Abstract
Enchondromas are benign tumors located primarily in long bones, some of which can be accidentally discovered during imaging exams conducted for other pathologies. These benign cartilaginous tumors are hard to differentiate from low grade chondrosarcomas, which require periodic follow ups. The purpose of this study was to identify the incidence of enchondromas in pediatric patients, to determine medical imaging criteria (Computed Tomography-CT and Magnetic Resonance Imaging-MRI) in order to differentiate enchondromas from other atypical cartilaginous tumors, and to identify a potential correlation between imaging aspects and clinical signs. The aim of this study was to review imaging findings of enchondromas in children
Keywords: Enchondromas , Pediatric , Benign cartilage tumors , Imaging
Introduction
Osseous tumors are generally less frequently found in patients, with benign tumors being more common than malignant osseous tumors [1, 2].
Enchondroma is a tumor of the medullary canal consisting primarily in hyaline cartilage.
This is one of the most common osseous tumors, making up approximately 12-14% of all benign bone tumors and 3-10% of all osseous tumors, benign and malignant [3].
Enchodroma is in the second place after osteochondroma with regards to the incidence of cartilaginous substrate osseous tumors in pediatric patients, representing approximately 24% of all benign osseous tumors in children and adolescents [3].
Other tumors can also be identified in the intra-medullary space, such being the case of chondrosarcoma, which makes up approximately 20-27% of all primary osseous sarcomas [3].
Osteochondromas, enchondromas, periosteal chondromas, chondroblastomas and chondromyxoid fibromas are all cartilaginous-type benign osseous tumors [2].
Enchondromas are usually located in the center of long bones and can grow in an asymmetric manner, resulting in endosteal scalloping [4].
In general, enchondromas are benign bone tumor lesions located in the short and long tubular bones, especially around the knee joint and proximal humerus, mostly detected after radioimaging investigations for other musculoskeletal pathologies, as enchondromas are conditions with almost no symptomatic response [5].
Clinically, enchondromas are painless, except in cases where they are associated with pathological bone fractures.
In the case of intraosseous cartilaginous lesions presenting with painful symptoms, the suspicion of chondrosarcoma can be risen [6].
Approximately 10% of patients diagnosed with enchondroma will have multiple tumors [6].
These patients are usually young and may have one of these syndromes: enchondromatosis (Maffucci syndrome or Ollier's disease) or, rarely, metachondromatosis (multiple enchondromas and osteochondromas) [6].
In adults, enchondromas are identified in 50% of cases in the medial or distal regions of metacarpal bones and in the proximal phalanges.
Other areas where these tumors can be found are the proximal and distal regions of the diaphysis in the femur and the humerus.
These lesions are not typically followed by any clinical signs, as they are usually identified in individuals in the 3rd and 4th decades of life, most times incidentally [2].
With the increasing use of MRI in the investigation of musculoskeletal (MSK) disorders, there has been an increase in the identification of incidental asymptomatic bone tumors with different locations, this being the case of enchondromas [7].
The therapeutic protocol for asymptomatic enchondromas is clinical and radio-imaging follow-up, but symptomatic lesions or those with suspicious radiographic features should be biopsied or excised.
Lesions that are increased in size (>5cm) or those located in expendable bones may be excised [6].
As for recurrence, this is less common and may be due to an incomplete surgical procedure, but should be a warning sign for chondrosarcoma [6].
Materials and Methods
This study included patients aged 13 to 17 years old, male and female, who have been examined radiologically, through Computed Tomography or MRI, on the recommendation of the pediatric surgeons that referred the patients to the Radiology Department of Craiova Emergency County Hospital.
Some patients had only X-ray exams, which are still useful for orienting in the diagnosis of enchodroma, but in some patients more performant imaging exams were needed to describe the potential lesions in more detail.
This retrospective study aimed to highlight the incidence of benign cartilaginous bone tumors, in particular enchondromas, in pediatric patients, in relation to their age, sex and location of the tumor, including the proportion in which imaging features of the lesions were present.
The radiological and imaging investigations were obtained from the electronic archive of the Radiology and Imaging Department of the Craiova Emergency Clinical County Hospital, as well as from the Department's library.
Patients aged up to 17 years old who had definite imaging characteristics for enchondroma were selected, while patients with lesions that did not fit the imaging characteristics for enchondroma or who had an uncertain presumptive diagnosis were not included in the study.
The selected patients received radiological, CT or MRI evaluations, the Department presenting with the following equipment:
-Perform X and Philips digital X-ray machines;
-Eltex X-ray and fluoroscopy machine;
-Toshiba Astelion 16-slice and General Electric Revolution 128-slice computer tomography machines;
-General Electric Signa 1.5T magnetic resonance imaging machine.
The MRI protocol consisted of T1-and T2-weighted sequences in at least one of the three planes (axial, coronal or sagittal) to which PD (proton density) and STIR (short tau inversion recovery) sequences were added to reveal the presence of possible edema in the soft tissue adjacent to the bone lesion.
Another type of sequence is 3D MERGE in the axial plane (multiple echo recombined gradient echo).
The sequences were taken with a FoV (field-of-view) between 220-240mm, and the sections had a thickness (gap) of 4.0/1.0 and 5.0/1.0mm.
All acquisitions were performed with localized markings superior and inferior to the lesion, and joints adjacent to the tumor lesions were included in the examination.
The CT examination protocol was limited to assessing the affected area in order to minimize the radiation dose, with bone and soft tissue window reconstructions at a 3mm gap.
The acquisition and reconstruction parameters were performed as following: tube current 150-200mA, tube voltage 100 or 120kV, pitch 0.8, matrix size 512×512.
Imaging evaluations were performed both with and without contrast agent, taking into account the glomerular filtration rate of the patients and possible contraindications such as: allergies to certain drugs, foods, iodine allergies, etc., and even background medication contraindicating the administration of iodine or Gadolinium-based contrast agent.
A written informed consent was obtained from all the representatives of pediatric patients, as well as the approval of the Craiova County Hospital Ethics Committee.
Anonymity and confidentiality of patients’ data were ensured.
Results
The clinical cases included in this study were pediatric patients who presented in the Pediatric Surgery Department of Craiova Emergency County Hospital during a three-year period, 2019 to 2022.
Of the 18 patients selected, 12 were male and 6 were female, indicating a predisposition to enchondromas in male patients.
Patients selected as part of the study were aged 9 to 17 years old, with a median age of 13 years and 4 months.
Male patients were aged 11 to 17 years old, with a median of 14 years and 6 months, whereas female patients were aged 9 to 14 years old, with a median of 11 years.
The present study aimed to highlight the incidence of enchondromas in pediatric patients depending on the location of the tumor.
The location of the lesion can be classified according to the bone affected, the position of the lesion on the bone and its incidence according to the part of the body involved.
The localization of enchondromas can vary from regions of the upper limb, lower limb and on the rib body.
Thus, different results could be observed with regards to lesion localization: 1 case of enchodroma (5.55%) was found the rib cage on the right side, 1 case (5.55%) was found in the right upper limb and, and 16 (88,8%) out of all 18 cases were found in the lower limbs in the regions of left and right tibia, left femur and right ankle, in the talus/astragalus (Figure 1).
Figure 1.

Lesion localization
Lesion localization could be presented as following:
- right humerus-5,55%;
- right rib cage-5,55%;
- right tibia-33,33%;
- left tibia-22,22%;
- left femur-27,77%
- right ankle (talus)-5,55%
Of the total number of patients, 15 had tumor lesions adjacent to the knee joint: 10 patients in the tibia and 5 patients in the femur (Figure 2).
Figure 2.

Lower limb lesion localization
All lesions were in the metaphyseal-diaphyseal region or even at the level of the bone diaphysis, and no patient had lesions located at the level of the growth plate.
Another important aspect regarding tumor localization is the central (intramedullary) or marginal (subperiosteal) position of the tumors in the bone involved, because in the present study, lesions were found both intramedullary and subperiosteal.
Intramedullary positioning was the most common in 14 patients (77,7%) and subperiosteal positioning was identified in only 4 patients (22,2%).
Out of these cases, 13 patients had lesions on the right side of the body (72,2%) and 5 patients had lesions on the left side of the body (27,7%).
The imaging features of enchondromas that this study attempted to highlight are the following: polylobate appearance, sclerotic border, endosteal scalloping, internal calcifications and the presence of bone edema.
All lesions found in this study had the same well-defined polylobate shape, which is one of the pathognomonic features of enchondromas.
This feature could be identified both radiologically and through imaging techniques.
As for the sclerotic border that may accompany the enchondroma, this feature was found only in centrally positioned (intramedullary) lesions, while lesions with a subperiosteal position did not show this aspect.
This accounted for 77.7% of the total (Figure 3).
Figure 3.

Imaging features of the observed enchondromas
One of the most important imaging features of enchondromas is endosteal scalloping.
This feature is present only in lesions with marginal localization, since they tend to bulge at the inner cortical level and can cause cortical thinning, with or without signs of cortical intrusion.
Endosteal scalloping may be associated with bone remodeling or periosteal reaction.
Since only 4 (22,2%) of the 18 patients had a marginal position of the enchondromas, endosteal scalloping phenomena were identified in these patients, but without associative periosteal reactions.
Another important feature of enchondromas are internal calcifications.
In their case, our study could not generate a very clear statistic because the patients did not receive the same radio-imaging examination; some of them performed only X-rays, others only CT or MRI, and some performed two types of examinations when appropriate.
Calcifications are much better detected by CT, but not all patients had this type of evaluation, some of the lesions being identified by chance after MRI examinations for another type of musculoskeletal pathology.
However, we can say that calcifications with a punctate and "popcorn" or "rings and arcs" appearance, which is specific to enchondromas, have been identified.
X-rays and CT scans were conducted on only 12 out of the 18 cases, revealing punctate or "popcorn-like" calcifications in 9 out of these 12 patients.
In patients who underwent only MRI examinations, it was difficult to identify punctate calcifications, but it was possible to identify popcorn-like calcifications, which were coarser and hypo-intense in all the sequences used.
In the patients included in the present study, bone edema that may accompany tumor formation was not very common.
A number of 6 patients who represented 38.8% had bone edema and in one of them the edema extended to the soft tissue (Figure 3).
In regards to the types of examinations conducted in patients suspected with benign osseous lesions, these ranged from conventional X-rays to Computed Tomography and Magnetic Resonance with or without contrast agents.
A total of 22 imaging exams were performed on all 18 patients, presented as following: 6 X-ray exams (27.27%), 7 CT scans (31.81%), with the most frequently conducted being 9 MRI exams (40.90%).
Case Series
The following are a series of the most representative cases of patients who presented with imaging features of enchondroma.
Case 1
Male patient, 17 years old, with a subperiosteal, well-defined enchondroma, located at the metaphyseal-diaphyseal region of the left femur-polylobate appearance, with endosteal scalopping phenomena without any adjacent periosteal reaction.
Minimal bone edema was present, the lesion structure was heterogeneous with the presence of "popcorn" type calcifications on the inside, but without any sclerotic margin.
Postcontrast sequence showed a pattern of ‘’ring and arcs’’ of contrast agent uptake (Figure 4).
Figure 4.

A-Coronal PD FS, B-Axial PD sequence, C-Coronal T1+C sequence sequence.
Case 2
Female patient, 16 years old, with an enchondroma located in the diaphyseal region of the right tibia, centrally positioned (intramedullary).
The enchondroma had a polylobate shape, well defined, with hypodense sclerotic margin in all sequence used, heterogeneous structure due to well-represented popcorn-type calcifications, hypointense in all sequence used.
No endosteal scalloping phenomena or presence of peritumoral bone edema were noted.
Instead, bone edema at the tibial plateau and minimal joint fluid were noted, with the patient experiencing pain in the knee joint, the enchondroma being diagnosed incidentally (Figure 5).
Figure 5.
A Coronal PD, BSagittal STIR
Case 3
Male patient, 17 years old, with benign, subperiosteal cartilaginous tumor located at the level of the anterior arch of rib no. 4 on the left side.
We could observe an enchondroma with polylobate appearance and endosteal scalloping phenomena without any cortical lysis adjacent to the tumor or any evidence of calcifications inside.
In such a case, CT examination is the imaging standard for the study of calcifications in a tumor lesion (Figure 6).
Figure 6.

The axial (A,B) and sagittal (C) planes bone reconstruction CT
Case 4
A 15-year-old male patient presented for right ankle pain and had CT examination of the right ankle joint.
The CT examination revealed the presence of an osteolytic lesion at the level of the talus, well defined, with osteosclerotic margin and calcifications inside-microcalcifications and "popcorn" type calcifications.
The CT examination was completed with contrast agent which showed minimal uptake (Figure 7).
Figure 7.

CT scan with bone reconstruction in sagittal (A) and axial (B, C); pre-contrast (B) axial sections and in post-contrast ones (C).
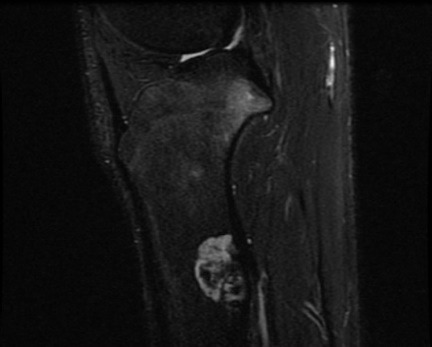
Due to the persistent painful symptoms, the patient underwent MRI examination, which revealed a cartilaginous tumor lesion at the level of the talus, with a polylobate shape, well defined, with sclerotic margin and "popcorn"-type calcifications in the hypointense area in all the sequences used.
These imaging features correlated with those of the CT investigation.
In addition to this, the MRI exam identified associative bone edema, including soft tissue edema.
Soft tissue edema can be generated by both tumor lesions and extensive tendon-ligamentous lesions (Figure 8).
Figure 8.

Sagittal T1 (A), Sagittal PD (B) and Coronal STIR (C).
Case 5
Male patient, 8 years old, with a recent post-traumatic episode, for whom X-rays of the left lower limb were taken.
The radiological examination did not reveal any post-traumatic fracture lesions, but instead showed a well-defined osteolytic lesion, polylobate, with sclerotic margins and coarse calcifications on the inside.
The enchondroma was located intramedullary, in the region of the left tibial diaphysis (Figure 9).
Figure 9.

X-ray exam of the lower limb
Discussions
Bone tumors in pediatric patients are relatively rare, with a higher frequency of benign bone tumours than malignant ones.
Enchondroma is a benign cartilaginous tumor and is the second most common benign cartilaginous bone tumor in childhood after osteochondroma, accounting for up to 24% of all benign bone tumors found in children or adolescents [8].
In the present study the incidence of enchondromas reported by sex was higher among male patients, a different ratio compared to that found in the study by Matysiakiewicz J et al. [9].
Around 25% of enchondromas are found in pediatric patients, most in the 2nd life decade.
Regarding the age of the selected patients, they ranged between 9 and 17 years, a slightly higher age range compared to the patients studied by Saiji E et al. where the patients were aged between 4 and 18 years [10].
The localization incidence of enchondroma in the patients included in the present study was found to be high in the long bones (especially in the tibia and femur), with only one patient having a tumor lesion in the small bones of the lower limb, in the talus, results similar to those of Davies et al.
Previously, it was assumed that enchondromas were most commonly located in the short tubular bones of the hands and feet. However, Davies et al. found an incidence in these regions of 0.07% on conventional radiographs, whereas the incidence of enchondromas in MRI examinations of the shoulder and knee was approximately 2.5-2.9%, and their occurrence on conventional radiographs was between 17-77% [11].
According to Jeffe’s hypothesis, cartilaginous embryo cells deriving from the epiphyseal growth plate move to the metaphysis during growth and development and can be linked to the potential occurrence of enchondromas.
This hypothesis has not been confirmed, and recent molecular studies have highlighted a link between the development of enchondromas and mutations to IDH1 and IDH2 genes [2].
However, the tumor lesions found in the patients included in our study were located in the metaphyseal-diaphyseal or diaphyseal regions of the short bones, with no lesions found in the growth plates.
This was also pointed out by Edgel, who noted that the location of enchondromas in short tubular bones is usually diaphyseal, while the location in long tubular bones is usually metadiaphyseal, rarely epiphyseal, and they are usually located in the center of the medullary cavity of the tubular bones [11].
Intramedullary (central) localization being a majority in our patients, 14 of them presented with central tumor lesions.
Apart from singular lesions, enchondromas can also be found in multiple forms in the Ollier syndrome or multiple enchondromatosis, in which numerous cartilaginous lesions are located in the metaphyseal and diaphyseal regions [5].
Ollier syndrome has first been described in 1900 and is a rare syndrome, with a non-familial characteristic, with mutations in IDH1 and IDH2 genes.
This pathology is characterized by the presence of numerous enchondromas and areas of cartilaginous dysplasia, located primarily in long bones such as tibia, femur and fibula, but these lesions can also be found in flat bones such as those of the base of the cranium and the pelvic skeleton [12, 13].
Multiple enchondromatosis can be associated with cutaneous hemangiomas, and in this case the pathology is called the Maffucci Syndrome [14].
Differentiating between these two syndromes is important, because Maffucci Syndrome has a higher potential of malignant transformation of enchondromas in comparison to Ollier Syndrome [11, 14].
In the present study, no multiple enchodromatosis cases were discovered and that is because no genetic tests were run to determine possible mutations on genes IDH1 and IDH2, and, besides this, no “total body” CT or MRI exams were conducted, which could have potentially detected other lesions in different regions.
The imaging aspects of enchondromas are dependent on their localization. Enchondromas found in short bones such as the bones of the hand or the feet have a classic, osteolytic, expansile aspect, which results in a thinned cortical bone that is associated with punctate areas of chondroid calcifications.
Most of these lesions are accidentally discovered, many times due to fractures in the affected bones [15].
Radiographically visible calcifications appear as fine, punctate dots and, if larger in size, these may suggest a bone infarction.
Calcifications can range in size from punctate to rings. Depending on the size of the lesion, the lesion may be mistaken for a bone infarction or bone islands [16].
In long bones, lesions are typically intramedullary and present with multiple chondroid calcifications, which give the image a “popcorn” or “rings and arcs” aspect, having sclerotic margins or subjacent osteolysis.
Some lesions can be completely calcified, while other lesions that are bigger in volume can determine cortical scalloping with small areas of calcification that are disseminated in the interior of the lesion [15].
Some imaging aspects described in literature could also be found in patients included in the present study.
These were mainly represented by chondroid calcifications, with a so-called “popcorn” aspect located inside the lesion, or in the adjacent area, which in MRI exams were in low signal intensity in every sequence used.
Calcifications within the lesions were present in 9 of the 13 cases that underwent radiological/CT examinations.
Matrix mineralization was emphasized in only 20% of the cases included in the study conducted by Bierry G. et al.
CT scans show the same imaging aspects as conventional X-rays, but show the calcifications inside the tumor matrix in a far superior resolution and also help better quantify the endosteal scalloping [8].
CT exams have replaced conventional X-rays where we need to identify mineralization areas, thickening of the bone cortex and the presence of fracture paths that cannot be visualized through conventional radiology [17].
One of the phenomena that enchondroma lesions can determine is cortical scalloping. CT exams are the primary imaging techniques for the study of bone cortex and are especially useful in determining the grade of endosteal scalloping, which is defined as a local, focal loss of inner cortical bone, irrespective of the extension of the lesion.
In the case of our patients, only 4 of them presented endosteal scalloping phenomena, the location of the lesions being marginal, adjacent to the cortical bone.
However, in the study conducted by Bierry G. et al. endosteal scalloping was present in 75% of the patients (9 out of 12), but it should be mentioned that the majority of endosteal scalloping lesions were found in the phalanges-7 patients and only 2 lesions were in the femur.
Most patients examined through conventional X-ray and Computed Tomography exams have also been examined with the help of MRI exams in order to identify a potential osseous edema or an extension of the lesion in the surrounding soft tissues in the case of sub-periosteal lesions.
This is why the percentage of MRI exams conducted on patients included in this study was at 40.9%.
MRI exams help identify a polylobate mass, with intermediary T1 signal and a more intense signal in T2 sequence, which is due to the high content of water in the hyaline cartilage, whereas chondroid calcifications present with a reduced intensity signal in T1 and T2-weighted images.
In T1 sequences, the fatty component in the bone marrow can be seen in between the cartilaginous lobulations of long bone enchondromas [15].
A polylobate growth pattern of cartilaginous bone tumors is a well-known feature of these tumors, with a septal vascular structure, which explains their contrast uptake in the form of “rings and arcs” of both enchondromas and chondrosarcomas [18].
In the case of chondrosarcomas, two other types of enhancement patterns have been shown to be more commonly present in chondrosarcomas.
Besides contrast-enhanced MRI, diffusion-weighted imaging is another functional sequence used in diagnostic imaging; however, it does not help to distinguish or classify cartilage tumors [19].
With regards to osseous infarctions located in long bones, these can resemble enchondroma lesions without any endosteal scalloping, although a characteristic aspect of these lesions is the presence of peripheral serpiginous calcifications [15].
Another imaging feature that may be present in bone tumors is peritumoral edema.
The vast majority of enchondromas are not accompanied by bone edema, unlike chondrosarcomas. Janzen et al. conducted a study of 23 patients, (10 enchondromas and 13 chondrosarcomas) and reported no peritumoral bone marrow edema around the enchondromas, but peritumoral edema was seen in the 13 chondrosarcomas present in their study [20].
In the case of our patients, 38.8% of them had bone oedema, but in some cases, it could also be generated by associative musculoskeletal lesions.
Another characteristic of these lesions is the increased uptake of 99Tc-methylene diphosphonate (MDP), but this should not be used as an indicator for potential malignant transformations.
The radiological aspects that do indicate a malignant transformation can refer either to lesions that alter their characteristics in time, with an increase in osteolysis areas and resorption of internal calcifications, or to lesions that present with discontinuity in the bone cortex and invasions in the adjacent soft tissues [14, 15].
Studies from authors like Saifuddin et al. and Yoshimura et al. have emphasized the role and the efficiency of MRI examinations in differentiating atypical cartilaginous tumors and high-grade chondrosarcomas.
MRI exams have a high sensitivity in identifying the fatty component, the “ring and arc” enhancement and the characteristics of the adjacent soft tissue lesions, with an accuracy of approximately 92% and a sensitivity of 91% prior to biopsy.
Despite all of this, many authors have highlighted the importance of Computed Tomography and conventional X-rays in detecting calcifications, scalloping and cortical invasion, these types of imaging techniques being more sensitive in detecting these lesion characteristics in comparison to MRI exams [20].
For example, Murphey et al, retrospectively analyzed the MRI characteristics of enchondromas and chondrosarcomas of the appendicular skeleton [21].
They assessed lesion size, endosteal scalloping size, cortical remodeling, cortical destruction, pathological fracture, periosteal reaction, cortical thickening, and soft tissue extension [21].
It was found that the mean length of the enchondromas was 5cm, while the mean length of the chondrosarcomas was 8cm.
Similarly, endosteal scalloping depth and extension was significantly different in enchondromas and chondrosarcomas, being present in more than two-thirds of the lesion length and being observed in 67% of chondrosarcomas and 11% of enchondromas [22].
Douis et al. found that symptoms such as pain generated by the lesion and features such as tumor length, endosteal scalloping, bone expansion, cortical destruction, and soft tissue mass could distinguish enchondromas from low-grade chondrosarcomas, whereas dynamic contrast MRI was not useful in differentiating enchondromas from low-grade chondrosarcomas [22].
Another study such as the one conducted by Deng X.Y. et al. found that sex, calcified shape and endosteal scalloping were independent predictors of the differentiation of benign and malignant cartilaginous tumors.
Enchondromas always show popcorn and ring-shaped calcifications, indicating mature differentiation of the cartilaginous matrix [23].
The rate of malignant transformation of a solitary enchondroma into a secondary central chondrosarcoma is currently unknown, but it was estimated at around 4.2%.
In patients presenting multiple enchondromatosis, the rate of malignant transformation is around 40%, but these patients are generally 10 to 15 years younger in comparison to those patients that develop primary chondrosarcomas [13, 24, 25].
Conclusions
In the present study we have highlighted the incidence of benign tumors with cartilaginous matrix (enchondroma) according to sex, age and location.
As for the localization, it was studied on three levels: incidence in the bone, position of the lesions in the bone and the part of the body that is more affected.
The main radio-imaging aspects of this type of lesion were highlighted in the present study, some being present in all lesions, such as the polylobate aspect, others being present to a greater extent depending on the location of the lesion in the affected bone, such as sclerotic border and endosteal scalloping.
Others were present to a lesser extent. As far as bone edema is concerned, this is a more common feature in chondrosarcomas.
The patients included in the study who were found to have bone edema also had tendon-ligamentous changes in addition to the tumor following posttraumatic episodes, so bone edema could be due to both tumor lesion or posttraumatic changes.
Therefore, a radio-imaging follow-up of enchondromas is necessary to highlight possible changes in the tumor and the appearance of adjacent aggressive characters.
Conventional X-ray examinations generally help discover the lesions usually by accident, and in these cases the radiological and clinical characteristics were clear and indicated the diagnosis of enchondroma.
In other cases, conventional radiology was supplemented with MRI exams in order to help determine the cartilaginous component of the lesion and investigate the way it affected adjacent osseous, muscular or tendinous and ligament structures.
Nevertheless, CT scans with and without contrast agent were used to better evaluate the different alterations to the bone structure, from osteolysis to osteocondenstation, including the evaluation of the calcification patterns in the interior of the tumor.
Furthermore, with regards to the assessment of the cortical bone, CT scans presented with a superior accuracy in comparison to the accuracy of MRI exams.
Conflict of interests
None to declare.
Source of funding
This work was supported by the grant POCU/993/6/13/153178, “Performanță în cercetare”-“Research performance” co-financed by the European Social Fund within the Sectorial Operational Program Human Capital 2014-2020.
References
- 1.Akoh CC, Craig E, Troester AM, Miller BJ. Radiographic Enchondroma Surveillance: Assessing Clinical Outcomes and Costs Effectiveness. Iowa Orthop J. 2019;39(1):185–193. [PMC free article] [PubMed] [Google Scholar]
- 2.Bierry G, Kerr DA, Nielsen GP, Rosenberg AE, Huang AJ, Torriani M, Bredella MA. Enchondromas in children: imaging appearance with pathological correlation. Skeletal Radiol. 2012;41(10):1223–1229. doi: 10.1007/s00256-012-1377-6. [DOI] [PubMed] [Google Scholar]
- 3.Walden MJ, Murphey MD, Vidal JA. Incidental enchondromas of the knee. AJR Am J Roentgenol. 2008;190(6):1611–1615. doi: 10.2214/AJR.07.2796. [DOI] [PubMed] [Google Scholar]
- 4.Dumitriu DI, Menten R, Clapuyt P. Pitfalls in the diagnosis of common benign bone tumours in children. Insights Imaging. 2014;5(6):645–655. doi: 10.1007/s13244-014-0356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davies AM, Patel A, Azzopardi C, James SL, Botchu R. Prevalence of Enchondromas of the Proximal Femur in Adults as an Incidental Finding on MRI of the Pelvis. Indian J Radiol Imaging. 2021;31(3):582–585. doi: 10.1055/s-0041-1735915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerr DA, Cipriani NA. Benign Cartilage-forming Tumors. Surg Pathol Clin. 2021;14(4):585–603. doi: 10.1016/j.path.2021.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Lam Y. Bone Tumors: Benign Bone Tumors. FP Essent. 2020;493:11–21. [PubMed] [Google Scholar]
- 8.van den, Slaar A, Kroon HM, Taminiau AH, Hogendoorn P. Results of diagnostic review in pediatric bone tumors and tumorlike lesions. J Pediatr Orthop. 2008;28(5):561–564. doi: 10.1097/BPO.0b013e31817bb800. [DOI] [PubMed] [Google Scholar]
- 9.Matysiakiewicz J, Tomasik P, Miszczyk L, Spindel J, Widuchowski J, Koczy B, Chrobok A, Mrozek T. Manifestations, diagnosis and surgical treatment of enchondroma--own experience. Ortop Traumatol Rehabil. 2010;12(2):155–159. [PubMed] [Google Scholar]
- 10.Saiji E, Pause FG, Lascombes P, Cerato Biderbost, Marq NL, Berczy M, Merlini L, Rougemont AL. IDH1 immunohistochemistry reactivity and mosaic IDH1 or IDH2 somatic mutations in pediatric sporadic enchondroma and enchondromatosis. Virchows Arch. 2019;475(5):625–636. doi: 10.1007/s00428-019-02606-9. [DOI] [PubMed] [Google Scholar]
- 11.Mellon CD, Carter JE, Owen DB. Ollier's disease and Maffucci's syndrome: distinct entities or a continuum. Case report: enchondromatosis complicated by an intracranial glioma. J Neurol. 1988;235(6):376–378. doi: 10.1007/BF00314239. [DOI] [PubMed] [Google Scholar]
- 12.D'Angelo L, Massimi L, Narducci A, Di Rocco. Ollier disease. Childs Nerv Syst. 2009;25(6):647–653. doi: 10.1007/s00381-009-0873-z. [DOI] [PubMed] [Google Scholar]
- 13.Sharif B, Lindsay D, Saifuddin A. Update on the imaging features of the enchondromatosis syndromes. Skeletal Radiol. 2022;51(4):747–762. doi: 10.1007/s00256-021-03870-0. [DOI] [PubMed] [Google Scholar]
- 14.El Abiad, Robbins SM, Cohen B, Levin AS, Valle DL, Morris CD, de Macena. Natural history of Ollier disease and Maffucci syndrome: Patient survey and review of clinical literature. Am J Med Genet A. 2020;182(5):1093–1103. doi: 10.1002/ajmg.a.61530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Na K , Park YK . In: Tumors and tumor-like lesions of bone . Santini-Araujo E , Kalil RK , Bertoni F , Park YK , et al., editors. Switzerland : Springer ; 2020 . Cartilage-forming tumors ; pp. 25 – 108 . [Google Scholar]
- 16.Enchondroma. 2023 Available from: https://www.ncbi.nlm.nih.gov/books/NBK536938/
- 17.Afonso PD, Isaac A, Villagrán JM. Chondroid Tumors as Incidental Findings and Differential Diagnosis between Enchondromas and Low-grade Chondrosarcomas. Semin Musculoskelet Radiol. 2019;23(1):3–18. doi: 10.1055/s-0038-1675550. [DOI] [PubMed] [Google Scholar]
- 18.Deng XY, Chen HY, Yu JN, Zhu XL, Chen JY, Shao GL, Yu RS. Diagnostic Value of CT-and MRI-Based Texture Analysis and Imaging Findings for Grading Cartilaginous Tumors in Long Bones. Front Oncol. 2021;11:700204–700204. doi: 10.3389/fonc.2021.700204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mulligan ME. How to Diagnose Enchondroma, Bone Infarct, and Chondrosarcoma. Curr Probl Diagn Radiol. 2019;48(3):262–273. doi: 10.1067/j.cpradiol.2018.04.002. [DOI] [PubMed] [Google Scholar]
- 20.Aoki J, Sone S, Fujioka F, Terayama K, Ishii K, Karakida O, Imai S, Sakai F, Imai Y. MR of enchondroma and chondrosarcoma: rings and arcs of Gd-DTPA enhancement. J Comput Assist Tomogr. 1991;15(6):1011–1106. doi: 10.1097/00004728-199111000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Douis H, Parry M, Vaiyapuri S, Davies AM. What are the differentiating clinical and MRI-features of enchondromas from low-grade chondrosarcomas. Eur Radiol. 2018;28(1):398–409. doi: 10.1007/s00330-017-4947-0. [DOI] [PubMed] [Google Scholar]
- 22.Alhumaid SM, Alharbi A, Aljubair H. Magnetic Resonance Imaging Role in the Differentiation Between Atypical Cartilaginous Tumors and High-Grade Chondrosarcoma: An Updated Systematic Review. Cureus. 2020;12(10):e11237–e11237. doi: 10.7759/cureus.11237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deng XY, Chen HY, Yu JN, Zhu XL, Chen JY, Shao GL, Yu RS. Diagnostic Value of CT- and MRI-Based Texture Analysis and Imaging Findings for Grading Cartilaginous Tumors in Long Bones. Front Oncol. 2021;11:700204–700204. doi: 10.3389/fonc.2021.700204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Müller PE, Dürr HR, Nerlich A, Pellengahr C, Maier M, Jansson V. Malignant transformation of a benign enchondroma of the hand to secondary chondrosarcoma with isolated pulmonary metastasis. Acta Chir Belg. 2004;104(3):341–344. doi: 10.1080/00015458.2004.11679569. [DOI] [PubMed] [Google Scholar]
- 25.Nelson DL, Abdul-Karim FW, Carter JR, Makley JT. Chondrosarcoma of small bones of the hand arising from enchondroma. J Hand Surg Am. 1990;15(4):655–659. doi: 10.1016/s0363-5023(09)90032-6. [DOI] [PubMed] [Google Scholar]


