Abstract
Background
Evidence suggests diabetes management was negatively impacted early in the pandemic. However, the impact of the pandemic on key healthcare services for diabetes control and diabetes self-management practices is less known. We examined changes in diabetes care and management practices before and during the COVID-19 pandemic.
Methods
Population-based data regarding 4 diabetes-related healthcare engagement and 4 self-management indicators were obtained from adults with diabetes surveyed in 19 US States and Washington DC through the Behavioral Risk Factor Surveillance System. Using logistic regression, we estimated changes in the prevalence of each indicator, overall and by sociodemographic subgroups, before (2019; n = 15,307) and during (2021; n = 13,994) the COVID-19 pandemic.
Results
Between 2019 and 2021, the prevalence of biannual HbA1c tests reduced by 2.6 percentage points (pp, 95% CI :−4.8, −0.4), from 75.4–73.1%, and prevalence of annual eye exams fell by 4.0 pp (−6.2, −2.8), from 72.2–68.7%. The composite indicator of engagement with healthcare for diabetes control fell by 3.5 pp (−5.9, −1.1), from 44.9–41.9%. Reductions in engagement with healthcare were largely seen across sex, age, education, employment status, marital status, insurance status, and urbanicity; and were more pronounced among those aged 18–34 and the uninsured. Reductions in engagement with healthcare were seen in several states, with Delaware and Washington DC reporting the largest decrease. Of self-management behaviors, we only observed change in avoidance of smoking, an increase of 2.0 pp (0.4, 3.6) from 84.7–87.1%.
Conclusions
The pandemic had mixed impacts on diabetes care and self-management. The findings suggest a deterioration of the uptake of evidence-based, preventive health services requiring laboratory services and clinical examination for diabetes control during the pandemic. On the other hand, smoking rates decreased, suggesting potential positive impacts of the pandemic on health behaviors in people with diabetes.
Keywords: Diabetes management, COVID-19, health services
Background
Diabetes is a chronic condition that requires both continual engagement with healthcare and routine self-management, without which poor glycemic control and diabetes-related complications are more likely1. With respect to engagement with healthcare, the American Diabetes Association (ADA) recommends that at minimum diabetes care includes biannual glycated hemoglobin checks from a health professional2, annual foot and eye exams3. For routine self-management of diabetes, the ADA recommends daily foot checks3, regular physical activity,4 tobacco avoidance5, and participating in educational classes to manage diabetes6.
People with diabetes are at particularly high risk for severe outcomes following COVID-19 disease. Simultaneously, diabetes care and self-management in this high-risk group may have been negatively impacted by the pandemic and associated policies to curb viral transmission. Disruptions to health services7,8, changes to routine care8, and fear of getting severely ill from the virus9 may have prevented some individuals living with diabetes from getting the care they need during the COVID-19 pandemic. Lockdowns and social distancing may have impacted diabetes self-management behaviors such as physical activity10. Evidence suggests diabetes management was negatively impacted early in the pandemic. For instance, studies have shown a decrease in blood glucose testing11–13 and health professional visits for diabetes during the COVID-19 pandemic in the US11,14 in select samples. However, the impact of the pandemic on key healthcare services for diabetes control and diabetes self-management practices is less known, especially in population-based studies covering diverse geographies. Furthermore, it is unclear if there was variation in engagement and self-management across different socio-demographic groups, some of whom may have been resilient to the economic impacts of the pandemic.
Identifying the indirect impact of the pandemic on diabetes management and care is critical to understanding the needs and requirements of those living with diabetes as we move into post-public health emergency recovery. Using the Behavioral Risk Factor Surveillance System (BRFSS), we examined changes in four indicators of engagement with healthcare and five indicators of self-management practices for diabetes— before (2019) and during (2021) the COVID-19 pandemic among people living diabetes.
Materials and Methods
Data and sample
The BRFSS is a state-based system of health-related telephone surveys that collect data about non-institutionalized US residents’ health-related risk behaviors, chronic health conditions, and use of preventive services. We used publicly available data from the 2019 and 2021 BRFSS adult samples to obtain measures of engagement with healthcare and diabetes self-management and socio-demographic characteristics before and during the pandemic, respectively. The overall response rates for BRFSS 2019 and 2021 were 49.4% and 44.0% respectively. The combined surveys included 112,323 respondents living with diabetes (excluding gestational diabetes) in the District of Columbia (DC) and the 50 US states. The analysis was further restricted to 37,639 individuals with diabetes in states that asked information on diabetes care practices in both 2019 and 2021 samples. Nineteen states—Alaska, Delaware, Illinois, Indiana, Iowa, Kentucky, Maine, Michigan, Minnesota, Montana, New Hampshire, New Mexico, North Carolina, North Dakota, Pennsylvania, Texas, Virginia, Wisconsin, Wyoming, and the District of Columbia (Washington DC), collected data on needed indicators. Among respondents surveyed in states covering the diabetes module, 22% were excluded due to missing data on any outcome and socio-demographic characteristic, resulting in a final unweighted analytic sample size of 29,301 across the two surveys. The distribution of the socio-demographic characteristics in the 1. total BRFSS sample, 2. among all adults with diabetes (excluding gestational diabetes), 3. states that were asked diabetes-specific questions, and 4. our analytic sample is shown in Additional File 1 in the Supplement.
Variables and description
Pandemic status
Data from participants surveyed in BRFSS 2019 were classified as pre-pandemic and data from participants surveyed in BRFSS 2021 were classified as post-pandemic.
Outcomes
Diabetes care practices included four indicators of engagement with healthcare and four indicators of self-management of diabetes, all measured as binary variables (yes/no) and derived from the measures proposed by the ADA. Engagement with healthcare included 1. biannual health professional visits for diabetes, 2. biannual HbA1c testing by a health professional, 3. annual foot exams for sores or irritations by a health professional, and 4. having had an eye exam in which pupils were dilated. Self-management of diabetes included 1. daily glucose self-monitoring if on insulin, 2. checking feet for sores or irritations daily, including by family members or friends, 3. participating in any physical activities or exercise in the past 30 days, and 4. avoiding smoking. The BRFSS survey questions for each indicator are shown in Additional File 2 in the Supplement. We further created a composite measure which indicated whether an individual engaged in all applicable practices for engagement with healthcare for diabetes control.
Socio-demographic characteristics
Demographic characteristics included sex (male/female), age (divided into five groups; 18–34, 35–44, 45–54, 55–64, and 65 and older), race/ethnicity (as non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, and Other), and marital status (married or living with a partner). Socioeconomic characteristics included educational attainment (classified as high school or less, some college, or 4 or more years of college), urbanicity (metropolitan or nonmetropolitan), employment status (employed, retired, unemployed/not working), and health insurance (yes or no).
STATISTICAL ANALYSIS
We first described the distribution of the socio-demographic subgroups by pandemic status. We then described the prevalence of diabetes care practices (both engagement with healthcare and self-management) before and during the pandemic. The change in the prevalence of the outcomes were predicted marginal differences computed between independent samples of US adults before and during the pandemic, defined by survey timepoint, from the logistic regression models15. Pre-pandemic served as the reference group. Both unadjusted and adjusted prevalence differences were estimated. Adjusted estimates accounted for age, sex, race, marital status, urbanicity, insurance status, education level, and employment status. Similarly, we examined the prevalence of engagement with healthcare composite before and during the pandemic among each level of the socio-demographic subgroups and by states with data available on diabetes-specific care modules. All data were analyzed using SAS version 9.4 and SUDAAN version 11.0.1, accounting for the complex survey design.
Results
Socio-demographic characteristics of respondents in states that administered diabetes-care modules before (2019) and during the pandemic (2021) are shown in Table 1. The demographic composition of adults surveyed before the pandemic and during the pandemic was similar. Respondents with self-reported diabetes had a relatively even sex distribution (49.3% female pre-pandemic; 48% female pandemic), a large proportion of those aged 65 years or older (43.0% pre-pandemic; 44.1% pandemic), and a greater share of Non-Hispanic White individuals (67.0% pre-pandemic; 65.4% pandemic).
Table 1.
Socio-demographic characteristics of adults living with diabetes, pre- and during pandemic
| Pre-pandemica 2019 | Pandemicb 2021 | |
|---|---|---|
| Overall unweighted n | 15,307 | 13,994 |
| Sex | ||
| Female | 49.3 (47.7, 50.9) | 48.0 (46.2, 49.8) |
| Age | ||
| 18–34 | 4.2 (3.6, 5.0) | 4.3 (3.5, 5.3) |
| 35–44 | 7.9 (6.8, 9.1) | 8.1 (7.0, 9.3) |
| 45–54 | 17.1 (15.8, 18.4) | 17.6 (16.1, 19.1) |
| 55–64 | 27.8 (26.4, 29.3) | 25.9 (24.4, 27.5) |
| 65 and above | 43.0 (41.4, 44.6) | 44.1 (42.4, 45.9) |
| Race/ethnicity | ||
| Non-Hispanic White | 67.0 (65.2, 68.7) | 65.4 (63.5, 67.3) |
| Non-Hispanic Black | 14.2 (13.1, 15.4) | 15.7 (14.4, 17.1) |
| Hispanic | 13.9 (12.4, 15.6) | 14.6 (12.9, 16.4) |
| Non-Hispanic Asian | 1.8 (1.4, 2.5) | 1.7 (1.3, 2.2) |
| Other | 3.1 (2.7, 3.5) | 2.6 (2.2, 3.0) |
| Education | ||
| High school or less | 46.5 (44.9, 48.2) | 44.5 (42.7, 46.4) |
| Some college | 33.5 (31.9, 35.0) | 33.8 (32.1, 35.5) |
| 4 years of college or more | 20.0 (19.0, 21.1) | 21.6 (20.4, 22.9) |
| Employment status | ||
| Employed | 37.0 (35.4, 38.6) | 36.3 (34.5, 38.0) |
| Retired | 37.8 (36.2, 39.3) | 39.1 (37.4, 40.8) |
| Unemployed/not working | 25.3 (23.9, 26.7) | 24.7 (23.0, 26.4) |
| Married or living with a partner | 57.7 (56.1, 59.3) | 59.2 (57.4, 60.9) |
| Insured | 92.7 (91.6, 93.6) | 93.8 (92.2, 95.0) |
| Metropolitan | 76.7 (75.6, 77.9) | 77.7 (76.3, 79.0) |
BRFSS 2019
BRFSS 2021
P-value comparing difference in characteristics between adults surveyed pre pandemic and during the pandemic were as follows; sex (p = 0.0916); age (p = 0.4657); race/ethnicity (p = 0.1668); education (p = 0.0527); employment status (p = 0.3561); marital status (p = 0.1373); insurance status (p = 0.1120); urbanicity (p = 0.2894)
Table 2 shows the prevalence of diabetes care practices before (2019) and during (2021) the pandemic. Receipt of an annual eye exam dropped from 72.2% (95% Confidence Interval, CI: 70.7, 73.6) before the pandemic to 68.7% (95% CI: 66.9, 70.5) during the pandemic. The adjusted prevalence difference (aPD) between pre- and during pandemic for having an eye exam in the past year was − 4.0 (95% CI: −6.2, −2.8) percentage points (pp) after accounting for differences in socio-demographic characteristics of the two samples. Receiving biannual HbA1c tests reduced from 75.4% (95% CI: 73.9, 76.8) before the pandemic to 73.1% (95% CI: 71.3, 74.7) during the pandemic (aPD= −2.6 pp [95% CI: −4.8, −0.4]). Among self-management practices for diabetes, the prevalence of avoiding smoking increased from 84.7% (95% CI: 83.5, 85.9) before the pandemic to 87.1% (95% CI: 85.9, 88.2) during the pandemic (aPD = 2.0 pp [95% CI: 0.4, 3.6]).
Table 2.
Prevalence of diabetes care and management practices among adults with diabetes, pre- and during pandemic
| Pre pandemica | Pandemicb | |||
|---|---|---|---|---|
| Unweighted n | 14,972 | 13,647 | ||
| % (95% CI) | % (95% CI) | PD (95% CI) | aPDc (95% CI) | |
| Diabetes care practices | ||||
| Engagement with healthcare | ||||
| Biannual health professional visits for diabetes | 75.9 (74.5, 77.3) | 74.2 (72.7, 75.7) | −1.7 (−3.7, 0.3) | −1.9 (−3.9, 0.1) |
| Biannual HbA1c tests | 75.4 (73.9, 76.8) | 73.1 (71.3, 74.7) | −2.3 (−4.5, −0.1) | −2.6 (−4.8, −0.4) |
| Annual foot exam | 78.3 (76.9, 79.6) | 77.3 (75.7, 78.7) | −1.0 (−3.0, 1.0) | −1.4 (−3.4, 0.6) |
| Annual eye exam | 72.2 (70.7, 73.6) | 68.7 (66.9, 70.5) | −3.5 (−5.9, −1.1) | −4.0 (−6.2, −1.8) |
| Self-management | ||||
| Exercise in past 30 days | 61.7 (60.1, 63.2) | 61.8 (60.0, 63.6) | 0.1 (−2.3, 2.5) | −0.4 (−2.8, 2.0) |
| Not current smoker | 84.7 (83.5, 85.9) | 87.1 (85.9, 88.2) | 2.4 (0.8, 4.0) | 2.0 (0.4, 3.6) |
| Daily foot checks | 57.6 (56.0, 59.2) | 59.6 (57.8, 61.4) | 2.0 (−0.4, 4.4) | 2.1 (−0.3, 4.5) |
| Daily glucose self-monitoring‡ | 87.9 (85.8, 89.7) | 89.2 (87.5, 90.7) | 1.3 (−1.2, 3.8) | 3.3 (−6.1, 12.7) |
BRFSS 2019
BRFSS 2021
Restricted to adults using insulin (n = 5,159, pre-pandemic; n = 4599, pandemic)
Consists of all the following healthcare practices- biannual health professional visits for diabetes, biannual HbA1c tests, annual foot, and eye exams
Adjusted for age, sex, race, urbanicity, insurance status, employment status, education level, marital status
Error bars represent 95% CI of the adjusted prevalence difference
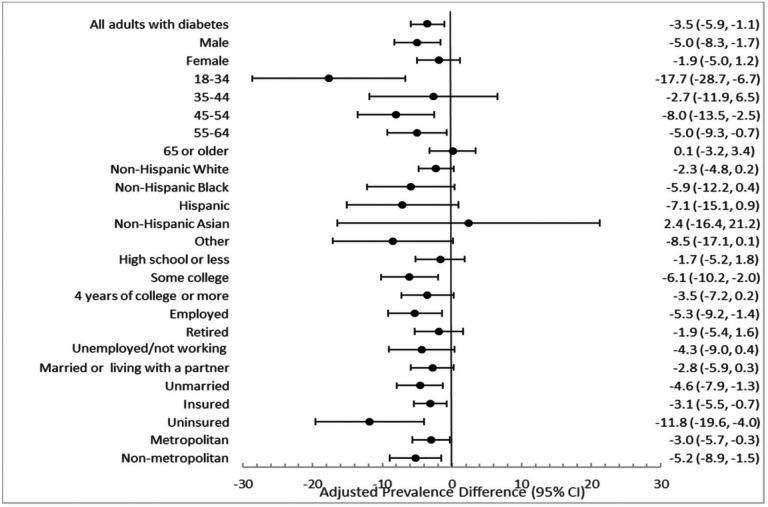
Between the pre-pandemic to pandemic period, there was a reduction of 3.5 pp (95% CI: −5.9, −1.1) from 44.9% (95% CI: 43.3, 46.5) to 41.9% (95% CI: 40.1, 43.7) in the composite measure of 4 indicators of engagement with healthcare in all people with diabetes (Fig. 1; Additional File 3 in the Supplement). This decrease was consistently observed across 23 of 24 socio-demographic groups, with statistically significant decreases in healthcare engagement from pre-pandemic to during the pandemic in 12 of 24 socio-demographic subgroups. The largest reductions were among those aged 18–34 years (aPD=−17.7 [95% CI: −28.7, −6.7]), from 38.6% (95% CI: 30.6, 47.2) before the pandemic to 23.2% (95% CI: 18.0, 34.1) (Fig. 1; Additional File 3 in the Supplement). Individuals who were uninsured saw the second largest decrease (aPD= −11.8 [95% CI: −19.6, −4.0]), from 23.6% (95% CI: 18.1, 30.2) before the pandemic to 13.0% (95% CI: 8.1, 20.3) during the pandemic.
Figure 1. Adjusted prevalence difference (aPD) between 2021 and 2019 for all applicable practices for engagement with healthcare*, among adults with diabetes overall and by socio-demographic subgroups.
*Consists of all the following healthcare practices- biannual health professional visits for diabetes, biannual HbA1c tests, annual foot, and eye exams
aAdjusted for age, sex, race, urbanicity, insurance status, employment status, education level, marital status
Error bars represent 95% CI of the adjusted prevalence difference
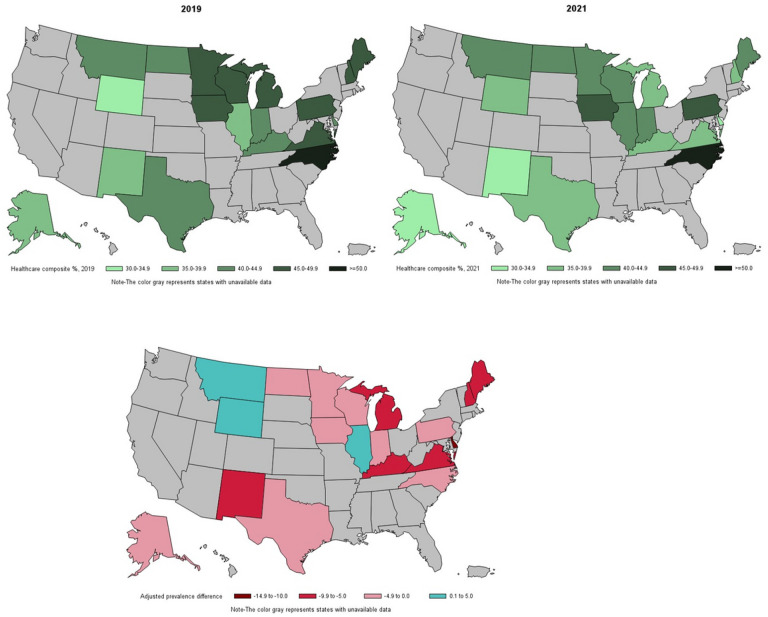
Among 19 US states and Washington DC with data on diabetes-specific care modules, 7 saw a significant decrease in the engagement with healthcare composite measure from pre-pandemic to during the pandemic. These included Delaware, Washington DC, Maine, Michigan, New Hampshire, New Mexico, and Virginia (Fig. 2; Additional File 4 in the Supplement). Delaware and Washington DC saw the largest reduction in the engagement with healthcare (−11.5 [95% CI: −19.7, −3.3] and − 12.8 [95% CI: −24.2, −1.4] respectively). North Carolina reported the highest engagement with health care both pre-pandemic and during pandemic (> 50%). No states experienced a significant increase in engagement with healthcare.
Figure 2. Prevalence of adults with diabetes engaging in all healthcare indicators and adjusted prevalence difference (aPD) between 2021 and 2019.
*Adjusted for age, sex, race, urbanicity, insurance status, employment status, education level, marital status
Discussion
Corresponding to the COVID-19 pandemic, between 2019 and 2021, US adults with diabetes reported reductions in engagement with healthcare, including a 2.6 pp decrease in biannual HbA1c tests and 4 pp decrease annual eye exams. On the other hand, the proportion of people with diabetes who reported not smoking increased while all other self-management practices for diabetes control stayed similar. Reduction in engagement with healthcare was seen across nearly all socio-demographic subgroups and was more pronounced among those aged 18–34 and the uninsured. Similarly, we observed reductions in engagement with healthcare in 18 of 20 states, with Delaware and Washington DC reporting the largest decrease. These findings suggest that the pandemic had a negative impact on uptake of diabetes related health services – including HbA1c testing and eye examination—with little impact on diabetes self-management behaviors at home.
Existing studies lack data on the impact of the COVID-19 pandemic on other specific components of diabetes care, such as annual eye exams; however, this study presents a unique opportunity to understand the ramifications caused by the pandemic on these relatively unexplored components. In our study, we saw a decrease in having an annual eye exam during the pandemic. The limited existing evidence suggests that the pandemic negatively impacted eye exams as part of diabetes care16. Diabetic retinopathy screening was also severely impacted by the pandemic, especially in areas of high SARS-CoV-2 transmission17. The decline in receiving eye exams is especially concerning due to the importance of regular screening in preventing diabetic retinopathy and severe vision loss18.
Unlike annual health exams, there was no change in biannual health professional visits for diabetes. A possible explanation for this is the rise in telehealth during the pandemic, and its potential to replace routine healthcare visits not requiring specialty examinations. Yet, despite no change in routine healthcare visits, there was a reduction in the proportion receiving HbA1c tests. Data from the nationally representative National Health Interview Survey (NHIS) also indicated a decrease in blood glucose testing during the pandemic13. In serial cross-sectional NHIS, the prevalence of annual HbA1c checking in US adults with diabetes reduced from 96.8% in 2019 to 94.2% in 2021, suggesting that the drop in glucose checking by health professionals may have extended beyond the first year of the pandemic12. The ADA recommends at minimum, biannual HbA1c testing in those with diabetes, and we observed a reduction in biannual HbA1c testing, from 75.9% in 2019 to 74.2% in 2021. Whether receipt of biannual healthcare visits in the absence of HbA1c testing benefits people with diabetes may also be explored in future studies.
Overall healthcare engagement was investigated through a composite of biannual health professional visits for diabetes, biannual HbA1c tests, annual foot, and eye exams. The magnitude of reduction in overall healthcare engagement was largest in younger adults. Those aged 18–34 years reported a 17.7 pp decrease in healthcare engagement, compared with the national average of 3.5 pp. Younger age groups have reported elevated levels of stress and anxiety due to reasons such as poor sleep19, and education-related challenges20 during the COVID-19 pandemic, which may have contributed to their lack of visitation to a health professional. Additionally, younger people with diabetes have historically more likely been non-adherent to diabetes complication screening guidelines such as retinal screening, and this reluctance to attend screening visits could have been exacerbated during the pandemic21,22.
Uninsured adults with diabetes reported an 11.8 pp decrease in engagement with healthcare, the second largest reduction after younger adults. It has previously been shown that uninsured individuals had a lower odds of having a primary care encounter during the pandemic, which may put them at risk for uncontrolled HbA1c levels23.
Notably, there were no statistically significant differences in the magnitude of reduction in healthcare engagement by race. Both Non-Hispanic Black and Hispanic race and ethnicity saw a large decrease in engagement with healthcare, although the prevalence between pre and during pandemic was not statistically significant. However, adults classified in the Other race group reported a large statistical decrease, suggesting the pandemic’s negative impact on health services among minority groups that largely comprise this category, including American Indian/Alaskan Native and Multiracial groups.
While the reduction in healthcare engagement was also consistently observed across surveyed states, 7 states reported statistically significant reductions of 5 pp or larger: Delaware, Maine, Michigan, New Hampshire, New Mexico, Virginia, and Washington DC. Further investigation regarding factors contributing to these large declines is warranted.
Our study has several strengths. First, we report key differences in practices for engagement with healthcare that are specific to diabetes, such as receiving biannual HbA1c tests and annual eye exams, pre and during pandemic. Second, our data afforded us the opportunity to examine changes in previously unexplored diabetes self-management behaviors, such as daily foot checks and daily glucose monitoring. Third, we investigated differences in pandemic impacts on diabetes healthcare services by socio-demographic subgroup, addressing major concerns around health equity in the pandemic. Fourth, we reported changes in diabetes healthcare services by US states.
Several limitations of this study should be acknowledged. We had to limit our analysis to the states which had data for the diabetes care and management practices in both 2019 and 2021; of note, is the fact that the study sample did not include states in the Southeastern US, which report the highest prevalence of diabetes24. Relatedly, state-level and subgroup analyses among people with diabetes may have been underpowered to detect statistically significant changes. Individuals with the worst controlled diabetes may have died early in the pandemic25,26 eliminating them from this analysis. Therefore, our results may have been conservative and underestimate the lack of self-management and engagement with healthcare practices. BRFSS data are self-reported and subject to recall bias. We were not able to distinguish diabetes type.
Conclusion
Among US adults with diabetes residing 19 US states and Washington DC, we found reductions in having biannual HbA1c tests, annual eye exams, and participation in diabetes self-management education during the COVID-19 pandemic. Reductions were consistent across socio-demographics and across states. The findings suggest a deterioration of the uptake of evidence-based, preventive health services requiring laboratory services and clinical examination for diabetes control during the pandemic. In contrast, most measures of at-home self-management diabetes behaviors remained comparable before and during the pandemic, while smoking rates decreased. Examining the indirect impact of the pandemic on diabetes care is critical in understanding the needs and requirements of those living with diabetes as we move into a post-pandemic environment. If these changes are further sustained, healthcare systems may need to introduce new measures to rehabilitate diabetes care practices in the post-pandemic era.
Funding
This work was supported by was supported by the National Institute Of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number P30DK111024. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding Statement
This work was supported by was supported by the National Institute Of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number P30DK111024. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Ethics approval and consent to participate
This study used publicly available data containing no personal identifying information and is therefore deemed not human subjects research by the Emory IRB.
Competing Interests
The authors declare that they have no competing interests.
Supplementary Files
- Supplement.docx
Contributor Information
Kushagra Vashist, Emory University.
Jennifer K. Frediani, Emory University Nell Hodgson Woodruff School of Nursing
Mary Beth Weber, Emory University.
Mohammed K. Ali, Emory University
K. M. Venkat Narayan, Emory University.
Shivani A. Patel, Emory University
Availability of data and materials
The datasets generated and/or analyzed during the current study are available on the Centers for Disease Control and Prevention (CDC) website and can be accessed through this link-https://www.cdc.gov/brfss/index.html
References
- 1.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12:14. 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ElSayed NA, Aleppo G, Aroda VR, et al. 6. Glycemic Targets: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement1):97–S110. 10.2337/dc23-S006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ElSayed NA, Aleppo G, Aroda VR, et al. 12. Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement1):203–S215. 10.2337/dc23-S012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ElSayed NA, Aleppo G, Aroda VR, et al. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement1):128–S139. 10.2337/dc23-S008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Standards of Care in Diabetes—2023 Abridged for Primary Care Providers. Clin Diabetes. 2022;41(1):4–31. 10.2337/cd23-as01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.ElSayed NA, Aleppo G, Aroda VR, et al. 1. Improving Care and Promoting Health in Populations: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement1):10–S18. 10.2337/dc23-S001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gregg EW, Sophiea MK, Weldegiorgis M. Diabetes and COVID-19: Population Impact 18 Months Into the Pandemic. Diabetes Care. 2021;44(9):1916–23. 10.2337/dci21-0001. [DOI] [PubMed] [Google Scholar]
- 8.Hartmann-Boyce J, Morris E, Goyder C, et al. Diabetes and COVID-19: Risks, Management, and Learnings From Other National Disasters. Diabetes Care. 2020;43(8):1695–703. 10.2337/dc20-1192. [DOI] [PubMed] [Google Scholar]
- 9.Sujan MSH, Tasnim R, Islam MS, et al. COVID-19-specific diabetes worries amongst diabetic patients: The role of social support and other co-variates. Prim Care Diabetes. 2021;15(5):778–85. 10.1016/j.pcd.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singhai K, Swami MK, Nebhinani N, Rastogi A, Jude E. Psychological adaptive difficulties and their management during COVID-19 pandemic in people with diabetes mellitus. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020;14(6):1603–5. 10.1016/j.dsx.2020.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel SY, McCoy RG, Barnett ML, Shah ND, Mehrotra A. Diabetes Care and Glycemic Control During the COVID-19 Pandemic in the United States. JAMA Intern Med. 2021;181(10):1412–4. 10.1001/jamainternmed.2021.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casagrande SS, Lawrence JM. Blood glucose, blood pressure, and cholesterol testing among adults with diabetes before and during the COVID-19 pandemic, USA, 2019 vs 2021. BMJ Open Diabetes Research and Care. 2023;11(3):e003420. 10.1136/bmjdrc-2023-003420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vashist K, Hassan S, Weber MB, Quarells RC, Patel SA. National Changes in Diabetes Care Practices during the COVID-19 Pandemic: Prospective Study of US Adults. Published online August 9, 2023:2023.08.06.23293722. 10.1101/2023.08.06.23293722. [DOI] [Google Scholar]
- 14.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Intern Med. 2021;181(3):388–91. 10.1001/jamainternmed.2020.5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MULTILOG Example 5.pdf. Accessed September 9., 2023. https://sudaanorder.rti.org/examples/MULTILOG%20Example%205.pdf.
- 16.Luo S, Lock LJ, Xing B, Wingelaar M, Channa R, Liu Y. Factors Associated with Follow-Up Adherence After Teleophthalmology for Diabetic Eye Screening Before and During the COVID-19 Pandemic. Telemedicine and e-Health. 2023;29(8):1171–8. 10.1089/tmj.2022.0391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shih KC, Kwong ASK, Wang JHL, et al. Diabetic retinopathy screening during the coronavirus disease 2019 pandemic. Eye. 2020;34(7):1246–7. 10.1038/s41433-020-0928-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.FLIII Ferris. How Effective Are Treatments for Diabetic Retinopathy? JAMA. 1993;269(10):1290–1. 10.1001/jama.1993.03500100088034. [DOI] [PubMed] [Google Scholar]
- 19.Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110236. 10.1016/j.pnpbp.2020.110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hawes MT, Szenczy AK, Klein DN, Hajcak G, Nelson BD. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol Med. 2022;52(14):3222–30. 10.1017/S0033291720005358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoon J, Chen C, Chao S, Wong E, Rosland AM. Adherence to Diabetes Medications and Health Care Use During the COVID-19 Pandemic Among High-Risk Patients. J Am Board Fam Med. 2023;36(2):289–302. 10.3122/jabfm.2022.220319R1. [DOI] [PubMed] [Google Scholar]
- 22.Delevry D, Ho A, Le QA. Association between processes of diabetes care and health care utilization in patients with diabetes: Evidence from a nationally representative US sample. J Diabetes. 2021;13(1):78–88. 10.1111/1753-0407.13109. [DOI] [PubMed] [Google Scholar]
- 23.Hooker SA, Truitt A, Anderson JP, Kane S, O’Connor PJ, Sperl-Hillen JM. Impact of the COVID-19 Pandemic on Type 2 Diabetes Care Delivery. Clin Diabetes. 2022;40(4):442–8. 10.2337/cd21-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barker LE, Kirtland KA, Gregg EW, Geiss LS, Thompson TJ. Geographic Distribution of Diagnosed Diabetes in the U.S.: A Diabetes Belt. Am J Prev Med. 2011;40(4):434–9. 10.1016/j.amepre.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 25.Ran J, Zhao S, Han L, et al. Increase in Diabetes Mortality Associated With COVID-19 Pandemic in the U.S. Diabetes Care. 2021;44(7):e146–7. 10.2337/dc21-0213. [DOI] [PubMed] [Google Scholar]
- 26.Lv F, Gao X, Huang AH, et al. Excess diabetes mellitus-related deaths during the COVID-19 pandemic in the United States. eClinicalMedicine. 2022;54. 10.1016/j.eclinm.2022.101671. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available on the Centers for Disease Control and Prevention (CDC) website and can be accessed through this link-https://www.cdc.gov/brfss/index.html