Abstract
Background:
Medical students are prone to high levels of perceived stress and anxiety, which can negatively impact their academic performance, as well as their physical and mental health. This study aimed to assess the main stressors, levels of perceived stress and anxiety, and their predictors among medical students.
Design and methods:
A structured questionnaire was used to collect data from 1696 medical students at Helwan University. A cross-sectional study was designed to evaluate their perceived stress, stressors, and anxiety using the Perceived Stress Scale, Medical Students Stressor Questionnaire, and Beck Anxiety Inventory, respectively.
Results:
Approximately 93% of medical students experienced moderate to high levels of stress, while 54.9% of medical students experienced moderate to concerning levels of anxiety. The main stressors were academic, teaching, social, intrapersonal, group activity, and desire-related stressors. Risk factors associated with higher perceived stress included being female, young age, living away from the family, obtaining lower academic percentages, having psychiatric, neurological, or other chronic medical illnesses, and experiencing higher levels of academic, intrapersonal, drive, and group activities-related stressors. Risk factors for higher anxiety included being female, residing in rural areas, having psychiatric, neurological, or other chronic medical illnesses, perceiving a high level of stress, and experiencing higher levels of academic, intrapersonal, and social-related stressors.
Conclusions:
The findings indicate that a significant proportion of medical students experience various levels of stress and anxiety. These results underscore the urgent need for a stress management program, to help medical students to cope with different stressors.
Keywords: Stress, anxiety, medical students, Egypt
Introduction
Stress is a global phenomenon that has been described as the “Health Epidemic of the 21st Century” by the World Health Organization. 1 Stress is defined as a psychological state in which individuals perceive that their personal or environmental demands exceed their coping resources. 2 University students are more susceptible to stress compared to the general public. 3 The college years are a crucial period when students transition from late adolescence to adulthood. 4 This transition occurs during a highly sensitive part of the life cycle, exposing students to various stressors related to academic issues, personal situations, environment, time, and economic circumstances. 5
University students burdened by perceived psychological stress may experience deterioration in their academic performance, physical health, and mental health. 6 Stress can hinder students’ ability to concentrate, solve problems, make decisions, and complicate their overall learning experience. 7 High levels of stress among students contribute to unhealthy dietary behaviors, increasing their risk of metabolic syndrome and future cardiovascular diseases.8,9 Moreover, stress can affect interpersonal relationships and emotional state, and increase students’ liability to anxiety disorders, depression, and even suicide.10,11
Results of the WHO World Mental Health Surveys International College Student Initiative revealed that most students (93.7%) reported experiencing stress in at least one of the six life areas (financial situation, health, love life, relationships with family, relationships at work/school, and problems experienced by loved ones). Additionally, college students’ stress was associated with the common six mental disorders (Major Depressive Disorder, Bipolar Disorder, Generalized Anxiety Disorder, Panic Disorder, Alcohol Use Disorder, and Drug Use Disorder). It suggests that up to 46.9%–80% of mental disorder prevalence might be eliminated if stress prevention interventions were developed among college students within 12 months. 12
Medical students are more vulnerable to high levels of stress compared to other college students. 13 This could be explained by both academic and psychosocial pressures. 14 Factors such as the broadness of the academic curriculum, frequency of examinations, higher expectations of themselves, little time for hobbies or exercise, social isolation, competition with their peers, worrying about their future as doctors, and higher parental expectations contribute to their increased stress level compared to non-medical students.13,14
The prevalence rate of anxiety among medical students was 33.8% and 42.4%, globally and in the Middle East, respectively. 15 More than two-thirds of Egyptian medical students at Zagazig and Assiut Universities demonstrated moderate to high levels of stress and anxiety.16,17
To the best of our knowledge, little is known about the levels of stress and anxiety among Helwan Medical Students, a newly borne institution, located at “Ain Helwan” which is 30 km south of Cairo. Therefore, the objective of this study is to assess the levels of stress, anxiety, and the main stressors among these medical students. Consequently, this information could help in designing a future stress management intervention focusing on addressing their main stressors, and helping them effectively cope with stress and anxiety during college life.
Design and methods
Study setting
The study was conducted at the Faculty of Medicine, Helwan University, Egypt.
Study design and sample size
This study was a cross-sectional study targeting medical students. The estimated sample size was 384, calculated using the EPI info statistical package version 7.2.01. Assuming a proportion of stress among medical students of 0.5, a 95% confidence level, a 5% margin of error, and a 20% nonresponse rate, the sample size was increased to 460 students.
A pilot test was performed on 40 medical students, who were not included in the results of the study. This pilot test was conducted from April 1, 2022, to April 15, 2022, to fulfill the following purposes: testing the questionnaire form, detecting any necessary modifications, and estimating the time needed to collect data. Minor modifications were made to the sociodemographic part of the questionnaire after pilot testing to account for additional places of living that were not originally considered. Then, an online survey using Google Forms was published to all medical students in all academic years from April 16, 2022, to September 1, 2022. The questionnaire was filled out by 1696 medical students who responded to the survey.
Study participants
All medical students at the Faculty of Medicine, Helwan University (4000 students at the time of data collection), were eligible and received the survey without exclusion. Forty-two percent of medical students (1696 students) agreed to participate in the study and fill out the online survey.
Data collection tools
An online administered questionnaire composed of four parts: socio-demographic factors, perceived stress scale, medical student’s stressor questionnaire, and Beck anxiety inventory.
a. Socio-demographic factors included age, nationality, gender, marital status, residence, academic year, academic achievement in the last year, place of living during studying, whether working beside studying or not, smoking, taking drugs or alcohol, having chronic mental illness, consuming psychiatric drugs within the past 6 months, having chronic neurological illness, and having other chronic medical illness.
b. The Perceived Stress Scale (PSS) is the most widely used psychological instrument for measuring the perception of stress. 8 It was developed by Cohen et al. in 1983 and was designed to measure the degree to which situations in one’s life are appraised as stressful. The scale consists of 14 items that measure feelings and thoughts over the past month. Each item is scored on a five-point Likert scale, ranging from 0 to 4, where 0 represents “Never” and 4 represents “Very Often.” However, for items numbered 4, 5, 6, 7, 9, 10, and 13, the Likert scale from 0 to 4 is reversed, with 0 representing “Very Often” and 4 representing “Never.” The total score ranges from 0 to 56. Overall items were summed to determine the level of stress as follows: low level of stress ranged from (0–18), moderate level of stress (19–37), and high level of stress (38–56). 18 The validated Arabic version of PSS was used in the present study, 19 and the Cronbach’s Alpha was 0.848.
c. The Medical Students Stressor Questionnaire (MSSQ) was developed by Yusoff et al. in 2010. 20 MSSQ, indexed in the PsycTESTS database published by the American Psychologist Association, is widely used to assess sources of stress among medical students. It consists of 40 MSSQ items classified into six domains: academic-related stressors (ARS), intrapersonal- and interpersonal-related stressors (IRS), teaching- and learning-related stressors (TLRS), social-related stressors (SRS), drive-and desire-related stressors (DRS), and group activities-related stressors (GARS). Rating is done by choosing from five responses that scored respectively from 0 to 4 as follows: no stress at all, causing mild stress, causing moderate stress, causing high stress, and causing severe stress. 20 Each domain of MSSQ is scored separately according to its mean (total domain/no of items for each domain). Mean domain score: mild stressors (0–1), moderate stressors (1.01–2), high stressors (2.01–3) and severe stressors (3.01–4). 20 The questionnaire was translated from English into Arabic by the researchers, revised by a psychologist and experts, and subjected to reliability testing. The Cronbach’s Alpha of the MSSQ in this study was 0.924.
d. Beck Anxiety Inventory (BAI) is a 21-item scale developed by Beck et al. 1988 21 and is widely used to assess anxiety among students. 15 The rating is done by choosing from four responses that scored respectively from 0 to 3. The total score range is from 0 to 63. A score of 0–21 indicates low anxiety, a score of 22–35 indicates moderate anxiety, and a score of 36 and above indicates potentially concerning levels of anxiety. 21 The validated Arabic version of BAI was used in the present study, 22 and the Cronbach’s Alpha was 0.919.
Statistical analysis
Data were analyzed using SPSS version 28. First, descriptive data were presented. Quantitative data were expressed as mean and standard deviation, while frequencies and percentages were used to express the qualitative data. Then, both the Perceived Stress Scale used to assess students’ stress and the Beck Anxiety Inventory scale used to assess anxiety were assessed for data normality and were not normally distributed (Shapiro-Wilk significance was less than 0.05 in both scales). Therefore, bivariate analysis was performed to explore the variables that were significantly associated with the stress and anxiety of medical students, respectively. The Mann–Whitney U test, Independent-samples Kruskal-Wallis Test, and Spearman’s correlation coefficient test were used.
The Mann–Whitney U test was used to compare two independent groups. It was used to identify the difference in stress and anxiety levels between male and female students, Egyptians and non-Egyptians, singles and married, urban and rural students, workers and non-working students, smokers and non-smokers, alcoholic/drug takers, and non-alcoholic/drug takers, students diagnosed with chronic mental illness and others not diagnosed with chronic mental illness, consumers of psychiatric drugs within the past 6 months and non-consumers, students diagnosed with chronic neurological illness and others not diagnosed with chronic neurological illness and finally students diagnosed with chronic illness other than mental and neurological illness and others not diagnosed with chronic illness. The Independent-samples Kruskal-Wallis test was used to compare more than two independent groups. It was used to identify the difference in stress and anxiety levels between students of different academic years from 1 to 6 and students living in different places while studying (students living with their families or in external housing with other students or in the university hostel or living alone). Spearman’s correlation coefficient was used to assess the association between two quantitative variables, it was used to identify the correlation between PSS and BAI and the correlation between each of the previous scales with age, academic achievements in percentages, and MSSQ. Finally, linear regression models were conducted to detect risk factors of both stress and anxiety separately.
To detect risk factors of stress among medical students, a linear regression model for stress was performed. The dependent variable in the model was PSS. The independent variables were the socio-demographic, medical condition, and stressors, which were significantly associated with PSS in bivariate analysis (p-value < 0.05). Assumption of collinearity between the independent variables that could undermine the statistical significance of association of linear regression was assessed. Tolerance value less than 0.2 and Variance Inflation Factor more than 5 were used as indicators of collinearity. 23 Only two independent variables; having chronic mental illness and consuming psychiatric drugs were colinear (tolerance < 0.2 and VIF > 5). So, the variable consuming psychiatric drugs was deleted from the regression model to correct collinearity (adjusted R square value of the linear regression was not affected by this variable removal).
Another linear regression model was conducted to detect risk factors of anxiety. The dependent variable in the model was BAI. The independent variables were the socio-demographic, PSS, medical condition, and stressors, which were significantly associated with PSS in bivariate analysis. The two independent variables; having chronic mental illness and consuming psychiatric drugs were colinear (tolerance < 0.2 and VIF > 5). So, the variable consuming psychiatric drugs was deleted from the regression model to correct collinearity (adjusted R square value of the linear regression was not affected by this variable removal).
Results
Table 1 shows the socio-demographic characteristics of the studied students at the Faculty of Medicine, Helwan University (2022). Eighty percent of students were Egyptians, with ages ranging from 17 to 28 years. Females represented 53.2% of the sample, while males accounted for 46.8%. More than half of the students were in first and second grades (64.9%), and the mean academic percentage (achievement) was 76.1 ± 9.7. Most of the students were single (99.6%), and more than two-thirds of them were urban residents (76.9%). More than half of them lived with their families during academic studying (54.6%). Only 7.7% were working besides studying. Most of the students were not smokers and did not take drugs or alcohol (94.2% and 99.6%, respectively). A minority of the studied students suffered from mental, neurological, or other chronic medical illnesses (2.7%, 0.9%, and 8.7%, respectively).
Table 1.
Socio-demographic characteristics of the studied students at the Faculty of Medicine, Helwan University (2022).
| Variable | No. (n = 1696) | % |
|---|---|---|
| Age: (years) | ||
| Range | (17–28) | |
| Mean ± SD | (20.56 ± 1.63) | Mean ± SD |
| Nationality | ||
| Egyptian | 1356 | 80 |
| Sudanese | 278 | 16.4 |
| Other Arabian and African Countries | 62 | 3.6 |
| Gender | ||
| Male | 793 | 46.8 |
| Female | 903 | 53.2 |
| Marital status | ||
| Single | 1689 | 99.6 |
| Married | 7 | 0.4 |
| Academic year | ||
| First | 486 | 28.7 |
| Second | 614 | 36.2 |
| Third | 180 | 10.6 |
| Fourth | 214 | 12.6 |
| Fifth | 101 | 6.0 |
| Six | 101 | 6.0 |
| Academic achievement in the previous year (100%) | ||
| Range | (40–98) | |
| Mean ± SD | (76.11 ± 9.68) | |
| Excellent | 401 | 23.6 |
| Very good | 588 | 34.7 |
| Good | 517 | 30.5 |
| Accepted | 163 | 9.6 |
| Fail | 27 | 1.6 |
| Residence | ||
| Urban | 1305 | 76.9 |
| Rural | 391 | 23.1 |
| Living during studying | ||
| With the family | 926 | 54.6 |
| Sharing home with other students | 393 | 23.2 |
| In the university hostel | 260 | 15.3 |
| Living alone in a separate home | 117 | 6.9 |
| Working beside studying | ||
| No | 1565 | 92.3 |
| Yes | 131 | 7.7 |
| Smoking | ||
| No | 1597 | 94.2 |
| Yes | 71 | 4.2 |
| Ex-smoker | 28 | 1.7 |
| Taking drugs or alcohol | ||
| No | 1690 | 99.6 |
| Yesa | 6 | 0.4 |
| Having diagnosed chronic mental illness | ||
| No | 1650 | 97.3 |
| Yes | 46 | 2.7 |
| Consuming psychiatric drugs currently or within the past 6 months | ||
| No | 1640 | 96.7 |
| Yes | 56 | 3.3 |
| Having a chronic neurological disease | ||
| No | 1681 | 99.1 |
| Yesa | 15 | 0.9 |
| Having chronic medical illness other than mental or neurological illness | ||
| No | 1549 | 91.3 |
| Yes | 146 | 8.7 |
Ten students consumed psychiatric drugs without being diagnosed with any mental illness.
The mean scores of the PSS total scale, BAI, and MSSQ were 31.8 ± 8.6, 24.2 ± 13.1, and 76.1 ± 25, respectively. The main stressors, in order of significance, among medical students, as shown in Table 2, were academic, teaching, social, intrapersonal, group activity, and drive- and desire-related stressors (Means = 29.2 ± 9.4, 15.3 ± 7.3, 10.5 ± 5, 9.7 ± 7, 6.3 ± 4.1, and 5.2 ± 3.3, respectively). Approximately 70% of students perceived academic stressors as high/severe stressors. More than half of students perceived teaching and learning stressors as high/severe stressors (54.3%). At the same time, social stressors represented high/severe stressors for 33.1% of the studied students.
Table 2.
Main stressors among the studied students at the Faculty of Medicine, Helwan University (2022).
| Name of the scale | Range | Mean ± SD/median + interquartile range | ||
|---|---|---|---|---|
| Medical Student Stressor Questionnaire | (0–152) | 76.10 ± 25.04/76 + 33 | ||
| ARS | (2–48) | 29.18 ± 9.36/30 + 14 | ||
| ARS categories | Mild No. (%) |
Moderate No. (%) |
High No. (%) |
Severe No. (%) |
| 78 (4.6) | 440 (25.9) | 767 (45.2) | 411 (24.2) | |
| IRS | (0–28) | 9.72 ± 7.02/9 + 11 | ||
| IRS categories | Mild No. (%) |
Moderate No. (%) |
High No. (%) |
Severe No. (%) |
| 723 (42.6) | 541 (31.9) | 326 (19.2) | 106 (6.3) | |
| TLRS | (0–28) | 15.28 ± 7.31/15 + 12 | ||
| TLRS categories | Mild No. (%) |
Moderate No. (%) |
High No. (%) |
Severe No. (%) |
| 298 (17.6) | 477 (28.1) | 528 (31.1) | 393 (23.2) | |
| SRS | (0–24) | 10.45 ± 4.96/11 + 7 | ||
| SRS categories | Mild No. (%) |
Moderate No. (%) |
High No. (%) |
Severe No. (%) |
| 385 (22.7) | 749 (44.2) | 477 (28.1) | 85 (5) | |
| DRS | (0–12) | 5.19 ± 3.29/5 + 4 | ||
| DRS categories | Mild No. (%) |
Moderate No. (%) |
High No. (%) |
Severe No. (%) |
| 602 (35.5) | 536 (31.6) | 339 (20) | 219 (12.9) | |
| GARS | (0–16) | 6.30 ± 4.12/6 + 6 | ||
| GARS categories | Mild No. (%) |
Moderate No. (%) |
High No. (%) |
Severe No. (%) |
| 653 (38.5) | 571 (33.7) | 327(19.3) | 145(8.5) | |
ARS: academic-related stressors; IRS: intrapersonal- and interpersonal-related stressors; TLRS: teaching- and learning-related stressors; SRS: social-related stressors; DRS: drive- and desire-related stressors; GARS: group activities-related to stressors.
Figure 1 illustrates that 93.2% of medical students were exposed to moderate to high levels of stress, while 54.9% were exposed to moderate to concerning levels of anxiety, as shown in Figure 2.
Figure 1.
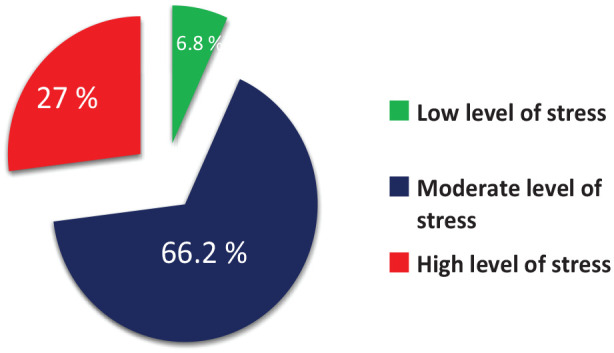
Levels of perceived stress of the studied students at the Faculty of Medicine, Helwan University (2022).
Figure 2.
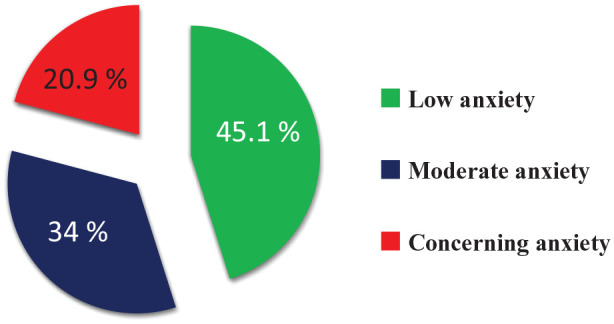
Levels of Anxiety of the studied students at the Faculty of Medicine, Helwan University (2022).
The significant variables associated with stress in bivariate analysis (p < 0.05) were entered as independent variables in the multivariable linear regression model for risk factors of stress. Table 3 showed that the risk factors for higher perceived stress of the studied students were as follows: being female (ß = 3.768, p-value < 0.001), younger age students (ß = − 0.327, p-value = 0.008), living away from the family (ß = 0.953, p-value = 0.025), obtaining lower academic percentages (ß = −0.050, p-value = 0.012), having chronic psychiatric, neurological or other chronic medical illnesses (ß = 4.164, 5.087, 1.584, p-value < 0.001, 0.011, 0.017, respectively), and having higher academic-, intrapersonal-, drive- and group-activities related stressors (ß = 2.618, 0.791, 1.049, and 0.750, p-value < 0.001, p-value < 0.001, p-value < 0.001, p-value = 0.001, respectively)
Table 3.
Linear regression model of the socio-demographic data and MSSQ on perceived stress among the studied students at the Faculty of Medicine, Helwan University, 2022.
| Variable | Unstandardized coefficient (ß) | p-Value | Collinearity statistics | |
|---|---|---|---|---|
| Tolerance | VIF | |||
| Age of the students | –0. 327 | 0.008* | 0.839 | 1.192 |
| Nationality (Non-Egyptians) | –0.969 | 0.151 | 0.469 | 2.131 |
| Gender (female) | 3.768 | <0.001* | 0.930 | 1.075 |
| Grade (one) | 0.852 | 0.115 | 0.573 | 1.745 |
| Living away from the family | 0.953 | 0.025* | 0.765 | 1.308 |
| Residence (rural) | 0.138 | 0.773 | 0.834 | 1.199 |
| Academic percent | –0.050 | 0.012* | 0.911 | 1.098 |
| Taking drugs or alcohol (yes) | –6.083 | 0.053 | 0.982 | 1.018 |
| Having diagnosed with chronic mental illness (yes) | 4.164 | <0.001* | 0.981 | 1.019 |
| Having chronic neurological disease (yes) | 5.087 | 0.011* | 0.986 | 1.015 |
| Having another chronic medical illness (yes) | 1.584 | 0.017* | 0.977 | 1.023 |
| Academic stressors | 2.618 | <0.001* | 0.687 | 1.455 |
| Intrapersonal stressors | 0.791 | <0.001* | 0.701 | 1.426 |
| Teaching stressors | 0.046 | 0.832 | 0.663 | 1.509 |
| Social stressors | 0.250 | 0.376 | 0.628 | 1.592 |
| Drive stressors | 1.049 | <0.001* | 0.730 | 1.369 |
| Group stressors | 0.750 | 0.001* | 0.643 | 1.555 |
Adjusted linear regression model; F = 29.284, p-value < 0.001, adjusted R square = 0.221.
Reference groups were Egyptians, males, grades other than one, living with the family, urban, not taking drugs or alcohol, not diagnosed with chronic mental illness, not diagnosed with chronic neurological illness, and not diagnosed with other chronic medical illness.
Significant variable.
The significant variables associated with anxiety in bivariate analysis (p-value < 0.05) were entered as independent variables in the multivariable linear regression model for risk factors of anxiety. Table 4 showed that the risk factors for higher anxiety among the studied students were as follows: being female (ß = 3.990, p-value < 0.001), rural residents (ß = 2.449, p-value < 0.001), having chronic psychiatric, chronic neurological or other chronic medical illnesses (ß = 6.894, 6, 569, 3.633, p-value < 0.001, p-value = 0.018, p-value < 0.001, respectively), perceiving high level of stress (ß = 0.492, p-value < 0.001) and having higher academic-, intrapersonal-, and social-related stressors (ß = 1.322, 1.779 and 2.035, p-value = 0.001, p-value < 0.001, p-value < 0.001, respectively).
Table 4.
Linear regression model of the socio-demographic data, MSSQ, and PSS on Anxiety (BAI) among the studied students at the Faculty of Medicine, Helwan University, 2022.
| Variable | Unstandardized coefficient (ß) | p-Value | Collinearity statistics | |
|---|---|---|---|---|
| Tolerance | VIF | |||
| Age of the students | –0.204 | 0.241 | 0.836 | 1.197 |
| Nationality (Non-Egyptians) | 1.613 | 0.088 | 0.469 | 2.133 |
| Gender (female) | 3.990 | <0.001* | 0.880 | 1.136 |
| Grade (one) | 0.273 | 0.718 | 0.572 | 1.748 |
| Living away from the family | 0.482 | 0.417 | 0.762 | 1.312 |
| Residence (rural) | 2.449 | <0.001* | 0.834 | 1.199 |
| Academic percent | –0.024 | 0.398 | 0.907 | 1.102 |
| Taking drugs or alcohol (yes) | 2.787 | 0.526 | 0.980 | 1.020 |
| Having diagnosed with chronic mental illness (yes) | 6.894 | <0.001* | 0.974 | 1.027 |
| Having chronic neurological disease (yes) | 6.569 | 0.018* | 0.982 | 1.019 |
| Having another chronic medical illness (yes) | 3.633 | <0.001* | 0.974 | 1.027 |
| Perceived stress scale total score | 0.492 | <0.001* | 0.771 | 1.297 |
| Academic stressors | 1.322 | 0.001* | 0.654 | 1.528 |
| Intrapersonal stressors | 1.779 | <0.001* | 0.696 | 1.437 |
| Teaching stressors | 0.071 | 0.814 | 0.663 | 1.509 |
| Social stressors | 2.035 | <0.001* | 0.628 | 1.593 |
| Drive stressors | 0.234 | 0.401 | 0.718 | 1.392 |
| Group stressors | 0.292 | 0.352 | 0.639 | 1.565 |
Adjusted linear regression model; F = 48.612, p-value < 0.001, adjusted R square = 0.336.
Reference groups were as follows: Egyptians, males, grades other than one, living with the family, urban, not taking drugs or alcohol, not diagnosed with mental illness, not consuming psychiatric drugs, not diagnosed with chronic neurological illness, and not diagnosed with other chronic medical illness.
Significant variable.
Discussion
A large number of the studied students suffered from stress and anxiety, especially females, students with chronic illness, and students who suffered mainly from academic and intrapersonal stressors.
The current study demonstrated that 93.2% of students suffered from moderate to high levels of stress, with the mean for PSS being 31.76 ± 8.63. This is higher than that demonstrated in similar studies in Saudi Arabia, Australia, China, and India, where the mean of PSS was 22.97 ± 5.80, 17.7 ± 5.5, 16.29 ± 5.71, and 27.98 + 3.09, respectively.8,24 –26 This finding could be justified by many factors. Helwan University is located away from Cairo (30 km south of Cairo). So, the long traveling distance and living away from the family could increase the stress of medical students. In addition, a large number of medical students are not Egyptians. The new integrated system of medical education and shifting of the classic system of 6 + 1 to 5 + 2 may be another factor that increases academic stress and consequently increases both the stress and anxiety of the studied students. Regarding anxiety levels, students who suffered from moderate and concerning levels of anxiety were 34% and 20.9%, respectively. This is higher than a similar Egyptian study where moderate and concerning levels of anxiety among medical students in Alexandria were 33.5% and 10.4%, respectively. 27 Switching from physical learning to either online or hybrid learning conducted in our faculty during the COVID-19 pandemic may create a stressful environment for the students, which could increase their stress and anxiety levels.
Females had a higher vulnerability to manifest stress and anxiety than males in the current study. Gender vulnerability in the experience of stress and anxiety has been recognized in different studies, with female medical students being more liable to stress and anxiety than males.17,27 –29 This discrepancy could be explained by fewer learning opportunities and fewer recreational activities available for females than males. 24 In addition, females’ cyclic hormonal changes (normal fluctuations in females sex hormones because of the menstrual cycle), result in modification of basal endogenous anxiolytics that is, serotonin and allopregnanolone activity. 30 This could lead to intermittent periods of sensitive vulnerability to anxiety, due to periodic declines in the ability to regulate anxious emotions, independent of environmental context. 30 A qualitative study revealed that female medical students usually worry more and feel more insecure about their capabilities and their performance than male students do. 31
Medical students with chronic illness struggle with facing the stress of medical education in addition to the stress triggered by their illness. Chronic illness has a negative impact on the physical, psychological, and academic performance of medical students.32,33 The current study demonstrated that having chronic mental, neurological and other medical illnesses was correlated with a higher perception of stress and anxiety among the studied medical students.
Regarding stressors, academic stressor was demonstrated as the leading cause of stress for more than two-thirds of Helwan medical students and a predictor of high stress and anxiety (ß = 2.618, 1.322, p-value < 0.001 and 0.001 respectively). These findings were in agreement with similar studies conducted in China, Iran, Ireland, and India, which concluded that academic and medical education were the main stressors among medical students.34 –37 Additionally, these findings were consistent with a systematic review of the effect of academic stress on medical students’ mental health status, which concluded that academic stress was the leading cause of high student stress, anxiety, depression, and emotional burnout. 38 An Indian study revealed that 125 suicide deaths occurred among medical students from 2010 to 2019, where academic stress emerged to be the first cause of suicide, even superior to having diagnosed mental illness among medical students. 39 Academic performance is important in shaping the level of stress and anxiety of medical students. The current study revealed that decreasing academic performance (academic percent) was correlated with increased stress levels of the studied students. In fact, stress and academic performance can be a part of a vicious cycle; poor academic performance increases the level of stress, which in turn decreases academic performance and so on. 40 For anxiety level, academic performance was negatively correlated with the anxiety level of medical students in univariate analysis, although it could not predict anxiety level in multivariable regression. This is consistent with what was reported in a similar Saudi Arabian study, where academic achievement was an insignificant predictor of anxiety. 41
Another stressor that significantly increases stress and anxiety levels among medical students is intrapersonal stressor. 42 In our study, intrapersonal stressors were predictors of higher stress and anxiety among medical students (ß = 0.032, 0.072, p-value < 0.001, respectively). Poor peer relations and intrapersonal stressors can negatively predict the academic performance of medical students. 43 Similarly, intrapersonal stressors were among the predictors of depression, anxiety, and burnout among medical students in Nepal. 42
The first year of medical school represents a major transition in the student’s life that may exceed the medical student’s ability to cope. Studies revealed that first-year students experienced higher stress scores than other years.16,44,45 However, another longitudinal study revealed a consistent increase in stress and anxiety scores as medical students progressed through their years of studying. 46 In our current study, the year of studying did not modulate the levels of stress or anxiety of the studied students. The studied medical students maintained their perceived stress and anxiety throughout their all-academic years. However, the place of living during studying was a modulator of the students stress in the current study (living away from family was correlated with higher stress among the studied students). Families are usually the main source of support for their members. Living away from family, whether in the university hostel or external housing, usually creates an unfamiliar environment for many students. Changes in food, people, and living accommodations, in addition to financial burdens, can create a stressful environment. 47 On the other hand, families can exaggerate the stress experienced by medical students. It has been reported that family pressure to study medicine is a common stressor for medical students. 20 Desire- and derive-related stressors (DRS) caused by family pressure to study medicine were among the predictors of stress in the current study.
Younger students in the current study perceived higher stress levels in linear regression (ß = −0.327, p-value = 0.008). However, younger German students were correlated with lower stress and higher academic performance. Further future research in this area is needed to identify the potential confounding factors. 40 Smoking and alcohol use were not correlated with levels of stress or anxiety among the studied medical students. This is consistent with a similar study from Saudi Arabia, where smoking was not found to be a modulating factor of undergraduate medical students’ stress (ß = 0.154, p-value = 0.704). Smoking has been reported as one of the avoidant stress-coping strategies of medical students, 48 and both smoking and alcohol intake have been associated with higher stress in medical students. 49
Finally, the stress experienced by the studied medical students was found to be a risk factor for increasing anxiety levels in our study (ß = 0.492, p-value < 0.001). Similar cross-sectional study among medical students in Malaysia supported this finding and demonstrated that stress was a significant predictor for both anxiety and depression among the participants (ß = 0.201, ß = 2.11, p-value < 0.001 for both). 50
Limitations of the study
Despite the large sample size of the study, conducting it in a single medical college limits the generalization of its results to all medical students across Egypt. The cross-sectional nature of the study hinders a complete understanding of the causal relationship between determinants and outcomes.
Conclusions and recommendations
The current study aimed to assess the levels of stress, anxiety, and the main stressors among medical students. Unfortunately, the majority of studied medical students suffered from moderate to high levels of stress, with more than half of them experiencing moderate to concerning levels of anxiety. Academic stress was found to be the leading stressor among medical students. Therefore, interventions are necessary to assist medical students in managing their stress and anxiety. Lessening the academic overload and provision of counseling and academic support is highly recommended. Such interventions should be applied to students throughout their years of study, with a particular focus on those with chronic illness. A future national representative study is recommended to explore stress and anxiety perception among medical students across all grades and to compare the situation between different Egyptian Medical Universities. A qualitative study is recommended to explore details of both genders’ perception of stress and anxiety in a greater depth.
Implications for the field of public health
Stress tends to proliferate during the life course of medical students, and its damaging impacts on physical and mental health are extensive. The current study objective was to assess the levels of stress and anxiety and detect the main stressors among medical students. The findings of the current study can serve as a foundation for designing a stress management intervention that focuses on the main stressors and facilitates healthy coping mechanisms with stress. As a result, medical students can maintain their physical, mental, and social health.
Acknowledgments
The authors gratefully thank all medical students who participated in the current study. Special thanks to Peter Dawoud Awad for revising the manuscript. Department of Public Health, Theodor Bilharz Research Institute. MBBCh.peterdawad@icloud.com. ORCID: 0000-0002-1607-1589.
Footnotes
List of abbreviations: WHO, World Health Organization; PSS, Perceived Stress Scale; BAI, Beck Anxiety Inventory; MSSQ, Medical Students Stressor Questionnaire; ARS, academic-related stressors; IRS, intrapersonal- and interpersonal-related stressors; TLRS, teaching- and learning-related stressors; SRS, social-related stressors; DRS, drive- and desire-related stressors; GARS, group activities-related stressors.
Authors’ contributions: OSE contributed to the study design, collected, analyzed, interpreted the data, and prepared the main manuscript. HAS contributed to the study design, analysis, interpretation of the data, and revision of the manuscript. SR suggested the research problem and contributed to the study design, analysis, interpretation of the data, and revision of the manuscript. NH contributed to the study design, analysis, interpretation of the data, and writing the manuscript. All authors approved the final manuscript.
Availability of data and material: The data sets that were generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Consent for publication: Not applicable.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval and consent to participate: Approval to conduct the study was obtained before starting the data collection via the Research Ethics Committee for Human and Animal Research at Helwan University, Faculty of Medicine (approval code 16-2022 date 21/2/2022). Official approval was obtained from the administrative authority of the Faculty of Medicine at Helwan University. Informed consent was obtained from the study participants themselves prior to submitting their responses to the questionnaire. Privacy and confidentiality of all data were assured by ensuring the anonymity of the questionnaire and keeping data files in a safe place.
ORCID iD: Omnya S Ebrahim  https://orcid.org/0000-0001-8021-3206
https://orcid.org/0000-0001-8021-3206
References
- 1. World Health Organisation. Doing what matters in times of stress: an illustrated guide. Geneva: World Health Organisation, 2020. [Google Scholar]
- 2. Fink G. Stress: Concepts, definition and history. 2017. DOI: 10.1016/B978-0-12-809324-5.02208-2. [DOI]
- 3. Karaman MA, Lerma E, Vela JC, et al. Predictors of academic stress among college students. J Coll Couns 2019; 22: 41–55. [Google Scholar]
- 4. The world Health Organization. The WHO World Mental Health International College Student (WMH-ICS) Initiative. Geneva: The world Health Organization, 2021. www.hcp.med.harvard.edu/wmh/college_student_survey.php [Google Scholar]
- 5. Lalithamma A, Vadivel S. Stress level comparison between pharmacy students and non-pharmacy students in Indonesia. Int J Pharm Res 2020; 12: 147–150. [Google Scholar]
- 6. You M, Laborde S, Dosseville F, et al. Associations of chronotype, Big Five, and emotional competences with perceived stress in university students. Chronobiol Int 2020; 37: 1090–1098. [DOI] [PubMed] [Google Scholar]
- 7. Alias N, Mustafa S, Hamzah L. The symptoms of stress as perceived by university students. Adv Res J Soc Sci 2020; 1: 11–20. [Google Scholar]
- 8. Chaudhuri A. A study to compare the effects of perceived stress on waist hip ratio and cardiovascular profile of MBBS and paramedical students in a Medical College of West Bengal. Int J Res Rev 2019; 6: 251–257. [Google Scholar]
- 9. Choi J. Impact of stress levels on eating behaviors among college students. Nutrients 2020; 12: 1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hamblin E. Stress in college students: associations with anxiety and perfectionism. Honors Theses, e Grove University of Mississippi, USA, 2018. [Google Scholar]
- 11. Nandagaon VS, Raddi SA. Depression and suicidal ideation as a consequence of academic stress among adolescent students. Indian J Forensic Med Toxicol 2020; 14(4): 4464–4468. [Google Scholar]
- 12. Karyotaki E, Cuijpers P, Albor Y, et al. Sources of stress and their associations with mental disorders among college students: results of the World Health Organization World Mental Health Surveys International College Student Initiative. Front Psychol 2020; 11: 1759–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Haque M. Stress among medical students - a global concern. Asian J Pharm Clin Res 2017; 10: 76. [Google Scholar]
- 14. Steiner-Hofbauer V, Holzinger A. How to cope with the challenges of medical education? Stress, depression, and coping in undergraduate medical students. Acad Psychiatry 2020; 44: 380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Quek TT, Tam WW, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health 2019; 16: 2735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abdallah AM, Sharafeddin MA, Ahmed H. Stress and coping strategies among medical students in Zagazig University - a prospective cohort study. Egypt J Community Med 2021; 39: 1–12. [Google Scholar]
- 17. Fawzy M, Hamed SA. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res 2017; 255: 186–194. [DOI] [PubMed] [Google Scholar]
- 18. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983; 24: 385–396. [PubMed] [Google Scholar]
- 19. Almadi T, Cathers I, Hamdan Mansour AM, et al. An Arabic version of the perceived stress scale: translation and validation study. Int J Nurs Stud 2012; 49: 84–89. [DOI] [PubMed] [Google Scholar]
- 20. Yusoff M, Abdul Rahim A, Yaacob M. The development and validity of the Medical Student Stressor Questionnaire (MSSQ). ASEAN J Psychiatry 2010; 11: 231–235. [Google Scholar]
- 21. Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988; 56: 893–897. [DOI] [PubMed] [Google Scholar]
- 22. Talaat H, Abdelfatah E, El Abedein A. Standardization of the Arabic version of Beck anxiety inventory in Egyptian population. Menoufia Med J 2020; 33: 361–366. [Google Scholar]
- 23. Shrestha N. Detecting multicollinearity in regression analysis. Am J Appl Math Stat 2020; 8: 39–42. [Google Scholar]
- 24. Khalil A, Professor A, Almutairi N, et al. Prevalence of stress and its association with body weight among medical students in Taibah University. Pharmacophore 2020; 11: 36–45. [Google Scholar]
- 25. Moore S, Barbour R, Ngo H, et al. Determining the feasibility and effectiveness of brief online mindfulness training for rural medical students: A pilot study. BMC Med Educ 2020; 20(1): 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Song X, Ding N, Jiang N, et al. Time use in out-of-class activities and its association with self-efficacy and perceived stress: data from second-year medical students in China. Med Educ Online 2020; 25(1):1759868. DOI: 10.1080/10872981.2020.1759868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ibrahim MB, Abdelreheem MH. Prevalence of anxiety and depression among medical and pharmaceutical students in Alexandria University. Alex J Med 2015; 51: 167–173. [Google Scholar]
- 28. Ragab EA, Dafallah MA, Salih MH, et al. Stress and its correlates among medical students in six medical colleges: an attempt to understand the current situation. Middle East Curr Psychiatry 2021; 28: 75. DOI: 10.1186/s43045-021-00158-w [DOI] [Google Scholar]
- 29. Awadalla NJ, Alsabaani AA, Alsaleem MA, et al. Increased mental stress among undergraduate medical students in south-western Saudi Arabia during the COVID-19 pandemic. PeerJ 2022; 10: e13900–e13914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Li SH, Graham BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet Psychiatry 2017; 4: 73–82. [DOI] [PubMed] [Google Scholar]
- 31. Verdonk P, Räntzsch V, de Vries R, et al. Show what you know and deal with stress yourself: A qualitative interview study of medical interns’ perceptions of stress and gender. BMC Med Educ 2014; 14: 96. DOI: 10.1186/1472-6920-14-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Thongseiratch T, Chandeying N. Chronic illnesses and student academic performance. J Heal Sci Med Res 2020; 38: 245–253. [Google Scholar]
- 33. Blignaut M. Reflection of a second year medical student: navigating medical school with chronic illness. Int J Med Stud 2021; 9: 169–170. [Google Scholar]
- 34. Liu Z, Xie Y, Sun Z, et al. Factors associated with academic burnout and its prevalence among university students: a cross-sectional study. BMC Med Educ 2023; 23(1): 317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jowkar Z, Masoumi M, Mahmoodian H. Psychological stress and stressors among clinical dental students at shiraz school of dentistry, Iran. Adv Med Educ Pract 2020; 11: 113–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gaughran F, Dineen S, Dineen M, et al. Stress in medical students. Rom J Morphol Embryol 2014; 55: 1263–1266. [PubMed] [Google Scholar]
- 37. Premnath A, Sivan S, Velayudhan R, et al. Effect of a stress reduction programme on academic stress and coping skills of first year medical students. Kerala J Psychiatry 2020; 33: 27–33. [Google Scholar]
- 38. Ruzhenkova VV, Ruzhenkov V, Lukyantseva I, et al. Academic stress and its effect on medical students’ mental health status. Drug Invent Today 2018; 10: 1171–1174. [Google Scholar]
- 39. Chahal S, Nadda A, Govil N, et al. Suicide deaths among medical students, residents and physicians in India spanning a decade (2010–2019): an exploratory study using on line news portals and Google database. Int J Soc Psychiatr 2022; 68: 718–728. [DOI] [PubMed] [Google Scholar]
- 40. Kötter T, Wagner J, Brüheim L, et al. Perceived medical school stress of undergraduate medical students predicts academic performance: an observational study. BMC Med Educ 2017; 17(1): 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Junaid MAL, Auf AI, Shaikh K, et al. Correlation between academic performance and anxiety in medical students of majmaah university - KSA. J Pak Med Assoc 2020; 70: 865–868. [DOI] [PubMed] [Google Scholar]
- 42. Pokhrel NB, Khadayat R, Tulachan P. Depression, anxiety, and burnout among medical students and residents of a medical school in Nepal: A cross-sectional study. BMC Psychiatry 2020; 20(1): 298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yu W, Yao W, Chen M, et al. School climate and academic burnout in medical students: a moderated mediation model of collective self-esteem and psychological capital. BMC Psychol 2023; 11(1): 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Abdulghani HM, AlKanhal AA, Mahmoud ES, et al. Stress and its effects on medical students: A cross-sectional study at a college of medicine in Saudi Arabia. J Health Popul Nutr 2011; 29: 516–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ramlan H, Shafri NI, Wahab S, et al. Depression, anxiety and stress in medical students: an early observation analysis. Miditerianean J Clin Psychol 8(2). DOI: 10.6092/2282-1619/mjcp-2516 [Google Scholar]
- 46. Niemi PM, Vainiomäki PT. Medical students’ distress–quality, continuity and gender differences during a six-year medical programme. Med Teach 2006; 28: 136–141. [DOI] [PubMed] [Google Scholar]
- 47. Yasmin H, Khalil S, Mazhar R. Covid 19 : Stress Management among students and its impact on their effective learning. Int Technol Educ J 2020; 4: 65–74. [Google Scholar]
- 48. Abouammoh N, Irfan F, AlFaris E. Stress coping strategies among medical students and trainees in Saudi Arabia: a qualitative study. BMC Med Educ 2020; 20(1): 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Melaku L, Mossie A, Negash A. Stress among medical students and its association with substance use and academic performance. J Biomed Educ 2015; 2015: 1–9. [Google Scholar]
- 50. Saravanan C, Wilks R. Medical students experience of and reaction to stress: the role of depression and anxiety. Sci World J 2014; 2014: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


