Outdoor air pollution affects lung development and leads to morbidity from asthma in children and adults. Current evidence supports a causal link between pre- and early-postnatal exposure to outdoor pollutants and childhood asthma. Recent findings suggest that several factors attenuate or enhance the detrimental effects of outdoor pollutants on asthma, including genetic variants, exposure to violence and chronic psychosocial stress, indoor pollutants, diet, and obesity (Figure 1).
Fig 1.
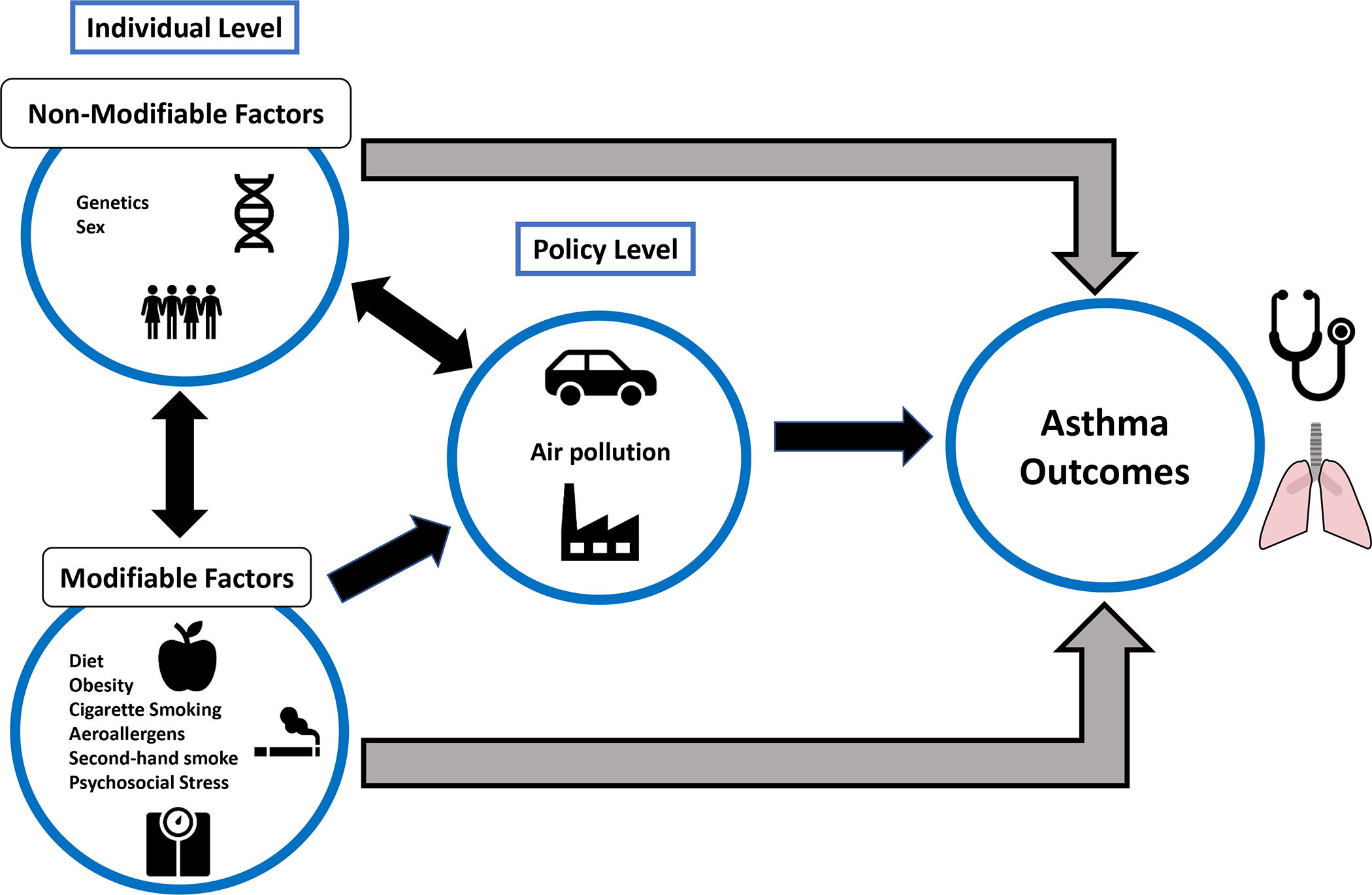
Factors that may mitigate or augment the harmful effects of air pollution on asthma are shown. Non-modifiable factors can interact with modifiable factors, and both can in turn interact with air pollution. Modifiable and non-modifiable factors should be considered when addressing air pollution at the policy level.
Candidate-gene studies have identified gene-by-pollutant interactions on asthma (i.e. between the GSTM1 null genotype and ozone), but no firm conclusions can be drawn due to inconsistent results or insufficient replication. A recent genome-wide interaction study in 1,534 European children identified gene by NO2 interactions on asthma, but only those for adenylate cyclase 2 were partially replicated in one of two North American cohorts,1 Similarly, candidate-gene studies of pollutant-related methylation markers have been limited by small sample size or inadequate replication.
Air pollution and chronic psychosocial stress can increase oxidative stress, and pre- or post-natal stress and pollutants may have synergistic detrimental effects on asthma and lung function in children. In a birth cohort study, prenatal exposure to nitrate or PM2.5 was significantly associated with asthma and reduced lung function at age 6 years in boys exposed to chronic stress, but not in girls.2 In another birth cohort, post-natal NO2 exposure was associated with asthma in children with high lifetime exposure to violence but not in those with lower lifetime exposure to violence. Similarly, longitudinal studies found that postnatal exposure to total oxides of nitrogen and other forms of traffic-related air pollution (TRAP) were linked to asthma and reduced lung function in children whose parents were highly stressed.3 There have been no clinical trials of stress reduction to reduce pollutant effects on asthma.
Cigarette smoking may modify the effect of air pollution on asthma in adults, as current or former smokers appear to be more prone to develop incident asthma related to outdoor pollutants than never smokers. Although SHS increases the risk of childhood asthma and may thus worsen the effects of air pollution on asthma, few studies have directly examined this potential interaction. Since eliminating active smoking and SHS has beneficial effects not only on asthma but on general health, vigorous efforts to help prevent or quit smoking must continue.
Concurrent exposure to aero-allergens and air pollutants may enhance airway inflammation and lead to asthma exacerbations. A cross-sectional study using population-level data showed that high exposure to fungal and pollen allergens may interact with PM2.5 or PM10 to increase the risk of hospitalizations for asthma. In another study, co-exposure to DEP and dust mite allergen increased TH2 cytokines and airway responsiveness in a murine model, and high exposure to DEP was associated with asthma in atopic children but not in non-atopic children.4 Small clinical trials in adults have demonstrated enhanced allergen-induced airway inflammation in participants exposed to DEP, ozone, and NO2.5 Whether modifying outdoor activity during high pollen season or reducing indoor allergen levels attenuates pollutant effects on asthma merits further study.
Obesity has been reported to modify the effects of air pollution on asthma in most, but not all, published studies. A large cross-sectional study of European adults found that PM2.5 exposure was significantly associated with wheeze and shortness of breath, without any significant interaction between obesity and air pollution on respiratory symptoms. In contrast, a longitudinal 10-year study of Swiss adults found that improved air quality reduced the rates of age-related decline in FEF25–75, FEF25–75/FVC and FEV1/FVC in participants with low to normal weight, but not in overweight or obese participants.6 Moreover, a large cross-sectional study of Chinese children found that the estimated effect of NO2 and SO2 on respiratory symptoms or asthma was significantly greater in overweight or obese children than in children of normal weight. In addition, two studies reported that short- or long-term exposure to ozone was significantly associated with greater reductions in lung function in overweight or obese adults than in non-overweight adults, with one of these studies showing this interaction only in women. Obesity is a major public health problem, and thus campaigns to prevent obesity in childhood have benefits that extend beyond any amelioration of pollution effects on asthma.
Diet and certain vitamins may attenuate the effects of air pollution on asthma. For example, gamma-tocopherol (an isoform of vitamin E) was recently shown to reduce sputum eosinophils and mucins, as well as airway responsiveness after lipopolysaccharide challenge, in a clinical trial in 15 adults with mild asthma.7 Another clinical trial examined the effects of antioxidants, including vitamin C and vitamin E, on lung function in Mexican children exposed to high levels of air pollutants. In that study, ozone levels were associated with lower FEF25–75 (−13.32 ml/second/10 ppb, P<0.001) and FEV1 (−4.59 ml/10 ppb, P=0.04) in children with moderate to severe asthma in the placebo arm, but not in those in the intervention arm.8 Regarding vitamin D, a murine model showed that vitamin D supplementation reduces the combined effects of TRAP and allergen exposure on airway responsiveness and TH2 and TH17 immune responses in the lung. Moreover, a prospective study of urban children found that higher exposure to PM2.5 was only associated with asthma symptoms in obese and vitamin D deficient children. This is partly consistent with results from a cross-sectional study that showed that children with vitamin D insufficiency who lived near a major highway (a marker of TRAP) had nearly fivefold higher odds of severe asthma exacerbations than those without either risk factor.9 With regard to diet, a prospective study demonstrated that dietary intake of fruits and vegetables was significantly and positively associated with FEV1 and FVC, particularly among children exposed to ozone. Similar findings were reported for a Mediterranean diet and FVC among children exposed to ozone. Thus, current evidence suggests that a healthy diet and, perhaps, vitamins with antioxidant properties could protect against pollution effects on asthma.
Future directions
A large longitudinal study of children in California demonstrated that improved air quality is associated with positive effects on lung function growth and reduced bronchitic symptoms during childhood,10 emphasizing that the most effective way to eliminate the detrimental effects of air pollution on asthma is through health policies to ensure “clean air” for all. Such policies should address not only pollutant levels but factors that could increase pollution, including climate change and wildfires. Similarly, public health policies designed to prevent or eliminate smoking and obesity would have beneficial effects on general health, beyond those of reducing pollutant effects on respiratory health. This said, identifying other modifiable factors that mitigate the effects of air pollution could be beneficial to populations that remain exposed to pollutants due to lack of effective policies. Moreover, studies of genetic and epigenetic modifiers of the effects of air pollution on asthma could not only identify high-risk individuals but also provide novel insights into asthma pathogenesis.
Current evidence suggests that chronic stress and an unhealthy diet or low levels of antioxidant vitamins interact with air pollution to cause or worsen asthma. Well-designed randomized clinical trials should help determine the extent to which dietary interventions or vitamin supplementation mitigate the harmful effects of air pollution on asthma. Because of the complex etiology of asthma, multifactorial trials examining several interventions (i.e. reducing SHS, weight loss, stress reduction, and a healthy diet) may be best suited to identify the most effective modifiers of pollutant-related effects.
Supplementary Material
Declaration of funding:
This work was supported by grants HL117191, HL119952, and MD011764 from the U.S. NIH. Dr. Stevens is supported by grant T32 HL129949 from the U.S. NIH. Dr. Celedón has received research materials from GSK and Merck (inhaled steroids) and Pharmavite (vitamin D and placebo capsules), to provide medications free of cost to participants in NIH-funded studies, unrelated to this work.
Abbreviations:
- DEP
Diesel exhaust particles
- FEF25–75
Forced expiratory flow at 25–75 percent of the forced vital capacity
- FEV1
Forced expiratory volume in 1 second
- FVC
Forced vital capacity
- NO2
Nitrogen dioxide
- PM2.5
Coarse particulate matter measuring less than 2.5 μm in diameter
- PM10
Coarse particulate matter measuring less than 10 μm in diameter
- SHS
Second-hand Smoke
- SO2
Sulfur dioxide
- TH2
Type 2 T helper cell
- TH17
Type 17 T helper cell
- TRAP
Traffic-related air pollution
Footnotes
conflicts of interest: The other authors have no conflicts of interest to declare.
REFERENCES
- 1.Gref A, Merid SK, Gruzieva O, Ballereau S, Becker A, Bellander T, et al. Genome-wide interaction analysis of air pollution exposure and childhood asthma with functional follow-up. Am J Respir Crit Care Med 2017;195:1373–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee A, Leon Hsu H-H, Mathilda Chiu Y-H, Bose S, Rosa MJ, Kloog I, et al. Prenatal fine particulate exposure and early childhood asthma: Effect of maternal stress and fetal sex. J Allergy Clin Immunol 2018;141:1880–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shankardass K, McConnell R, Jerrett M, Milam J, Richardson J, Berhane K. Parental stress increases the effect of traffic-related air pollution on childhood asthma incidence. Proc Natl Acad Sci USA 2009;106:12406–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brandt EB, Biagini Myers JM, Acciani TH, Ryan PH, Sivaprasad U, Ruff B, et al. Exposure to allergen and diesel exhaust particles potentiates secondary allergen-specific memory responses, promoting asthma susceptibility. J Allergy Clin Immunol 2015;136:295–303.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlsten C, Blomberg A, Pui M, Sandstrom T, Wong SW, Alexis N, et al. Diesel exhaust augments allergen-induced lower airway inflammation in allergic individuals: a controlled human exposure study. Thorax 2016;71:35–44. [DOI] [PubMed] [Google Scholar]
- 6.Schikowski T, Schaffner E, Meier F, Phuleria HC, Vierkötter A, Schindler C, et al. Improved air quality and attenuated lung function decline: modification by obesity in the SAPALDIA cohort. Environ Health Perspect 2013;121:1034–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burbank AJ, Duran CG, Pan Y, Burns P, Jones S, Jiang Q, et al. Gamma tocopherol-enriched supplement reduces sputum eosinophilia and endotoxin-induced sputum neutrophilia in volunteers with asthma. J Allergy Clin Immunol 2018;141:1231–1238.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romieu I, Sienra-Monge JJ, Ramírez-Aguilar M, Téllez-Rojo MM, Moreno-Macías H, Reyes-Ruiz NI, et al. Antioxidant supplementation and lung functions among children with asthma exposed to high levels of air pollutants. Am J Respir Crit Care Med 2002;166:703–9. [DOI] [PubMed] [Google Scholar]
- 9.Rosser F, Brehm JM, Forno E, Acosta-Pérez E, Kurland K, Canino G, et al. Proximity to a major road, vitamin D insufficiency, and severe asthma exacerbations in Puerto Rican children. Am J Respir Crit Care Med 2014;190:1190–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gauderman WJ, Urman R, Avol E, Berhane K, McConnell R, Rappaport E, et al. Association of improved air quality with lung development in children. N Engl J Med 2015;372:905–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


