Abstract
Objectives
To investigate self-reported sleep duration, sleep timing, sleep status and influencing factors in the Chinese population.
Methods
This web-based cross-sectional survey was conducted in 2022, covering 31 provinces (91%) in China. 11,000 questionnaires were collected, of which 8970 were valid for analysis. Self-reported sleep habits, problems and quality were investigated. Good or fair sleep ratings, enough duration, regular, with no sleep disturbances and <30 min sleep latency was defined as a composite variable: ‘Good sleep’. Factors influencing sleep patterns and ‘Good sleep’ were analyzed by multivariate logistic regression.
Results
Most participants sleep less than 7 h per night (55.13%), usually go to bed at 10–12 pm (47.99%), wake up at 6–8 am (49.86%), and take less than 30 min to fall asleep (66.30%) with regular sleep schedule (76.01%). Only 12.36% have ‘Good sleep’. In the past 3 months, 46.80% of the participants reported symptoms of insomnia, and 21.54% had snoring problems. Among the adults, the young, males, college students, freelancers, and those who resided in urban areas and pandemic-free areas slept later, and the northerners woke up earlier. The adults with low-moderate and moderate income and the minors at elementary and middle school slept earlier and woke up earlier. Mid-aged adults who often napped at noon were more likely to have ‘Good sleep’ than any other age group, and urban dwellers with the same habit were more likely to have ‘Good sleep’ than people dwelled in other regions. While people who slept late, woke up too early or too late, slept too little or too much, resided at GMT 7–8 area or pandemic area, had high income, or took up some occupations (entrepreneurs/individuals, professionals, manual and non-manual workers, housewives) were less likely to get a ‘Good sleep’.
Conclusions
The national survey provided a sleep profile of the Chinese population. Both socio-economic status and personal sleep hygiene habits had an impact on ‘Good sleep’.
Keywords: Sleep, sleep duration, sleep quality, sleep health
Introduction
Sleep health is defined as a multidimensional pattern of sleep-wakefulness that is adapted to individual, social, and environmental needs and promotes physical and mental well-being [1]. Sleep deficiencies, which include insufficient or long sleep duration, poor sleep quality, and irregular sleep schedules, contribute to a range of suboptimal health outcomes, poorer overall functioning, and well-being [2,3].
The American Academy of Sleep Medicine (AASM) recommends that healthy adults should sleep >7 h per night on a regular basis to promote optimal health, while <7 h sleep is associated with an increased risk of obesity, diabetes, high blood pressure, heart disease and stroke, depression and death [4]. The National Sleep Foundation in the United States recommends 7–9 h of sleep per day for young adults and adults, and 7–8 h for older adults [5,6]. Epidemiological results of sleep duration have been reported in many countries [7–11]. In 2014, the Centers for Disease Control and Prevention (CDC) of the United States surveyed 444,306 adult respondents in all 50 states and the District of Columbia, 65.2% of whom reported the recommended amount of healthy sleep [7]. In 2017, a study reported the sleep patterns of 10,976 Canadian adults across the country. The mean sleep duration was 7.12 h per night, and an estimated 54–65% of adults slept the recommended duration (7–9 h) [8]. Another national report of 8649 Mexicans in 2020 showed that the average sleep duration of adults was 7:19 h [9]. Sleep duration in Asians tends to be short. The average sleep duration of Koreans and Japanese was 6.8 h [10] and 5.96 h [11], respectively.
The prevalence of poor sleep quality and self-reported suboptimal sleep has also been noted. A national study from South Korea in 2019 reported that the overall prevalence of poor sleepers (poor sleep quality was defined as the total score >5 of the Pittsburgh Sleep Quality Index) was 41.0% among 165,193 adult participants aged 19 years and older [12]. In Australia, a national survey of 1265 adults showed that 42% were considered to have suboptimal sleep (sleep of inadequate/excessive duration or poor quality), with fairly low rates of professional assessment (16%) and treatment (10%) [13].
In China, the results of a survey from Jilin province showed that the average sleep duration of adults was 7.31 h [14]. Another survey of 0.5 million people from five urban and five rural areas in China showed an average sleep duration of 7.38 h, with 17% reporting symptoms of insomnia [15].
Sleep status varied by geographic areas, socio-economic differences, and lifestyle factors in China [15–20]. Studies showed that the proportion of insomnia was higher in the rural population than in the urban population in China (19% vs 15%) [15], and that advanced age, unemployment, and low income are associated with poor sleep quality in the rural population [21]. In China, different occupations affect sleep status, e.g. farmers sleep the longest and civil servants sleep the shortest; farmers have the best sleep quality, while professional workers have the worst [18]. In addition, since the outbreak of the COVID-19 pandemic in China, researchers have found that the pandemic increases anxiety and depressive symptoms in the population and increases the risk of developing sleep disorders [22,23].
However, China is a vast country with various geographic and climatic conditions. Southern and northern China have quite different climatic characteristics and lifestyles [24,25]. Previous studies of sleep duration and sleep quality in the Chinese population mainly focused on specific regions and populations, and there is a lack of national-level reports. In this study, we chose questions that we were concerned most to survey about people’s sleep status and sleep hygiene habits, shedding light on sleep timing, sleep duration and sleep quality nationwide with the hypothesis that demographic factors, geographic regions and socio-economic factors might exert an effect on sleep in the Chinese population.
Methods
In this study, a web-based questionnaire survey was conducted from January 5th to January 25th, 2022, covering 31 of the 34 provinces, autonomous regions, and municipalities of China. The sleep timing, sleep duration, sleep problems and sleep quality of the Chinese population and their influencing factors were investigated.
Study design and participants
This survey was distributed online, mainly through a professional online questionnaire platform, People’s Daily WeChat, and was approved by the Chinese Sleep Research Society. This study was performed in line with the principles of the Declaration of Helsinki. Respondents across the nation voluntarily clicked on a link on the platform and answered the questions. This was an anonymous survey, so the respondents did not provide information that could identify their ID, and no informed consent form was signed. A total of 11,000 questionnaires were collected. Each questionnaire corresponded to one participant. All the incomplete (as long as one question was not answered) and invalid questionnaires (for example, network problems resulting in abnormal submissions or missing information) were excluded. The final sample size was 8970, with an effective rate of 81.5%.
Questionnaires
The questionnaire was divided into four parts (Table 1). The first part focused on the demographic information of the participants, including age, sex, residential area (urban/rural area and exact district or counties), annual personal income and occupation. In the second part, we investigated the sleep hygiene habits of the participants over the past three months. Participants were asked to choose their bedtime, waketime, and sleep duration, with a 1-h cut-off. We also investigated sleep latency and the frequency of naps during lunch breaks. The third part was the self-evaluated sleep status, including sleep disturbances, sleep quality, and sleep schedule. Since the study coincided with the COVID-19 outbreak, in the fourth part, we also investigated the pandemic in the region where the participants were located. The details of the questionnaire are shown in Table 1. All questions were single or multiple-choice so that participants could complete this survey in five minutes.
Table 1.
Questionnaires.
| Part 1. Demographic information | |
|---|---|
| How old are you? | A. 0–18 y B. 19–25 y C. 26–35 y D. 36–45 y E. 46–60 y F. >60 y |
| Are you male or female? | A. Male B. Female |
| Where do you currently live? Please select your detailed address. |
A. Urban area B. Rural area C. Others |
| (Please select the exact province, city, district or counties) | |
| What is your annual personal income (¥)? | A. 0 B. ≤30,000 C. 30,000–80,000 D. 80,000–150,000 E. 15,000–300,000 F. 300,000–500,000 G. 500,000–100,000 H. Over 1 million |
| What is your occupation? | A. Elementary/middle school students B. Farmers C. College students D. Professionals E. Freelancers F. Individuals, entrepreneurs G. Corporate white-collar workers H. Civil servant I. Workers J. Service workers K. Housewife L. Retired M. Others |
| Part 2. Sleep hygiene status | |
| When do you usually go to bed? | A. Before 7 pm B. 7–8pm C.8–9pm D. 9–10pm E. 10–11pm F. 11–12 pm G. 0–1 am H. 1–2 am I. After 3 am |
| When do you usually get up? | A. Before 5 am B. 5–6 am C. 6–7 am D. 7–8 am E. 8–9 am F. 9–10 am G. 10–11 am H. 11–12 am I. After 1 pm |
| How long do you sleep each night on average? | A. Less than 3 h B. 3–4 h C. 4–5 h D. 5–6 h E. 6–7 h F. 7–8 h G. 8–9 h H. 9–10 h I. More than 10 h |
| How long does it take to fall asleep at night? | A. <30 min B. 30–60 min C. >60 min |
| How often do you take a nap during lunch break? | A. Never B. Occasionally C. Often |
| Part 3. Self-evaluated sleep status | |
| Are you getting enough sleep? | A. Yes B. No, Sleep too little C. No, Sleep too much |
| Do you have a regular sleep schedule? | A. Yes B. No |
| Do you have the following sleep disturbances in the past 3 months? (You can choose more than one answer) |
A. Symptoms of insomnia B. Difficulty falling asleep C. Snoring D. Sleepiness E. Easy to wake up F. Dreamy at night G. Others H. No disturbances |
| How would you rate your sleep quality? | A. Good B. Fair C. Poor |
| Part 4. The impact of COVID-19 on sleep | |
| Is there an outbreak of COVID-19 in your area? | A. Yes B. No |
Terminology interpretation and analysis
Geographic regions
The geographic regions of the participants were categorized in two ways based on their reported locations - northern China and southern China, separated by the Qinling-Huaihe line, and five time zones based on Greenwich Mean Time (GMT). Since the national standard time is GMT 8, we converted the actual sleep and wake-up time according to the time zone in which the participants lived to exclude time zone interference with sleep patterns.
Possible sleep disturbances
Possible sleep disturbances were inferred from the sleep problems reported by the participants. If participants reported symptoms of insomnia or difficulty falling asleep, they were considered to have possible insomnia. If participants reported snoring, participants were considered to have possible sleep-related breathing disorders. And if participants reported both kinds of troubles, participants were considered to have both insomnia and sleep-related breathing disorders. If participants did not report the above problems but reported sleepiness, easy to wake up, dreamy at night, or other situations, participants were considered to have suboptimal sleep status and may have other sleep problems.
In this study, we also screened participants for possible sleep rhythm problems (advanced and delayed sleep-wake phases) based on self-reported bedtime and waketime without time zone interference. Rhythm abnormality was set at 2 h beyond the average bedtime and waketime according to ICSD-3 [4].
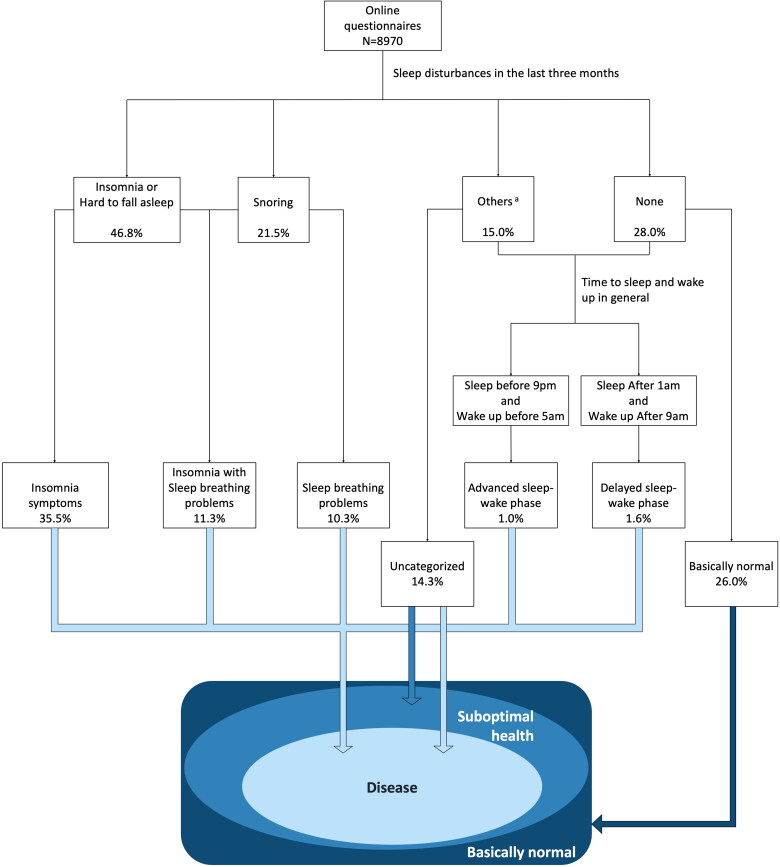
If the self-reported sleep problems cannot be classified as one of the above, the participant was categorized into other sleep problems. The detailed screening flowchart of each questionnaire is shown in Figure 1.
Figure 1.
The screening process for the prevalence of sleep disturbances (classified according to the presence of sleep disturbances in the last 3 months). aIf the participants could not be classified but reported sleepiness, easy to wake up, dreamy at night, or other situations, participants were considered to have suboptimal sleep status and may have other sleep problems.
Good sleep
Based on the results of self-evaluated sleep status, we defined good or fair sleep quality ratings, enough duration, regular, with no sleep disturbances and <30 min sleep latency as composite variable: ‘Good sleep’. If participants did not meet any of the criteria above, they were considered of no-‘Good sleep’.
Statistical analysis
Age was categorized into minors (0–18 y), young adults (19–35 y), middle-aged adults (36–60 y) and old adults(>60 y). According to the wage data released by the National Bureau of Statistics of China (NBSC), income was classified into six levels: no income, low-income (<¥30,000), low-moderate income (¥30,000–80,000), moderate-income (¥80,000–300,000), high-income (¥300,000–1,000,000), and ultra-high-income (Over 1 million RMB) (as of March 15, 2023, 1¥=$0.145US). According to the EGP Classification of Hierarchies [26], workers and service workers were combined into manual workers, and corporate white-collar workers and civil servants were combined into non-manual workers. According to the recommended sleep time [4–6], sleep duration was classified into three categories (<7 h, 7–9 h, >9 h). Bedtime (before 10 pm, 10–12 pm, after 12 am) and wakeup time (before 6 am, 6–8 pm, after 8 am) were also grouped into three categories.
The sleep status of adults and minors was analyzed separately. Descriptive statistics were used to present demographic data, socioeconomic characteristics, sleep habits and self-evaluation of sleep status. Chi-square tests were used to compare differences in sample sizes for variables in adults and minors. Multivariate logistic regression was used to analyze the socio-demographic factors (age, sex, residence, geographical region, geographical time zone, annual personal income, occupation, pandemic) for differences in sleep patterns. Binary logistic regression analyses were performed to analyze the above socio-demographic factors and sleep hygiene habits on ‘Good sleep’. Odds ratios (ORs) with 95% confidence intervals (CIs) were presented in the results. A two-sided Wald test was performed to determine if the ORs in the regression model were statistically significant. Statistical significance was determined using a threshold p-value of .05. Statistical analysis was performed in SPSS 26.0.
Results
Demographic and socioeconomic characteristics
Of the total participants, 12.22% were minors and 87.78% were adults, with a high proportion of the young (48.09%) and the mid-aged (36.37%) adults. 58.07% were female and 41.93% were male, with no difference in the gender composition of adults and minors (X2 = 0.13, p = .72). Regarding the area of residence, 22.08% resided in rural areas and 74.67% in urban areas, while more minors (34.22%) lived in rural areas than adults (20.40%). According to the geographical regions, 47.18% were southerners and 52.82% were northerners, with no difference in the north-south composition of adults and minors (X2 = 1.06, p = .32). In the total sample, 62.35% of the population lived in GMT 8 and 29.54% in GMT 7, and the proportion of minors living in GMT 6 was high (17.43%). 67.84% had a COVID-19 pandemic in their place of residence. 24.23% were low-moderate income and 31.05% were moderate income. Non-manual workers accounted for the largest proportion of the total occupational type with 25.24%, followed by college students (18.76%) and professionals (10.68%), while farmers accounted for the least with only 1.22%. 22.45% of minors were already college students. Details of the participants’ demographic and socioeconomic information are shown in Table 2.
Table 2.
Demographic and socioeconomic characteristics, sleep hygiene habits and self-evaluation of sleep status.
| Total |
Adults |
Minors |
Adults vs Minorsd |
Total |
Adults |
Minors |
Adults vs Minorsd |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | X 2 | p value | N | % | N | % | N | % | X 2 | p value | ||
| Demographic and socioeconomic characteristics | Sleep hygiene habits | ||||||||||||||||
| Age | Bedtimeb | ||||||||||||||||
| Minors | 1096 | 12.22 | – | – | 1096 | 100.00 | – | – | Before 10 pm | 2860 | 31.88 | 2388 | 30.33 | 472 | 43.07 | 74.16 | <.001** |
| Young adults | 4314 | 48.09 | 2518 | 31.98 | – | – | 10-12pm | 4305 | 47.99 | 3883 | 49.31 | 422 | 38.50 | ||||
| Middle-aged adults | 3262 | 36.37 | 1796 | 22.81 | – | – | After 12am | 1805 | 20.12 | 1603 | 20.36 | 202 | 18.43 | ||||
| Old adults | 298 | 3.32 | 298 | 3.78 | – | – | Wakeup timeb | ||||||||||
| Sex | Before 6am | 2329 | 25.96 | 2002 | 25.43 | 327 | 29.84 | 13.16 | .001** | ||||||||
| Male | 3761 | 41.93 | 3296 | 41.86 | 465 | 42.43 | 0.13 | .72 | 6-8am | 4472 | 49.86 | 3931 | 49.92 | 541 | 49.36 | ||
| Female | 5209 | 58.07 | 4578 | 58.14 | 631 | 57.57 | After 8am | 2169 | 24.18 | 1941 | 24.65 | 228 | 20.80 | ||||
| Area of residence | Sleep duration | ||||||||||||||||
| Rural area | 1981 | 22.08 | 1606 | 20.40 | 375 | 34.22 | 115.31 | <.001** | Less than 7h | 4945 | 55.13 | 4463 | 56.68 | 482 | 43.98 | 111.73 | <.001** |
| Urban area | 6698 | 74.67 | 6023 | 76.49 | 675 | 61.59 | 7–9 h | 3432 | 38.26 | 2960 | 37.59 | 472 | 43.07 | ||||
| Others | 291 | 3.24 | 245 | 3.11 | 46 | 4.20 | More than 9 h | 593 | 6.61 | 451 | 5.73 | 142 | 12.96 | ||||
| Geographical regiona | Sleep latency | ||||||||||||||||
| Northern China | 4232 | 47.18 | 3699 | 46.98 | 533 | 48.63 | 1.06 | .32 | <30 min | 5947 | 66.30 | 5072 | 64.41 | 875 | 79.84 | 103.13 | <.001** |
| Southern China | 4738 | 52.82 | 4175 | 53.02 | 563 | 51.37 | 30–60 min | 1947 | 21.71 | 1812 | 23.01 | 135 | 12.32 | ||||
| Geographical time zone | >60 min | 1076 | 12.00 | 990 | 12.57 | 86 | 7.85 | ||||||||||
| GMT 6 | 494 | 5.51 | 303 | 3.85 | 191 | 17.43 | 434.21 | <.001** | Nap during lunch break | ||||||||
| GMT 7 | 2650 | 29.54 | 2318 | 29.44 | 332 | 30.29 | Basically no lunch break | 2044 | 22.79 | 1796 | 22.81 | 248 | 22.63 | 6.17 | .046* | ||
| GMT 8 | 5593 | 62.35 | 5087 | 64.61 | 506 | 46.17 | Occasional lunch break | 2784 | 31.04 | 2410 | 30.61 | 374 | 34.12 | ||||
| GMT 9 | 233 | 2.60 | 166 | 2.11 | 67 | 6.11 | Often take a lunch break | 4142 | 46.18 | 3668 | 46.58 | 474 | 43.25 | ||||
| COVID-19 pandemic | Self-evaluation of sleep status | ||||||||||||||||
| No | 2885 | 32.16 | 2408 | 30.58 | 477 | 43.52 | 73.84 | <.001** | Sleep adequacy | ||||||||
| Yes | 6085 | 67.84 | 5466 | 69.42 | 619 | 56.48 | Adequate sleep | 3052 | 34.02 | 2570 | 32.64 | 482 | 43.98 | 57.14 | <.001** | ||
| Annual personal income | Sleep too little | 4428 | 49.36 | 3953 | 50.20 | 475 | 43.34 | ||||||||||
| No income | 1970 | 21.96 | 1127 | 14.31 | 843 | 76.92 | – | – | Sleep too much | 1490 | 16.61 | 1351 | 17.16 | 139 | 12.68 | ||
| With income | – | – | – | – | 253 | 23.08 | Sleep schedule | ||||||||||
| Low income | 1466 | 16.34 | 1290 | 16.38 | – | – | Irregular | 2152 | 23.99 | 1908 | 24.23 | 244 | 22.26 | 2.05 | .162 | ||
| Low-moderate income | 2173 | 24.23 | 2133 | 27.09 | – | – | Regular | 6818 | 76.01 | 5966 | 75.77 | 852 | 77.74 | ||||
| Moderate income | 2785 | 31.05 | 2759 | 35.04 | – | – | Possible sleep disturbances | ||||||||||
| High income | 496 | 5.53 | 493 | 6.27 | – | – | Insomnia symptoms | 3186 | 35.52 | 2885 | 36.64 | 301 | 27.46 | 246.73 | <0.001** | ||
| Ultra-high income | 80 | 0.89 | 72 | 0.91 | – | – | Sleep breathing problems | 920 | 10.26 | 870 | 11.05 | 50 | 4.56 | ||||
| Occupation | Insomnia with Sleep breathing problems | 1012 | 11.28 | 928 | 11.79 | 84 | 7.66 | ||||||||||
| Farmers | 109 | 1.22 | 105 | 1.33 | – | – | – | – | Others | ||||||||
| Entrepreneurs, individuals | 531 | 5.92 | 527 | 6.69 | – | – | Advanced sleep-wake phase | 89 | 0.99 | 59 | 0.75 | 30 | 2.74 | ||||
| Professionals | 958 | 10.68 | 949 | 12.05 | – | – | Delayed sleep-wake phase | 144 | 1.61 | 129 | 1.64 | 15 | 1.37 | ||||
| Manual workers | 887 | 9.89 | 882 | 11.20 | – | – | Uncategorizedc | 1286 | 14.34 | 1136 | 14.43 | 150 | 13.69 | ||||
| Non-manual workers | 2264 | 25.24 | 2258 | 28.68 | – | – | None | 2333 | 26.01 | 1867 | 23.71 | 466 | 42.52 | ||||
| Freelancers | 480 | 5.35 | 471 | 5.98 | – | – | Sleep quality rating | ||||||||||
| Housewife | 278 | 3.1 | 272 | 3.45 | – | – | Good | 3803 | 42.40 | 3233 | 41.06 | 570 | 52.01 | 61.24 | <.001** | ||
| College students | 1683 | 18.76 | 1437 | 18.25 | 246 | 22.45 | Fair | 3685 | 41.08 | 3270 | 41.53 | 415 | 37.86 | ||||
| Elementary/middle school students | 839 | 9.35 | 42 | 0.53 | 797 | 72.72 | Poor | 1482 | 16.52 | 1371 | 17.41 | 111 | 10.13 | ||||
| Retired | 361 | 4.02 | 360 | 4.57 | – | – | Good sleep | ||||||||||
| Others | 580 | 6.47 | 571 | 7.25 | 53 | 4.84 | No | 7861 | 87.64 | 6999 | 88.89 | 862 | 78.65 | 93.07 | <.001** | ||
| Yes | 1109 | 12.36 | 875 | 11.11 | 234 | 21.35 | |||||||||||
aAccording to the location of the participants, northern China and southern China are divided by the Qinling-Huaihe line.
bWe converted the bedtime and wakeup time according to the actual time zone where the participants were living.
cUncategorized other symptoms such as sleepiness, easy to wake up, and excessive dreaming.
dA chi-square test was used to compare differences in sample sizes for each variable between adults and minors.
Sleep patterns
38.26% of the total sample met the criteria of 7–9 h of sleep per night, and most adults (56.68%) slept less than 7 h. However, only 56.03% of minors slept more than 7 h. Most people slept at 10–12 pm (47.99%) and woke up at 6–8 am (49.86%). Compared to adults (30.33%), minors (43.07%) were more likely to fall asleep before 10 pm. Most people (64.41% adults and 79.84% minors) fell asleep within 30 min, 21.71% of the total participants fell asleep within 30–60 min, and it took more than 60 min for 12.00% of participants to fall asleep. In terms of habits of napping, 46.18% of the participants (46.58% adults and 43.25% minors) often napped during lunch breaks, while 22.81% never napped (Table 2).
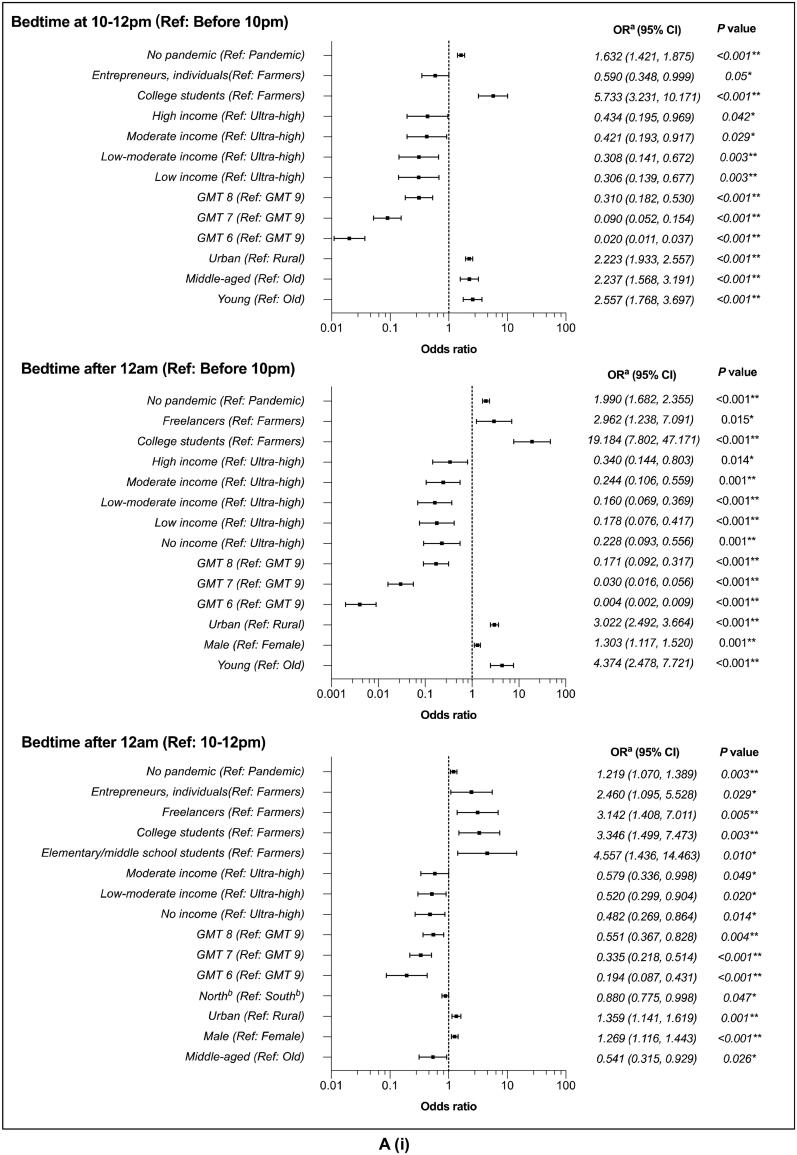
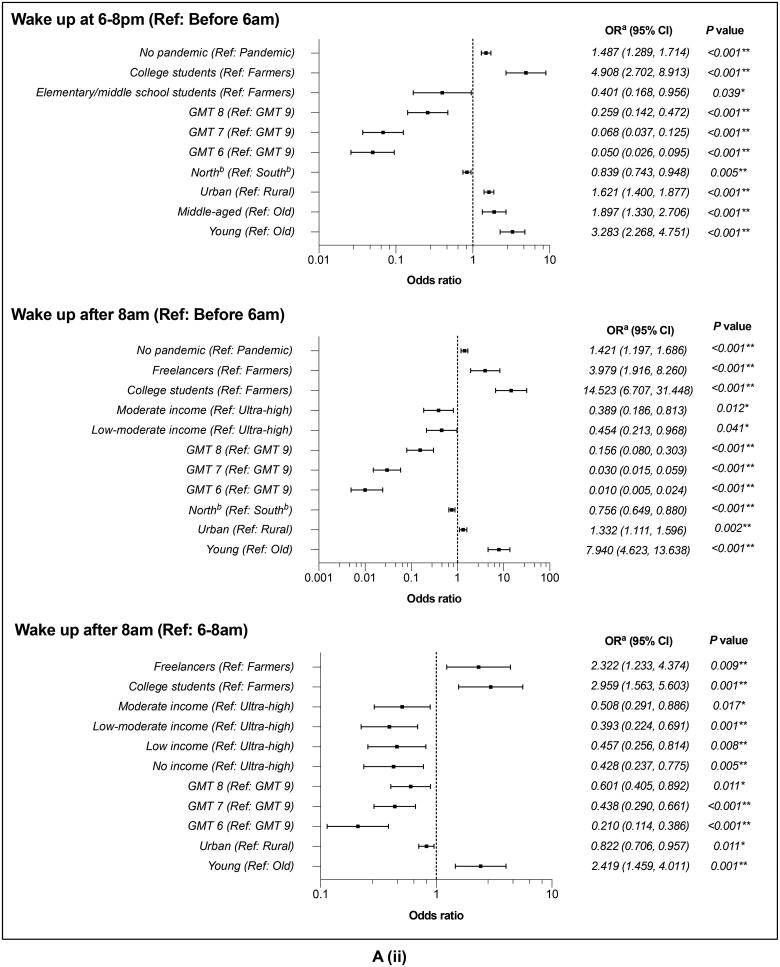
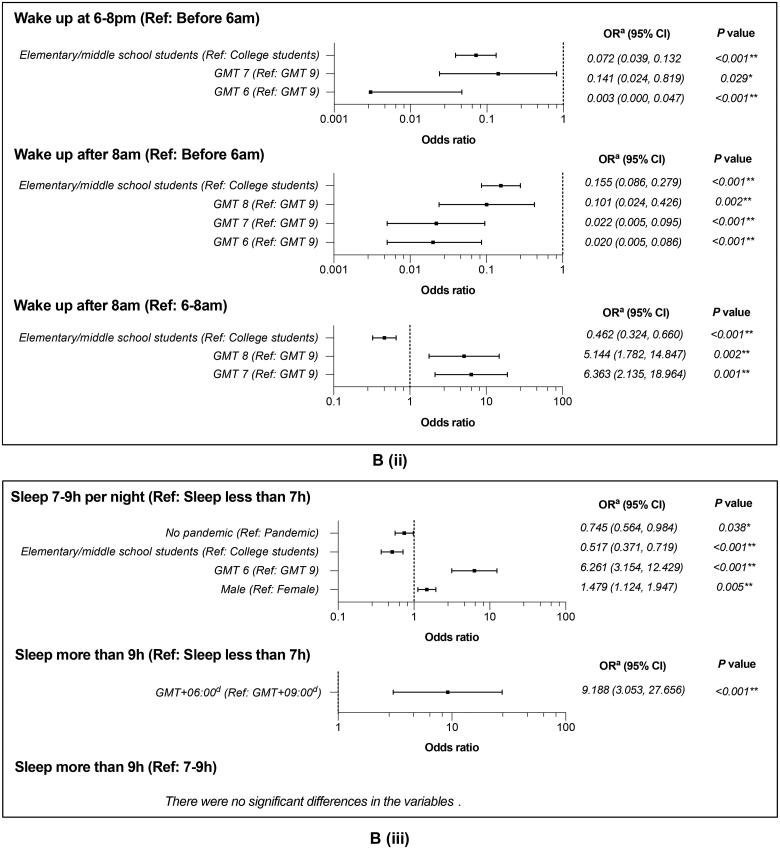
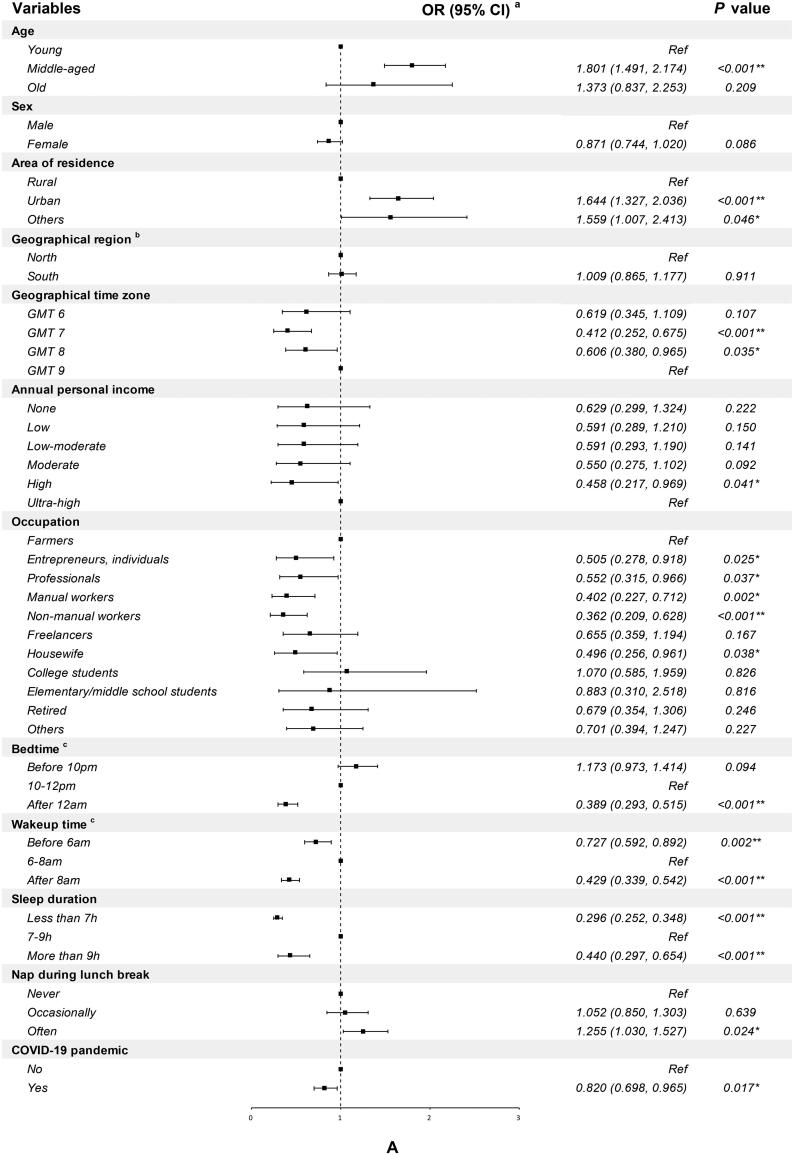
In adults, the young slept later and woke up later. The middle-aged tended to go to bed at 10–12 pm and slept <9 h. Men were more likely to fall asleep after 12 am compared to women. Compared to rural areas, the urban population slept later and less, and was more likely to wake up between 6–8 am. Northerners woke up early and slept <9 h compared to southerners. For time zone, the further west (e.g. GMT 6), the closer people go to bed to sunset, and the further east (e.g. GMT 9), the later people wake up to sunrise. When there was no pandemic, people were more likely to sleep late, wake up after 6 am, and sleep <9 h. Compared to the ultra-high incomes, the low-moderate and moderate incomes slept earlier and woke up earlier. Compared to farmers, college students went to bed later and woke up later, sleeping >7 h. Freelancers tended to go to bed after 12 am and get up after 8 am Elementary and middle school students went to bed later (more after 12 am) but got up earlier (more before 6 am) (Figure 2A).
Figure 2.
Socio-demographic factors associated with sleep timec, wake timec and sleep duration. (A) Adults. (B) Minors. (i) Sleep time. (ii) Wake time. (iii) Sleep duration. aMultivariate logistic regression analysis of socio-demographic factors associated with sleep time, wake time and sleep duration (only results with significant differences were shown). bAccording to the location of the participants, northern China and southern China are divided by the Qinling–Huaihe line. cWe converted the bedtime and wakeup time according to the actual time zone where the participants were living and reclassified. *Indicates statistical significance (p < .05), **Indicates statistical significance (p < .01).
In minors, compared to college students, elementary and middle school students slept earlier, woke up earlier, and were more likely to sleep <7 h. Northerners (vs. southerners) and those in the GMT 7-8 (vs. GMT 9) area were more likely to fall asleep by 12 am (Figure 2B).
Prevalence of possible sleep disturbances
Based on the presence of sleep disturbances in the last 3 months, 35.52% of participants were suspected of having symptoms of insomnia, 10.26% of them having sleep-related breathing problems, and 11.28% of them having both disturbances. Among the other sleep disturbances, 0.99% of the participants were suspected to have an advanced sleep-wake phase, 1.61% were suspected to have a delayed sleep-wake phase, and the remaining 14.34% were unclassifiable. 26.01% of the participants were basically normal (Table 2).
Self-evaluation of sleep status and factors associated with ‘Good sleep’
Overall, participants were satisfied with their sleep status (42.40% considered their sleep quality to be good and 41.08% considered it to be fair), while 16.52% considered their sleep quality to be poor. Most people (76.01%) had regular sleep habits, and 23.99% thought they slept irregularly. For sleep adequacy (which means subjective enough sleep time), the majority of people thought they slept too little (49.36%), 34.02% thought they slept enough, and another 16.61% thought they slept too much. Only 12.36% (11.11% adults and 21.35% minors) of the total population met the criteria for ‘Good sleep’ (Table 2).
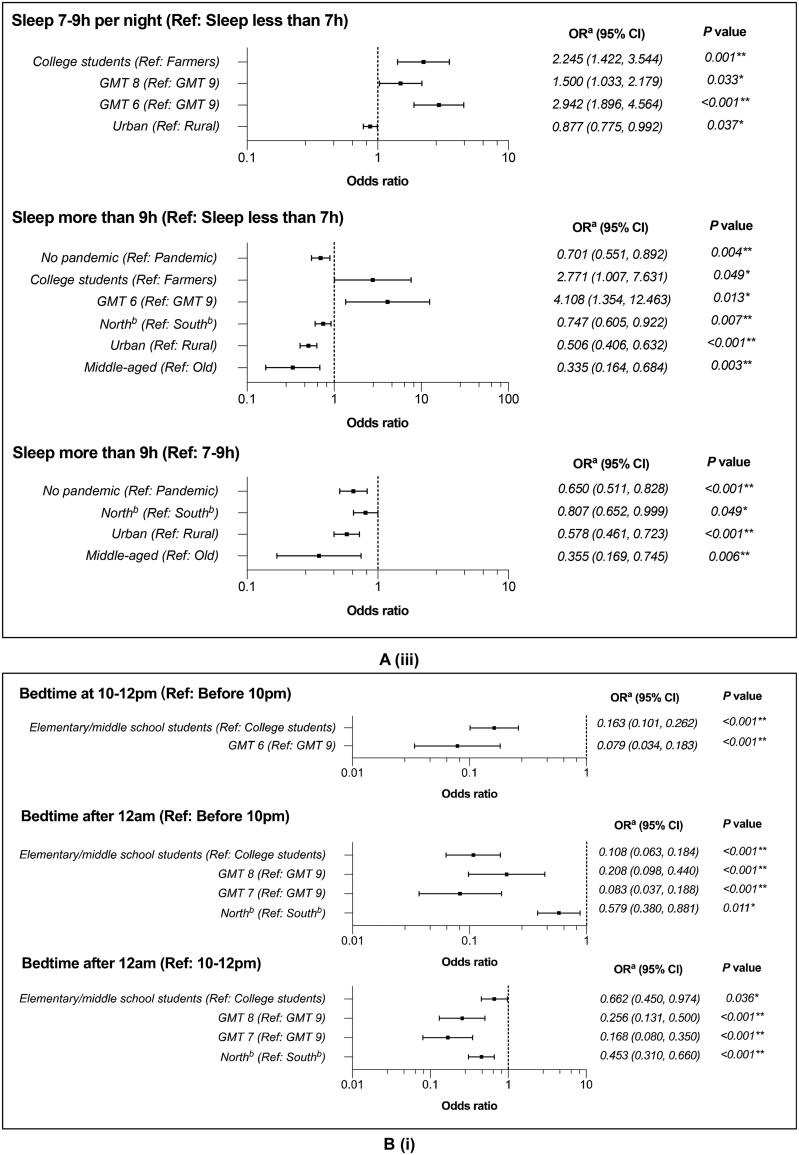
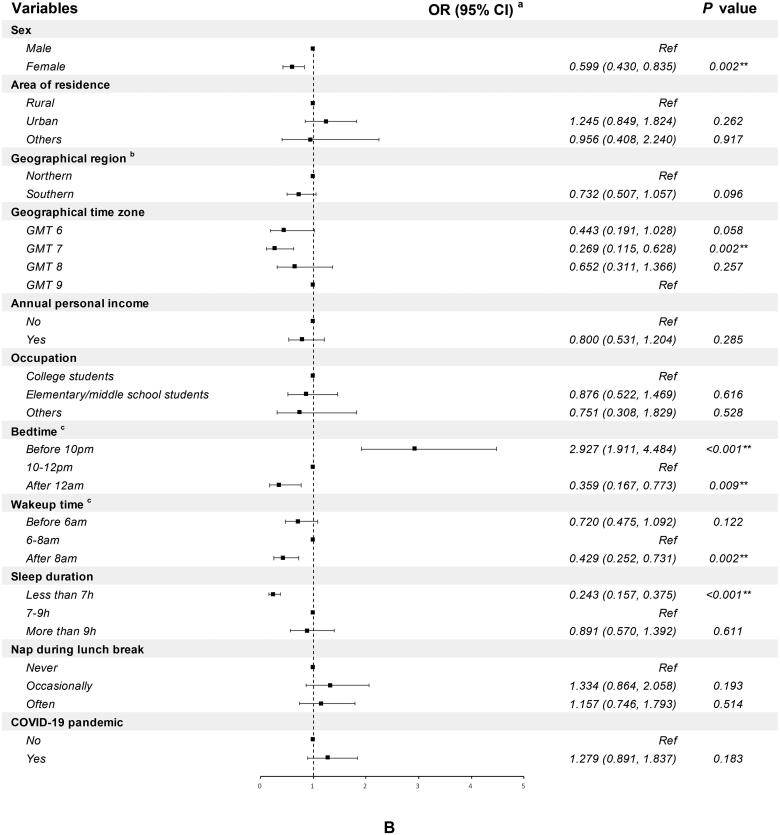
Among adults, the middle-aged, urban dwellers, and people who often took lunch breaks were more likely to get ‘Good sleep’, while people who lived in the GMT 7-8 area, had high income (¥300,000–1,000,000), took up some occupations (entrepreneurs/individuals, professionals, manual workers, non-manual workers, housewives), slept late (after 12 am), woke up too early (before 6 am) or too late (after 8 am), slept too little (less than 7 h) or too much (>9 h), and resided in areas with COVID-19 pandemic were less likely to fulfill the criteria. In minors, an early bedtime (before 10 am) can help to get a ‘Good sleep’, whereas females, in GMT 7 areas, with late bedtimes (after 12 am), late risers (after 8 am), and less sleep (less than 7 h) were less likely to get a ‘Good sleep’ (Figure 3).
Figure 3.
Socio-demographic factors and sleep habits associated with good sleep. (A) Adults. (B) Minors. aBinary logistic regression analysis of socio-demographic factors and sleep habits associated with good sleep. bAccording to the location of the participants, northern China and southern China are divided by the Qinling-Huaihe line. cWe converted the bedtime and wakeup time according to the actual time zone where the participants were living and reclassified. *Indicates statistical significance (p < .05), **Indicates statistical significance (p < .01).
Discussion
In this study, a web-based questionnaire survey was conducted, covering most regions of China. The sleep timing, sleep duration, sleep problems and influencing factors of ‘Good sleep’ in the Chinese population were investigated.
More than half of the Chinese population slept for less than 7 h in the present study (56.68% in adults and 43.98% in minors). In developed western countries, the prevalence of the population sleeping less than 7 h is about 1/3, such as the United States (34.8%) [7], Canada (31.9%) [8], and New Zealand (37%) [27]. In Asia, the length of sleep appears to be generally shorter. In this study, the Chinese slept longer than the Japanese but shorter than the Korean [10,11].
China covers a vast territory. In this study, three dimensions, urban-rural, north-south (latitude), and time zone (longitude), were used to categorize the geographical characteristics of different populations. Studies have reported shorter sleep duration in urban than rural populations in China [15]. In our study, the urban-rural factor influenced sleep patterns and ‘Good sleep’ in adults, but not in minors. In urban areas, adults slept late and less which could lead to poor sleep. In fact, living in urban areas was an advantageous factor for ‘Good sleep’ in adults, while lifestyle, mental health, physiological factors, occupation, and age can also affect sleep quality [18–20]. In addition to sleep patterns, other socioeconomic conditions in cities may weaken the unfavorable effects of bad sleep habits on ‘Good sleep’.
In this study, both adults and minors in the north slept earlier than in the south. During the study period, it was winter in the northern hemisphere. The southern China was relatively wet and warm, while northern China was mostly dry and cold. It might be the cold nights and large temperature difference between day and night that the northerners tend to go to bed early and wake up early, and reduce the number of recreational activities before bedtime.
China uses the GMT 8 as the national standard time, which can explain the differences of sleep habits among time zones. Besides, geographic and socio-economic factors may also influence the sleep status of populations in different time zones. In China, the GMT 9 area comprises the northeastern region, which used to be an important area for the development of heavy industry. But in recent years the aging population has increased significantly, and economic development has been slow in GMT 9 area. The GMT 8 region is the lifeblood of China’s economic development. The major developed cities (e.g. Shanghai, Beijing, Shenzhen and Guangzhou) are all located in this region. The GMT 7 region encompasses most areas of China’s ‘Western Development’ strategy. The large population but backward of educational resources may explain the poor sleep of elementary/middle school students of GMT 7. In the results of adults, those in the GMT 7-8 region did not sleep well compared to the GMT 9 region, probably due to high work pressure, and a relatively young population with a small proportion of retired people. The GMT 6 region encompasses the majority of highland areas of China (Xinjiang, Tibet, and Qinghai), which are sparsely populated and economically disadvantaged. Further studies were needed to deeply explain the sleep status between time zones in China.
In China, annual incomes of 300,000–1000,000RMB means a relatively high income in first- and second-tier cities. This group is usually considered to live more comfortably and have more existential and financial stability and longevity than the poorer and richer groups [28,29], yet this income group did not rate their sleep quality as good in our study. This result may be due to the fact that this group didn’t sleep as well as expected, or this group had a relatively high level of culture, education and social status, which requires a higher quality of sleep [30].
During this study, the COVID-19 pandemic was on a plateau in China, but adverse effects of the pandemic on sleep can still be found. Although it was more likely to go to bed early and wake up after 6 am during the pandemic, sleeping more did not equate to ‘Good sleep’. At the beginning of the COVID-19 pandemic, studies had reported delayed bedtime and wake-up time in Chinese populations compared to the pre-epidemic period [22,31]. According to our results, the pandemic disrupted the population’s sleep habits and rhythm of life, even during the plateau period.
In this study, no differences in sleep patterns and proportion of ‘Good sleep’ were found by gender among adults, but in minors, girls did not sleep well, and they were more likely to sleep less than 7 h. Reports of gender differences in sleep duration were inconsistent. Some studies have concluded that women sleep longer [32], while some suggest that women are more likely to be short sleepers [33,34]. Further exploration of sleep patterns and self-ratings in sex of different age groups may be necessary.
High proportion (46.80%) of participants had symptoms of insomnia in this study. However, without objective tools, we cannot make a diagnosis of whether the patients had chronic insomnia or other types of insomnia disorder. The American Academy of Sleep Medicine reported a high prevalence of insomnia symptoms in adults, with an estimated range of 35%–50%, which is similar to the findings of this study [35]. While the incidence of diagnosed chronic insomnia is relatively low, ranging from 5% to 15% [35]. Some studies have reported a higher prevalence of insomnia among young people than older people in China [36]. In this study, there was a high proportion of young people. Accelerated urbanization and industrialization, occupational stress and widespread use of streaming media may be responsible for the high prevalence of insomnia among young people [36]. The COVID-19 pandemic may contribute to insomnia, too [37,38].
The percentage of participants with snoring disturbances was 21.54%, of which 11.28% had both symptoms of insomnia and snoring disturbances. The snoring symptoms reported in this study may represent a category of diseases, from habitual snoring to obstructive sleep apnea (OSA). Studies have suggested that Asians have a higher risk of habitual snoring, and the prevalence is higher in older than in younger people [39–41]. As the sample group was young, the results may be lower than the populations.
In this study, symptoms of insomnia and snoring tend to co-occur: 52.3% of those with snoring disturbances reported insomnia symptoms, and 24.1% of those with insomnia symptoms reported snoring disturbances. Previous studies reported that 42%–80% of patients with OSA reported at least 1 symptom of insomnia, and 39% of OSA patients met the diagnostic criteria for insomnia [42,43]. The prevalence of OSA also ranged from 29.3% to 67% in the elderly population with insomnia [44–46]. However, this study was only a questionnaire survey, so medical diagnosis and further analysis based on demographic factors such as age and occupation are required.
In this study, the symptom of an advanced sleep-wake phase was considered to be 0.99% and a delayed sleep-wake phase was 1.61%. This rate may be high compared to the disease diagnosis. The prevalence of the advanced sleep-wake phase using the International Classification of Sleep Disorders (ICSD) criteria was estimated to be 0%–0.21% and the delayed sleep-wake phase was estimated to be 0.2%–16% [47]. Self-reported sleep disturbances may include sleep subhealth conditions outside of the diagnosis of disease and may affect systemic health as well [48,49].
Overall, multiple sociodemographic and economic factors influence sleep patterns, sleep status and problems. Our findings may contribute to public health decision-making and improve the health of citizens.
Limitations
First, the survey was conducted as an online questionnaire, so the investigators could not explain and check information with the respondents, which in turn affected the results. Second, the surveyed population was all Internet users, while those who had no access to the Internet could not participate in this survey, such as people who cannot afford electronic products in remote areas, and the illiterate or the elderly who couldn’t answer the questions online. Third, the age of participants was collected as a categorical parameter, and the high percentage of the young (48.09%) and the mid-aged (36.37%) with only 3.78% being over 60 years old may affect the accuracy of the results. Fourth, sleep duration was not calculated by objective measurements, such as polysomnography or actigraphy. Fifth, this survey could only speculate on the tendencies of suspected insomnia, suspected sleep-disordered breathing and other suspected sleep conditions, diagnosis of a specific disease and investigation of the prevalence requires verification of standard and proper medical methods in the future. In addition, some population groups were small and may lack the power to be compared with other groups. It is important to be cautious in generalizing the results to the broader Chinese population.
Acknowledgment
The authors were grateful to sleep research institute of DeRucci for their help in questionnaire distribution, collection and data entry.
Funding Statement
This work was not supported by any funding.
Ethical approval
Our study did not require an ethical board approval because this was a completely voluntary study with no interventions, clinical examinations, or sampling.
Our study did not require informed consent form because this was an anonymous survey, and the respondents did not provide information that could identify their ID.
This was a survey conducted by the China Sleep Research Society which did not have an ethics institute. Peking University and Fudan University had ethics institutes, but they cannot apply for ethics for a project that was not entirely led by them. This study was systematically designed to achieve privacy protection without ethical implications: a survey that was anonymous, voluntary, did not involve the collection of information that clearly identifies individuals, and did not violate the Helsinki Principles and their bylaws. This project was non-interventionist, required only privacy protection, and was not disseminated to people other than the researchers, who in fact did not even know who they are. Besides, the Helsinki Principles and their bylaws were essentially medical ethics, while this project was not strictly medical research. Therefore, we did not have ethical approval.
Authors contributions
Xuemei Gao, Zhili Huang and Heming Zuo were involved in the conception of the study. Wanxin Zhang, Min Yu, Ying Xu and Xiaoqing Li were involved in the data analysis and drafting the manuscript. All authors were involved in the interpretation of the findings. All authors reviewed and approved the final manuscript and agree to be held accountable for all aspects of the work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Anonymized data are available upon reasonable request.
References
- 1.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):1–16. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gohari A, Baumann B, Jen R, et al. Sleep deficiency: epidemiology and effects. Clin Chest Med. 2022;43(2):189–198. doi: 10.1016/j.ccm.2022.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Jackson CL, Walker JR, Brown MK, et al. A workshop report on the causes and consequences of sleep health disparities. Sleep. 2020;43(8):zsaa037. doi: 10.1093/sleep/zsaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AASM . International classification of sleep disorders. 3rd ed. Darien (IL): American Academy of Sleep Medicine; 2014. [Google Scholar]
- 5.Hirshkowitz M, Whiton K, Albert SM, et al. National sleep foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1(4):233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 6.Chaput JP, Dutil C, Sampasa-Kanyinga H.. Sleeping hours: what is the ideal number and how does age impact this? Nat Sci Sleep. 2018;10:421–430. doi: 10.2147/NSS.S163071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Wheaton AG, Chapman DP, et al. Prevalence of healthy sleep duration among adults–United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 8.Chaput JP, Wong SL, Michaud I.. Duration and quality of sleep among canadians aged 18 to 79. Health Rep. 2017;28(9):28–33. [PubMed] [Google Scholar]
- 9.Arrona-Palacios A, Gradisar M.. Self-reported sleep duration, sleep quality and sleep problems in Mexicans adults: results of the 2016 Mexican national halfway health and nutrition survey. Sleep Health. 2021;7(2):246–253. doi: 10.1016/j.sleh.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Cho J, Kwak N, Choi SM, et al. Sleep duration and health-related quality of life in Korean adults: 2007-2015 Korea national health and nutrition examination survey. Sleep Breath. 2020;24(2):725–733. doi: 10.1007/s11325-019-01972-7. [DOI] [PubMed] [Google Scholar]
- 11.Ito K, Kadotani H, Okajima I, et al. Large questionnaire survey on sleep duration and insomnia using the TV hybridcast system by Japan broadcasting corporation (NHK). Int J Environ Res Public Health. 2021;18(5):2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SY, Ju YJ, Lee JE, et al. Factors associated with poor sleep quality in the Korean general population: providing information from the Korean version of the Pittsburgh sleep quality index. J Affect Disord. 2020;271:49–58. doi: 10.1016/j.jad.2020.03.069. [DOI] [PubMed] [Google Scholar]
- 13.Metse AP, Bowman JA.. Prevalence of self-reported suboptimal sleep in Australia and receipt of sleep care: results from the 2017 national social survey. Sleep Health. 2020;6(1):100–109. doi: 10.1016/j.sleh.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 14.Wang S, Li B, Wu Y, et al. Relationship of sleep duration with sociodemographic characteristics, lifestyle, mental health, and chronic diseases in a large Chinese adult population. J Clin Sleep Med. 2017;13(3):377–384. doi: 10.5664/jcsm.6484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen Y, Kartsonaki C, Clarke R, et al. Characteristics and correlates of sleep duration, daytime napping, snoring and insomnia symptoms among 0.5 million Chinese men and women. Sleep Med. 2018;44:67–75. doi: 10.1016/j.sleep.2017.11.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu X, Wu D, Qi X, et al. The associations between carbohydrate and protein intakes with habitual sleep duration among adults living in urban and rural areas. Clin Nutr. 2018;37(5):1631–1637. doi: 10.1016/j.clnu.2017.07.024. [DOI] [PubMed] [Google Scholar]
- 17.Qu S, Wang M, Peng Y.. Associations between residential environmental health and sleep quality: potential mechanisms. Sleep Med. 2023;103:16–23. doi: 10.1016/j.sleep.2023.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Sun W, Yu Y, Yuan J, et al. Sleep duration and quality among different occupations–China national study. PLOS One. 2015;10(3):e0117700. doi: 10.1371/journal.pone.0117700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farah NM, Yee TS, Mohd Rasdi HF.. Self-reported sleep quality using the Malay version of the Pittsburgh sleep quality index (PSQI-M) in Malaysian adults. Int J Environ Res Public Health. 2019;16(23):4750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang F, Biro E.. Determinants of sleep quality in college students: a literature review. Explore. 2021;17(2):170–177. doi: 10.1016/j.explore.2020.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Wu W, et al. Sleep quality and its associated factors among low-income adults in a rural area of China: a population-based study. Int J Environ Res Public Health. 2018;15(9):2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang Y, Zhao N.. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morin CM, Bjorvatn B, Chung F, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. 2021;87:38–45. doi: 10.1016/j.sleep.2021.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo J, Liu C, Wang X, et al. Relationships between depression, pain and sleep quality with doctor visits among community-based adults in North-west China. Public Health. 2017;147:30–38. doi: 10.1016/j.puhe.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 25.Wu H, Han S, Zhang G, et al. Health-related quality of life and determinants in North-China urban community residents. Health Qual Life Outcomes. 2020;18(1):280. doi: 10.1186/s12955-020-01522-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goldthorpe HJ, Keith H.. The social grading of occupations: a new approach and scale. Oxford: Clarendon PressG; 1974. [Google Scholar]
- 27.Lee CH, Sibley CG.. Sleep duration and psychological well-being among New Zealanders. Sleep Health. 2019;5(6):606–614. doi: 10.1016/j.sleh.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 28.Bor J, Cohen GH, Galea S.. Population health in an era of rising income inequality: USA, 1980-2015. Lancet. 2017;389(10077):1475–1490. doi: 10.1016/S0140-6736(17)30571-8. [DOI] [PubMed] [Google Scholar]
- 29.Guo E, et al. Socioeconomic disparities in health care consumption: using the 2018-China family panel studies. Int J Environ Res Public Health. 2022;19(12):7359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borowiec AA, Drygas W.. Work-Life balance and mental and physical health among Warsaw specialists, managers and entrepreneurs. Int J Environ Res Public Health. 2022;20(1):492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin Y, Liu S, Li S, et al. Relationships between the changes in sleep patterns and sleep quality among Chinese people during the 2019 coronavirus disease outbreak. Sleep Med. 2022;91:154–160. doi: 10.1016/j.sleep.2021.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Polo-Kantola P, Laine A, Kronholm E, et al. Gender differences in actual and preferred nocturnal sleep duration among Finnish employed population. Maturitas. 2016;94:77–83. doi: 10.1016/j.maturitas.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 33.John U, Meyer C, Rumpf H-J, et al. Relationships of psychiatric disorders with sleep duration in an adult general population sample. J Psychiatr Res. 2005;39(6):577–583. doi: 10.1016/j.jpsychires.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Liu X, Uchiyama M, Kim K, et al. Sleep loss and daytime sleepiness in the general adult population of Japan. Psychiatry Res. 2000;93(1):1–11. doi: 10.1016/s0165-1781(99)00119-5. [DOI] [PubMed] [Google Scholar]
- 35.Edinger JD, Arnedt JT, Bertisch SM, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2021;17(2):263–298. doi: 10.5664/jcsm.8988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cao X-L, Wang S-B, Zhong B-L, et al. The prevalence of insomnia in the general population in China: a meta-analysis. PLOS One. 2017;12(2):e0170772. doi: 10.1371/journal.pone.0170772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee PH, Marek J, Nalevka P.. Crowdsourced smartphone data reveal altered sleep/wake pattern in quarantined Chinese during the COVID-19 outbreak. Chronobiol Int. 2020;37(8):1181–1190. doi: 10.1080/07420528.2020.1792486. [DOI] [PubMed] [Google Scholar]
- 38.Lin L-Y, Wang J, Ou-Yang X-Y, et al. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021;77:348–354. doi: 10.1016/j.sleep.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen X, Wang R, Zee P, et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic study of atherosclerosis (MESA). Sleep. 2015;38(6):877–888. doi: 10.5665/sleep.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baldwin CM, Ervin A-M, Mays MZ, et al. Sleep disturbances, quality of life, and ethnicity: the sleep heart health study. J Clin Sleep Med. 2010;06(02):176–183. doi: 10.5664/jcsm.27768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.O'Connor GT, et al. Variation in symptoms of sleep-disordered breathing with race and ethnicity: the sleep heart health study. Sleep. 2003;26(1):74–79. [PubMed] [Google Scholar]
- 42.Sweetman A, Lack L, Bastien C.. Co-morbid insomnia and sleep apnea (COMISA): prevalence, consequences, methodological considerations, and recent randomized controlled trials. Brain Sci. 2019;9(12):371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith S, Sullivan K, Hopkins W, et al. Frequency of insomnia report in patients with obstructive sleep Apnoea hypopnea syndrome (OSAHS). Sleep Med. 2004;5(5):449–456. doi: 10.1016/j.sleep.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 44.Lichstein KL, Riedel BW, Lester KW, et al. Occult sleep apnea in a recruited sample of older adults with insomnia. J Consult Clin Psychol. 1999;67(3):405–410. doi: 10.1037//0022-006x.67.3.405. [DOI] [PubMed] [Google Scholar]
- 45.Gooneratne NS, Gehrman PR, Nkwuo JE, et al. Consequences of comorbid insomnia symptoms and sleep-related breathing disorder in elderly subjects. Arch Intern Med. 2006;166(16):1732–1738. doi: 10.1001/archinte.166.16.1732. [DOI] [PubMed] [Google Scholar]
- 46.Guilleminault C, Palombini L, Poyares D, et al. Chronic insomnia, postmenopausal women, and sleep disordered breathing: part 1. Frequency of sleep disordered breathing in a cohort. J Psychosom Res. 2002;53(1):611–615. doi: 10.1016/s0022-3999(02)00445-2. [DOI] [PubMed] [Google Scholar]
- 47.Valko PO, Hunziker S, Graf K, et al. Sleep-wake misperception. A comprehensive analysis of a large sleep lab cohort. Sleep Med. 2021;88:96–103. doi: 10.1016/j.sleep.2021.10.023. [DOI] [PubMed] [Google Scholar]
- 48.Tsai SC. Excessive sleepiness. Clin Chest Med. 2010;31(2):341–351. doi: 10.1016/j.ccm.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 49.Dubrovsky B, Janal MN, Lavigne GJ, et al. Depressive symptoms account for differences between self-reported versus polysomnographic assessment of sleep quality in women with myofascial TMD. J Oral Rehabil. 2017;44(12):925–933. doi: 10.1111/joor.12552. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data are available upon reasonable request.