Abstract
This comprehensive literature review addresses the scarcity and limited study of hypotension treatments compared to abundant antihypertensive drugs. Hypotension, categorized as absolute, relative, or orthostatic, has diverse causes. This review explores various treatments, including drugs affecting the sympathetic nervous system, such as midodrine, dihydroergotamine, and ergotamine, which have shown efficacy in managing hypotension. Dopamine agonists/antagonists and other drugs such as ephedrine, norepinephrine, and fludrocortisone are also discussed, each with distinct mechanisms and applications. Additionally, adjunctive agents such as non-steroidal anti-inflammatory agents, caffeine, and monoamine oxidase inhibitors are reviewed for their effects on blood pressure. This review underscores the importance of understanding the efficacy and safety profiles of hypotension treatments to guide healthcare professionals in optimal drug selection and management, emphasizing the need for further research and comparative studies for evidence-based guidelines.
Keywords: adrenergic medications, norepinephrine reuptake inhibitors, autonomic control, cardiovascular, hypotension
Introduction and background
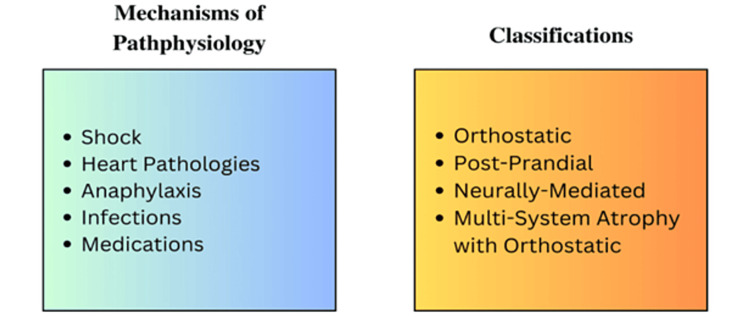
The definition of hypotension can vary but is commonly accepted as a decrease in blood pressure, typically identified as values lower than 90/60 mmHg [1]. Hypotension can also be identified by utilizing mean arterial pressure, with pressures less than 65 mmHg considered hypotensive [1]. The maintenance of blood pressure is controlled by the ability of the sympathetic nervous system to increase blood pressure through the constriction of arterioles and an increase in heart rate, as well as the ability of the parasympathetic nervous system to lower blood pressure [1]. There are four major classifications for hypotension, which include orthostatic hypotension, postprandial hypotension, neurally mediated hypotension, and multiple system atrophy with orthostatic hypotension [2]. Various bodily mechanisms can lead to a hypotensive state, including shock, heart pathologies, anaphylaxis, infections, and side effects of medications [2], as depicted in Figure 1. Given the various human conditions and pathologies, many drugs in today’s medical field are used to combat hypotension, and each available drug has a unique mechanism of action that may make one more suitable for a specific hypotensive condition.
Figure 1. Causes and classification of hypotension.
Image credits: Ghafary Suliman.
Review
Drugs affecting the sympathetic nervous system to manage hypotension
Midodrine
Midodrine is a Food and Drug (FDA)-approved drug used to treat orthostatic hypotension. It functions as an α-1 agonist by binding to alpha-adrenergic receptors, stimulating the constriction of arteries and veins [3]. Midodrine has been reported to increase standing systolic blood pressure, reduce lightheadedness symptoms, and improve global symptom relief scores for both patients and investigators [4]. Additionally, midodrine has been reported to alleviate symptoms of intradialytic hypotension [3]. The most common adverse effects in patients taking midodrine include pilomotor reactions, urinary retention, and supine hypertension [4]. Hypotensive patients with spinal cord injury receiving midodrine 10 mg have significantly elevated blood pressure and decreased episodes of hypotension [5].
Ergotamine
Ergotamine is commonly used to treat migraines due to its vasoactive properties. Ergotamine tartrate has a structural similarity to norepinephrine, epinephrine, dopamine, and serotonin, allowing it to act as an α-1 receptor agonist and a serotonin receptor agonist [6]. These vasoactive properties of ergotamine can also be used to treat hypotension. However, the oral bioavailability of ergotamine is less than 1%, which limits its effectiveness as a treatment for hypotension [6]. To improve its effectiveness and oral absorption rate, ergotamine is often combined with caffeine. A study reported that the combination of ergotamine and caffeine increased systolic blood pressure and improved presyncopal symptoms [7].
Yohimbine
Yohimbine is an α-2 receptor antagonist and, as a result, it increases plasma epinephrine and norepinephrine concentrations, which, in turn, raise heart rate, systolic blood pressure, and local blood flow [8]. These effects of yohimbine can make it a useful treatment for hypotension. In particular, yohimbine is used to treat orthostatic hypotension induced by the tricyclic antidepressant clomipramine. A study reports that patients suffering from clomipramine-induced hypotension and treated with yohimbine experienced a significant increase in systolic pressure when in an upright position, as well as an improvement in dizziness [9]. Another study reported that yohimbine also increased standing diastolic blood pressure and presyncope symptoms in patients with neurogenic orthostatic hypotension [10]. However, yohimbine has limited availability in the United States and is only marketed as a dietary supplement. Consequently, yohimbine is not typically used to treat hypotension in the United States.
Droxidopa
Droxidopa is an FDA-approved drug used to treat neurogenic orthostatic hypotension (nOH). nOH is caused by a decrease in the production of norepinephrine due to postganglionic sympathetic neuron degeneration and, as a result, deficient vascular adrenoceptor activation. Sympathetic neuron degeneration is commonly observed in conditions such as Parkinson’s disease, pure autonomic failure, or multiple system atrophy. Droxidopa can compensate for the decrease in norepinephrine because it is converted into norepinephrine by the aromatic amino acid decarboxylase, an enzyme abundantly expressed throughout the body. Studies have reported that droxidopa increases systolic blood pressure and improves symptoms of orthostatic hypotension. Droxidopa is generally well tolerated, but its side effects include nausea, dizziness, vision disturbances, weakness, and fatigue [11].
Dobutamine
Dobutamine is currently on the market as a short-term FDA-approved drug that affects the β adrenoceptors of the heart. It is mainly prescribed for the treatment of cardiogenic shock, heart failure, and in those with low blood pressure from decreased cardiac output. In one drug trial of dobutamine versus milrinone, it was found that higher outpatient hospital mortality risks were associated with dobutamine. Additionally, because of its cardiac effects dobutamine might cause worsening of tachycardia symptoms, introduce heart arrhythmias, and increase the myocardial oxygen demand [12]. However, it should be noted that the study did not directly measure hypotension outcomes, but rather mortality as the primary outcome which could have been influenced by other medications, changes in renal function, and other confounding influences. Other studies of dobutamine versus milrinone seem to contradict these findings and showed milrinone was associated with longer hospital stays, more intensive care unit admissions, and increased necessity for renal replacement therapy, but no significant difference in mortality outcomes between the two groups [13]. Additional studies have shown that it may be effective in the treatment of hypotensive preterm neonates as it improves mean arterial pressure, superior vena cava blood flow, and higher right ventricular outputs in comparison to treatments of dopamine [14,15].
Ephedrine
Ephedrine is both an alpha and beta-receptor agonistic activator. It releases norepinephrine by indirect activation and leads to α-1 and β-1 effects [16], with β-1 increasing the heart rate and α-1 causing peripheral vasoconstriction. Ephedrine is indicated for use in patients for prophylaxis and in cases of maternal hypotension during labor. In a sample of 80 full-term parturients, those who were given ephedrine via rapid intravenous bolus, compared to the placebo, showed a significant increase in heart rate and blood pressure [17]. Additionally, 150 patients undergoing valve surgery who were administered 0.07 to 0.1 mg/kg of ephedrine before propofol anesthesia showed improvements in mean arterial pressure, systemic vascular resistance index, cardiac index, stroke volume index, and left ventricular stroke work index [18]. Dusitkasem et al. showed that ephedrine does have an increased risk for fetal tachycardia and acidosis [19].
Norepinephrine
Norepinephrine is a potent vasoconstrictor and a precursor to epinephrine. Its main action is to increase systemic vascular resistance and heart rate. Norepinephrine is commonly indicated for use in cases of shock and hypotension [16]. Hasanin et al. compared norepinephrine to phenylephrine in a double-blinded controlled trial and showed that norepinephrine effectively maintained maternal systolic blood pressure [20]. While the study did show favorable outcomes for reduced post-spinal epidural hypotension, there were adverse effects such as nausea, vomiting, bradycardia, and dry gangrene.
Epinephrine is both a strong alpha-adrenoceptor and beta-adrenoceptor agonist [21]. It is another potent vasoconstrictor. Beta effects are shown at lower levels to increase both cardiac output and heart rate compared to α-1, which, at higher levels, is shown to increase both afterload and mean arterial pressure [16]. Wang et al. compared the effectiveness of epinephrine to phenylephrine during cesarean delivery, which demonstrated that maternal hypotension, bradycardia, nausea, and vomiting were similar in both groups, with the incidence of maternal bradycardia being reduced in the epinephrine group [21]. The study also concluded that there was a greater umbilical artery pH in the epinephrine group, suggesting that it is associated with better uteroplacental perfusion.
Etilefrine
Etilefrine is a well-known α-1 adrenergic receptor agonist and is known to be a potent vasoconstrictor, increasing blood pressure. Etilefrine is useful in the treatment of orthostatic hypotension induced by clozapine. Etilefrine therapy showed a decrease in the orthostatic reaction. Adverse effects include nausea, tremors, and palpitations [22].
Dopamine
Dopamine is synthesized via the same sequence as norepinephrine and is a precursor to norepinephrine. Dopamine works in a dosage-dependent fashion. At low infusion rates, it binds to alpha and beta receptors, causing vasodilation. At intermediate doses, it stimulates beta receptors, increasing myocardial contractility, SA rate, and impulse conduction in the heart. At high rates, dopamine affects alpha receptors, causing vasoconstriction and a rise in blood pressure. Therefore, dopamine is utilized to treat hemodynamic imbalances in shock [23-25]. The findings are summarized in Table 1.
Table 1. Drugs that affect the sympathetic nervous system.
HT: hydroxytryptamine; CNS: central nervous system
| Medication, author, year, and country | Study population | Mechanism of action | Benefits | Adverse effects/Other comments |
| Midodrine: Low et al., 1997, United States [4] | 171 | α-1 receptor agonist | Increases standing systolic blood pressure and alleviates intradialytic hypotension | Pilomotor reactions, urinary retention, supine hypertension, scalp paraesthesias, and heartburn |
| Ergotamine: Arnold et al., 2014, United States [7] | 12 | α-1 receptor agonist 5HT receptor agonist | Increases systolic blood pressure and improves presyncope symptoms | Nausea, headache, malaise, vomiting. Contraindicated in patients with coronary or peripheral artery disease |
| Yohimbine: Lecrubier et al., 1981, France [9] | 11 | α-2 receptor antagonist | Treats clomipramine-induced hypotension | Nervousness, insomnia, anxiety, and increased urinary frequency |
| Droxidopa: Kaufmann et al., 2014, United States [11] | 162 | Increases norepinephrine concentration | Increases systolic blood pressure and improves neurologic orthostatic hypotension symptoms | Nausea, dizziness, vision disturbance, weakness, and fatigue |
| Dobutamine: Zhu et al., 2021, China [13] | 235 | β-adrenoceptor agonist | Less cardiac arrhythmia occurrence, shorter hospital stays, and less requirement of renal replacement therapy in comparison to milrinone | Cardiotoxic and might induce cardiomyopathy |
| Ephedrine: Biricik et al., 2021, Turkey [16] | Electronic literature review | α and β receptor agonist. This leads to the activation of β-1, which increases heart rate | Used in the treatment of prophylaxis and maternal hypotension | Palpitations, headaches, dizziness, nausea, and vomiting. Contraindicated in patients with acute hypertension/tachycardia |
| Norepinephrine: Biricik et al., 2021, Turkey [16] | Electronic literature review | Stimulates α-1 receptors | Used for treatment of type 1 anaphylactic reactions | Tachycardia, hypertension, headache, and anxiety |
| Epinephrine: Hasanin et al., 2023, Egypt [20] | 271 | Acts on α-1 receptors | Used for the treatment of type 1 anaphylactic reactions | Tachycardia, hypertension, headache, and anxiety |
| Etilefrine: Tanzer et al., 2022, Australia [22] | Electronic literature review | α-agonist with a potent vasoconstrictor | Increases blood pressure and reduces symptoms of hypotension such as dizziness and headaches | CNS effects, difficulty with micturition |
| Dopamine: Li et al., 2020, Taiwan [23] | 7,410 | α-receptor- and β-receptor-stimulating actions | Naturally occurring potent vasoconstrictor and an inotropic agent | Greater mortality has a higher incidence of arrhythmic events than that of norepinephrine and alters hypothalamic-pituitary function. Decreases prolactin and growth hormone levels, pulmonary vasodilator. Vasoconstrictive effects are preserved during hypoxia and severe acidosis |
Norepinephrine-dopamine reuptake inhibitors
Atomoxetine
Atomoxetine is a selective norepinephrine reuptake inhibitor. It increases norepinephrine levels peripherally, and it dramatically raises blood pressure at small doses, specifically at doses of 18 mg. This medication can be useful in patients with severe symptoms of orthostatic hypotension, and it has been proven to be safe and effective, even in the elderly population. The side effects of atomoxetine include an increased heart rate and a significant increase in seated and standing systolic blood pressure when compared with placebo and current standards of care, such as midodrine. It has also been shown to raise systolic blood pressure only in patients with an intact central nervous system to avoid hypertension in patients treated with this drug [26]. The findings are summarized in Table 2.
Table 2. Norepinephrine-dopamine reuptake inhibitors.
| Article name, author, year, country | Study population | Mechanism of action | Benefits | Adverse effects/Other comments |
| Atomoxetine Patel et al., 2018, United States [26] | Electronic literature review limited to human studies from January 2000 to May 2017 | Increases norepinephrine levels and raises blood pressure with small doses | Improves orthostatic hypotension | Side effects include increased heart rate. Patients must have an intact central nervous system to avoid hypertension |
Other classes of targets for treating hypotension
Fludrocortisone
Fludrocortisone is a synthetic mineralocorticoid and is commonly used to treat hypotension. As a mineralocorticoid, fludrocortisone increases the rate of sodium reabsorption and water retention [27]. Studies have shown that fludrocortisone increases systolic blood pressure, improves symptoms, and decreases orthostatic tachycardia in patients suffering from neurogenic orthostatic hypotension caused by diabetic neuropathy or Parkinson’s disease [28,29]. The most common adverse effects include supine hypertension, peripheral edema, and headaches [27,29]. The use of fludrocortisone is contraindicated in treating patients with hypertension, hyperalbuminemia, and systemic fungal infections [27].
Pyridostigmine
Pyridostigmine belongs to a class of cholinesterase inhibitors and works to increase levels of acetylcholine, a neurotransmitter involved in muscle movement. Typically used in the treatment of myasthenia gravis, pyridostigmine may be prescribed off-label or in clinical trials for other conditions such as hypotension. In a comparison trial of pyridostigmine bromide versus fludrocortisone, the latter seemed to be more effective in raising mean arterial blood pressure and peripheral systolic supine blood pressure. Side effects of pyridostigmine bromide included softening of stool, lowered sodium levels, increased heart rate on Schellong maneuver, dizziness, and dry mouth [28]. Compared to midodrine, pyridostigmine also induced supine systolic blood pressure. The most effective treatment for hypotension appeared to be a combination trial of both midodrine and pyridostigmine to improve both systolic and diastolic blood pressure. Researchers noted side effects such as headaches, dizziness, gastrointestinal upsets, limb tremors, and potentially depression, lethargy, and sleep disturbances [30,31]. Similarly, the combination of pyridostigmine with other medications such as atomoxetine and propranolol or bisoprolol proved to be more efficacious than solely pyridostigmine [32,33].
Octreotide
Octreotide is a synthetic peptide that acts as a somatostatin analog, mimicking the action of somatostatin. Primarily used in other conditions such as acromegaly, gastroenteropancreatic neuroendocrine tumors, esophageal varices, or secretory diarrhea, octreotide may also be used off-label for postprandial hypotension. Octreotide improved fasting postural hypotension, fatigue, dizziness, standing heart rate, orthostatic syncope, increased stroke distance, cardiac index, resting skin temperature, systemic vascular resistance, and lowered plasma insulin levels but did not improve exercise-induced hypotension. It should be noted, however, that the effects of octreotide may be transient, with the first injection treatment having the most efficacy. Octreotide was well tolerated with no effects on nausea, abdominal cramps, or pain, though caution should be exercised for those with liver cirrhosis [34-36]. It is also known to increase supine hypertension, with researchers recommending the choice of other hypotensive therapies such as midodrine, mestinon, and subcutaneous octreotide instead of the very expensive intravenous octreotide [37].
Acarbose
Acarbose is an α-glucosidase inhibitor. It is largely used to treat type 2 diabetes because it slows down the small intestine’s enzymatic breakdown of carbohydrates. This enables more efficient metabolization of absorbed glucose. Acarbose may also be used to treat postprandial hypotension (PPH) in patients with severe autonomic failure because of its ability to effectively attenuate the drop in blood pressure that occurs after meals. Treatment with acarbose can cause a decrease in plasma insulin levels via lowering plasma glucose levels. As insulin is a recognized vasodilator, lowering its plasma levels reduces PPH [38]. Acarbose has a similar safety profile to placebo. Very rare instances of reversible liver transaminase elevations have been reported [39]. The findings are summarized in Table 3.
Table 3. Other classes of targets for treating hypotension.
| Medication, author, year, country | Study population | Mechanism of action | Benefits | Adverse effects/Other comments |
| Fludrocortisone: Campbell et al., 1976, United Kingdom [29] | 14 | Increases sodium reabsorption and water retention | Increases systolic blood pressure | Use caution in patients with congestive cardiac failure or nephrotic syndrome |
| Pyridostigmine: Byuan et al., 2017, South Korea [30] | 87 | Cholinesterase inhibitor | Improves orthostatic blood pressure drops and increases supine systolic blood pressure | Aggravated dizziness, headache, gastrointestinal upsets (nausea and diarrhea), limb tremors, and visual disturbances. Can potentially cause depression, lethargy, and sleep disturbances |
| Octreotide: Smith et al., 1995, United Kingdom [34] | 18 | Somatostatin analog | Improves fasting postural hypotension before exercise, blood pressure quicker to recover to pre-exercise levels, increases heart stroke distance, increases heart cardiac index, increases resting skin temperature, and lowers plasma insulin levels | Does not seem to reduce exercise-induced hypotension |
| Acarbose: Shibao et al., 2007, United States [38] | 13 | α-glucosidase inhibitor | Treats type 2 diabetes by slowing down the breakdown of carbohydrates | Similar safety profile to placebo. Very rare instances of elevated liver transaminases |
Adjunctive therapy
Non-steroidal Anti-inflammatory Agents
The primary mode of action for non-steroidal anti-inflammatory drugs (NSAIDs) involves blocking the action of the enzyme cyclooxygenase, essential for the formation of eicosanoids, leading to the therapeutic effects attributed to the reduced levels of these eicosanoids [40]. The FDA approved as antipyretic, anti-inflammatory, and analgesic agents, NSAIDs prove beneficial in addressing conditions such as muscle pain, dysmenorrhea, arthritis, pyrexia, gout, migraines, and serving as opioid-sparing agents in certain acute trauma cases [41,42]. However, the use of NSAIDs is associated with well-known adverse effects. In patients with renal dysfunction, the diminished prostaglandins via NSAIDs can lead to renal complications and electrolyte imbalance [43]. Potential cardiovascular adverse effects include myocardial infarction, thromboembolic events, and atrial fibrillation [44]. NSAIDs are not recommended in patients with hypersensitivity or salicylate hypersensitivity, previous allergic reactions, a history of coronary artery bypass graft surgery, and pregnant women during the third trimester [45].
Caffeine
Caffeine is an alkaloid and acts as an adenosine receptor blocker by competition mode, leading to a compensatory increase in adenosine. This subsequently stimulates circulating chemoreceptors and other receptors. This cascade results in heightened sympathetic tone, increased levels of catecholamines, peripheral vascular resistance, and augmented renin secretion. The net effect is an elevation in blood pressure [46]. At rest, caffeine is believed to enhance endothelial cell function by elevating intracellular calcium, prompting the expression of endothelial nitric oxide synthase, and thereby stimulating nitric oxide production [46]. Indirect tests in healthy individuals suggest improved endothelial cell function and vasodilation at rest. Therefore, adults engaging in daily activities while consuming this amount of caffeine are likely safe, given they are not caffeine-sensitive, pregnant, taking medications interacting with caffeine, or having medical conditions diminished by caffeine [47]. Various studies found minor changes in hemodynamic parameters, a slight increase in sympathetic activity, and subtle alterations in cardiac electrophysiological functions [48]. However, caution is advised for those consuming caffeine immediately before or during exercise, as it may potentially impede the typical physiological mechanisms supporting increased myocardial blood flow during heightened exercise requirements [47].
Monoamine Oxidase Inhibitors
Monoamine oxidase inhibitors (MAOIs) function by blocking the monoamine oxidase enzyme. This results in the breaking down of multiple neurotransmitters, such as tyramine, norepinephrine, serotonin, and dopamine, in the brain. By inhibiting the breakdown of these neurotransmitters, MAOIs elevate their levels, allowing them to persist and influence cells affected by depression [49]. Distinct from other antidepressants, MAOIs are effective in treating various forms of depression and addressing nervous system disorders such as panic disorder, social phobia, and depression with atypical features [50]. Additionally, MAOIs show benefits for patients with neurological disorders such as Parkinson’s disease and multiple system atrophy [51]. Common side effects include dry mouth, nausea, diarrhea, constipation, drowsiness, insomnia, dizziness, and lightheadedness. If administered via a patch, there is a possibility of a skin reaction at the patch site [52]. Individuals with a history of seizures or epilepsy, alcoholism, angina, severe headaches, blood vessel disease, diabetes, kidney or liver disease, recent heart attack or stroke, overactive thyroid, or pheochromocytoma should avoid MAOI therapy to prevent a hypertensive crisis [53]. MAOIs carry the risk of drug-to-drug interactions, drug-food interactions, and overdoses. Patients need to be cautious, avoiding combinations with other antidepressants such as selective serotonin reuptake inhibitors [54]. The findings are summarized in Table 4.
Table 4. Adjunctive agents used in the management of hypotension.
| Medication, author, year, country | Study population | Mechanism of action | Benefits | Adverse effects/Other comments |
| Non-steroidal anti-inflammatory drugs: Vane, 1971, United States [40] | Electronic literature review | Inhibit cyclooxygenase, which increases vasoconstriction | Treats muscle pain, dysmenorrhea, arthritic conditions, and migraines | Adverse effects on the renal and cardiovascular systems. Patients can experience allergic reactions |
| Caffeine: Echeverri et al., 2010, England [46] | Electronic literature review | Increases adenosine, which increases peripheral vascular resistance | Increases blood pressure and improves endothelial cell function | Minor alterations in heart rate and blood pressure accompanied by an elevation in sympathetic activity. Considered safe for patients unless they are reactive to caffeine, pregnant, or other drugs that are not compatible with it |
| Monoamine oxidase inhibitors: Baker et al., 1992, United States [49] | Electronic literature review | Block monoamine oxidase enzyme inhibits the breakdown of neurotransmitters | Treats depression as well as other nervous system disorders | Mouth dryness, nausea, constipation, diarrhea, and sleeplessness are some of the side effects. Monoamine oxidase inhibitors may cause a hypertensive crisis |
Conclusions
This review underscores the diversity of drugs targeting different mechanisms to address hypotension, emphasizing their effectiveness in managing symptoms as well as highlighting associated risks, including adverse effects and potential drug interactions. The prescription of these medications should consider individual patient characteristics and underlying conditions. Ongoing monitoring of patients on hypotension drugs is crucial for identifying and managing potential adverse effects or interactions. This analysis concludes by emphasizing the importance of personalized treatment approaches and expressing optimism about advancing medical research for a more comprehensive understanding of hypotension and improved patient outcomes. The need for further research is emphasized to enhance understanding, safety assessment, and establish evidence-based guidelines through clinical trials across diverse patient populations. For example, future studies could examine the effectiveness of combining pharmacological and non-pharmacological interventions for a synergistic approach to managing orthostatic hypertension. Additionally, another study could assess the long-term effects of various treatments on patient outcomes, including cardiovascular events, quality of life, and overall mortality. Lastly, future studies could assess the feasibility and effectiveness of personalized treatment plans based on patient characteristics, including age, comorbidities, and the underlying cause of orthostatic hypertension.
Acknowledgments
Our special thanks to California Health Sciences University College of Osteopathic Medicine (CHSU-COM) for their continuous support.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Sudhakar Pemminati, Zeyu Yu, Thomas Abel, Thangwaritorn Skylynn, Ghafary Suliman, Rivera Dominic, Lee Christopher, Varughese Joel
Acquisition, analysis, or interpretation of data: Sudhakar Pemminati, Zeyu Yu, Thomas Abel, Ghafary Suliman, Varughese Joel
Drafting of the manuscript: Sudhakar Pemminati, Zeyu Yu, Thomas Abel, Thangwaritorn Skylynn, Ghafary Suliman, Rivera Dominic, Lee Christopher, Varughese Joel
Critical review of the manuscript for important intellectual content: Sudhakar Pemminati
Supervision: Sudhakar Pemminati
References
- 1.Sharma S, Hashmi MF, Bhattacharya PT. Treasure Island, FL: StatPearls Publishing; 2023. Hypotension. [Google Scholar]
- 2.Hypotension: a clinical care review. Saljoughian M. https://www.uspharmacist.com/article/hypotension-a-clinical-care-review US Pharm. 2018;39:2–4. [Google Scholar]
- 3.Midodrine appears to be safe and effective for dialysis-induced hypotension: a systematic review. Prakash S, Garg AX, Heidenheim AP, House AA. Nephrol Dial Transplant. 2004;19:2553–2558. doi: 10.1093/ndt/gfh420. [DOI] [PubMed] [Google Scholar]
- 4.Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension. A randomized, double-blind multicenter study. Midodrine Study Group. Low PA, Gilden JL, Freeman R, Sheng KN, McElligott MA. JAMA. 1997;277:1046–1051. [PubMed] [Google Scholar]
- 5.Clinical trial of home blood pressure monitoring following midodrine administration in hypotensive individuals with spinal cord injury. Wecht JM, Weir JP, Katzelnick CG, Dyson-Hudson TA, Bauman WA, Kirshblum SC. J Spinal Cord Med. 2023;46:531–539. doi: 10.1080/10790268.2021.1977904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ergotamine and dihydroergotamine: a review. Bigal ME, Tepper SJ. Curr Pain Headache Rep. 2003;7:55–62. doi: 10.1007/s11916-003-0011-7. [DOI] [PubMed] [Google Scholar]
- 7.Combination ergotamine and caffeine improves seated blood pressure and presyncopal symptoms in autonomic failure. Arnold AC, Ramirez CE, Choi L, et al. Front Physiol. 2014;5:270. doi: 10.3389/fphys.2014.00270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.A literature perspective on the pharmacological applications of yohimbine. Jabir NR, Firoz CK, Zughaibi TA, et al. Ann Med. 2022;54:2861–2875. doi: 10.1080/07853890.2022.2131330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Favourable effects of yohimbine on clomipramine-induced orthostatic hypotension: a double-blind study. Lecrubier Y, Puech AJ, Des Lauriers A. Br J Clin Pharmacol. 1981;12:90–93. doi: 10.1111/j.1365-2125.1981.tb01863.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Comparative efficacy of yohimbine against pyridostigmine for the treatment of orthostatic hypotension in autonomic failure. Shibao C, Okamoto LE, Gamboa A, et al. Hypertension. 2010;56:847–851. doi: 10.1161/HYPERTENSIONAHA.110.154898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Droxidopa for neurogenic orthostatic hypotension: a randomized, placebo-controlled, phase 3 trial. Kaufmann H, Freeman R, Biaggioni I, et al. Neurology. 2014;83:328–335. doi: 10.1212/WNL.0000000000000615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Effect of inpatient dobutamine versus milrinone on out-of-hospital mortality in patients with acute decompensated heart failure. King JB, Shah RU, Sainski-Nguyen A, Biskupiak J, Munger MA, Bress AP. Pharmacotherapy. 2017;37:662–672. doi: 10.1002/phar.1939. [DOI] [PubMed] [Google Scholar]
- 13.The effect of dobutamine vs milrinone in sepsis: a big data, real-world study. Zhu Y, Yin H, Zhang R, Ye X, Wei J. Int J Clin Pract. 2021;75:0. doi: 10.1111/ijcp.14689. [DOI] [PubMed] [Google Scholar]
- 14.Randomized trial of dobutamine versus dopamine in preterm infants with low systemic blood flow. Osborn D, Evans N, Kluckow M. J Pediatr. 2002;140:183–191. doi: 10.1067/mpd.2002.120834. [DOI] [PubMed] [Google Scholar]
- 15.Response to dobutamine and dopamine in the hypotensive very preterm infant. Rozé JC, Tohier C, Maingueneau C, Lefèvre M, Mouzard A. Arch Dis Child. 1993;69:59–63. doi: 10.1136/adc.69.1_spec_no.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vasopressors for the treatment and prophylaxis of spinal induced hypotension during caesarean section. Biricik E, Ünlügenç H. Turk J Anaesthesiol Reanim. 2021;49:3–10. doi: 10.5152/TJAR.2020.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Comparing slow and rapid bolus of ephedrine in pregnant patients undergoing planned cesarean section under spinal anesthesia. Gunasekaran P, Elakkumanan LB, Balachander H, Satyaprakash MV. J Anaesthesiol Clin Pharmacol. 2017;33:92–96. doi: 10.4103/0970-9185.202183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Preoperative ephedrine counters hypotension with propofol anesthesia during valve surgery: a dose dependent study. El-Tahan MR. Ann Card Anaesth. 2011;14:30–40. doi: 10.4103/0971-9784.74397. [DOI] [PubMed] [Google Scholar]
- 19.Comparison of phenylephrine and ephedrine in treatment of spinal-induced hypotension in high-risk pregnancies: a narrative review. Dusitkasem S, Herndon BH, Somjit M, Stahl DL, Bitticker E, Coffman JC. Front Med (Lausanne) 2017;4:2. doi: 10.3389/fmed.2017.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The use of epinephrine infusion for the prevention of spinal hypotension during caesarean delivery: a randomized controlled dose-finding trial. Hasanin AM, Abou Amer A, Hassabelnaby YS, et al. Anaesth Crit Care Pain Med. 2023;42:101204. doi: 10.1016/j.accpm.2023.101204. [DOI] [PubMed] [Google Scholar]
- 21.Comparison of continuous infusion of epinephrine and phenylephrine on hemodynamics during spinal anesthesia for cesarean delivery: a randomized controlled trial. Wang YB, Yang ZY, Zhang WP. Clin Ther. 2020;42:2001–2009. doi: 10.1016/j.clinthera.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Treatment strategies for clozapine-induced hypotension: a systematic review. Tanzer TD, Brouard T, Pra SD, et al. Ther Adv Psychopharmacol. 2022;12:20451253221092931. doi: 10.1177/20451253221092931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Comparison of dopamine and norepinephrine use for the treatment of hypotension in out-of-hospital cardiac arrest patients with return of spontaneous circulation. Li CJ, Wu KH, Chen CC, Law YY, Chuang PC, Chen YC. Emerg Med Int. 2020;2020:7951025. doi: 10.1155/2020/7951025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Comparison of dopamine and norepinephrine in the treatment of shock. De Backer D, Biston P, Devriendt J, et al. N Engl J Med. 2010;362:779–789. doi: 10.1056/NEJMoa0907118. [DOI] [PubMed] [Google Scholar]
- 25.Vasopressin versus dopamine for treatment of hypotension in extremely low birth weight infants: a randomized, blinded pilot study. Rios DR, Kaiser JR. J Pediatr. 2015;166:850–855. doi: 10.1016/j.jpeds.2014.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Evaluating the effectiveness of atomoxetine for the treatment of primary orthostatic hypotension in adults. Patel H, Simpson A, Palevoda G, Hale GM. J Clin Hypertens (Greenwich) 2018;20:794–797. doi: 10.1111/jch.13260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rahman M, Anjum F. Treasure Island, FL: StatPearls Publishing; 2023. Fludrocortisone. [PubMed] [Google Scholar]
- 28.Pyridostigmine bromide versus fludrocortisone in the treatment of orthostatic hypotension in Parkinson's disease - a randomized controlled trial. Schreglmann SR, Büchele F, Sommerauer M, et al. Eur J Neurol. 2017;24:545–551. doi: 10.1111/ene.13260. [DOI] [PubMed] [Google Scholar]
- 29.Therapeutic experience with fludrocortisone in diabetic postural hypotension. Campbell IW, Ewing DJ, Clarke BF. Br Med J. 1976;1:872–874. doi: 10.1136/bmj.1.6014.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Efficacy of single or combined midodrine and pyridostigmine in orthostatic hypotension. Byun JI, Moon J, Kim DY, et al. Neurology. 2017;89:1078–1086. doi: 10.1212/WNL.0000000000004340. [DOI] [PubMed] [Google Scholar]
- 31.Pyridostigmine treatment trial in neurogenic orthostatic hypotension. Singer W, Sandroni P, Opfer-Gehrking TL, et al. Arch Neurol. 2006;63:513–518. doi: 10.1001/archneur.63.4.noc50340. [DOI] [PubMed] [Google Scholar]
- 32.Synergistic pressor effect of atomoxetine and pyridostigmine in patients with neurogenic orthostatic hypotension. Okamoto LE, Shibao CA, Gamboa A, et al. Hypertension. 2019;73:235–241. doi: 10.1161/HYPERTENSIONAHA.118.11790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Efficacy of propranolol, bisoprolol, and pyridostigmine for postural tachycardia syndrome: a randomized clinical trial. Moon J, Kim DY, Lee WJ, et al. Neurotherapeutics. 2018;15:785–795. doi: 10.1007/s13311-018-0612-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Effect of the somatostatin analogue, octreotide, on exercise-induced hypotension in human subjects with chronic sympathetic failure. Smith GD, Alam M, Watson LP, Mathias CJ. Clin Sci (Lond) 1995;89:367–373. doi: 10.1042/cs0890367. [DOI] [PubMed] [Google Scholar]
- 35.Long-term haemodynamic effects of octreotide on postprandial splanchnic hyperemia in humans: a placebo-controlled echo-doppler study. Ludwig D, Terai S, Brüning A, Stange EF. Aliment Pharmacol Ther. 1999;13:1119–1129. doi: 10.1046/j.1365-2036.1999.00583.x. [DOI] [PubMed] [Google Scholar]
- 36.Octreotide effects on orthostatic hypotension in patients with multiple system atrophy: a controlled study of acute administration. Bordet R, Benhadjali J, Destée A, Belabbas A, Libersa C. Clin Neuropharmacol. 1995;18:83–89. doi: 10.1097/00002826-199502000-00012. [DOI] [PubMed] [Google Scholar]
- 37.Treatment of autonomic neuropathy, postural tachycardia and orthostatic syncope with octreotide LAR. Hoeldtke RD, Bryner KD, Hoeldtke ME, Hobbs G. Clin Auton Res. 2007;17:334–340. doi: 10.1007/s10286-007-0436-x. [DOI] [PubMed] [Google Scholar]
- 38.Acarbose, an alpha-glucosidase inhibitor, attenuates postprandial hypotension in autonomic failure. Shibao C, Gamboa A, Diedrich A, Dossett C, Choi L, Farley G, Biaggioni I. Hypertension. 2007;50:54–61. doi: 10.1161/HYPERTENSIONAHA.107.091355. [DOI] [PubMed] [Google Scholar]
- 39.Critical evaluation of the role of acarbose in the treatment of diabetes: patient considerations. Rosak C, Mertes G. Diabetes Metab Syndr Obes. 2012;5:357–367. doi: 10.2147/DMSO.S28340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Vane JR. Nat New Biol. 1971;231:232–235. doi: 10.1038/newbio231232a0. [DOI] [PubMed] [Google Scholar]
- 41.Analgesic pharmacology: II. Specific analgesics. Phillips WJ, Currier BL. J Am Acad Orthop Surg. 2004;12:221–233. doi: 10.5435/00124635-200407000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Nonopioid management of acute pain associated with trauma: focus on pharmacologic options. Oyler DR, Parli SE, Bernard AC, Chang PK, Procter LD, Harned ME. J Trauma Acute Care Surg. 2015;79:475–483. doi: 10.1097/TA.0000000000000755. [DOI] [PubMed] [Google Scholar]
- 43.Nephrotoxicity of nonsteroidal anti-inflammatory drugs: physiologic foundations and clinical implications. Whelton A. Am J Med. 1999;106:13–24. doi: 10.1016/s0002-9343(99)00113-8. [DOI] [PubMed] [Google Scholar]
- 44.Adverse effects of nonsteroidal antiinflammatory drugs: an update of gastrointestinal, cardiovascular and renal complications. Harirforoosh S, Asghar W, Jamali F. J Pharm Pharm Sci. 2013;16:821–847. doi: 10.18433/j3vw2f. [DOI] [PubMed] [Google Scholar]
- 45.Ghlichloo I, Gerriets V. Treasure Island, FL: StatPearls Publishing; 2023. Nonsteroidal Anti-inflammatory Drugs. [PubMed] [Google Scholar]
- 46.Caffeine's vascular mechanisms of action. Echeverri D, Montes FR, Cabrera M, Galán A, Prieto A. Int J Vasc Med. 2010;2010:834060. doi: 10.1155/2010/834060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Caffeine reduces myocardial blood flow during exercise. Higgins JP, Babu KM. Am J Med. 2013;126:730–738. doi: 10.1016/j.amjmed.2012.12.023. [DOI] [PubMed] [Google Scholar]
- 48.The effect of caffeine on ventricular ectopic activity in patients with malignant ventricular arrhythmia. Graboys TB, Blatt CM, Lown B. Arch Intern Med. 1989;149:637–639. [PubMed] [Google Scholar]
- 49.Insights into the mechanisms of action of the MAO inhibitors phenelzine and tranylcypromine: a review. Baker GB, Coutts RT, McKenna KF, Sherry-McKenna RL. https://pubmed.ncbi.nlm.nih.gov/1362653/ J Psychiatry Neurosci. 1992;17:206–214. [PMC free article] [PubMed] [Google Scholar]
- 50.Reducing the burden of difficult-to-treat major depressive disorder: revisiting monoamine oxidase inhibitor therapy. Culpepper L. Prim Care Companion CNS Disord. 2013;15:0. doi: 10.4088/PCC.13r01515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Diagnostic approach to atypical Parkinsonian syndromes. McFarland NR. Continuum (Minneap Minn) 2016;22:1117–1142. doi: 10.1212/CON.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.The role of monoamine oxidase inhibitors in current psychiatric practice. Fiedorowicz JG, Swartz KL. J Psychiatr Pract. 2004;10:239–248. doi: 10.1097/00131746-200407000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dietary restrictions and drug interactions with monoamine oxidase inhibitors: the state of the art. Rapaport MH. https://pubmed.ncbi.nlm.nih.gov/17640157/ J Clin Psychiatry. 2007;68 Suppl 8:42–46. [PubMed] [Google Scholar]
- 54.Dietary restrictions and drug interactions with monoamine oxidase inhibitors: an update. Flockhart DA. J Clin Psychiatry. 2012;73 Suppl 1:17–24. doi: 10.4088/JCP.11096su1c.03. [DOI] [PubMed] [Google Scholar]