Summary
Background
Early behavioural risk factors such as unbalanced diets, physical inactivity and tobacco and alcohol consumption lead to chronic diseases in later life. We conducted a cluster-randomised controlled trial to measure the effect of a school-based health-promotion intervention in reducing the behavioural risk factors of chronic diseases.
Methods
Twelve public schools in the Chandigarh, India were randomised to the intervention and control arm. Adolescents studying in eighth grade (n = 453), their parents (n = 395) and teachers (n = 94) were recruited for the current study. The Precede-Proceed Model was followed for intervention development. Intervention in each cluster comprised of one classroom session, four physical activity (PA) sessions every week for adolescents and four separate sessions for parents and teachers. Primary outcomes were eight binary or continuous measures of behavioural risk factors among adolescents (n = 359). Physical Activity Questionnaire-Adolescents (PAQ-A) scores were used to estimate physical activity. The ANCOVA based on cluster proportions or means was used to estimate the intervention effect accounting for baseline data.
Findings
Among adolescents, the intervention reduced salt intake by 0.5 g/d (95% CI: −0.9, −0.1), proportion of current alcohol users by 5% (95% CI: −9, −0.007), and increased fruit consumption by 18 g/d (95% CI: 5, 30) and PA by 0.2 PAQ-A score (95% CI: 0.07, 0.3). However, the intervention had no effect on the sugar and vegetable intake and on smokers and tobacco chewers. Exploratory analysis revealed that among parents, PA increased by 205 metabolic equivalents task (MET) units (95% CI: 74.5, 336), fruits intake by 20 g/d (95% CI: 6, 34), and vegetable intake by 117 g/d (95% CI: 50.5, 183). Whereas salt consumption decreased by 0.5 g/d (95% CI: 0.15, 0.9) and the proportion of current alcohol users declined by 5% (95% CI: 9, −1) among parents. Vegetable consumption increased by 149 g/d (95% CI: 12, 286) among teachers.
Interpretation
The intervention package implemented among adolescents by involving parents and teachers is an effective model for school-based behaviour-change interventions.
Funding
MK received partial funding from the George Institute for Global Health, Hyderabad, India for the salt-reduction component of the study.
Keywords: Adolescents, Diet, Physical activity, Tobacco, Alcohol, Non-communicable diseases, Health promotion, Health education, School
Research in context.
Evidence before this study
Behavioural risk factors such as unbalanced diets, physical inactivity, and tobacco and alcohol consumption that develop in young age group lead to chronic diseases in later life. The prevalence of behavioural risk factors that make people more vulnerable to chronic diseases and interventions to reduce these diseases were reviewed using MeSH words. Google Scholar and PubMed were searched comprehensively and extensively using the following search string: (((((((((((Diabetes∗) OR (Diabetes prevalence∗)) OR (Hypertension∗)) OR (Hypertension prevalence)) OR (Behavior intervention∗)) OR (Health promotion intervention)) OR (Chronic disease)) OR (Non-communicable disease)) OR (School intervention [MeSH Terms])))) AND (((((Adolescents) OR (Behavior risk factors)) OR (Health education)))). Out of all relevant research and intervention studies, 14 were international studies and out of these only 5 were Indian studies. Of all the international studies, only few had used theoretical framework for implementing and evaluating the intervention, but these interventions were found effective in changing the outcome measures in focus. Most of these studies had shorter intervention duration and did not assess the effect of the intervention through robust study designs. None of the Indian studies have involved parents and teachers even though school and home environments may influence early-life behaviours. Use of models and theories increases the sustainability of the intervention. Interventional studies based on various health promotion theories and interventions appropriate for the study design and target population need to be carried out to increase the sustainability of the changed behaviours to reduce the subsequent burden of chronic diseases in later life. Further, the intervention studies for low and middle income countries (LMICs) such as India need to be developed considering the sociodemographic, cultural, and economic context for effective and sustainable behaviour change.
Added value of this study
The present study is first of its kind that has involved parents and teachers to provide supportive environments for the effective behaviour change among early adolescents (aged 10–15 years). Formative research was carried out to develop an intervention based on participants’ needs. Community consultation and Proceed-Precede Model for planning, implementation, and evaluation helped design a pragmatic intervention with potential for scale-up if found effective. Micro planning of the intervention helped maintain uniformity of the delivered intervention across all six clusters with the same messages implemented simultaneously following the same pattern and flow of sessions. Cluster randomised controlled trials (RCT) design was chosen over an individual RCT to minimise the threat of any intervention contamination, and ANCOVA entirely at cluster means helped in assessing the intervention's effect by not underestimating or overestimating the impact due to time-invariant factors other than the intervention.
The present study has also provided evidence that the health promotion intervention can be implemented smoothly in school settings by fitting the intervention activities in the spare time of the adolescents. This further makes it easy to incorporate health promotion intervention in the present school curriculum that can be easily replicated.
Implications of all the available evidence
The present study demonstrated the potential of setting-based behaviour change model for reducing risk factors to prevent chronic diseases in LMICs. The present study provides evidence that the health promotion intervention package implemented in the school settings with the involvement of parents' and teachers' is an effective model for replicating behaviour change interventions in public schools. To sustain the changed behaviours, it is recommended to integrate the implemented health promotion intervention package in the school curriculum that can be delivered through teachers or health professionals after testing in implementation research mode.
Introduction
Technological advancements and fast-paced globalisation have improved the living conditions of people worldwide. This transition has shifted dietary behaviours from traditional home-cooked meals to processed food (high in salt, sugar and fat) along with low consumption of fruits and vegetables. With the increased use of machines and technologies, there is a proportional increase in the sedentary behaviours of individuals. The growing availability and early exposure to alcohol and tobacco-related products have increased their use early in life.1 Unbalanced diets, physical inactivity, and tobacco and alcohol use are risky behaviours for health. These risky behaviours, over time, develop into conditions like obesity, high blood pressure, and elevated blood lipids and glucose levels, which often develop into several chronic diseases in adulthood.2 Epidemiological evidence suggests that the prevalence of these chronic conditions in low and middle income countries (LMICs) has increased.2
Currently, 71% of the global disease burden is imposed solely by chronic diseases such as diabetes, cancer, and cardiovascular diseases. Globally, chronic diseases are responsible for 40 million deaths.3 More than one-third of these deaths are premature. Out of these premature deaths, around 85% occur in LMICs.3 India resonates with the global scenario. The top ten risk factors leading to more than half (58%) of the disability-adjusted life years (DALYs) globally in 2019 were responsible for nearly half of the DALYs (49%) in India in the same year.4,5 Chronic diseases impose a considerable economic burden on LMICs like India. First, once chronic diseases develop, they require lifelong medications, increasing the total treatment costs. Second, productivity losses due to premature deaths and disabilities indirectly affect India's gross domestic product.6
The burden of chronic diseases cannot be addressed until efforts are made to reduce associated behavioural risk factors.7 As chronic diseases of adulthood result from behavioural risk factors that usually begin during early adolescence (10–15 years), interventions should be started in early adolescence to prevent and reduce their burden in later life. Behavioural interventions are more effective when implemented at a younger age.6 Schools are known to be health-promoting hubs as adolescents spend a lot of their daytime learning at school. Peer involvement is necessary for interventions targeting peer-driven behaviours like tobacco and alcohol consumption.7
Out of a few studies carried out earlier among adolescents in the school settings of LMICs, most studies lack a theoretical framework for developing and implementing interventions.8 Many studies focused on one risk factor or implemented interventions of shorter duration.9 The interventions from high-income countries (HICs) may not be effective in LMICs like India, as interventions need to be developed considering the socio-demographic and cultural context.10 Therefore, the present study was designed to evaluate the effectiveness of a school-based health-promotion intervention package in reducing behavioural risk factors of chronic diseases among adolescents, their parents and teachers.
Methods
Study setting and design
A cluster-randomised controlled trial (cRCT) was carried out in the public schools of the Union Territory of Chandigarh, India. A baseline assessment was carried out in 12 randomly selected schools from May 2018 to September 2019. After baseline assessment, an intervention was developed and implemented in the intervention arm from September 2019 to March 2020. Both arms were assessed for the outcome indicators at the end-line assessment from September 2020 to April 2021.
Sample size
The data from the Department of School Education, Chandigarh, revealed that 106 public schools had eighth-grade classes. On average, 10,790 adolescents studied in eighth grade in these schools in previous years. Most schools had four to five sections in eighth-grade classes. Each section of the class had about 30 adolescents. Therefore, the sample size was estimated for a cluster size of 30 adolescents.
The required number of clusters for 80% power for each primary outcome was calculated separately using expected means or proportions for the control arm, intervention effects, and coefficient of variation values based on data for adolescents from recent studies.11, 12, 13, 14, 15 Out of all risk factors, the maximum number of clusters (n = 12) was considered the sample size for the study.
From all the 12 clusters, one parent of each participating adolescent and their class teachers were recruited (on average, seven teachers from each cluster). The details of the sample size calculation are mentioned in the protocol published earlier.16
Sampling method
Permission from the Director of Public Instruction (DPI), School Education, Chandigarh, was obtained to conduct the study in public schools. As DPI did not allow enrolment of private schools, these schools were not included in the study. Simple random sampling was used to select twelve public schools and one eighth-grade class in each selected school (Supplementary Figure S1). First, twenty-four schools, double the number required for the study, were randomly selected using a random number table from the list of 106 public schools with 8th-grade classes.17 Administrators of these 24 schools were approached from the list sequentially to obtain their consent. For each refusal, the next school on the list was approached. After receiving approval from the first twelve schools, the list was closed. Second, within each of the 12 selected schools, a section of the eighth-grade class was chosen randomly. As each school has four eighth-grade sections, namely, A, B, C and D, a number was assigned on folded paper slips for all the sections of the eighth-grade class. Later, a person other than the first author randomly selected a paper slip from the shuffled lot. After completing the baseline assessment, all twelve clusters were stratified into the income quartiles with strata sizes of 2, 4, 4 and 2 clusters, respectively. From each income quartile category, half of the clusters were randomised into the intervention arm and the other half to the comparison arm. This was done so the intervention and comparison clusters have a similar economic profile. The corresponding author randomised schools by selecting folded paper slips from shuffled lots.
Participants
Behavioural risk factors for chronic diseases emerge during early adolescence. Based on this knowledge and analysis of the school curriculum, consenting adolescents from eighth grade were selected, along with their one parent, based on the adolescents' and parents' choice, and those teachers who were in direct contact with adolescents. Teachers with direct contact were the subject teachers, mid-day meal in-charge, counsellors, physical education (PE) teachers and class in-charges. Additional inclusion criteria were the participants not intending to leave the city for another year from the recruitment date and parents and teachers below the age of 65.
Outcome measures
Primary measures were changes in dietary behaviours, salt intake (g/day [g/d]), sugar intake (g/d), fruits and vegetable intake (g/d), physical activity (Physical Activity Questionnaire-Adolescents [PAQ-A] scores for adolescents and metabolic equivalents [METs] for parents and teachers) and tobacco and alcohol (current tobacco and alcohol users). Secondary outcome measures were changes in BMI (mm Kg2), systolic blood pressure (SBP), diastolic blood pressure (DBP) (mmHg), and excretory urinary salt (g/d).
Data collection tools and methods
The data collection tool included socio-demographic and behavioural risk factor assessment, anthropometric measures, blood pressure (BP), and spot urine sample collection. Socio-economic status (SES) was assessed using the 'Kuppuswamy 2018 scale'.18 This scale uses information about the education and occupation of the head of the household and the household's total monthly income to score and rank participants into five categories of socio-economic status, i.e., lower, upper-lower, lower-middle, upper-middle, and upper.18 The first author (SK) recorded the dietary, PA, tobacco, alcohol, anthropometric and BP data. A team of three members, including SK, collected spot urine samples. Standard operating procedures were developed to maintain uniformity and standardisation in sample collection.
The 24-h dietary recall questionnaire was used twice on non-consecutive days to assess dietary behaviours (Nutritional status was defined in terms of salt sugar, fruit and vegetable intake, and BMI).19 The details of estimations of the dietary behaviours, such as salt, sugar, fruits and vegetable intake into g/d, are presented in the supplement (Appendix S1). For adolescents, the Physical Activity Questionnaire-Adolescents (PAQ-A) and the short International Physical Activity Questionnaire (IPAQ) for parents and teachers were used to assess physical activity (PA) levels.20,21 For adolescents, the Global School-based Health Survey (GSHS)-2007 and relevant questions from the WHO STEPS survey questionnaire for parents and teachers were used to assess tobacco and alcohol behaviours.22,23
Self-administered tools were used among adolescents in the classroom setting. SK was present to explain each question to adolescents before they recorded their responses. SK conducted interviews in school settings with parents and teachers. After data collection, participants' anthropometric and BP measurements were recorded in a separate room. The height and weight were recorded using standardised tools and methods (Appendix S2). BP of all participants was recorded using a digital sphygmomanometer (Appendix S2). The spot urine samples were collected during house visits on Monday mornings and analysed using standardised laboratory tests for urinary salt levels on the same day (Appendix S3). To further assess the 24-h excretory salt levels through spot urine samples, the INTERSALT with potassium equation was used (Appendix S4).
Intervention development
All six Precede-Proceed Model (PPM) phases were followed.24 The first four phases of the PPM were used to develop the intervention package, phase five to implement the intervention, and phase six dealt with impact evaluation.24
Formative research comprised ten group meetings with adolescents, parents, and teachers from October 2017 to February 2018 and a consultation workshop with school principals, teachers, and the medical officer-in-charge of school health in August 2018. The descriptive analysis of group meetings revealed adolescents' preference for spicy food. Low affordability was mentioned for low consumption of fruits and vegetables. Barriers to PA were hectic class schedules and subject teachers using the physical education (PE) classes to complete pending syllabi. On the other hand, adolescents wanted to have more PE classes. Exposure to tobacco and alcohol was readily available at home due to parents' or elder siblings' using these substances. Parents agreed their involvement could be crucial in building supportive home environments for behaviour change. Teachers suggested that free time in the curriculum can be used to conduct classroom intervention sessions.
In a one-day consultation workshop, the study's objectives, a summary of baseline assessment, a descriptive analysis of group meetings, and the proposed intervention developed until that time were presented to the participants. Participants agreed that teachers' involvement is essential in PA, and time-slot allotment for intervention can be done without disturbing the school routine. Based on these findings, the intervention was micro-planned to identify potential barriers and facilitators for developing a robust intervention. Thus, the final intervention was based on epidemiological and social diagnosis and was aligned with the school curriculum.
Intervention package
The intervention package for adolescents comprised of interactive learning sessions of 30 min per week, a PA session of 30 min four times per week, and the use of measuring spoons for salt and sugar measurement while preparing food at home during the 6-month intervention period (Appendix S5 and S6). Participants were provided with informational pamphlets in the local language. These pamphlets were based on the dietary guidelines of the National Institute of Nutrition (NIN), India.25 The physical activity levels for adolescents and adults and the consequences of tobacco and alcohol were as per WHO recommendations.26,27 Among adolescents, the main focus of the intervention was dietary behaviours, PA, tobacco, and alcohol use, while medication adherence was a minor part of the intervention. The four behavioural risk factors and medication adherence were focused equally among parents and teachers. All sessions were implemented as decided for adolescents, parents, and teachers.
Intervention implementation
One hundred and fifteen sessions were planned for adolescents and four sessions each for parents and teachers during the six-month intervention period. On average, the participation rate for each intervention session was 30 adolescents, 22 parents and three teachers. Process evaluation was carried out through a self-administered questionnaire two months after the start of intervention among the adolescents from the intervention arm. For each session, the participation rate was 86% among adolescents, 63% and 100% for parents and teachers, respectively.
Impact evaluation
The end-line evaluation for all participants started eight months after intervention implementation was over. The same tools and data collection methodology were used to assess the end-line and baseline assessment. Generalising estimating equations (GEEs) that accounted for the data's clustering were used to assess change within each arm. Data were aggregated by the cluster at each time point to assess the change between arms before performing conventional ANCOVA on the cluster means.28
Ethical considerations
Permission was obtained from the Institutional Ethics Committee of the Post-Graduate Institute of Medical Education and Research, Chandigarh (INT/IEC/2018/000082). The DPI, School Education, Chandigarh, granted permission to conduct the study in the schools (1296-DSE-UT-S5-11(65)11-II). The study was registered in the Clinical Trial Registry-India (CTRI/2019/09/021452). Written assent of adolescents and consent from their parents and teachers were obtained. They were informed about the study purpose, data to be collected, estimated time for data collection, the confidentiality of the data, and the risks involved (a behavioural-intervention study with no potential harm to the participants), before their enrolment in the study.
The reports for urinary salt excretion were provided to the participants. Participants with BP above 140/90 mmHg and abnormal urine test reports were referred to the doctors of the local health centre. The comparison arm participants were provided informational pamphlets as a standard of care.
Results
Baseline assessment
Of the 462 eligible adolescents, 453 consented to the baseline assessment (Fig. 1). One parent was supposed to be enrolled in the study for each adolescent. However, 395 consenting parents enrolled in the study. Adolescents were encouraged to enrol their mothers, as most mothers prepared meals at home; their involvement could lead to healthy dietary practices (Fig. 1). Though the sample size estimate of teachers was 84, 94 teachers interacting with eighth-grade adolescents were eligible at the time of data collection. All teachers consented to be part of the study (Fig. 1).
Fig. 1.
Participants' response rate for the primary outcomes at the baselineassessment.
Adolescents
At baseline, the majority were boys (55%), most (78%) belonged to the age category of 11–13 years, Hindu religion (87%), general caste category (66%), and upper-lower SES category (61%). The socio-demographic characteristics of the participants in the intervention arm were similar to the participants in the comparison arm at the baseline (Table 1).
Table 1.
Socio-demographic characteristics of the adolescents (n = 462).
| Characteristics | Comparison (n = 227) n (%) |
Intervention (n = 235) n (%) |
|---|---|---|
| Sex | ||
| Male | 126 (56) | 127 (54) |
| Female | 101 (44) | 108 (46) |
| Age (years) | ||
| 11–13 | 125 (55) | 115 (49) |
| 14–16 | 102 (45) | 120 (51) |
| Religion | ||
| Hindu | 198 (87) | 206 (88) |
| Muslim | 18 (8) | 19 (8) |
| Sikh | 9 (4) | 8 (3) |
| Others | 2 (1) | 2 (1) |
| Caste | ||
| General | 143 (63) | 161 (69) |
| OBC | 25 (11) | 23 (10) |
| Scheduled caste | 59 (26) | 51 (21) |
| Socio-economic status | ||
| Lower | 15 (7) | 24 (10) |
| Upper lower | 136 (62) | 142 (61) |
| Lower middle | 58 (26) | 49 (21) |
| Upper middle and upper | 12 (5) | 17 (8) |
The mean salt, sugar, fruit and vegetable consumption was 4.5 g/d, 36 g/d, 32.7 g/d and 193 g/d, respectively. Most adolescents (84%) had low PA levels. Fourteen percent of adolescents had used alcohol at least once, and 7% were current alcohol users. Seven percent of the adolescents had smoked at least once. Three percent were current smokers, and 6% were current tobacco chewers.
The prevalence of thinness was more than overweight and obesity; 9% and 15% were in the severe thinness and thinness category, respectively, compared to 7% and 3% in the overweight and obese categories. The BP among adolescents was categorised using percentiles based on their sex, age and height. Three percent of adolescents had elevated BP, and 5% had borderline-elevated BP. Evaluating spot urine samples using INTERSALT with potassium equation revealed that almost all adolescents (99.5%) had high to extremely high levels of excretory salt.
Parents and teachers
Among 395 enrolled parents, 61% were mothers; most of them (68%) belonged to the 30–39-year age group, Hindu religion (89%), general caste category (55%), and upper-lower SES (61%). Among 94 teachers, 79% were females, and the majority belonged to the 30–49-year age category (75%), Hindu religion (69%), general caste category (82%), and upper SES (66%). The distribution of behavioural risk factors at baseline has been presented in Supplementary Table S1 of the supplement.
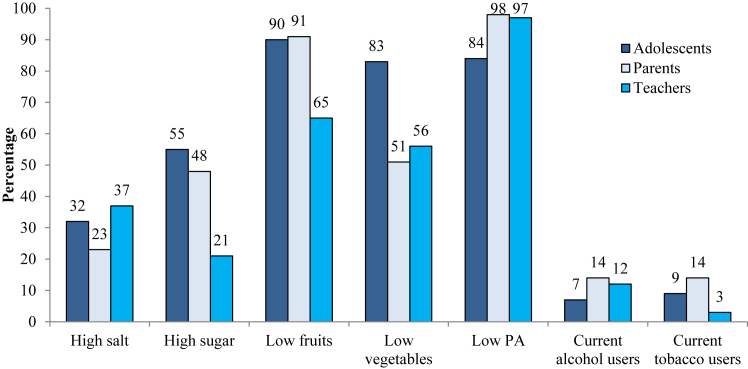
Adolescents had the highest proportion of high sugar (more than 20 g/d for females, 25 g/d for males) and low vegetable intake (below 300 g/d for both sexes). Parents had the highest proportion of low PA levels (between 1 and 2.5 PAQ-A scores for adolescents and less than 600 METs/min/week for parents and teachers) and alcohol and tobacco use. Almost the same proportion of adolescents and parents had low fruit intake (below 100 g/d for both sexes) (91%). Teachers had the highest proportion of high salt intake (more than 5 g/d for both sexes) (Fig. 2).
Fig. 2.
Prevalence of behavioural risk factors among participants at the baselineassessment.
Intervention implementation and process evaluation
There were few modifications during intervention implementation for adolescents (Appendix S7). Intervention sessions were conducted across all clusters simultaneously. One hundred sixteen sessions were carried out in each of the six clusters for adolescents, including 96 PA sessions that respective PE teachers conducted. Four classroom sessions were carried out for parents in each intervention cluster. As parents usually came at different times to the school, one school day was kept exclusively for each session. Each session was repeated three times in one cluster, with an average number of seven parents in one session. The absentees were contacted telephonically to share classroom discussions. Teachers had different schedules and were approached during lunch breaks or free periods. On average, three teachers were part of each session. Three such sessions were repeated on a school day to cover all teachers from each cluster on the same day. Of all respondents (n = 173) who were administered the process evaluation questionnaire, 94% reported that intervention positively affected their daily routine and behaviours. The barriers and actions to improve intervention uptake during process evaluation have been provided in the supplement (Supplementary Table S2).
Impact evaluation
The end-line evaluation started eight months after the intervention was implemented. The drop-outs rate during impact evaluation was high due to the COVID-19 pandemic (Fig. 3). The net effect of the intervention was assessed by measuring changes in primary and secondary outcome measures among adolescents by performing ANCOVA at cluster means. The intra-cluster coefficient (ICC) with 95% CI for each primary outcome is presented in the Supplementary Table S10. The exploratory analysis was carried out due to high dropouts among parents and a small sample size of teachers. Socio-demographic characteristics were compared among dropouts and follow-up participants at the endline (Supplementary Table S3).
Fig. 3.
Participants' response rate for the primary outcomes at the endlineassessment.
The intervention significantly reduced salt consumption and increased fruit intake among adolescents. The PA decreased in both arms; however, the decrease in the comparison arm was substantially higher than the intervention arm. The net effect of the intervention was significant in limiting the reduction in PA levels despite COVID-19 pandemic restrictions. The intervention had no significant effect on sugar and vegetable intake (Table 2). The net mean effect of the intervention was a significant reduction in alcohol use (−6.3%) among adolescents, but it had no effect on tobacco smoking and chewing (Table 3).
Table 2.
Primary outcomes: changes in the dietary intakes and physical activity levels among adolescents.
| Indicators | Comparison group (n = 227) |
P | Intervention group (n = 235) |
P | ANCOVA |
P | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | End-line | Change (95% CI) | Baseline | End-line | Change (95% CI) | Net change (95% CI) | ||||
| Mean (SE) | Mean (SE) | |||||||||
| Salt consumption (g/d) | 4.5 (0.13) | 4.9 (0.15) | 0.4 (−0.03, 0.8) | 0.07 | 4.6 (0.12) | 4.3 (0.12) | −0.2 (−0.5, 0.09) | 0.2 | −0.5 (−0.9, −0.1) | 0.007 |
| Sugar consumption (g/d) | 38.5 (2.7) | 32.3 (1.8) | −6.2 (−12.7, 0.2) | 0.06 | 33.5 (1.7) | 30.4 (1.8) | −3.1 (−7.8, 1.5) | 0.2 | −2 (−7, 3) | 0.5 |
| Fruits intake (g/d) | 34.7 (5) | 28.4 (4.5) | −6.3 (−18.7, 6.1) | 0.3 | 30.8 (5.5) | 45.8 (4.5) | 14.9 (1.5, 28.4) | 0.03 | 18 (5, 30) | 0.006 |
| Vegetable intake (g/d) | 177.8 (11.4) | 271.8 (18.1) | 93.9 (53.6, 134.4) | <0.001 | 207.9 (11.4) | 283.3 (16.6) | 75.3 (38.5, 112.1) | <0.001 | 7 (−42, 55) | 0.8 |
| Physical inactivity (PAQ-A score 1–5) | 2.3 (0.04) | 2.05 (0.04) | −0.27 (−0.4, −0.17) | <0.001 | 2.3 (0.04) | 2.26 (0.04) | −0.06 (−0.2, 0.04) | 0.04 | 0.2 (0.07, 0.3) | 0.001 |
Recommended Dietary Allowance: Salt-5 g/d (both sexes), sugar-20 g/d for females, 25 g/d for males, fruits-100 g/d (both sexes), vegetables. 300 g/d (both sexes).
PA level: Low = 1–2.5 PAQ-A score, moderate = 2.5–3.5 PAQ-A scores and high = 3.5–5 PAQ-A score.
Table 3.
Primary outcomes: changes in the alcohol and tobacco consumption among adolescents.
| Primary outcomes | Comparison group (n = 227) |
P | Intervention group (n = 235) |
P | ANCOVA |
P | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | End-line | Change (95% CI) | Baseline | End-line | Change (95% CI) | Net change (95% CI) | ||||
| n (%) | n (%) | |||||||||
| Current alcohol users | 11 (4.8) | 10 (4.9) | 0.1 (−3, 3) | 0.9 | 18 (8) | 4 (1.7) | −6.2 (−10, −2) | 0.005 | −5 (−9, −0.007) | 0.02 |
| Current smokers | 6 (2.6) | 7 (3.6) | 0.9 (−2, 4) | 0.5 | 7 (3) | 8 (4) | 1.0 (−3, 5) | 0.6 | 0.3 (−4, 5) | 0.8 |
| Current tobacco chewers | 5 (2.2) | 3 (1.5) | −0.7 (−3, 1) | 0.5 | 20 (9) | 2 (1) | −8 (−10, −4) | <0.001 | −1.3 (−4, 1) | 0.4 |
Current alcohol use: More than one drink in the past thirty days (one drink-350 ml of beer/150 ml wine/44 ml distilled whisky). Current smokers: Smoked in the past 30 days. Current tobacco chewers: Use any chewable tobacco such as gutkha, pan-masala, chaini-khaini, etc., in the past thirty days.
The net change signifies that intervention did not affect adolescents' SBP, DBP, BMI, or urinary excretory salt (Table 4).
Table 4.
Secondary outcomes: changes in the BMI, blood pressure, and excretory salt among adolescents.
| Secondary Outcomes | Comparison group (n = 227) |
P | Intervention group (n = 235) |
P | ANCOVA |
P | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | End-line | Change (95% CI) | Baseline | End-line | Change (95% CI) | Net change (95% CI) | ||||
| Mean (SE) | Mean (SE) | |||||||||
| Body mass index (kg/m2) | 17.2 (0.2) | 19.04 (0.3) | 1.8 (1.3, 2.4) | <0.001 | 17.6 (0.2) | 19.7 (0.3) | 2.1 (1.6, 2.6) | <0.001 | 0.5 (−0.2, 1.3) | 0.2 |
| Systolic blood pressure (mmHg) | 99.7 (1.2) | 119 (1.3) | 19.3 (16.2, 22.3) | <0.001 | 105.8 (1) | 120.2 (1.4) | 14.4 (11.1, 17.5) | <0.001 | 1 (−3, 5) | 0.6 |
| Diastolic blood pressure (mmHg) | 60.7 (0.8) | 72.2 (0.9) | 11.5 (9.3, 13.8) | <0.001 | 59 (0.8) | 70.3 (1) | 11.3 (9, 13.6) | <0.001 | −1 (−4, 2) | 0.4 |
| Urinary excretory Salt (g/d) | 6.9 (0.16) | 7.8 (0.2) | 0.9 (0.4, 1.4) | <0.001 | 7.3 (0.17) | 7.4 (0.22) | 0.14 (−0.4, 0.6) | 0.6 | −0.4 (−1, 3) | 0.3 |
In the exploratory analysis, among parents, the intervention increased fruit intake by 20 g/d, vegetable consumption by 117 g/d and PA by 205 METs and decreased salt intake by 0.5 g/d and current alcohol users by 5% (Supplementary Table S4). The intervention increased the net consumption of vegetables among teachers by 149 g/d (Supplementary Table S5). There were no changes in tobacco consumption and secondary outcomes among parents and teachers (Supplementary Tables S6–S9).
Discussion
Impact evaluation revealed that the intervention was effective in increasing fruit intake and reducing salt intake and alcohol use and limiting the decline in PA levels. Most of the present study's findings align with earlier studies. Intervention in an another study significantly increased fruit consumption but had no effect on adolescents’ vegetable intake.29 The salt intake decreased in the intervention arm and increased in the comparison arm.30 Sugar consumption decreased in both groups, but the net difference was not statistically significant.31 The intervention reduced alcohol consumption and effectively limited the decrease in PA levels.8 The intervention had no effect on SBP and DBP.32 There was an insignificant net decrease in urinary excretory salt levels.30
In the present study, the proportion of obesity increased in the comparison group and decreased in the intervention group, but the net difference was not statistically significant. In an earlier study, there was less increase in BMI among the intervention group.33 The decrease in PA and increase in obesity may have occurred because of COVID-19 imposed lockdown that restricted mobility.
Adolescents consumed 4.5 g/d of salt in the present study which is within the guidelines.25 In HICs intake of salt is higher compared to Indian studies.34 Mean sugar consumption was almost double compared to the current recommendations,25 which is close to other Indian studies,35,36 however, it is much lower than other countries.37,38 The mean fruit intake was within the recommended dietary allowance (RDA), which was not the case in a study carried out in Tanzania (another LMIC).39 In the present study, only 8% of the adolescents consumed vegetables adequately, whereas in Iran 23% followed the RDA.40 The low consumption of vegetables in the present study may be because most adolescents were from the lower socio-economic groups. Moreover, the data collection tools, and different RDA criteria may add to this difference across countries. Eighty-four percent of adolescents had low physical activity levels in the present study. Other studies support these findings.41, 42, 43 The proportion of physical inactivity was more in the females than males, which was higher than most of the studies carried out in the world.44 One possible explanation for these differences could be cultural practices in different geographical locations. Tobacco chewers (6%) in the present study were similar to another Indian study.13 However, alcohol consumption (7%) was lower than a study carried out in Ghana.45
In the present study most of the above mentioned variables were quantitative but sample size was estimated based on the prevalence of risk factors16 however, changes in the outcomes were estimated quantitatively in this cRCT as this approach is more efficient in measuring the intervention effects and the study had adequate power to evaluate these effects quantitatively. In addition, standard measurement tools were used to minimise measurement errors.
The 24-h dietary recall was used over other nutritional assessment tools, such as Food Frequency Questionnaire, which has high recall bias.46 One of the limitations of using 24-dietary recall for salt assessment was underestimation of the salt intake.19 To overcome this limitation, the salt was also estimated from urine samples. The mean salt levels estimated from dietary recall were nearly half compared to the levels estimated through urine samples. The PAQ-A tool was used to assess adolescent PA levels as it has high retention and response rates.20 It also provides flexibility regarding different sports played by adolescents. The PAQ-A tool had previously been modified based on the requirements of Indian adolescents.47 The short-IPAQ was used to assess PA levels among parents and teachers which has been validated to measure all dimensions of physical activities among adults.21
Tobacco and alcohol questions were adopted from the Global School-Based Student Health Survey (GSHS) and WHO STEPS-Survey.22,23 These tools have been widely used globally and have a high response rate and reliability. The pre-intervention and post-intervention assessments were done confidentially without identifying the school and the adolescent. This approach may have increased accurate reporting for alcohol and tobacco use.
Overweight and obesity were identified using BMI as it strongly correlates with metabolic and disease outcomes.48 Digital and mercury sphygmomanometers vary about three mmHg from the reference value.49 For accuracy, the BP was recorded three times for each participant, with a gap of 1 min between each reading. The average of the three readings was recorded as the participant's BP. In addition, intervention planning and implementation was also done systematically.
The intervention was also implemented among parents and teachers as parents and teachers provide adolescents with supportive environments for behaviour change.50 The intervention duration was 6 months as previous studies suggest that an intensive intervention for a minimum of six months may lead to sustainable behaviour changes.50 As adolescents are in the growing stage, the intervention focused more on PA. The PA component was incorporated into the school curriculum with the help of PE teachers. The intervention components related to dietary behaviours and tobacco and alcohol use were allotted equal time, and sessions were delivered by SK. A thorough micro-planning helped in identification of potential barriers and facilitators. The home environment was utilised for promoting healthy diets and reducing tobacco and alcohol. The Parents Teacher Association (PTA) meetings were used to interact with parents, and school hours were the best time to interact with teachers in groups.
One significant issue faced was the occurrence of COVID-19 pandemic during the study timeline. After the intervention implementation, the lockdown was imposed in March 2020. This delayed data collection for impact evaluation by eight months. This delay might not have shown the intervention's actual effect due to the dilution of the intervention. However, the effect measured after eight months may reflect the sustainable impacts of the intervention. Refreshers of the intervention were given to participants twice during the lockdown period to sustain behaviours. Delay in impact evaluation assessment due to COVID-19 lockdown may not have shown the immediate effect of the intervention. However, the effect measured after eight months may reflect the sustainable impacts of the intervention.
There were several methodological considerations taken into account, such as a cluster RCT design was chosen over an individual RCT to minimise the threat of intervention contamination. Health education interventions are likely to diffuse out into the comparison schools, therefore, school clusters were located at a distance in different sectors of the city. Every sector has a government public school, with adolescents usually enrolled from the same sector, thus, contamination chances were minimised.
Confounders may have effects even in the cRCTs, mainly when the number of clusters is small. The present study had six clusters each in the intervention and comparison arm. Therefore, stratified random sampling based on households' income status was used to allocate clusters in both arms. The mixed regression is not valid for small sample size; therefore, ANCOVA at cluster means was used. It assessed the effect of the intervention at the cluster level with the lowest type-1 error rate and maximum power compared to other statistical methods for this number of clusters.28 The lack of blinding in the data collection and intervention implementation may have led to observer bias. However, to minimise bias, the objective measures, such as BMI, BP and urinary excretory salt levels, were assessed using standardized tools and methods. There are several strengths of the study, such as formative research and PPM for planning, implementation and evaluation helped streamline intervention and design a pragmatic intervention with the potential for scale-up. Quality control of the data and repeated follow-up, especially for urine sample collection, is another strength of the study. Smooth intervention implementation by fitting intervention activities in the spare time of the adolescents indicates that health-promotion intervention could be incorporated into the school curriculum. Public schools usually cater to the lower socio-economic groups in India. The implication of excluding private schools may lead to a lack of representation of all socio-economic groups, limiting generalisability. However, the low-middle income group is the largest section of Indian society, and their representation is one of the strengths of this study. The main limitations of the study were using multiple primary outcomes and non-adjustment of P-values in several statistical tests and the lack of any policy-related component in the intervention.
Due to ethical reasons, the comparison group was provided with informational pamphlets. The comparison arm was not the actual ‘control’ group but had a low-intensity standard of care intervention. High drop-out rates at the end-line assessment among parents may lead to bias in the impact assessment, and the small sample size of the teachers increases the likelihood of type 2 errors. Hence, the exploratory analysis was carried out among parents and teachers during the impact assessment.
The health-promotion intervention package was acceptable to users as the intervention was implemented without disturbing the school activities. The involvement of parents and teachers in school-based interventions provided a supportive environment. Among adolescents, the intervention was effective in reducing salt intake and alcohol use and increasing fruit consumption and physical activity but had no effect on sugar intake, vegetable intake, and tobacco use.
The school-based intervention activities can be replicated in other settings with modifications to account for differences in contextual factors. Integrating the intervention package into the school curriculum should be tried, which can be delivered by teachers or health professionals for sustainable behaviour change. Parents and teachers influence adolescents' behaviour choices, and their involvement is recommended for school-based interventions designed for behaviour change.
Future studies should test the effectiveness of pictorial health education promoting healthy behaviours painted on the school walls to promote and sustain healthy behaviours. The impact of introducing policies such as food labels and taxes for tobacco and alcohol should be made to test the effectiveness of policy-level interventions. In addition, one needs to ensure that healthy food options at school canteens replace processed foods high in salt and sugar.
Contributors
SK conceptualised the study, carried out the data collection and curation and its formal analysis and prepared and wrote the original draft of the manuscript. RK and MK provided their supervision for the study and contributed to the data presentation. MK contributed to conceptualising and in acquiring partial funds used in the present study and applying models for intervention development. RK, PVML and MK validated the data and results and provided the resources required to carry out this study. All authors were involved in reviewing and editing and gave their final approval for the version to be published.
Data sharing statement
Three years after collecting the end-line assessment, a wholly de-identified data set would be delivered to an appropriate data archive for sharing purposes.
Declaration of interests
MK received partial funding from the George Institute for Global Health, Hyderabad, India for the salt-reduction component of the study (payment made to the institution's account with project ID 5562). SK received senior research fellowship from University Grants Commission under NET-JRF scheme (payment made directly). Authors received no support for the present manuscript in terms of study materials, medical writing, article processing charges, etc. Authors declare no other conflicts of interest.
Acknowledgements
We extend our special thanks to the George Institute of Global Health, Hyderabad, India, for providing us with the funds for the salt-reduction component of the study.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2024.100353.
Appendix A. Supplementary data
References
- 1.Beaglehole R., Epping-Jordan J., Patel V., et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372(9642):940–949. doi: 10.1016/S0140-6736(08)61404-X. [DOI] [PubMed] [Google Scholar]
- 2.Forouzanfar M., Afshin A., Alexander L., et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1659–1724. doi: 10.1016/S0140-6736(16)31679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Non-communicable diseases - fact sheet. World Health Organization; Geneva: 2018. http://www.who.int/en/news-room/factsheets/detail/noncommunicable-diseases [cited 2022 Dec 21]. Available from: [Google Scholar]
- 4.GBD 2019 Viewpoint Collaborators Five insights from the global burden of disease study 2019. Lancet. 2020;396(10258):1135–1159. doi: 10.1016/S0140-6736(20)31404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Global health estimates: leading causes of DALYs. World Health Organization; Geneva: 2018. https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/global-health-estimates-leading-causes-of-dalys [cited 2022 Jan 15]. Available from: [Google Scholar]
- 6.Jayawardena R., Ranasinghe P., Byrne N.M., Soares M.J., Katulanda P., Hills A.P. Prevalence and trends of the diabetes epidemic in South Asia: a systematic review and meta-analysis. BMC Public Health. 2012;12:380. doi: 10.1186/1471-2458-12-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Health education: theoretical concepts, effective strategies and core competencies. World Health Organization; Geneva: 2012. https://applications.emro.who.int/dsaf/EMRPUB_2012_EN_1362.pdf#:∼:text=Health%20education%3A%20theoretical%20concepts%2C%20effective%20strategies%20and%20core,health%20and%20healthy%20public%20policy%20and%20health%20outcomes [cited 2022 Jan 23]. Available from: [Google Scholar]
- 8.Reddy K.S., Arora M., Perry C.L., et al. Tobacco and alcohol use outcomes of a school-based intervention in New Delhi. Am J Health Behav. 2002;26(3):173–181. doi: 10.5993/ajhb.26.3.2. [DOI] [PubMed] [Google Scholar]
- 9.Salwa M., Atiqul Haque M., Khalequzzaman M., Al Mamun M.A., Bhuiyan M.R., Choudhury S.R. Towards reducing behavioral risk factors of non-communicable diseases among adolescents: protocol for a school-based health education program in Bangladesh. BMC Public Health. 2019;19(1):1002. doi: 10.1186/s12889-019-7229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mall A.S.K., Bhagyalaxmi A. An informal school-based, peer-led intervention for prevention of tobacco consumption in adolescence: a cluster randomized trial in rural Gandhinagar. Indian J Community Med. 2017;42(3):143–146. doi: 10.4103/ijcm.IJCM_25_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Global school-based student health survey (Age 13-15) Central Board of Secondary Education; India: 2007. https://www.who.int/ncds/surveillance/gshs/2007_India_CBSE_fact_sheet.pdf [cited 2021 Nov 16]. Available from: [Google Scholar]
- 12.Peltzer K., Pengpid S. Fruits and vegetables consumption and associated factors among in-school adolescents in five Southeast Asian countries. Int J Environ Res Public Health. 2012;9(10):3575–3587. doi: 10.3390/ijerph9103575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar P., Kumar D., Ranjan A., Singh C.M., Pandey S., Agarwal N. Prevalence of hypertension and its risk factors among school going adolescents of Patna, India. J Clin Diagn Res. 2017;11(1):SC01–SC04. doi: 10.7860/JCDR/2017/23886.9196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ha K., Chung S., Lee H.S., et al. Association of dietary sugars and sugar-sweetened beverage intake with obesity in Korean children and adolescents. Nutrients. 2016;8(1):31. doi: 10.3390/nu8010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National survey on drug use and health (NSDUH), 2013, (Age 12 or older for Asian population). North Carolina, USA. https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health Department of Health and Human Services; [cited 2021 May 17]. Available from:
- 16.Kaur S., Kaur M., Kumar R. Health promotion intervention to prevent risk factors of chronic diseases: protocol for a cluster randomized controlled trial among adolescents in school settings of Chandigarh (India) PLoS One. 2022;17(2) doi: 10.1371/journal.pone.0263584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chandigarh school administation. http://chdeducation.gov.in/?q=node/144 Chandigarh: Department of Education; [cited 2021 Dec 2]. Available from:
- 18.Sharma R. Revised Kuppuswamy's socioeconomic status scale: explained and updated. Indian Pediatr. 2017;54(10):867–870. [PubMed] [Google Scholar]
- 19.Jonnalagadda S.S., Mitchell D.C., Smiciklas-Wright H., et al. Accuracy of energy intake data estimated by a multiple-pass, 24-hour dietary recall technique. J Am Diet Assoc. 2000;100(3):303–308. doi: 10.1016/s0002-8223(00)00095-x. (quiz 309-11) [DOI] [PubMed] [Google Scholar]
- 20.Kowalski K.C., Crocker P.R., Donen R.M. The physical activity questionnaire for older children (PAQ-C) and adolescents (PAQ-A) manual. Coll Kinesiol Univ Sask. 2004;87(1):1–38. https://www.prismsports.org/UserFiles/file/PAQ_manual_ScoringandPDF.pdf Available from: [Google Scholar]
- 21.Lee P.H., Macfarlane D.J., Lam T.H., Stewart S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011;8:115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Global school-based student health survey (GSHS) World Health Organization; Geneva: 2013. https://www.who.int/ncds/surveillance/gshs/GSHS_Core_Modules_2013_English.pdf [cited 2022 Jan 2]. Available from: [Google Scholar]
- 23.Non-communicable Diseases and Mental Health Cluster . World Health Organization; Geneva: 2005. WHO STEPS surveillance manual : the WHO STEPwise approach to chronic disease risk factor surveillance.https://apps.who.int/iris/handle/10665/43376 [cited 2021 Aug 29]. Available from: [Google Scholar]
- 24.Green L., Kreuter M. 3rd ed. Mayfield Publishing Company; Mountain View, CA: 1999. Health promotion planning: an educational and ecological approach. [Google Scholar]
- 25.Nutrient requirements for Indians. Indian Council of Medical Research-National Institute of Nutrition; Hyderabad, India: 2020. https://www.im4change.org/upload/files/RDA_short_report%281%29.pdf [cited 2021 Dec 3]. Available from: [Google Scholar]
- 26.Bull F.C., Al-Ansari S.S., Biddle S., et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Report on tobacco use. World Health Organization; Geneva: 2021. https://apps.who.int/iris/bitstream/handle/10665/344222/9789240032842-eng.pdf [cited 2021 Dec 17]. Available from: [Google Scholar]
- 28.Hooper R., Forbes A., Hemming K., Takeda A., Beresford L. Analysis of cluster randomised trials with an assessment of outcome at baseline. BMJ. 2018;360 doi: 10.1136/bmj.k1121. [DOI] [PubMed] [Google Scholar]
- 29.Covelli M.M. Efficacy of a school-based cardiac health promotion intervention program for African-American adolescents. Appl Nurs Res. 2008;21(4):173–180. doi: 10.1016/j.apnr.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 30.He F.J., Wu Y., Feng X.X., et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ. 2015;350 doi: 10.1136/bmj.h770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahajan A., Negi P.C., Gandhi S., Sharma D., Grover N. Impact of school-based health behavioral intervention on awareness, practice pattern of healthy lifestyle, and cardiometabolic risk factors among school children of Shimla: a cluster-randomized, intervention study. Indian J Pediatr. 2022;89(4):343–350. doi: 10.1007/s12098-021-03786-6. [DOI] [PubMed] [Google Scholar]
- 32.Mcmurray R.G., Harrell J.S., Bangdiwala S.I., Bradley C.B., Deng S., Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. J Adolesc Health. 2002;31(2):125–132. doi: 10.1016/s1054-139x(02)00348-8. [DOI] [PubMed] [Google Scholar]
- 33.Friedemann C., Heneghan C., Mahtani K., Thompson M., Perera R., Ward A.M. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ. 2012;345 doi: 10.1136/bmj.e4759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh G.M., Micha R., Khatibzadeh S., et al. Global, regional, and national consumption of sugar-sweetened beverages, fruit juices, and milk: a systematic assessment of beverage intake in 187 countries. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0124845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bowen L., Ebrahim S., De Stavola B., et al. Dietary intake and rural-urban migration in India: a cross-sectional study. PLoS One. 2011;6(6) doi: 10.1371/journal.pone.0014822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Radhika G., Sathya R.M., Ganesan A., et al. Dietary profile of urban adult population in South India in the context of chronic disease epidemiology (CURES-68) Public Health Nutr. 2011;14(4):591–598. doi: 10.1017/S136898001000203X. [DOI] [PubMed] [Google Scholar]
- 37.Gatenby S.J., Aaron J.I., Jack V.A., Mela D.J. Extended use of foods modified in fat and sugar content: nutritional implications in a free-living female population. Am J Clin Nutr. 1997;65(6):1867–1873. doi: 10.1093/ajcn/65.6.1867. [DOI] [PubMed] [Google Scholar]
- 38.Paineau D.L., Beaufils F., Boulier A., et al. Family dietary coaching to improve nutritional intakes and body weight control: a randomized controlled trial. Arch Pediatr Adolesc Med. 2008;162(1):34–43. doi: 10.1001/archpediatrics.2007.2. [DOI] [PubMed] [Google Scholar]
- 39.Nicholaus C., Martin H.D., Kassim N., Matemu A.O., Kimiywe J. Dietary practices, nutrient adequacy, and nutrition status among adolescents in boarding high schools in the Kilimanjaro Region, Tanzania. J Nutr Metab. 2020;2020 doi: 10.1155/2020/3592813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Al Ani M.F., Al Subhi L.K., Bose S. Consumption of fruits and vegetables among adolescents: a multi-national comparison of eleven countries in the Eastern Mediterranean Region. Br J Nutr. 2016;115(6):1092–1099. doi: 10.1017/S0007114515005371. [DOI] [PubMed] [Google Scholar]
- 41.Roy S., Dasgupta A. Physical activity pattern among the adolescents of a rural community in West Bengal. Indian J Community Med. 2009;34(4):366–367. doi: 10.4103/0970-0218.58404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Swaminathan S., Selvam S., Thomas T., Kurpad A.V., Vaz M. Longitudinal trends in physical activity patterns in selected urban South Indian school children. Indian J Med Res. 2011;134(2):174–180. [PMC free article] [PubMed] [Google Scholar]
- 43.Odunaiya N.A., Ayodele O.A., Oguntibeju O.O. Physical activity levels of senior secondary school students in Ibadan, Western Nigeria. West Indian Med J. 2010;59(5):529–534. [PubMed] [Google Scholar]
- 44.Nath A., Garg S., Deb S., Ray A., Kaur R. Profile of behavioural risk factors of non-communicable diseases in an urban setting in New Delhi. Indian J Public Health. 2009;53(1):28–30. [PubMed] [Google Scholar]
- 45.Oppong Asante K., Meyer-Weitz A., Petersen I. Substance use and risky sexual behaviours among street connected children and youth in Accra, Ghana. Subst Abuse Treat Prev Policy. 2014;9:45. doi: 10.1186/1747-597X-9-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jaceldo-Siegl K., Knutsen S.F., Sabaté J., et al. Validation of nutrient intake using an FFQ and repeated 24 h recalls in black and white subjects of the adventist health study-2 (AHS-2) Public Health Nutr. 2010;13(6):812–819. doi: 10.1017/S1368980009992072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fernández I., Canet O., Giné-Garriga M. Assessment of physical activity levels, fitness and perceived barriers to physical activity practice in adolescents: cross-sectional study. Eur J Pediatr. 2017;176(1):57–65. doi: 10.1007/s00431-016-2809-4. [DOI] [PubMed] [Google Scholar]
- 48.Pal A., Pari A.K., Sinha A., Dhara P.C. Prevalence of undernutrition and associated factors: a cross-sectional study among rural adolescents in West Bengal, India. Int J Pediatr Adolesc Med. 2017;4(1):9–18. doi: 10.1016/j.ijpam.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.A'Court C., Stevens R., Sanders S., Ward A., McManus R., Heneghan C. Type and accuracy of sphygmomanometers in primary care: a cross-sectional observational study. Br J Gen Pract. 2011;61(590):e598–e603. doi: 10.3399/bjgp11X593884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Michie S., van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.