Abstract
The transient ischemic attack (TIA) is a common cerebrovascular ischemic disease whose symptoms resolve within a maximum of 24 hours. The study carried out by us is a retrospective descriptive one, in which we sought to highlight the main characteristics of TIA in patients admitted to the Emergency Hospital in Turnu-Severin municipality in Mehedinți county, in the period 2016-2020, including a group of 53 patients, mainly from Mehedinți county. The analysis of the study group and the risk factors showed that TIA mainly affects the elderly, over 50 years old, with the highest incidence being recorded in the 60-80-year age groups, with an extremely low incidence under 40 years. Significant differences were found between the sexes and between the social environments, with women and people from the urban environment being more prone to suffer a TIA. Among the most important modifiable risk factors encountered in TIA patients included in the study, the following were highlighted: HTN, obesity and atherosclerosis. Knowing the modifiable factors and combating them can improve the prognosis of AIT.
Keywords: Transient ischemic accidents , cerebral ischemia , modifiable and non-modifiable risk factors
Introduction
The transient ischemic attack (TIA) is a common cerebrovascular ischemic disease [1] whose symptoms are relieved in a maximum of 24 hours [2].
The American Heart Association/American Stroke Association in 2009 defined TIA as a transient episode of neurological dysfunction determined by acute cerebral, spinal or retinal ischemia, without the appearance of the infarction [5].
Patients with TIA present a high risk for the subsequent development of an ischemic vascular accident [3,5].
TIA represents a major public health problem worldwide, as it affects a large number of people [5] and creates high costs for diagnosis, treatment and subsequent evaluations [4].
Among the modifiable risk factors in the literature are mentioned: hypertension, smoking, obesity, diabetes, cardiovascular diseases, atrial fibrillation, hypercholesterolemia, unhealthy diet and lack of physical activity [6, 7, 8, 18].
As unmodifiable risk factors we note: age over 55 years, gender, family history, genetic profile and ethnicity [9, 10, 18].
AIM
Starting from data published in the last 10-15 years, in the present study we proposed an analysis of TIA cases admitted to the Emergency Hospital in Drobeta Turnu-Severin municipality in Mehedinți county, in the period 2016-2020, in order to highlight the particularities of these patients compared to other studies.
Materials and Methods
The study conducted by us is a retrospective descriptive one, in which we aimed to highlight the main characteristics of transient ischemic attack (TIA) in patients, namely the modifiable and non-modifiable risk factors, and compare our results with others reported in the literature in order to observe notable differences.
The study included a total of 53 patients, mainly from Mehedinți County, but also from neighbouring counties (Gorj, Caraș-Severin) admitted to the Emergency Hospital in Turnu Severin, Mehedinți County, during the period 2016-2020.
All clinical data (age, gender, social environment, medical history, symptoms, comorbidities) and paraclinical were extracted from the patients' clinical observation sheets and medical records, and was organized into the "Microsoft Excel" program as a data base for further processing in the form of graphs or charts, for a more accurate and efficient interpretation.
Prior approval from the manager of the Emergency Hospital in Drobeta Turnu Severin, the hospital's Ethics Committee and every patient was obtained for the extraction and processing of data from the medical documents.
Patient’s data was collected using Excel (Microsoft, USA), ensuring patient anonymization upon insertion.
Data exploration was carried out using the built-in chart options.
An age histogram was created using the Data>Data analysis>Histogram function, with bins of 10 starting at the age of 40 (years).
For the histogram, a column chart representation was used, while for the other variables-pie charts.
The comprehensive dataset employed in this study encompasses a compilation of information such as demographic characteristics and parameters related to comorbidities, collected for the entire cohort of patients included in the study.
The recorded variables span a wide spectrum encompassing age group categorizations, gender distribution, socio-economic background, the presence or absence of hypertension, obesity, atherosclerosis, diabetes mellitus, atrial fibrillation, metabolic diseases and renal failure.
Also, data related to the presence or absence of anxiety syndrome was collected.
Results
Analysis of the group of patients with TIA (Transient Ischemic Attack), who required hospitalization in the Neurology Department of the Emergency Hospital in Turnu Severin, showed that the disease predominantly affects elderly individuals, with a very low incidence in young people under the age of 50 (Figure 1).
Figure 1.
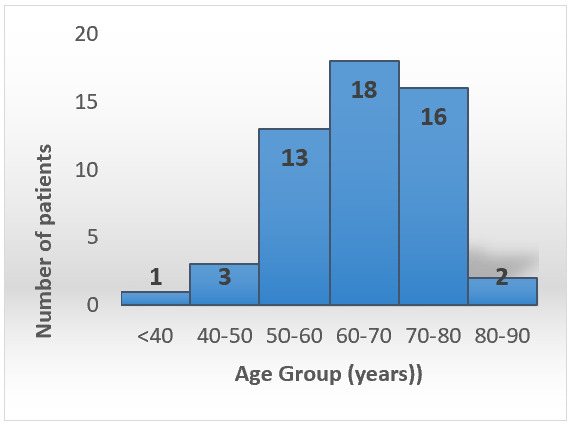
Distribution of TIA patients according to age groups.
The majority of patients (49 individuals, i.e., 92.45%) with TIA were over 50 years old.
Our study observed how the incidence of TIA increased with advancing age.
The highest number of stroke cases were recorded in the age groups of 60-80 years (18 individuals, i.e., 33.96%).
The reduction in TIA incidence after the age of 80 is attributed to the decrease in the elderly population due to deaths caused by other conditions.
Regarding the gender of individuals affected by TIA, our study indicated a slight predominance of females (30 females, i.e., 57%) compared to males (23 males, i.e., 43%) (Figure 2).
Figure 2.
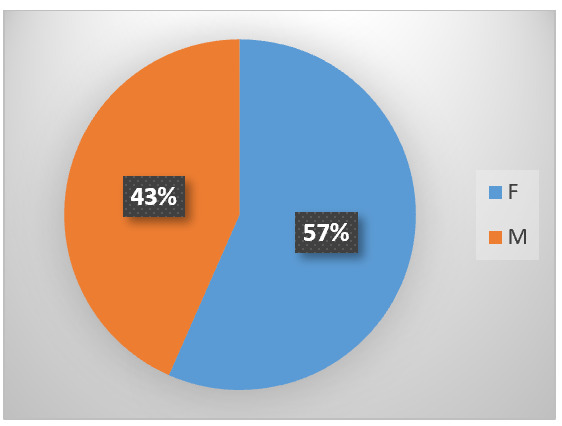
Distribution of TIA based on sex (F=females; M=males).
Concerning the social environment of TIA patients, it was found that the disease affects nearly three times more people in urban areas compared to rural areas.
In our study, 39 cases of TIA (74%) originated from urban areas, and 14 cases (26%) from rural areas (Figure 3).
Figure 3.
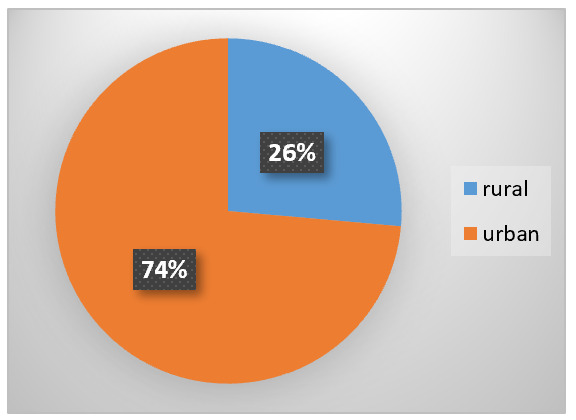
Distribution of stroke cases according to the social environment
These data suggest that the risk factors for TIA are predominantly found in urban settings
The analysis of risk factors involved in the etiopathogenesis of TIA revealed that cardiovascular diseases, especially hypertension, rank first.
Out of the 53 patients included in the studied group, 40 (75%) presented with elevated blood pressure (Figure 4).
Figure 4.
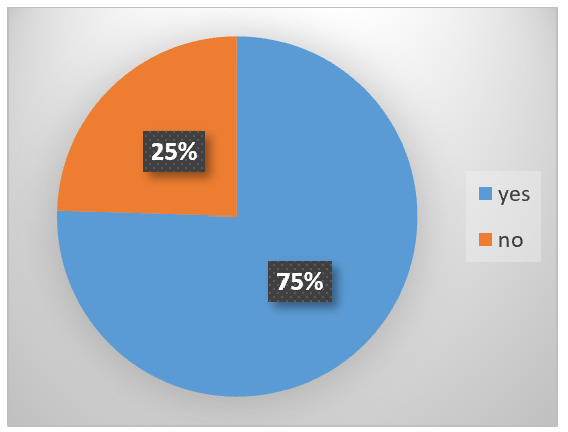
Association between TIA and Hypertension
The data obtained confirm the strong relationship between TIA and cardiovascular diseases, with hypertension being the most significant modifiable risk factor for all types of strokes.
Obesity represents another major risk factor for TIA, as it is associated with dyslipidemia, hypercholesterolemia, coagulation disorders, etc.
In our study, 33 patients (62%) with TIA were also diagnosed with obesity (Figure 5).
Figure 5.
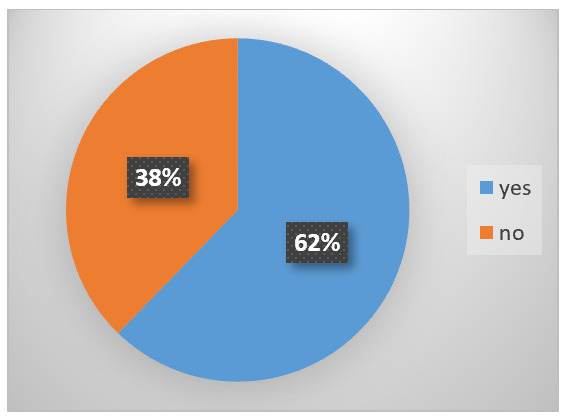
Association between TIA and Obesity
Atherosclerosis, through the remodelling of cerebral blood vessel walls, is another major factor contributing to TIA alongside hypertension.
In our study, 46 patients (87%) with TIA were also diagnosed with atherosclerosis(Figure 6).
Figure 6.
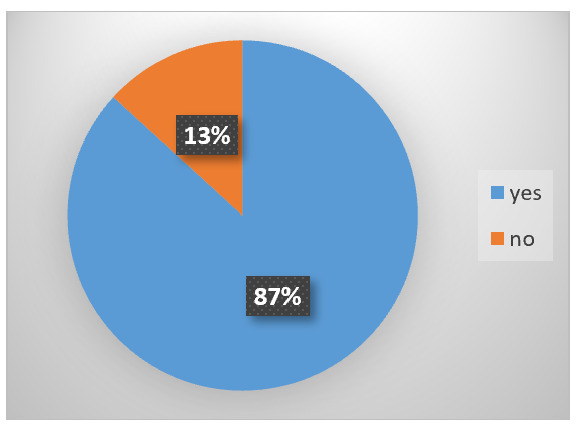
Association between TIA and Atherosclerosis
Diabetes mellitus is a well-known risk factor for neurovascular disease. In our study, only 10 patients (19%) presented with diabetes mellitus (Figure 7).
Figure 7.
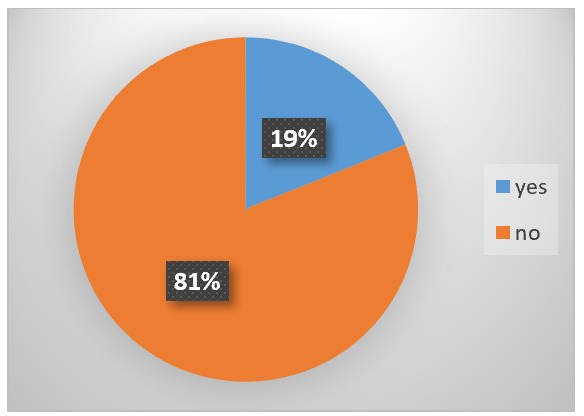
Association between TIA and Diabetes Mellitus
Renal failure was another comorbidity investigated in our study.
The analyzed medical records showed that only 1 patient with TIA (2%) had renal failure (Figure 8).
Figure 8.
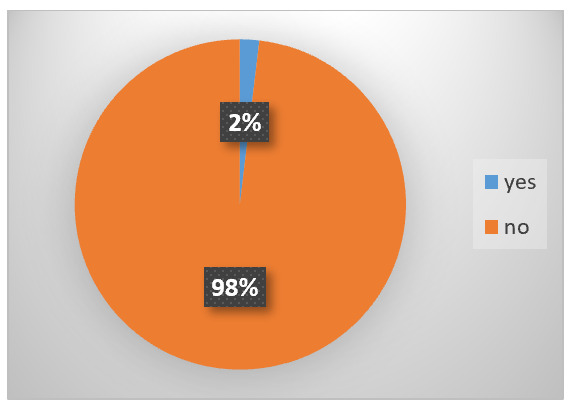
Association between TIA and Renal Failure
Atrial fibrillation was observed in 4 patients (8%) within the scope of the study (Figure 9).
Figure 9.
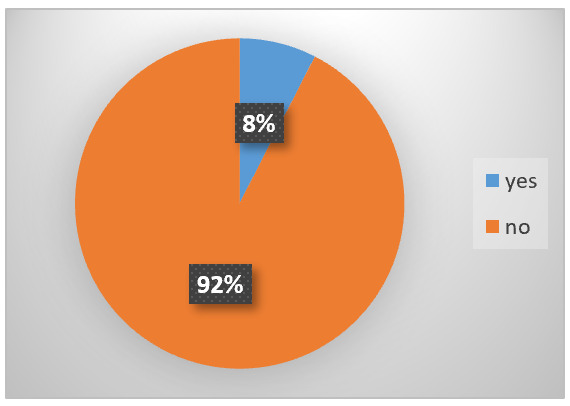
Association between TIA and Atrial Fibrillation
Metabolic diseases represented another important risk factor for the occurrence of TIA, in our study at 50 patients (94%) we found this factor (Figure 10).
Figure 10.
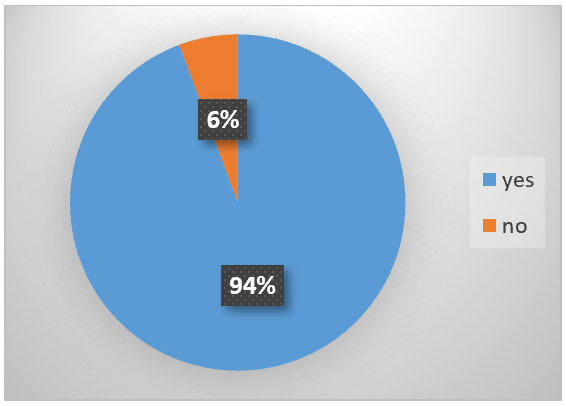
Association of AIT with metabolic diseases
A particular thing found in most patients with TIA (48 patients-91%) was an anxious syndrome, most likely appearing after the onset of the first symptoms (Figure 11).
Figure 11.
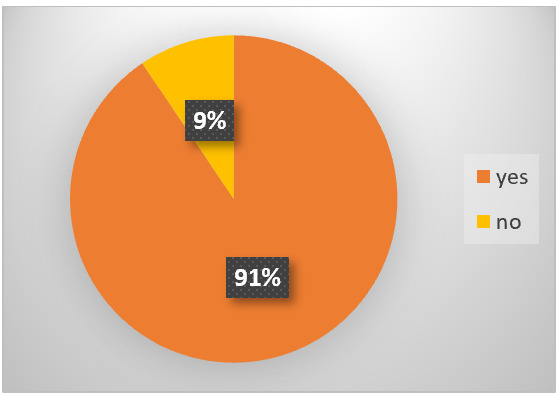
. The association of AIT with the anxious syndrome
Discussions
The transient ischemic attack is becoming a major global public health problem due to the aging of the population.
The data obtained in our study confirmed that advanced age is a risk factor, most patients with TIA (92.45%) being over 50 years old, with a preponderance among women (57%)
Most patients with TIA (33.96%) were registered in the age decades of 60-70-80 years.
The data available from the specialized literature confirm our results, the highest reported incidence being in people over 55 years old, increasing with age [9, 10, 11, 12], and it is more frequent among women [12].
The cause of the increase in the incidence of AIT is urbanization and lifestyle changes, including diet, a fact confirmed both in our study and by others [9, 10, 13].
An unhealthy diet is a major risk factor for several chronic diseases including high blood pressure, high cholesterol, diabetes, abnormal blood lipids, overweight/obesity, cardiovascular diseases, and cancer [14].
The World Health Organization has estimated that 2.7 million deaths each year are attributable to a diet low in fruit and vegetables during the 21st century [15].
Globally, unhealthy diets are estimated to cause about 19% of gastrointestinal cancer, 31% of ischemic heart disease, and 11% of strokes, thus making it one of the leading preventable causes of death worldwide, and the 4th leading risk factor for any disease [15, 16, 17].
As an example, the Western pattern diet is "rich in red meat, dairy products, processed and artificially sweetened foods, and salt, with minimal intake of fruits, vegetables, fish, legumes, and whole grains," contrasted by the Mediterranean diet which is associated with less morbidity and mortality [18].
Reducing the incidence of TIA can be achieved by addressing modifiable risk factors.
In this sense, preventing and treating hypertension (HTN), atrial fibrillation, diabetes, dyslipidaemia, combating smoking and excessive alcohol consumption, combating obesity, changing dietary habits, encouraging physical activity, could contribute to reducing the incidence of TIA [6, 7, 8, 19, 20].
In our study, the most common comorbidity associated with TIA was hypertension.
Thus, 75% of TIA patients had elevated blood pressure values. Several studies have demonstrated the correlation between hypertension and TIA [6, 21].
The second modifiable risk factor we identified in TIA patients was obesity.
Thus, 62% of all patients in the study group with TIA presented obesity of various degrees and hypercholesterolemia, an association that was found in several specialized studies [6, 20, 2, 23, 24].
Another modifiable risk factor highlighted in our study was diabetes.
Only 19% of the patients included in the study group had diabetes, something confirmed by other authors [6].
Diabetes mellitus increases the risk of ischemic stroke 1.5-3.7 times and may account for at least 8% of first ischemic strokes [24].
As we mentioned, many risk factors are involved in the etiopathogenesis of AIT, some modifiable, others not.
Knowing the modifiable factors, and combating them, can improve the prognosis of AIT.
Among the modifiable risk factors, the most important in terms of morbidity is HTN [4].
Patients with hypertension have an increased risk of stroke, and blood pressure control reduces this risk [6].
Blood pressure control after TIA is associated with a greater decrease in stroke risk [6].
The risk of a vascular accident increases proportionally with the increase in systolic blood pressure above 160mmHg or diastolic blood pressure above 95mmHg [25].
Even the smallest adjustment in hypertension control can reduce vascular events significantly [25].
Clinical studies have shown that a decrease in arterial pressure by 5-6 mmHg leads to a decrease in the risk of vascular events by 42% [26].
Diet and lifestyle changes that can reduce blood pressure are: decreasing sodium intake, weight loss, a diet rich in vegetables, fruits and low-fat products, moderate alcohol consumption and regular physical activity [27].
When these changes are not sufficient, it is necessary to resort to antihypertensive medication.
Variable blood pressure readings in a patient with hypertension may be an important predictor of cerebral ischemia, as well as the effects of antihypertensive agents [6].
In a cohort of patients with TIA, increased visit-to-visit variability of systolic blood pressure and maximum systolic blood pressure reached were strong predictors of subsequent stroke (hazard ratios were 6.22 and 15.01, respectively).
Calcium channel blockers have been shown to reduce this variability, thus lowering the risk of stroke [6].
Another risk factor that increases blood pressure and precipitates atherosclerosis is smoking.
Several studies have demonstrated that smoking increases the incidence of acute vascular events two to four times [28, 29].
Quitting smoking is recommended both for people with a history of TIA and for healthy people, the most efficient way being triple therapy: social support, nicotine replacement therapy and behavioral therapy [30].
Diabetes mellitus is associated with the occurrence of atherosclerosis, hypertension, obesity, hypercholesterolemia and vascular accidents [31, 32].
Patients with newly diagnosed diabetes have double the rate of stroke compared with the general population [6].
Studies have shown that strict control of serum glucose levels is not associated with a decrease in the risk of vascular accidents, but hypertension control associated with control of serum glucose levels has been shown to reduce the risk of vascular accidents [32, 33, 34].
Obesity (defined as a body mass index of 30kg per m2 or more) is associated with a greater risk of death [6].
More than one in four persons will become clinically obese, and increased waist-to-hip ratio increases the risk of stroke [6].
Obesity has individual, socioeconomic, and environmental causes.
Some known causes are diet, physical activity, automation, urbanization, genetic susceptibility, medications, mental disorders, economic policies, endocrine disorders, and exposure to endocrine-disrupting chemicals [35, 36].
Hypercholesterolemia is the presence of high levels of cholesterol in the blood [37].
Elevated levels of non-HDL cholesterol and LDL in the blood may be a consequence of diet, obesity, inherited (genetic) diseases (such as LDL receptor mutations in familial hypercholesterolemia), or the presence of other diseases such as type 2 diabetes and an underactive thyroid, diet, and stress [37].
Dyslipidaemia is a significant risk factor for ischemic stroke (OR=1.89).
A large prospective cohort study showed a strong association between serum cholesterol levels and cerebral ischemia, with risk increasing proportionally to serum levels [6].
A large meta-analysis studying the effect of statins on stroke reduction showed that the larger the reduction in low-density lipoprotein cholesterol levels, the greater the reduction in stroke risk [6].
Atherosclerosis is characterized by development of abnormalities called lesions in walls of arteries.
The exact cause of atherosclerosis is unknown and is proposed to be multifactorial.
Risk factors include abnormal cholesterol levels, elevated levels of inflammatory biomarkers, high blood pressure, diabetes, smoking (both active and passive smoking), obesity, genetic factors, family history, lifestyle habits, and an unhealthy diet [38].
Atherosclerosis and destabilization of atheromatous plaque are well-documented mechanisms for ischemic stroke and TIA [4].
Atherosclerosis is a frequent complication of diabetes and a cause for carotid artery stenosis.
The recently emerging understanding of atherosclerosis as an inflammatory disease has contributed significantly to the cast of possible players in stroke generation [4].
Thus, a balanced diet associated with the medication corresponding to the underlying diseases, where necessary, and the measures mentioned above can lead to a decrease in the incidence of AIT.
Public stroke educational campaigns may be effective in improving knowledge and awareness.
In a review of 13 studies of public stroke education, stroke symptom recognition as well as intention to call emergency medical services were significantly improved in adults aged <65 years.
In Denmark, among 852 strokes and TIA patients, the knowledge of core symptoms of stroke improved both in patients and bystanders, but patient or system delays did not reduce significantly 1 year after the initiation of the Danish stroke campaign.
However, the FAST (Face, Arm, Speech, Time) campaign in the United Kingdom had no impact on response to TIA or minor stroke, whereas in patients with major stroke the delay in seeking medical attention was reduced after the campaign [11].
The dissemination of knowledge to primary care and emergency room physicians could have a substantial impact on patient care, as it would decrease the number of patients falsely labelled with a TIA event.
As such, the quality and volumes of referrals to SPCs could be improved, contributing to enhanced efficiency of stroke prevention interventions.
High rates of TIA mimics referred for assessment contributes to delays in care through bottlenecking.
If we are able to improve wait times, particularly for high-risk TIA patients, this could ultimately reduce stroke rates.
The implications on health services are also significant, as better referrals would lead to marked cost savings by decreasing the number of unnecessary tests ordered for referred patients, and ultimately reducing the costs associated with preventable strokes [13].
Conclusions
AIT predominantly affects elderly individuals over the age of 50, with the highest incidence recorded in the age groups of 60-80 years, and an extremely low incidence in individuals under 40 years old.
Significant differences were found between genders and social environments, with females and individuals from urban areas being more predisposed to suffer from TIA.
Among the most important risk factors identified in patients with TIA included in the study were: hypertension, obesity, atherosclerosis, diabetes and metabolic diseases.
Conflict of interests
None to declare.
Source of funding
This study was conducted with the support of the POCU/993/6/13/153178 grant, "Research Performance" co-financed by the European Social Fund under the Sectoral Operational Programme Human Capital 2014-2020
References
- 1.Hu H, Zhang X, Zhao J, Li Y, Zhao Y. Transient Ischemic Attack and Carotid Web. Am J Neuroradiol. 2019;40(2):313–318. doi: 10.3174/ajnr.A5946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Rooij, Kessels RPC, Richard E, De Leeuw, van Dijk. Cognitive Impairment in Transient Ischemic Attack Patients: A Systematic Review. Cerebrovasc Dis. 2016;42(1-2):1–9. doi: 10.1159/000444282. [DOI] [PubMed] [Google Scholar]
- 3.Yao Q, Zhang L, Zhou J, Li M, Jing W, Li X, Han J, He L, Zhang Y. Imaging Diagnosis of Transient Ischemic Attack in Clinic and Traditional Chinese Medicine. BioMed Res Int. 2019;2019:5094842–5094842. doi: 10.1155/2019/5094842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gorelick PB. Epidemiology of transient ischemic attack and ischemic stroke in patients with underlying cardiovascular disease. Clin Cardiol. 2004;(5 Suppl 2):II4–11. doi: 10.1002/clc.4960271403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simmons BB, Cirignano B, Gadegbeku AB. Transient ischemic attack: Part I. Diagnosis and evaluation. Am Fam Physician. 2012;86(6):521–6. [PubMed] [Google Scholar]
- 6.Simmons BB, Gadegbeku AB, Cirignano B. Transient ischemic attack: Part II. Risk factor modification and treatment. Am Fam Physician. 2012;86(6):527–532. [PubMed] [Google Scholar]
- 7.About Stroke: Types of Stroke - TIA (Transient Ischemic Attack) Available from: https://www.stroke.org/en/about-stroke/types-of-stroke/tia-transient-ischemic-attack.
- 8.Transient Ischaemic Attack (TIA) 2023 Available from: https://www.nhs.uk/conditions/transient-ischaemic-attack-tia/#:~:text=A%20transient%20ischaemic%20attack%20(TIA)%20is%20often%20a%20sign%20that,having%20either%20in%20the%20future.
- 9. Smith WS , Johnston SC , Hemphill III JC . In: Harrison's Principles of Internal Medicine . 20th . Jameson J , Fauci AS , Kasper DL , Hauser SL , Longo DL , Loscalzo J , editors. McGraw Hill ; 2018 . Cerebrovascular Diseases ; pp. 3068 – 3078 . [Google Scholar]
- 10.Boehme AK, Esenwa C, Elkind MS. Stroke Risk Factors, Genetics, and Prevention. Circulation Research. 2017;120(3):472–495. doi: 10.1161/CIRCRESAHA.116.308398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Komulainen T, Koivisto A, Jäkälä P. Incidence of first-ever transient ischemic attack in Eastern Finland. Acta Neurol Scand. 2022;146(5):615–622. doi: 10.1111/ane.13689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wong KS , Caplan LR , Kim JS . Intracranial Atherosclerosis: Pathophysiology, Diagnosis, and Treatment . Frontiers of Neurology and Neuroscience ; 2016 . Stroke Mechanisms ; pp. 58 – 71 . [DOI] [PubMed] [Google Scholar]
- 13.Fitzpatrick T, Gocan S, Wang CQ, Hamel C, Bourgoin A, Dowlatshahi D, Stotts G, Shamy M. How do neurologists diagnose transient ischemic attack: A systematic review. Int J Stroke. 2019;14(2):115–124. doi: 10.1177/1747493018816430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diet and physical activity: a public health priority. 2021 Available from: https://cdn.who.int/media/docs/default-source/obesity/who-discussion-paper-on-obesity---final190821.pdf?sfvrsn=4cd6710a_1&download=true.
- 15.WHO and FAO announce global initiative to promote consumption of fruit and vegetables. 2003 Available from: https://www.who.int/news/item/11-11-2003-who-and-fao-announce-global-initiative-to-promote-consumption-of-fruit-and-vegetables.
- 16.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 17.Hebden L, O'Leary F, Rangan A, Singgih Lie, Hirani V, Allman-Farinelli M. Fruit consumption and adiposity status in adults: A systematic review of current evidence. Critical Reviews in Food Science and Nutrition. 2017;57(12):2526–2540. doi: 10.1080/10408398.2015.1012290. [DOI] [PubMed] [Google Scholar]
- 18.Bloomfield HE, Kane R, Koeller E, Greer N, MacDonald R, Wilt T. Benefits and Harms of the Mediterranean Diet Compared to Other Diets. VA Evidence-based Synthesis Program Reports. 2015 [PubMed] [Google Scholar]
- 19.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 20.Sonni S, Thaler DE. Transient ischemic attack: Omen and opportunity. Cleve Clin J Med. 2013;80(9):566–576. doi: 10.3949/ccjm.80a.12141. [DOI] [PubMed] [Google Scholar]
- 21.Manktelow BN, Potter JF. Interventions in the management of serum lipids for preventing stroke recurrence. Cochrane Db syst rev. 2009;2009(3):CD002091–CD002091. doi: 10.1002/14651858.CD002091.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng SF, Brown MM. Atherosclerotic carotid artery disease: Contemporary medical therapies. Semin Vasc Surg. 2017;30(1):8–16. doi: 10.1053/j.semvascsurg.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 23.O'Regan C, Wu P, Arora P, Perri D, Mills EJ. Statin therapy in stroke prevention: A meta-analysis involving 121,000 patients. Am J Med. 2008;121(1):24–33. doi: 10.1016/j.amjmed.2007.06.033. [DOI] [PubMed] [Google Scholar]
- 24.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 25.Heart Disease and Stroke Statistics, A Public Health Action Plan to Prevent Heart Disease and Stroke . 2003 Available from: https://www.cdc.gov/dhdsp/action_plan/pdfs/action_plan_full.pdf.
- 26.Collins R, Peto R, MacMahon S, Hebert P, Fiebach NH, Eberlein KA, Godwin J, Qizilbash N, Taylor JO, Hennekens CH. Blood pressure, stroke, and coronary heart disease. Part 2: Short-term reductions in blood pressure: Overview of randomized drug trials in their epidemiological context. Lancet. 1990;335:827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 27.Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: A systematic review. Stroke. 2003;34(11):2741–2748. doi: 10.1161/01.STR.0000092488.40085.15. [DOI] [PubMed] [Google Scholar]
- 28.O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, Rangarajan S, Islam S, Pais P, McQueen MJ, Mondo C, Damasceno A, Lopez-Jaramillo P, Hankey GJ, Dans AL, Yusoff K, Truelsen T, Diener HC, Sacco RL, Ryglewicz D, Czlonkowska A, Weimar C, Wang X, Yusuf S. INTERSTROKE investigators. Risk factors for ischemic and intracerebral hemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet. 2010;376(9735):112–123. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 29.Wannamethee SG, Shaper AG, Whincup PH, Walker M. Smoking cessation and the risk of stroke in middle-aged men. JAMA. 1995;274(2):155–160. [PubMed] [Google Scholar]
- 30. Fiore MC , et al. Rockville, MD : U.S. Department of Health and Human Services. Public Health Service ; 2008 . A Clinical Practice Guideline for Treating Tobacco Use and Dependence: 2008 Update . [Google Scholar]
- 31.Sacco RL, Benjamin EJ, Broderick JP, Dyken M, Easton JD, Feinberg WM, Goldstein LB, Gorelick PB, Howard G, Kittner SJ, Manolio TA, Whisnant JP, Wolf PA. American Heart Association Prevention Conference IV: Prevention and rehabilitation of stroke. Risk factors. Stroke. 1997;28:1507–1517. doi: 10.1161/01.str.28.7.1507. [DOI] [PubMed] [Google Scholar]
- 32.Gorelick PB, Sacco RL, Smith DB, Alberts M, Mustone-Alexander L, Rader D, Ross JL, Raps E, Ozer MN, Brass LM, Malone ME, Goldberg S, Booss J, Hanley DF, Toole JF, Greengold NL, Rhew DC. Prevention of a first stroke: A review of guidelines and a multidisciplinary consensus statement from the National Stroke Association. J Am Med Assoc. 1999;281:1112–1120. doi: 10.1001/jama.281.12.1112. [DOI] [PubMed] [Google Scholar]
- 33.Goldstein LB, Adams R, Becker K, Furberg CD, Gorelick PB, Hademenos G, Hill M, Howard G, Howard VJ, Jacobs B, Levine SR, Mosca L, Sacco RL, Sherman DG, Wolf PA, del Zoppo. Primary prevention of ischemic stroke: A statement for healthcare professionals from the Stroke Council of the American Heart Association. Circulation. 2001;103:163–182. doi: 10.1161/01.cir.103.1.163. [DOI] [PubMed] [Google Scholar]
- 34. Boden-Albala B , Sacco RL . In: The Prevention of Stroke . Gorelick PB , Alter M , et al., editors. New York : Parthenon Publishing Group ; 2002 . Modifiable risk factors for stroke: Hypertension, diabetes mellitus, lipids, tobacco use, physical inactivity, and alcohol ; pp. 21 – 37 . [Google Scholar]
- 35.Obesity and overweight Fact sheet N°311 . 2006 Available from: https://www.mclveganway.org.uk/Publications/WHO_Obesity_and_overweight.pdf.
- 36.Kassotis CD, Vandenberg LN, Demeneix BA, Porta M, Slama R, Trasande L. Endocrine-disrupting chemicals: economic, regulatory, and policy implications. Lancet. Diabetes & Endocrinology. 2020;8(8):719–730. doi: 10.1016/S2213-8587(20)30128-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Durrington P. Dyslipidaemia. Lancet. 2003;362(9385):717–731. doi: 10.1016/S0140-6736(03)14234-1. [DOI] [PubMed] [Google Scholar]
- 38.Atherosclerosis, What is Atherosclerosis . 2022 Available from: https://www.nhlbi.nih.gov/health/atherosclerosis.


