Abstract
Objectives
This review study aimed to evaluate the impact of therapeutic exercises on Upper-Crossed Syndrome (UCS). The study utilized a systematic review and meta-analysis approach to investigate the effects of various therapeutic exercises on forward head posture, rounded shoulders, and hyperkyphosis associated with upper crossed syndrome.
Methods
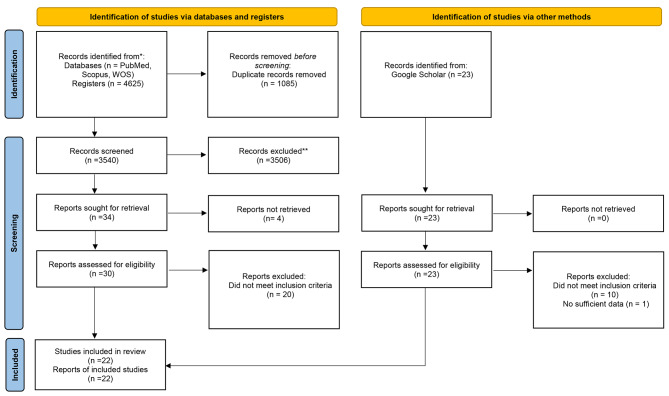
The study identified relevant keywords for each independent and dependent variable and conducted a search in scientific databases, including PubMed, Web of Science, Scopus, and Google Scholar, without any time limitations until 12 August 2023. Overall, 4625 articles were found in the selected databases, which were reduced to 1085 after being entered into the EndNote software and removing duplicate data. The full texts of 30 remaining studies were reviewed; ten articles meeting the criteria were included. Additionally, 12 studies from the Google Scholar database were included, resulting in 22 studies. Using Comprehensive meta-analysis software (CMA ver 3), data heterogeneity was measured with I2 and the Q tests. The Funnel Plot and Egger test methods were utilized to determine the possibility of publication bias. The JBI checklist was used to assess the quality of the studies.
Results
The results of the meta-analysis showed that therapeutic exercises were effective in improving forward head, rounded shoulders, and thoracic kyphosis angles (CI 95% = -1.85–1.161, P = 0.001, P = 0.001, CI95%=-1.822–1.15, and P = 0.001, CI 95%= -1.83–1.09, respectively).
Conclusion
Based on the results, it appears that performing therapeutic exercises in the form of strength exercises, stretching, shoulder-based exercises, and incredibly comprehensive exercises that target all muscles may be effective in reducing forward head, rounded shoulders, thoracic kyphosis, and overall UCS.
Level of evidence
1
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-024-07224-4.
Keywords: Upper crossed syndrome, Forward head, Forward shoulder, Round shoulder, Kyphosis
Introduction
Upper Crossed Syndrome (UCS) is characterized by upper quarter abnormalities, such as increased thoracic kyphosis, rounded shoulders, and forward head posture [1, 2]. The prevalence of UCS ranges from 11 to 60% in different populations and age groups [3]. This disorder affects the upper quarter of the body and has multiple causes [2, 4]. Musculoskeletal abnormalities may develop over extended periods due to biomechanical, psychological, and social stresses and repetitive activities [5, 6]. Repetitive movements can cause muscle length, strength, and stiffness changes, which may lead to movement disorders [7]. Some adverse effects of UCS include early fatigue, pain in the back, neck, and shoulder segments, decreased respiratory capacity and increased residual volume, reduced aerobic endurance, an unattractive appearance, and vertebral fractures [8]. This highlights the importance of preventing and correcting this postural abnormality [7].
In addition, it has been observed that UCS can lead to a chain reaction of disorders in more distant segments, such as the lower limbs [1, 2]. For instance, an increase in lumbar hyper-lordosis resulting from changes in the thoracic hyper-kyphosis and cervical hyper-lordosis is one of the indicators of this chain reaction phenomenon, which affects the back muscles and anterior thigh muscles [9]. Therefore, selecting appropriate exercises to correct UCS and prevent further disorders is crucial. In this regard, several studies have explored the effectiveness of various therapeutic exercises for this condition, including therapeutic exercises in games, strength training, stretching exercises, shoulder-specific exercises, and comprehensive exercises [10–13].
UCS is characterized by tightness in specific neck muscles and weakness in others [14]. Therapists emphasize the importance of assessing the head, shoulders, and spine position because misalignment in these areas can affect several biomechanical variables, motor control, and performance [15]. Exercise is assumed to correct existing muscular disorders [16]. However, despite postural correction interventions being widely included in exercise interventions [16–19], there is limited or conflicting empirical data to prove the effectiveness of exercise. Additionally, little information about which exercise is the most effective intervention [1, 20]. In this line, two systematic and meta-analytical reviews have shown that therapeutic exercise can improve inappropriate postural control in individuals with other postural misalignments [19, 21]. Therefore, exercise practitioners require evidence-based recommendations for effective exercises for individuals with postural deviations. Moreover, it is essential to be aware of practical and effective intervention strategies with detailed descriptions to improve inappropriate postural control or prevent its consequences.
The UCS is one of the prevalent postural malalignments in society, which various physical disorders and symptoms may accompany. Therefore, therapeutic exercise has been suggested to improve posture in UCS individuals. Despite several studies investigating the efficacy of therapeutic exercises for UCS, discrepancies persist among their findings. Consequently, prescribing therapeutic exercise programs to enhance the posture of people with UCS requires more robust scientific evidence. Thus, a systematic review and meta-analysis are necessary to provide a comprehensive summary and make definitive conclusions. Consequently, this systematic review aimed to compile and assess the effectiveness of various therapeutic exercises on forward head posture, rounded shoulder, and hyperkyphosis among people with upper crossed syndrome.
Methods
Search strategy
The study at hand follows the Cochrane guidelines and PRISMA checklist, and it is a systematic review and meta-analysis. A search strategy was employed to identify eligible articles, searching for English and Persian articles using specific keywords. The keywords were grouped with AND between each group, and OR was used between the keywords within each group. The search terms used for the search were: (“Upper crossed syndrome” OR “Upper-crossed syndrome” OR “Forward head” OR “rounded shoulder” OR hyperkyphosis OR “thoracic kyphosis”) AND (Exercise OR Training OR Protocol OR Rehabilitation OR “physical therapy” OR “therapeutic exercise” OR “exercise therapy” OR “Exercise Movement Techniques” OR physiotherapy). The searches were performed in the SCOPUS, PUBMED, and Web of Science databases. Moreover, the eligible paper citations and Google Scholar were searched as additional sources to find the relevant sources. To conduct a search in the Google Scholar database, only the terms “Upper Crossed Syndrome,” “Exercise,” and “Training” were queried using the AND operator, and the identified sources were subjected to examination. The articles considered for this study were original, full-text articles published in peer-reviewed journals, and they must meet the following criteria: written in either Persian or English, with no restrictions on publication date, focused on the efficacy of a common exercise program for individuals with UCS, investigated at least one of the dependent variables of interest in the present study, and had an intervention program duration of at least three weeks. There was no time limitation for the search strategy and the searches were done on 6 July 2023.
Search process
Initially, a search was conducted in selected databases, and the information, including author names, titles, and abstracts, was entered into an EndNote file. After removing duplicate records, two researchers independently reviewed the studies while retaining the original author names, titles, and abstracts. Any discrepancies were resolved by the group supervisor, who acted as the final reviewer. The full-text articles that met the inclusion criteria for this study, including the name of the first author, publication year, quality, sample size, participants’ characteristics (age, gender, relevant indices, etc.), intervention and exercise specifications (type, intensity, duration, etc.), methods and tools for data collection, and the most important results obtained, were summarized in Table 1.
Table 1.
Characteristics of included studies, NA; not available
| Author and Year | Participants | Number of participants (Male/Female) (Age ± Standard Deviation) | Interventions | Comparison | Duration of Exercise (weeks), (day/week), (Time/session (min)) | Variable / Condition | Result |
|---|---|---|---|---|---|---|---|
| Salamat et al., 2020 [22] | Students |
Corrective Functional Exercises: 12 (12/0) (11.5 ± 1.16) Corrective Plays: 12 (12/0) (11.33 ± 1.07) Control Group: 12 (12/0) (11.66 ± 1.07) |
Group 1: Functional Corrective Exercises Group 2: Corrective Plays | No Exercise | (8), (3), (NA) | Forward Head, Forward Shoulder, Kyphosis | Significant differences were observed in forward head, forward shoulder, and kyphosis in the intervention groups. Corrective plays had a higher positive effect on the forward head and kyphosis. |
| Maarouf et al., 2020 [13] | Basketball Players in Wheelchairs | Intervention group: 12 (12/0) (5.08 ± 39.80) Control Group: 12 (12/0) (11.23 ± 43) | Scapular Stability exercises | No Exercise | (8), (5), (60) | Forward Head, Forward Shoulder, Kyphosis | Significant improvement in forward head, forward shoulder, and kyphosis angles in the intervention group |
| Karimian et al., 2019 [23] | Teachers |
Group: 12 (45.2 ± 8.1) Control Group: 11 (44.1 ± 7.8) |
Corrective Exercises with Ergonomic Interventions | No Exercise | (12), (3), (45–60) | Forward Head, Forward Shoulder, Kyphosis | In exercise groups, significant differences were observed in the forward head, forward shoulder, and kyphosis angles. |
| Piri et al., 2021 [18] | Beautician women |
Experimental Group: 20 (0/20) (33.40 ± 2.30) Control Group: 20 (0/20) (31.95 ± 1.47) |
Myofascial Release, Stretching Exercises, and Dynamic Exercises | No Exercise | (12), (3), (60) | Forward Head, Forward Shoulder, Kyphosis | Significantly reduced forward head, forward shoulder, and kyphosis angles in the intervention group |
| Abdolahzade et al., 2019 [10] | Female Students |
Intervention Group: 15 (0/15) (20.53 ± 1.55) Control Group: 15 (0/15) (20.00 ± 2.00) |
Corrective Exercises based on NASM | No Exercise | (8), (3), (30–70) | Forward Head, Forward Shoulder, Kyphosis | Significant improvement was found in the NASM group’s forward head, forward shoulder, and kyphosis angles. |
| Hajizadeh et al., 2021 [11] | Martial Artists |
Intervention group: 15 (15/0) (24.20 ± 4.12) Control Group: 15 (15/0) (24.66 ± 3.56) |
General corrective Exercises | No Exercise | (10), (3), (30–70) | Forward Head, Forward Shoulder, Kyphosis | Significant changes in forward head, forward shoulder, and kyphosis angles in the experimental group |
| Cheshomi et al., 2017 [24] | Female volleyball and handball players |
Intervention group: 18 (18/0) (29.18 ± 4.92) Control Group: 18 (18/0) (27.11 ± 5.74) |
Strengthening and stretching exercises | No Exercise | (6), (3), (NA) | Forward Head, Forward Shoulder, Kyphosis | Significant changes in forward head, forward shoulder, and kyphosis angles in the experimental group |
| Hosseini and et al., 2016 [25] | Male Students |
General corrective exercise group: 15 (15/0) (23.07 ± 2.03) Vibration group: 15 (15/0) (23.05 ± 2.03) Control Group: 15 (15/0) (24.40 ± 2.10) |
Group 1: General corrective exercises Group 2: corrective exercises combined with vibration |
No Exercise | (6), (3), (30–60) | Forward Head, Forward Shoulder, Kyphosis | Significant reduction in forward head, forward shoulder, and kyphosis angles was observed in both intervention groups—the vibration group showed greater improvement . |
| Haji Hosseini et al., 2014 [12] | Female Students |
Strengthening exercise group: 10 (10/0) (21.50 ± 1.08) Stretching exercise group: 10 (10/0) (22.10 ± 1.80) Combined exercise group: 10 (10/0) (22.08 ± 1.97) Control Group: 10 (10/0) (22.90 ± 2.07) |
Group 1: Strength Exercises Group 2: Stretching Exercises Group 3: Combined Exercises |
No Exercise | (6), (3), (30–70) | Forward Head, Forward Shoulder, Kyphosis | Significant reduction in forward head, forward shoulder, and kyphosis angles was observed in all exercise groups, with the combination group showing the most significant reduction. |
| Miri et al., 2022 [26] | Female Students |
Corrective exercise group: 8 (8/0) (16.75 ± 0.07) Postural education group: 8 (8/0) (15.50 ± 0.75) Combined group: 8 (8/0) (16.75 ± 1.03) Control Group: 8 (8/0) (16.00 ± 1.19) |
Group 1: corrective exercises Group 2: postural training Group 3: corrective exercises and postural training |
No Exercise | (8), (3), (60) | Forward Head, Forward Shoulder, Kyphosis | Significant differences were observed in forward head, forward shoulder, and kyphosis angles in all intervention groups. |
| Javazi et al., 2019 [27] | Female Students |
Intervention group: 12 (12/0) (22.00 ± 1.53) Control Group: 12 (12/0) (21.58 ± 1.88) |
Corrective exercises with physioball | No Exercise | (6), (3), (60) | Forward Head, Forward Shoulder, Kyphosis | Significant differences were observed in the intervention group’s forward head, forward shoulder, and kyphosis angles. |
| Ahmadi et al, 2022 [28] | Female Students | Intervention Group: 12 (0/12)( 22.4 ± 1.3) Control Group: 12 (0/12)( 22.2 ± 0.33) | Aquatic Corrective Exercises | No Exercise | 8), (3), (50–70) | Forward Head, Forward Shoulder, Kyphosis | Significantly reduced forward head, forward shoulder, and kyphosis angles in the aquatic exercise group |
| Sarvari et al., 2022 [29] | Students | Intervention group: 20 (0/20)( 14.54 ± 1.82 ) Control group: 20 (0/20)( 14.43 ± 1.16) | Online Corrective Exercises | No Exercise | (8), (3), (30–45) | Forward Head, Kyphosis | Significant improvements in forward head and kyphosis angles in intervention group |
| Seidi et al., 2020 [17] | Students | Intervention group: 12 (12/0)( 25.3 ± 2.5 ) Control group: 12 (12/0)( 25.4 ± 1.5) | Comprehensive Corrective Exercises | No Exercise | (8), (3), (NA) | Forward Head, Forward Shoulder, Kyphosis | No exercise, comprehensive corrective exercises |
| Yaghoubitajani et al., 2022 [30] | office workers | Workplace group: 12 ( 37.00 ± 8.12) Online-supervised group: 12 ( 38.58 ± 7.34) Control group: 12 ( 38.91 ± 3.87) |
Group 1: corrective exercises at the workplace Group 2: Online-supervised : corrective exercises |
No Exercise | (8), (3), (50–60) | Forward Head, Forward Shoulder, Kyphosis | both intervention groups improved from baseline to follow-up for Forward Head, Forward Shoulder, and Kyphosis. |
| Guo et al., 2023 [31] | College students | Intervention group: 20 (11/9)( 19.00 ± 0.97) Control group: 20(7/13)( 18.85 ± 0.88) |
cervical and thoracic “Daoyin” training. |
No Exercise | (8), (5), (NA) | Forward Head, Forward Shoulder |
obvious improvement in the forward head angle, forward shoulder angle, |
| Park et al., 2014 [32] | children | Intervention group: 20 (10/10)( 13.55 ± 2.21) Control group: 20(10/10)( 13.75 ± 1.80 | Strengthening and stretching exercise | No Exercise | (25), (3), (NA) | Forward Head, Forward Shoulder | The complex training improved posture |
| Firouzjah et al., 2023 [33] | volleyball players | Intervention group: 15 ( 16/46 ± 0/63) Control group: 15 ( 16/80 ± 0/77) | Strengthening and stretching exercise | No Exercise | (10), (3), (30–70) | Forward Head, Forward Shoulder, Kyphosis |
significant good effect on forward head, forward shoulder, and kyphosis. |
| Ruivo et al., 2016 [34] | adolescents | Intervention group: 42(16/26) (15.5 ± 1.0) Control group: 46(15/31) (15.9 ± 1.1) | Strengthening and stretching exercise in addition to Physical Education classes | Physical Education classes | (32), (2), (NA) | Forward Head, Forward Shoulder | The exercise intervention successfully decreased the forward head and protracted shoulder in adolescents. |
| Lynch et al.,2010 [5] | National Collegiate Athletic | Intervention group: 14 (19.29 ± 1.44) Control group: 14 (19.29 ± 1.20) | Strengthening and stretching exercise | No Exercise | (8), (3), (NA) | Forward Head, Forward Shoulder | The exercise intervention was successful at decreasing forward head and rounded shoulder |
| Nitayarak et al., 2021 [35] | women | Intervention group: 19(0/20) (20.26 ± 1.20) Control group: 20(0/20) (20.15 ± 1.27) | d scapular stabilization exercises using elastic bands | No Exercise | (4), (3), (NA) | Forward Head, Forward Shoulder, Kyphosis | significant improvement in the cervical and shoulder angle |
| Shalamzari et al., 2022 [36] | formal nurses | Intervention group: 31(31/0) (34.77 ± 9.19) Control group: 31(31/0) (37.12 ± 8.76) | Strengthening and stretching exercise | No Exercise | (8), (3), (30–70) | Forward Head, Kyphosis | Significant improvements in forward head and kyphosis angles in the intervention group |
Quality assessment
We utilized the JBI checklist to assess the quality of the studies. As this checklist provides separate criteria for different study types, we employed the quasi-experimental and clinical trial checklists for the studies included in this article. The assessment results are presented in a detailed Table 2.
Table 2.
Score of Quality Assessment
| study | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Semi Experimental Studies | ||||||||||||||
| Hajihosseini et al., 2015 [12] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Cheshomi et al., 2018 [24] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Karimian et al., 2019 [23] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Abdolahzade et al., 2019 [10] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Hajihoseini et al., 2017 [25] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Javazi et al., 2019 [27] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Maarouf et al., 2020 [13] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Salamat et al., 2020 [22] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Hajizadeh et al., 2021 [11] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Ahmadi et al., 2022 [37] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Sarvari et al., 2022 [29] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | -- | -- | -- | -- | -- | 8 |
| Miri et al., 2022 [26] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Park et al.,2014 [32] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | 7 | |
| Firouzjah et al., 2023 [33] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Shalamzari et al., 2022 [36] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | -- | -- | -- | -- | -- | 7 |
| Randomized Controlled Trials | ||||||||||||||
| Seidi et al., 2020 [17] | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 9 |
| Piri et al., 2021 [18] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 10 |
| Nitayarak et al., 2021 [35] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 10 |
| Lynch et al.,2010 [5] | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 8 |
| Ruivo et al., 2016 [34] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 |
| Guo et al., 2023 [31] | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 10 |
| Yaghoubitajani et al., 2022 [30] | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 9 |
Statistical analyses
In the current study, we employed the Comprehensive Meta-Analyses (CMA ver3) statistical software for data analysis. We gathered data from the articles selected for the study, including pre-and post-test means, standard deviation, P-values, sample sizes, and mean differences (if obtainable). Data heterogeneity was assessed using the I2 and Q test. Funnel Plot and Egger test were utilized to evaluate publication bias. In instances where significant publication bias was detected, we utilized the trim-and-fill method to gauge the possible effect on the final meta-analysis results and to determine the extent of studies missed in this domain.
Results
There were a total of 4625 articles identified in the selected databases. Once the data was entered into EndNote software and duplicate records were removed, 3540 articles remained. After reviewing the abstracts and titles, 34 articles were selected for further analysis, and the remaining articles were excluded. Following this, the complete text of the 30 chosen articles was carefully analyzed; ultimately, ten papers were deemed suitable for the study. Additionally, 12 studies from the Google Scholar database were included, resulting in 22 studies. Each of the three abnormalities associated with UCS (forward head posture, rounded shoulders, and hyper-kyphosis) were analyzed separately to aid in data analysis. The effect of therapeutic exercise has been the subject of research about UCS. In this study, in the 22 eligible studies, a total of 903 participants were involved, and this data is presented in Fig. 1.
Fig. 1.
Search and selection of studies for systematic review according to PRISMA guidelines
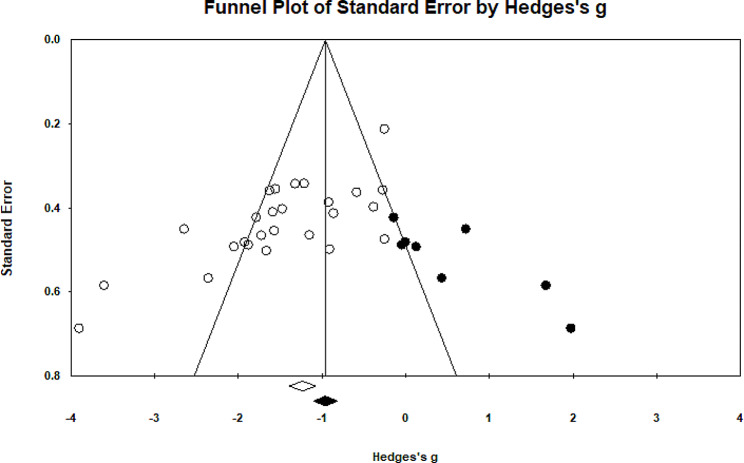
Forward head posture
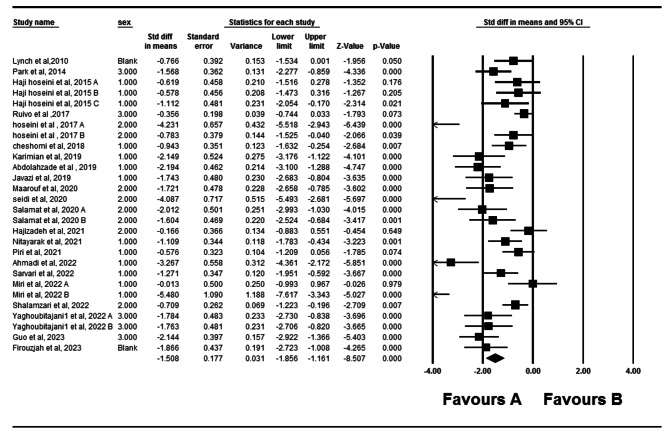
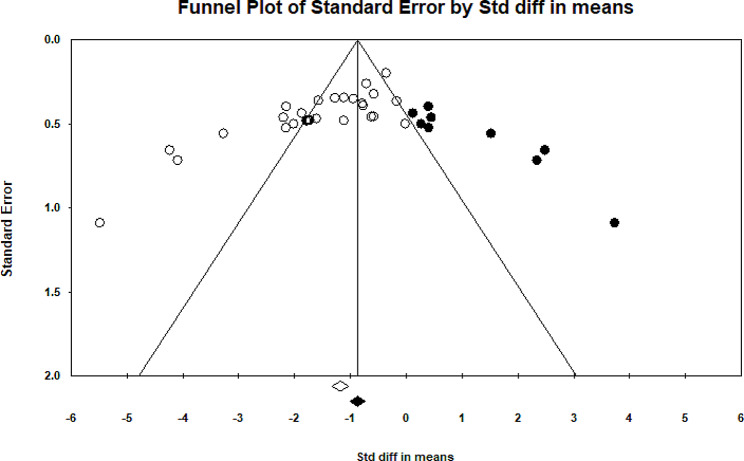
Twenty- two eligible studies have investigated the impact of therapeutic exercise on forward head posture [5, 10–13, 17, 18, 22–36]. Of these studies, three studies had two independent intervention groups that were analyzed. In total, 903 participants took part in these studies. Forest plot analysis of the data showed a significant improvement in forward head posture with therapeutic exercise (CI 95% = -1.85–1.161, P = 0.001) (Fig. 2). The I2 and Q tests were used to assess heterogeneity, which showed significant heterogeneity (P = 0.001) (I2 = 80.39) among data. Funnel plot and Egger’s tests suggested the possibility of publication bias (P = 0.001) (Fig. 3). Furthermore, the results of the Trim and Filled also indicated that adding nine random articles cannot change the overall results of this study. Because of the heterogeneity, meta-regression was used to examine the possible effect of age on the eligible studies’ results. Age and weight did not significantly impact the studies’ results (P < 0.05).
Fig. 2.
Forest plot of the effect of therapeutic exercise on Forward head posture
Fig. 3.
Funnel plot of studies worked on forward head posture
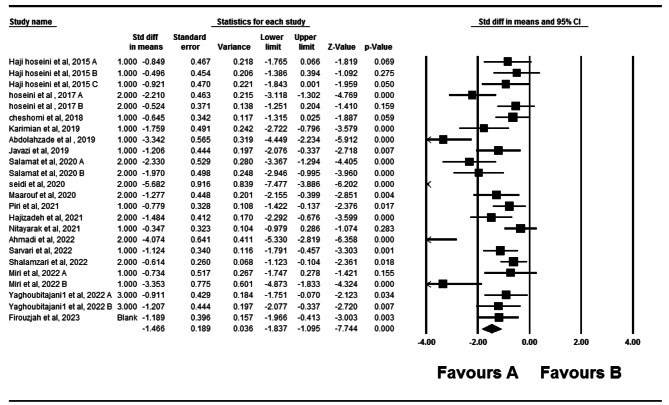
Rounded shoulders
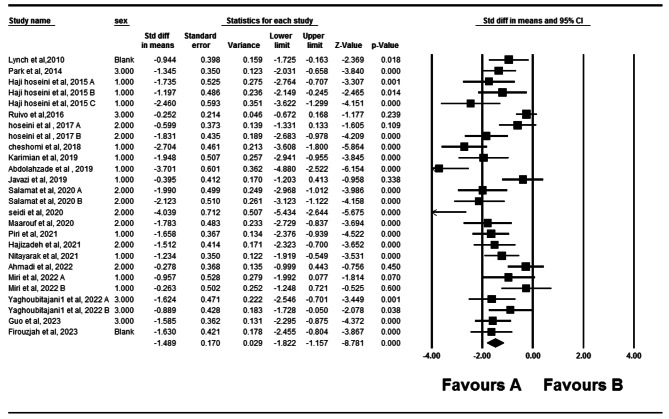
Twenty studies have examined the impact of therapeutic exercise on rounded shoulders [5, 10–13, 17, 18, 22–28, 30–35]. Two of these studies had two independent intervention groups, while one study had three independent intervention groups. A total of 774 participants were involved in these studies. Forest plot analysis of the data showed a significant improvement in rounded shoulders with therapeutic exercise (P = 0.001, CI 95%=-1.822–1.157) (Fig. 4). After assessing heterogeneity, significant heterogeneity was observed (P = 0.001) (I2 = 75.38). Funnel plot and Egger’s tests indicated publication bias in the studies (P = 0.001) (Fig. 5). Furthermore, the results of the Trim and Filled also showed that adding eight random articles cannot change the overall results of this study. Meta-regression was used to examine the possible effect of age on the eligible studies’ results. Age and weight did not significantly impact the studies’ results (P < 0.05).
Fig. 4.
Forest plot of the effect of therapeutic exercise on Rounded shoulders
Fig. 5.
Funnel plot of studies worked on Rounded shoulders
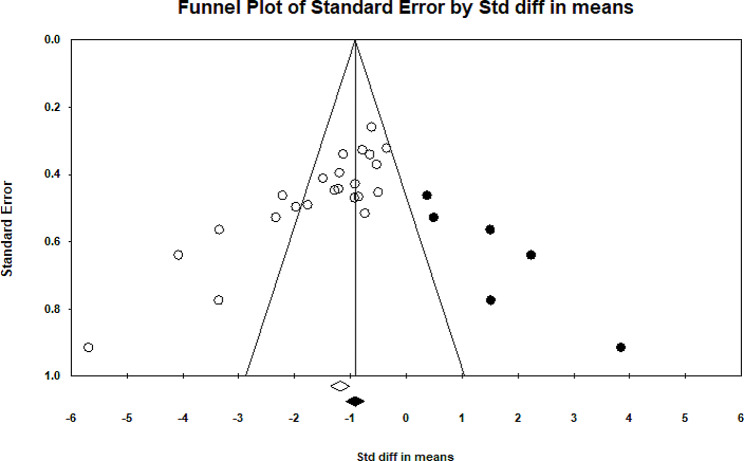
Thoracic kyphosis
Eighteen studies have examined the effect of therapeutic exercise on thoracic kyphosis [10–13, 17, 18, 22–30, 33, 35, 36]. In three studies, both independent intervention groups were utilized, while in one study, all three independent intervention groups were included. A total of 673 participants were involved in these studies. Data analysis using CMA and Forest plot analysis demonstrated a significant improvement in thoracic kyphosis with therapeutic exercise (P = 0.001, CI 95%= -1.83–1.09) (Fig. 6). After assessing heterogeneity, significant heterogeneity was observed (P = 0.001) (I2 = 77.86). Funnel plot and Egger’s tests indicated publication bias in the studies (P = 0.001) (Fig. 7). Furthermore, the results of the Trim and Filled also showed that adding six random articles cannot change the overall results of this study. Meta-regression was used to examine the possible effect of age and weight on the eligible studies’ results. It is demonstrated that age and weight did not significantly impact the studies’ results (P < 0.05).
Fig. 6.
Forest plot of the effect of therapeutic exercise on Thoracic Kyphosis
Fig. 7.
Funnel plot of studies worked on Thoracic kyphosis
Discussion
The results of this study indicate that prescribing therapeutic exercises can be an effective intervention in modifying the angles of the forward head, rounded shoulder, and thoracic kyphosis. The meta-analysis results showed a significant difference in the change in the forward head angle between the groups participating in therapeutic exercise programs and the control groups.
The result of this study is consistent with other research indicating the effectiveness of therapeutic exercises in improving forward head posture in individuals with UCS. For instance, previous studies have demonstrated that therapeutic exercises using vibration devices [25], NASM-based corrective exercises [10, 23], strength, stretching, and a combination of both exercises, as well as comprehensive corrective exercises [17] all have a significant impact on forward head angle reduction in individuals with UCS. It seems that the better forward head posture may result from decreases in the anterior displacement of the head secondary to better mechanical advantage and biomechanical function of the neck muscles that contribute to cervical flexion [38, 39]. In this line, to address forward head posture, selected therapeutic exercises aimed to stretch the shortened muscles of the neck, such as the sternocleidomastoid, levator scapulae, scalenes, and pectoralis major, and to strengthen the deep neck flexor muscles, such as the longus colli, longus capitis, and anterior scalene. Additionally, exercises aimed to strengthen the thoracic spine and shoulder muscles to reduce the forward head angle [18, 19].
On the other hand, this study’s results indicate that therapeutic exercise significantly improves rounded shoulder posture in individuals with UCS. Previous studies have also demonstrated that various therapeutic programs, including two functional therapeutic programs and therapeutic games [22], NASM-based corrective exercises, selected corrective exercises [24], and strength, stretching, or a combination of both exercises [17], have a significant impact on improving rounded shoulder posture in individuals with UCS.
Ultimately, this study demonstrates that therapeutic exercise can significantly reduce the thoracic kyphosis angle in individuals with UCS. In support of this, various studies have shown that different therapeutic exercises can effectively mitigate the thoracic kyphosis angle in individuals with UCS [17, 18, 22, 24].
To explain why therapeutic exercises are effective in improving postural alignment in people with UCS, several points can be considered [2]. Muscle imbalances resulting from prolonged positioning or repetitive movements in a specific and static position can affect upper body posture. Biomechanical studies have shown that the deep flexor muscles of the neck, upper back extensors, and shoulder adductors become weakened and strained compared to their antagonists [40]. This leads to an imbalance in the upper quarter of the body, resulting in forward head posture, abnormal scapular protraction, increased thoracic kyphosis, and neck flexion, which can eventually lead to painful shoulders and shortening of anterior shoulder muscles, such as the pectoralis major and minor [35, 41]. These abnormalities are interrelated in a kinetic chain, and a significant change in the natural pattern of one of the spinal column curves can lead to compensatory changes in other curves [40]. Therefore, researchers have selected various therapeutic exercises that focus on the body’s chain reaction and simultaneously address the three abnormalities associated with UCS: forward head posture, rounded shoulders, and hyper-kyphosis. This seems to be the primary reason for the positive results found in the studies included in this review [17]. The rhomboid, trapezius, and serratus anterior muscles are the most important stabilizers of the shoulder, primarily controlling shoulder movements in a coordinated fashion [42]. In UCS, these muscles tend to weaken, and inhibition of the rhomboid and serratus anterior muscles can lead to increased shoulder abduction with anteriorly rotated shoulders [43]. According to Kendall [7], this abnormality can result from the shortening of the pectoralis minor muscle and weakness of the middle trapezius muscle. Additionally, in anterior shoulder dysfunction, the humerus bone is influenced by its connection to the glenoid cavity, causing the arm to move forward and rotate internally. This condition can result in weakness and strain of the shoulder’s external rotator muscles and shortening of the internal rotator muscles of the shoulder [7]. Therefore, exercise interventions in the reviewed studies may have helped reduce UCS by creating balance in muscular activity.
Moreover, this analysis revealed significant heterogeneity in the findings of different studies across all three variables of forward head posture, rounded shoulder, and thoracic kyphosis. It is worth noting that these studies were conducted on individuals with various age ranges, jobs, and interventions employed to improve UCS. Therefore, these factors may contribute to the heterogeneity in the results of the studies included in the analysis. In this context, the meta-regression results demonstrated that age and weight did not significantly affect the studies’ results.
When generalizing the findings of this study, it is essential to consider some of its limitations. Firstly, most studies have not focused on investigating the long-term effects of therapeutic exercise on UCS, so it is unclear how long-lasting the effects mentioned in this article would be. Secondly, this study aimed to investigate the effects of therapeutic exercises on the postural alignment of individuals with UCS. It did not examine the impact of therapeutic exercises on performance, psychological, or social characteristics. Thirdly, it should be noted that the UCS is a cluster of symptoms, including postural deviations, specific patterns of muscle tightness and weakness, and scapular dyskinesia. However, it should be considered that most articles have relied solely on postural variables for diagnosing UCS. Therefore, they may lack the necessary accuracy in identifying this condition. Moreover, in this study the quality assessment was not limited to JBI score cut-off value and had no limitations regarding the mean age or the participants’ jobs. This point may have resulted in heterogeneity among the meta-analysis results, and therefore, caution should be exercised in generalizing these findings to other groups. Ultimately, this study only assessed Persian and English-language peer-reviewed journals and did not include other scientific literature like conference proceedings, books, and textbook chapters. It may be worthwhile to consider a broader range of academic sources and include materials in different languages to broaden the scope of future research.
Conclusion
The results revealed that prescribing various therapeutic exercises effectively improves postural alignment in individuals with UCS. Exercise prescription can significantly improve such individuals’ forward head posture, rounded shoulder, and thoracic kyphosis angles. Moreover, it seems that the effectiveness of therapeutic exercise for this condition may be slightly less in children than in adults.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: The datasets generated and analysed during the current study
Supplementary Material 2: Raw data reviewd in this paper from various database
Acknowledgements
Not Applicable.
Author contributions
The original idea, writing the manuscript, protocol development, data analysis, abstracted data, and prepared the manuscript: all authors.
Funding
No funding was obtained for this study.
Data availability
The datasets generated and analyzed during the current study are available in supplementary file 1, and the search results from various databases are presented in supplementary file 2.
Declarations
Ethics approval guidelines, and consent to participate
Not Applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harman K, Hubley-Kozey CL, Butler H. Effectiveness of an exercise program to improve forward head posture in normal adults: a randomized, controlled 10-week trial. J Man Manipulative Therapy. 2005;13(3):163–76. doi: 10.1179/106698105790824888. [DOI] [Google Scholar]
- 2.Chang MC, Choo YJ, Hong K, Boudier-Revéret M, Yang S. Treatment of Upper crossed syndrome: a narrative systematic review. Healthcare. 2023;11(16):2328. doi: 10.3390/healthcare11162328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nadler SF, Malanga GA, Bartoli LA, Feinberg JH, Prybicien M, Deprince M. Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med Sci Sports Exerc. 2002;34(1):9–16. doi: 10.1097/00005768-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Muscolino J. Upper crossed syndrome. J Australian Traditional-Medicine Soc. 2015;21(2):80. [Google Scholar]
- 5.Lynch SS, Thigpen CA, Mihalik JP, Prentice WE, Padua D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br J Sports Med. 2010;44(5):376–81. doi: 10.1136/bjsm.2009.066837. [DOI] [PubMed] [Google Scholar]
- 6.Salsali M, Sheikhhoseini R, Sayyadi P, Hides JA, Dadfar M, Piri H. Association between physical activity and body posture: a systematic review and meta-analysis. BMC Public Health. 2023;23(1):1670. doi: 10.1186/s12889-023-16617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. Muscles: testing and function with posture and pain. Lippincott Williams & Wilkins Baltimore, MD; 2005.
- 8.Fatima A, Ashraf HS, Sohail M, Akram S, Khan M, Azam H. Prevalence of upper cross syndrome and associated postural deviations in computer operators. A qualitative study. Asian J Allied Health Sci (AJAHS). 2022;7(3).
- 9.Katzman WB, Sellmeyer DE, Stewart AL, Wanek L, Hamel KA. Changes in flexed posture, musculoskeletal impairments, and physical performance after group exercise in community-dwelling older women. Arch Phys Med Rehabil. 2007;88(2):192–9. doi: 10.1016/j.apmr.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 10.Abdolahzadeh M, Daneshmandi H. The Effect of an 8-week NASM Corrective Exercise Program on Upper crossed syndrome. J Sport Biomech. 2019;5(3):156–67. [Google Scholar]
- 11.Hajizadeh F, Sedaghati P, Saki F. The Effect of Comprehensive Corrective exercises on posture of Wushu Practitioners with Upper Cross Syndrome. J Sport Biomech. 2021;7(1):30–43. doi: 10.32598/biomechanics.7.1.2. [DOI] [Google Scholar]
- 12.Hhajihosseini E, Norasteh A, Shamsi A, Daneshmandi H. The comparison of effect of three programs of strengthening, stretching and comprehensive on upper crossed syndrome. J Res Rehabilitation Sci. 2015;11(1):51–61. [Google Scholar]
- 13.Maarouf A, Norasteh A, Daneshmandi H, Ebrahimi-Atri A. Effect of a corrective Exercise Program based on Scapular Stability on Upper Cross Syndrome in Wheelchair basketball athletes. Iran J War Public Health. 2020;12(1):19–27. doi: 10.29252/ijwph.12.1.19. [DOI] [Google Scholar]
- 14.Rautenbach M. The effectiveness of spinal manipulative therapy in conjunction with a stretching program in the treatment of upper crossed syndrome. University of Johannesburg (South Africa); 2012.
- 15.Claus AP, Hides JA, Moseley GL, Hodges PW. Thoracic and lumbar posture behaviour in sitting tasks and standing: progressing the biomechanics from observations to measurements. Appl Ergon. 2016;53:161–8. doi: 10.1016/j.apergo.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Bae W-S, Lee H-O, Shin J-W, Lee K-C. The effect of middle and lower trapezius strength exercises and levator scapulae and upper trapezius stretching exercises in upper crossed syndrome. J Phys Therapy Sci. 2016;28(5):1636–9. doi: 10.1589/jpts.28.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seidi F, Bayattork M, Minoonejad H, Andersen LL, Page P. Comprehensive corrective exercise program improves alignment, muscle activation and movement pattern of men with upper crossed syndrome: randomized controlled trial. Sci Rep. 2020;10(1). [DOI] [PMC free article] [PubMed]
- 18.Piri H, Hajian M, Mirkarimpour SH, Sheikhhoseini R, Rahimi M. The Effect of 12-Week corrective exercises on the postural angles of Beautician females with Upper crossed syndrome: a clinical Trial Study. Women’s Health Bulletin. 2021;8(2):91–7. [Google Scholar]
- 19.Sheikhhoseini R, Shahrbanian S, Sayyadi P, O’Sullivan K. Effectiveness of Therapeutic Exercise on Forward Head posture: a systematic review and Meta-analysis. J Manipulative Physiol Ther. 2018;41(6):530–9. doi: 10.1016/j.jmpt.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Bansal S, Katzman WB, Giangregorio LM. Exercise for improving age-related hyperkyphotic posture: a systematic review. Arch Phys Med Rehabil. 2014;95(1):129–40. doi: 10.1016/j.apmr.2013.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.González-Gálvez N, Gea-García GM, Marcos-Pardo PJ. Effects of exercise programs on kyphosis and lordosis angle: a systematic review and meta-analysis. PLoS ONE. 2019;14(4):e0216180. doi: 10.1371/journal.pone.0216180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salamat H, Ghani Zadeh Hesar N, Roshani S, Mohammad Ali Nasasb Firouzjah E. Comparison of the Effect of Functional Corrective exercises and Corrective games on Upper Cross Syndrome in 10–13 year-old boys. Sci J Rehabilitation Med. 2020;9(4):19–31. [Google Scholar]
- 23.Karimian R, Rahnama N, Ghasemi G, Lenjannejadian S. Photogrammetric analysis of upper cross syndrome among teachers and the effects of national academy of sports medicine exercises with ergonomic intervention on the syndrome. J Res Health Sci. 2019;19(3):e00450. [PMC free article] [PubMed] [Google Scholar]
- 24.Cheshomi S, Alizadeh MH, Barati AH, Akochakian M. The effect of six weeks corrective exercise on upper-crossed syndrome of overhead athletes. J Appl Exerc Physiol. 2018;14(27):153–66. [Google Scholar]
- 25.Hosseini SM, Rahnama N, Barati AH. Comparing the effects of ten weeks of regular corrective exercise and corrective exercise with whole body vibration apparatus on upper cross syndrome. Stud Sport Med. 2017;8(20):89–106. [Google Scholar]
- 26.Miri H, Shahrokhi H, Dostdar Rozbahani A, Nasirzare F. Comparison of the effect of comprehensive corrective exercises with and without posture training on upper cruciate syndrome in female students. Med J Mashhad. 2022;61(1):344–65. [Google Scholar]
- 27.Javazi F, Sedaghati P, Daneshmandi H. The effect of selected corrective exercises with physioball on the posture of female computer users with upper crossed syndrome. J Sport Biomech. 2019;5(2):112–23. doi: 10.32598/biomechanics.5.2.5. [DOI] [Google Scholar]
- 28.Ahmadi H, Yalfani A, Gandomi F. Effectiveness of Eight Weeks of Corrective Exercises in Water on Postural Status of Young Men with Upper crossed syndrome: a Randomized Controlled Clinical Trial. Sci J Rehabilitation Med. 2022;11(2):292–305. doi: 10.32598/SJRM.11.2.6. [DOI] [Google Scholar]
- 29.Sarvari S, Saei SM, Rahimzadeh M, Salehian MH. The Effect of an online corrective training intervention on the Upper Cross Syndrome and feelings of fatigue and Pain in adolescents. Int J Pediatrics-Mashhad. 2022;10(4):15813–22. [Google Scholar]
- 30.Yaghoubitajani Z, Gheitasi M, Bayattork M, Andersen LL. Corrective exercises administered online vs at the workplace for pain and function in the office workers with upper crossed syndrome: randomized controlled trial. Int Arch Occup Environ Health. 2022;95(8):1703–18. doi: 10.1007/s00420-022-01859-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo Y, Li M, Xie C, Liu X, Chen Y, Yang J et al. Effect of the cervical and thoracic daoyin training on college students with upper crossed syndrome: a randomized controlled trial. 2023.
- 32.Park HC, Kim YS, Seok SH, Lee SK. The effect of complex training on the children with all of the deformities including forward head, rounded shoulder posture, and lumbar lordosis. J Exerc Rehabil. 2014;10(3):172–5. doi: 10.12965/jer.140113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Firouzjah MH, Firouzjah E, Ebrahimi Z. The effect of a course of selected corrective exercises on posture, scapula-humeral rhythm and performance of adolescent volleyball players with upper cross syndrome. BMC Musculoskelet Disord. 2023;24(1):489. doi: 10.1186/s12891-023-06592-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruivo RM, Carita AI, Pezarat-Correia P. The effects of training and detraining after an 8 month resistance and stretching training program on forward head and protracted shoulder postures in adolescents: Randomised controlled study. Man Ther. 2016;21:76–82. doi: 10.1016/j.math.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 35.Nitayarak H, Charntaraviroj P. Effects of scapular stabilization exercises on posture and muscle imbalances in women with upper crossed syndrome: a randomized controlled trial. J Back Musculoskelet Rehabil. 2021;34(6):1031–40. doi: 10.3233/BMR-200088. [DOI] [PubMed] [Google Scholar]
- 36.Shalamzari MH, Motaqi M, Ghanjal A. The effects of a corrective exercise on pain and quality of life factors and spinal curvature angles of nurses with kyphosis and forward head position in a military medical center. J Military Med. 2022;23(11).
- 37.Ahmadi H, Yalfani A, Gandomi F. Effect of eight weeks of Corrective exercises carried out in Water on Static and Semi dynamic balance on students with Upper crossed syndrome) Janda approach. Sci J Rehabilitation Med. 2020;9(3):286–96. [Google Scholar]
- 38.Cho J, Lee E, Lee S. Upper cervical and upper thoracic spine mobilization versus deep cervical flexors exercise in individuals with forward head posture: a randomized clinical trial investigating their effectiveness. J Back Musculoskelet Rehabil. 2019;32:595–602. doi: 10.3233/BMR-181228. [DOI] [PubMed] [Google Scholar]
- 39.Mylonas K, Angelopoulos P, Billis E, Tsepis E, Fousekis K. Combining targeted instrument-assisted soft tissue mobilization applications and neuromuscular exercises can correct forward head posture and improve the functionality of patients with mechanical neck pain: a randomized control study. BMC Musculoskelet Disord. 2021;22(1):212. doi: 10.1186/s12891-021-04080-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Page P, Frank CC, Lardner R. Assessment and treatment of muscle imbalance. (No Title). 2010.
- 41.Ranđelović I, Jorgić B, Antić V, Hadžović M. Effects of exercise programs on upper crossed syndrome: a systematic review. Fizičko Vaspitanje i Sport kroz Vekove. 2020;7(2):152–68. doi: 10.2478/spes-2020-0012. [DOI] [Google Scholar]
- 42.Comel JC, Nery RM, Garcia EL, da Silva Bueno C, de Oliveira Silveira E, Zarantonello MM, et al. A comparative study on the recruitment of shoulder stabilizing muscles and types of exercises. J Exerc Rehabilitation. 2018;14(2):219. doi: 10.12965/jer.1835198.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weon JH, Oh JS, Cynn HS, Kim YW, Kwon OY, Yi CH. Influence of forward head posture on scapular upward rotators during isometric shoulder flexion. J Bodyw Mov Ther. 2010;14(4):367–74. doi: 10.1016/j.jbmt.2009.06.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: The datasets generated and analysed during the current study
Supplementary Material 2: Raw data reviewd in this paper from various database
Data Availability Statement
The datasets generated and analyzed during the current study are available in supplementary file 1, and the search results from various databases are presented in supplementary file 2.