Abstract
Objective:
The objectives of this study were to (1) investigate whether electrodiagnostic (EDX) findings reflect the preoperative symptom severity and functional impairment in patients with carpal tunnel syndrome (CTS) and (2) evaluate the relationship between EDX findings and the clinical outcomes reported according to the self-administered patient questionnaires.
Methods:
Patients diagnosed with idiopathic CTS who underwent carpal tunnel release between May 2016 and July 2018 were included. Carpal tunnel syndrome was clinically diagnosed and confirmed based on the EDX findings. The association between EDX findings, such as motor latency, motor amplitude, sensory latency, sensory amplitude, and severity (mild, moderate, and severe), and the Boston symptom and function scores were analyzed. The change in the Boston symptom and function scores from the preoperative baseline values (visit 1) to those recorded 1 year postoperatively (visit 5) was assessed. The effect of disease severity based on the EDX findings on the change in Boston symptom and function scores by visit was also investigated.
Results:
The EDX severity, motor latency, motor amplitude, sensory latency, and sensory amplitude were not correlated with the Boston symptom and function scores preoperatively and postoperatively. Electrodiagnostic severity did not affect the improvement in the Boston symptom and function scores recorded at each visit.
Conclusion:
We found no association between the EDX severity and perioperative Boston questionnaire scores, and the degree of improvement in patient symptoms and function did not differ according to the CTS severity based on the EDX findings.
Level of Evidence:
Level IV, Prognostic study.
Keywords: Carpal tunnel syndrome, Electromyography, Self-report, Carpal tunnel release, Treatment outcome
Highlights
An electrodiagnostic study is commonly conducted to confirm the diagnosis of carpal tunnel syndrome. This study was conducted to investigate the relationship between the clinical severity of carpal tunnel syndrome and electrodiagnostic findings.
The results showed no significant correlation between electrodiagnostic study findings and preoperative Boston symptom and function scores. Moreover, The EDX severity did not affect the improvement in the Boston symptom and function scores.
The results indicate that It is difficult to predict the degree of improvement in patients’ symptoms and functions after carpal tunnel release through an electrodiagnostic study.
Introduction
Carpal tunnel syndrome (CTS), the most common compressive neuropathy of the upper extremity, is diagnosed based on various criteria, including symptoms and physical examination findings. In many cases, an electrodiagnostic (EDX) study is also conducted to confirm the diagnosis since EDX findings, provide objective information about the patient’s condition, and make an informed disease prognosis.1,2 Moreover, the sensitivity of EDX studies is reportedly 80%-90%, while the rate of false-negative CTS findings is reportedly 10%-35%.3 However, there is controversy regarding the relationship between the clinical severity of CTS and EDX findings. Some studies have reported that preoperative symptom severity correlates with the EDX findings4,5 and that the postoperative clinical outcome is associated with the EDX results.6,7 Other studies reported no correlation between symptom severity or clinical outcomes and EDX findings.8,9 The American Academy of Orthopedic Surgeons recently graded the EDX findings as moderate-level evidence in the Clinical Practice Guideline for the Diagnosis and Treatment of CTS.10
In this study, we investigated whether EDX findings reflect the preoperative symptom severity and functional impairment in patients with CTS and whether EDX findings are related to the clinical outcomes reported according to the self-administered patient questionnaires. We also investigated whether the degree of improvement in the patient’s symptoms varied according to CTS severity.
Materials and methods
Patient characteristics
The institutional review board of Gangneung Asan Hospital, University of Ulsan College of Medicine (Approval No: GNAH 2019-01-026, Date: February 18, 2019) approved the study. Because this study was a retrospective study and was based on data that did not identify patients' personal information, informed consent was waived. We included patients who were diagnosed with idiopathic CTS and had undergone carpal tunnel release (CTR) between May 2016 and July 2018. Carpal tunnel release was clinically diagnosed and confirmed based on an electrophysiological examination.
We excluded patients with any comorbidity that may affect the outcome, such as cervical radiculopathy or cubital tunnel syndrome, thoracic outlet syndrome, polyneuropathy, diabetes mellitus, or thyroid disease, as well as those who had CTS, with a worker’s compensation claim or a previous history of CTR in the same hand. Patients who refused to answer the questionnaire were also excluded. A total of 163 hands of 113 patients were included in this study. There were 105 women and 8 men, with a total of 47 right hands, 44 left hands, and 36 pairs of hands. The patients’ mean age was 57.7 (range, 38-82) years. The CTR procedure was performed by a surgeon (J.Y.B.) using a previously described limited open technique under a brachial plexus block or general anesthesia.11
Perioperative assessments
The EDX studies were performed by an experienced physiatrist (J.H.K.) using a Nicolet Synergy EDX device (Natus Medical Inc., San Carlos, Calif, USA). All EDX procedures conformed to the American Association of Neuromuscular and Electrodiagnostic Medicine (AANEM) recommendations for the diagnosis of CTS. The evaluation process was performed under a standard room temperature of 25°C and hand temperature of more than 32°C. The motor nerve conduction study of the median nerve was recorded with surface electrodes from the abductor pollicis brevis muscle. Median motor nerve proximal and distal latencies, median motor nerve conduction velocity, and compound muscle action potential (CMAP) amplitudes at the wrist and elbow were measured. The median sensory nerve action potential (SNAP) was recorded with ring electrodes placed antidromically on the third digit at 7 and 14 cm proximal to the recording electrode. Needle electromyography was performed on a sample of muscles that are innervated by the C5–T1 nerve roots, brachial plexus, and peripheral nerves of the upper extremity. The EDX results were graded as mild, moderate, or severe according to the AANEM-modified criteria for the diagnosis of CTS.12
We asked the patients to complete the Boston Carpal Tunnel Questionnaire (BCTQ) for a total of 5 visits: preoperatively, 6 weeks, 3 months, 6 months, and 1 year postoperatively (visit 1 to visit 5). The BCTQ, which is used to evaluate symptom severity and dysfunction in patients with CTS,13 comprises a symptom severity scale and a functional scale. The symptom severity scale consists of 11 questions covering pain, nocturnal symptoms, numbness, tingling, and weakness. The 8 questions on the functional scale evaluate difficulty in performing daily tasks. Each question is scored on a 5-point scale, with scores ranging from 1 to 5 points. The results are expressed as mean values for each scale.
We analyzed the association between EDX findings, such as motor and sensory latency, motor and sensory amplitude,severity (mild, moderate, and severe), and the Boston symptom and function scores. We also investigated the changes in the Boston symptom and function scores according to the visits, i.e., from the baseline preoperatively (visit 1) to 1 year postoperatively (visit 5). We assessed the effect of EDX severity on the changes in Boston symptom and function scores by visit. We also checked the effect of bilateral CTR on the Boston scores.
Statistical analysis
Descriptive data are expressed as mean ± SD or median and interquartile range, as appropriate. A correlation analysis was performed to identify the strength of the relationships between the variables. The Pearson correlation coefficient was used to report the distribution of the variables.
To investigate the changes in pain and function among the patients after CTR, we used the linear mixed model for analyzing the doubly repeated measures data with 2 repeated factors (i.e., visit and side if the operation was performed bilaterally) using the PROC MIXED procedure. A doubly repeated measures regression analysis model was used to evaluate the effect of EDX severity and bilateral operation on the changes in pain and function.
All calculations were performed using Statistical Analysis System (SAS) version 9.4; (SAS Institute, Cary, NC, USA). Significance was defined as P < 0.05.
Results
The preoperative EDX study revealed that 16, 74, and 73 hands had mild, moderate, and severe findings, respectively. The CMAP and SNAP were not measurable in 22 and 38 patients, respectively. Accordingly, the motor latency and amplitude of 141 patients and the sensory latency and amplitude of 125 patients were examined using the Pearson analysis.
In the Pearson analysis, the EDX severity, motor latency, motor amplitude, sensory latency, and sensory amplitude did not have a significant correlation with the Boston symptom and function scores preoperatively to 1 year postoperatively (Table 1).
Table 1.
Pearson correlation coefficient for the electrodiagnostic severity and Boston score
| Score | Electrodiagnostic grade | P |
Motor latency |
P | Motor amplitude | P | Sensory latency | P | Sensory amplitude | P |
|---|---|---|---|---|---|---|---|---|---|---|
| P1 | −0.001 | .98 | 0.026 | .76 | −0.140 | .10 | −0.001 | .99 | −0.126 | .15 |
| P2 | 0.054 | .61 | 0.047 | .68 | −0.053 | .64 | −0.052 | .66 | −0.019 | .87 |
| P3 | −0.022 | .85 | 0.008 | .95 | 0.030 | .81 | −0.087 | .49 | −0.110 | .39 |
| P4 | 0.006 | .96 | −0.021 | .87 | 0.145 | .26 | 0.032 | .81 | 0.121 | .36 |
| P5 | −0.019 | .80 | 0.056 | .50 | 0.068 | .42 | 0.036 | .68 | −0.011 | .89 |
| F1 | 0.064 | .42 | 0.091 | .28 | −0.151 | .07 | 0.077 | .39 | −0.096 | .28 |
| F2 | 0.145 | .17 | 0.064 | .57 | −0.141 | .21 | −0.143 | .23 | −0.018 | .88 |
| F3 | 0.006 | .96 | −0.021 | .87 | 0.145 | .26 | 0.032 | .81 | 0.121 | .36 |
| F4 | −0.066 | .59 | −0.053 | .68 | 0.141 | .28 | −0.007 | .96 | 0.097 | .46 |
| F5 | 0.003 | .97 | 0.091 | .27 | 0.056 | .51 | 0.028 | .75 | −0.030 | .74 |
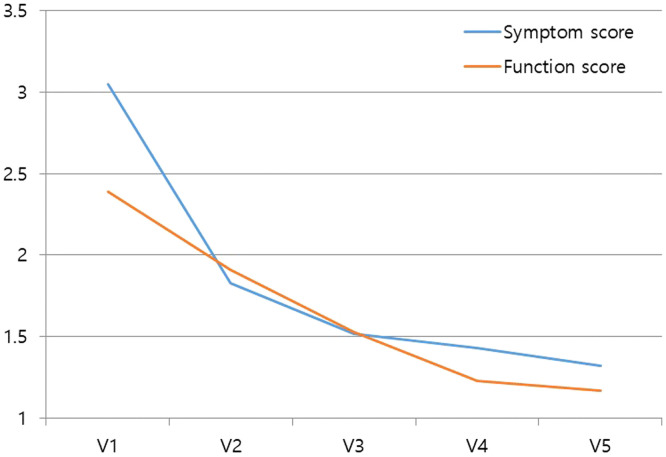
The postoperative improvement in the BCTQ scores was observed in all patients (P < .0001; Figure 1, Table 2). This relationship was similar after adjusting for the EDX findings. The EDX severity did not affect the improvement in the Boston symptom scores (P = .726) and function scores (P = .264) measured at each visit (Table 3). Bilaterality also did not affect the change in the Boston symptom scores (P = .33) and function scores (P = .799; Table 4).
Figure 1.
Changes in the Boston symptom and function scores after carpal tunnel release. V1, preoperative visit; V2, 6 weeks postoperatively; V3, 3 months postoperatively; V4, 6 months postoperatively; V5, 1 year postoperatively.
Table 2.
Changes in the Boston symptom and function scores after carpal tunnel release
| Outcome | P (visit) | Visit | Mean | 95% CI |
|---|---|---|---|---|
| Boston symptom score | <.0001 | 1 | 3.05 | (2.91-3.2) |
| 2 | 1.83 | (1.68-1.97) | ||
| 3 | 1.52 | (1.4-1.63) | ||
| 4 | 1.43 | (1.28-1.58) | ||
| 5 | 1.32 | (1.18-1.46) | ||
| Boston function score | <.0001 | 1 | 2.39 | (2.24-2.54) |
| 2 | 1.91 | (1.74-2.07) | ||
| 3 | 1.53 | (1.39-1.67) | ||
| 4 | 1.23 | (1.08-1.38) | ||
| 5 | 1.17 | (1.02-1.32) |
Table 3.
Effect of the visits adjusted with the electrodiagnostic findings on the Boston symptom and function scores
| Outcome | P (visit) | P (electrodiagnostic study) | Visit | Mean | 95% CI |
|---|---|---|---|---|---|
| Boston symptom score | <.0001 | .7256 | 1 | 3.06 | (2.91-3.21) |
| 2 | 1.83 | (1.67-1.99) | |||
| 3 | 1.52 | (1.39-1.65) | |||
| 4 | 1.43 | (1.27-1.6) | |||
| 5 | 1.33 | (1.18-1.48) | |||
| Boston function score | <.0001 | .2643 | 1 | 2.37 | (2.21-2.52) |
| 2 | 1.89 | (1.72-2.06) | |||
| 3 | 1.5 | (1.35-1.65) | |||
| 4 | 1.2 | (1.04-1.36) | |||
| 5 | 1.15 | (0.99-1.31) |
Table 4.
Effect of the visits adjusted with unilateral or bilateral surgery on the Boston symptom and function scores
| Outcome | P (visit) | P (bilaterality) | Visit | Mean | 95% CI |
|---|---|---|---|---|---|
| Boston symptom score | <.0001 | .33 | 1 | 3.07 | (2.93-3.22) |
| 2 | 1.84 | (1.69-1.99) | |||
| 3 | 1.53 | (1.41-1.65) | |||
| 4 | 1.45 | (1.29-1.6) | |||
| 5 | 1.34 | (1.19-1.49) | |||
| Boston function score | <.0001 | .7991 | 1 | 2.38 | (2.23-2.54) |
| 2 | 1.9 | (1.73-2.07) | |||
| 3 | 1.52 | (1.38-1.67) | |||
| 4 | 1.22 | (1.06-1.38) | |||
| 5 | 1.17 | (1.01-1.32) |
Discussion
This study showed no correlation between the EDX findings and BCTQ scores. Electrodiagnostic severity, motor and sensory latency, and motor and sensory amplitude did not correlate with the symptom score pre- or postoperatively. There was no difference in the degree of symptom or functional improvement according to the EDX severity. We assumed that EDX severity may be correlated with symptom severity or functional impairment of patients; however, the effect of surgery (i.e., change in the Boston symptom and function scores according to the visits) did not differ according to the EDX severity.
The demyelination of compressed nerves is the primary pathology noted in compressive neuropathies, but axonal damage may be observed as the disease progresses.14 Kanatani et al15 reported that in several patients, axonal damage was recovered after CTR; however, in some cases, the damage was irreversible, as noted during 2 years of follow-up. Pauda et al16 showed that EDX abnormalities persisted in 40% of the cases in the moderate CTS group, despite complete symptom improvement, and that there was no significant normalization of EDX findings, despite significant symptom and functional improvement in the severe CTS group. Modelli et al9 also demonstrated a lack of correlation between the clinical outcomes and EDX severity in patients with severe CTS.
This study primarily included patients with moderate- or severe-grade disease (44.7% of the patients had severe-grade disease); therefore, it may be more difficult to observe the association between the scores and EDX findings. A patient-reported questionnaire is a good tool for assessing a patient’s clinical condition.13 However, the pain in the musculoskeletal system is related to both the patient’s disease and emotional state.17 The effects of anxiety and depression on pain and disability experienced by the patient undergoing hand surgery have been reported.18 These affective mood states of the patients before and after CTR can affect the symptom severity. Preoperative BCTQ scores were higher in patients with preoperative depression; however, postoperatively, the severity of depression and BCTQ scores decreased simultaneously.19 In patients with preoperative depression, the clinical outcome was poor after CTR.20,21 Even in patients with postoperative depression, the clinical outcome was poor after CTR.22 This relationship between pain and psychological distress may account for the poor association between symptom severity and EDX findings.
In this study, not only the patients’ symptom severities but also functional impairments were not related to the EDX severity. The motor function associated with CTS is affected by the abductor pollicis brevis; however, after surgery, thenar atrophy persists and EDX findings improve partially.9 Mondelli et al9 reported that the BCTQ function scale score improved postoperatively owing to the decrease in pain and sensory improvement. We agree with the above opinion and believe that the degree of sensory improvement leads to a significant improvement in function.
The strengths of the study are the performance of a correlation analysis between EDX severity and BCTQ scores and the confirmation of the effect of EDX severity on the improvement in the BCTQ scores during the follow-up period after CTR. Kronlage and Menendez reported that the degree of improvement in the BCTQ score after CTR differed between the moderate and severe CTS groups7; however, there was no effect of EDX severity on the degree of improvement in the BCTQ score in this study.
There are some limitations to this study. First, this was a retrospective study and included a small number of patients. Second, the study population included patients who underwent bilateral CTR. Bilateral CTS develops in 50%-70% of the patients, and the clinical outcomes do not differ between unilateral and bilateral CTR.23 We also confirmed that bilateral surgery does not significantly affect the clinical course.
Graham reported that when CTS was diagnosed using the CTS-6 criteria, it was unlikely that CTS would be further diagnosed based on the EDX findings.1 Despite the limited role of the EDX study as a diagnostic tool for CTS, approximately 60% of the cases are diagnosed based on EDX findings.2 Various attempts have been made to complement the diagnosis of CTS using other modalities, such as ultrasound; however, these modalities also have a limited role. Electrodiagnostic findings can aid in differentiating between mononeuropathy and polyneuropathy, radiculopathy, and even chronicity,24 and presently, an EDX study is an important tool for objectively detecting CTS. However, an EDX study cannot accurately assess the preoperative symptom severity of the patients or predict their prognosis. In conclusion, we found no association between the EDX findings and preoperative or postoperative Boston questionnaire scores. Moreover, the degree of improvement in patients’ symptoms and functions did not differ according to the CTS severity based on EDX findings.
Funding Statement
The authors declared that this study has received no financial support.
Footnotes
Ethics committee approval: This study was approved by Ethics Committee of Gangneung Asan Hospital, University of Ulsan College of Medicine (Approval No: GNAH 2019-01-026, Date: February 18, 2019).
Informed consent: Because this study was a retrospective study and was based on data that did not identify patients' personal information, informed consent was waived.
Peer-review: Externally peer-reviewed.
Author contributions: Concept – J.H.K.; Design – J.Y.B.; Supervision – J.Y.B.; Resources – J.Y.B.; Materials – J.Y.B.; Data Collection and/or Processing – H.S.P.; Analysis and/or Interpretation – J.H.K., K.L.; Literature Search – H.S.P.; Writing – J.H.K.; Critical Review – J.Y.B., K.L.
Declaration of interests: The authors have no conflict of interest to declare.
References
- 1. Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2008;90(12):2587 2593. ( 10.2106/JBJS.G.01362) [DOI] [PubMed] [Google Scholar]
- 2. Sears ED, Swiatek PR, Hou H, Chung KC. Utilization of preoperative electrodiagnostic studies for carpal tunnel syndrome: an analysis of national practice patterns. J Hand Surg Am. 2016;41(6):665 672.e1. ( 10.1016/j.jhsa.2016.03.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Padua L, LoMonaco M, Gregori B, Valente EM, Padua R, Tonali P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol Scand. 1997;96(4):211 217. ( 10.1111/j.1600-0404.1997.tb00271.x) [DOI] [PubMed] [Google Scholar]
- 4. You H, Simmons Z, Freivalds A, Kothari MJ, Naidu SH. Relationships between clinical symptom severity scales and nerve conduction measures in carpal tunnel syndrome. Muscle Nerve. 1999;22(4):497 501. () [DOI] [PubMed] [Google Scholar]
- 5. Taewon Jeong DSA. Efficiency of the Boston questionnaire in carpal tunnel syndrome: comparing scores with provocation tests and electrophysiological studies. J Korean Soc Surg Hand. 2011;16. [Google Scholar]
- 6. Bland JD. Do nerve conduction studies predict the outcome of carpal tunnel decompression? Muscle Nerve. 2001;24(7):935 940. ( 10.1002/mus.1091) [DOI] [PubMed] [Google Scholar]
- 7. Kronlage SC, Menendez ME. The benefit of carpal tunnel release in patients with electrophysiologically moderate and severe disease. J Hand Surg Am. 2015;40(3):438 44.e1. ( 10.1016/j.jhsa.2014.12.012). [DOI] [PubMed] [Google Scholar]
- 8. Chan L, Turner JA, Comstock BA, et al. The relationship between electrodiagnostic findings and patient symptoms and function in carpal tunnel syndrome. Arch Phys Med Rehabil. 2007;88(1):19 24. ( 10.1016/j.apmr.2006.10.013) [DOI] [PubMed] [Google Scholar]
- 9. Mondelli M, Reale F, Padua R, Aprile I, Padua L. Clinical and neurophysiological outcome of surgery in extreme carpal tunnel syndrome. Clin Neurophysiol. 2001;112(7):1237 1242. ( 10.1016/s1388-2457(01)00555-7) [DOI] [PubMed] [Google Scholar]
- 10. Graham B, Peljovich AE, Afra R, et al. The American Academy of Orthopaedic Surgeons evidence-based clinical practice guideline on: management of carpal tunnel syndrome. J Bone Joint Surg Am. 2016;98(20):1750 1754. ( 10.2106/JBJS.16.00719) [DOI] [PubMed] [Google Scholar]
- 11. Cellocco P, Rossi C, Bizzarri F, Patrizio L, Costanzo G. Mini-open blind procedure versus limited open technique for carpal tunnel release: a 30-month follow-up study. J Hand Surg Am. 2005;30(3):493 499. ( 10.1016/j.jhsa.2005.02.007) [DOI] [PubMed] [Google Scholar]
- 12. Stevens JC. AAEM minimonograph #26: the electrodiagnosis of carpal tunnel syndrome. American Association of electrodiagnostic medicine. Muscle Nerve. 1997;20(12):1477 1486. () [DOI] [PubMed] [Google Scholar]
- 13. Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585 1592. ( 10.2106/00004623-199311000-00002) [DOI] [PubMed] [Google Scholar]
- 14. Tapadia M, Mozaffar T, Gupta R. Compressive neuropathies of the upper extremity: update on pathophysiology, classification, and electrodiagnostic findings. J Hand Surg Am. 2010;35(4):668 677. ( 10.1016/j.jhsa.2010.01.007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kanatani T, Fujioka H, Kurosaka M, Nagura I, Sumi M. Delayed electrophysiological recovery after carpal tunnel release for advanced carpal tunnel syndrome: a two-year follow-up study. J Clin Neurophysiol. 2013;30(1):95 97. ( 10.1097/WNP.0b013e31827ed839) [DOI] [PubMed] [Google Scholar]
- 16. Padua L, LoMonaco M, Aulisa L, et al. Surgical prognosis in carpal tunnel syndrome: usefulness of a preoperative neurophysiological assessment. Acta Neurol Scand. 1996;94(5):343 346. ( 10.1111/j.1600-0404.1996.tb07077.x) [DOI] [PubMed] [Google Scholar]
- 17. Vranceanu AM, Barsky A, Ring D. Psychosocial aspects of disabling musculoskeletal pain. J Bone Joint Surg Am. 2009;91(8):2014 2018. ( 10.2106/JBJS.H.01512) [DOI] [PubMed] [Google Scholar]
- 18. Vranceanu AM, Jupiter JB, Mudgal CS, Ring D. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg Am. 2010;35(6):956 960. ( 10.1016/j.jhsa.2010.02.001) [DOI] [PubMed] [Google Scholar]
- 19. Datema M, Tannemaat MR, Hoitsma E, et al. Outcome of carpal tunnel release and the relation with depression. J Hand Surg Am. 2018;43(1):16 23. ( 10.1016/j.jhsa.2017.08.020) [DOI] [PubMed] [Google Scholar]
- 20. Bae JY, Kim JK, Yoon JO, Kim JH, Ho BC. Preoperative predictors of patient satisfaction after carpal tunnel release. Orthop Traumatol Surg Res. 2018;104(6):907 909. ( 10.1016/j.otsr.2018.04.004) [DOI] [PubMed] [Google Scholar]
- 21. Shin YH, Yoon JO, Kim YK, Kim JK. Psychological status is associated with symptom severity in patients with carpal tunnel syndrome. J Hand Surg Am. 2018;43(5):484.e1 484.e8. ( 10.1016/j.jhsa.2017.10.031) [DOI] [PubMed] [Google Scholar]
- 22. Lozano Calderón SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg Am. 2008;33(3):303 307. ( 10.1016/j.jhsa.2007.11.025) [DOI] [PubMed] [Google Scholar]
- 23. Osei DA, Calfee RP, Stepan JG, Boyer MI, Goldfarb CA, Gelberman RH. Simultaneous bilateral or unilateral carpal tunnel release? A prospective cohort study of early outcomes and limitations. J Bone Joint Surg Am. 2014;96(11):889 896. ( 10.2106/JBJS.M.00822) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li JM, Tavee J. Electrodiagnosis of radiculopathy. Handb Clin Neurol. 2019;161:305 316. ( 10.1016/B978-0-444-64142-7.00056-4) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a