20]. Five categories are customarily used during colonoscopy for evaluating bowel cleansing at Hiroshima University Hospital, and thus we followed that practice in this study. Second, the possibility that the preceding preparation may have affected the grading of the acceptability of the study regimen cannot be ruled out. Also, patients who have previously undergone a colonoscopy and are familiar with the procedure may have introduced bias. Enrolling patients who were undergoing colonoscopy for the first time would have been more ideal. Third, we did not describe the changes in physiological parameters in detail, such as weight, vital signs, serum electrolytes, blood chemistry, and complete blood count. Fourth, tolerability, acceptability, preference, and adverse events were investigated using a questionnaire, and this led to there being some missing values. Fifth, in this study we did not assess comorbidities in detail, but rather estimated whether or not patients had a previous colonoscopy, prior colectomy, and past history of constipation. Furthermore, the definition of constipation was ambiguous because this study was conducted before the clinical guidelines for chronic constipation were published in 2017. Therefore, evaluation of constipation may differ among facilities, and thus the degree to which oral medication was administered for constipation could not be evaluated. Taken together, this is the source of the bias. Sixth, we did not collect polyp and adenoma detection rates, which are one of the main outcomes of colonoscopy. In consideration of these factors, the findings of this study regarding differences between the study formulations are inconclusive.
Conclusions
The Mov+Modified Brown method provided significantly shorter bowel preparation time, although there were no significant differences in total intake volume among the 3 regimens. The Mov+Laxative group had significantly less distension than the other groups and achieved bowel preparation that was equivalent to that with the Nif+Modified Brown method.
Conflicts of Interest
There are no conflicts of interest.
Source of Funding
This study was funded by EA Pharma Co., Ltd., under contract, but the funding source was not involved in the planning, implementation, analysis, or publication of the results.
Author Contributions
NA, SN and SO conceived and designed the study, performed the statistical analysis, interpreted the data, and drafted the manuscript. NA, SO, SN, TM, TA, TK, TK, YH, KN, MK, MO, and ST acquired the data. All authors critically revised the article for important intellectual content and approved the article for publication.
Disclaimer
Shinji Tanaka is one of the Associate Editors of Journal of the Anus, Rectum and Colon and on the Journal's Editorial Board. He was not involved in the editorial evaluation or decision to accept this article for publication at all.
References
- 1.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993 Dec; 329(27): 1977-81. [DOI] [PubMed] [Google Scholar]
- 2.Lieberman DA, Rex DX, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the us multi-society task force on colorectal cancer. Gastroenterology. 2012 Sep; 143(3): 844-57. [DOI] [PubMed] [Google Scholar]
- 3.Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012 Feb; 366(8): 687-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Belsey J, Epstein O, and Heresbach D. Systematic review: adverse event reports for oral sodium phosphate and polyethylene glycol. Aliment Pharmacol Ther. 2009 Jan; 29(1): 15-28. [DOI] [PubMed] [Google Scholar]
- 5.Oka S, Tanaka S, Yoshida S, et al. Ingenuity and usefulness of the preliminary tablet-based regimens for bowel cleansing prior to colonoscopy-Prospective comparative test regarding patient acceptability and cleansing effect. J Gastrointestinal Cancer Screen. 2012 Jan; 50(1): 20-29. Japanese. [Google Scholar]
- 6.Wilson JX. Regulation of vitamin C transport. Annu Rev Nutr. 2005 Feb; 25: 105-25. [DOI] [PubMed] [Google Scholar]
- 7.Fujita I, Akagi Y, Hirano J, et al. Distinct mechanisms of transport of ascorbic acid and dehydroascorbic acid in intestinal epithelial cells (IEC-6). Res Commun Mol Pathol Pharmacol. 2000 Mar; 107: 219-31. [PubMed] [Google Scholar]
- 8.Xie Q, Chen L, Zhao F, et al. Ameta-analysis of randomized controlled trials of low-volume polyethylene glycol plus ascorbic acid versus standard-volume polyethylene glycol solution as bowel preparations for colonoscopy. PLoS ONE. 2014 Jun; 9(6): Article ID e99092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai EJ, Calderwood AH, Doros D, et al: The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009 Mar; 69(3 Pt 2): 620-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoshida N, Naito Y, Murakami T, et al. Safety and Efficacy of a Same-Day Low-Volume 1 L PEG Bowel Preparation in Colonoscopy for the Elderly People and People with Renal Dysfunction. Dig Dis Sci 2016 Aug; 61(11): 3229-35. [DOI] [PubMed] [Google Scholar]
- 11.Maeda N, Higashimori A, Nakatani M, et al. Efficacy and tolerability of 1 L polyethylene glycol plus ascorbic acid with senna versus 2 L polyethylene glycol plus ascorbic acid for colonoscopic bowel preparation: Prospective, randomized, investigator-blinded trial. Dig Endosc. 2022 Dec. doi: 10.1111/den.14504. [DOI] [PubMed] [Google Scholar]
- 12.Yamano HO, Matsushita HO, Yoshikawa K, et al. Randomised clinical study comparing the effectiveness and physiological effects of hypertonic and isotonic polyethylene glycol solutions for bowel cleansing. BMJ Open Gastroenterol. 2016 Jul; 3(1): e000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seo EH, Kim TO, Park MJ, et al. Low-volume morning-only polyethylene glycol with specially designed test meals versus standard-volume split-dose polyethylene glycol with standard diet for colonoscopy: a prospective, randomized trial. Digestion. 2013 Aug; 88(2): 110-8. [DOI] [PubMed] [Google Scholar]
- 14.Hookey LC, Depew WT, Vanner SJ. Combined low volume polyethylene glycol solution plus stimulant laxatives versus standard volume polyethylene glycol solution: a prospective, randomized study of colon cleansing before colonoscopy. Can J Gastroenterol. 2006 Feb; 20(2): 101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chokshi RV, Hovis CE, Hollander T, et al. Prevalence of missed adenomas in patients with inadequate bowel preparation on screening colonoscopy. Gastrointest Endosc. 2012 Jun; 75(6): 1197-203. [DOI] [PubMed] [Google Scholar]
- 16.Horimatsu T, Sano Y, Tanaka S, et al. Next-generation narrow band imaging system for colonic polyp detection: a prospective multicenter randomized trial. Int J Colorectal Dis. 2015 Jul; 30(7): 947-54. [DOI] [PubMed] [Google Scholar]
- 17.Yoshida N, Hisabe T, Hirose R, et al. Improvement in the visibility of colorectal polyps by using blue laser imaging (with video). Gatrointest Endosc. 2015 Sep; 82(3): 542-9. [DOI] [PubMed] [Google Scholar]
- 18.Yuge R, Fujii T, Shinagawa K, et al. A Questionnaire Survey on the Sequence of Events Prior to Undergoing Colonoscopy: The Influence of the Behabioral Response after a Facal Occult Blood Test on the Early Detectional of Colorectal Cancer. Intern Med. 2019 Jun; 58(11): 1541-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parente F, Marino B, Crosta C. Bowel preparation before colonoscopy in the era of mass screening for colo-rectal cancer: a practical approach. Dig Liver Dis. 2009 Feb; 41(2): 87-95. [DOI] [PubMed] [Google Scholar]
- 20.Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc. 2004 Apr; 59(4): 482-6. [DOI] [PubMed] [Google Scholar]


