Abstract
Sporotrichosis is caused by Sporothrix schenckii. The cat is the animal species most affected by this mycosis and plays an important role in the zoonotic transmission of this disease. The definitive diagnosis is made by isolation of the fungus in culture; however, cytopathological examination is frequently used in cats. Medical records from cats treated at Instituto de Pesquisa Clínica Evandro Chagas/Fiocruz, Rio de Janeiro, Brazil, between 2004 and 2006 were reviewed. Criteria for inclusion were a diagnosis by isolation of S schenckii in culture and cytopathological examination of the same lesion as that used for collection of the culture material. Eight hundred and six cats were included in the study. Yeast-like structures suggestive of S schenckii were observed in 636 cases. The sensitivity of the method was 78.9%. Its practicality, low cost and sensitivity validate cytopathology as a safe technique for the presumptive diagnosis of sporotrichosis in cats.
Sporotrichosis is an infectious disease caused by the dimorphic fungus Sporothrix schenckii, which is usually localized to the skin and subcutaneous tissue. 1 The disease affects humans and a wide variety of animals, especially cats. 2,3 This mycosis shows a worldwide geographic distribution but is more common in tropical and subtropical climates. 4 Sporotrichosis is the most frequent subcutaneous mycosis in Latin America. 5 In Rio de Janeiro, Brazil, a large number of cases involving humans, dogs and cats have been reported since 1998. 2 Classically, S schenckii is transmitted by traumatic inoculation of skin with plant matter or soil contaminated with the fungus. Cases of zoonotic transmission through scratches, bites or contact with sick cats have been described during the epidemic occurring in Rio de Janeiro. 6 From 2005 through 2008, 804 human patients were diagnosed with sporotrichosis at the Instituto de Pesquisa Clínica Evandro Chagas (IPEC)/Fiocruz, Rio de Janeiro, Brazil. Contact with cats, either with clinically evident disease or with no clinical signs, was reported in 91% of the human cases. Bites and/or scratches were reported by 68% of these patients, suggesting such lesions as the putative means of transmission of the fungus. 7 Cats can be infected with the fungus during fights with cats with infections. 8 Infection of cats ranges from a subclinical form, which might progress to multiple skin lesions and fatal systemic involvement. 9 Subcutaneous nodules and ulcers are the most frequent skin lesions in sick cats and can be found at three or more non-contiguous anatomical sites. 3,9
The definitive diagnosis of sporotrichosis requires the isolation of S schenckii by culture at a temperature below 37°C for the hyphal form and above 37°C for the yeast form. 10 Yeast-like structures can be detected by histopathological and cytopathological examination. 11,12 The polymerase chain reaction (PCR) has been used to detect S schenckii infection in biopsy specimens from infected cats with good results. 13,14 However, this technique has not been applied to a clinical test population and is not currently commercially available.
For cytopathological examination, specimens can be obtained by aspiration of nodules, impression smears of ulcerated skin or exudate and by fine-needle aspiration of the lesion. 15 Smears are air-dried and stained with Romanowsky-type stains (eg, Wright or DiffQuik). 16 These stains are used in veterinary practice because of its low cost and simple preparation. 15 Analysis of exudate from skin lesions of cats with sporotrichosis often reveals numerous round, oval or cigar-shaped yeast-like structures inside macrophages and neutrophils or in the extracellular medium. These structures measure 3–5 μm in diameter and 5–9 μm in length, and are surrounded by a clear halo (Fig 1). 16
Fig 1.
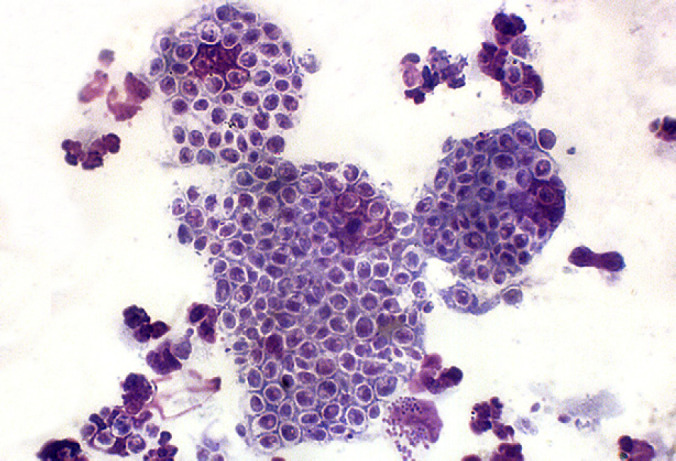
Photomicrograph of impression smear from ulcerated skin lesion in cat with sporotrichosis showing numerous cigar-shaped to oval or round budding yeast-like organisms fulfilled with blue cytoplasm with a single round pink nucleus surrounded by a non-staining cell wall within macrophages and extracellularly (Quick Panoptic stain, 100×).
The rapid, practical and reliable diagnosis of feline sporotrichosis is important for the early treatment of cats and prevention of zoonotic transmission. Although cytopathology is considered to be the fastest, most straightforward, and least expensive method for the diagnosis of feline sporotrichosis, 15 its sensitivity has not been investigated. Therefore, the objective of the present study was to establish the sensitivity of cytopathological examination in the diagnosis of feline sporotrichosis using mycological culture as the gold standard.
Materials and methods
Medical records from a cat cohort treated at the Laboratório de Pesquisa Clínica em Dermatozoonoses em Animais Domésticos (Lapclin-Dermzoo), IPEC/Fiocruz, Rio de Janeiro, Brazil, between 2004 and 2006 were reviewed. Criteria for inclusion were a diagnosis of sporotrichosis by isolation of S schenckii in culture and cytopathological examination of the same skin lesion as that used for collection of the culture material.
For culture, the material collected with a sterile swab was seeded onto Sabouraud dextrose agar and Mycobiotic agar (Difco) and incubated at 25°C. Dimorphism was confirmed by conversion to the yeast phase in brain-heart infusion broth at 37°C. For cytopathology, impression smears of the skin lesion were prepared on clean and dry glass slides and stained by the Quick Panoptic method (Instant Prov; Newprov), a Romanowsky-type stain similar to DiffQuik. The slides were analyzed by light microscopy using 40 and 100× objective lenses for the identification of yeast-like structures suggestive of S schenckii. A database was created and the sensitivity of the cytopathological method in relation to mycological culture was calculated using the SPSS program, version 17.0.
Results
A total of 806 cases of feline sporotrichosis from the metropolitan region of Rio de Janeiro were included in the study (Fig 2). Cytopathological examination of the skin lesions of these cats revealed the presence of yeast-like structures suggestive of S schenckii in 636 cases (Fig 1). The sensitivity of this method in relation to mycological culture was 78.9%.
Fig 2.

Feline sporotrichosis: ulcer on the bridge of the nose.
Discussion
This study represents the largest series of feline sporotrichosis cases diagnosed by fungal isolation and cytopathological examination. Several investigators reported the observation of abundant yeast-like structures by cytopathological examination of impression smears prepared from lesions of cats with feline sporotrichosis 11,17–23 , but the sensitivity of the method was not evaluated.
The sensitivity of cytopathology was considered to be satisfactory. This value was higher than that reported for histopathology (62.2%) using hematoxylin–eosin, Grocott's silver stain and periodic acid-Schiff for the diagnosis of feline sporotrichosis in 90 cats compared to isolation of S schenckii in culture. 9 The present results agree with other investigators who generally consider cytopathology to be an easy method for the diagnosis of feline sporotrichosis. 15,16 However, the percentage of false-negative cytopathological results observed in this study indicates that the visualization of yeast-like structures might be difficult in some cases and sporotrichosis should, therefore, not be excluded based only on the result of this method, in agreement with other investigators. 24 The factors that may have influenced the percentage of false-negative results include poor sample collection, too thick material on the slides, and also prior treatment with topical or systemic antifungal agents. Furthermore, practitioners with varying degrees of experience were responsible for reading the slides. In contrast to cats, dogs with sporotrichosis generally present a small number of yeast-like structures of S schenckii, a fact that impairs the cytopathological diagnosis in these animals. 16 In a study including 28 dogs with sporotrichosis confirmed by mycological culture, cytopathological examination identified yeast-like structures in nine smears (32%), 25 a value much lower than that found in the present study on cats.
In order to obtain adequate samples for cytological examination for feline sporotrichosis thin smears of lesions with more vital-appearing tissue rather than those consisting of primarily dried, crusted exudate should be sampled. 15 Additionally, at least two slides with three impressions on each of them are recommended to better obtain positive specimens.
For biosafety purposes the collection of cytology samples should be undertaken with standard safety procedures including disposable gloves, long sleeved impermeable gowns and optimal physical restraint of the animal. 26
Despite its lower sensitivity compared to mycological culture and the fact that the fungal elements observed might be confused with poorly encapsulated Cryptococcus strains and Histoplasma capsulatum in some situations, 15 cytopathology has several advantages. Whereas the growth of the hyphal form of S schenckii in culture generally starts a few days after seeding 27 and requires some additional days until conversion to the yeast phase, 28 the collection, processing and analysis of the material for cytopathology are performed consecutively and the result is obtained on the same day. In addition, cytopathology is more practical and less costly and is particularly important in situations in which culture is not possible because of its cost or lack of a microbiology laboratory, or in regions where the incidence of cases of feline disease is high, as observed in the metropolitan region of Rio de Janeiro.
Considering the sensitivity of cytopathology found in the present study, a positive result in a cat with a clinical suspicion of sporotrichosis permits the immediate initiation of antifungal treatment and the establishment of measures to prevent the transmission of S schenckii while awaiting the result of mycological culture. Therefore, in view of this feature and the rapidity, simplicity and low cost of the method, the routine use of cytopathology for the presumptive diagnosis of feline sporotrichosis at veterinary clinics is strongly recommended.
Acknowledgements
The authors thank the staff of Mycology Laboratory of IPEC/Fiocruz, Raquel de Oliveira and Ingrid Paes for technical support. This study was partially supported by the Health Strategic Research Support Program (PAPES V) – Fiocruz and by Grant Programme for the Study of Neglected and Reemerging Diseases/The Carlos Chagas Filho Foundation for the Support of Research in the State of Rio de Janeiro (FAPERJ). TMPS has a fellowship from the Technological and Scientific Development National Council (CNPq).
References
- 1.Kauffman C.A. Sporotrichosis, Clin Infect Dis 29, 1999, 231–236. [DOI] [PubMed] [Google Scholar]
- 2.Schubach A., Barros M.B., Wanke B. Epidemic sporotrichosis, Current Opin Infect Dis 21, 2008, 129–133. [DOI] [PubMed] [Google Scholar]
- 3.Pereira S.A., Passos S.R.L., Silva J.N., et al. Response to azolic antifungal agents for treating feline sporotrichosis, Vet Rec 166, 2010, 290–294. [DOI] [PubMed] [Google Scholar]
- 4.Ramos-e-Silva M., Vasconcelos C., Carneiro S., Cestari T. Sporotrichosis, Clin Dermatol 25, 2007, 181–187. [DOI] [PubMed] [Google Scholar]
- 5.Costa E.O., Diniz L.S., Netto C.F., Arruda C., Dagli M.L. Epidemiological study of sporotrichosis and histoplasmosis in captive Latin American wild mammals, Sao Paulo, Brazil, Mycopathologia 125, 1994, 19–22. [DOI] [PubMed] [Google Scholar]
- 6.Barros M.B., Schubach A.O., Schubach T.M., Wanke B., Lambert-Passos S.R. An epidemic of sporotrichosis in Rio de Janeiro, Brazil: epidemiological aspects of a series of cases, Epidemiol Infect 136, 2008, 1192–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freitas D.F., Valle A.C., Paes R. Almeida, Bastos F.I., Galhardo M.C. Zoonotic sporotrichosis in Rio de Janeiro, Brazil: a proctated epidemic yet to be curbed, Clin Infect Dis 50, 2010, 453. [DOI] [PubMed] [Google Scholar]
- 8.Larsson C.E., Goncalves M.A., Araujo V.C., Dagli M.L., Correa B., Neto C. Fava. Feline sporotrichosis: clinical and zoonotic aspects, Rev Inst Med Trop Sao Paulo 31, 1989, 351–358. [DOI] [PubMed] [Google Scholar]
- 9.Schubach T.M., Schubach A., Okamoto T., et al. Evaluation of an epidemic of sporotrichosis in cats: 347 cases (1998–2001), J Am Vet Med Assoc 224, 2004, 1623–1629. [DOI] [PubMed] [Google Scholar]
- 10.Schubach T.M., Schubach A., Okamoto T., et al. Canine sporotrichosis in Rio de Janeiro, Brazil: clinical presentation, laboratory diagnosis and therapeutic response in 44 cases (1998–2003), Med Mycol 44, 2006, 87–92. [DOI] [PubMed] [Google Scholar]
- 11.Crothers S.L., White S.D., Ihrke P.J., Affolter V.K. Sporotrichosis: a retrospective evaluation of 23 cases seen in northern California (1987–2007), Vet Dermatol 20, 2009, 249–259. [DOI] [PubMed] [Google Scholar]
- 12.Schubach T.M., Ade O. Schubach, Cuzzi-Maya T., et al. Pathology of sporotrichosis in 10 cats in Rio de Janeiro, Vet Rec 152, 2003, 172–175. [DOI] [PubMed] [Google Scholar]
- 13.Kano R., Watanabe K., Murakami M., Yanai T., Hasegawa A. Molecular diagnosis of feline sporotrichosis, Vet Rec 156, 2005, 484–485. [DOI] [PubMed] [Google Scholar]
- 14.Hirano M., Watanabe K., Murakami M., et al. A case of feline sporotrichosis, J Vet Med Sci 68, 2006, 283–284. [DOI] [PubMed] [Google Scholar]
- 15.Clinkenbeard K.D. Diagnostic cytology: sporotrichosis, Compend Contin Educ Pract Vet 13, 1991, 207–211. [Google Scholar]
- 16.Welsh R.D. Sporotrichosis, J Am Vet Med Assoc 223, 2003, 1123–1126. [DOI] [PubMed] [Google Scholar]
- 17.Freitas D., Migliano M., Neto L. Zani. Esporotricose – Observação de caso espontâneo em gato doméstico (F catus), Rev Fac Med Vet Univ Sao Paulo 5, 1956, 601–604. [Google Scholar]
- 18.Peaston A. Sporotrichosis, J Vet Int Med 7, 1993, 44–45. [DOI] [PubMed] [Google Scholar]
- 19.Nogueira R.H.G., Guedes R.M.C., Cassali G.D., Gheller V.A., Moreira Y.K. Cat sporotrichosis (Sporothrix schenckii) with transmission to human being: clinical, microbiological and pathological aspects, Arq Bras Med Vet Zootec 47, 1995, 43–51. [Google Scholar]
- 20.Meinerz A.R.M., Nascente P.S., Schuch L.F.D., et al. Esporotricose felina: relato de casos, Ci Anim Bras 8, 2007, 575–577. [Google Scholar]
- 21.Silva D.T., Pereira S.A., Gremião I.D.F., et al. Esporotricose conjuntival felina, Act Sci Vet 36, 2008, 181–184. [Google Scholar]
- 22.Colodel M.M., Jark P.C., Ramos C.J.R., Martins V.M.V., Schneider A.F., Pilati C. Esporotricose cutânea felina no Estado de Santa Carina: relatos de casos, Vet Foco 7, 2009, 18–27. [Google Scholar]
- 23.Iachini R. Sporotrichosis in a domestic cat, Rev Argent Microbiol 41, 2009, 27. [PubMed] [Google Scholar]
- 24.Kennis R.A., Rosser E.J., Jr., Dunstan R.W. Difficult dermatologic diagnosis, J Am Vet Med Assoc 204, 1994, 51–52. [PubMed] [Google Scholar]
- 25.dos Santos I.B., Schubach T.M., Leme L.R., et al. Sporotrichosis: the main differential diagnosis with tegumentary leishmaniosis in dogs from Rio de Janeiro, Brazil, Vet Parasitol 143, 2007, 1–6. [DOI] [PubMed] [Google Scholar]
- 26.Gremião I.D.F., Pereira S.A., Nascimento A., Jr., et al. Procedimento operacional padrão para o manejo de gatos com suspeita de esporotricose, Clin Vet 65, 2006, 69–70. [Google Scholar]
- 27.Nobre M.O., Castro A.P., Caetano D., Souza L.L., Meireles M.C.A., Ferreiro L. Recurrence of sporotrichosis in cats with zoonotic involvement, Rev Iberoam Micol 18, 2001, 137–140. [PubMed] [Google Scholar]
- 28.Werner A.H., Werner B.E. Sporotrichosis in man and animal, Int J Dermatol 33, 1994, 692–700. [DOI] [PubMed] [Google Scholar]


