Abstract
Newborn hearing screening (NHS) programs are essential to identify hearing loss early in life and to improve outcomes in children. In Saudi Arabia, the national NHS program has been operational since 2016; however, few studies have evaluated its status, and none have covered all provinces across the country. This cross-sectional retrospective study provides an overview of the program's status across all provinces, focusing on screening coverage rates, referral/fail rates, and follow-up procedures. In 2021, 199,034 newborns were screened, with a coverage rate of 92.6% and an overall referral/fail rate of 1.87%. These performance measures provide a foundation for future progress and improvements. This study highlights the importance of ongoing efforts to enhance the program's effectiveness and sustainability.
Keywords: Hearing screening, Hearing loss, Newborn, Auditory brainstem response, Saudi Arabia
1. Introduction
Hearing loss is a major cause of disability globally (Banda et al., 2018). According to the World Health Organization (WHO), approximately 1.5 billion individuals suffer from hearing loss worldwide, with 1.1 billion young individuals at risk of permanent hearing loss (WHO, 2023). More than 2.5 billion individuals are predicted to suffer from disabling hearing loss by 2050 (WHO, 2023). According to Wood et al. (2015), permanent hearing loss affects 1 to 2 per 1000 newborns. In 2019, data from Centers for Disease Control and Prevention (CDC) reported a hearing loss prevalence of 1.7 per 1000 newborns. According to previous studies, the prevalence of sensorineural hearing loss in children in Saudi Arabia ranges between 7.7% (Bafaqeeh et al., 1994; Mathers et al., 2000) and 13% (Daghistani et al., 2002). Children are considered disabled if their hearing threshold exceeds 35 dB HL in the better-hearing ear (WHO, 2023). Even minimal hearing loss has a negative impact on quality of life. For example, the ability to understand soft speech in the presence of background noise or from a distance is impeded in children with hearing loss exceeding 26 dB HL (WHO, 2023).
The first major effect of hearing loss in children is a delay in their ability to develop receptive and expressive communication skills (Shukla et al., 2020). A consequence of communication disorders is a reduction in academic achievement owing to learning problems (Foster et al., 2023; Wren et al., 2021). Children with hearing loss have communication challenges, which cause feelings of loneliness, isolation, frustration, and a poor sense of self-worth (Shukla et al., 2020). In addition, hearing loss may influence career choices (Joint Committee on Infant Hearing (JCIH), 2000; Mehl and Thomson, 1998).
Researchers have found that early identification and intervention are key to minimizing or preventing the negative consequences of hearing loss (Yoshinaga-Itano, 2004; Kennedy et al., 2005; JCIH, 2007). The National Institutes of Health (NIH) recommends screening of all newborns for hearing loss before discharge from the hospital (NIH, 1993). It is, therefore, necessary to implement a universal newborn hearing screening (UNHS) program for early detection and intervention of congenital hearing loss. Before the implementation of the UNHS, only high-risk infants were tested. The UNHS program is increasingly used because 33–50% of congenital hearing loss cannot be detected by a selective hearing screening that includes only “at-risk” newborns (WHO, 2021). Despite hearing loss severity, early intervention before the age of 6 months can facilitate normal language development (WHO, 2023).
In Saudi Arabia, the national transformation program launched in 2016 aimed to achieve the country's “Vision, 2030.” The vision strategically aimed to strengthen the prevention of health threats (Saudi Vision, 2030). Early identification of hearing loss could not only prevent or reduce the negative consequences of hearing loss but could also significantly reduce the cost of rehabilitation programs for children with unidentified hearing loss (Mohr et al., 2000). In Saudi Arabia, a higher prevalence of hearing loss has been reported compared to the international prevalence of hearing loss (Al-Abduljawad and Zakzouk, 2003; Habib and Abdulgaffar, 2005; Maisoun and Zakzouk, 2003). However, these studies focused on an isolated region within the country. Other studies that have investigated the prevalence of hearing loss in Saudi Arabia have either targeted both congenital and acquired hearing loss and collected data from older children (El Sayed and Zakzouk, 1996; Alqudah et al., 2021) or targeted infants with a high risk of hearing loss (Maisoun and Zakzouk, 2003). The data from these investigations overestimated the prevalence of congenital hearing loss. These efforts were individualized and provided data that helped justify the need to initiate and mandate the UNHS program in Saudi Arabia.
In Saudi Arabia, the Ministry of Health (MoH) is primarily responsible for newborn screening programs across all birth hospitals around the country. Although the UNHS program in Saudi Arabia has been operational since 2016, few studies have been conducted to evaluate the program(Alqudah et al., 2021). A study by Alanazi (2020) concluded that the program's referral/fail rate was 1.33%. However, the data used in the study were collected from only two major hospitals in Riyadh, the capital city of Saudi Arabia. Another study reviewed the status of the UNHS program as of 2021 and reported that approximately 1 million newborns had been screened in Saudi Arabia since 2016, with a coverage rate of 96% and a referral rate of 0.7% (Alaql, 2021). Therefore, it is of interest to continue to assess the performance of the current UNHS program in detail, including the performance of all provinces within Saudi Arabia.
This study aimed to assess the current status of the UNHS program in Saudi Arabia by examining the following performance measures: coverage and pass/refer rates.
2. Materials and methods
This was a retrospective descriptive cross-sectional study. Newborns born in hospitals across all provinces of Saudi Arabia between January 1, 2021 and December 31, 2021 were included in the study sample. A total of 147 birthing hospitals were included in the study. Only hospitals under the MoH administration were included in the current study, as they were mandated to implement the UNHS program at the time of data collection. This study was ethically approved by the Institutional Review Board of Princess Nourah Bint Abdulrahman University and the MoH (Number: 20-0018 and 20-46E, respectively).
UNHS data were retrieved from the national registry by a third-party entity after obtaining permission. The data included the following: the total number of live births across all provinces, total number of newborns screened in each province, total number of newborns who passed or failed the first screening stage, and total number of newborns who passed or failed the second and/or third stages for only those who completed all required stages of screening. Therefore, newborns who did not return for the second and third stages of the screening were not included in the data. Descriptive statistics were used to analyze the data.
The UNHS program utilized a three-stage screening protocol as follows. Automated auditory brainstem response (AABR) was the screening test used, and it involved using a click stimulus at 35 dB nHL. This protocol has been confirmed as valid and reliable for screening the hearing of newborns (Kanji and Khoza-Shangase, 2018. Each newborn was screened 24 h after birth or before discharge. Each ear was individually screened. If any ear failed (“refer” result) the first AABR screening, a second screening was conducted before discharge. If any ear still failed (“refer” result), a third screening was arranged within 2–3 weeks of birth. If any ear failed the third screening, a referral for a full diagnostic audiological evaluation was completed at no later than 3 months of age. All screenings were performed by trained nurses in quiet rooms.
The AABR screening was conducted using the ALGO Newborn Hearing Screener (Natus Medical Inc., USA). A “pass” result was obtained if an individual trace matched with the template, with a statistically significant level of at least 99% (Meier et al., 2004).
3. Results
Of the 214,971 delivered babies (births reported by the UNHS Program National Registry*), 199,034 newborns were screened (92.6%). The initial pass rate was 96.4% (191,194 newborns) and the referral rate for one or both ears was 3.6% (7840 newborns). Of the 7840 newborns who failed at the first-stage screening, 43.5% (3412 newborns) passed the second screening, while 56.5% (4428 newborns) failed and were set for the third screening. Of the 4428 newborns who failed the second screening, 6.2% (274 newborns) passed the third screening, while 93.8% (4154 newborns; 2266 in one ear and 1888 in both ears) failed the third screening and were referred for diagnostic audiologic evaluation (Fig. 1).
Fig. 1.
Flowchart of pass and referral rates at each stage of the newborn hearing screening program.
* The number of births reported by the UNHS Program National Registry may differ slightly from that reported by the national birth notification system in the same year.
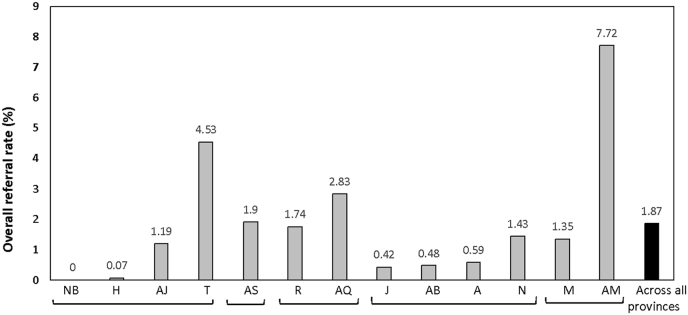
Table 1 shows the referral rates at each of the three screening stages for the 13 Saudi Arabian provinces. The referral rate ranged from 0.03 (Northern Borders) to 12.19 (Al-Madina) at the first screening, 33.33 (Northern Borders) to 87.5 (Hail) at the second screening and 0 (Northern Borders) to 98.38 (Al-Qassim) at the third stage. The referral rate increased from the first to the third screening for all provinces except for the Northern Borders and Hail. Fig. 2 shows the overall referral rate at the end of the screening, which ranged from 0 (Northern Borders) to 7.72 (Al-Madina). The overall referral rate across all provinces was 1.87%.
Table 1.
Number of newborns who were referred at each of the three-stage screenings in one or both ears for each of the 13 provinces of Saudi Arabia. The overall referral rates (%) for all screening stages are also listed.
| Province | Newborns screened | First stage screening |
Second stage screening |
Third stage screening |
Overall Referral rate (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Two ears | One ear | Referral rate (%) | Two ears | One ear | Referral rate | Two ears | One ear | Referral rate (%) | ||||
| Northern | Al-Jouf | 13247 | 210 | 114 | 2.33 | 87 | 85 | 53.08 | 78 | 80 | 91.86 | 1.19 |
| Northern Borders | 5479 | 3 | 0 | 0.03 | 1 | 0 | 33.33 | 0 | 0 | 0 | 0 | |
| Tabouk | 8304 | 410 | 270 | 8.18 | 178 | 234 | 60.58 | 149 | 228 | 91.5 | 4.53 | |
| Hail | 8488 | 4 | 4 | 0.08 | 4 | 3 | 87.5 | 4 | 2 | 85.71 | 0.07 | |
| Eastern | Ash-Sharqiyah | 22909 | 997 | 221 | 4.96 | 260 | 207 | 38.34 | 247 | 190 | 93.57 | 1.90 |
| Middle | Riyadh | 18324 | 324 | 353 | 2.50 | 122 | 223 | 50.96 | 111 | 208 | 92.46 | 1.74 |
| Al-Qassim | 15055 | 600 | 217 | 4.92 | 237 | 197 | 53.12 | 233 | 194 | 98.38 | 2.83 | |
| Southern | A-Baha | 3285 | 36 | 2 | 0.65 | 16 | 2 | 47.36 | 15 | 1 | 88.88 | 0.48 |
| Jazan | 17765 | 166 | 55 | 1.24 | 39 | 49 | 39.81 | 35 | 41 | 86.36 | 0.42 | |
| Aseer | 24176 | 418 | 69 | 2.01 | 125 | 52 | 36.34 | 94 | 50 | 81.35 | 0.59 | |
| Najran | 4865 | 39 | 50 | 0.83 | 26 | 48 | 83.14 | 23 | 47 | 94.59 | 1.43 | |
| Western | Makkah | 35959 | 379 | 316 | 1.93 | 216 | 293 | 73.9 | 201 | 286 | 95.67 | 1.35 |
| Al Medina | 21178 | 1451 | 1132 | 12.19 | 781 | 943 | 66.74 | 698 | 939 | 94.95 | 7.72 | |
Fig. 2.
Overall referral rate (%) at the end of screening for each of the 13 provinces (gray columns) and across all provinces (black column). AJ: Al-Jouf; NB: Northern Borders; T: Tabouk; H: Hail; AS: Ash-Sharqiyah; R: Riyadh; AQ: Al-Qassim; AB: A-Baha; J: Jazan; A: Aseer; N: Najran; M: Makkah; AM: Al-Medina.
When considering the regions within the geographical locations of Saudi Arabia, the highest overall referral rate was found in the western region (4.5%), followed by the regions in the middle (2.3%). The southern region had the lowest referral rate (0.7%). The Southern and eastern regions had referral rates of 1.5% and 1.9%, respectively (Fig. 3).
Fig. 3.
Overall referral rate (%) at the end of screening for the five geographical regions of Saudi Arabia.
4. Discussion
In Saudi Arabia, the UNHS program was implemented in 2016. This study is the first to provide an overview of the program at the national level across all provinces of Saudi Arabia. The data provided in this study focus on the overall UNHS program coverage rate and pass and referral/fail rates across the country's provinces. As any new national program, it is expected to undergo a learning curve until it reaches optimal performance and outcomes. The data obtained in this study provide evidence that despite the recent implementation of the UNHS program in Saudi Arabia (5 years at the time of data retrieval), the performance measures of the program (coverage and referral rates) are highly promising and comparable with internationally successful program performance measures. Notably, the data reported in this study, including the coverage and referral/fail rates, are only reflective of MoH hospitals in Saudi Arabia. Other hospitals (non-MoH hospitals and private hospitals) are not mandated by the government to implement the UNHS program. Efforts to include private hospitals and non-MoH hospitals in the UNHS program are currently underway.
4.1. Coverage rate
The UNHS program coverage rate across all provinces was found to be 92.6% (among MoH hospitals mandated to implement the program at this point) in this study. This coverage rate shows an improvement in screening coverage compared to the 89% rate reported by the MoH in 2018 (MoH, 2018). In 2021, Alaql (2021) reported a coverage rate of 96% since the start of the UNHS program in 2016. However, the coverage rate reported in this study (for 2021) is reflective of the increased number of hospitals that implement the UNHS program as more hospitals join the program every year. This study's coverage rate (92.6%) is comparable to that of well-established international newborn hearing screening (NHS) programs, and therefore superior to that of other local programs around the region. Data from the UNHS program in the United States (US), the 2019 summary of the CDC, and Early Hearing Detection and Intervention (EHDI) data reported a coverage rate of 98.4% (CDC, 2019). When the UNHS program was approximately 10 years old in the US, the coverage rate (newborns who were screened before hospital discharge) was reported to be only 70% in 2002 (White, 2010). In Egypt, a UNHS program coverage rate of 55% was reported in 2020, 56% in 2021, and 73% in the first two quarters of 2022 (Ghorab, 2022). In Oman, the UNHS coverage rate in 2008 was estimated to be approximately 72%, using a two-stage protocol (WHO, 2010), and progressed to 90% by 2020 (Kolethekkat et al., 2020). In Europe, a coverage rate of 80% was reported in 2010. This reported coverage rate is for 80% of the European countries that implemented a nationwide NHS program (WHO, 2010).
The international guidelines for the UNHS programs recommend a coverage rate of 95% (NIH, 1993; JCIH, 2007). This target coverage rate encourages improvement of the UNHS program in Saudi Arabia.
4.2. Referral rate
The UNHS program's overall referral/fail rate across all provinces was found to be 1.87% in this study. This referral rate is acceptable and comparable to the referral rates found in other national and international NHS programs. In the US, the 2019 summary of the CDC and EHDI data reported the referral rate of the UNHS program to be 1.6–1.7%. Compared to more local programs, Alanazi (2020) reported a referral rate of 1.33% from NHS programs conducted in two hospitals in Riyadh, Saudi Arabia. These two programs utilize a two-stage transient otoacoustic emission screening protocol, which is expected to result in higher referral rates than those associated with protocols utilizing AABR. The referral rate reported in this study is greater than that previously reported by Alaql (2021) (0.7%) for the same UNHS program across Saudi Arabia. Current international guidelines for NHS programs recommend a referral rate not exceeding 4% (NIH, 1993; JCIH, 2007). In 2022, the UNHS in Egypt reported a referral rate of 0.61% (Ghorab, 2022). In Oman, the UNHS program was reported to have a referral rate of 6.6% (Kolethekkat et al., 2020), which exceeds the recommended maximum international benchmark of 4%.
The referral rates reported in this study varied drastically among the provinces of Saudi Arabia. For example, the referral rate was found to be 0% in the Northern borders and 7.2% in Al-Medina. This variability cannot be explained because of many factors. This variation could reflect the actual regional variation in the prevalence of congenital hearing loss. Another possible explanation for this variation is the lack of information regarding screened infants who were lost to follow-up. The data presented in this study included newborns who were screened and completed the three stages of screening (as needed). Newborns who failed to return for the second or third screening were excluded. The loss to follow-up rate was higher in provinces such as the Northern Borders, resulting in a lower referral rate than the actual referral rate that could have been obtained if all screening follow-ups were completed.
4.3. Limitations and recommendations
To improve the current national UNHS program, this study recommends the following based on the current status of the program:
-
(1)
Provide a method to document and report those screened but lost to follow-up. In the current study, it was difficult to extract this information from the retrieved data. Such data are essential to provide feedback on the effectiveness of NHS programs. One major reason why the Saudi MoH decided to adopt a three-stage AABR screening protocol is the expected high rate of those lost to follow-up (Alaql, 2021). Alanazi (2020) reported a high lost-to-system rate (combining lost to follow-up and lost to documentation) of 34.9% in NHS programs conducted in two hospitals in Riyadh, Saudi Arabia. Once lost to follow-up information is identified within the program's national registry, a method for tracking and monitoring this population becomes possible. The reported referral rate is expected to differ (increase) if the screening registry can track cases lost to follow-up.
-
(2)
Incorporation of the diagnostic stage into the UNHS national registry. One of the main measures of the effectiveness of a screening program is an assessment of the extent to which it minimizes the negative consequences of the disease of interest in the community. Data regarding the prevalence of hearing loss could not be presented in this study because data on identified hearing loss post-screening (diagnostic information) are not currently incorporated within the program's national registry. This missing connection is a major limitation of the current program. The audiologic diagnostic results should be incorporated with the national screening registry for early identification of hearing loss, which is the main goal of the UNHS program. The current status of the UNHS program along with its current national registry system mandates the entry of all screening stage results; however, it does not incorporate audiologic evaluation results. The current program with the current registry system can only aim to identify infants at risk of hearing loss (Alaql, 2021). However, it cannot validate the program's main goal of early identification and intervention for newborn congenital hearing loss, which is the gold standard for well-established global UNHS programs.
-
(3)
The current data do not include newborns in private and non-MoH sector hospitals. Efforts to include all non-governmental hospitals are currently underway, and the national NHS program will eventually cover all newborns across the country, regardless of the hospital sector (governmental or private). This will allow a more accurate estimate of the coverage rate of the universal national program.
In the meantime, public awareness is recommended to encourage parents of newborns born in non-governmental (not under the MoH) hospitals, where the UNHS program is not mandated, to seek completion of hearing screening as soon as possible after birth if not completed by the birthing hospital. Moreover, more efforts are needed to enhance the knowledge, attitude, and practice of family physicians in Saudi Arabia in counseling parents and caregivers regarding the need for follow-up visits during hearing screening and diagnosis (Alqudah et al., 2021; Malas et al., 2022).
5. Conclusion
The current status of the UNHS program in Saudi Arabia is promising. The performance measures of the program obtained at this stage provide a foundation for future progress and improvements. As of 2021, the current study reported a UNHS program coverage rate of 92.6%, with a referral/fail rate of 1.87%. The referral rate may have been underestimated because of the lack of lost to follow-up data in the screening program. Such performance measures for the ongoing UNHS program allow for instant identification and improvement of challenging issues in the program.
Acknowledgements
The authors would like to thank the Ministry of Health in Saudi Arabia for providing data from the newborn hearing screening national registry.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
Contributor Information
Noura Alothman, Email: nialothman@pnu.edu.sa.
Reem Elbeltagy, Email: reem.elbeltagy@yahoo.com.
Reem Mulla, Email: rmmulla@pnu.edu.sa.
References
- Al-Abduljawad K., Zakzouk S. The prevalence of sensorineural hearing loss among Saudi children.”. Int. Congr. 2003;240:199–204. doi: 10.1016/S0531-5131(03)00913-0. [DOI] [Google Scholar]
- Alanazi A.A. Referral and lost to system rates of two newborn hearing screening programs in Saudi Arabia. International Journal of Neonatal Screening. 2020;6(3):50. doi: 10.3390/ijns6030050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaql F.A.M. Realization of successful universal newborn hearing screening program in Saudi Arabia. Journal of Pediatric Neonatal Medicine. 2021;3(4):147. [Google Scholar]
- Alqudah O., Alqudah S., Al-Bashaireh A.M., Alharbi N., Alqudah A.M. Knowledge, attitude and management of hearing screening in children among family physicians in the kingdom of Saudi Arabia. PLoS One. 2021;16(8) doi: 10.1371/journal.pone.0256647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bafaqeeh S.A., Zakzouk S.M., S M., Almuhaimeid H., Essa A. Relevant demographic factors and hearing impairment in Saudi children: epidemiological study. J. Laryngol. Otol. 1994;108(4):294–298. doi: 10.1017/s0022215100126581. [DOI] [PubMed] [Google Scholar]
- Banda F.M., Powis K.M., Mokoka A.B., Mmapetla M., Westmoreland K.D., David T., Steenhoff A.P. Hearing impairment among children referred to a public audiology clinic in Gaborone, Botswana. Global Pediatric Health. 2018;5 doi: 10.1177/2333794X18770079. 2333794X18770079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention 2019 summary of national CDC EHDI data. 2019. https://www.cdc.gov/ncbddd/hearingloss/2019-data/01-data-summary.html
- Daghistani K.J., Jamal T.S., Zakzouk S.M. The management of hearing impaired Saudi children: an epidemiological survey. Bahrain Med. Bull. 2002;24(1):7–12. [Google Scholar]
- El Sayed Y., Zakzouk S. Prevalence and etiology of childhood sensorineural hearing loss in Riyadh. Ann. Saudi Med. 1996;16(3):262–265. doi: 10.5144/0256-4947.1996.26221. [DOI] [PubMed] [Google Scholar]
- Foster M.E., Choo A.L., Smith S.A. Speech-language disorder severity, academic success, and socioemotional functioning among multilingual and English children in the United States: the National Survey of Children's Health. Front. Psychol. 2023;14 doi: 10.3389/fpsyg.2023.1096145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghorab E. 2022. Egyptian Experience for the Implementation of a National Neonatal Hearing Screening Program: Challenges and Points of Success. Paper Presented at the Biennial Meeting for the Saudi Society of Speech-Language Pathology and Audiology, Riyadh. October 1-2. [Google Scholar]
- Habib H.S., Abdelgaffar H. Neonatal hearing screening with transient evoked otoacoustic emissions in western Saudi Arabia. Int. J. Pediatr. Otorhinolaryngol. 2005;69(6):839–842. doi: 10.1016/j.ijporl.2005.01.018. [DOI] [PubMed] [Google Scholar]
- Joint Committee on Infant Hearing Year 2000 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2000;106(4):798–817. doi: 10.1542/peds.106.4.798. [DOI] [PubMed] [Google Scholar]
- Joint Committee on Infant Hearing Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898–921. doi: 10.1542/peds.2007-2333. [DOI] [PubMed] [Google Scholar]
- Kanji A., Khoza-Shangase K. Objective hearing screening measures: an exploration of a suitable combination for risk-based newborn hearing screening. J. Am. Acad. Audiol. 2018;29(6):495–502. doi: 10.3766/jaaa.16155. [DOI] [PubMed] [Google Scholar]
- Kennedy C., McCann D., Campbell M.J., Kimm L., Thornton R. Universal newborn screening for permanent childhood hearing impairment: an 8-year follow-up of a controlled trial. Lancet. 2005;366(9486):660–662. doi: 10.1016/S0140-6736(05)67138-3. [DOI] [PubMed] [Google Scholar]
- Kolethekkat A.A., Al Abri R., Hlaiwah O., Al Harasi Z., Al Omrani A., Sulaiman A.A., Mathew J. Limitations and drawbacks of the hospital-based universal neonatal hearing screening program: first report from the Arabian Peninsula and insights. Int. J. Pediatr. Otorhinolaryngol. 2020;132 doi: 10.1016/j.ijporl.2020.109926. [DOI] [PubMed] [Google Scholar]
- Maisoun A.M., Zakzouk S. Hearing screening of neonates at risks. Saudi Med. J. 2003;24(1):55–57. [PubMed] [Google Scholar]
- Malas M., Aboalfaraj A., Alamoudi H., Kurdi A., Alahmadi T., Zawawi F. Pediatricians' knowledge and attitude toward hearing loss and newborn hearing screening programs. Int. J. Pediatr. Otorhinolaryngol. 2022;161 doi: 10.1016/j.ijporl.2022.111265. [DOI] [PubMed] [Google Scholar]
- Mathers C., Smith A., Concha M. Global burden of hearing loss in the year 2000. Global Burden of Disease. 2000;18(4):1–30. [Google Scholar]
- Mehl A.L., Thomson V. Newborn hearing screening: the great omission. Pediatrics. 1998;101(1):E4. doi: 10.1542/peds.101.1.e4. [DOI] [PubMed] [Google Scholar]
- Meier S., Narabayashi O., Probst R., Schmuziger N. Comparison of currently available devices designed for newborn hearing screening using automated auditory brainstem and/or otoacoustic emission measurements. Int. J. Pediatr. Otorhinolaryngol. 2004;68(7):927–934. doi: 10.1016/j.ijporl.2004.02.008. [DOI] [PubMed] [Google Scholar]
- Ministry of Health MOH news: 90% of the newborns had cardiac diagnosis. 2018. https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/news-2018-03-12-003.aspx
- Mohr P.E., Feldman J.J., Dunbar J.L., McConkey-Robbins A., Niparko J.K., Rittenhouse R.K., Skinner M.W. The societal costs of severe to profound hearing loss in the United States. Int. J. Technol. Assess. Health Care. 2000;16(4):1120–1135. doi: 10.1017/s0266462300103162. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health Early identification of hearing impairment in infants and young children: summary of the NIH consensus development conference, March 1-3, 1993. Online J. Curr. Clin. Trials. 1993;2(1) [Google Scholar]
- Shukla A., Harper M., Pedersen E., Goman A., Suen J.J., Price C., Applebaum J., Hoyer M., Lin F.R., Reed N.S. Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngology-Head Neck Surg. (Tokyo) 2020;162(5):622–633. doi: 10.1177/0194599820910377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saudi Vision 2030 National transformation program: strategic objectives. https://vision2030.gov.sa/en
- White K.R., Forsman I., Eichwald J., Munoz K. The evolution of early hearing detection and intervention programs in the United States. Semin. Perinatol. 2010;34(2):170–179. doi: 10.1053/j.semperi.2009.12.009. [DOI] [PubMed] [Google Scholar]
- Wood S.A., Sutton G.J., Davis A.C. Performance and characteristics of the newborn hearing screening programme in england: the first seven years. Int. J. Audiol. 2015;54(6):353–358. doi: 10.3109/14992027.2014.989548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2010. Newborn and Infant Hearing Screening: Current Issues and Guiding Principles for Action.https://apps.who.int/iris/bitstream/handle/10665/339288/9789241599496-eng.pdf [Google Scholar]
- World Health Organization . 2021. Hearing Screening: Considerations for Implementation.https://apps.who.int/iris/bitstream/handle/10665/344797/9789240032767-eng.pdf [Google Scholar]
- World Health Organization Deafness and hearing loss. 2023. https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
- Wren Y., Pagnamenta E., Peters T.J., Emond A., Northstone K., Miller L.L., Roulstone S. Educational outcomes associated with persistent speech disorder. Int. J. Lang. Commun. Disord. 2021;56(2):299–312. doi: 10.1111/1460-6984.12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshinaga-Itano C. Levels of evidence: universal newborn hearing screening (UNHS) and early hearing detection and intervention systems (EHDI) J. Commun. Disord. 2004;37(5):451–465. doi: 10.1016/j.jcomdis.2004.04.008. [DOI] [PubMed] [Google Scholar]