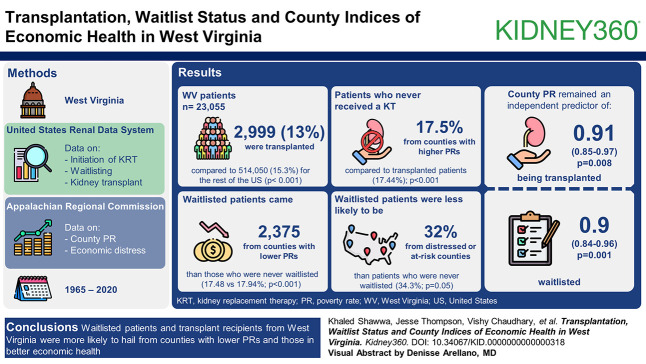
Visual Abstract
Keywords: ESKD, hemodialysis, renal transplantation, social determinants of health
Abstract
Key Points
Patients with ESKD coming from impoverished counties are less likely to be waitlisted or transplanted.
Insurance status modified the relationship between county poverty rates and waitlisting/transplant.
Background
Kidney transplantation is the optimal treatment for patients with ESKD. Given lower rates of kidney transplant in West Virginia (WV), we searched for potential predictors, focusing on the indices of economic health.
Methods
Data on the initiation of RRT, being waitlisted for, and receiving a kidney transplant between 1965 and 2020 were collected from United States Renal Data System. Data on county poverty rate (PR) and economic distress were collected from the Appalachian Regional Commission.
Results
Of the 23,055 WV patients identified, 2999 (13%) were transplanted compared with 514,050 (15.3%) for the rest of the United States (P < 0.001). Patients who never received a kidney transplant were from counties with higher PRs (17.95%) compared with transplanted patients (17.44%; P < 0.001). Waitlisted patients (2,375) came from counties with lower PRs than those who were never waitlisted (17.48 versus 17.94%; P < 0.001). Waitlisted patients were less likely to be from distressed or at-risk counties (32 versus 34.3%; P = 0.05) than patients who were never waitlisted. In multivariable logistic regression, county PR remained an independent predictor of being transplanted (odds ratio, 0.91; 95% confidence interval, 0.85 to 0.97; P = 0.008) or waitlisted (odds ratio, 0.9; 95% confidence interval, 0.84 to 0.96; P = 0.001) per 5% increase in PR after adjusting for age, sex, body mass index, alcohol use, functional status, and comorbid medical conditions. Group/employer health insurance seemed to modify the relationship between PR and waitlist, where PR remained an independent predictor of waitlisting among patients with insurance.
Conclusions
Waitlisted patients and transplant recipients from WV were more likely to hail from counties with lower PRs and those in better economic health.
Introduction
Kidney transplantation increases survival and improves quality of life for patients with ESKD receiving dialysis.1 The mortality benefit of kidney transplantation persisted even after patients spend a decade on dialysis.2 Most patients, however, are never waitlisted for a kidney transplant and may die without being waitlisted. Indeed, in 2020, only 12.7% of prevalent patients on dialysis were waitlisted.3 In the United States Renal Data System (USRDS) 2022 annual data report, at 6 months after initiation of dialysis, the cumulative incidence of death (11.2%) was more than 4 times that of waitlisting (2.6%).3 Despite being the preferred treatment for ESKD, this life-saving procedure remains out of reach for many patients.
The scarcity of organs available for transplantation remains an important obstacle to kidney transplantation. In addition, geographic and socioeconomic barriers facing patients, donors, and families make the transplant process overwhelming and challenging to navigate. Disparities and access to care may occur at any level before referral and evaluation, in between referral and waitlisting, or both.4 Currently, national surveillance systems do not capture data on transplant referral and evaluation. Beyond clinical factors, social determinants of health play an important role in the process of receiving a kidney transplant. Social determinants of health are the conditions in the environments where people are born, live, learn, work, play, worship, and age.5 Black patients were 25% less likely to be listed for transplantation than White patients and 26% less likely to receive any kidney transplant after accounting for social determinants of health.6,7 In a study in Southeastern United States where 57% of the patients with ESKD were Black, Black patients were less likely to be waitlisted when compared with White patients across different degrees of neighborhood poverty.8 However, Black patients were more likely to live in high poverty areas.
West Virginia (WV) has a high poverty rate (PR) with 33 of its 55 counties recognized as economically distressed or thereby at risk.9 This means that WV counties are ranked among the worst 10% or 10%–25% of US counties on the basis of an index calculated from PR, per capita market income and 3-year average unemployment rate. Many patients travel long distances to receive dialysis and often travel out of state to be evaluated for a kidney transplant. Since 1965, the total transplant rate of patients with ESKD from WV was only 13% compared with 15.3% for the rest of the United States (P < 0.001).3 WV presents a unique cohort where 91% of the ESKD cohort is White, which contrasts with patient populations evaluated in other studies. In these studies, the effect of poverty on waitlisting and transplantation was evaluated either in the context of racial disparities or the racial composition of neighborhood.4,10 Therefore, we evaluated the effect of socioeconomic factors on the rates of kidney waitlisting and transplantation in WV using data from the USRDS.
Methods
Patients
We collected data on patients with incident ESKD residing in WV, between January 1, 1965, and January 1, 2020, from the USRDS. The Institutional Review Board approved this project (protocol 2006045538).
County-Level Poverty and Economic Distress
Data on PR and county economic distress status were collected from Appalachian Regional Commission (ARC) (https://data.arc.gov/data). County-level PR is calculated as the ratio of the persons below the poverty level to the total number of persons for whom poverty status has been determined.9 Data on PR started to be collected in 1980s. We recorded data on the basis of each patient's county depending on the year patients started RRT. For patients starting RRT before 1990, we used the data from ARC on poverty from 1980. We used the 1990 data on poverty for patients starting RRT between 1990 and 1999 and data from 2000 for patients starting RRT between 2000 and 2004. Subsequently, yearly data corresponding to the specific RRT year between 2005 and 2016 were used. Finally, for patients starting RRT during or after year 2017, we used ARC's data from 2017 to 2020. Economic status of US counties is determined based on an index value. This index value is calculated based on PR, per capita market income and 3-year average unemployment rate. Distressed counties are defined as being the worst 10% of US counties. At-risk counties are the worst 10%–25% of US counties (Supplemental Table 1).
Statistical Analysis
We reported continuous variables as means and SD or median and interquartile range depending on data distribution and normality. We reported categorical variables as frequencies and percentages. Our primary outcome was to investigate the predictors of being waitlisted or receiving a kidney transplant. Chi-square or Fisher exact tests were used to compare proportions. The two-way independent t-test was used to compare means. Logistic regression was used to construct multivariable models. P value < 0.05 was considered statistically significant. All analysis was performed using SAS software 9.4 (SAS Institute Inc., Cary, NC). The maps were created using Leaflet package in RStudio 2023.03.1. We also used OpenStreetMap (OpenStreetMap contributors) as the base layer.
Results
Demographics
A total of 23,055 patients in WV started RRT between 1965 and 2020. There were 542 (2.35%) patients who received a preemptive kidney transplant; the remaining incident patients started RRT with dialysis. In-center hemodialysis was the most common modality with 19,205 (83.3%) patients. This was followed by peritoneal dialysis in 3015 (13.3%) patients and home hemodialysis in 152 (0.66%) patients. Most patients were White (91%). There were 10,508 (45.6%) female patients. The most common attributed cause for ESKD was diabetes in 10,614 (46%) patients, followed by hypertension in 3494 (15.1%) patients (Table 1).
Table 1.
Overall cohort demographics
| Variable | Value (N=23,055) |
|---|---|
| Female sex, count (%) | 10,508 (45.6) |
| Age at first RRT, mean (SD) | 62.6 (15.4) |
| Race, count (%) | |
| White | 20,932 (90.8) |
| Black/African American | 1951 (8.5) |
| Other races | 172 (0.7) |
| Primary cause of ESKD, count (%) | |
| DM | 10,614 (46) |
| HTN | 3494 (15.1) |
| Glomerulonephritis | 1809 (7.8) |
| Genetic disease | 723 (3.1) |
| Other | 6415 (28) |
| First RRT, count (%) | |
| In-center HD | 19,205 (83.3) |
| PD | 3051 (13.2) |
| Preemptive kidney transplant | 542 (2.3) |
| Home HD | 152 (0.7) |
| Unknown | 105 (0.5) |
| Primary insurance, count (%) | |
| Employer group | 4549 (20) |
| Medicare | 12,546 (56) |
| Medicaid | 4695 (21) |
| Other | 3448 (16) |
| No insurance | 460 (2) |
| Type of dialysis unit, count (%) | |
| For profit | 16,442 (71.3) |
| Nonprofit | 6134 (26.7) |
| Unknown or missing | 479 (2) |
| Received kidney transplant, count (%) | 2999 (13) |
| Ever waitlisted, count (%) | 2576 (11) |
| Kidney transplant after waitlisting, count (%) | 1784 (69) |
| Neither waitlisted nor transplanted, count (%) | 19,258 (83) |
DM, diabetes; HTN, hypertension; PD, peritoneal dialysis.
Transplant and Waitlist in WV
A minority of the cohort of 2576 (11%) patients were waitlisted with most receiving a kidney transplant (1784 [69%]). Most patients were never transplanted (20,056 [87%]). Compared with the rest of the United States, the percentage of patients from WV who were transplanted was significantly lower (2999/23,055 [13%] versus 514,050/2,848,405 [15.3%]; P < 0.001). Among patients who received a kidney transplant, 2457 (82%) were on dialysis before receiving transplant and 542 (18%) received a preemptive kidney transplant. In total, 2075 (69.2%) were from deceased donors, 836 (27.8%) were from living donors, and 88 (3%) were from unknown donor type. As for the rest of the United States, 333,039 (64.7%) were from deceased donor kidney transplant, 164,269 (31.9%) were from living donor, and 16,742 (3.2%) were from unknown donor type.
Patients who were transplanted or waitlisted differed significantly from patients who were not transplanted or waitlisted in comorbid medical conditions. They were less likely to have common comorbidities including diabetes, hypertension, diagnosis of chronic obstructive pulmonary disease, cerebrovascular accidents or transient ischemic attacks, congestive heart failure, ischemic heart disease, peripheral vascular disease, or history of amputation (P < 0.001). Similarly, patients who were transplanted or waitlisted were less likely to have alcohol use disorder, tobacco use, be institutionalized, or have compromised mobility (P < 0.001) (Table 2).
Table 2.
Patient characteristics on the basis of waitlist and transplant status
| Characteristicsa | Transplant (N=2999) | Not Transplanted (N=20,056) | P Value | Waitlisted (N=2576) | Not Waitlisted (N=20,479) | P Value |
|---|---|---|---|---|---|---|
| Age, mean (SD) | 44.7 (15) | 65.3 (14) | <0.001 | 49 (15) | 64 (15) | <0.001 |
| Female sex, count (%) | 1166 (39) | 9342 (47) | <0.001 | 1016 (39) | 9492 (46) | <0.001 |
| BMI, mean (SD) | 28.5 (7) | 29.6 (8) | <0.001 | 29.1 (7) | 29.5 (8) | <0.01 |
| DM, count (%) | 858 (29) | 9756 (49) | <0.001 | 931 (36) | 9683 (47) | <0.001 |
| HTN, count (%) | 1851 (89) | 13,437 (85) | <0.001 | 1784 (89) | 13,504 (85) | <0.001 |
| Institutionalizedb, count (%) | 28 (1.3) | 1216 (7) | <0.001 | 21 (1) | 1223 (7) | <0.001 |
| Compromised mobilityc, count (%) | 116 (5) | 2784 (17) | <0.001 | 108 (5) | 2792 (17) | <0.001 |
| COPD, count (%) | 96 (5) | 3050 (19) | <0.001 | 107 (5) | 3039 (19) | <0.001 |
| CVA/TIA, count (%) | 78 (4) | 1751 (11) | <0.001 | 87 (4) | 1742 (11) | <0.001 |
| CHF, count (%) | 309 (15) | 6472 (41) | <0.001 | 355 (18) | 6426 (40) | <0.001 |
| IHD, count (%) | 269 (17) | 4727 (44) | <0.001 | 296 (21) | 4700 (43) | <0.001 |
| Alcohol use, count (%) | 14 (0.7) | 247 (1.6) | <0.001 | 14 (0.7) | 247 (1.6) | <0.001 |
| Tobacco use, count (%) | 158 (7.6) | 1374 (8.7) | 0.08 | 145 (7) | 1387 (9) | 0.02 |
| PVD/history of amputation, count (%) | 147 (7) | 2675 (17) | <0.001 | 144 (7) | 2678 (17) | <0.001 |
| Received nephrology care, count (%) | 1168/1293 (90) | 7158/9570 (75) | <0.001 | 1134 (88) | 7192 (75) | <0.001 |
| Year first RRT, median (IQR) | 2006 (1998–2013) | 2000 (1992–2009) | <0.001 | 2004 (1996–2012) | 2006 (1998–2013) | <0.001 |
| Patient not informed of transplant due to medical, psychiatric or age, count (%) | 10 (0.3) | 1226 (6) | <0.001 | 11 (0.4) | 1225 (6) | <0.001 |
| Group/employer health insurance, count (%) | 948 (33) | 3601 (18) | <0.001 | 878 (35) | 3671 (18) | <0.001 |
| Distressed or at-risk counties, count (%) | 989 (33) | 6865 (34) | 0.2 | 828 (32.1) | 7026 (34.3) | 0.03 |
| PR, mean (SD) | 17.5% (5%) | 18% (5%) | <0.001 | 17.6% (5%) | 18% (5%) | <0.001 |
BMI, body mass index; CHF, congestive heart failure; CVA, cerebrovascular accident; DM, diabetes; HTN, hypertension; IHD, ischemic heart disease; IQR, interquartile range; PR, poverty rate; PVD, peripheral vascular disease.
Missing variables: hypertension, institutionalization, mobility, chronic obstructive pulmonary disease, cerebrovascular accident/transient ischemic attack, alcohol use, tobacco use, and peripheral vascular disease/amputation were missing in 5161 (22.4%) patients. Ischemic heart disease was missing in 10.602 (46%). Nephrology care before RRT was missing in 12,192 (53%) patients. Body mass index was missing in 4903 (21.2%) patients. Data on county economic distress level and poverty rate were missing in 9 (0.04%) patients.
Institutionalized: being in a nursing home, assisted living, or “other” institutions.
Compromised mobility was defined as inability to ambulate or transfer or if patients “need assistance” to ambulate.
County-Level Poverty and Economic Distress
Patients who never received a kidney transplant were from counties with higher PRs (17.95%) compared with transplanted patients (17.44%) (P < 0.001). Overall, waitlisted patients came from counties with lower PRs than those who were never waitlisted (17.48 versus 17.94%; P < 0.001). Waitlisted patients were less likely to be from distressed or at-risk counties (828 [32.1%] versus 7026 [34.3%]; P = 0.03). Poverty, transplant, and waitlist rates in WV counties are shown in Supplemental Figures 1–3.
Among those who were never transplanted, waitlisted patients (N=792) came from counties with lower PRs (17.1 versus 18%; P < 0.001) and less distressed or economically at-risk counties (28.9 versus 34.5%; P = 0.003) than those who were never waitlisted (N=19,258).
In multivariable logistic regression, county PR remained an independent predictor of lower odds of being transplanted (odds ratio [OR], 0.91; 95% confidence interval [CI], 0.85 to 0.97; P = 0.008) or waitlisted (OR, 0.9; 95% CI, 0.84 to 0.96; P = 0.001) per 5% increase in PR after adjusting for age, sex, body mass index, alcohol use, functional status, and comorbid medical conditions (Figures 1 and 2).
Figure 1.
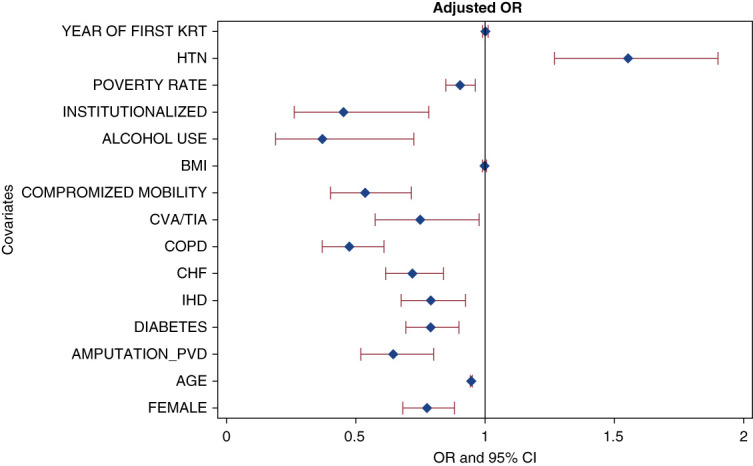
Predictors of being waitlisted. ORs for each variable: female sex 0.77 (95% CI, 0.68 to 0.88), age 0.94 (95% CI, 0.94 to 0.95), amputation/PVD 0.64 (95% CI, 0.52 to 0.8), DM 0.78 (0.7–0.9), IHD 0.8 (95% CI, 0.67 to 0.92), CHF 0.72 (95% CI, 0.6 to 0.84), COPD 0.47 (95% CI, 0.4 to 0.6), CVA/TIA 0.75 (95% CI, 0.6 to 0.97), compromised mobility 0.54 (95% CI, 0.4 to 0.71), BMI 0.99 (95% CI, 0.98 to 1), alcohol use 0.4 (95% CI, 0.2 to 0.7), institutionalized 0.45 (95% CI, 0.3 to 0.8), HTN 1.55 (95% CI, 1.3 to 1.9), year of first RRT 1 (95% CI, 0.99 to 1) for each one year increase, and PR 0.9 (95% CI, 0.84 to 0.96) for each 5% increase in PR. BMI, body mass index; CHF, congestive heart failure; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; DM, diabetes; HTN, hypertension; IHD, ischemic heart disease; OR, odds ratio; PR, poverty rate; PVD, peripheral vascular disease; TIA, transient ischemic attack.
Figure 2.
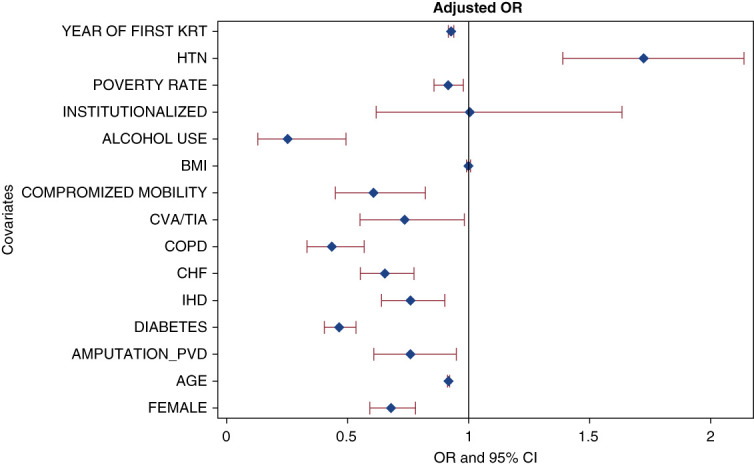
Predictors of being transplanted. ORs for each variable: female sex 0.67 (95% CI, 0.59 to 0.78), age 0.91 (95% CI, 0.91 to 0.92) for each one year increase, amputation/PVD 0.75 (95% CI, 0.6 to 0.94), DM 0.46 (0.4–0.53), IHD 0.75 (95% CI, 0.64 to 0.9), CHF 0.65 (95% CI, 0.55 to 0.77), COPD 0.43 (95% CI, 0.33 to 0.56), CVA/TIA 0.73 (95% CI, 0.55 to 0.98), compromised mobility 0.6 (95% CI, 0.44 to 0.82), BMI 0.99 (95% CI, 0.99 to 1), alcohol use 0.25 (95% CI, 0.12 to 0.49), institutionalized 0.45 (95% CI, 0.26 to 0.78), HTN 1.7 (95% CI, 1.4 to 2.1), year of first RRT 0.92 (95% CI, 0.91 to 0.93) for each one year increase, and PR 0.91 (95% CI, 0.85 to 0.97) for each 5% increase in PR.
Patients who had group/employer health insurance were more likely to come from counties with lower PR (17.75% versus 17.95%, P = 0.01) compared with those who did not. The interaction term between PR and group/employer health insurance was statistically significant in the analysis of waitlisting. Therefore, using the same model, we stratified the analysis by group/employer health insurance. PR was only statistically significant among patients who had group/employer health insurance (OR, 0.79 [95% CI, 0.71 to 0.89; P < 0.001]) for being waitlisted for every 5% increase in PR. When stratifying by group/employer insurance in analyzing the outcome of transplant, PR was not statistically significant (P = 0.09). Including the type of dialysis unit in the model as a sensitivity analysis did not change the results. PR remained associated with waitlisting among patients without group/employer health insurance only (OR 0.8 [95% CI, 0.71 to 0.9]; P < 0.001). For profit, dialysis unit was associated with lower odds of waitlisting (OR, 0.75 [95% CI, 0.57 to 0.97]; P = 0.03) compared with nonprofit dialysis units among patients with group/employer health insurance only. There was no association between type of dialysis unit and kidney transplant in the adjusted model (stratified by group/employer health insurance).
As a sensitivity analysis and to quantify the effect of insurance type, we created the following groups: Medicaid only (N=2347), Medicare with/without Medicaid but without group/employer health insurance (N=10,202), and patients who have group/employer health insurance irrespective of Medicare/Medicaid status (N=4549). In the same model that included comorbid medical conditions and demographics, PR (OR, 0.92 [95% CI, 0.87 to 0.97; P = 0.002] per 5% increase), Medicaid only (OR, 0.54 [95% CI, 0.44 to 0.67; P < 0.001]), and Medicare coverage (OR, 0.75 [95% CI, 0.62 to 0.9; P < 0.001]) were independently associated with lower odds and group/employer health (OR, 1.66 [95% CI, 1.39 to 1.98; P < 0.001]) with higher odds of waitlisting. As for transplant outcome, PR and Medicare coverage were not statistically significant; however, group/employer health (OR, 2.3 [95% CI, 1.88 to 2.8; P < 0.001]) was associated with higher odds and Medicaid only (OR, 0.46 [95% CI, 0.36 to 0.58; P < 0.001]) with lower odds of being transplanted. Including the type of dialysis unit in this model did not change the results and also showed that it was neither associated with transplant nor waitlisting.
Discussion
In this retrospective review of patients from WV initiating RRT between 1965 and 2020, waitlisted patients and transplant recipients were more likely to hail from counties with lower PRs and better economic health. Although insurance is an important factor in pursuing kidney transplant, higher PR remained an independent predictor of lower likelihood of being waitlisted among patients who had group/employer health insurance. Stratifying the analysis by group/employer health insurance eliminated the association between PR and receiving a kidney transplant.
A state of 1.8 million people, WV sits in the heart of Appalachia, a region comprised 423 counties in 13 states. All of WV's 55 counties are within the boundaries of this region, and the majority are considered fully (34) or in part (13) rural on the basis of the county being neither part nor adjacent to a metropolitan area.9 The median PR in our cohort was 17.2% (interquartile range, 14.4%–20.7%). This PR is based on the time patients started RRT and the estimated PR of that respective county during that year. This is significantly higher than the rest of the United States for which the PR has exceeded 15% only four times in the past six decades (1965, 1983, 1993, and 2011).11 Interestingly, the PR in the United States fell from 14.8% in 2009–2011 to 11.2% in 2019–2021 in contrast to the PR in WV which changed little during that same period12 except in 2019 when WV's PR reached its lowest level at 13.9%.13 The median PR in WV over the years has been close to 17%.13 WV differed from the rest of United States at many other levels, including income and unemployment rate (Supplemental Table 3).
Social determinants of health play an important role in the process of receiving a kidney transplant. This was also apparent in two studies taking place where there is a universal health care system. In a study in Sweden, both higher income and educational level were associated with better access to being waitlisted and receiving a kidney transplant.14 Lower degree of social deprivation (a score based on unemployment, car ownership, home ownership, and overcrowding) was associated with higher odds of waitlisting.15 There has been an abundance of evidence regarding the effect of racial disparity on kidney transplant rates. In a study in Southeastern United States where 57% of the patients with ESKD were Black, Black patients were less likely to be waitlisted when compared with White patients across different degrees of neighborhood poverty.8 However, Black patients were more likely to live in high poverty areas, with 28% of Black patients residing in areas with more than 25% of the population living below the poverty line. The effect of poverty as a risk factor was not quantified due to interaction with race in the evaluation of waitlisting.8 One study evaluated the effect of neighboring counties PRs on county-level transplant rates.16 Counties with high PRs that were surrounded by more affluent counties tended to have higher transplant rates than the ones surrounded by similar PRs.16 Conversely, counties with low and very low rates of poverty that were surrounded by relatively less wealthy counties had significantly lower transplant rates than their counterpart counties that were surrounded by other affluent counties. Because of the population-level evaluation of the effect of poverty on transplant rates, it is important to note that the analysis was not adjusted for patient-specific factors. In our study of WV, where White patients are the majority of the population, race did not influence the results (data not shown). We were able to quantify the effect of PR on waitlisting. As for kidney transplant, when taking insurance status into account, PR did not have much effect.
Despite an adjusted incidence rate that is slowly declining, the prevalence of ESKD continues to increase, reaching 2271 per million persons as reported by the 2020 USRDS Annual Data Report.3 Incidence and prevalence rates for WV patients with ESKD have trended similarly over the years, although WV's incident rate has been among the highest in the United States.3 Although the decrease in the incidence of ESKD is well-received, the rise in prevalence is accompanied by low rates of waitlisting among prevalent patients with ESKD on dialysis (12.7%), rates that are even lower for WV's ESKD patients (6.1%) in a state where the prevalence of ESKD continues to increase at a fast pace.17 That so few West Virginians are waitlisted suggests that patients in WV harbor unique challenges in addition to the many complexities known to face all patients undergoing the kidney transplant process. In fact, most incident patients in 2020 started RRT through in-center HD 84% or peritoneal dialysis 12.7%.3 This is especially true in WV, where added hurdles, such as low socioeconomic status and poverty, may further complicate an already complex situation where geographic and economic barriers are dense. Much of WV is considered impoverished with only 11 of the state's 55 counties having a PR between 2016 and 2020 that was lower that of the United States.9 Although not specific to WV, complicated logistics and difficulties navigating the evaluation process may be magnified in importance because of the limited opportunities to be transplanted in state. WV has two transplant centers currently available to patients, only one of which has been in full operation on a consistent basis over the past several decades. Many patients travel to adjacent states for transplant evaluation and management. Nonetheless, the ability to travel is likely to be influenced by patients' socioeconomic status who may not be able to afford the expenses of travel and lodging to meet transplant center requirement and remain active on the transplant list.
Our study had limitations. First, this was a retrospective analysis. However, this study included a relatively homogenous patient population in WV over 5 decades. In addition, knowing that data on PR for each county can vary over a long period of time, we matched each patient's county data with their respective year of starting RRT, whenever available. Second, we relied on one source for our information for both PRs and patient demographics and outcomes, separately. We did have missing variables; however, it seems that the missingness pattern was at random (Supplemental Table 2). Nonetheless, the USRDS is well-established national data system with standardized data collection process. The PRs were collected from Appalachia Region Commission that relies on data from the US Census Bureau, while there might be some bias, this is the closest estimate of true PR. Third, our findings may not be generalizable to other states given the population demographic and that 92.5% of WV residents are White. Finally, unmeasured confounding from other psychosocial factors, such as lack of caregiver involvement, along with posttransplant support may play an important role in candidacy for transplantation.18 Our study, with its focused view of a homogeneous population adds to the ever-growing body of literature on health disparities by showing that inequity and inequality in the global outcomes of kidney transplant and waitlisting may exist beyond race.
Compared with the United States overall, significantly fewer numbers of WV patients with ESKD received kidney transplants between 1965 and 2020. Improving access to kidney transplantation has been the subject of much attention of late. Our results underscore the importance of economic distress as an independent barrier to transplantation and speak to the need to address the challenges faced by patients with low socioeconomic status when developing national efforts aimed at reducing barriers.
Supplementary Material
Disclosures
R. Schmidt reports the following: Consultancy: Outset; Research Funding: Arbor Research, NIH/NIDDK, and Retrophin; Advisory or Leadership Role: Board of Directors, Past President and Counselor, Renal Physicians Association; Member, American Association of Kidney Patients Medical Advisory Board; Member, Kidney Transplant Collaborative Board of Directors; and Member, Quality Insights Board of Directors; Speakers Bureau: US Renal Care; and Other Interests or Relationships: Husband's company leases building space to a dialysis corporation. K. Shawwa reports the following: Employer: West Virginia University; and Ownership Interest: CRWD, DG, ENPH, FTCI, IREN, MYRG, and TSLA. J. Thompson reports the following: Employer: West Virginia University; and Ownership Interest: Apple, Google, and Tesla. All remaining authors have nothing to disclose.
Funding
None.
Author Contributions
Conceptualization: Bethany Pellegrino, Rebecca Schmidt, Khaled Shawwa.
Data curation: Rebecca Schmidt, Khaled Shawwa, Jesse Thompson.
Formal analysis: Rebecca Schmidt, Khaled Shawwa.
Investigation: Bethany Pellegrino, Rebecca Schmidt, Khaled Shawwa.
Methodology: Rebecca Schmidt, Khaled Shawwa.
Project administration: Rebecca Schmidt.
Resources: Rebecca Schmidt.
Software: Khaled Shawwa.
Supervision: Rebecca Schmidt, Khaled Shawwa.
Visualization: Khaled Shawwa.
Writing – original draft: Rebecca Schmidt, Khaled Shawwa.
Writing – review & editing: Vishy Chaudhary, Anthony Parravani, Bethany Pellegrino, Mark Poling, Jesse Thompson.
Data Sharing Statement
All data is included in the manuscript and/or supporting information.
Supplemental Material
This article contains the following supplemental material online at http://links.lww.com/KN9/A409.
Supplemental Table 1. County economic status designation.
Supplemental Table 2. Missing variables by waitlist and transplant status.
Supplemental Table 3. Economic parameters for West Virginia and the United States.
Supplemental Figure 1. Poverty rate in WV counties.
Supplemental Figure 2. Transplant rate in WV counties.
Supplemental Figure 3. Waitlisting rate in WV counties.
References
- 1.Tonelli M Wiebe N Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–2109. doi: 10.1111/j.1600-6143.2011.03686.x [DOI] [PubMed] [Google Scholar]
- 2.Rose C, Gill J, Gill JS. Association of kidney transplantation with survival in patients with long dialysis exposure. Clin J Am Soc Nephrol. 2017;12(12):2024–2031. doi: 10.2215/CJN.06100617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.United States Renal Data System. 2022 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.2022.
- 4.Patzer RE Perryman JP Schrager JD, et al. The role of race and poverty on steps to kidney transplantation in the Southeastern United States. Am J Transplant. 2012;12(2):358–368. doi: 10.1111/j.1600-6143.2011.03927.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. Social Determinants of Health. Accessed July 7, 2023. https://health.gov/healthypeople/priority-areas/social-determinants-health [Google Scholar]
- 6.Ng YH Pankratz VS Leyva Y, et al. Does racial disparity in kidney transplant waitlisting persist after accounting for social determinants of health?. Transplantation. 2020;104(7):1445–1455. doi: 10.1097/tp.0000000000003002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wesselman H Ford CG Leyva Y, et al. Social determinants of health and race disparities in kidney transplant. Clin J Am Soc Nephrol. 2021;16(2):262–274. doi: 10.2215/CJN.04860420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM. Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol. 2009;20(6):1333–1340. doi: 10.1681/ASN.2008030335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Data Reports. Appalachian Regional Commission. Accessed July 11, 2023. https://data.arc.gov/data [Google Scholar]
- 10.Saunders MR, Cagney KA, Ross LF, Alexander GC. Neighborhood poverty, racial composition and renal transplant waitlist. Am J Transplant. 2010;10(8):1912–1917. doi: 10.1111/j.1600-6143.2010.03206.x [DOI] [PubMed] [Google Scholar]
- 11.Jessica Semega MK, Shrider EA, Creamer JF. Income and Poverty in the United States: 2019. US Department of Commerce. US Census Bureau. Accessed July 11, 2023. https://www.census.gov/library/publications/2020/demo/p60-270.html [Google Scholar]
- 12.Shrider E. Most States Had Lower Official Poverty Rates in 2019-2021 than a Decade Earlier. February 07, 2023. Accessed July 13, 2023. https://www.census.gov/library/stories/2023/02/state-official-poverty-rates-changed-over-10-years.html [Google Scholar]
- 13.US Census Bureau. Historical Poverty Tables: People and Families - 1959 to 2021, Accessed July 13, 2023. https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-people.html [Google Scholar]
- 14.Zhang Y, Gerdtham UG, Rydell H, Jarl J. Socioeconomic inequalities in the kidney transplantation process: a registry-based study in Sweden. Transplant Direct. 2018;4(2):e346. doi: 10.1097/txd.0000000000000764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dudley CR, Johnson RJ, Thomas HL, Ravanan R, Ansell D. Factors that influence access to the national renal transplant waiting list. Transplantation. 2009;88(1):96–102. doi: 10.1097/TP.0b013e3181aa901a [DOI] [PubMed] [Google Scholar]
- 16.Mohan S, Mutell R, Patzer RE, Holt J, Cohen D, McClellan W. Kidney transplantation and the intensity of poverty in the contiguous United States. Transplantation. 2014;98(6):640–645. doi: 10.1097/tp.0000000000000125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Institute of Diabetes and Digestive and Kidney Diseases. Strategic Plans and Reports. SRDS. Data Query Tools. ESRD Prevalent Count. Accessed July 15, 2023. https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds/data-query-tools/esrd-incident-count [Google Scholar]
- 18.Reed RD, Locke JE. Social determinants of health: going beyond the basics to explore racial disparities in kidney transplantation. Transplantation. 2020;104(7):1324–1325. doi: 10.1097/tp.0000000000003003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data is included in the manuscript and/or supporting information.