Abstract
The incidence of acute rheumatic fever (ARF), which most commonly affects children aged 5-15 years after group A Streptococcus (GAS) infection, ranges from 8 to 51 per 100 000 people worldwide. Rheumatic heart disease (RHD), which occurs when patients with ARF are inappropriately treated or not given regular prophylaxis, is the most common cause of non-congenital heart disease in children and young adults in low-income countries. Timely treatment of GAS infection can prevent ARF, and penicillin prophylaxis can prevent recurrence of ARF. Secondary prophylaxis with benzathine penicillin G has been shown to decrease the incidence of RHD and is a key aspect of RHD control. The most important factor determining the prognosis of RHD is the severity of cardiac involvement. Although approximately 70% of patients with carditis in the acute phase of the disease recover without sequelae, carditis is important because it is the only complication of ARF that causes sequelae. One-third of patients with ARF are asymptomatic. Patients with mild symptoms of recurrent ARF and silent RHD will develop severe morbidities within 5-10 years if they do not receive secondary preventive treatments. A new screening program should be established to prevent cardiac morbidities of ARF in moderate- and high-risk populations. In the present study, we examined the applicability of echocardiographic screening programs for RHD.
Keywords: Acute rheumatic fever, rheumatic heart disease, echocardiography, echocardiographic screening
Introduction
Acute rheumatic fever (ARF) results from an autoimmune response to pharyngitis induced by group A Streptococcus (GAS) (Streptococcus pyogenes). It is characterized by inflammation affecting different regions of the body, including inflammation of the joints (polyarthritis) and heart with associated valvular regurgitation. Although approximately 70% of patients with carditis in the acute phase of the disease recover without sequelae, it is the only clinically important complication of ARF that has sequelae. Autoimmune inflammation of the basal ganglia may result in chorea, but this is rare. The progression of ARF is generally an acute process, resolving in 3-4 weeks; however, inflammation of the heart, particularly the valves, may result in rheumatic heart disease (RHD). Acute rheumatic fever itself is not life-threatening, but RHD can cause severe morbidities including heart failure and stroke, which can result in death.
The diagnosis of subclinical RHD requires systematic and active screening of children and young adults in the general population. However, such screening is very costly and may not be suitable for low-income countries. Subclinical RHD can be recognized by echocardiographic scans, and the progression of the disease can then be prevented.1 Echocardiography can also detect disease progression, and its findings are reproducible. In very heterogeneous populations, screening for RHD by auscultation in low-risk areas and by echocardiography in high-risk areas may be helpful. Echocardiographic screening in low-risk areas may cause unnecessary concern to children and their families. In addition, the benefit of treating subclinical RHD remains unclear.2
Excluding the resurgence of the disease in some high-income countries, RHD is mostly seen in low- and moderate-income countries. The high seroprevalence of the disease results in some diagnostic challenges.
We performed a literature search of PubMed, Embase, the Cochrane Library, the Cochrane Central Register of Controlled Trials, Web of Science, Scopus, Google Scholar, and Medline Plus to identify studies published as original articles in English. We investigated the feasibility of echocardiographic screening for ARF and RHD in high-risk populations and the possibility of reducing the cardiac morbidity and mortality associated with these diseases. The cost of screening and the availability of health-care professionals were also considered in these analyses.
Pathogenesis
The pathogenesis of ARF is incompletely understood. Evidence suggests that ARF is an autoimmune response to pharyngeal disease, and there may be a genetic predisposition component.3 Streptococcal antigens activate the humoral and cell-dependent immune systems and cause tissue injury by cross-reacting with human proteins.4 The structural similarity between myosin epitopes and heart valve proteins such as laminin and vimentin is thought to be responsible for antibody-dependent damage to the heart valves.5 The binding of cross-reactive antibodies to the heart valve surface activates vascular cell adhesion molecule 1,6 which in turn activates the tissue adhesion and infiltrating properties of CD4 T cells and B lymphocytes. Local tissue damage within the valve is mainly caused by the T-helper 1 cell response.7 This inflammation eventually resolves and is replaced by fibrosis, resulting in RHD.
Epidemiology
Group A Streptococcushas no natural hosts apart from humans. In low-income countries, the incidence of RHD is increasing because of poverty, overcrowded living conditions, and lack of easy access to hygiene and health-care services. There is a direct association between the prevalence of RHD and poverty, malnutrition, and inadequate health-care resources in such countries.8,9
The Global Burden of Disease study revealed 33.4 million cases of RHD worldwide in 2015, leading to approximately 320 000 deaths.10 Even with these RHD-related deaths, the age-standardized mortality rate decreased by 47.8% in the 25 years leading up to 2015 (1990-2015).10 The incidence of ARF and RHD varies markedly worldwide; it can also vary between regions within the same country, especially in areas with different socioeconomic statuses.11 During the 20th century, the incidence of ARF and the prevalence of RHD tended to decrease in developed countries.12 In high-income countries, ARF and RHD have not been a public health concern during the past 4 to 6 decades. However, random cases can still occur,13 and temporary resurgence of the disease is seen in some of these countries.8
Diagnosis
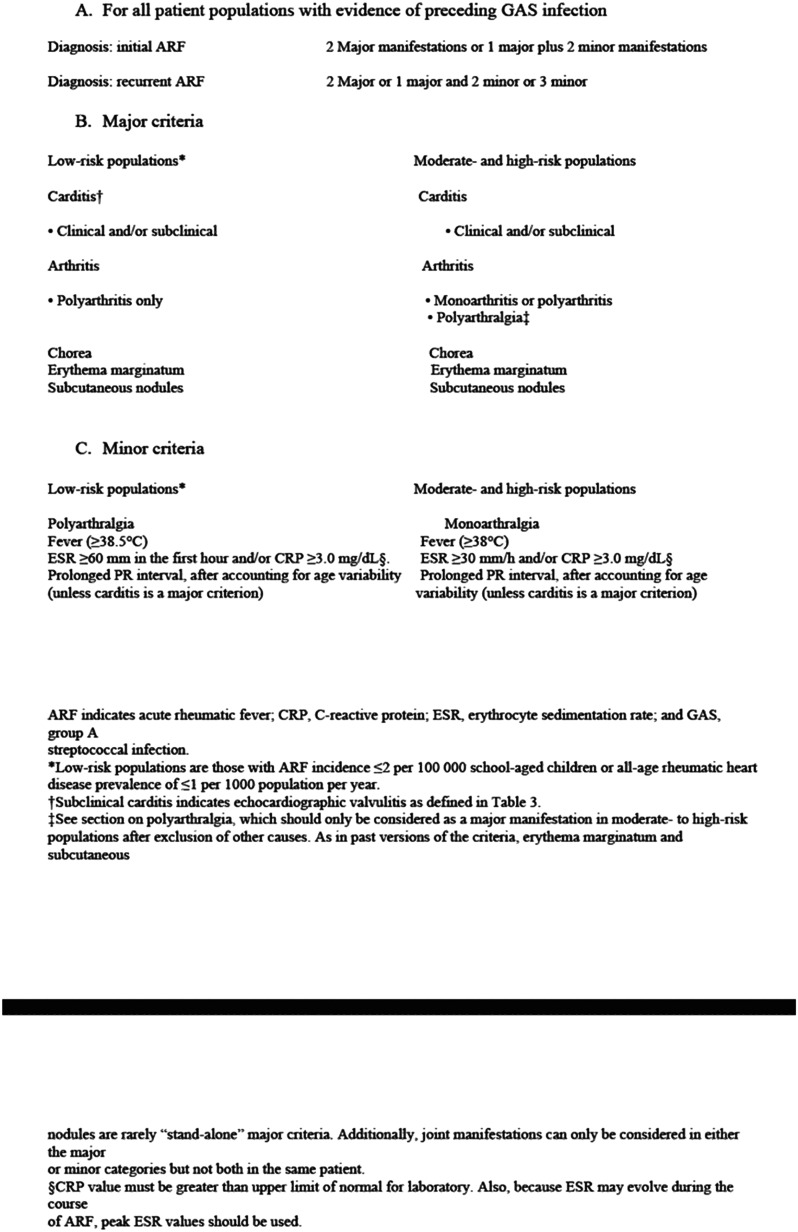
The diagnosis of ARF depends on laboratory findings and clinical symptoms. Diagnosis is confirmed by the application of clinical criteria (revised Jones criteria) and exclusion of other differential diagnoses (Box 1). In 2015, the American Heart Association revised the 1992 Jones criteria.14 The aim of the revision was to maximize the sensitivity of the criteria for ARF in endemic areas and to support high specificity in low-risk areas. In the revised Jones criteria, echocardiography is considered an indispensable diagnostic tool. In addition, diagnostic criteria for recurrent ARF were added to the revised Jones criteria. According to recent studies, the revised Jones criteria have increased the accuracy of the diagnosis of ARF in moderate- and high-risk populations and decreased the long-term sequelae of subclinical RHD.15,16
Echocardiographic findings indicative of cardiac valve involvement are the most important findings for predicting RHD.17 Findings related to joint involvement are insufficient for the diagnosis of ARF. Only 15%-41% of patients with ARF have joint involvement.18 Therefore, in endemic areas, echocardiography should be performed in all children and adolescents with joint involvement who have an elevated erythrocyte sedimentation rate or C-reactive protein concentration, even if no fever is present. In patients without carditis, the risk of developing it later is low. Because of the nature of the disease, recurrence is unlikely unless the initial infection causes cardiac damage that closely resembles the damage typically associated with RHD.19
Rheumatic heart disease should be diagnosed according to the echocardiographic criteria established by the World Heart Federation (WHF).1 An algorithm for the diagnosis of ARF and RHD is shown in Figure 1.
Figure 1.
Diagnoses of ARF and RHD are described according to the revised Jones criteria (2015) and World Heart Federation RHD diagnosis guidelines (2012). AR, aortic regurgitation; ARF, acute rheumatic fever; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; MR, mitral regurgitation; PR, pulmonary regurgitation; RHD, rheumatic heart disease.
Subclinical Rheumatic Heart Disease
Subclinical RHD is defined as the presence of echocardiographic signs of RHD in a patient with no symptoms of ARF. In previous studies, the natural course of subclinical RHD was characterized by persistence or progression of lesions in 53%-68% of patients over 6-30 months of follow-up.20,21 In a more recent study, 48% of cases of persistence or progression were detected in patients with subclinical RHD.22 It is important to detect individuals with subclinical RHD to ensure that they receive prophylactic antibiotic treatment and follow-up. The only way to detect individuals with subclinical RHD is to carry out echocardiographic screening programs in endemic areas.
Borderline Rheumatic Heart Disease
The definition of borderline RHD is reserved for individuals aged <20 years (Box 2).1 Individuals in this age range are unlikely to show echocardiographic features that are sufficient to meet the criteria for definitive RHD because cardiac pathologies often take time to develop.23,24 Borderline RHD is diagnosed when at least 1 of the following 2 criteria is met: the patient has pathological mitral regurgitation or mitral stenosis (Figure 2) or at least 2 morphological features of RHD of the mitral valve without pathological aortic regurgitation (Figure 3). Such patients should be followed up because these mild findings may progress to serious disease over time, potentially leading to definitive RHD in the future. These patients are most likely to benefit from secondary prophylaxis.
Figure 2.
Echocardiologic view of mitral valve sequel in RHD. A) Moderate mitral regurgitation due to rheumatic heart disease (arrow) B) Chronic changes in the mitral valve, thickening, irregularity, and prolapse tip of the anterior mitral valve leaflet (long arrow), and limitation of movement of the posterior mitral valve leaflet (short arrow). Ao, aorta; LA, left atrium; LV, left ventricle; MV, mitral valve; MVAL, mitral valve-anterior leaflet; MVPL, mitral valve-posterior leaflet; RHD, rheumatic heart disease.
Figure 3.
Echocardiologic view of aortic valve sequel in RHD. Severe aortic regurgitation due to rheumatic heart disease (black arrow). Ao, aorta; LA, left atrium; LV, left ventricle; MV, mitral valve.
Few studies to date have evaluated the progression of borderline RHD detected by echocardiography. In a study of 55 Aboriginal Australians, a 23% rate of progression to definitive RHD was detected during a follow-up period of 2.5 to 5.0 years.25 In a study conducted in Uganda, improvement of RHD was seen in 18 of 43 patients, and only 4 of the 43 patients developed definitive RHD over the 2-year follow-up period.26 These studies concluded that the disease progression was mostly due to morphological changes in the mitral valve and less commonly due to aortic valve involvement.
The incidence of valvular regurgitation increases after the age of 20 years. Therefore, the definition of borderline RHD is not appropriate for patients older than 20 years.27,28 The WHF criteria for echocardiographic diagnosis of RHD, including definitive RHD and borderline RHD, are shown in Box 2.1
Prevention and Treatment of Acute Rheumatic Fever and Rheumatic Heart Disease
Four main objectives are considered in the prevention and treatment of ARF: primordial prevention, treatment of pharyngeal GAS infection, prevention of RHD and treatment of arthritis and chorea (other complications of ARF), and (in patients with RHD) continuation of treatment to prevent chronic heart disease.
Primordial Prevention
Both ARF and RHD are more common in poor people living in crowded families with conditions of poor hygiene. The most important strategy to reduce the incidence of ARF is to improve the living situation of these communities. Unfortunately, such improvement is not easy to accomplish in low- and middle-income societies. Being a member of a low- or middle-income population increases the risk of developing ARF and delays the treatment of the disease. Even some developed countries with heterogeneous social populations, such as Australia and New Zealand, have been attempting numerous strategies to protect their lower-income citizens from ARF for many years; however, they have not yet been fully successful.29 Several reports have described the risk factors for ARF and RHD, which include living in an ARF-endemic geographic area, having a personal history of ARF or RHD, and being aged <40 years.30 Other possible risk factors are a recent history of ARF or RHD within the family or household, overcrowding of the household (>2 people per bedroom), a low socioeconomic status, and being a migrant or refugee from a low- or middle-income country (or being a child of such a migrant or refugee).30 The most commonly recommended practical interventions for individuals at high risk are ensuring good hygiene, especially by regular washing, and reducing the negative impacts of overcrowding.30
Primary Prevention
The first goal in patients with ARF is to treat and eradicate the GAS infection. Treatment generally involves a single intramuscular injection of benzathine benzylpenicillin. However, there are alternatives to this treatment, including oral phenoxymethylpenicillin, oral amoxicillin, oral cephalosporins, and high-dose azithromycin.31 These alternative treatments have similar efficacy to oral penicillin. Individuals with penicillin allergy should receive oral erythromycin (250 mg twice per day).32
Secondary Prevention
Although the abovementioned treatments are currently applied for ARF and RHD, their level of evidence is low. Few studies have compared treated and untreated individuals.33
Only 3 randomized controlled studies to date have compared the efficacy of penicillin for RHD with a control group,34-36 and the quality of the methodology applied in these studies was low. In one of these 3 studies, penicillin reduced the recurrence of RHD; however, approximately 25% of patients were not followed up.36 In another randomized controlled study that involved 10 220 Ugandan children and adolescents with subclinical RHD, patients who received penicillin (benzathine benzylpenicillin) prophylaxis for 2 years were compared to those who did not. Disease progression was reduced in the treatment group.37 More detailed studies are needed to elucidate the benefit of secondary antibiotic prophylaxis in patients with subclinical RHD.
The optimal time point at which to stop prophylaxis has not been established. However, a recent guideline recommended that individuals with moderate RHD should continue prophylaxis until the age of 30-35 years and that those with severe RHD should continue until the age of 40 years.38
There is no proven anti-inflammatory or immunosuppressive therapy to reduce or delay the progression of RHD. There is a need for randomized controlled trials to assess alternative therapies for RHD. Certain genomic and proteomic approaches may be useful to prevent the tissue damage associated with ARF and RHD. Some promising studies have focused on the therapeutic application of early plasma and tissue proteomic factors.39,40
Screening Program for Rheumatic Heart Disease
The only cost-effective approach to prevent recurrent ARF and avoid the sequelae of RHD is secondary prophylaxis by monthly intramuscular injections of long-term antibiotics.41 However, one-third of patients with ARF are asymptomatic. Patients with mild symptoms of recurrent ARF and silent RHD sequelae will develop severe morbidities within 5-10 years if they do not receive secondary preventive treatments. A new screening program should be established to prevent the cardiac morbidities of ARF for people who live in moderate- and high-risk populations.42,43
Cardiac Auscultation
Cardiac auscultation is the most important part of the cardiac examination and has long been used to detect the valvular pathology in patients with RHD. Cardiac auscultation can detect diastolic murmurs resulting from mitral regurgitation; in severe cases of mitral regurgitation, an additional diastolic murmur known as a Carey Coombs murmur may also be identified.44 However, research has shown that RHD can be detected by cardiac auscultation alone in only 10% of cases.45
Echocardiographic Screening for Rheumatic Heart Disease
Echocardiography is a noninvasive diagnostic tool that is more sensitive and specific than auscultation.20,46,47 Subclinical RHD, in which clinical signs of valvular regurgitation are absent, can be detected by echocardiography.46 Advances in technology have facilitated the manufacture of portal echocardiography devices. This developing technology has enabled echocardiography to be performed at low cost even in remote settings.48 Such interventions may support early diagnosis of RHD and reduce morbidity and mortality.
Several studies involving school-aged children have shown that echocardiographic scanning increases the diagnostic accuracy by 5 to 50 times compared to auscultation.49-51 The prevalence of RHD in these studies was 8-57/1000. If this is calculated for the entire worldwide population, then 62-78 million people are affected by RHD globally, and 1.4 million people will die of this disease annually.52
There is insufficient evidence to support echocardiographic screening for the detection of RHD in any given population. However, such screening should be considered in extreme circumstances, such as populations in which the incidence of RHD is suspected to be very high or when clusters of ARF are detected.53
Echocardiographic screening should only be considered in populations at high risk for RHD. Epidemiologic data are needed to estimate whether a society is at high risk. However, the true incidence of RHD cannot be estimated because of the silent progression of the disease. Hospitalization records for ARF, RHD, or both can be used to estimate the true incidence of the disease. School echocardiographic screening programs should be considered as an epidemiological tool to establish the disease burden. In one Australian study, 61% of cases of RHD were diagnosed in females.30 In geographic regions endemic to ARF, females of childbearing age should be screened by echocardiography before conception. If this is not possible, a nationwide health-care policy that includes mandatory echocardiographic screening of pregnant women in the first trimester of pregnancy should be established in endemic areas. Pregnancy may worsen the symptoms of RHD, including breathlessness, orthopnea, wheezing, and fatigue. Studies from South Africa and Senegal showed that 25% of all indirect maternal deaths in developing countries were caused by RHD.54,55
Families will benefit from a periodic echocardiographic screening program covered by the state and implemented under the supervision of health-care professionals.
Benefits of Echocardiographic Screening for Rheumatic Heart Disease
Subclinical RHD refers to echocardiographic evidence of RHD in the absence of symptoms or a history of ARF.56 Early diagnosis and administration of penicillin in individuals with subclinical RHD may reduce the risk for severe cardiac disease.57
According to the Turkey National Institute of Statistics, the incidence of ARF in Turkey was 8.84 per 100 000 population in the year 2016.58 We previously studied echocardiographic screening for RHD in school-aged children in Turkey and identified definitive subclinical RHD in 15 per 1000 school-aged children.59 The screening identified children who could receive secondary preventive therapy. In low-risk populations, the all-age prevalence of RHD is ≤1 per 1000 population per year.14 In the abovementioned study, screening for RHD in a moderate- to high-risk area resulted in treatment for approximately 15 per 1000 individuals. Treatment will prevent an estimated 20%-80% of cases of RHD progression.60 The rate of rheumatic valvular heart disease was 5.9%-13.0% after negative echocardiographic screening with an average follow-up of 2.6-3.5 years. In endemic geographic areas, repetitive echocardiographic screening should be considered because it can detect cases of subclinical RHD and new cases of definitive RHD even in patients with previously negative echocardiographic screening results.
Another advantage of such screening is the detection of some asymptomatic congenital heart diseases. Asymptomatic or undiagnosed pathologies may be detected, especially in individuals with atrial septal defects, patent ductus arteriosus, partial anomalous pulmonary venous return, and bicuspid aorta.59
The 2012 WHF criteria are limited with respect to the echocardiographic diagnosis of RHD. The aim is to differentiate mild RHD from normal findings in echocardiography. The WHF criteria were formulated based on 2-dimensional, color Doppler, and continuous-wave Doppler echocardiography. However, more sophisticated methods are available to determine the severity of valve pathology. In addition, the WHF criteria are relatively complex and can be misinterpreted by inexperienced echocardiographers. Another limitation is the possibility of misinterpreting other variations that cause mitral regurgitation, such as interscallop separations of the posterior mitral valve leaflet, as RHD.61 In addition, some valvular pathologies, such as mitral cleft and bicuspid aorta, can be mistakenly evaluated as RHD by nonexpert echocardiographers.
Implementation and Cost of Echocardiographic Screening for Rheumatic Heart Disease
Technological advances in the last 20 years have led to the widespread use of ultrasonographic techniques, including echocardiography.45,47 The development of handheld portable echocardiographic devices has made community screening easier to implement. Along with these technological developments, the WHF defined criteria for the echocardiographic diagnosis of RHD based on the presence of pathologic-grade left-sided valvular regurgitation and typical morphologic features of the valve leaflets in 2012.1
Handheld echocardiography devices show promise for use in RHD scanning programs. Initially, there were some concerns that their diagnostic sensitivity and specificity for RHD might be less than those of stable echocardiography devices. However, studies have shown that handheld echocardiography devices can diagnose RHD with a sensitivity of 79% and specificity of 87%, and the sensitivity is even higher at 97.9% in children with definitive RHD.62 Notably, the scarcity of trained health-care personnel who can perform echocardiographic screening is an obstacle to echocardiographic screening programs. In a study conducted in Fiji, 2 nurses who had undergone echocardiography training could detect mitral regurgitation with sufficient sensitivity and specificity.21 Such interventions can be applied in societies with insufficient human power.
Several studies have focused on the cost of echocardiographic screening.63-65 In a study in New Zealand, the cost of echocardiographic screening was 60-230 NZD per patient screened.65 To successfully implement screening programs, health policies should be developed together with the public, and sufficient funds should be allocated.
Conclusion
Echocardiography is a noninvasive imaging technique in which ultrasound is used to visualize the structure and function of the heart. It is considered the gold standard for diagnosing RHD. Echocardiographic screening involves the use of this imaging technique to assess the heart valves and identify any abnormalities or signs of RHD in asymptomatic individuals. The screening is typically performed by trained health-care professionals, such as cardiologists or sonographers.
The aim of such screening is to detect the disease at an early stage, when interventions can prevent further damage and complications. Screening allows for the identification of subclinical or silent RHD, in which individuals may not yet show symptoms despite the presence of underlying cardiac abnormalities. Early detection enables the initiation of appropriate treatment, such as prophylactic antibiotics to prevent recurrent streptococcal infections, as well as close monitoring of the condition to prevent disease progression.
Although echocardiographic screening has shown promise in identifying RHD, it also presents certain challenges. One of the main challenges is the need for trained personnel and access to echocardiographic equipment. In resource-limited settings, where the RHD burden is often high, there may be limited availability of skilled health-care providers and adequate imaging facilities. This poses a barrier to widespread implementation of screening programs.
Another consideration is the cost of screening. Conducting screenings on a large scale requires significant financial resources, and the long-term benefits and costs of such programs must be carefully evaluated. Research into the feasibility and impact of echocardiographic screening in different settings is ongoing.
The burden of RHD remains a significant concern, particularly in low- and middle-income countries. Echocardiographic screening has emerged as a valuable tool for early detection and monitoring of RHD. While there are challenges to implementing widespread screening programs, efforts are being made to improve access to health-care, increase awareness, and address the burden of this preventable and treatable disease.
Unfortunately, approximately 30%-40% of adults who have RHD do not recall having had ARF in the past. These individuals will be symptomatic for RHD at some point in their lives.59 Studies conducted in the mid-20th century showed that 40%-60% of people who had an ARF attack later developed RHD.60,66 After penicillin began to be used for the prevention of RHD, the rate of regression of mitral valve regurgitation increased from 20% to 80%.60 Patients with undiagnosed RHD can be expected to have a disease prognosis similar to that before the use of penicillin. Therefore, echocardiographic screening programs can be a lifesaving intervention for individuals living in moderate- or high-risk populations.
Notably, the families of the individuals to be included in a screening program do not always give consent. In a previous study, the families of 2550 of 4517 school-aged children gave permission for echocardiographic screening.59 Although psychological problems are not usually seen in patients with negative screening program results or in their families, long-term anxiety and behaviors such as prevention of physical activity are observed in 25% of families with positive results.67
There are no clear data regarding the optimal timing of the next echocardiographic screening test in individuals with negative echocardiographic screening results. In previous studies, RHD was detected at a rate of 5.9% (mean follow-up time of 3.5 years)30 and 13% (mean follow-up time of 2.6 years)68 in individuals followed up after negative screening results.
Indisputably, the primordial approach should be the first-choice strategy for preventing RHD. However, because changes in social habits and economic development of a region may take many years, screening programs in moderate- and high-risk regions can at least identify individuals at risk for RHD and provide them with support to receive secondary treatment.
| Box 1. Revised Jones Criteria for Acute Rheumatic Fever 2015. |
|
| Box 2. 2012. World Heart Federation Criteria for Echocardiographic Diagnosis of Rheumatic Heart Disease. |

|
Funding Statement
This study received no funding.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – S.T.; Design – S.T.; Supervision – T.U.; Literature Search – S.T., T.U.; Writing – S.T.; Critical Review – T.U.
Declaration of Interests: The authors have no conflict of interest to declare.
References
- 1. Reményi B, Wilson N, Steer A, et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease--an evidence-based guideline. Nat Rev Cardiol. 2012;9(5):297 309. ( 10.1038/nrcardio.2012.7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Haran S, Crane N, Kazi S, Axford-Haines L, White A. Effect of secondary penicillin prophylaxis on valvular changes in patients with rheumatic heart disease in Far North Queensland. Aust J Rural Health. 2018;26(2):119 125. ( 10.1111/ajr.12379) [DOI] [PubMed] [Google Scholar]
- 3. Machipisa T, Chishala C, Shaboodien G, et al. Rationale, design, and the baseline characteristics of the RHDGen (the genetics of rheumatic heart disease) network Studydagger. Circ Genom Precis Med. 2023;16(1):e003641. ( 10.1161/CIRCGEN.121.003641) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Machipisa T, Chong M, Muhamed B, et al. Association of novel locus with rheumatic heart disease in black African individuals: findings from the RHDGen study. JAMA Cardiol. 2021;6(9):1000 1011. ( 10.1001/jamacardio.2021.1627) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Surve NZ, Kerkar PG, Deshmukh CT, et al. A longitudinal study of antibody responses to selected host antigens in rheumatic fever and rheumatic heart disease. J Med Microbiol. 2021;70(5). ( 10.1099/jmm.0.001355). [DOI] [PubMed] [Google Scholar]
- 6. Rafeek RA, Hamlin AS, Andronicos NM, et al. Characterization of an experimental model to determine streptococcal M protein-induced autoimmune cardiac and neurobehavioral abnormalities. Immunol Cell Biol. 2022;100(8):653 666. ( 10.1111/imcb.12571) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kirvan CA, Canini H, Swedo SE, et al. IgG2 rules: N-acetyl-beta-D-glucosamine-specific IgG2 and Th17/Th1 cooperation may promote the pathogenesis of acute rheumatic heart disease and be a biomarker of the autoimmune sequelae of Streptococcus pyogenes. Front Cardiovasc Med. 2022;9:919700. ( 10.3389/fcvm.2022.919700) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alberio AMQ, Pieroni F, Di Gangi A, et al. Toward the knowledge of the epidemiological impact of acute rheumatic fever in Italy. Front Pediatr. 2021;9:746505. ( 10.3389/fped.2021.746505) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beaton A, Okello E, Scheel A, et al. Impact of heart disease on maternal, fetal and neonatal outcomes in a low-resource setting. Heart. 2019;105(10):755 760. ( 10.1136/heartjnl-2018-313810) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Watkins DA, Johnson CO, Colquhoun SM, et al. Global, regional, and national burden of rheumatic heart disease, 1990-2015. N Engl J Med. 2017;377(8):713 722. ( 10.1056/NEJMoa1603693) [DOI] [PubMed] [Google Scholar]
- 11. Carapetis JR, Beaton A, Cunningham MW, et al. Acute rheumatic fever and rheumatic heart disease. Nat Rev Dis Primers. 2016;2:15084. ( 10.1038/nrdp.2015.84) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ou Z, Yu D, Liang Y, et al. Global burden of rheumatic heart disease: trends from 1990 to 2019. Arthritis Res Ther. 2022;24(1):138. ( 10.1186/s13075-022-02829-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bennett J, Zhang J, Leung W, et al. Rising ethnic inequalities in acute rheumatic fever and rheumatic heart disease, New Zealand, 2000-2018. Emerg Infect Dis. 2021;27(1):36 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gewitz MH, Baltimore RS, Tani LY, et al. Revision of the Jones criteria for the diagnosis of acute rheumatic fever in the era of Doppler echocardiography: a scientific statement from the American Heart Association. Circulation. 2015;131(20):1806 1818. ( 10.1161/CIR.0000000000000205) [DOI] [PubMed] [Google Scholar]
- 15. Beaton A, Carapetis J. The 2015 revision of the Jones criteria for the diagnosis of acute rheumatic fever: implications for practice in low-income and middle-income countries. Heart Asia. 2015;7(2):7 11. ( 10.1136/heartasia-2015-010648) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Szczygielska I, Hernik E, Kołodziejczyk B, Gazda A, Maślińska M, Gietka P. Rheumatic fever – new diagnostic criteria. Reumatologia. 2018;56(1):37 41. ( 10.5114/reum.2018.74748) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arvind B, Ramakrishnan S. Rheumatic fever and rheumatic heart disease in children. Indian J Pediatr. 2020;87(4):305 311. ( 10.1007/s12098-019-03128-7) [DOI] [PubMed] [Google Scholar]
- 18. Wojdas M, Dąbkowska K, Kuźnik-Trocha K, et al. Plasma glycosaminoglycans in children with juvenile idiopathic arthritis being treated with etanercept as potential biomarkers of joint dysfunction. Biomedicines. 2022;10(8):1845. ( 10.3390/biomedicines10081845) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dennison A, Peat B, Wilson E, et al. Rheumatic fever recurrences in New Zealand 2010-14. N Z Med J. 2020;133(1516):47 57. [PubMed] [Google Scholar]
- 20. Paar JA, Berrios NM, Rose JD, et al. Prevalence of rheumatic heart disease in children and young adults in Nicaragua. Am J Cardiol. 2010;105(12):1809 1814. ( 10.1016/j.amjcard.2010.01.364) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bhaya M, Beniwal R, Panwar S, Panwar RB. Two years of follow-up validates the echocardiographic criteria for the diagnosis and screening of rheumatic heart disease in asymptomatic populations. Echocardiography. 2011;28(9):929 933. ( 10.1111/j.1540-8175.2011.01487.x) [DOI] [PubMed] [Google Scholar]
- 22. Zühlke L, Engel ME, Karthikeyan G, et al. Characteristics, complications, and gaps in evidencebased interventions in rheumatic heart disease: the Global rheumatic heart disease Registry (the REMEDY study). Eur Heart J. 2015;36(18):1115 122a. ( 10.1093/eurheartj/ehu449) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vasan RS, Shrivastava S, Vijayakumar M, Narang R, Lister BC, Narula J. Echocardiographic evaluation of patients with acute rheumatic fever and rheumatic carditis. Circulation. 1996;94(1):73 82. ( 10.1161/01.cir.94.1.73) [DOI] [PubMed] [Google Scholar]
- 24. Câmara EJ, Neubauer C, Câmara GF, Lopes AA. Mechanisms of mitral valvar insufficiency in children and adolescents with severe rheumatic heart disease: an echocardiographic study with clinical and epidemiological correlations. Cardiol Young. 2004;14(5):527 532. ( 10.1017/S1047951104005104) [DOI] [PubMed] [Google Scholar]
- 25. Rwebembera J, Beaton A, Okello E, et al. Comparison of approaches to determine echocardiographic outcomes for children with latent rheumatic heart disease. Open Heart. 2022;9(2):e002160. ( 10.1136/openhrt-2022-002160). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nader V, Matta A, Canitrot R, et al. Evaluation of mitral and aortic valvular disease and left ventricular dysfunction in a Lebanese population: retrospective single-center experience. Med Sci Monit. 2021;27:e928218. ( 10.12659/MSM.928218) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Reid CL, Anton-Culver H, Yunis C, Gardin JM. Prevalence and clinical correlates of isolated mitral, isolated aortic regurgitation, and both in adults aged 21 to 35 years (from the CARDIA study). Am J Cardiol. 2007;99(6):830 834. ( 10.1016/j.amjcard.2006.10.048) [DOI] [PubMed] [Google Scholar]
- 28. Singh JP, Evans JC, Levy D, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol. 1999;83(6):897 902. ( 10.1016/s0002-9149(98)01064-9) [DOI] [PubMed] [Google Scholar]
- 29. Barth DD, Mullane MJ, Sampson C, et al. Missing Piece study protocol: prospective surveillance to determine the epidemiology of group A streptococcal pharyngitis and impetigo in remote Western Australia. BMJ Open. 2022;12(4):e057296. ( 10.1136/bmjopen-2021-057296) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ralph AP, Noonan S, Wade V, Currie BJ. The 2020 Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease. Med J Aust. 2021;214(5):220 227. ( 10.5694/mja2.50851) [DOI] [PubMed] [Google Scholar]
- 31. Mutagaywa RK, Wind AM, Kamuhabwa A, Cramer MJ, Chillo P, Chamuleau S. Rheumatic heart disease anno 2020: impacts of gender and migration on epidemiology and management. Eur J Clin Investig. 2020;50(12):e13374. ( 10.1111/eci.13374) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gopal R, Harikrishnan S, Sivasankaran S, Ajithkumar VK, Titus T, Tharakan JM. Once weekly azithromycin in secondary prevention of rheumatic fever. Indian Heart J. 2012;64(1):12 15. ( 10.1016/S0019-4832(12)60004-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Moran M, Guzman J, Ropars AL, et al. Neglected disease research and development: how much are we really spending? PLOS Med. 2009;6(2):e30. ( 10.1371/journal.pmed.1000030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kohn KH, Milzer A, Maclean H. Prophylaxis of recurrences of rheumatic fever with penicillin given orally; final report of a five year study. J Am Med Assoc. 1953;151(5):347 351. [PubMed] [Google Scholar]
- 35. Feinstein AR, Spagnuolo M, Levitt M, Jonas S, Tursky E. Discontinuation of antistreptococcal prophylaxis. A double-blind study in rheumatic patients free of heart disease. JAMA. 1966;197(12):949 952. ( 10.1001/jama.197.12.949) [DOI] [PubMed] [Google Scholar]
- 36. Padmavati S, Sharma KB, Jayaram O. Epidemiology and prophylaxis of rheumatic fever in Delhi—a five year follow-up. Singapore Med J. 1973;14(3):457 461. [PubMed] [Google Scholar]
- 37. Beaton A, Okello E, Rwebembera J, et al. Secondary antibiotic prophylaxis for latent rheumatic heart disease. N Engl J Med. 2022;386(3):230 240. ( 10.1056/NEJMoa2102074) [DOI] [PubMed] [Google Scholar]
- 38. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients with valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521 e643. ( 10.1161/CIR.0000000000000031) [DOI] [PubMed] [Google Scholar]
- 39. Faé KC, Diefenbach da Silva D, Bilate AM, et al. PDIA3, HSPA5 and vimentin, proteins identified by 2-DE in the valvular tissue, are the target antigens of peripheral and heart infiltrating T cells from chronic rheumatic heart disease patients. J Autoimmun. 2008;31(2):136 141. ( 10.1016/j.jaut.2008.04.023) [DOI] [PubMed] [Google Scholar]
- 40. Gao G, Xuan C, Yang Q, Liu XC, Liu ZG, He GW. Identification of altered plasma proteins by proteomic study in valvular heart diseases and the potential clinical significance. PLoS ONE. 2013;8(8):e72111. ( 10.1371/journal.pone.0072111) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wood HF, Simpson R, Feinstein AR, Taranta A, Tursky E, Stollerman G. Rheumatic fever in children and adolescents. A long-term epidemiologic study of subsequent prophylaxis, streptococcal infections, and clinical sequelae. I. Description of the investigative techniques and of the population studied. Ann Intern Med. 1964;60(suppl 5):SUPPL 5:6 SUPPL 517. ( 10.7326/0003-4819-60-2-6) [DOI] [PubMed] [Google Scholar]
- 42. Ma'u E, Cullum S, Cheung G, Livingston G, Mukadam N. Differences in the potential for dementia prevention between major ethnic groups within one country: A cross sectional analysis of population attributable fraction of potentially modifiable risk factors in New Zealand . Lancet Reg Health West Pac. 2021;13:100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rwebembera J, Nascimento BR, Minja NW, et al. Recent advances in the rheumatic fever and rheumatic heart disease continuum. Pathogens. 2022;11(2). ( 10.3390/pathogens11020179) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Seitler S, Zuhair M, Shamsi A, et al. Cardiac imaging in rheumatic heart disease and future developments. Eur Heart J Open. 2023;3(2):oeac060. ( 10.1093/ehjopen/oeac060) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Marijon E, Ou P, Celermajer DS, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med. 2007;357(5):470 476. ( 10.1056/NEJMoa065085) [DOI] [PubMed] [Google Scholar]
- 46. Marijon E, Celermajer DS, Tafflet M, et al. Rheumatic heart disease screening by echocardiography: the inadequacy of World Health Organization criteria for optimizing the diagnosis of subclinical disease. Circulation. 2009;120(8):663 668. ( 10.1161/CIRCULATIONAHA.109.849190) [DOI] [PubMed] [Google Scholar]
- 47. Carapetis JR, Hardy M, Fakakovikaetau T, et al. Evaluation of a screening protocol using auscultation and portable echocardiography to detect asymptomatic rheumatic heart disease in Tongan schoolchildren. Nat Clin Pract Cardiovasc Med. 2008;5(7):411 417. ( 10.1038/ncpcardio1185) [DOI] [PubMed] [Google Scholar]
- 48. Rwebembera J, Beaton AZ, de Loizaga SR, et al. The global impact of rheumatic heart disease. Curr Cardiol Rep. 2021;23(11):160. ( 10.1007/s11886-021-01592-2) [DOI] [PubMed] [Google Scholar]
- 49. Basnet K, Bhattarai SR, Shah S, et al. Rheumatic heart disease among patients with valvular heart disease admitted to the in-patient department of a tertiary Care Centre: A descriptive crosssectional study. JNMA J Nepal Med Assoc. 2022;60(249):419 424. ( 10.31729/jnma.7457) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ali F, Hasan B, Ahmad H, et al. Detection of subclinical rheumatic heart disease in children using a deep learning algorithm on digital stethoscope: a study protocol. BMJ Open. 2021;11(8):e044070. ( 10.1136/bmjopen-2020-044070) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Saxena A, Ramakrishnan S, Roy A, et al. Prevalence and outcome of subclinical rheumatic heart disease in India: the RHEUMATIC (Rheumatic Heart Echo Utilisation and Monitoring Actuarial Trends in Indian Children) study. Heart. 2011;97(24):2018 2022. ( 10.1136/heartjnl-2011-300792) [DOI] [PubMed] [Google Scholar]
- 52. Zühlke L, Mayosi BM. Echocardiographic screening for subclinical rheumatic heart disease remains a research tool pending studies of impact on prognosis. Curr Cardiol Rep. 2013;15(3):343. ( 10.1007/s11886-012-0343-1) [DOI] [PubMed] [Google Scholar]
- 53. Francis JR, Fairhurst H, Hardefeldt H, et al. Hyperendemic rheumatic heart disease in a remote Australian town identified by echocardiographic screening. Med J Aust. 2020;213(3):118 123. ( 10.5694/mja2.50682) [DOI] [PubMed] [Google Scholar]
- 54. Soma-Pillay P, MacDonald AP, Mathivha TM, Bakker JL, Mackintosh MO. Cardiac disease in pregnancy: a 4-year audit at Pretoria Academic Hospital. S Afr Med J. 2008;98(7):553 556. [PubMed] [Google Scholar]
- 55. Diao M, Kane A, Ndiaye MB, et al. Pregnancy in women with heart disease in sub-Saharan Africa. Arch Cardiovasc Dis. 2011;104(6-7):370 374. ( 10.1016/j.acvd.2011.04.001) [DOI] [PubMed] [Google Scholar]
- 56. Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet. 2012;379(9819):953 964. ( 10.1016/S0140-6736(11)61171-9) [DOI] [PubMed] [Google Scholar]
- 57. Noubiap JJ, Agbor VN, Bigna JJ, Kaze AD, Nyaga UF, Mayosi BM. Prevalence and progression of rheumatic heart disease: a global systematic review and meta-analysis of population-based echocardiographic studies. Sci Rep. 2019;9(1):17022. ( 10.1038/s41598-019-53540-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gürses D, Koçak G, Tutar E, Özbarlas N, Turkish ARF study group. Incidence and clinical characteristics of acute rheumatic fever in Turkey: results of a nationwide multicentre study. J Paediatr Child Health. 2021;57(12):1949 1954. ( 10.1111/jpc.15619) [DOI] [PubMed] [Google Scholar]
- 59. Atalay S, Tutar E, Uçar T, Topçu S, Köse SK, Doğan MT. Echocardiographic screening for rheumatic heart disease in Turkish schoolchildren. Cardiol Young. 2019;29(10):1272 1277. ( 10.1017/S1047951119002075) [DOI] [PubMed] [Google Scholar]
- 60. Bland EF, Duckett Jones T. Rheumatic fever and rheumatic heart disease; a twenty year report on 1000 patients followed since childhood. Circulation. 1951;4(6):836 843. ( 10.1161/01.cir.4.6.836) [DOI] [PubMed] [Google Scholar]
- 61. Hunter LD, Monaghan M, Lloyd G, et al. Interscallop separations of the posterior mitral valve leaflet: a solution to the 'borderline RHD' conundrum? Open Heart. 2020;7(2):e001452. ( 10.1136/openhrt-2020-001452) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Beaton A, Lu JC, Aliku T, et al. The utility of handheld echocardiography for early rheumatic heart disease diagnosis: a field study. Eur Heart J Cardiovasc Imaging. 2015;16(5):475 482. ( 10.1093/ehjci/jeu296) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ubels J, Sable C, Beaton AZ, et al. Cost-Effectiveness of rheumatic heart disease Echocardiographic Screening in Brazil: data from the PROVAR+ Study: cost-effectiveness of RHD screening in Brazil. Glob Heart. 2020;15(1):18. ( 10.5334/gh.529) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Roberts K, Cannon J, Atkinson D, et al. Echocardiographic screening for rheumatic heart disease in Indigenous Australian children: A cost-utility analysis. J Am Heart Assoc. 2017;6(3):e004515. ( 10.1161/JAHA.116.004515) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bennett J, Rentta NN, Leung W, et al. Early diagnosis of acute rheumatic fever and rheumatic heartdisease as part of a secondary prevention strategy: narrative review. J Paediatr Child Health. 2021;57(9):1385 1390. ( 10.1111/jpc.15664) [DOI] [PubMed] [Google Scholar]
- 66. Ash R. Rheumatic infection in childhood; 15 to 20 year follow-up. Am J Dis Child (1911). 1948;76(1):46 52. ( 10.1001/archpedi.1948.02030030053005) [DOI] [PubMed] [Google Scholar]
- 67. Condemi F, Rossi G, Lupiz M, et al. Screening of asymptomatic rheumatic heart disease among refugee/migrant children and youths in Italy. Pediatr Rheumatol Online J. 2019;17(1):12. ( 10.1186/s12969-019-0314-9) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Zimmerman M, Scheel A, DeWyer A, et al. Determining the risk of developing rheumatic heart disease following a negative screening echocardiogram. Front Cardiovasc Med. 2021;8:632621. ( 10.3389/fcvm.2021.632621) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a 

