Abstract
Background
Arthroscopic surgery has been established as an efficacious intervention for the treatment of rotator cuff tears. The primary aim of this study was to analyze the modifications in the lateral acromial angle (LAA) subsequent to rotator cuff repair surgery using single‐row rivet fixation and double‐row rivet fixation techniques. Furthermore, we sought to investigate the influence of LAA on the prognosis of rotator cuff repair surgery.
Method
This observational study retrospectively enrolled 105 patients diagnosed with degenerative rotator cuff tears who underwent arthroscopic rotator cuff repair between 2016 and 2019. Following the exclusion of two patients with subscapularis or superior labrum anterior and posterior (SLAP) tears, as well as three patients who were lost to follow‐up, a cohort of 100 patients was included for clinical and imaging evaluation. Among these individuals, 50 were assigned to the double‐row repair group, whereas the remaining 50 comprised the single‐row repair group. Bilateral shoulder magnetic resonance imaging (MRI) scans were conducted no less than 24 months post‐surgery. Experienced arthroscopic surgeons, blinded to the LAA measurements, assessed the rotator interval (RI) using a control MRI. Functional assessment was performed using the University of California, Los Angeles (UCLA) quick disability of the shoulder and arm, shoulder and hand (qDASH) score. The Wilcoxon signed‐rank test for dependent samples was employed to compare data between the pre‐ and post‐intervention groups. Pearson correlation coefficients were calculated to evaluate the relationship between different parameters.
Results
The study population consisted of 73 female patients and 27 male patients, with a mean age of 58.32 ± 5.29 years and a mean follow‐up duration of 25.88 ± 8.11 months. Preoperatively, the mean LAA was 75.81° ± 11.28°, RI was 4.78 ± 0.62, UCLA score was 17.54 ± 2.44, and qDASH score was 2.45 ± 0.25. The average tear size was 8.95 ± 2.11 mm. A statistically significant difference in LAA was observed between the preoperative and postoperative measurements, with the double‐row repair group exhibiting a greater LAA than the single‐row repair group. Finally, a significant correlation was identified between LAA, RI, and qDASH scores after a 24‐month follow‐up period.
Conclusion
According to our findings, the utilization of double‐row rivet fixation has a greater LAA angle than single‐row rivet fixation. Moreover, this preservation of LAA is significantly associated with the functional recovery of the shoulder joint.
Keywords: Arthroscopy, Lateral acromion angle, Rotator cuff repair
Changes in the Lateral Acromion Angle in Rotator Cuff Tear Patients with Acromioplasty.
Introduction
Over the past two decades, surgeons have increasingly shown a preference for acromioplasty surgery over open surgery in the management of rotator cuff tear (RCT), based on clinical practice and outcomes. 1 , 2 , 3 Over the past two decades, surgeons have increasingly shown a preference for acromioplasty surgery over open surgery in the management of RCT, based on clinical practice and outcomes. 4 Arthroscopic surgery has demonstrated favorable outcomes in patients with varying degrees of rotator cuff injury. 1 , 5 Numerous arthroscopic rotator cuff repair techniques have been proposed, with the double‐row repair technique gaining popularity in the past decade. 6 , 7 The double‐row repair technique has been shown to possess better tolerance and reduced risk of retearing compared to single‐row riveting techniques. 8 , 9 However, certain studies have reported no significant distinction between the double‐row and single‐row rivet repair techniques (visual analog scale [VAS], 1.2 vs. 1.1; Subjective Shoulder Value [SSV], 91.3 vs. 91.8; American Shoulder and Elbow Surgeons [ASES], 91.0 vs. 91.4; UCLA, 31.9 vs. 32.1). 10 Therefore, the therapeutic efficacy of single‐row rivet and double‐row rivet fixation requires further study, especially for small or mid‐RCTs.
The morphology of the acromion significantly affects the quality of the rotator cuff and the outcome of treatment. 11 It has been found that a low LAA is strongly associated with shoulder impingement, especially during arm elevation. 12 , 13 A low LAA can be associated with a higher incidence of rotator cuff impingement with some authors suggesting a cut off of around 70–75 degrees as lower limits of normal. 14 , 15 The LAA intensifies stress on the supraspinatus tendon, while a substantial subacromial gap may further reduce the distance between the supraspinatus tendon and the base of the subacromial hook. 16 Additionally, the elevation of the arm may subject the supraspinatus tendon and bursa to irritant friction. MRI has revealed a statistically significant correlation between the lateral acromion angle (LAA) and rotator cuff disease (RCD). 14
Orthopedic surgeons are progressively performing arthroscopic procedures for repairing the rotator cuff. 17 The primary goals of rotator cuff repair comprise achieving substantial initial fixation strength, minimizing gap formation, maintaining mechanical stability during cyclic loading, and optimizing the biology of the tendon‐bone interface until the cuff biologically heals to the bone. 18 Single‐row and double‐row suture techniques are commonly employed in shoulder arthroscopy for rotator cuff repair. 19 In addition, the concept of the “Acromial Index” (AI), introduced by Nyffeler et al., which signifies the lateral extension of the acromion above the humeral head, has emerged as a prognostic marker for RCTs. 20 While AI aids in distinguishing between healthy shoulders and those afflicted with subacromial pathology, it might not provide the same discriminatory capacity between impingement and cuff tears. 21 , 22 , 23 In large or massive RCTs, factors such as trauma and degeneration in addition to acromion morphology may play an important role. However, in small or moderate RCTs, the morphology of the acromion may play an important role. 24 Beeler et al. used multiplanar computed tomography (CT) to examine the three‐dimensional (3D) shape of the acromion and reported that the axial (more externally rotated acromion) and coronal tilt of the acromion was larger and the posterior glenoid coverage was wider in patients with RCTs than in those with osteoarthritis (OA). In patients without RCTs, the anterior coverage was reported to have been significantly wider. 25 The morphological characteristics of the acromion have been categorized using various measurements due to its linkage with shoulder pathologies. Previous investigations have demonstrated that a reduction in LAA can lead to subacromial decompression. 14 , 26 To our knowledge, no relationship between the degree of small or middle rotator cuff injury and the angle of LAA has not been reported.
Despite prior hypotheses, the connection between LAA and postoperative recovery following rotator cuff repair surgery for rotator cuff injuries remains a contentious subject. Consequently, our study aims to analyze: (i) changes in LAA in the context of rotator cuff injuries; and (ii) investigate the relationship between LAA and rotator cuff injuries and their healing process. This will be accomplished through the utilization of single‐row or double‐row rivet fixation to observe the long‐term alteration of LAA angles after rotator cuff repair.
Materials and Methods
The study design employed here is a retrospective study, which has received approval from the Ethics Committee of Beijing Chaoyang Hospital and the Institutional Review Board (IRB) (BJCY20150032). Informed consent has been obtained from all participating patients. These research endeavors adhere to the principles outlined in the Declaration of Helsinki and the CONSORT guidelines.
Patients
A total of 105 patients who underwent arthroscopic rotator cuff repair at our institution between January 1, 2015, and December 31, 2019, were enrolled in our study. The inclusion criteria comprised: (i) clinically diagnosed repairable small or medium RCTs; (ii) symptoms persisting for more than 3 months; (iii) inadequate results from conservative treatment, and visibility on MRI (small to medium sized repairable full thickness tears; and (iv) excluded associated subscapularis or superior labrum anterior and posterior (SLAP) tears, grade 3–4 fatty infiltration (Goutallier Classification). Exclusion criteria comprised: (i) associated subscapularis tendon tears or SLAP injury; and (ii) grade 3–4 fatty infiltration, and acute traumatic tears, shoulder instability, acromioclavicular arthritis, glenohumeral arthritis, inflammatory arthritis, history of previous shoulder surgery, glenoid labral lesions, and adhesive capsulitis.
Measures of LAA and RI
The measurements of the LAA and rotator interval (RI) were conducted on T1‐weighted MR images of the preoperative, postoperative, and contralateral shoulder MRI by the primary surgeon and two experienced arthroscopic surgeons. To determine the LAA, the angles were drawn according to Banas' method, which involved connecting the lateral aspects of the upper and lower points of the glenoid cavities, resembling the critical shoulder angle. Subsequently, a line parallel to the lower surface of the acromion was drawn, and the angle formed between these two lines was defined as the LAA. The evaluation of the RI on the postoperative MRI followed the parameters described by Sugaya et al. 27 They categorized the RI into five groups: type 1 indicating adequate thickness and uniformly low intensity; type 2 representing adequate thickness and high intensity; type 3 indicating insufficient thickness without any discontinuity (cuff thinning); type 4 indicating slight discontinuity; and type 5 suggesting significant discontinuity. Follow‐up MRIs were performed every 6 months for a duration of 24 months. For the MRI protocol, a 4‐mm thin coronal section was taken, and sagittal turbo‐spin echo proton density‐weighted images (WI), T2‐WIs, coronal STIR sequences, and oblique coronal images were used. The coronal oblique images were taken in a plane parallel to the supraspinatus tendon 28 (Figures 1 and 2).
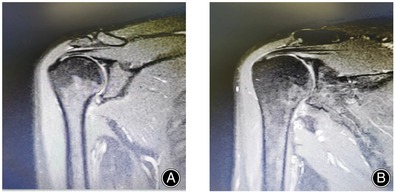
FIGURE 1.
The unmarked representative figure MRI of rotator cuff injury (A, B).
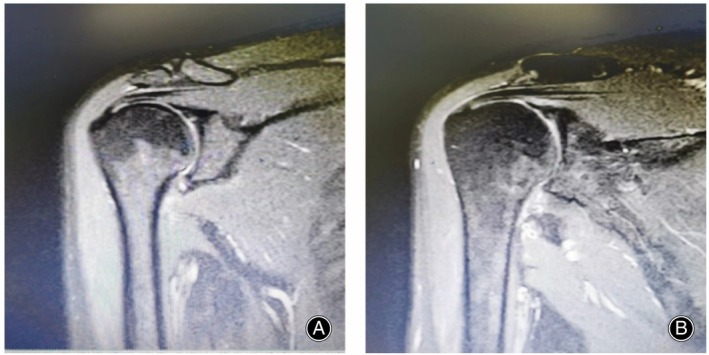
FIGURE 2.
Representative figure MRI of rotator cuff injury were tested for lateral acromial angle followed up at 6 months before and after surgery (A, B). Red indicates marker lines.
Surgery Procedure
The surgical procedures were performed by a single surgeon with the patient positioned laterally using a conventional arthroscopic portal. Tear size was measured using a probe and ruler. The initial 50 patients underwent single‐row repairs, whereas the subsequent 50 patients underwent double‐row repairs, regardless of the tear type. Shoulder sutureplasty was conducted routinely for all patients, and if a biceps lesion was present, a biceps tenotomy was performed. The repair procedure involved the use of one suture anchor for the single‐row repair, while the double‐row repair employed two suture anchors. Following the surgical intervention, patients were immobilized using a sling along with an abductor pillow, and passive range of motion exercises commenced on the day after the surgery.
Patients underwent the surgical procedure under general anesthesia and were positioned in the lateral decubitus posture with shoulder abduction traction. After preparing the surgical site through routine disinfection and towel placement, arthroscopy was performed using the soft point approach situated below and behind the acromion. Thorough cleaning of the inflammatory synovium was carried out, followed by the opening of the rotator cuff interval and loosening of the anterior and posterior articular as well as axillary sacs using a vaporized electric knife. Patients underwent the surgical procedure under general anesthesia and were positioned in the lateral decubitus posture with shoulder abduction traction. After preparing the surgical site through routine disinfection and towel placement, arthroscopy was performed using the soft point approach situated below and behind the acromion. Thorough cleaning of the inflammatory synovium was carried out, followed by the opening of the rotator cuff interval and loosening of the anterior and posterior articular as well as axillary sacs using a vaporized electric knife. In the single‐row fixation group, the anchors were positioned at a distance of 5 mm from the cartilage margin, subsequent to which the rotator cuff was sutured and secured with knots. In the double‐row suture bridge group, the anchors were inserted at the cartilage edge of the healing area, and the rotator cuff was sutured, knotted, and fixed. The proximal end of the rotator cuff was secured on the inner edge of the bone bed. The loose ends of each suture thread were inserted into the outer‐row anchor. Following tightening, the outer‐row anchor was placed approximately 8–10 mm from the cartilage edge, ensuring a firm attachment of the torn end of the rotator cuff to the greater tuberosity bed. 29
Post‐operative Rehabilitation
The rehabilitation program for all patients was under the supervision of the surgeon, encompassing passive range of motion exercises exclusively until the sixth week. Subsequently, the sling was removed, and a gradual transition to more active range of motion exercises was initiated. The rehabilitation process extended over a period of 3–4 months, focusing on progressive strengthening with the guidance of a skilled shoulder physiotherapist. Examinations are performed every 6 months after MRI. A bilateral shoulder MRI was conducted at a minimum of 24 months post‐surgery. The University of California, Los Angeles (UCLA) quick disability of the shoulder and arm, shoulder and hand (qDASH) score was utilized during the final follow‐up to evaluate functional outcomes (Figure 3).
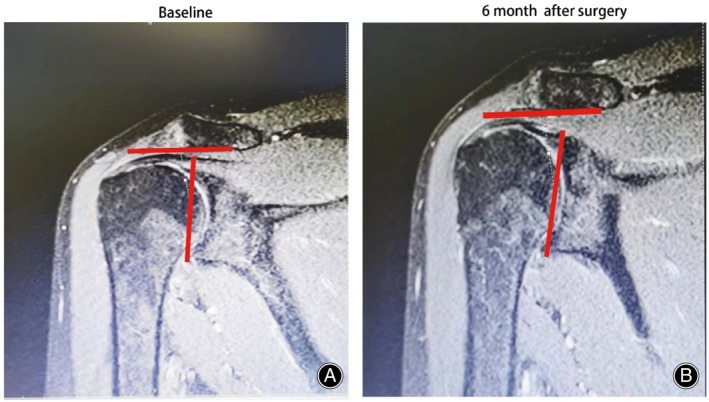
FIGURE 3.
Shoulder MRI was performed at 24 months after surgery (A–D).The rivets used in rotator cuff repair can be clearly seen while we took LAA angle measurements and analyzed the results.
Evaluation Indicators
The UCLA Shoulder Score, originally published in 1981 in the journal Clinical Orthopedics and Related Research, was initially designed to assess clinical outcomes specifically after total shoulder arthroplasty. 30 It comprises two sections: the physician section and the patient section. The physician section relies on physical examination and includes two single‐item sub‐scales, namely “active forward flexion” (scored up to a maximum of five points and completed by physicians) and “strength of forward flexion” (scored up to a maximum of five points and completed by physicians). 31 , 32 On the other hand, the Disabilities of the Arm, Shoulder and Hand (qDASH) questionnaire consist of 30 items that assess the patient's ability to perform specific upper extremity activities. This self‐report questionnaire allows patients to rate the level of difficulty and interference with their daily life activities on a five‐point Likert scale. 33 , 34
Statistical Analysis
The statistical analysis was conducted using SPSS (version 17, Chicago, IL, USA). Data are presented as median (range, min‐max) or mean ± standard deviation. Normal distribution of data such as tear size, mean age were assessed using the Kolmogorov–Smirnov test. The Wilcoxon signed‐rank test for dependent samples was employed to compare data between the pre‐ and post‐intervention groups, for example, LAA, RI, UCLA and qDASH. Pearson correlation coefficients were calculated to evaluate the relationship between different parameters. Statistical significance was defined as a p‐value <0.05.
Results
Patients' Characteristic
This study included a total of 100 eligible patients, consisting of 73 female and 27 male patients, with a mean age of 58.32 ± 5.29 years (coefficient of variation [CV]:0.08) and a mean follow‐up time of 25.88 ± 8.11 months (CV: 0.01). Preoperatively, the LAA was 75.81 ± 11.28 (CV: 0.02), RI was 4.78 ± 0.62 (CV: 0.01), UCLA was 17.54 ± 2.44 (CV: 0.03), and qDASH was 2.45 ± 0.25 (CV: 0.01). The mean size of tears was 8.95 ± 2.11 mm (CV: 0.03) (Table 1).
TABLE 1.
Patients' demography
| Indexes | Single‐row (50) | Double‐row (50) |
|---|---|---|
| Gender (female, %) | 38 (76%) | 35 (70%) |
| Dominate side (right, %) | 42 (84%) | 41 (82%) |
| Surgery side (right, %) | 37 (74%) | 34 (68%) |
| Age (years) | 54.28 ± 1.25 | 57.54 ± 2.41 |
| Follow‐up (months) | 25.18 ± 4.22 | 26.15 ± 4.10 |
Clinical Outcomes of Single‐row and Double‐row Repairs in the Treatment of Rotator Cuff Injuries
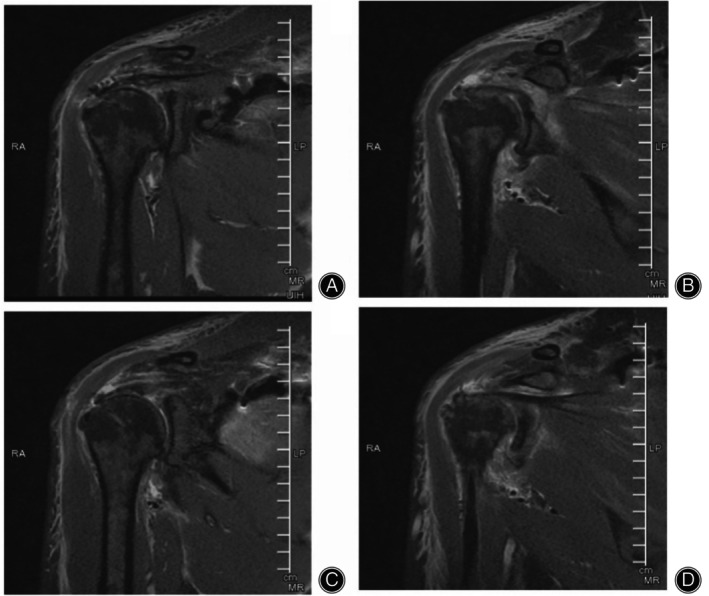
The repairs included 50 single‐row and 50 double‐row repairs. Prior to surgery, 97 patients had RI grade 5 and three patients had grade 4. MRI results were reviewed 24 months after surgery, revealing three cases with grade 5, four tears with grade 4, 16 cases with grade 3, 72 cases with grade 2, and five cases in grade 1 (Figure 4), further demonstrating the success of rotator cuff repair surgery in restoring the structure of the patient's shoulder joint. At the two‐year follow‐up, four patients in the single‐row repair group and three in the double‐row repair group had retears.
FIGURE 4.
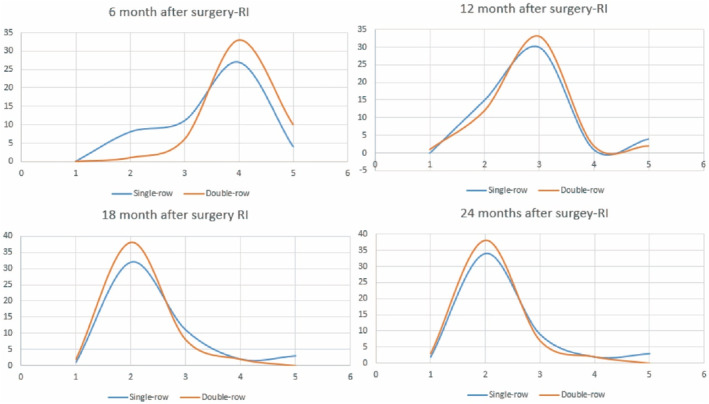
Surgery related repair integrity (RI) at 6, 12, 18 and 24 months between single and double row acromioplasty.
Analysis of LAA Correlation Results
Post‐operative measurements of LAA outcomes showed statistically significant differences between single and double rows of rivets at 6 months (p = 0.032, CV: 0.03) and 24 months (p = 0.001, CV: 0.01). Additionally, RI at 24 months after surgery showed a significant difference between single‐row and double‐row repairs (p = 0.041, CV: 0.09). There was also a significant difference in UCLA between 12 months and 18 months after surgery (p < 0.05, CV: 0.03). Double‐row repair significantly improved qDASH at 6 months after surgery compared to single‐row repair (p < 0.05, CV:0.05) (Table 2). Furthermore, our results showed a significant correlation between LAA and RI (p < 0.05, CV:0.01), UCLA (p < 0.05, CV:0.08), and qDASH (p < 0.05, CV:0.04) for both single‐row and double‐row rivet fixation in 12 months after surgery (Table 3, Figure 5).
TABLE 2.
Preoperative, postoperative 6, 12, 18, and 24 months follow‐up with result of LAA, RI, UCLA, qDASH change
| Parameter | Single‐row (50) | Double‐row (50) | p value | |
|---|---|---|---|---|
| LAA (°) | Probative data | 76.28 ± 12.85 | 75.98 ± 9.25 | 0.251 |
| 6 months after surgery | 80.26 ± 2.85 | 82.61 ± 8.00 | 0.032 | |
| 12 months after surgery | 81.01 ± 1.85 | 83.25 ± 2.85 | 0.015 | |
| 18 months after surgery | 82.95 ± 1.08 | 84.69 ± 5.22 | 0.011 | |
| 24 months after surgery | 83.21 ± 2.84 | 87.99 ± 7.21 | 0.001 | |
| RI | Probative data | 4.62 ± 1.05 | 4.88 ± 1.25 | 0.058 |
| 6 months after surgery | 4.58 ± 1.52 | 4.85 ± 2.00 | 0.055 | |
| 12 months after surgery | 3.86 ± 1.05 | 3.85 ± 0.0.86 | 0.075 | |
| 18 months after surgery | 3.24 ± 0.61 | 2.95 ± 0.68 | 0.042 | |
| 24 months after surgery | 2.25 ± 0.52 | 2.15 ± 0.48 | 0.041 | |
| UCLA | Probative data | 18.52 ± 3.28 | 17.05 ± 2.77 | 0.152 |
| 6 months after surgery | 26.58 ± 0.51 | 27.22 ± 2.25 | 0.095 | |
| 12 months after surgery | 27.15 ± 4.28 | 28.99 ± 5.17 | 0.041 | |
| 18 months after surgery | 33.15 ± 4.89 | 35.28 ± 4.87 | 0.021 | |
| 24 months after surgery | 34.25 ± 4.98 | 35.86 ± 4.88 | 0.077 | |
| qDASH | Probative data | 2.65 ± 0.99 | 2.28 ± 0.05 | 0.178 |
| 6 month after surgery | 4.47 ± 0.61 | 4.05 ± 0.18 | 0.001 | |
| 12 months after surgery | 4.08 ± 0.84 | 4.11 ± 0.99 | 0.058 | |
| 18 months after surgery | 4.00 ± 0.25 | 4.03 ± 0.21 | 0.379 | |
| 24 months after surgery | 4.08 ± 0.84 | 4.01 ± 0.28 | 0.221 |
Abbreviations: LAA, lateral acromial angle; qDASH, quick disability of the shoulder and arm, shoulder and hand; RI, rotator interval; UCLA, University of California, Los Angeles.
TABLE 3.
Correlation analysis between Single row‐LAA or Double row‐LAA
| RI | UCLA | qDASH | ||
|---|---|---|---|---|
| Single row‐LAA | r | 0.085 | 0.745 | −0.285 |
| p | 0.025 | 0.011 | 0.001 | |
| Double row‐LAA | r | 0.088 | 0.775 | −0.251 |
| p | 0.011 | 0.001 | 0.002 |
Abbreviations: LAA, lateral acromial angle; qDASH, quick disability of the shoulder and arm, shoulder and hand; RI, rotator interval; UCLA, University of California, Los Angeles.
FIGURE 5.
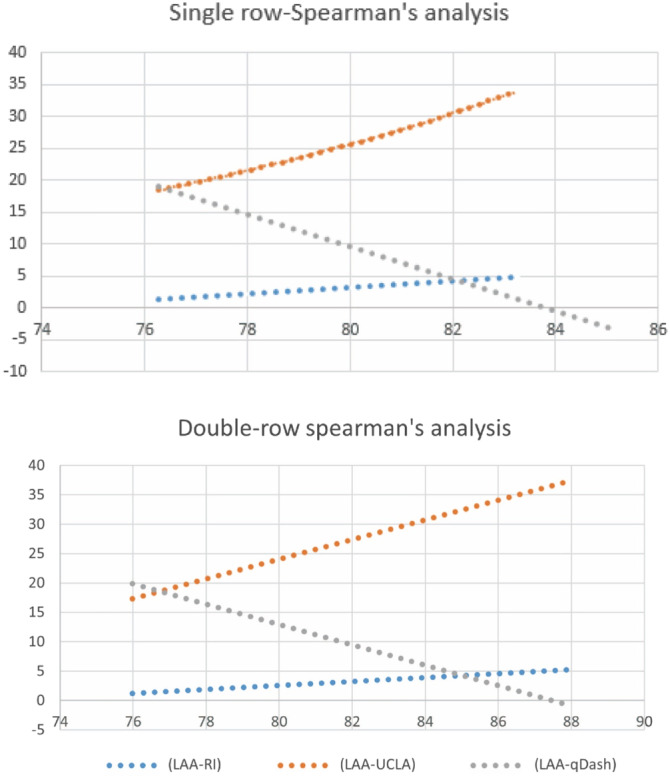
Spearmen analysis between single or double row acromioplasty and functional assessment such as University of California, Los Angeles (UCLA) quick disability of the shoulder and arm, shoulder and hand (qDASH) score in 12 months after surgery. LAA, lateral acromial angle; RI, rotator interval.
Discussion
Our research demonstrates that double‐row suture fixation leads to a greater LAA compared to single‐row suture fixation. Furthermore, we observed a significant correlation between LAA and the integrity of the shoulder joint, as well as shoulder‐related functional scores. These findings suggest that LAA could serve as a valuable predictor of arthroscopic surgery outcomes in the shoulder.
Rotator cuff repair surgery with double‐row rivet‐fixing and single‐row rivet‐fixation.
Distinct shoulder arthroscopy procedures have varying impacts on the functional recovery of patients with rotator cuff injuries. The double‐row rotator cuff repair technique involves the use of medial and lateral row suture anchors in the repair configuration. Biomechanical studies on double‐row repairs have demonstrated increased failure loads, enhanced contact area and pressure, and reduced gap formation at the site of healing attachment. 35 The advantages of double‐row suture fixation technology are as follows: first, the rotator cuff is inserted in the distribution of the footprint at the greater tubercle of the humerus. Single‐row fixation creates a point‐by‐point contact of the rotator cuff with the bone surface, which cannot ensure complete coverage of the sutured rotator cuff on the footprint area, making anatomical healing challenging to achieve. In terms of the anatomy, the contact area between the rotator cuff and the bone surface is relatively limited, which predisposes the formation of a gap at the suture site, thereby impacting the healing process of the bone‐tendon unit. Additionally, the fixation of anchors at the distal end of the rotator cuff leads to a concentrated stress distribution, contributing to the occurrence of retears. 28 , 36 , 37 , 38 However, the investigation conducted by Ying et al. failed to yield a definitive conclusion concerning the overall outcomes associated with double‐row and single‐row techniques used for repairing small to medium (<3 cm) or large to massive (>3 cm) RCTs. 39 Generally, double‐row techniques exhibit lower retear rates compared to single‐row techniques across most tear‐size categories. Notably, there were no disparities in retear rates between single‐row and double‐row techniques. 36 Nevertheless, Millett et al. discovered that single‐row repairs present significantly higher retear rates, particularly in cases of partial‐thickness retears, when compared to double‐row repairs. 40 Irrespective of tear categorization (isolated or combined) or repair approach (single or double row), arthroscopic subscapularis repair yielded substantial improvements across all outcome measures. 41
The Role of LAA in RCTs
The LAA serves as a frequently employed diagnostic tool for patients diagnosed with rotator cuff injuries. Yilmazturk et al. observed that patients exhibiting smaller LAA values in MRI images are more prone to RCTs. 42 Furthermore, Balke et al. discovered significant deviations in the LAA between patients with RCTs and control subjects or individuals diagnosed with impingement. Notably, LAA values below 70° were exclusive to patients suffering from RCTs. 43 The degenerative group had a significantly lower LAA (p = 0.001) than the normal group. 44 The investigation conducted within the Japanese population revealed that there existed no substantial correlation between the LAA and the incidence of RCTs. 45 In a parallel vein, Liu et al. observed a lack of discernible disparity in LAA values between individuals afflicted with degenerative articular‐sided partial thickness RCTs and their corresponding control subjects. 21 Consequently, a comprehensive meta‐analysis was undertaken to delve further into the intricate interplay between morphological parameters and the manifestation of rotator cuff injuries. The resultant findings distinctly demonstrated a statistically significant connection between degenerative RCTs and the LAA parameter. 46 In congruence with this established outcome, our study also disclosed a marked association between LAA and rotator cuff injuries, complemented by a notable escalation in LAA subsequent to surgical intervention.
In the course of our investigation, an intricate analysis was executed to discern alterations in the LAA angle following rotator cuff repair surgeries, encompassing diverse suture surgical bridge techniques. Analogous to our research findings, Li et al. corroborated a robust positive correlation between parameters such as CSA or AI and the tendon supraspinatus Neer quality (SNQ). 47 , 48 Additionally, Wu et al. undertook an exploration that underscored the pivotal role of the LAA in influencing the onset of postoperative discomfort and unfavorable outcomes, as indicated by JOA scores, among patients. 12 Further scholarly inquiry by Banas et al. accentuated a noteworthy inverse relationship between the reduction of the LAA and the prevalence of rotator cuff pathology (p < 0.0001). Furthermore, a substantial correlation was observed between advancing age and the manifestation of rotator cuff disorders (p < 0.0001). The outcome of a meticulous regression analysis lent credence to the assertion that both the LAA and the patient's age independently served as predictors of the rotator cuff score. 14 Moreover, Guo et al. advanced the understanding of the subject by identifying the acromial angle (AA) as a salient anatomical landmark situated at the confluence of the lateral border of the acromion. 49 Andrade et al. conducted an investigation into the impact of osseous risk factors on the development of degenerative full‐thickness primary RCTs. Their findings indicate a significant association between lower LAAs and a type III acromion with the occurrence of degenerative full‐thickness RCTs. 50 Furthermore, the utilization of single or double row rivet fixation technology, primarily affixed to the humeral head, exerts minimal influence on the LAA.
The assessment of acromion morphology through the employment of the LAA technique on X‐ray and MRI scans has been established as a reliable measure, both through objective evaluation and the expertise of seasoned observers. 51 Thiesemann et al. unveiled noteworthy alterations in the LAA subsequent to anterolateral acromioplasty and postoperative procedures. 52 Morphological analysis of the acromion in patients with degenerative supraspinatus tendon tears has highlighted resemblances to those with traumatic tears. This is characterized by a narrower subacromial gap, heightened lateral extension, and an inclination of the acromion angle. 53
Links between the LAA Indicator and Other Acromion Morphological Indicators
Our investigation has unveiled a significant correlation between the LAA and the AI. In concurrence with previous studies, Hanciau et al. have similarly determined that the lateral tilt of the acromion exhibits a higher clinical correlation (82.61%) when analyzed in isolation as opposed to comparison with the AI. 15 In a comprehensive examination that jointly considers lateral tilt and the AI, coupled with a positive Neer test, statistically significant data was ascertained (p < 0.083). This finding substantiates and enhances the reliability of evaluating the radiographic angle of lateral tilt, as corroborated by various references. 21 , 43 , 54 , 55 These findings collectively underscore the potential existence of a discernible correlation between LAA and the AI. It is noteworthy, however, that some investigations have reported a less pronounced association between LAA and AI. For instance, Xie et al. conducted a study suggesting that there is no statistically significant relationship between AI or LAA. 56 Consequently, further research is warranted to elucidate the precise nature of the relationship between LAA and AI.
The current body of literature presents a dearth of research concerning the association between LAA and upper limb clinical assessment (ULCA). Notably, Abrams et al. observed that their study results did not reveal any discernible disparity in clinical outcomes, such as the degree of correlation between LAA and ULCA, following rotator cuff repair procedures performed with or without acromioplasty at the two‐year postoperative mark. 57 Similarly, Xie et al. found that the University of California, Los Angeles (UCLA) score exhibited a statistically significant improvement in the no‐retear group compared to both the partial‐thickness retear and full‐thickness retear groups.
Moreover, our own study has uncovered a gradual postoperative transformation in LAA, potentially attributable to local calcification and other factors. Although a multitude of clinical and radiological investigations have scrutinized the relationship between LAA and degenerative RCT in the past decade, no biomechanical studies have hitherto been conducted to substantiate this theoretical connection. The potential significance of LAA as a determinant in degenerative RCT remains largely unverified. Should future biomechanical research corroborate this association, LAA could emerge as a substantial factor influencing the development of degenerative RCT.
The first important finding of our study was that we first found that double‐row rivets had better rotator cuff repair for single‐row rivets. The second important finding is that there was a clear correlation between LAA angle and shoulder function in patients. This suggests that LAA may be diagnostic in future diagnoses of rotator cuff injury.
Limitations
There are several limitations to our study. First, the population we studied is somewhat heterogeneous due to the inclusion of patients with small and medium RCTs, but not those with large RCTs, for whom double‐ or triple‐row rivet fixation tends to yield better results. Second, although our measurements have good intra‐rater and inter‐rater accuracy, measurement bias should be considered. To mitigate this, we randomly assigned standardized anterior and posterior shoulder radiographic images to two independent observers who were blinded to whether the images were acquired before or after surgery. Additionally, we attempted to standardize the protocol and exclude low‐quality images to prevent radiographic bias that could affect the reliability of the measurements. Finally, the retrospective design of the study is a limitation. To minimize heterogeneity in data collection, we selected only two senior orthopedic surgeons with the same training background and surgical approach.
Conclusion
According to our research, double‐row repair is more effective in preserving a higher LAA compared to single‐row repair. Furthermore, a significant correlation was observed between LAA and functional recovery of the shoulder joint. These findings emphasize the importance of LAA in the treatment of rotator cuff injuries and its potential role in improving patient outcomes.
Funding Information
This research was not funded.
Conflict of Interest Statement
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Ethical Review Committee Statement
This research was authorized and approved by the ethical committee of Beijing Chaoyang Hospital and the institutional review board (IRB) (BJCY20150032). All patients were informed and signed an informed consent form. According to the CONSORT guidelines, these studies also comply with the Declaration of Helsinki.
Author Contributions
Guarantor of integrity of the entire study: Lei Zang. Study concepts: Xiaochuan Kong. Study design: Hong Gang. Definition of intellectual content: Literature research: Hong Gang Zhang Le. Clinical studies: Hong Gang. Experimental studies: Data acquisition: Zheng Yinfeng, Fan Ning. Data analysis: Zheng Yinfeng. Statistical analysis: Fan Ning. Manuscript preparation: Hong Gang. Manuscript editing: Hong Gang. Manuscript review: Xiaochuan Kong.
Consent for Publication
Not Applicable.
Acknowledgments
We would like to thank all participants and our hospital. All this work was finished in Beijing Chaoyang Hospital.
Data Availability Statement
The data used to support the findings of this study are included within the article.
References
- 1. Flores DV, Umpire DF, Rakhra KS, Jibri Z, Belmar GAS. Distal radioulnar joint: Normal anatomy, imaging of common disorders, and injury classification. Radiographics. 2023;43(1):e220109. [DOI] [PubMed] [Google Scholar]
- 2. Jain S, Modi P, Dayma RL, Mishra S. Clinical outcome of arthroscopic suture versus screw fixation in tibial avulsion of the anterior cruciate ligament in skeletally mature patients. J Orthop. 2023;35:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mancini MR, Horinek JL, Phillips CJ, Denard PJ. Arthroscopic rotator cuff repair: a review of surgical techniques and outcomes. Clin Sports Med. 2023;42(1):81–94. [DOI] [PubMed] [Google Scholar]
- 4. Guevara JA, Entezari V, Ho JC, Derwin KA, Iannotti JP, Ricchetti ET. An update on surgical Management of the Repairable Large‐to‐Massive Rotator Cuff Tear. J Bone Joint Surg Am. 2020;102(19):1742–1754. [DOI] [PubMed] [Google Scholar]
- 5. Yuan T, Yang S, Qian H, Lai C, Jiang H, Meng J, et al. All‐inside technique versus in situ transtendon repair for Ellman III partial articular supraspinatus tendon avulsion. J Shoulder Elbow Surg. 2023;32(1):24–32. [DOI] [PubMed] [Google Scholar]
- 6. Aydin N, Karaismailoglu B, Gurcan M, Ozsahin MK. Arthroscopic double‐row rotator cuff repair: a comprehensive review of the literature. Sicot J. 2018;4:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lapner P, Li A, Pollock JW, Zhang T, McIlquham K, McRae S, et al. A multicenter randomized controlled trial comparing single‐row with double‐row fixation in arthroscopic rotator cuff repair: long‐term follow‐up. Am J Sports Med. 2021;49(11):3021–3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huang AL, Thavorn K, van Katwyk S, MacDonald P, Lapner P. Double‐row arthroscopic rotator cuff repair is more cost‐effective than single‐row repair. J Bone Joint Surg Am. 2017;99(20):1730–1736. [DOI] [PubMed] [Google Scholar]
- 9. Noyes MP, Denard PJ. Outcomes following double‐row and medial double‐pulley rotator cuff repair. Orthopedics. 2021;44(1):e125–e130. [DOI] [PubMed] [Google Scholar]
- 10. Yoon JS, Kim SJ, Choi YR, Kim SH, Chun YM. Arthroscopic repair of the isolated subscapularis full‐thickness tear: single‐ versus double‐row suture‐bridge technique. Am J Sports Med. 2019;47(6):1427–1433. [DOI] [PubMed] [Google Scholar]
- 11. Tan RK. A review of the role of magnetic resonance imaging in the evaluation of shoulder impingement syndrome and rotator cuff tendon tears. Ann Acad Med Singapore. 1998;27(2):243–247. [PubMed] [Google Scholar]
- 12. Wu K, Su X, Roche SJL, Held MFG, Yang H, Dunn RN, et al. Relationship between the lateral acromion angle and postoperative persistent pain of distal clavicle fracture treated with clavicle hook plate. J Orthop Surg Res. 2020;15(1):217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lin HY, Wong PK, Ho WP, Chuang TY, Liao YS, Wong CC. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion‐dynamic sonographic evaluation. J Orthop Surg Res. 2014;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Banas MP, Miller RJ, Totterman S. Relationship between the lateral acromion angle and rotator cuff disease. J Shoulder Elbow Surg. 1995;4(6):454–461. [DOI] [PubMed] [Google Scholar]
- 15. Hanciau FA, Silva MAM, Martins FS, Ogliari A. Association clinical‐radiographic of the acromion ÍNDEX and the lateral acromion angle. Rev Bras Ortop. 2012;47(6):730–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gerber C, Catanzaro S, Betz M, Ernstbrunner L. Arthroscopic correction of the critical shoulder angle through lateral acromioplasty: a safe adjunct to rotator cuff repair. Art Ther. 2018;34(3):771–780. [DOI] [PubMed] [Google Scholar]
- 17. Cole BJ, ElAttrache NS, Anbari A. Arthroscopic rotator cuff repairs: an anatomic and biomechanical rationale for different suture‐anchor repair configurations. Art Ther. 2007;23(6):662–669. [DOI] [PubMed] [Google Scholar]
- 18. Burkhart SS, Lo IK. Arthroscopic rotator cuff repair. J Am Acad Orthop Surg. 2006;14(6):333–346. [DOI] [PubMed] [Google Scholar]
- 19. Saridakis P, Jones G. Outcomes of single‐row and double‐row arthroscopic rotator cuff repair: a systematic review. J Bone Joint Surg Am. 2010;92(3):732–742. [DOI] [PubMed] [Google Scholar]
- 20. Nyffeler RW, Werner CM, Sukthankar A, Schmid MR, Gerber C. Association of a large lateral extension of the acromion with rotator cuff tears. J Bone Joint Surg Am. 2006;88(4):800–805. [DOI] [PubMed] [Google Scholar]
- 21. Liu CT, Miao JQ, Wang H, an Ge H, Wang XH, Cheng B. The association between acromial anatomy and articular‐sided partial thickness of rotator cuff tears. BMC Musculoskelet Disord. 2021;22(1):760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Meissner‐Haecker A, Contreras J, Valenzuela A, Delgado B, Taglioni A, de Marinis R, et al. Critical shoulder angle and failure of conservative treatment in patients with atraumatic full thickness rotator cuff tears. BMC Musculoskelet Disord. 2022;23(1):561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Miyazaki AN, Itoi E, Sano H, Fregoneze M, Santos PD, da Silva LA, et al. Comparison between the acromion index and rotator cuff tears in the Brazilian and Japanese populations. J Shoulder Elbow Surg. 2011;20(7):1082–1086. [DOI] [PubMed] [Google Scholar]
- 24. Altintas B, Kääb M, Greiner S. Arthroscopic lateral acromion resection (ALAR) optimizes rotator cuff tear relevant scapula parameters. Arch Orthop Trauma Surg. 2016;136(6):799–804. [DOI] [PubMed] [Google Scholar]
- 25. Beeler S, Hasler A, Getzmann J, Weigelt L, Meyer DC, Gerber C. Acromial roof in patients with concentric osteoarthritis and massive rotator cuff tears: multiplanar analysis of 115 computed tomography scans. J Shoulder Elbow Surg. 2018;27(10):1866–1876. [DOI] [PubMed] [Google Scholar]
- 26. Pang X, Hao Y, Ma L, Zhuo L, Liu L, Feng J. Subacute combined degeneration of the spinal cord concurrent with acute pulmonary embolism: a case report. J Int Med Res. 2021;49(5):3000605211016815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full‐thickness rotator cuff repair: single‐row versus dual‐row fixation. Arthroscopy: the journal of arthroscopic & related surgery: official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2005;21(11):1307–16. [DOI] [PubMed] [Google Scholar]
- 28. Hohmann E, Tetsworth K. Glenoid version and inclination are risk factors for anterior shoulder dislocation. J Shoulder Elbow Surg. 2015;24(8):1268–1273. [DOI] [PubMed] [Google Scholar]
- 29. Li C, Zhang H, Bo X, Zha G, Pang Y, Zheng X, et al. Arthroscopic release combined with single‐row fixation or double‐row suture bridge fixation in patients with traumatic supraspinatus tear and adhesive capsulitis non‐responsive to conservative management: a prospective randomized trial. Orthop Traumatol Surg Res. 2021;107(4):102828. [DOI] [PubMed] [Google Scholar]
- 30. Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;155:7–20. [PubMed] [Google Scholar]
- 31. Booker S, Alfahad N, Scott M, Gooding B, Wallace WA. Use of scoring systems for assessing and reporting the outcome results from shoulder surgery and arthroplasty. World J Orthop. 2015;6(2):244–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kovacevic D, Suriani RJ Jr, Grawe BM, Yian EH, Gilotra MN, Hasan SA, et al. Management of irreparable massive rotator cuff tears: a systematic review and meta‐analysis of patient‐reported outcomes, reoperation rates, and treatment response. J Shoulder Elbow Surg. 2020;29(12):2459–2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther. 2014;44(1):30–39. [DOI] [PubMed] [Google Scholar]
- 34. Beaton DE, Davis AM, Hudak P, Mcconnell S. The DASH (disabilities of the arm, shoulder and hand) outcome measure: what do we know about it now? Brit J Hand Therapy. 2001;6(4):109–118. [Google Scholar]
- 35. Dines JS, Bedi A, ElAttrache NS, Dines DM. Single‐row versus double‐row rotator cuff repair: techniques and outcomes. J Am Acad Orthop Surg. 2010;18(2):83–93. [DOI] [PubMed] [Google Scholar]
- 36. Hein J, Reilly JM, Chae J, Maerz T, Anderson K. Retear rates after arthroscopic single‐row, double‐row, and suture bridge rotator cuff repair at a minimum of 1 year of imaging follow‐up: a systematic review. Art Ther. 2015;31(11):2274–2281. [DOI] [PubMed] [Google Scholar]
- 37. Maalouly J, Aouad D, Tawk A, el Rassi G. Modified double‐row suture bridge technique with double‐row biceps tenodesis for massive rotator cuff tear. Arthrosc Tech. 2020;9(6):e829–e835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tanpowpong T, Itthipanichpong T, Limskul D. How to maximize suture tension in double‐row suture‐bridge rotator cuff repair? Arthrosc Tech. 2021;10(10):e2207–e2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ying ZM, Lin T, Yan SG. Arthroscopic single‐row versus double‐row technique for repairing rotator cuff tears: a systematic review and meta‐analysis. Orthop Surg. 2014;6(4):300–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ. Clinical and structural outcomes after arthroscopic single‐row versus double‐row rotator cuff repair: a systematic review and meta‐analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23(4):586–597. [DOI] [PubMed] [Google Scholar]
- 41. Xiao M, Cohen SA, Cheung EV, Abrams GD, Freehill MT. Arthroscopic single and double row repair of isolated and combined subscapularis tears result in similar improvements in outcomes: a systematic review. Art Ther. 2022;38(1):159–173. [DOI] [PubMed] [Google Scholar]
- 42. Yilmazturk K, Birinci M, Kuyucu E, Bulbul AM. Is shoulder geometry important for rotator cuff tears? Int J Clin Pract. 2021;75(12):e15005. [DOI] [PubMed] [Google Scholar]
- 43. Balke M, Schmidt C, Dedy N, Banerjee M, Bouillon B, Liem D. Correlation of acromial morphology with impingement syndrome and rotator cuff tears. Acta Orthop. 2013;84(2):178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Liu HX, Xu XX, Xu DL, Hu YZ, Pan XY, Yu Z, et al. The acromion‐greater tuberosity impingement index: a new radiographic measurement and its association with rotator cuff pathology. J Orthop Surg (Hong Kong). 2020;28(1):13348. [DOI] [PubMed] [Google Scholar]
- 45. Watanabe A, Ono Q, Nishigami T, Hirooka T, Machida H. Association between the critical shoulder angle and rotator cuff tears in Japan. Acta Med Okayama. 2018;72(6):547–551. [DOI] [PubMed] [Google Scholar]
- 46. Zaid MB, Young NM, Pedoia V, Feeley BT, Ma CB, Lansdown DA. Anatomic shoulder parameters and their relationship to the presence of degenerative rotator cuff tears and glenohumeral osteoarthritis: a systematic review and meta‐analysis. J Shoulder Elbow Surg. 2019;28(12):2457–2466. [DOI] [PubMed] [Google Scholar]
- 47. Li H, Chen Y, Chen J, Hua Y, Chen S. Large critical shoulder angle has higher risk of tendon Retear after arthroscopic rotator cuff repair. Am J Sports Med. 2018;46(8):1892–1900. [DOI] [PubMed] [Google Scholar]
- 48. Park HB, Gwark JY, Kwack BH, Na JB. Are any radiologic parameters independently associated with degenerative postero‐superior rotator cuff tears? J Shoulder Elbow Surg. 2021;30(8):1856–1865. [DOI] [PubMed] [Google Scholar]
- 49. Guo X, Ou M, Yi G, Qin B, Wang G, Fu S, et al. Correction between the morphology of acromion and acromial angle in Chinese population: a study on 292 Scapulas. Biomed Res Int. 2018;2018:3125715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Andrade R, Correia AL, Nunes J, Xará‐Leite F, Calvo E, Espregueira‐Mendes J, et al. Is bony morphology and morphometry associated with degenerative full‐thickness rotator cuff tears? A Systematic Review and Meta‐Analysis. Arthroscopy. 2019;35(12):3304–3315. [DOI] [PubMed] [Google Scholar]
- 51. Viskontas DG, MacDermid JC, Drosdowech DS, Garvin GJ, Romano WM, Faber KJ. Reliability and comparison of acromion assessment techniques on X‐ray and magnetic resonance imaging (reliability of acromion assessment techniques). Can Assoc Radiol J. 2005;56(4):238–244. [PubMed] [Google Scholar]
- 52. Thiesemann S, Kirchner F, Fal MF, Albers S, Kircher J. Anterolateral acromioplasty does not change the critical shoulder angle and acromion index in a clinically relevant amount. Art Ther. 2022;38(11):2960–2968. [DOI] [PubMed] [Google Scholar]
- 53. Balke M, Liem D, Greshake O, Hoeher J, Bouillon B, Banerjee M. Differences in acromial morphology of shoulders in patients with degenerative and traumatic supraspinatus tendon tears. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2200–2205. [DOI] [PubMed] [Google Scholar]
- 54. Moor BK, Bouaicha S, Rothenfluh DA, Sukthankar A, Gerber C. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint? a radiological study of the critical shoulder angle. Bone Joint J. 2013;95‐b(7):935–941. [DOI] [PubMed] [Google Scholar]
- 55. Nyffeler RW, Meyer DC. Acromion and glenoid shape: why are they important predictive factors for the future of our shoulders? EFORT Open Rev. 2017;2(5):141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Xie L, Xu X, Ma B, Liu H. A high acromion‐greater tuberosity impingement index increases the risk of retear after arthroscopic rotator cuff repair. J Orthop Surg (Hong Kong). 2022;30(1):10225536221092219. [DOI] [PubMed] [Google Scholar]
- 57. Abrams GD, Gupta AK, Hussey KE, Tetteh ES, Karas V, Bach BR Jr, et al. Arthroscopic repair of full‐thickness rotator cuff tears with and without acromioplasty: randomized prospective trial with 2‐year follow‐up. Am J Sports Med. 2014;42(6):1296–1303. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.


