Abstract
Objectives:
Pediatric gastroenterology patients are at risk for co-occurring behavioral health concerns, like depression and anxiety, compared with youth without medical conditions. The objective of this systematic review was to assess the scientific literature supporting the hypothesis that integrating behavioral health services into gastroenterology clinics could improve patient psychosocial well-being.
Methods:
We searched MEDLINE, EMBASE, The Cochrane Library, Web of Science, PsycINFO, and CINAHL databases and grey literature to identify studies reporting the impact of behavioral health integration on the psychosocial well-being of pediatric gastroenterology patients. Two independent coders evaluated each study for inclusion and extracted data regarding patient demographics, study design, behavioral health integration approaches, and psychosocial outcomes. Results were synthesized using narrative review procedures.
Results:
Eighteen studies met the inclusion criteria. Most reported outcomes from research grant-funded randomized controlled trials or open trials investigating behavioral health interventions based on Cognitive-Behavioral Therapy, primarily with youth with irritable bowel disease or functional gastrointestinal disorders. Within the highest-quality, comparable studies, nearly 80% reported at least one statistically significant treatment effect on patient psychosocial well-being. Many studies used rigorous methods that minimize bias, but did not provide models for sustainable, programmatic behavioral health integration outside the bounds of a research study.
Conclusions:
The studies included in this review suggest that behavioral integration could have the potential to positively impact gastroenterology patients’ psychosocial functioning. However, more research is needed to investigate the appropriate intensity of behavioral health services and evaluate models for integrating behavioral healthcare in pediatric gastroenterology settings beyond the research-funded clinical trial context.
Keywords: Gastroenterology, pediatric, behavioral health, mental health, integration, psychosocial, quality of life
Introduction
Gastrointestinal (GI) disorders are conditions affecting the digestive system and any of its organs. Examples of GI disorders typically treated by gastroenterology subspecialists include inflammatory bowel disease (IBD), functional GI disorders, chronic liver disease, and celiac disease (1). The nervous system and psychosocial functioning can contribute to the development, maintenance, and recovery from chronic GI disorders (2,3) In fact, behavioral health interventions are considered effective treatments for several GI disorders (4–6) In addition, behavioral health services can be beneficial for pediatric populations living with chronic GI disorders, because these youth are at increased risk for developing mental health disorders compared to their peers without medical illness (7–9). Unfortunately, access to therapists who specialize in delivering behavioral health interventions for GI conditions is limited (10).
Integrating behavioral health services into subspecialty GI clinics may reduce access challenges (11–13). The World Health Organization defines integration as systems of healthcare that ensure all people have access to health services that are provided in ways “that are coordinated around their needs, respect their preferences, and are safe, effective, timely, affordable, and of acceptable quality” (14). Integrating behavioral health care into GI settings could promote quality of life (QOL), a multidimensional construct that describes an individual’s “perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (15). QOL encapsulates many diverse constructs related to psychosocial wellbeing, such as life satisfaction, psychological or physical health, and engagement in social and occupational activities. This is an important outcome to consider because pediatric populations living with GI disorders report poorer QOL than peers without medical illness even when their condition is controlled (16,17).
Despite a growing recognition that GI treatment should follow a biopsychosocial model, implementing integrated mental health programs in pediatric GI clinics is still novel, with the literature primarily focused on publishing exemplars (18,19). Samsel (2017) described a range of integrated behavioral health care models that have been delivered within pediatric subspecialty settings, with emerging evidence that this care model could decrease healthcare expenditures and increase family and provider satisfaction (20). For example, pediatric GI medical providers with access to integrated mental health providers report high levels of satisfaction and support expanding the resource. Providers report that integrated mental health services offer benefits to patients (e.g., improved identification and treatment of behavioral health components of physical health problems, increased patient compliance with medical recommendations, positive health behavior change) and providers (e.g., increasing efficiency during visits, assisting with medical decision-making) (21). However, integrated care models face barriers, such as inadequate reimbursement for services and logistical challenges, that keep behavioral health services siloed away from medical clinics (22). To our knowledge, no systematic review has been completed with a focus on behavioral health integration into pediatric GI care. The objective of this review is to evaluate how integrating behavioral health services into gastroenterological pediatric subspecialty care impacts youth psychosocial outcomes. See PICO-formatted research question in Table 1.
Table 1.
Research Question
| Criterion | Definition |
|---|---|
|
Population: Pediatric patients receiving subspeciality gastroenterology care |
The definition of pediatric patients includes infants, children, adolescents, and young adults (0–21 years old). Common conditions treated in subspeciality gastroenterology include liver diseases, inflammatory bowel disease, and functional disorders of the GI tract. |
|
Intervention: Behavioral health integration into pediatric gastroenterology subspecialty care settings |
Integration will be defined similarly to Chuah et al. (24): “Managerial or operational changes to health systems to bring together inputs, delivery, management and organization of particular [behavioral health service functions] as a means of improving coverage, access, quality, acceptability and (cost)-effectiveness.” Both outpatient and inpatient care settings will be included. |
|
Comparison: No behavioral health integration |
This included any contrast between patients receiving behavioral health integration and patients not receiving this (e.g., standard care, treatment as usual, unidisciplinary care). |
|
Outcome: Primary outcome: QOL and related constructs Secondary outcomes: Satisfaction with care and access to care |
Primary outcome: This was defined as patient- or proxy-reported quality of life, other measures of wellbeing or life satisfaction, psychological and physical symptoms, and indicators of engagement in meaningful life activities for pediatric populations. Secondary outcomes: This was defined as patient- or proxy-reported satisfaction with treatment received in the study and access to behavioral health care services. |
Methods
Eligibility Criteria
The protocol was registered at PROSPERO (CRD42021227576) before starting the review. Studies, either interventional or observational, investigating behavioral health integration in subspecialty gastroenterology settings were included. We included studies enrolling a primarily pediatric population, from birth through young adulthood. We excluded studies without quantitative outcomes or written in a language other than English, Spanish, or French.
Information Source
We searched 6 databases (MEDLINE, EMBASE, The Cochrane Library, Web of Science, PsycINFO, CINAHL). We also searched ClinicalTrials.gov, WHO International Clinical Trial Registry Platforms, and websites maintained by American Gastroenterological Association (https://gastro.org/), North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (https://naspghan.org/), Pediatric IBD Foundation (https://pedsibd.org/), the Society of Pediatric Liver Transplantation (https://tts.org/split-home), American Psychiatric Association (https://www.psychiatry.org), American Psychological Association (https://www.apa.org), and American Academy of Child and Adolescent Psychiatry (https://www.aacap.org) websites to identify grey literature. In addition, we reviewed conference abstracts from 2015 to 2020, by searching the PapersFirst and ProceedingsFirst databases using WorldCat. We searched for dissertations and theses in ProQuest Dissertations & Theses Global.
Search Strategy
Our search strategy included MeSH headings, Emtree, keywords, and exploded terms representing four concepts: 1) behavioral health, 2) integration, 3) GI disorders, and 4) pediatric patients. The universe of quantitative outcomes related to psychosocial well-being is large (e.g., QOL, child functioning, reduction in mental health symptoms), so rather than use search terms we identified articles reporting any of these outcomes through our full-text review process.
The timeline captured by the literature search spanned from the inception of databases to February 28, 2021. Find an example of the search strategy in the Supplemental Digital Content.
Data Management and Screening Process
We imported all title and abstract records retrieved by electronic searches into Covidence (Veritas Health Innovation, Melbourne, Australia), which automatically removes duplicates. Each title and abstract was reviewed by CS and one of nine independent reviewers. Title and abstract records were coded as ‘Maybe’, ‘No’ or ‘Yes’ based on the eligibility criteria. If either reviewer indicated uncertainty about whether the study meets inclusion or exclusion criteria, the record was included in the full-text screening phase. Full-text copies of the title and abstract records was obtained for those screened as ‘Maybe’ or ‘Yes’. Each full text article was reviewed by CS and a research assistant, who independently screened full text articles and coded them as ‘Include’ or ‘Exclude’. Reasons for excluding studies were documented. Any coding disagreements were resolved through consensus.
Data Extraction
We used Covidence Extraction 2.0 to extract data from all records included in the systematic review. CS and a research assistant independently extracted data from each study, resolving disagreements through consensus. We extracted the data related to research design, the setting and context of the research, population characteristics, the approach to behavioral health integration, and all outcomes relevant to psychosocial wellbeing.
In terms of research design, we coded whether the study was a randomized controlled trial, a non-randomized comparison trial, or a single-sample observational study. We extracted data related to sample size, setting, and funding. To characterize the details of populations enrolled in each study, we extracted variables relevant to race, ethnicity, gender, age range, socioeconomic status, and insurance type.
We also extracted information related to the approach to behavioral health integration. First, we used the template for intervention description and replication (TIDieR) checklist to extract details of the behavioral health integration intervention reported in the study (23). Then, we coded whether behavioral health services were integrated at the micro-level, meso-level, or macro-level (24,25). Micro-level integration is person-focused and involves coordinating mental health care for the individual patient through the GI clinic. This may include screening for mental health symptoms during GI visits or referring to an in-house mental health provider if a mental health concern arises during a GI clinic appointment. Meso-level integration focuses on bringing together professionals or organizations to coordinate care. This could occur through establishing processes that allow health care providers (e.g., physicians, nurses) to collaborate with mental health providers (e.g., psychologists, clinical social workers) to develop co-treatment plans. It could also include inter-agency collaborations between a particular GI clinic and mental health program. Macro-level integration is population-focused. It involves partnerships between entire systems of care to coordinate mental health and GI care, such as through changing funding structures, licensing requirements, or professional education to ensure mental health needs are addressed within healthcare systems.
We extracted outcomes closely related to youth psychosocial wellbeing. We included any quantitative measure specifically naming QOL, as well as measures focused on life satisfaction, child functioning, psychological symptoms, and engagement in meaningful life activities. We coded whether measures were completed by patients or proxies (e.g., parents, clinicians). We extracted data regarding the measures of central tendency (e.g., means, medians) and variability (e.g., standard deviation, interquartile range) for intervention and comparison groups, counts and proportions for any dichotomous measures reported, statistical tests run, p-values, and effect sizes for each measure relevant to QOL. If data was not reported in the included studies, we emailed the corresponding authors to request additional details.
Risk of bias
Risk of bias was assessed using the Critical Appraisal Skills Programme (CASP;(26) checklist appropriate for each study design. Checklist items center upon potential areas for bias and allow for yes/no/can’t tell responses. Manuscripts were also rated by two members of the team and given assessments of low, medium, or severe risk for bias. CS and a research assistant independently rated each study and resolved any disagreements by consensus.
Data synthesis
Due to the heterogeneity of behavioral health integration models and outcomes related to psychosocial wellbeing, the primary approach to synthesis was a narrative review (27). We also created tables organizing the extracted data.
Results
Our search yielded 33,111 unique studies. Eighteen studies met inclusion criteria for this systematic review (Figure 2). At the abstract review stage, the percent agreement between each reviewer pair ranged from 80.0–98.7%. At the full-text review stage, CS and a research assistant had 61.9% agreement.
Figure 1.
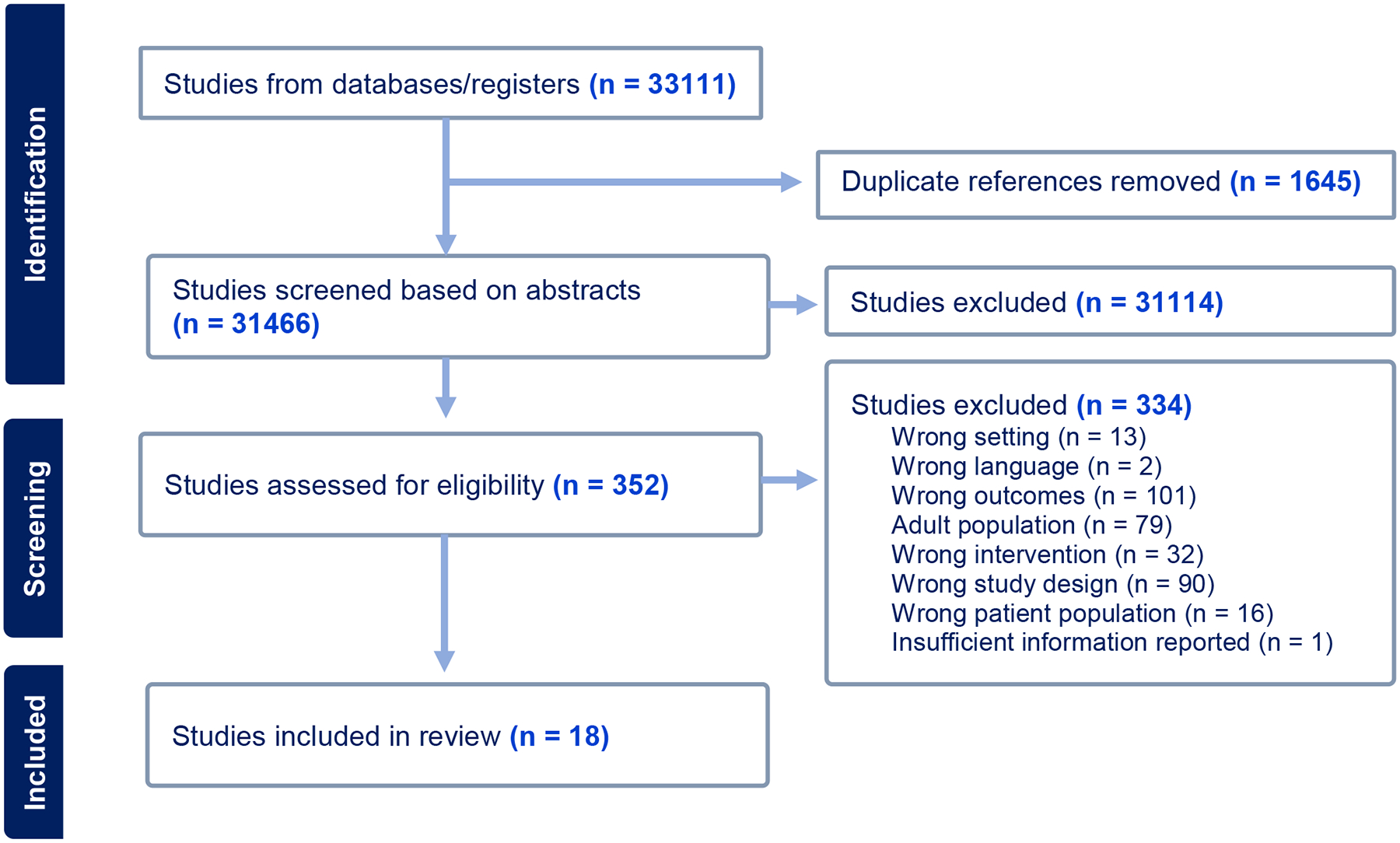
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Flow Chart.
Sample Characteristics
See Supplemental Digital Content 2 for detailed information regarding sample characteristics. Ten studies focused on patients with IBD (28–37), and eight on functional GI disorders (38–45). The weighted average age of all participants was 13.89 years old. The youngest patient across all studies was 6 and the oldest was 29 years old. Across the 17 studies to report race, ethnicity, and gender, 75.7% of all participants were White and 61.6% were girls.
Approaches to Integrating Behavioral Health Services
Sixteen of the studies described micro-level behavioral health integration (28–39,42–45), two of the studies described meso-level (40,41), and none described macro-level. The most common approach to micro-level integration was to recruit participants within a pediatric gastroenterology clinic to participate in a formal research study investigating a behavioral health intervention. Fourteen of those provided treatment based on a cognitive-behavioral therapy (CBT) model (28,30–39,42,43,45), one provided problem-solving skills training (29), and one provided gut-focused hypnotherapy (44). Among the micro-level studies, six reported services were funded by foundations or charitable institutions (28–30,34,35,45), five by federal research grants (32,37,38,42,44), one from a pharmaceutical company (31), one through a pediatric health system research grant (43), and two through a combination of these sources (36,39). We were unable to obtain funding information for one micro-level study (33).
The two meso-level integration examples were interdisciplinary pain clinics, which brought together clinicians from different disciplines to develop integrated treatment plans for patients (40,41). In private correspondence, Dr. Deacy explained that integrated services (41) were funded by insurance based on the patients’ medical diagnoses. We were unable to obtain funding information regarding the other meso-level study (40).
Half of the studies reported on integration strategies that offered services to all patients regardless of the presence of mental health symptoms (29–32,40,41,43–45). The other half offered services only to those patients with co-occurring mental health symptoms (28,33–39,42). Five studies enrolled youth with depression symptoms(28,33,35–37), three with anxiety symptoms (38,39,42), and one with either depression or anxiety symptoms (34). Twelve studies reported including parents/caregivers in the services (29,31,32,34–37,40–43,45). The table in Supplemental Digital Content 2 provides additional details about the behavioral health integration strategies and specific interventions.
Impact of Integrating Behavioral Health Services on Patient Quality of Life
The table in Supplemental Digital Content 2 also organizes the evidence of the impact of integrated care on patient psychosocial well-being, as well as the risk of bias in each study. Eleven studies employed an RCT design (28,29,32–34,36,37,39,43–45), and 7 were observational studies of a single sample (30,31,35,38,40–42). After completing CASP checklists, we appraised two to have severe risk of bias ((35,40), seven to have medium risk (30,31,33,38,41,42,44), and nine to have low risk (28,29,32,34,36,37,39,43,45).
Among the nine RCTs testing integrated behavioral health versus treatment-as-usual, a waitlist, or minimal behavioral health support (e.g., an information sheet) (28,29,32–34,36,39,43,45), seven (77.8%) reported at least one statistically significant positive impact of behavioral health services on psychosocial well-being, such as reductions in psychological symptoms or improvement in QOL ratings (28,29,32,33,36,39,45). The average sample size of these 9 trials was 81.22 (SD = 47.03), ranging from 16 to 185. The three studies failing to show any differences were 1) a study of CBT for (N = 86) youth with functional abdominal pain disorder (FAPD; (43); 2) a study of an intervention based on Social Learning Theory and CBT for (N = 185) youth with IBD (32); and 3) a study of CBT for (N = 70) youth with IBD and depression or anxiety (34). Of the RCTs testing behavioral health against minimal additional treatment beyond typical gastroenterological care, six directly assessed QOL (28,29,32–34,45), seven assessed psychological symptoms (28,32–34,36,39,45), and two assessed child functioning (36,43). The evidence for the impact of behavioral health integration on depression symptoms was the most consistent, with 60.0% of studies finding statistically significant treatment effects. The evidence for impact of behavioral health integration on QOL, anxiety symptoms, and child functioning was weaker, with 33.3%, 25%, and 50% reporting statistically significant treatment effects, respectively. The size of the between-group differences ranged widely, from Cohen’s d = 0.00 to 1.03.
Two RCTs tested one form of behavioral health intervention against another (i.e., CBT versus supportive therapy for youth with IBD (37); gut-focused hypnotherapy delivered by a therapist versus self-guided hypnotherapy with audio-recorded exercises for youth with irritable bowel syndrome (IBS) or FAPD (44)). In both CBT and supportive therapy, youth reported large pre-post changes in depression symptoms but not in anxiety or QOL (37). In both hypnotherapy conditions, participants reported significant improvements in QOL, depression, and anxiety (44).
Among the single-group observational studies, all those reporting results of statistical tests indicated significant pre-post changes (p > 0.05) in target outcomes. Two studies reported statistically significant improvements in anxiety (38,42), one in depression (35), one in QOL (30), and one in child functioning (35). Some studies presented descriptive results, such as the percentage of patients demonstrating clinically meaningful improvements in QOL (41) or child functioning (31) without conducting statistical tests. The two meso-level integration studies retrospectively reported outcomes for patients enrolled in interdisciplinary pain clinics (40,41), without using control groups. Although both studies shared preliminary evidence that integrated behavioral health services could positively impact QOL, we appraised the risk of bias as medium-to-severe.
Discussion
This systematic review evaluated the evidence in support of the hypothesis that integrating behavioral health services into pediatric gastroenterological subspecialty care improves youths’ psychosocial well-being. The bulk of the included studies reported outcomes from research-funded randomized controlled trials or open trials investigating CBT-based behavioral health interventions focused on youth with IBD or functional GI disorders. Behavioral health services were integrated primarily at the micro-level. Individual patients were linked with behavioral health services within pediatric gastroenterology settings, but services were only available within the timeframe and according to the constraints of a formal research study. Many of these studies used rigorous methods that minimize bias but did not provide blueprints for healthcare settings looking to integrate behavioral health services in a sustainable, programmatic way. Only two studies reported results from behavioral health services integrated at the meso-level. These were interdisciplinary pain clinics which brought professionals together to develop individual treatment plans for patients. However, these studies’ methodologies introduced more bias making it difficult to draw conclusions about the impact of these services. Without a control group, more systematic measurement of intervention exposure, and consideration of potential confounders, these studies provide uncertain evidence that behavioral health integration was a causal factor for outcomes.
Within the highest-quality, relatively comparable studies (i.e., randomized trials contrasting integrated behavioral health services versus minimal additional treatment beyond typical gastroenterological care), 77.8% reported at least one statistically significant effect on psychosocial wellbeing. Effect sizes ranged widely, and the pattern of results differed based on the specific outcome, with the most consistent evidence of impact on depression symptoms. The lack of statistically significant results was not limited to trials with smaller samples. It is possible that some of the statistically significant results could be chance findings, particularly because several studies measured multiple patient outcomes.
The lack of consistent evidence of treatment efficacy could be partially explained by many researchers’ choice to use a selective prevention strategy (46), offering behavioral health services to youth based on their status as GI patients rather than in response to demonstrated elevations in psychological symptoms. For example, Cunningham and colleagues (39) recruited patients with elevated anxiety symptoms, and found significant results, whereas Levy and colleagues (32)and van der Veek and colleagues (45)enrolled patients regardless of the presence of symptoms and found no effects on anxiety. Szigethy and colleagues’ (37) subgroup analyses suggested targeting those with more active GI disease could be more effective. More research is needed on personalizing the intensity of behavioral health services for youth based on severity of their GI disease and presenting mental health concerns, and with racially/ethnically diverse samples. In addition, meso-level integration models might be better suited to developing a menu of services that can be flexibly delivered according to specific patient needs. Further, some outcomes like QOL might function independently of behavioral health. That is, a pediatric patient could learn cognitive coping skills, and a parent could learn behavioral strategies, but the youth might still experience an illness flare impacting QOL.
Twelve studies included in this review were conducted in the United States, four in the Netherlands, one in Australia, and one in Greece. This likely reflects the resources available to US researchers rather than a particular commitment to mental health integration in the US versus other countries. When making global comparisons, we must recognize the impact of contextual variables like healthcare system structure and funding, mental health workforce availability, and cultural attitudes toward mental health on integration efforts. Globally, the best practices to integrating mental health care into medical settings include advocacy to shift attitudes and policies, securing financial and human resources, and facilitating collaborations between relevant governmental sectors, organizations, and communities (47).
Given the barriers subspecialty clinics face in implementing integration mental health services, identifying interventions that could be delivered by the existing GI workforce would be helpful to increasing patient access to mental health support. Within the interventions included in this systematic review, self-guided gut-focused hypnotherapy (44), problem-solving worksheets (29), CBT workbooks (35), and CBT web modules (38) could be resources other non-mental health providers might offer to patients. However, the efficacy of these resources might be reduced without the guidance of a mental health provider. More implementation research is needed to clarify how to integrate mental health services in GI settings, with practical and cost-effective strategies. Also of note, this literature review focused on GI clinics or settings with published studies regarding mental health integration. However, there may be numerous more GI clinics with integrated mental health care that do not collect or publish data. This precludes the ability to determine the range of available GI mental health services and their effectiveness. As more mental health professionals integrate into medical settings, collecting outcome data will be crucial to understanding how to optimize the harmonization of medical and mental health.
Strengths and Limitations
This systematic review has many strengths, including the broad search strategy using a large number of databases crossing multiple academic disciplines, the extensive search terms, and the efforts at identifying grey literature. These efforts increase confidence that the relevant research was identified in this undertaking. On the other hand, the number of included studies was relatively small, and those included were quite heterogenous, precluding quantitative assessments of meta-bias such as funnel plots. This limits our ability to estimate the effect size of integrated mental health services and makes the conclusions of this review less definitive. Another limitation is the lack of studies focused on meso- or macro-level integration. By selecting an inclusion criteria of reporting patient-level outcomes, we may have biased this review toward micro-level integration approaches. If we had also included hospital- or system-level outcomes, we might have identified models with deeper integration. The narrative synthesis benefitted from including a rich description of the varying behavioral health integration models, the funding sources and setting, demographic and socioeconomic qualities of the study samples, and the diverse patient-centered outcomes related to QOL. The wide range of outcomes complicates the synthesis of evidence of impact but reflects the varying presenting concerns of pediatric GI patients.
Conclusion
Behavioral health concerns are entwined with chronic GI disorders. Incorporating behavioral health services into subspecialty gastroenterological care settings could target both the psychoneurological and physical components of chronic GI disorders in a more comprehensive manner and offer behavioral health support in a setting with less stigma than psychiatric clinics. The results of this systematic review suggest that most investigators evaluating the impact of behavioral health integration in pediatric gastroenterology settings have focused on micro-level approaches funded by research grants. Most studies do report at least some support for treatment efficacy, underscoring behavioral health interventions in subspecialty GI clinics as a promising approach to increasing access to behavioral health care. However, perhaps due to variations in recruited samples and operationalization of outcomes, the evidence supporting behavioral health integration is mixed, making it challenging to draw definitive conclusions. Further research would benefit from greater harmonization of outcome measurement, to facilitate comparisons across studies and facilitate meta-analyses. With a more developed evidence base, quantitative meta-analyses could help the field form more certain conclusions about the value of integrated behavioral health services. More attention to meso- and macro-level integration, and examples of funding sources for such services outside of time-limited, structured research projects, is needed.
Supplementary Material
What is Known and What is New?
What is known?
The nervous system and psychosocial functioning can impact gastrointestinal disorders, termed “gut-brain axis”.
Youth with gastrointestinal disorders are at increased risk for mental health disorders.
Integrating behavioral health care into pediatric gastroenterology settings can increase family and provider satisfaction and decrease healthcare expenditures.
What is new?
Most studies investigating the impact of behavioral health integration on patients’ well-being focus on models created specifically for research objectives.
Nearly 80% of randomized controlled trials report at least one statistically significant impact on psychosocial well-being.
We need more research evaluating models for sustaining behavioral health integration in regular clinical practice.
Conflicts of Interest and Source of Funding:
None of the authors have conflicts of interest to report. This work was supported by grants UL1TR001855 and UL1TR000130 from the National Center for Advancing Translational Science (NCATS) of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Informed Patient Consent: As this is a systematic review, we did not enroll human subjects in this study.
Registration Number: PROSPERO (CRD42021227576)
References
- 1.Sauer CG, Robson J, Turmelle YP, et al. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition position paper on entrustable professional activities: Development of Pediatric Gastroenterology, Hepatology, and Nutrition entrustable professional activities. J Pediatr Gastroenterol Nutr 2020;71:136–43. [DOI] [PubMed] [Google Scholar]
- 2.MacKner LM, Clough-Paabo E, Pajer K, et al. Psychoneuroimmunologic factors in inflammatory bowel disease. Inflamm Bowel Dis 2011;17:849–57. [DOI] [PubMed] [Google Scholar]
- 3.Cryan JF, O’riordan KJ, Cowan CSM, et al. The microbiota-gut-brain axis. Physiol Rev 2019;99: 1877–2013. [DOI] [PubMed] [Google Scholar]
- 4.Feingold J, Murray HB, Keefer L. Recent advances in cognitive behavioral therapy for digestive disorders and the role of applied positive psychology across the spectrum of GI care. J Clin Gastroenterol 2019;53:477–85. [DOI] [PubMed] [Google Scholar]
- 5.Yeh AM, Wren A, Golianu B. Mind–body interventions for pediatric inflammatory bowel disease. Children 2017; 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Oudenhove L, Törnblom H, Störsrud S, et al. Depression and somatization are associated with increased postprandial symptoms in patients with irritable bowel syndrome. Gastroenterol 2016;150: 866–74. [DOI] [PubMed] [Google Scholar]
- 7.Dipasquale V, Corica D, Gramaglia SMC, et al. Gastrointestinal symptoms in children: Primary care and specialist interface. Int J Clin Pract 2018;72: e13093. [DOI] [PubMed] [Google Scholar]
- 8.Mackner LM, Crandall WV. Long-term psychosocial outcomes reported by children and adolescents with inflammatory bowel disease. Am J Gastroenterol 2005;100:1386–92. [DOI] [PubMed] [Google Scholar]
- 9.Greenley RN, Hommel KA, Nebel J, et al. A meta-analytic review of the psychosocial adjustment of youth with inflammatory bowel disease. J Pediatr Psychol 2010;35:857–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong JJ, Maddux M, Park KT. Mental health service needs in children and adolescents with inflammatory bowel disease and other chronic gastrointestinal disorders. J Pediatr Gastroenterol Nutr 2018;67:314–17. [DOI] [PubMed] [Google Scholar]
- 11.Christian K, Cross RK. Improving outcomes in patients with inflammatory bowel disease through integrated multi-disciplinary care—the future of IBD care. CGH 2018;16: 1708–9. [DOI] [PubMed] [Google Scholar]
- 12.Fairbrass KM, Gracie DJ. Mood and Treatment Persistence in Inflammatory Bowel Disease: Time to Consider Integrated Models of Care? CGH 2021;19:1111–3. [DOI] [PubMed] [Google Scholar]
- 13.Lee CK, Melmed GY. Multidisciplinary team-based approaches to IBD management: How might “one-stop shopping” work for complex IBD care? Am J Gastroenterol 2017;112:45–53. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Framework on integrated, people-centred health services: Report by the Secretariat. World Health Assembly. 2016. [Google Scholar]
- 15.Harper A, Power M, Orley J, et al. Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol Med 1998;28:551–8. [DOI] [PubMed] [Google Scholar]
- 16.Varni JW, Bendo CB, Nurko S, et al. Health-related quality of life in pediatric patients with functional and organic gastrointestinal diseases. J Pediatr 2015;166:85–90. [DOI] [PubMed] [Google Scholar]
- 17.Knowles SR, Keefer L, Wilding H, et al. Quality of life in inflammatory bowel disease: A systematic review and meta-analyses - Part II. Inflamm Bowel Dis 2018;24: 966–976. [DOI] [PubMed] [Google Scholar]
- 18.Winnick JB, Focht DR, Sukumar K, Kuhn BR, Muldowney R, O’Dell SM. Utilization of pediatric psychology services in outpatient pediatric gastroenterology within a rural health system. J Pediatr Gastroenterol Nutr. 2022;75: 52–5. [DOI] [PubMed] [Google Scholar]
- 19.Moser NL, Plante WA, LeLeiko NS, et al. Integrating behavioral health services into pediatric gastroenterology: A model of an integrated health care program. Clin Pract Pediatr Psychol. 2014;2:1–12. [Google Scholar]
- 20.Samsel C, Ribeiro M, Ibeziako P, et al. Integrated behavioral health care in pediatric subspecialty clinics. Child Adolesc Psychiatr Clin N Am 2017;26:785–794. [DOI] [PubMed] [Google Scholar]
- 21.Nicolotti LM, Koehler AN, Quinones EC, et al. Medical provider satisfaction with integrated care in a pediatric gastroenterology clinic. Fam Syst Health. 2022;41:207–13. [DOI] [PubMed] [Google Scholar]
- 22.Wakida EK, Talib ZM, Akena D, et al. Barriers and facilitators to the integration of mental health services into primary health care: A systematic review. Syst Rev 2018;7:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. [DOI] [PubMed] [Google Scholar]
- 24.Chuah FLH, Haldane VE, Cervero-Liceras F, et al. Interventions and approaches to integrating HIV and mental health services: A systematic review. Health Policy Plann 2017;32:iv27–iv47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Valentijn PP, Schepman SM, Opheij W, et al. Understanding integrated care: A comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care 2013;13:e010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.CASP. Critical Appraisal Skills Programme Checklists. Critical Appraisal Skills Programme. 2020. [Google Scholar]
- 27.Popay J, Roberts H, Sowden A, et al. Developing guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC Methods Programme Lancaster: Institute of Health Research. 2005;59. [Google Scholar]
- 28.Ewais T, Begun J, Barclay J, et al. A randomized controlled trial of mindfulness-based cognitive therapy for youth living with inflammatory bowel disease and depression. Aust N Z J Psychiatry 2017;51:110594. [Google Scholar]
- 29.Greenley RN, Gumidyala AP, Eve Nguyen, et al. Can you teach a teen new tricks? Problem solving skills training improves oral medication adherence in pediatric patients with inflammatory bowel disease participating in a randomized trial. Inflamm Bowel Dis 2015;21:2649–57. [DOI] [PubMed] [Google Scholar]
- 30.Grootenhuis MA, Maurice-Stam H, Derkx BH, et al. Evaluation of a psychoeducational intervention for adolescents with inflammatory bowel disease. Eur J Gastroenterol Hepatol 2009;21:430–5. [PubMed] [Google Scholar]
- 31.Hayutin LG, Blount RL, Lewis JD, et al. Skills-based group intervention for adolescent girls with inflammatory bowel disease. Clin Case Stud 2009;8:355–65. [Google Scholar]
- 32.Levy R, Langer SL, Romano J, et al. Results of a large RCT testing the effect of cognitive behavior therapy on school absences, quality of life and flares in pediatric ibd. Gastroenterol 2015;148. [Google Scholar]
- 33.Maragkoudaki M, Chouliaras G, Papadopoulou A, et al. Feasibility and effectiveness of a psycho-educational program in adolescents with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 2016;62. [Google Scholar]
- 34.Stapersma L, van den Brink G, van der Ende J, et al. Psychological outcomes of a cognitive behavioral therapy for youth with inflammatory bowel disease: Results of the HAPPY-IBD randomized controlled trial at 6- and 12-Month follow-p. J Clin Psychol Med Settings 2020;27:490–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Szigethy E, Whitton SW, Levy-Warren A, et al. Cognitive-behavioral therapy for depression in adolescents with inflammatory bowel disease: A pilot study. J Am Acad Child Adolesc Psychiatry 2004;43:1469–77. [DOI] [PubMed] [Google Scholar]
- 36.Szigethy E, Kenney E, Carpenter J, et al. Cognitive-behavioral therapy for adolescents with inflammatory bowel disease and subsyndromal depression. J Am Acad Child Adolesc Psychiatry 2007;46:1290–8. [DOI] [PubMed] [Google Scholar]
- 37.Szigethy E, Bujoreanu SI, Youk AO, et al. Randomized efficacy trial of two psychotherapies for depression in youth with inflammatory bowel disease. J Am Acad Child Adolesc Psychiatry 2014;53:726–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cunningham NR, Nelson S, Jagpal A, et al. Development of the aim to decrease anxiety and pain treatment for pediatric functional abdominal pain disorders. J Pediatr Gastroenterol Nutr 2018;66:16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cunningham NR, Kalomiris A, Peugh J, et al. Cognitive behavior therapy tailored to anxiety symptoms improves pediatric functional abdominal pain outcomes: A randomized clinical trial. J Pediatr 2021;230:62–70.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.D’Amico S, Goh VL, Morera C, et al. Initial experience with co-management of pediatric patients with functional abdominal pain between pediatric gastroenterology and a pediatric pain clinic within an urban safety net hospital. In: North American Society For Pediatric Gastroenterology, Hepatology & Nutrition. J Pediatr Gastroenterol Nutr 2017. [Google Scholar]
- 41.Deacy A, Friesen CA, Staggs VS, et al. Evaluation of clinical outcomes in an interdisciplinary abdominal pain clinic: A retrospective, exploratory review. World J Gastroenterol. 2019;25:3079–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Masia Warner C, Reigada LC, Fisher PH, et al. CBT for anxiety and associated somatic complaints in pediatric medical settings: An open pilot study. J Clin Psychol Med Settings 2009;16:169–77. [DOI] [PubMed] [Google Scholar]
- 43.Robins PM, Smith SM, Glutting JJ, et al. A randomized controlled trial of a cognitive-behavioral family intervention for pediatric recurrent abdominal pain. J Pediatr Psychol 2005;30:397–408. [DOI] [PubMed] [Google Scholar]
- 44.Rutten JMTM, Vlieger AM, Frankenhuis C, et al. Home-based hypnotherapy self-exercises vs individual hypnotherapy with a therapist for treatment of pediatric irritable bowel syndrome, functional abdominal pain, or functional abdominal pain syndrome a randomized clinical trial. JAMA Pediatr 2017;171:470–7. [DOI] [PubMed] [Google Scholar]
- 45.van der Veek SMC, Derkx BHF, Benninga MA, et al. Cognitive behavior therapy for pediatric functional abdominal pain: A randomized controlled trial. Pediatr 2013;132:e1163–72. [DOI] [PubMed] [Google Scholar]
- 46.O’Connell ME, Boat T, Warner KE. Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. National Research Council (US) and Institute of Medicine (US) Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults: Research Advances and Promising Interventions. 2009. [Google Scholar]
- 47.World Health Organization. Integrating mental health in primary care: A global perspective. London Journal of Primary Care. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


