Abstract
Objectives:
Adverse childhood experiences, or early life trauma (ELT), may be a potential risk factor for opioid use disorders (OUD) that could be further influenced by depression, anxiety, and stress. The prevalence and strength of these associations are largely unknown.
Methods:
This study examined the association between current OUD severity and lifetime history of ELT, and the degree to which current depression, anxiety, and stress influenced this association, in persons (n=310) with at least one lifetime exposure to opioids using an online survey.
Results:
93% of respondents experienced at least one trauma in their lifetime and 65% met criteria for OUD. ELT was largely unassociated with demographics but demonstrated an almost “dose-dependent” association between all forms of ELT (total, general, physical, emotional, sexual), whereby more ELT was associated with more severe current OUD. A multivariate mediation model found perceived stress to be a robust mediator of this association. Current psychiatric functioning did not significantly moderate the relationship between ELT and OUD, suggesting ELT may impact OUD severity at varying levels of psychiatric functioning.
Conclusions:
These data support existing evidence that greater ELT may influence adult OUD severity and identify perceived stress as a potential mechanistic contributor to this association. Results are preliminary in nature but support continued research into mechanisms underlying the association between ELT and OUD, particularly conformational changes in the stress system resultant from ELT, and interventions to mitigate the impact of ELT on OUD development and/or develop trauma-informed OUD treatment approaches.
Keywords: opioid use disorder, opioid, adverse childhood experiences, stress
1. Introduction
Opioid use disorder (OUD) is associated with elevated rates of morbidity and mortality and an estimated economic burden of approximately $504 billion per year1. The chronic, relapsing nature of OUD places extreme burden on patients and their loved ones, as well as on the healthcare industry, which is presently working to scale up efforts to address the large unmet need for OUD care. Better understanding of psychological and biological factors that increase risk of transitioning from opioid use to misuse and OUD may help to optimize delivery of care by better targeting key ingredients that help to maintain the cycle of addiction.
One putative risk factor for the development of OUD is early life trauma (ELT). ELTs are defined as general, physical, emotional, and/or sexual events that occur prior to age 18, which may alter normal development and have the potential to confer long-lasting harmful effects on the individual’s physical and psychological functioning2. ELTs are highly prevalent; up to 62% of non-institutionalized US adults report experiencing >1 traumatic event during childhood and close to 25% experienced >33. ELT has been associated with greater psychological distress, emotional reactivity, and risks for myriad emotional and physical health problems in adulthood, including substance use disorders (SUDs).4,5 Findings of several studies have shown that opioid-dependent individuals report greater incidence of ELT than healthy controls6–7 and, in fact, may have the higher rates of ELT than patients with other types of psychiatric disorders8.
Although little is known about factors that influence the course or strength of these relationships, investigators have recently begun to speculate that symptoms of psychological distress may be mechanistically involved. This includes internalizing behaviors such as depression and anxiety, which are known mental health consequences of ELT9 and phenotypic markers of risks for alcohol and drug misuse10–13. Psychological stress is another factor that could hypothetically play a role. A large body of evidence has demonstrated that chronically high levels of glucocorticoids during the early stages of trauma exposure may lead to altered neuroendocrine and behavioral responses to stress in adulthood14–17, which may, in turn, contribute to the pathogenesis and progression of SUDs18–19. However, to our knowledge, no studies have thus far evaluated the mediating or moderating role of psychological stress in the relationship between ELT and OUD and only two have explored the role of internalizing/externalizing symptoms, focusing primarily on non-medical prescription opioid use20–21.
In this study, we evaluated whether ELT is associated with OUD risk status or disease severity and whether depression, anxiety, and/or perceived stress explain the process or influence the strength or direction of the relationship between ELT and OUD severity. These data can help expand our understanding of these relationships and establish a foundation from which more prospective studies on this topic could be supported.
2. Methods
2.1. Respondents
Respondents were recruited through Amazon Mechanical Turk (mTurk), a crowdsourcing platform that is regularly used in the recruitment of clinical research participants22, between 9/15/2020 and 10/13/2020. The study advertised a “survey on health behaviors” and eligible respondents had to reside within the United States, have a prior mTurk task approval rating of >90%, be over the age of 18, and report using either heroin, or prescription opioids or engaging in non-medical use of prescription opioids (NMPO) >1 in their lifetime. This latter criterion ensured all study participants had an opportunity to have developed opioid misuse or OUD. Respondents earned $0.10 for completing a brief (1-minute) eligibility screening and $3 for completing the survey. Respondent enrollment was continually monitored and periodic adjustments to study admission were made to allow oversampling of persons who did meet criteria for OUD (at any level); this decision was made to support adequate assessment of the study hypotheses. Best practices for quality control monitoring (e.g., multiple choice and qualitative probe questions) were embedded throughout the questionnaire and 100% accuracy was required for data to be retained for analyses. Overall, 2276 persons initiated the study, 639 (28%) were eligible and completed the survey and 310 (13.6%) passed all embedded quality control checks. The Johns Hopkins Medicine Institutional Review Board (JHM-IRB) acknowledged this study.
2.2. Measures
2.2.1. Demographics:
Respondents completed a series of standardized demographic items (e.g., age, gender, race, ethnicity, household income, marital status, and childcare responsibilities) and the number of non-opioid substances they endorsed using to get high or outside of a prescription (range 0–12) was summed and analyzed as a measure of polysubstance exposure.
2.2.2. Opioid Use:
Current OUD severity was assessed using a (past year) Diagnostic and Statistical Manual of Mental Disorders (DSM-523) checklist for OUD; results were summed into a total score and also categorized into none, mild (2–3), moderate (4–5), or severe (>6 symptoms). The number of OUD criteria endorsed (0–11) was analyzed as a continuous measure of OUD severity and the scale yielded a Cronbach’s alpha of 0.85. Secondary OUD-related outcomes included >1 lifetime use of heroin (yes/no), number of opioid withdrawal symptoms experienced following opioid discontinuation (0–12), OUD treatment history (none, past, current treatment), money ($) spent on opioids in the past 30 days, known history of opioid overdose, and the extent to which they believed their early life traumatic experiences contributed to their current opioid use (5-point Likert rating from “not at all” to “extremely”).
2.2.3. Early Life Trauma (ELT):
ELT was assessed using the Early Life Trauma Inventory-self report (ETI-SR)24, a 27-item self-report form that asks respondents to indicate (yes/no) whether they had experienced any general (11 items), physical (5 items), emotional (5 items), or sexual (6 items) traumas before the age of 18. Analyzed outcomes were total and subscale scores, with higher score values representing more early life traumas.
2.2.4. Psychiatric Functioning:
Stress was assessed using the Perceived Stress Scale (PSS)25, a 10-item self-report measure on which items related to stress over the past 30 days are rated on a 5-point (0=never to 4=often) Likert scale; results were summed into a total score wherein higher values represent greater current stress. Current depression and anxiety were assessed using the PROMIS DSM-5 Level 2 Depression and Anxiety scales26, two 8-item self-report measures on which symptoms are rated using a 5-item Likert scale (1-never to 5=always). Results were normalized into t-scores based upon age and gender-based norms.
2.3. Data Analyses
The analyses explored whether a relationship between ELT and OUD existed and the degree to which other psychiatric domains may influence the association. Respondent characteristics were summarized and associations between demographic and drug use characteristics and ratings on the ETI-SR subscale and Total scores were compared using independent groups T-tests for continuous variables and chi-squares for binary comparisons. Kruskal Wallace nonparametric tests were used to compare ratings on the ETI-SR scales as a function of respondent DSM-5 OUD status (none, mild, moderate, severe). The relationship between ETI-SR scales and current psychiatric functioning was examined first using Pearson Product correlations. Mediation and moderation analyses (SPSS Process v3.527) were then conducted, wherein the ETI Total score was the independent variable and OUD severity (operationalized as the number of symptoms endorsed) was the dependent variable. Depression, anxiety, and perceived stress total scores were included in the models as potential mediators or moderators, and all analyses controlled for the demographic variables age, gender, and race. Mediation analyses were first conducted as univariate analyses that examined depression, anxiety, and perceived stress as independent constructs; the three potential mediators were then examined together in a multiple mediation model analysis. Moderation analyses examined each of the three constructs independently. All analyses were conducted using SPSS version 25 and alpha was set at 0.05.
3. Results
3.1. Respondent Characteristics (see Supplemental Table 1):
Respondents were a mean (SD) 38.6 (11.9) years old, mostly female (58.4%), and white/Caucasian (79.7%), with 21.2% reporting Hispanic ethnicity. Respondents reported a greater lifetime history of exposure to prescription opioids (87.4%) than to heroin (38.4%) and endorsed a mean of 4.0 (2.4) OUD symptoms on the DSM-5 checklist, corresponding to no OUD symptoms (34.8%), as well as mild (10.0%), moderate (13.9%), and severe (41.3%) OUD. Almost half (47.7%) had never received treatment for OUD, and 52% had no known experience with opioid overdose. Among persons with current OUD, the mean (SD) money spent on opioids in the past 30 days was $401.49 ($1,520.78). Overall, 93% of respondents reported experiencing at least one trauma in their lifetime, with a mean (SD) number of 3.7 (2.5, range 0–11) general traumas, 2.3 (1.5, range 0–5) physical traumas, 2.2 (1.7, range 0–5) emotional traumas, and 1.6 (1.8, range 0–6) sexual traumas before the age of 18, representing a mean number of 9.9 (5.9, range 0–27) traumas total.
3.2. Early Life Stress
3.2.1. Associations with Demographics (see Supplemental Table 1):
ETI-SR ratings generally did not vary depending on demographic variables. The exceptions were that being Native Hawaiian was associated with higher scores on the Sexual scale (X2(36)=56.6, p=0.016), and being Black/African American was associated with higher Total scores (X2(156)=257.5, p<.001) relative to persons from other racial backgrounds. Persons of Hispanic ethnicity also reported a greater history of Emotional (X2(5)=16.9, p=0.005) and Sexual (X2(6)=18.0, p=0.006) trauma relative to persons without Hispanic ethnicity. Finally, persons who had never been married had higher scores on the Emotional scale (X2(5)=12.0, p=0.04) compared to those with marriage history and persons with current childcare responsibilities had higher scores on the General (X2(10)=18.7, p=0.04) and Emotional (X2(5)=14.3, p=0.014) scales relative to persons without current childcare responsibilities.
3.2.2. Associations with OUD:
A robust relationship was observed between ELT-SR scores and OUD severity. Meeting criteria for current OUD (yes/no), independent of OUD severity level, was significantly associated with more trauma as rated on the General (t(308)=5.515, p<.001), Physical (t(308)=2.49, p=0.013), Emotional (t(308)=2.449, p=0.015), Sexual (t(308)=5.323, p<.001) subscales as well as the Total score (t(308)=5.302, p<.001). The mean (SD) number of ELT events reported by individuals with and without OUD was 11.0 (5.5) and 7.3 (5.6), respectively. When the association of ELT was examined as a function of current OUD severity classification, an almost a “dose-dependent” relationship between the number of traumatic events endorsed and current OUD severity was observed (Figure 1) for each of the General (X2(3)=54.99, p<.001), Physical (X2(3)=19.50, p<.001), Emotional (X2(3)=16.66, p=0.002), Sexual (X2(3)=50.50, p<.001), and Total (X2(3)=50.21, p<.001) scales.
Figure 1.
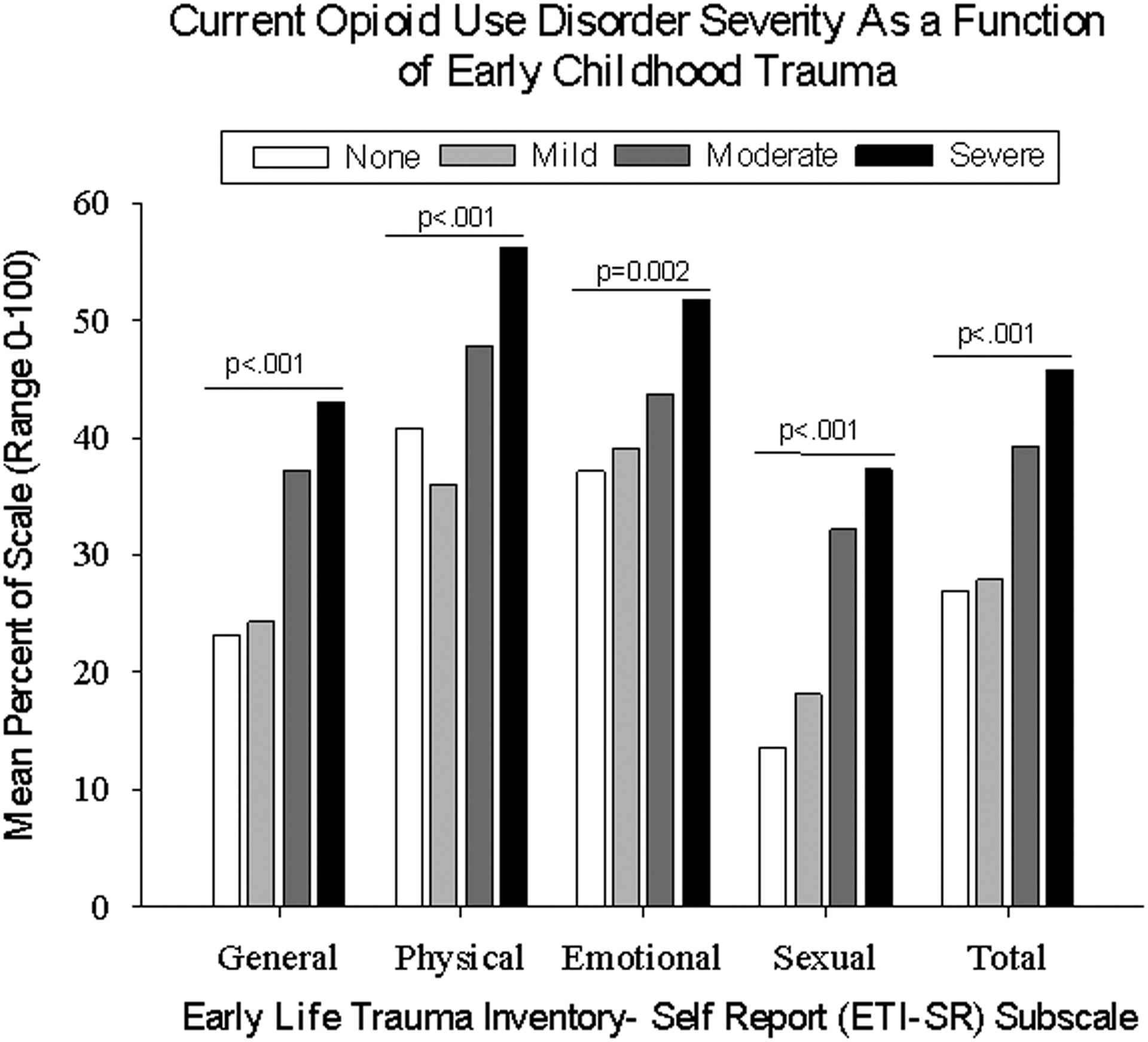
Current Opioid Use Disorder Severity as a Function of Early Childhood Trauma. X-axis represents subscales from the Early Trauma Inventory-Self Report (ETI), representing general (range 0–11 items), physical (0–5 items), emotional (0–5 items), sexual (0–6 items), and total (0–27) traumas reported as having happened before the age of 18. Data were converted to the mean percent of scale (MPE, mean traumas as a percent of possible endorsements) on the Y-axis to allow scales to be plotted together. Bars represent current OUD severity, including none (open), mild (light gray), moderate (dark gray), and severe (black) OUD. Values compared within each trauma category using Kruskal Wallace nonparametric tests; p<.05 is significant.
These associations were supported by trends observed in other secondary measures of OUD severity, including having ever used heroin, having a known history of opioid overdose, and having been treated for OUD were all associated with significantly greater ELT (See Supplemental Figure 1). Spending more money on opioids in the past 30 days was correlated with significantly greater endorsement of past trauma on the General (r(310)=.125, p=0.03) and Total (r(310)=.119, p=0.04) scales, and experiencing a greater number of opioid withdrawal symptoms was associated with significantly higher traumas as rated by the General (r(310)=.238, p<.001), Physical (r(310)=.151, p=0.008), Emotional (r(310)=.172, p=0.002), Sexual (r(310)=.169, p=0.003), and Total (r(310)=.240, p<.001) scales. Moreover, when asked directly, the majority of respondents (67.7%) believed their early childhood trauma contributed a little, moderately, or a lot to their opioid use.
3.2.3. Associations with Psychological Functioning:
Higher ratings on ELT subscales were significantly correlated with more severe depression, anxiety, and perceived stress (Table 1), with emotional ELT showing the most frequent associations with current problematic functioning.
Table 1.
Correlations Between Early Life Trauma and Current Comorbidities
| Early Trauma Inventory | |||||
|---|---|---|---|---|---|
| General Trauma | Physical Trauma | Emotional Trauma | Sexual Trauma | Total Score | |
| PROMIS | |||||
| DSM-5 Level 2 Anxiety SFa | .318** | .242** | .311** | .255** | .362** |
| DSM-5 Level 2 Depression SFa | .297** | .245** | .332** | .265** | .363** |
| Perceived Stress Scaleb | .195** | .191** | .315** | .127* | .260** |
SF=short form; Data represent two-tailed Pearson Product correlations;
=p<.05,
=p<.001
Values represent t-score normalized for age and gender/sex.
Rated as 1=never/none to 5=always/very severe/often
3.3. Mediation and Moderation Analyses
Mediation analyses (Table 2) revealed that the total effect of ELT on OUD severity was positive and statistically significant (b=0.23, p <.001), but was reduced somewhat when depression (b=0.19, p<.001), anxiety (b=0.20, p<.001) or perceived stress (b=0.19, p<.001) were included in the models. Indirect effects of depression (b=0.04, p<0.05, proportion mediated = 17%), anxiety (b=0.03, p<0.05, proportion mediated = 13%), and perceived stress (b=0.04, p < .05, proportion mediated = 17%) were all significant. Each of the models accounted for nearly a quarter of the variance in OUD severity when both the independent variable and mediator were included as predictors (R-square = 22%, 23%, 22% for anxiety, depression, and perceived stress, respectively). The multiple mediation model evaluating the combined and adjusted mediation effects of depression, anxiety, and perceived stress on this association revealed a significant indirect effect of the mediators (b=0.04, p<0.05, proportion mediated = 17%). However, perceived stress was the only mediator that continued to have a significant independent indirect effect in this model (b=0.03, p<.05, proportion mediated = 13%).
Table 2.
Mediation and Moderation Analyses
| Model | Independent Variable | Dependent Variable | Model | p | b | SE | t | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||||
| Anxiety Model | |||||||||
| 1 | ETI-SR Total Score | Promis Anxiety T-score | R2=0.14, F(4, 305)=13.0, p<.001 | <.001 | 0.54 | 0.08 | 6.92 | 0.34 | 0.69 |
| 2 | ETI-SR Total Score | OUD Symptoms (#)a | R2=0.20, F(4, 305)=18.9, p<.001 | <.001 | 0.23 | 0.03 | 7.84 | 0.17 | 0.29 |
| 3 | ETI-SR Total Score | OUD Symptoms (#)a | R2=0.22, F(5, 305)=17.01 p<.001 | <.001 | 0.20 | 0.03 | 6.43 | 0.14 | 0.26 |
| Promis Anxiety T-score | OUD Symptoms (#) | 0.01 | 0.06 | 0.02 | 2.63 | 0.01 | 0.10 | ||
| Indirect Effect (mediator = Promis Anxiety T-score)b | 0.03 | 0.01 | 0.01 | 0.06 | |||||
| Depression Model | |||||||||
| 1 | ETI-SR Total Score | Promis Depression T-score | R2=0.14, F(4, 305)=12.3, p<.001 | <.001 | 0.51 | 0.07 | 6.96 | 0.37 | 0.66 |
| 2 | ETI-SR Total Score | OUD Symptoms (#)a | R2=0.20, F(4, 305)=18.79, p<.001 | <.001 | 0.23 | 0.03 | 7.84 | 0.17 | 0.29 |
| 3 | ETI-SR Total Score | OUD Symptoms (#)a | R2=0.23, F(5, 305)=18.26, p<.001 | <.001 | 0.19 | 0.03 | 6.14 | 0.13 | 0.25 |
| Promis Depression T-score | OUD Symptoms (#) | <.001 | 0.08 | 0.02 | 3.62 | 0.04 | 0.12 | ||
| Indirect Effect (mediator = Promis Depression T-score)b | 0.04 | 0.01 | 0.02 | 0.07 | |||||
| Perceived Stress Model | |||||||||
| 1 | ETI-SR Total Score | Perceived Stress Scale | R2=0.09, F(4, 305)=7.63, p<.001 | <.001 | 0.25 | 0.05 | 4.84 | 0.15 | 0.35 |
| 2 | ETI-SR Total Score | OUD Symptoms (#)a | R2=0.20, F(4, 305)=18.8, p<.001 | <.001 | 0.23 | 0.03 | 7.84 | 0.17 | 0.29 |
| 3 | ETI-SR Total Score | OUD Symptoms (#)a | R2=0.25, F(5, 305)=20.6, p<.001 | <.001 | 0.19 | 0.03 | 6.63 | 0.14 | 0.25 |
| Perceived Stress Scale | OUD Symptoms (#) | <.001 | 0.15 | 0.03 | 4.73 | 0.09 | 0.21 | ||
| Indirect Effect (mediator = Perceived Stress Scale)b | 0.04 | 0.01 | 0.02 | 0.06 | |||||
| Multiple Mediation Model | |||||||||
| 1 | ETI-SR Total Score | Promis Depression T-score | R2=0.14, F(4, 305)=12.9, p<.001 | <.001 | 0.51 | 0.74 | 6.96 | 0.37 | 0.66 |
| 2 | ETI-SR Total Score | Promis Anxiety T-score | R2=0.15, F(4, 305)=13.0, p<.001 | <.001 | 0.54 | 0.08 | 6.91 | 0.38 | 0.69 |
| 3 | ETI-SR Total Score | Perceived Stress Scale | R2=0.09, F(4, 305)=7.63, p<.001 | <.001 | 0.25 | 0.05 | 4.84 | 0.15 | 0.35 |
| 4 | ETI-SR Total Score | OUD Symptoms (#)c | R2=0.20, F(4, 305)=18.9, p<.001 | <.001 | 0.23 | 0.03 | 7.84 | 0.17 | 0.29 |
| 5 | ETI-SR Total Score | OUD Symptoms (#)c | R2=0.25, F(7, 302)=14.76, p<.001 | <.001 | 0.19 | 0.03 | 6.17 | 0.13 | 0.25 |
| Promis Depression T-score | OUD Symptoms (#) | 0.37 | 0.03 | 0.04 | 0.90 | −0.04 | 0.11 | ||
| Promis Anxiety T-score | OUD Symptoms (#) | 0.66 | −0.01 | 0.03 | −0.44 | −0.08 | 0.05 | ||
| Perceived Stress Scale | OUD Symptoms (#) | <.001 | 0.13 | 0.04 | 3.11 | 0.05 | 0.21 | ||
| Indirect Effect (mediator = Promis Anxiety T-score)b | −0.01 | 0.02 | −0.05 | 0.03 | |||||
| Indirect Effect (mediator = Promis Depression T-score)b | 0.02 | 0.02 | −0.02 | 0.06 | |||||
| Indirect Effect (mediator = Perceived Stress Scale)b | 0.03 | 0.02 | 0.01 | 0.06 | |||||
| Anxiety Moderation Model | R2=0.23, F(6, 303)=15.10, p<.001 | ||||||||
| OUD Symptoms (#) | ETI-SR Total Score | <.001 | 0.19 | 0.03 | 6.18 | 0.13 | 0.25 | ||
| Promis Anxiety T-score | 0.01 | 0.06 | 0.02 | 2.74 | 0.02 | 0.10 | |||
| Interaction | 0.04 | 0.01 | 0.00 | 2.07 | 0.00 | 0.01 | |||
| 16% | <.001 | 0.14 | 0.04 | 3.12 | 0.05 | 0.22 | |||
| 50% | <.001 | 0.20 | 0.03 | 6.35 | 0.14 | 0.26 | |||
| 84% | <.001 | 0.25 | 0.04 | 6.44 | 0.17 | 0.32 | |||
| Depression Moderation Model | R2=0.25, F(6, 303)=16.5, p<.001 | ||||||||
| OUD Symptoms (#) | ETI-SR Total Score | <.001 | 0.18 | 0.03 | 6.02 | 0.12 | 0.24 | ||
| Promis Depression T-score | <.001 | 0.08 | 0.02 | 3.74 | 0.04 | 0.13 | |||
| Interaction | 0.03 | 0.01 | 0.00 | 2.24 | 0.00 | 0.01 | |||
| 16% | <.001 | 0.13 | 0.04 | 3.16 | 0.05 | 0.21 | |||
| 50% | <.001 | 0.19 | 0.03 | 6.11 | 0.13 | 0.25 | |||
| 84% | <.001 | 0.24 | 0.04 | 6.32 | 0.16 | 0.31 | |||
| Perceived Stress Moderation Model | R2=0.26, F(6, 303)=17.4, p<..001 | ||||||||
| OUD Symptoms (#) | ETI-SR Total Score | <.001 | 0.19 | 0.03 | 6.57 | 0.14 | 0.25 | ||
| Perceived Stress Scale Score | <.001 | 0.15 | 0.03 | 4.65 | 0.09 | 0.21 | |||
| Interaction | 0.79 | 0.00 | 0.00 | 0.26 | −0.01 | 0.01 | |||
Only significant models are presented.
OUD=opioid use disorder; ETI-SR= Early Trauma Inventory Self-Report, SE= standard error, CI=confidence interval
Model 2=total effect and Model 3=direct effect of early life trauma on opioid use disorder severity in the univariate mediation analyses.
T-scores and p-values not available for this method; indirect effects that do not include 0 in the confidence interval are significant.
Model 4=total effect and Model 5=direct effect in the multiple mediation analysis.
Moderation analyses also revealed significant main effects for ELT, depression, anxiety, and perceived stress (Table 2), such that higher levels of psychological distress were associated with a greater number of OUD symptoms. The interaction terms for depression and anxiety, but not perceived stress (p=0.79), were significant (p<.05). Yet, despite reaching significance, the inclusion of 0.00 in the confidence intervals of the anxiety and depression models prevented the null hypothesis from being rejected. Simple or conditional effects analyses that examined the relationship between OUD and ELT at lower (16th), mid (50th) and upper (84th) percentiles of anxiety and depression revealed significant relationships between ELT and OUD all levels of depression or anxiety (p<0.001 in all cases; Table 2). Despite not being able to reject the null hypothesis, visual inspection (Figure 2) suggests that the slopes of the regression lines are somewhat steeper at higher versus lower levels of psychological distress.
4. Discussion
This study examined associations between ELT and OUD severity in a community of sample of adults and provides additional data on the degree to which depression, anxiety, and stress function as mediators/moderators of this relationship. All respondents were persons who had a lifetime history of at least one opioid exposure, and therefore had an opportunity to have developed problematic opioid misuse. In this sample, greater exposure to ELT was associated with more severe current OUD as well as greater psychiatric impairment. Although the mediator analyses are somewhat tempered by the retrospective versus longitudinal nature of these data, as well as the relatively small effect sizes of the outcomes, some initial conclusions can be reached. First, each of the psychological variables examined appeared to mediate a significant portion of the relationship between ELT and OUD severity, and perceived stress stood out as the only significant mediator in a multiple mediation model that examined the effects of all three psychological variables simultaneously. These outcomes are theoretically grounded in preclinical and human retrospective research and expand our limited evidence base regarding adverse consequences of ELT.
The proportion of the sample who met self-reported DSM-5 criteria for OUD (65.4%) was higher than would generally be expected in a community sample, likely related to our oversampling admission strategy and the fact that persons with no lifetime exposure to opioids were not eligible for participation. In this sample, adults who had OUD also had a disproportionate amount of exposure to ELTs. Prior studies have found almost 50% of persons with OUD reported experiencing >4 ELT events6, 28, as opposed to approximately 16% of the general population29. In our sample, persons who did not meet criteria for OUD reported a mean (SD) of 7.6 (5.5), whereas persons who met criteria for OUD reported experiencing 9.9 (5.6), traumatic events in childhood. These rates are remarkably similar to mean (SD) ETI-SR scores of 7.5 (5.) in healthy adults, 11.8 (8.6) in persons with major depression, and 20.7 (11.2) in persons with post-traumatic stress disorder (PTSD)30.
The strong and nearly “dose-dependent” relationship between the number of ELT events experienced and current OUD severity observed in this study is also consistent with reports from other SUD populations29,31. These associations were evident for total ETI as well as individual domains (e.g., general, physical, emotional, sexual) and provide initial evidence that greater trauma exposure may contribute to vulnerability for OUD regardless of the type of trauma experienced. The fact that these trends were also evident in a range of other secondary metrics of OUD severity serves as a valuable positive control that both strengthens the reliability of these results and also helps to generalize these findings to prior reported associations between ELT and misuse of prescription opioids32, OUD7,21, age of opioid use initiation, injection drug use, overdose28, addiction severity33, odds of relapse34, heroin craving35 and more rapid transition from heroin use to OUD36. These outcomes support more focused, prospective research in this area.
Greater recall of ELT was also robustly correlated with more problematic psychiatric functioning, reflected by higher scores on measures of depression, anxiety, and stress. These results are somewhat limited by the retrospective nature of the data collection, as opposed to a longitudinal design that would more appropriately detect mediation and moderation trends. Nevertheless, they provide some compelling results consistent with the study premise that support more focused research. Specifically, the mediating effect of stress is particularly impactful because it aligns closely with preclinical and human neuroimaging data showing that ELT profoundly alters neuroendocrine stress systems, mesocorticolimbic brain structures, and opioid and dopamine neurotransmitter circuits that are integrally involved in stress regulation, emotion processing, and reinforcement.37. Alterations in these neural systems have been associated with internalizing symptoms, deranged physiological and emotional responses to stress, dysfunctional reward processing, poor decision-making, and increased incidence of SUDs38–40. These outcomes also conform to more than 20 years of evidence that both acute and chronic stress are meaningfully associated with the onset of SUDs13, 19, 41–42. Overall, these data provide preliminary support for the hypothesis that ELT can cause conformational changes in functioning that influence sensitivity to the reinforcing and antinociceptive effects of opioids37. These findings lend initial support to our overarching hypothesis that ELT-induced changes in brain function may represent biological endophenotypes that portend the development of an OUD vulnerability pathway mediated by internalizing symptoms and altered stress sensitivity.
The present study also replicates evidence of the mediating role of depression and anxiety in the ELT to OUD relationship. To date this has been reported by two studies20–21, both of which found internalizing/externalizing symptoms to weakly mediate associations between ELT and non-medical prescription opioid use in univariate but not multivariate models20, and to be associated with greater likelihood of having past year and lifetime OUD21. These data extend prior studies by suggesting stress, but not depression or anxiety, may be integral to these associations. The fact that ELT was associated in the current study with OUD independent of current levels of depression, anxiety, or stress was somewhat unexpected because prior studies have suggested phenotypic differences exist between individuals who do and do not develop depression following ELT44. These results may be a function of the sample size and potential underpowering to detect an effect across groups, which is also supported by the relatively low effect sizes of some study results.
Strengths of this study include the large sample of persons with variable levels of OUD and inclusion of several positive control OUD metrics that strengthen face validity of the results. Outcomes from mediation analyses also align closely with existing literature regarding ELT, mental disorders, and stress. Limitations include the inherent weaknesses of the remote, online, and self-report retrospective nature of the data collection, which was characterized by a high rate of quality control exclusions. The primary outcome data were collected using a self-reported DSM checklist approach, which has been validated for the DSM-IV but not DSM-545. One person who met criteria for mild OUD endorsed only physical symptoms of withdrawal and tolerance, and as a result they could be misclassified as having an OUD. The results of this study, while consistent with prior studies and the overarching study premise, were of low effect size. This may be a consequence of a low sample size or methodological issues with the retrospective or self-reported design. Ideally, future prospective studies would examine this in a longitudinal manner using clinical interviews that would help differentiate physical dependence from OUD. However, in the absence of such studies, the current approach is able to contribute to a broader understanding of how ELT may influence OUD and provide a foundation upon which additional work can be premised. These data should therefore be considered an important signal to promote more focused and prospective empirical research in this area.
5. Conclusions
These data add to limited existing evidence that persons with OUD have a high frequency of ELTs and demonstrate that more ELTs correspond to greater current OUD severity and problematic psychiatric functioning. The findings suggest that associations between ELT and drug misuse may be at least partially mediated by psychological symptoms and stress sensitivity and suggest ELT may have a significant impact on risks for OUD across disparate levels of psychological function. While preliminary in nature, these data reveal potentially meaningful associations between ELS, OUD, and internalizing disorders that warrant more focused prospective work in this area. Ultimately this study provides initial insight into how ELT may influence adult OUD severity and outlines direction for prospective research that aims to establishing causal associations as well as mechanisms underlying these relationships to help inform prevention and intervention strategies.
Supplementary Material
Footnotes
Disclosures: No authors have relevant conflicts to report. In the past 3 years KED has consulted for Canopy Corporation and MindMed, and served on an advisory board for Beckley-Canopy and Peabody Pharmaceuticals.
References
- 1.Gostin LO, Hodge JG, & Noe SA (2017). Reframing the opioid epidemic as a national emergency. Jama, 318(16), 1539–1540. [DOI] [PubMed] [Google Scholar]
- 2.Finkelhor D (2018). Screening for adverse childhood experiences (ACEs): Cautions and suggestions. Child Abuse & Neglect, 85, 174–179. [DOI] [PubMed] [Google Scholar]
- 3.Merrick MT, Ford DC, Haegerich TM, & Simon T (2020). Adverse childhood experiences increase risk for prescription opioid misuse. The Journal of Primary Prevention, 41(2), 139–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mersky JP, Topitzes J, & Reynolds AJ (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the US. Child Abuse & Neglect, 37(11), 917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothman EF, Edwards EM, Heeren T, & Hingson RW (2008). Adverse childhood experiences predict earlier age of drinking onset: results from a representative US sample of current or former drinkers. Pediatrics, 122(2), e298–e304. [DOI] [PubMed] [Google Scholar]
- 6.Winstanley EL, Mahoney III JJ, Lander LR, Berry JH, Marshalek P, Zheng W, & Haut MW (2020). Something to despair: Gender differences in adverse childhood experiences among rural patients. Journal of Substance Abuse Treatment, 116, 108056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garami J, Valikhani A, Parkes D, Haber P, Mahlberg J, Misiak B, Frydecka D, & Moustafa AA (2019). Examining perceived stress, childhood trauma and interpersonal trauma in individuals with drug addiction. Psychological Reports, 122(2), 433–450. [DOI] [PubMed] [Google Scholar]
- 8.Heffernan K, Cloitre M, Tardiff K, Marzuk PM, Portera L, Leon AC. Childhood trauma as a correlate of lifetime opiate use in psychiatric patients. Addict Behav. 2000. Sep-Oct;25(5):797–803. doi: 10.1016/s0306-4603(00)00066-6. [DOI] [PubMed] [Google Scholar]
- 9.Heim C, & Nemeroff CB (2001). The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biological Psychiatry, 49(12), 1023–1039. [DOI] [PubMed] [Google Scholar]
- 10.Cicchetti D, & Handley ED (2019). Child maltreatment and the development of substance use and disorder. Neurobiology of Stress, 10, 100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim Y, Kim K, Chartier KG, Wike TL, & McDonald SE (2021). Adverse childhood experience patterns, major depressive disorder, and substance use disorder in older adults. Aging & Mental Health, 25(3), 484–491. [DOI] [PubMed] [Google Scholar]
- 12.Mezquita L, Ibánez MI, Moya J, Villa H, & Ortet G (2014). A longitudinal examination of different etiological pathways to alcohol use and misuse. Alcoholism: Clinical and Experimental Research, 38(6), 1770–1779. [DOI] [PubMed] [Google Scholar]
- 13.Strine TW, Edwards VJ, Dube SR, Wagenfeld M, Dhingra S, Prehn AW, Rasmussen S, McKnight-Eily L, & Croft JB (2012). The mediating sex-specific effect of psychological distress on the relationship between adverse childhood experiences and current smoking among adults. Substance Abuse Treatment, Prevention, and Policy, 7(1), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Bellis MD, & Zisk A (2014). The biological effects of childhood trauma. Child and Adolescent Psychiatric Clinics, 23(2), 185–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maccari S, Krugers HJ, Morley‐Fletcher S, Szyf M, & Brunton PJ (2014). The consequences of early‐life adversity: neurobiological, behavioural and epigenetic adaptations. Journal of Neuroendocrinology, 26(10), 707–723. [DOI] [PubMed] [Google Scholar]
- 16.Pervanidou P, & Chrousos GP (2012). Posttraumatic stress disorder in children and adolescents: neuroendocrine perspectives. Science Signaling, 5(245), pt6. [DOI] [PubMed] [Google Scholar]
- 17.Plotsky PM, Thrivikraman KV, Nemeroff CB, Caldji C, Sharma S, & Meaney MJ (2005). Long-term consequences of neonatal rearing on central corticotropin-releasing factor systems in adult male rat offspring. Neuropsychopharmacology, 30(12), 2192–2204. [DOI] [PubMed] [Google Scholar]
- 18.George O, & Koob GF (2017). Individual differences in the neuropsychopathology of addiction. Dialogues in Clinical Neuroscience, 19(3), 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oswald LM, Wand GS, Kuwabara H, Wong DF, Zhu S, & Brasic JR (2014). History of childhood adversity is positively associated with ventral striatal dopamine responses to amphetamine. Psychopharmacology, 231(12), 2417–2433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quinn K, Frueh BC, Scheidell J, Schatz D, Scanlon F, Khan MR. Internalizing and externalizing factors on the pathway from adverse experiences in childhood to non-medical prescription opioid use in adulthood. Drug Alcohol Depend. 2019. Apr 1;197:212–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang R, Howe LD, Suderman M, Relton CL, Crawford AA, & Houtepen LC (2020). Adverse childhood experiences, DNA methylation age acceleration, and cortisol in UK children: a prospective population-based cohort study. Clinical Epigenetics, 12(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Strickland JC, & Stoops WW (2019). The use of crowdsourcing in addiction science research: Amazon Mechanical Turk. Experimental and Clinical Psychopharmacology, 27(1), 1. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 24.Bremner JD, Vermetten E, & Mazure CM (2000). Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: the Early Trauma Inventory. Depression and Anxiety, 12(1), 1–12. [DOI] [PubMed] [Google Scholar]
- 25.Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 385–396. [PubMed] [Google Scholar]
- 26.Schalet BD, Pilkonis PA, Yu L, Dodds N, Johnston KL, Yount S, Riley W, & Cella D (2016). Clinical validity of PROMIS depression, anxiety, and anger across diverse clinical samples. Journal of Clinical Epidemiology, 73, 119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hayes AF (2012). PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling,
- 28.Stein MD, Conti MT, Kenney S, Anderson BJ, Flori JN, Risi MM, & Bailey GL (2017). Adverse childhood experience effects on opioid use initiation, injection drug use, and overdose among persons with opioid use disorder. Drug and Alcohol Dependence, 179, 325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merrick MT, Ford DC, Ports KA, & Guinn AS (2018). Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatrics, 172(11), 1038–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bremner JD (2007). Functional neuroimaging in post-traumatic stress disorder. Expert Review of Neurotherapeutics, 7(4), 393–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, & Anda RF (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics, 111(3), 564–572. [DOI] [PubMed] [Google Scholar]
- 32.Swedo EA, Sumner SA, de Fijter S, Werhan L, Norris K, Beauregard JL, Montgomery MP, Rose EB, Hillis SD, & Massetti GM (2020). Adolescent opioid misuse attributable to adverse childhood experiences. The Journal of Pediatrics, 224, 102–109. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gerra G, Zaimovic A, Castaldini L, Garofano L, Manfredini M, Somaini L, Leonardi C, Gerra ML, & Donnini C (2010). Relevance of perceived childhood neglect, 5‐HTT gene variants and hypothalamus–pituitary–adrenal axis dysregulation to substance abuse susceptibility. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 153(3), 715–722. [DOI] [PubMed] [Google Scholar]
- 34.Derefinko KJ, García FIS, Talley KM, Bursac Z, Johnson KC, Murphy JG, McDevitt-Murphy ME, Andrasik F, & Sumrok DD (2019). Adverse childhood experiences predict opioid relapse during treatment among rural adults. Addictive Behaviors, 96, 171–174. [DOI] [PubMed] [Google Scholar]
- 35.Ghorbani F, Khosravani V, Mohammadzadeh A, & Shadnia S (2019). The role of emotion dysregulation in the relation of childhood trauma to heroin craving in individuals with heroin dependence. Drug and Alcohol Dependence, 195, 132–139. [DOI] [PubMed] [Google Scholar]
- 36.Larance B, Gisev N, Cama E, Nelson EC, Darke S, Larney S, & Degenhardt L (2018). Predictors of transitions across stages of heroin use and dependence prior to treatment-seeking among people in treatment for opioid dependence. Drug and Alcohol Dependence, 191, 145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oswald LM, Dunn KE, Seminowicz DA, & Storr CL (2021). Early Life Stress and Risks for Opioid Misuse: Review of Data Supporting Neurobiological Underpinnings. Journal of Personalized Medicine, 11(4), 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adinoff B Neurobiologic processes in drug reward and addiction. Harv Rev Psychiatry. 2004. Nov-Dec;12(6):305–20. doi: 10.1080/10673220490910844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kaul D, Schwab SG, Mechawar N, Matosin N. How stress physically re-shapes the brain: Impact on brain cell shapes, numbers and connections in psychiatric disorders. Neurosci Biobehav Rev. 2021. May;124:193–215. doi: 10.1016/j.neubiorev.2021.01.025. Epub 2021 Feb 5. [DOI] [PubMed] [Google Scholar]
- 40.Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. 2016. Aug;3(8):760–773. doi: 10.1016/S2215-0366(16)00104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Back SE, Brady KT, Waldrop AE, Yeatts SD, McRae AL, & Spratt E (2008). Early life trauma and sensitivity to current life stressors in individuals with and without cocaine dependence. The American Journal of Drug and Alcohol Abuse, 34(4), 389–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maclean MJ, Sims SA, & O’Donnell M (2019). Role of pre-existing adversity and child maltreatment on mental health outcomes for children involved in child protection: population-based data linkage study. BMJ Open, 9(7), e029675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tang R, Howe LD, Suderman M, Relton CL, Crawford AA, & Houtepen LC (2020). Adverse childhood experiences, DNA methylation age acceleration, and cortisol in UK children: a prospective population-based cohort study. Clinical Epigenetics, 12(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cisler JM, James GA, Tripathi S, Mletzko T, Heim C, Hu XP, Mayberg HS, Nemeroff CB, Kilts CD. Differential functional connectivity within an emotion regulation neural network among individuals resilient and susceptible to the depressogenic effects of early life stress. Psychol Med. 2013. Mar;43(3):507–18. [DOI] [PubMed] [Google Scholar]
- 45.Feingold A, Rounsaville B. Construct validity of the dependence syndrome as measured by DSM-IV for different psychoactive substances. Addiction. 1995;90(12):1661–1669. doi: 10.1046/j.1360-0443.1995.901216618.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


