Abstract
Soft-tissue grafts are an option for anterior cruciate ligament reconstruction. One of the major drawbacks of soft-tissue grafts is the delay in the osteointegration and ligamentization of the implanted graft. Enveloping the ends of the graft with periosteum sleeves can hasten the osteointegration process and help in quicker rehabilitation of the patient. This article describes a simple and unique way to augment the soft-tissue graft with periosteum for anterior cruciate ligament reconstruction.
Technique Video
Patient’s right knee positioned in supine in 90 degree flexion using lateral support, being viewed from medial side and arthroscopically via Anterolateral portal.
Regardless of single- or double-bundle reconstruction, the quintessential goal of anterior cruciate ligament (ACL) reconstruction is to restore the native kinematics of the knee joint. It has been demonstrated through biomechanical studies that 65% to 80% of the ACL function is carried out by the direct fibers attached to the proximal-central part of the femoral foot print.1 Histologic studies show that these direct fibers attach in greater angles and have 4 distinct anatomical zones: ligament, uncalcified fibrocartilage, calcified fibrocartilage, and bone.2
While choosing the graft to reconstruct the ACL, one of the particular areas of concern is to restore the enthesis, ie, the interface between the bone and the ligament, through the tendon graft.3 In view of the significance of enthesis in load transfer and osteointegration, bone–patellar tendon–bone (BPTB) graft is preferred by some surgeons. The BPTB graft harvested from the middle third of the patellar tendon has an intact enthesis on either end, which accelerates the graft’s incorporation into the tunnels. However, owing to the complications of the BPTB graft, such as donor-site morbidity and fracture of patella, many surgeons prefer hamstring grafts despite their impaired integration with bone.4 Studies have shown that the major causes of failure of soft-tissue graft (hamstring) next to tunnel malposition (70%-80%) are biological causes, which include poor regeneration of the enthesis and failure of ligamentization process with hamstring graft compared with BPTB graft.5
Chen et al.6 studied 312 patients to evaluate the clinical outcome of arthroscopic ACL reconstruction with periosteum-enveloped hamstring graft with a follow-up range of 2 to 7 years. The technique used in this study comprised 2 free periosteal sleeves harvested separately and sutured on to the either end of the prepared hamstring graft. This study concluded that enveloping the hamstring graft with periosteum resulted in better osteointegration of the graft with minimal tunnel widening compared with other similar fixation methods.
The current article describes a technique to harvest and envelop periosteum onto a quadrupled semitendinosus tendon (STT) graft used for arthroscopic reconstruction of ACL. Our technique involves in harvesting one free flap of periosteum and other harvested in continuation with the insertion of STT.
Surgical Technique (With Video Illustration)
Patient Evaluation
The index patient presented with injury to the right knee. On clinical evaluation and radiologic investigation (magnetic resonance imaging), a complete ACL tear of right knee was noted.
Indications
All cases of primary complete ACL reconstruction using hamstring graft can be considered for this technique. Patients with ligamentous laxity (Beighton score >4/9) would be a relative contraindication. However, revision ACL reconstruction with tunnel widening is a contraindication for this technique.
Patient Positioning
At our center, arthroscopy of the knee is performed with the patient in the supine position with lateral side support. Although a tourniquet is routinely applied for all patients, it would be selectively inflated in those who have heavy bleeding that obscures the field of vision.
Graft and Periosteum Harvest
An oblique linear incision of 4 to 5 cm (Fig 1A) is made medial to the tibial tubercle along the direction of the STT. This incision is used for both the tendon graft and periosteal sleeve harvesting. Subcutaneous dissection is carried out until the sartorius fascia is exposed. The pes anserine tendons are palpated and the borders of gracilis tendon (GT) and STT are delineated (Fig 1B). The sartorius fascia is incised and the STT is isolated (Fig 2A). The STT can be easily identified by its distal location and the direction of fibers, which point below the popliteal crease toward the ischial tuberosity (Fig 2B). Once the STT is isolated and secured, all soft-tissue adhesions and vincula are released. Conventionally, STTs have 3 to 5 vincula that should be released, and one should make sure that they are free completely by (1) palpating the musculotendinous junction with the finger (Fig 2B); (2) pulling the free end of STT across proximal tibia, where it can reach until the head of the fibula (Fig 3A); and (3) passing the tendon harvester freely along the STT for at least 15 cm (Fig 3A). Approximately 2.5 cm of periosteum sleeve starting from the STT insertion on to the bone is marked (Fig 2 C and D) and incised (Fig 4A) and isolated (Fig 4C). The STT is then harvested in standard fashion in continuity with periosteum (Figs 3A and 5A).
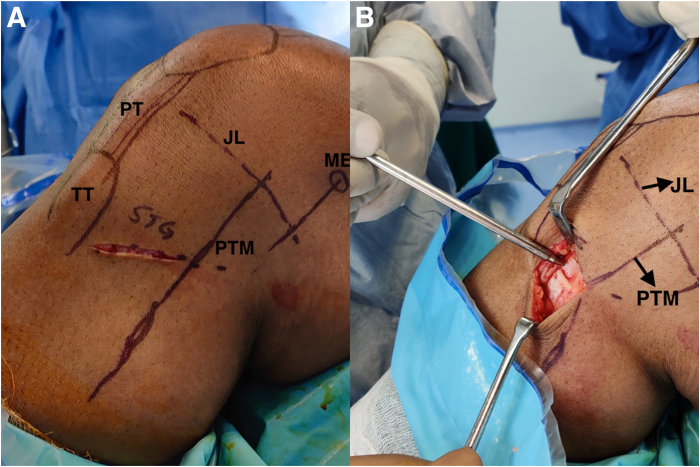
Fig 1.
Clinical photographs of patient’s right knee, viewed from the medial side, depicting (A) incision to harvest the hamstring graft along the orientation of pes anserine tendon and (B) following dissection through the subcutaneous tissue exposing the pes anserine insertion. (JL, joint line; ME, medial epicondyle; PT, patellar tendon; PTM, posterior tibial margin; STG, semitendinosus gracilis; TT, tibial tubercle.)
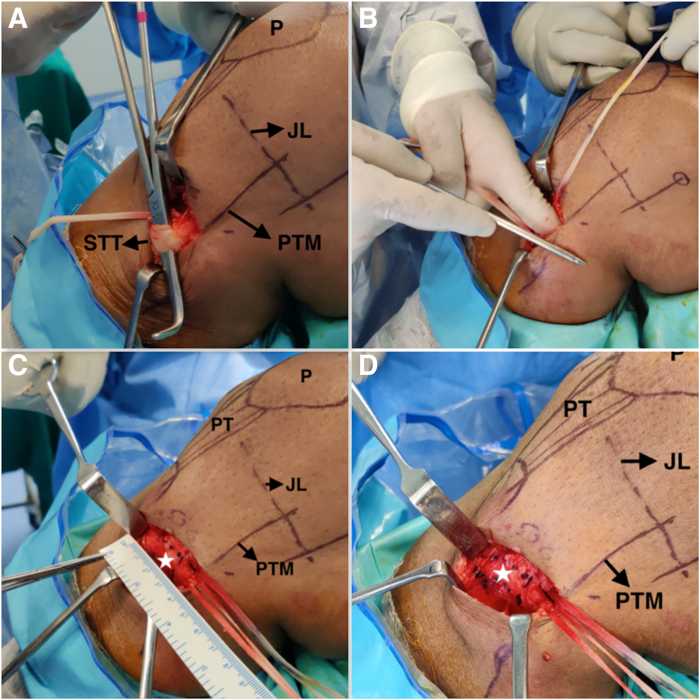
Fig 2.
Clinical photographs of patient’s right knee, viewed from the medial side, depicting (A) STT isolated by passing a Lahey’s right angled forceps underneath; (B) illustrating the direction of orientation of STT, which points below the popliteal crease towards the ischial tuberosity; (C-D) approximately 2.5 cm of periosteum sleeve attached to the STT is marked (white asterisk) Note that the periosteum sleeve is continuous with the insertion of the STT. (JL, joint line; P, patellar; PT, patellar tendon; PTM, posterior tibial margin; STT, semitendinosus tendon.)
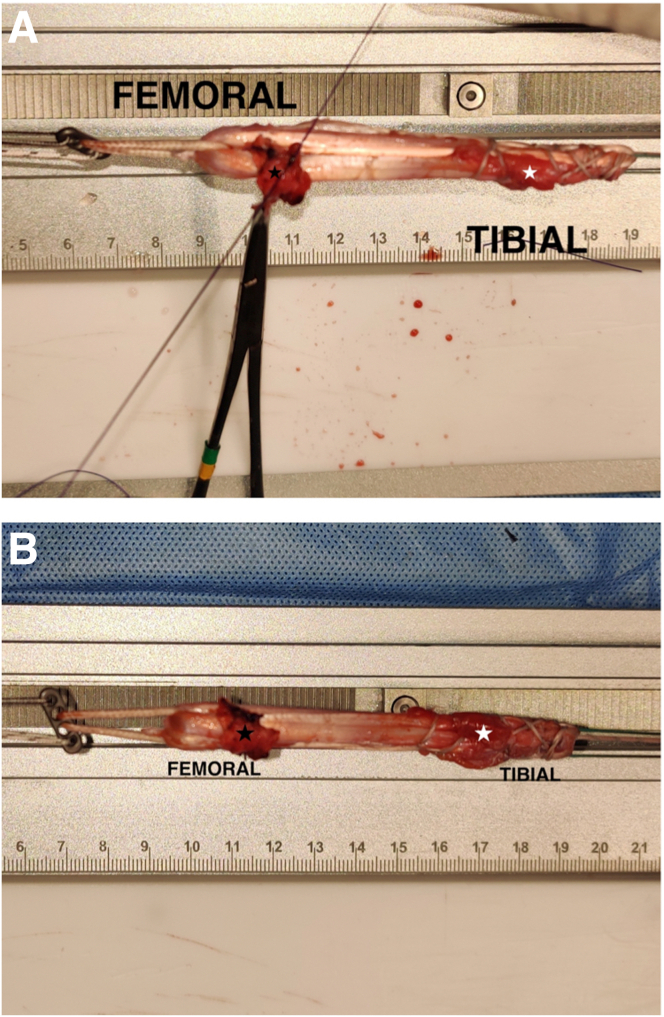
Fig 3.
Clinical photographs of patient’s right knee, viewed from the medial side, depicting (A) STT with attached periosteum sleeve released of all soft-tissue attachments note: once all the soft-tissue attachments are released, the tip of the released STT can be pulled across proximal tibia until the head of the fibula. (B) Bare area on the bone (white arrow) once the STT with the attached periosteal sleeve is harvested. (JL, joint line; ME, medial epicondyle; P, patellar; PT, patellar tendon; PTM, posterior tibial margin; STT, semitendinosus tendon.)
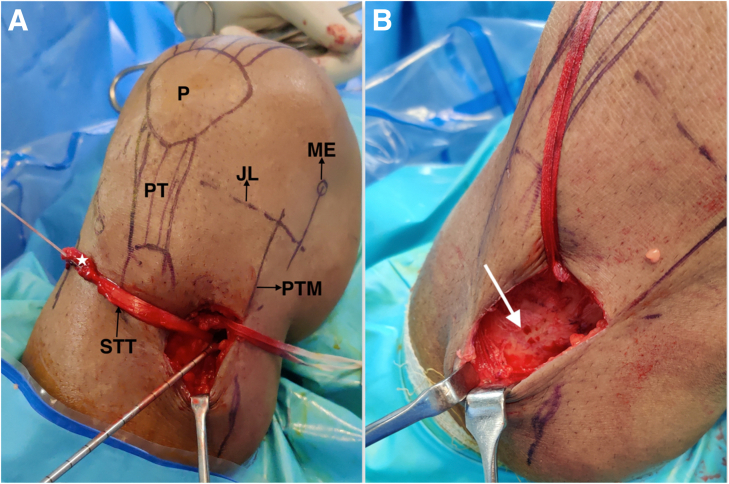
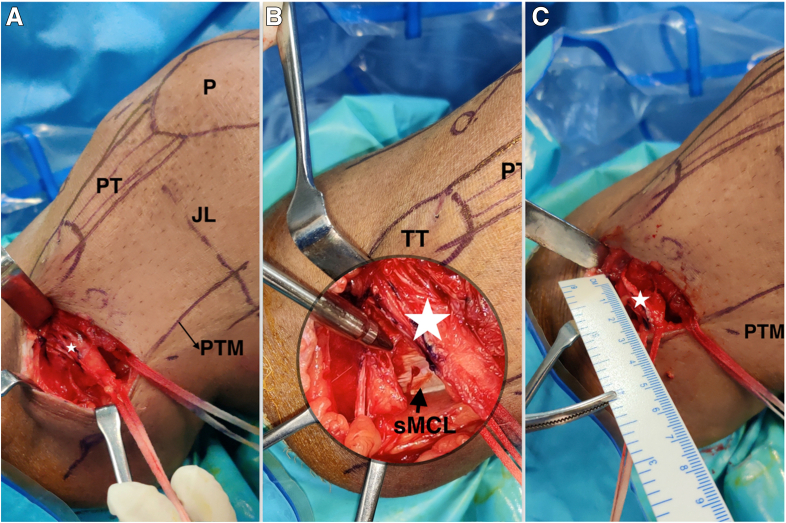
Fig 4.
Clinical photographs of patient’s right knee, viewed from the medial side, depicting (A) periosteum sleeve (white asterisk) attached to the STT insertion is incised. (B) Note the proximity of the STT insertion to the sMCL insertion. (C) STT with attached periosteum of approximately 2.5 cm is released from the bone. White asterisk: Periosteal sleeve attached to the semitendinosus tendon. (JL, joint line; P, patellar; PT, patellar tendon; PTM, posterior tibial margin; sMCL, superficial medial collateral ligament; STT, semitendinosus tendon; TT, tibial tubercle.)
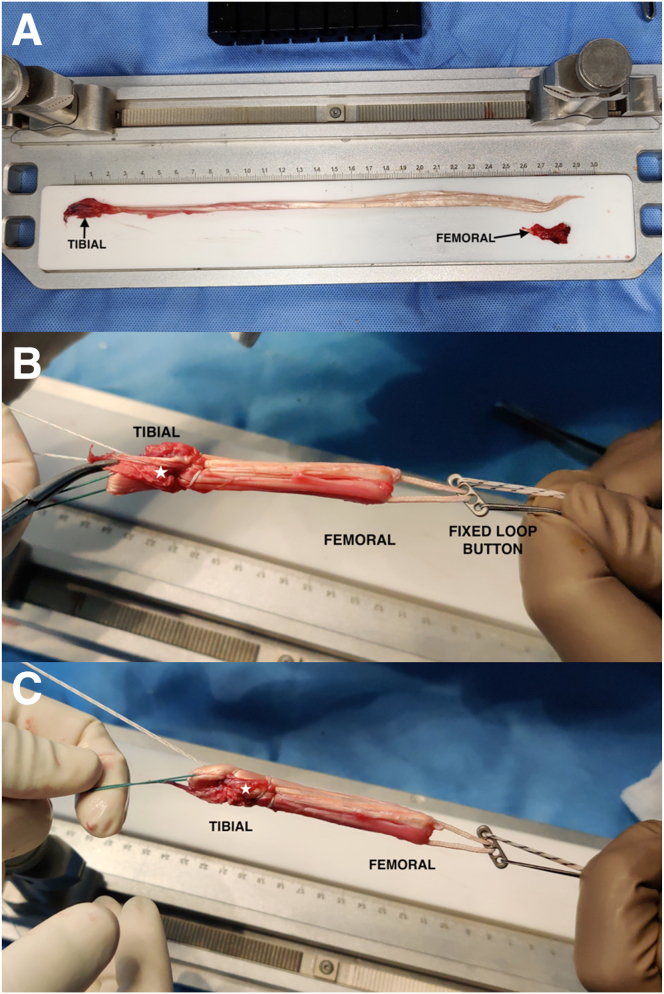
Fig 5.
Clinical photographs depicting (A) harvested STT with attached periosteal sleeve that will be at the tibial end of the graft; the free flap that will be sutured onto the femoral end of the graft is also shown. (B-C) Quadrupled STT over a fixed loop button with attached periosteal sleeve enveloping the tibial end (white asterisk). (STT, semitendinosus tendon.)
The STT is prepared by whip-stitching either end with 2-0 FibreWire loop (Healthium Pvt Ltd., Peenya, Bengaluru, Karnataka, India) and quadrupled over a fixed button loop (25 mm) (INFILOOP; Healthium Pvt Ltd.) (Fig 5B) in such a way that the periosteal sleeve at the end of the STT covers the tibial end of the graft (Fig 5 B and C and Video 1).
The free periosteal sleeve of 2.5 × 1.5 cm (Fig 6A) can be harvested from proximal tibia, medial to tibial tubercle, either distal to the STT insertion or proximal to the GT insertion. In the current scenario, it was harvested proximal to GT tendon (Fig 6B). Once the free periosteal sleeve is harvested, it is flipped inside out and sutured on to the femoral end of the quadrupled STT graft using 3-0 MONOCRYL (Ethicon, Somerville, NJ; Fig 7A) in such a way that the cambium layer faces towards the periphery, ie, the cambium layer comes in contact with the tunnel surfaces once the graft is secured. The location of the periosteal sleeves on either end of the graft should be designed in such a way that they lie close to the mouths of the tunnels when graft is secured in the tunnels (Fig 7B and Video 1). The ends of the periosteal sleeves along the graft are marked to facilitate intraoperative identification and accurate placement (Fig 8).
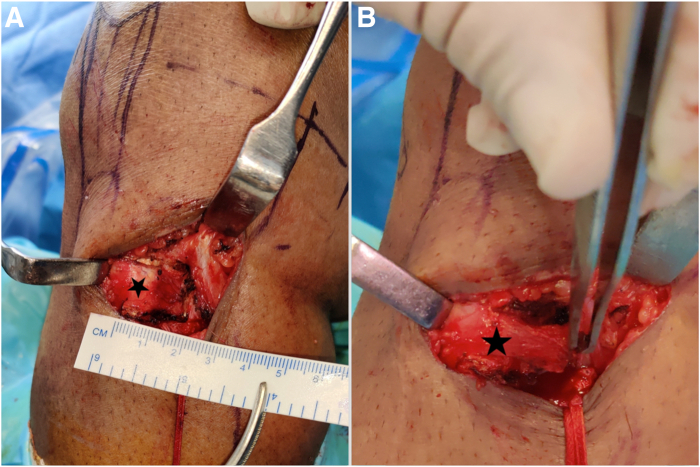
Fig 6.
Clinical photographs of patient’s right knee, viewed from the medial side, depicting (A) area for harvest of free flap of periosteum of 2.5 × 1.5 cm (black asterisk) proximal to the gracilis insertion is marked. (B) Free flap of periosteum is isolated and harvested from the aforementioned location.
Fig 7.
Clinical photographs depicting (A) free flap of periosteum (black asterisk) flipped inside out and being sutured onto the femoral end of the quadrupled STT. (B) Quadrupled STT graft over a fixed loop button with periosteal sleeves on either, Note the location of the periosteal sleeves on the quadrupled graft, which must be positioned at intra-articular margins of the planned femoral and tibial tunnels. White asterisk: Periosteal sleeve attached to STT, which will be at the tibial side of the graft; black asterisk: Free flap of periosteum sutured on to the femoral side of the graft. (STT, semitendinosus tendon.)
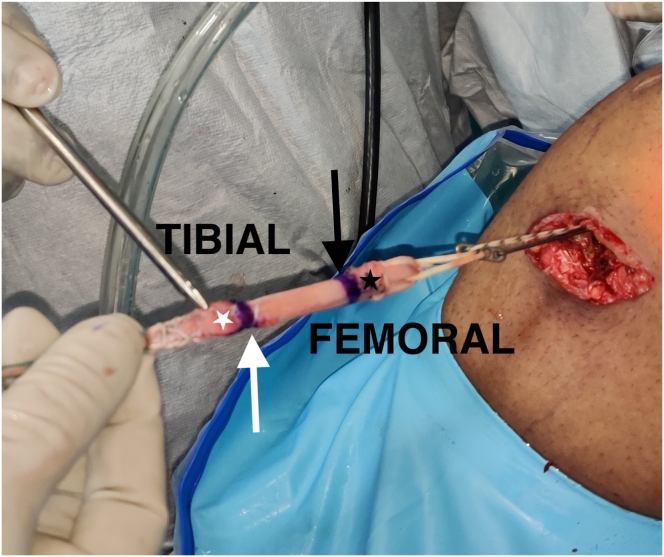
Fig 8.
Clinical photograph of quadrupled STT graft being railroaded through the tibial tunnel. Patients right knee viewed from medial side. Note the position of the periosteal sleeves (white asterisk: tibial, black asterisk: femoral) with respect to circumferential reference markings (white arrow: tibial margin, black arrow: femoral margin), which denote the intra-articular margins of the bone tunnels. (STT, semitendinosus tendon.)
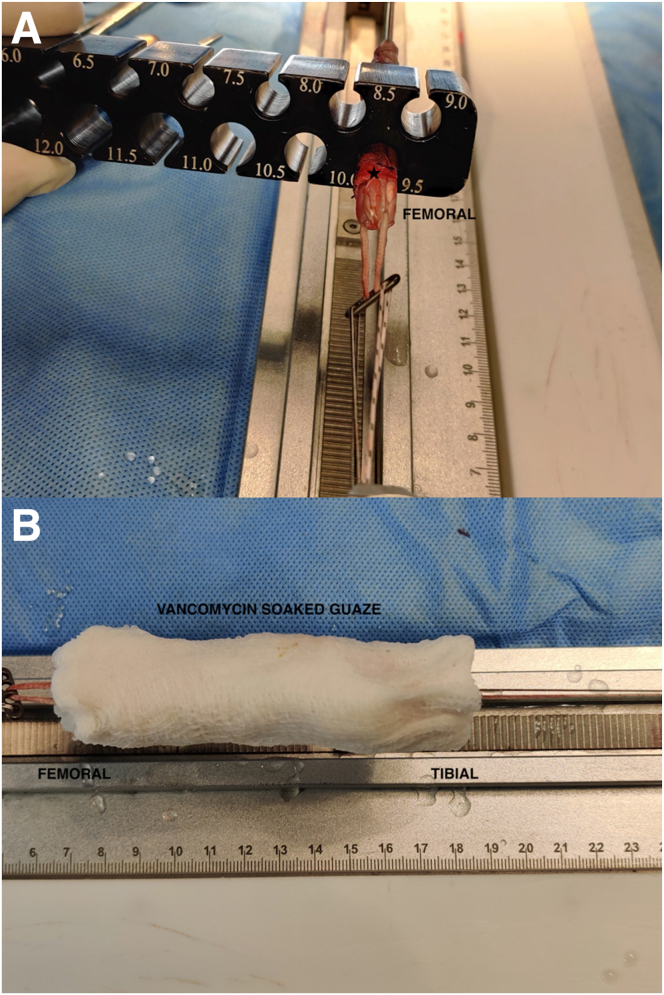
The diameter of the graft is ascertained (Fig 9A). Note that the addition of free periosteal sleeve onto the femoral end of the graft may increase the diameter by 0.5 to 1.0 mm, hence adjustments to tunnel placements must be planned accordingly.
Fig 9.
Clinical photographs depicting (A) sizing of the prepared graft. Note that the final diameter of the graft will be increased by 0.5 to 1.0 mm after the periosteum augmentation. (B) Enveloping the prepared graft with vancomycin-soaked gauze while tensioning it. Black asterisk: free flap of periosteum sutured on to the femoral side of the graft.
Tunnel Preparation
Once the graft diameters at both ends are ascertained individually, sequential drilling of the femoral and tibial tunnels is carried out. For the femoral tunnel, the index knee is flexed to 110°, and the optimum point for tunnel position is determined and a 4-mm Beath pin over a 7-mm offset guide is drilled, exiting midway between the superior and mid third of lateral thigh. The tunnel length is measured using a depth gauge, which determines the length of the fixed loop button to be selected which in turn dictates the intratunnel length of the graft. Over the Beath pin, a close-ended femoral tunnel is sequentially reamed to the appropriate diameter. Similarly, for tibial tunnel, the optimal point in the ACL tibial footprint is determined and tip- or elbow-aimed tibial guide is used with 55° angle to place a guide pin pointing through the posterior half and medial-lateral center of native ACL tibial foot print. Then, an open-ended tibial tunnel is sequentially reamed over the guide pin to the desired size. A suture shuttle is used in standard fashion to railroad the quadrupled STT graft with periosteum sutured on either end.
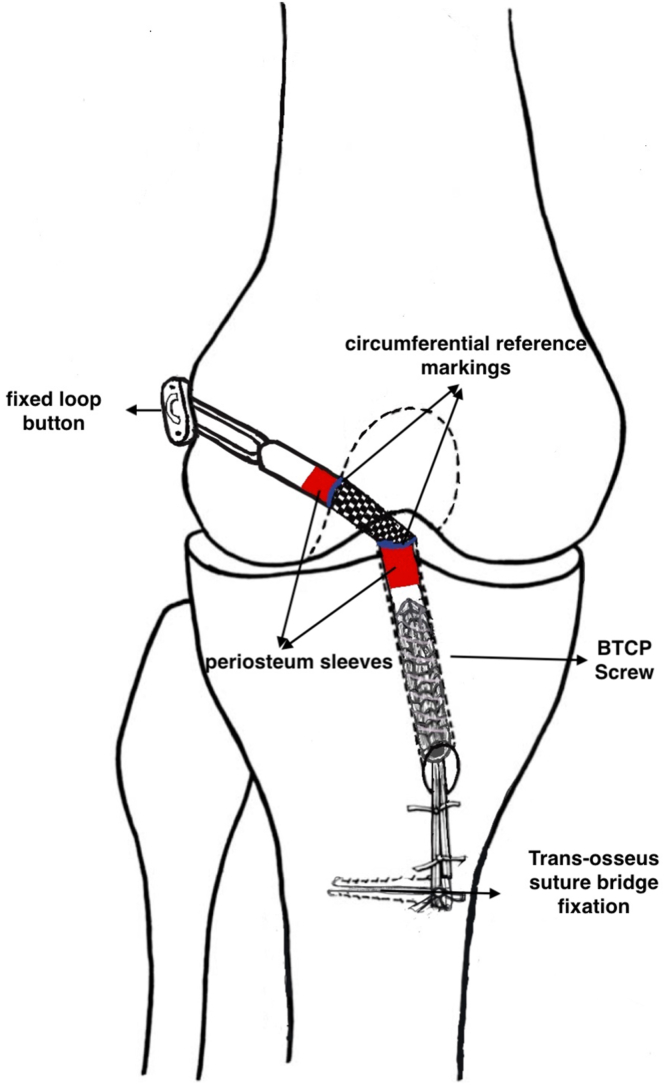
Graft Shuttling and Fixation
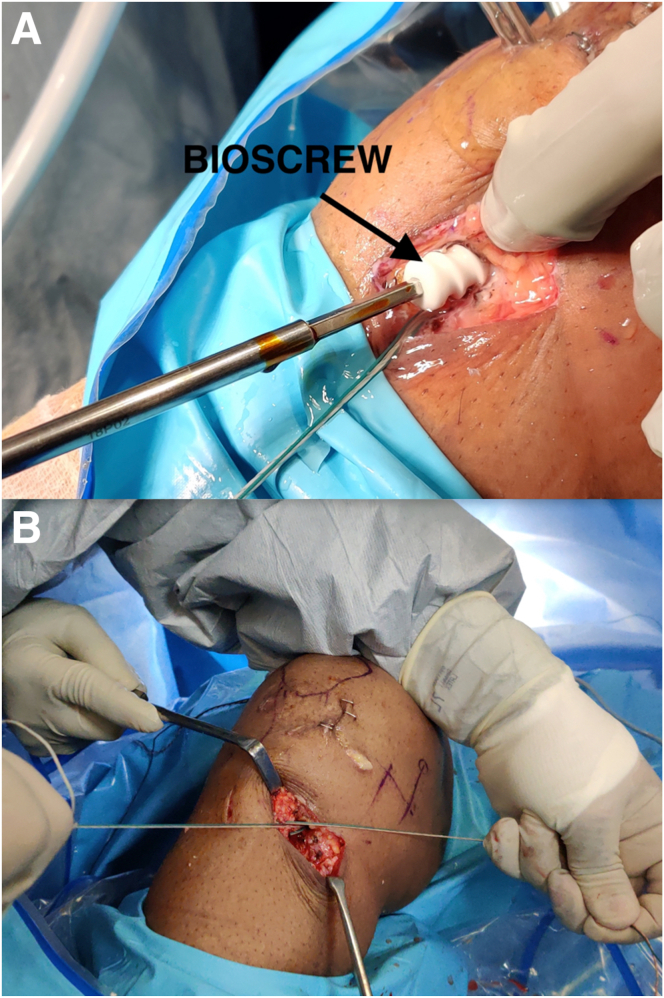
The prepared graft is railroaded in retrograde fashion with the help of suture loop (Fig 8 and Video 1). Once the button is intra-articular, under arthroscopy guidance, the graft is assisted into the femoral tunnel with an arthroscopy probe to avoid the stripping of the sutured periosteum (Video 1). The premarked circumferential reference markings help in confirming the position of the periosteal sleeves in the tunnels. Ideally, the periosteal sleeves should be located inside and close to the intra-articular opening of the tunnels (Video 1). Once the graft is satisfactorily in place, the button on the femoral side is flipped over the outer cortex to establish far cortex suspensory fixation. The tibial tunnel is fixed after tensioning with a biphasic tri-calcium phosphate screw (Fig 10A) (Helysis; Healthium Pvt Ltd.) of appropriate length and diameter in near extension, making sure it doesn’t crush the periosteum as shown in the diagram (Fig 11). Instead of interference screw fixation at the tibial end, far cortex suspensory fixation may be considered as an alternative. Supplementary transosseous suture bridge fixation (Fig 10B and Video 1) using the suture tails of the graft is done as a rule in all cases of ACL reconstruction at our institute. The step-by-step description of the procedure is enumerated in Table 1. It is advised to refer to Table 2 for some useful tips during the surgery.
Fig 10.
Clinical photographs depicting (A) fixation of the tibial side of the graft with a variable-pitch biphasic tri-calcium phosphate screw with the knee in 25° to 30° of flexion. (B) Supplementary transosseous suture bridge fixation being done. Patients right knee viewed from medial side.
Fig 11.
Diagram depicting the final fixation of the graft illustrating the location of the periosteal sleeves in the bone tunnels. Note that the length of the screw is selected such that it is long enough to fix the graft in the tibial tunnel but stops short of periosteal sleeve ensuring its integrity. (BTCP, biphasic tri-calcium phosphate.)
Table 1.
Step-by-Step Description of the Procedure
|
BTCP, biphasic tri-calcium phosphate.
Table 2.
Pearls and Pitfalls
Pearls
|
Pitfalls
|
GT, gracilis tendon.
Postoperative Rehabilitation
A criteria-based rehabilitation protocol is followed. This includes immediate and early weight-bearing, early range of motion with focus on restoring complete extension range of motion, and exercise progressions based on the patient achieving clinical and functional milestones.7 The rehabilitation program consists of a preoperative rehabilitation phase and 3 criterion-based postoperative phases: (1) impairment-based progression phase; (2) sport-specific training phase; and (3) return to play phase. Postoperative rehabilitation continues for 9 months at varying levels of supervision based on the patient compliance and functional goals.
Discussion
In ACL reconstruction with hamstring graft, tunnel widening may compromise tendon graft incorporation into the bone, which is a major area of concern. A study conducted by Baumfeld et al.8 states that the incidence of tunnel widening is significantly greater with far cortex suspensory fixation when compared with in-tunnel fixation. Tunnel expansion is a concern in cases in which accelerated rehabilitation is followed.
Histologically, periosteum has a superficial fibrous layer that contains fibroblasts, which help in forming a scar tissue containing collagen fibers, and a deep cambium layer that contains progenitor cells, which differentiate to osteoblasts and chondroblasts that subsequently differentiate into unmineralized fibrocartilage and mineralized fibrocartilage, which can hasten the incorporation of the graft into the tunnel.9 This early healing can facilitate early rehabilitation and quicker return to sports activities. In 1930, a study conducted by Burman and Umansky10 showed that a free periosteal graft wrapped around a tendon could generate bony ingrowth in as early as 2 weeks. Chen et al.6 conducted a study showing that periosteum enveloping of hamstring graft on either side, minimizes the tunnel widening.
The technique described in this article illustrates a simple autogenous technique to envelope the hamstring graft with periosteal sleeves on either end, which would facilitate early osteointegration of the graft into the tunnels and promote early return to sport. The advantages and limitations of the procedure are enumerated in Table 3.
Table 3.
Advantages and Limitations of the Procedure
Advantages
|
Limitations
|
Disclosure
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Acknowledgments
The authors acknowledge Ms. Mary, Scrub Nurse, Department of Orthopaedics, St. John’s Medical College, Mr. Paramesh, OT Technician, St John’s Medical College, Bangalore, India, and Ms. Hannah Rajkumar and Ms. Chrislyn Rajkumar for their technical support in this project.
Supplementary Data
Patient’s right knee positioned in supine in 90 degree flexion using lateral support, being viewed from medial side and arthroscopically via Anterolateral portal.
References
- 1.Moulton S.G., Steineman B.D., Haut Donahue T.L., Fontboté C.A., Cram T.R., LaPrade R.F. Direct versus indirect ACL femoral attachment fibres and their implications on ACL graft placement. Knee Surg Sports Traumatol Arthrosc. 2017;25:165–171. doi: 10.1007/s00167-016-4188-9. [DOI] [PubMed] [Google Scholar]
- 2.Kopf S., Musahl V., Tashman S., Szczodry M., Shen W., Fu F.H. A systematic review of the femoral origin and tibial insertion morphology of the ACL. Knee Surg Sports Traumatol Arthrosc. 2009;17:213–219. doi: 10.1007/s00167-008-0709-5. [DOI] [PubMed] [Google Scholar]
- 3.Eriksson K., Kindblom L.G., Wredmark T. Semitendinosus tendon graft ingrowth in tibial tunnel following ACL reconstruction: A histological study of 2 patients with different types of early graft failure. Acta Orthop Scand. 2000;71:275–279. doi: 10.1080/000164700317411870. [DOI] [PubMed] [Google Scholar]
- 4.Hardy A., Casabianca L., Andrieu K., Baverel L., Noailles T. Complications following harvesting of patellar tendon or hamstring tendon grafts for anterior cruciate ligament reconstruction: Systematic review of literature. Orthop Traumatol Surg Res. 2017;103:S245–S248. doi: 10.1016/j.otsr.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 5.Di Benedetto P., Di Benedetto E., Fiocchi A., Beltrame A., Causero A. Causes of failure of anterior cruciate ligament reconstruction and revision surgical strategies. Knee Surg Relat Res. 2016;28:319–324. doi: 10.5792/ksrr.16.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen C.H., Chang C.H., Su C.I., et al. Arthroscopic single-bundle anterior cruciate ligament reconstruction with periosteum-enveloping hamstring tendon graft: Clinical outcome at 2 to 7 years. Arthroscopy. 2010;26:907–917. doi: 10.1016/j.arthro.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 7.van Melick N., van Cingel R.E., Brooijmans F., et al. Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506–1515. doi: 10.1136/bjsports-2015-095898. [DOI] [PubMed] [Google Scholar]
- 8.Baumfeld J.A., Diduch D.R., Rubino L.J., et al. Tunnel widening following anterior cruciate ligament reconstruction using hamstring autograft: A comparison between double cross-pin and suspensory graft fixation. Knee Surg Sports Traumatol Arthrosc. 2008;16:1108–1113. doi: 10.1007/s00167-008-0606-y. [DOI] [PubMed] [Google Scholar]
- 9.Li M., Amizuka N., Oda K., et al. Histochemical evidence of the initial chondrogenesis and osteogenesis in the periosteum of a rib fractured model: Implications of osteocyte involvement in periosteal chondrogenesis. Microsc Res Tech. 2004;64:330–342. doi: 10.1002/jemt.20088. [DOI] [PubMed] [Google Scholar]
- 10.Burman M.S., Umansky M. An experimental study of free periosteal transplants, wrapped around tendon: With a review of the literature. J Bone Joint Surg. 1930;12 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient’s right knee positioned in supine in 90 degree flexion using lateral support, being viewed from medial side and arthroscopically via Anterolateral portal.
Patient’s right knee positioned in supine in 90 degree flexion using lateral support, being viewed from medial side and arthroscopically via Anterolateral portal.