Abstract
‘Wound man’ refers to a stylised diagram used in early medical textbooks to illustrate the various injuries that the human body can sustain in battle. We have adapted this concept to create ‘Wound cat’, as a way to emphasise the type and location of injuries cats may inflict on one another during combat. We have further extended this concept to include wounds that may result from interactions with rodents and snakes. It is hoped that our ‘Wound cat’ concept will assist less experienced clinicians locate sites of cat bites and scratches, and to recognise why certain infections arise in particular stereotyped locations. In addition, this approach should assist veterinarians in determining which pathogens are most likely to be involved in wounds located in a given anatomical region.
Readers of crime fiction may be familiar with the concept of ‘Wound man’, as the symbolic importance of this historic image was critical in FBI Special Agent Will Graham catching the serial killer, Hannibal ‘the cannibal’ Lecter in the novel Red Dragon (Harris 1981). During a visit to Lecter's office, Graham notices an antique medical textbook open to a picture of ‘Wound man’. Upon seeing this image, Graham deduced Lecter was the killer he sought because an earlier victim, a deer hunter with an arrow wound, had been killed in his workshop and laced to a pegboard in a manner reminiscent of the ‘Wound man’ motif.
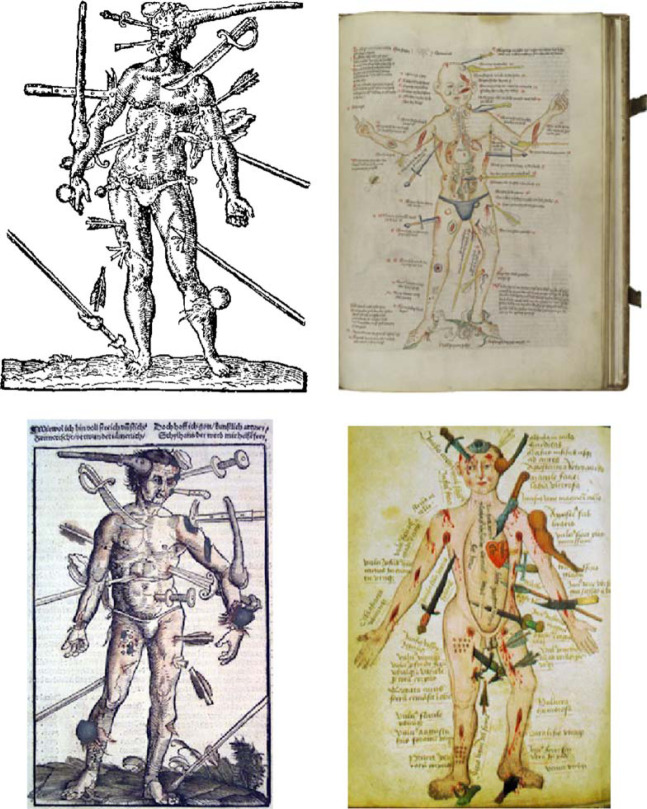
‘Wound man’ is a mnemonic figure used in many early medical textbooks to illustrate representative injuries to which the human body is prone in battle. These range from blows to the head, to stab and arrow wounds, and bites by snakes, insects and dogs. Fine examples of this figure occur in a number of manuscripts and printed books. One of the illustrations in Fig 1 comes from a wood engraving on the title-page of the first English edition of The Method of Curing Wounds made by Gun-shot published in London in 1617. A similar illustration, also called ‘Wound man’, is on the cover of Hans von Gersdorff's Feldtbuch der Wundartzney (Fieldbook of Wound Surgery) published in Strasbourg in 1530. Indeed, it is likely the ‘Wound man’ concept was introduced into medieval surgery in the German-speaking world (http://library.wellcome.ac.uk/doc_WTL038432.html; http://www.st-mike.org/medicine/woundman.html).
Fig 1.
Several versions of the ‘Wound man’ mnemonic figure.
It would be useful in feline practice to have an iconic image akin to ‘Wound man’ and we have developed such an image, which we propose to call ‘Wound cat’. This image attempts to represent diagrammatically the range of wounds which cats are likely to inflict on one another during combat.
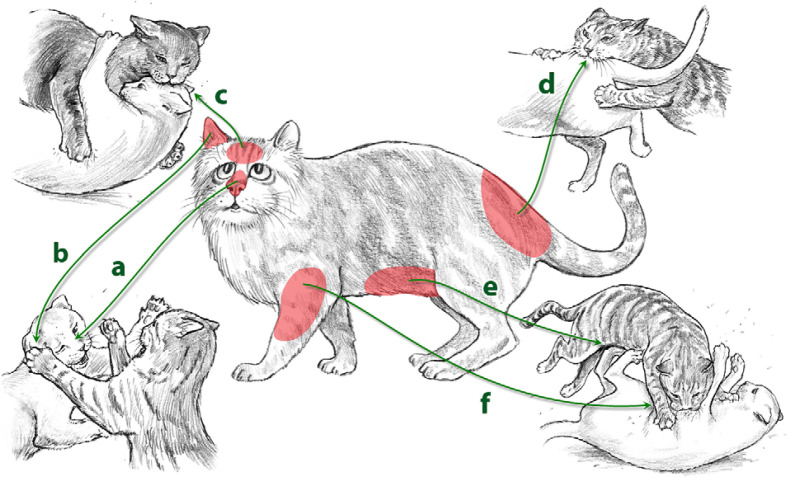
The point of having a ‘Wound cat’ is to preserve an image in one mind's eye, as an aide-mémoir, when examining patients that may have been in a cat fight. Target areas likely to be subjected to injury, such as the head (Fig 2; locations a–c), antebrachium (Fig 2; location f), tail base (Fig 2; location d), axilla, and ventral abdomen (Fig 2; location e) should be subjected to increased scrutiny during physical examination. In addition to locating wounds, ‘Wound cat’ provides a guide to the most likely sources of injury and, therefore, the organisms most likely to be involved in wound infections (Table 1). Knowledge of the organisms implicated most commonly provides a guide for prophylactic antimicrobial intervention.
Fig 2.
‘Wound cat’.
Table 1.
Wound site and organisms most likely to be the cause of infection
| Source of injury | Wound site | Origin of organisms | Organisms frequently isolated |
|---|---|---|---|
| Cat bite(s) | Head | Normal flora of the gingival cleft and oral cavity of assailant | Closed abscesses – polymicrobial anaerobic infections |
| Antebrachium | |||
| Tail base | |||
| Axilla | |||
| Ventral abdomen | 72% obligate anaerobes | ||
|
|||
| 28% facultative anaerobes (or microaerophilic anaerobes) | |||
|
|||
| These polymicrobial infections have a predictable susceptibility pattern. Antibiotics of choice include: benzyl penicillin, amoxycillin, amoxycillin clavulanate, doxycycline, clindamycin, metronidazole but not the fluoroquinolones, cephalosporins or aminoglycosides. | |||
| Cat scratch | Head | Soil/environmental saprophytes or transient commensals on skin surface | Bacteria |
| Ears | Gram-positive bacteria, eg, Staphylococcus species, Rhodococcus equii, Corynebacterium species, Nocardia species, Mycobacterium species (rapid and slow growing saprophytes) | ||
| Ventral and lateral abdomen and thorax | |||
| Antebrachium | |||
| Nasal bridge | |||
| Fungi | |||
| Sporothrix schenkii, Paecilomyces species, Alternaria species, dermatiaceous (pigmented) fungi and numerous others | |||
| Algae | |||
| Prototheca wickerhamii | |||
| These disparate infections with saprophytes have unpredictable susceptibility. Prophylaxis with doxycycline is prudent, but for documented infections it is vital to characterise the isolate by culture and perform susceptibility testing, ideally at a reference laboratory. | |||
| Rodent bite(s) | Face | ||
| Distal limbs | |||
| Rat | Mycobacterium lepraemurium | ||
| Vole | Mycobacterium tuberculosis variant (?M microti) | ||
| Drugs of choice include two to three of rifampicin, clarithromycin, clofazimine and moxifloxacin; linezolid may prove to have a place in future studies. |
Many cats suffering from wounds received in serious fights present for veterinary attention for non-specific signs, before the development of bacterial cellulitis or abscessation. Typically, they are lame, sore, inappetent and miserable the day following the fight. The wounds, which may be hidden by fur, can be missed by inexperienced clinicians, especially when a suggestive history is lacking. A clue to a traumatic underlying aetiology may be provided by detecting moderate to markedly elevated blood creatine kinase levels. The best way to confirm the clinical suspicion is by palpation of at risk areas (for hyperaesthesia, scabs, swelling, etc) or by clipping the overlying fur to look for evidence of penetrating injury (ie, teeth puncture wounds, scratches or other raking injuries). Detection of contaminated injuries at this early stage allows the clinician to confidently prescribe a short course of antibiotics (such as amoxicillin clavulanate or doxycycline), which, if given sufficiently early, may prevent an anaerobic cat bite abscess developing.
Thinking of ‘Wound cat’ is also useful when analysing the distribution of lesions resulting from unusual microbial pathogens. For example, saprobes may be introduced via contamination of penetrating injuries with soil or dirt. A recent paper on naso-ocular lesions attributable to a range of saprophytic organisms (fungi, bacteria, algae) could be explained nicely using the ‘Wound cat’ concept (Figs 2a, 3) (Malik et al 2004). Similarly, lesions seen months after the bites from infected rodents result in the characteristic ‘face, forearm and digits’ lesion distribution of feline leprosy due to Mycobacterium lepraemurium (Malik et al 2002).
Fig 3.

Localised infection of the subcutis of the nasal bridge with the fungus Paecilomyces lilacinus. This likely arose following a contaminated cat scratch injury to the cat's face.
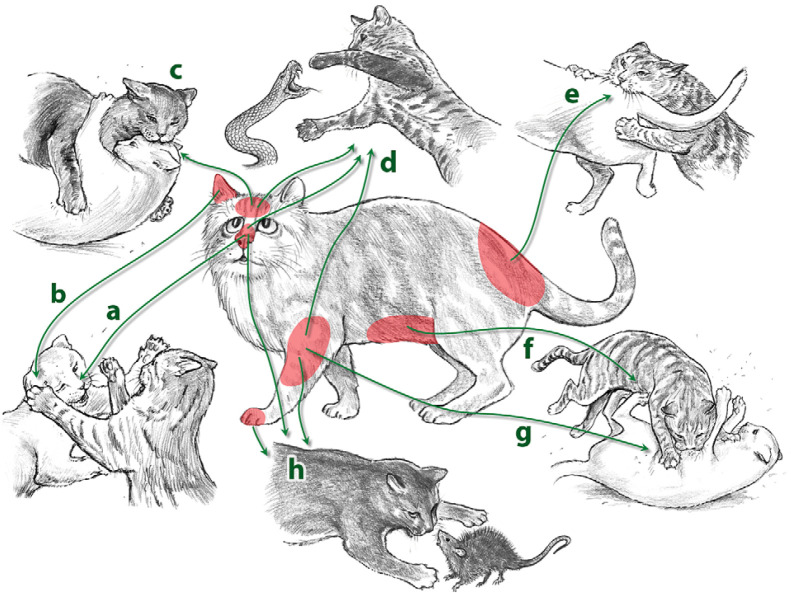
Figures 3–8 illustrate cat lesions which correspond to specific ‘Wound cat’ locations. These lesions include an infection of the nasal bridge (Fig 3) with the fungal organism Paecilomyces lilacinus, auricular sporotrichosis (Fig 4), two cat fight abscesses, including one before and after drainage (Figs 5, 6a, b), inguinal panniculitis due to rapidly growing mycobacteria such as M fortuitum and M smegmatis (Fig 7), and feline leprosy attributable to M lepraemurium (Fig 9).
Fig 4.

Localised infection of the pinna of a cat attributable to Sporothrix schenckii. Presumably organisms were instilled following a bite or scratch injury contaminated by soil or plant material (Wigney and Oxenford 1993).
Fig 5.

Cat fight abscess in the pre-auricular area. This likely resulted from a cat bite injury and inoculation of a variety of obligate anaerobic and facultatively anaerobic bacteria (Love et al 2000).
Fig 6.

Anaerobic cat fight abscess on the side of a cat's face, before (a) and after (b) surgical drainage and insertion of a latex drain.
Fig 7.

Inguinal panniculitis due to a rapidly growing Mycobacterium, in this instance M fortuitum. The organism was probably inoculated following a raking scratch injury inflicted by the perpetrators hind claws (Malik et al 2000). The cats head is at the top of the photo, while its tail is at the bottom.
Fig 8.
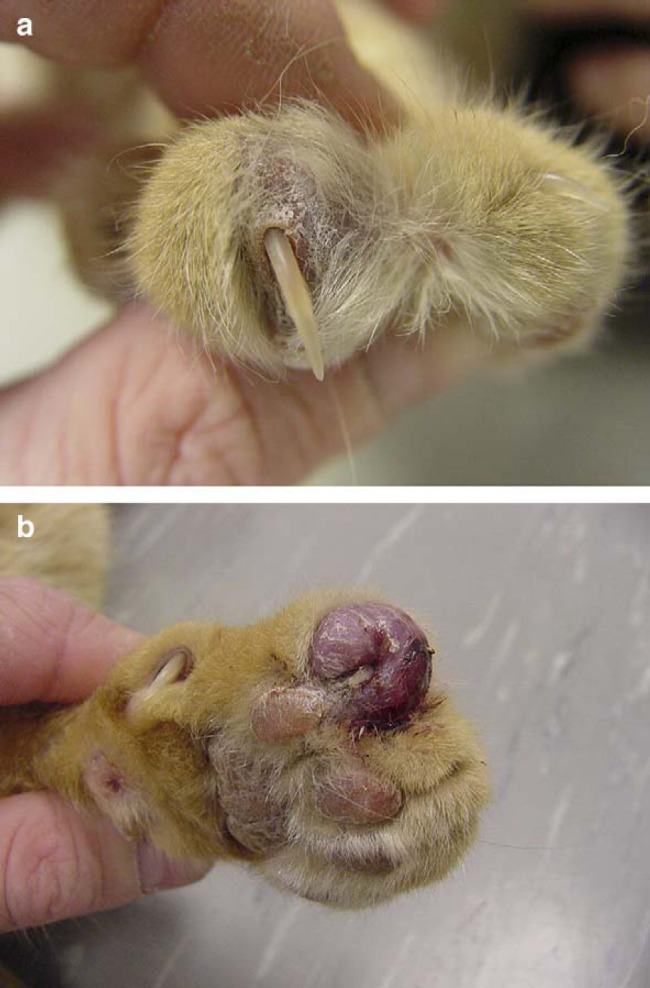
Lesion on the distal limb of a cat due to inoculation of M lepraemurium following a rat bite injury.
Fig 9.
More complex version of ‘Wound cat’, incorporating bites from snakes and rats, in addition to cat fight injuries.
Although we are proud of Bozena's artwork, this must be considered a first attempt at ‘Wound cat’. Further reiterations will need to encompass other wounds sustained by cats, including rat bites, snakebites (whose major impact is envenomation) (Fig 9), injuries from projectiles such as air guns and arrows, and dog bite injuries. Perhaps this challenge will be taken up by other feline-empathic veterinary investigators?
References
- Harris T. Red Dragon, 1981, Arrow Books: London. [Google Scholar]
- Love D.N., Malik R., Norris J.M. Bacteriological warfare amongst cats: what have we learned about cat bite infections?, Veterinary Microbiology 74, 2000, 179–193. [DOI] [PubMed] [Google Scholar]
- Malik R., Wigney D.I., Dawson D., Martin P., Hunt G.B., Love D.N. Infection of the subcutis and skin of cats with rapidly growing mycobacteria: a review of microbiological and clinical findings, Journal of Feline Medicine and Surgery 2, 2000, 35–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik R., Hughes M.S., James G., Chen S.C.A., Mitchell D.H., Wigney D.I., Martin P., Canfield P.J., Love D.N. Feline leprosy: two different clinical syndromes, Journal of Feline Medicine and Surgery 4, 2002, 43–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik R., Vogelnest L., O'Brien C.R., White J., Hawke C., Wigney D.I., Martin P., Norris J.M. Infections and some other conditions affecting the skin and subcutis of the naso-ocular region of cats – clinical experience 1987–2003, Journal of Feline Medicine and Surgery 6, 2004, 383–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigney D.I., Oxenford C.J. Feline sporotrichosis: successful surgical resolution, Australian Veterinary Practitioner 23, 1993, 28–30. [Google Scholar]