Abstract
Uganda’s proximity to the tenth Ebola virus disease (EVD) outbreak in the Democratic Republic of the Congo (DRC) presents a high risk of cross-border EVD transmission. Uganda conducted preparedness and risk-mapping activities to strengthen capacity to prevent EVD importation and spread from cross-border transmission. We adapted the World Health Organization (WHO) EVD Consolidated Preparedness Checklist to assess preparedness in 11 International Health Regulations domains at the district level, health facilities, and points of entry; the US Centers for Disease Control and Prevention (CDC) Border Health Capacity Discussion Guide to describe public health capacity; and the CDC Population Connectivity Across Borders tool kit to characterize movement and connectivity patterns. We identified 40 ground crossings (13 official, 27 unofficial), 80 health facilities, and more than 500 locations in 12 high-risk districts along the DRC border with increased connectivity to the EVD epicenter. The team also identified routes and congregation hubs, including origins and destinations for cross-border travelers to specified locations. Ten of the 12 districts scored less than 50% on the preparedness assessment. Using these results, Uganda developed a national EVD preparedness and response plan, including tailored interventions to enhance EVD surveillance, laboratory capacity, healthcare professional capacity, provision of supplies to priority locations, building treatment units in strategic locations, and enhancing EVD risk communication. We identified priority interventions to address risk of EVD importation and spread into Uganda. Lessons learned from this process will inform strategies to strengthen public health emergency systems in their response to public health events in similar settings.
Keywords: Ebola virus disease, Risk mapping, Public health preparedness/response, Viral hemorrhagic fevers
Ebola virus disease (EVD) is a highly infectious, acute, and often fatal hemorrhagic illness caused by the filo-virus Ebola.1 Ebola virus is transmitted to humans through contact with body fluids of infected primates and fruit bats. Since 1976, Ebola virus has caused several sporadic disease outbreaks in Africa, including the 2014 epidemic in West Africa that ultimately caused more than 28,000 cases and 11,000 deaths.2
On August 1, 2018, the Ministry of Health of the Democratic Republic of the Congo (DRC) declared an EVD outbreak, the tenth in the DRC, in the northeastern North Kivu and Ituri provinces, which border Uganda.3 Based on Uganda’s proximity to the areas where EVD cases have been reported and on the large-scale movement of people and goods across borders, the World Health Organization (WHO) classified Uganda among the 4 priority 1 countries for enhanced preparedness activities to ensure they could effectively and safely detect, investigate, report, and contain EVD cases.4 More specifically, these activities included strengthening coordination, public health surveillance, rapid response teams, point-of-entry public health capacities, laboratory capacity, case management and infection prevention and control, risk communication, and logistics. Here we describe Uganda’s initial risk assessment and preparedness initatives for EVD prevention, detection, and emergency response following the declaration of the tenth EVD outbreak in the DRC.
Materials and Methods
National Coordination Mechanism
Uganda has established a state-of-the-art public health emergency operations center (PHEOC), where designated public health emergency management personnel assemble to coordinate operational information and resources for strategic management of public health events and emergencies. Immediately following the August 1, 2018, declaration of the DRC’s EVD outbreak, the Uganda Ministry of Health activated the public health emergency operations center and the EVD National Task Force.5 The operations center serves as the ministry of health’s central focal point for organizing, coordinating, supporting, and managing all aspects of evidence-based public health emergency response efforts and as the central public health incident management center for coordinating and supporting the national task force. The national task force initiated a multiagency incident management system to coordinate central- and field-level EVD preparedness and response activities, resource management, communication, and information management. The incident management system established 11 subcommittees to address priority WHO EVD preparedness activities, including infection prevention and control, contact tracing, and community engagement. The national task force nominated an overall incident commander and leaders for the subcommittees. The subcommittee leaders composed the National Rapid Response Team (NRRT) and were responsible for leading and coordinating national and district-level activities across each of the 11 domains in the incident management system.
Initially, the national task force classified all 127 districts of Uganda into 3 cross-border EVD transmission risk categories (Figure 1).5 Category 1 (n = 20) included high-risk districts that have a physical border with the affected region in the DRC and those with refugee settlements that received refugees from the DRC, as well as the large urban areas of Kampala and Wakiso. Category 2 (n = 10) included medium-risk districts that have a physical border with the DRC but had no direct route to the outbreak area in the DRC. Category 3 (n = 97) included low-risk districts from the rest of the country that did not share a border with the outbreak area of the DRC or receive individuals from the DRC seeking refugee status.
Figure 1.
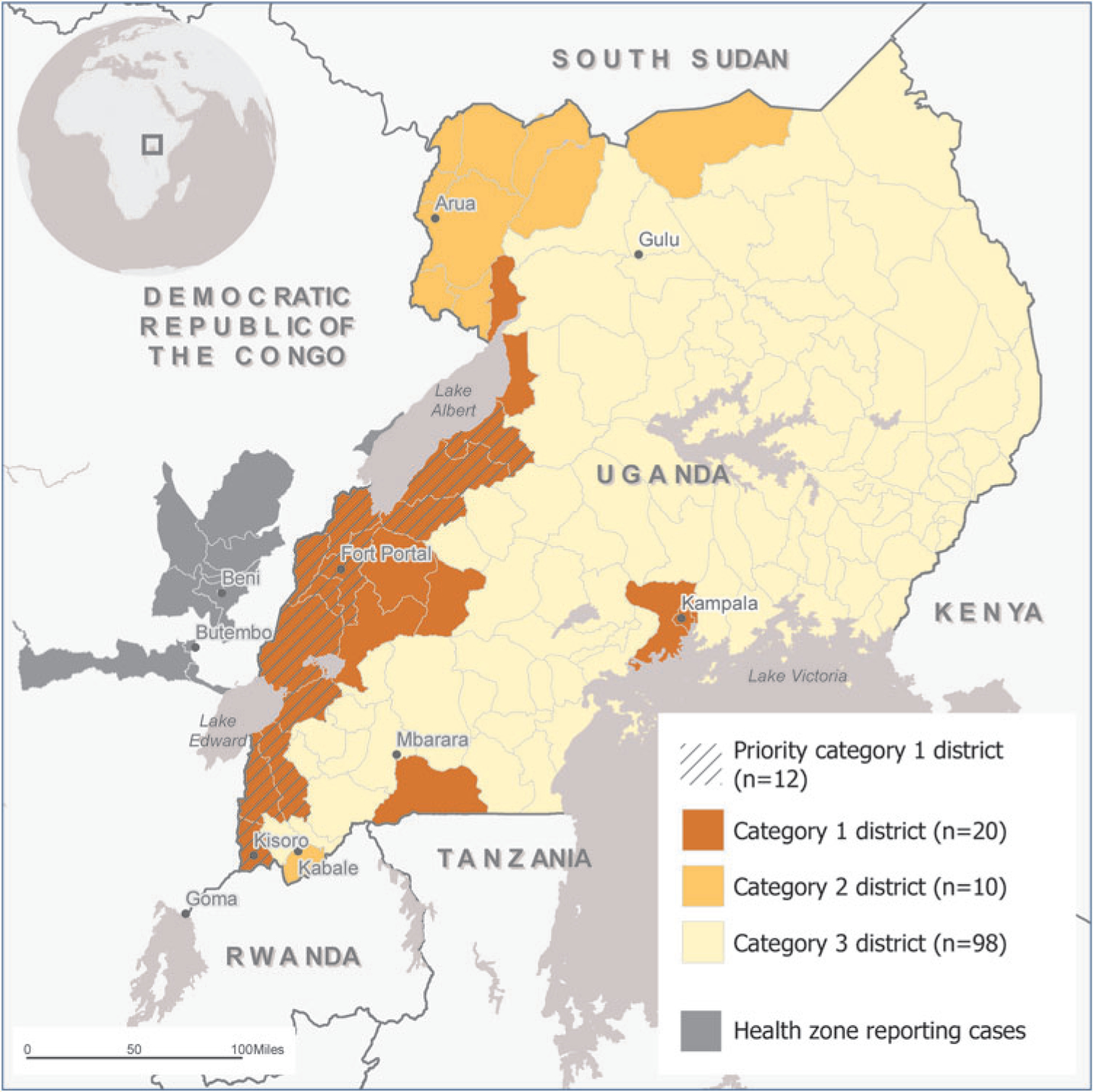
District categorization of risk of Ebola virus disease importation from the Democratic Republic of Congo, Uganda, as of August 2018. Color images are available online.
Preparedness Assessments Initiated
The ministry of health selected 12 priority high-risk districts in category 1 for the preparedness assessment because of their large-scale border crossing and refuggee settlements from the DRC. On August 4, 2018, the national task force deployed a team of border health–focused staff from the ministry of health and partner organizations to the 12 category 1 districts with a land border crossing with the DRC to assess preparedness and identify strategies to address gaps, and to complete risk mapping to select locations with high connectivity to the outbreak area for targeted interventions. The team used rapidly adapted versions of 3 internationally developed tools to complete the preparedness assessments: the WHO EVD Consolidated Preparedness Checklist, the US Centers for Disease Control and Prevention (CDC) Border Health Capacity Discussion Guide, and risk mapping using the CDC Population Connectivity Across Borders (PopCAB) tool kit. They worked across the 12 priority districts, communicating regularly with each other and with district task force teams about progress, results, and next steps, guided by the information they collected.
Tool 1: WHO EVD Consolidated Preparedness Checklist
To establish district-level preparedness, the national rapid response team oversaw the implementation of the WHO EVD Consolidated Preparedness Checklist.6 Several high-risk countries have used the checklist to identify potential gaps in readiness and concrete actions leaders can take to strengthen the health system for an EVD response.7 The checklist has 11 sections: coordination, rapid response team, public awareness and community engagement, infection prevention and control, case management, epidemiologic surveillance, contact tracing, laboratory, capacities at points of entry, budget, and logistics. Each section has multiple elements that national and subnational leadership and international partners should implement within 30, 60, and 90 days from the date of assessment.
To complete the checklist, the border health team and additional national rapid response team members worked in the 12 priority districts to facilitate face-to-face interviews and group discussions with district leaders, including district health officers, resident district commissioners, health facility staff, community leaders, security leaders, and community health teams. For additional assessment, the border health team interviewed representatives from all hospitals in the 12 districts as well as smaller health facilities in busy townships and places with frequent access by migrants and other mobile populations from the DRC.
The team assigned binary scores to each element within the 11 components of the checklist: 1 represented complete and 0 represented incomplete. The team then computed the percentage of completed elements for each component. The team aggregated by district the percentage complete for all components to gauge overall EVD preparedness.
Tool 2: CDC Border Health Capacity Discussion Guide
At the same locations where the team completed the checklist, they also implemented the CDC Border Health Capacity Discussion Guide.8 The guide is designed to facilitate qualitative information gathering with national, district, and point-of-entry stakeholders on relevant International Health Regulations (IHR 2005) capacities for public health preparedness and response at ground crossings. Specifically, it focuses on evaluating border characteristics, availability of medical and public health services, response plans and training, surveillance systems, communication systems, social mobilization, and national and regional data sharing. This tool was used to collect data that identified strengths and areas for improvement in public health aspects of border health systems (eg, public health preparedness plans, standard operating procedures for notification to appropriate surveillance personnel, and memoranda of understanding with cross-border counterparts). The guide was adapted by selecting a limited number of point-of-entry-level questions that complemented the WHO EVD checklist questions. The team combined the qualitative results from implementing the adapted guide with the quantitative results from the checklist to create a deeper assessment of district-level EVD preparedness. The guide entailed questions about the number of ground crossings in the areas visited, daily load of travelers crossing, existing documentation, reporting and communication procedures, public health services such as health facilities, transportation, and equipment and health staffing capacity available to detect, respond, and control diseases of public health concern. Questions were directed to key informants, such as district security personnel and disease surveillance focal people, and group discussions were held with district and village health teams, community leaders, and transport operatives.
Before using the guide, the team adapted it by selecting a limited number of district-level and point-of-entry-level questions to complement rather than duplicate checklist questions. The team combined the qualitative results from implementing the adapted Guide with the quantitative results from the checklist to create a deeper assessment of district-level EVD preparedness.
Tool 3: CDC Population Connectivity Across Borders (PopCAB)
On August 6, 2018, the team initiated risk mapping using the CDC PopCAB tool kit to identify geographic areas and specific locations with increased community connectivity to the DRC through community-level qualitative data collection with participatory mapping.8 Initially, the team facilitated key informant interviews with district leaders knowledgeable about cross-border population movement, including district health officers, township chairpersons, town clerks, sub-county chiefs, mayors, and transport operators. Through these interviews, the team developed an understanding of routes and destinations preferred by travelers and migrants from eastern DRC or by Ugandans who travel to the DRC and back.
Subsequently, the team facilitated focus group discussions with a range of stakeholders knowledgeable about areas and pathways identified during the key informant interviews. The focus group discussion participants, including community health volunteers, point-of-entry officials, health facility officials, taxi drivers, fishermen, and market vendors, characterized the people who come to their community, from where, for what purpose, how long they stay, and where they go when they depart. The PopCAB facilitators annotated details about locations and routes on the printed maps used for the participatory mapping element. The team tracked the multisectoral PopCAB activities through a mobile phone–based survey to ensure all district rapid response teams and the national task force were aware of progress. Through September 30, 2018, the team implemented 30 PopCAB events in 7 of the 12 priority category 1 districts (Figure 2).
Figure 2.
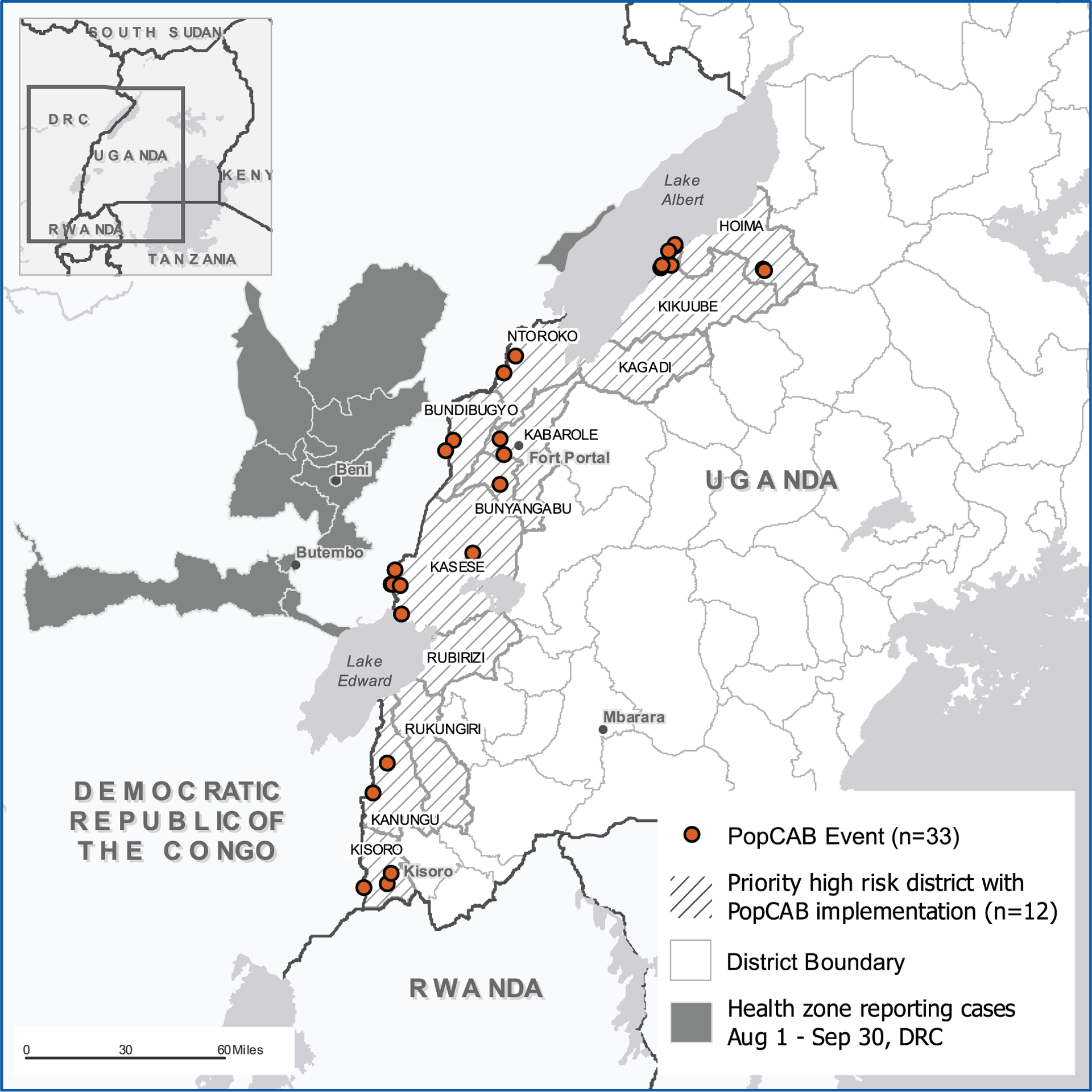
Map of locations in Uganda where population connectivity across borders activities were implemented between August 6 and September 30, 2018, as part of an Ebola virus disease risk assessment and mapping exercise. Color images are available online.
At each event, the border health team and district task force teams used PopCAB results to prioritize assessment and guide preparedness activities for the subsequent day. More specifically, the team consolidated the PopCAB results each evening after field work to help identify priority geographic areas and sites where public health preparedness measures should be strengthened, based on a forecast of where EVD importation could occur. Additionally, they generated qualitative and spatial databases to analyze and visualize the results.
Results
Ebola Virus Disease Preparedness
Overall, the 12 priority category 1 districts were most prepared in the laboratory, surveillance, and infection prevention and control areas (Table 1). The districts were, on average, least prepared in budgeting capacities. However, there was a lot of variation between districts. Only 2 districts had an average score across all 11 WHO preparedness activities above 50%. All other districts had at least 1 element with a 0% score. The lowest scores were in the domains of budgeting, safe burial, contact tracing, case management, and rapid response teams.
Table 1.
Ebola virus disease (EVD) preparedness score by WHO EVD Preparedness Checklist key component in each of 12 priority category 1 high-risk districts in Uganda, August 4 to September 30, 2018
| Key Component (number of included elements) |
Districts | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Average Scores | |
| Coordination (9) | 78a | 100 | 22 | 25 | 25 | 0 | 25 | 0 | 0 | 0 | 56 | 11 | 31 |
| Epidemiologic surveillance (8) | 57 | 63 | 50 | 40 | 20 | 80 | 20 | 0 | 13 | 13 | 63 | 38 | 42 |
| Rapid response team (6) | 83 | 83 | 17 | 0 | 0 | 33 | 33 | 0 | 0 | 0 | 0 | 17 | 24 |
| Case management (a) Clinical care (6) | 54 | 71 | 0 | 25 | 0 | 25 | 25 | 25 | 0 | 15 | 0 | 0 | 22 |
| Case management (b) Safe and dignified burials (5) | 40 | 60 | 0 | 0 | 50 | 50 | 0 | 0 | 0 | 0 | 0 | 0 | 18 |
| Contact tracing (5) | 60 | 100 | 0 | 0 | 0 | 33 | 33 | 0 | 0 | 0 | 0 | 0 | 21 |
| Public awareness and community engagement (4) | 58 | 100 | 0 | 50 | 0 | 25 | 25 | 0 | 0 | 17 | 50 | 38 | 33 |
| Infection prevention and control (4) | 42 | 100 | 25 | 33 | 33 | 33 | 67 | 33 | 0 | 25 | 0 | 0 | 36 |
| Laboratory (4) | 38 | 100 | 25 | 50 | 25 | 75 | 25 | 0 | 50 | 0 | 50 | 75 | 47 |
| Travel/points of entry (7) | 29 | 100 | 57 | 0 | 0 | 20 | 0 | 0 | 14 | 14 | 14 | 57 | 28 |
| Budget (6) | 50 | 67 | 0 | 0 | 0 | 25 | 25 | 0 | 0 | 0 | 0 | 0 | 15 |
| Logistics (12) | 67 | 82 | 33 | 11 | 11 | 33 | 33 | 11 | 17 | 0 | 17 | 33 | 32 |
| Average scores | 55 | 86 | 19 | 20 | 14 | 36 | 26 | 6 | 8 | 7 | 21 | 22 | 29 |
Numbers reflect percentage of completed elements for each key component.
The CDC Border Health Capacity Discussion Guide results identified key deficiencies at points-of-entry, including irregular movements with no space to screen all travelers; inadequate screening and isolation capacity, with irregular staff attendance and lack of equipment to screen travelers; lack of referral systems to safely transfer ill travelers to the referral facilities; inadequate infection control and prevention capacity, such as water supply; limited surveillance capacity with no lists of priority diseases and real-time reporting platforms; insufficient staff training in response to public health emergencies at border posts, such as EVD screening procedures, EVD detection, and response in a case of a suspected EVD case. Not all points of entry had specific contingency plans to take care of the abovementioned key issues to improve border health.
Risk Mapping
Between August 6 and September 30, 2018, the team used PopCAB to map 13 official and 27 unofficial ground crossings on the DRC-Uganda border, 153 health facilities, and many more townships, markets, residences, schools, places of worship, and workplaces, as well as traditional healers, with disproportionately high community connectivity to the DRC. The team also mapped out travel routes, including typical stopping points associated with movement by land, air, and water between Uganda and the DRC. Additionally, the team identified where DRC refugees often cross into Uganda to travel to reception and transit centers before they are transported to Kyangwali, Kyaka II, and other refugee settlements. The team and district task force teams used these results, in combination with checklist and guide results, to reprioritize healthcare facilities and points of entry for subsequent preparedness assessments. These identified locations were often in the district where the team was completing assessments but were also found in other high-risk districts.
Initial EVD Preparedness Initiatives
Guided by the preparedness assessments and risk mapping results, the national task force developed a national EVD contingency plan to prioritize geographic areas for capacity building and to address the gaps in preparedness to detect, respond to, and rapidly contain any potential EVD cases in Uganda. The major activities in the national EVD contingency plan included training and capacity building, point-of-entry public health screening, logistical support, public health awareness and community engagement, and EVD vaccination.
Training and Capacity Building
After development of the National EVD Contingency plan, the ministry of health mobilized several partners to develop the national 4W matrix guided by the WHO health cluster. The matrix highlighted partner support activities and human resource and financial contributions to EVD preparedness for the 11 core capacities, specifying which partner is doing what, where, and when.
The estimated total budget to support both national and district-level activities was $18 million from more than 20 international organizations. The estimated budget to support epidemiology, surveillance, and infection prevention and control was $1 million, $200,000 of which was designated for training. The 5-day nonresidential workshop training sessions included the following:
A Training of trainers (ToT) for Community Event–Based Disease Surveillance (CEBDS) held in the 12 districts.
Training of laboratory personnel from each of the 30 high-risk districts on EVD sample management
Integrated Disease Surveillance and Response (IDSR) roll out in high-risk districts
Training of Ministry of Health Officers on International Public Health Emergency, Epidemiology and International Health Regulations
Using existing WHO EVD training materials, the national rapid response team held onsite EVD orientation training for more than 9,000 healthcare workers from 82 health facilities in the 12 priority category 1 districts. Orientation focused on EVD case definitions; community event–based surveillance strategies; biologic sample collection, packaging, and transportation procedures; EVD screening at points of entry; infection prevention and control strategies; case management; contact tracing; and psychosocial support. More than 4,000 community health workers and 6,000 community leaders, including 1,463 subcounty councillors, 330 religious leaders, 256 traditional healers, and 2,693 village councillors, were trained in community-based disease surveillance. Copies of case investigation forms and contact tracing guidelines were distributed to the trained teams. The training sessions included exercises on infection prevention and control, including donning and doffing of personal protective equipment for EVD case management and safe burial. Additionally, 5 major hospitals in the 12 priority districts formed rapid response, surveillance, case management, risk communication, and burial teams.
Point-of-Entry Public Health Screening
The national rapid response team point-of-entry subcommittee worked with many partners, including the Infectious Diseases Institute of Makerere University, WHO, and CDC, to develop Ebola screening standard operating procedures and job aids for identification, referral, and management of ill individuals at point of entry. They disseminated the materials to Entebbe International Airport and to ground crossings identified through guide implementation and risk mapping. Additional training and mentorship were provided for 102 screeners at 13 points of entry, including health and non-health personnel and volunteers on the Ebola screening standard operating procedures and job aids. The screeners learned infection prevention and control measures, such as correct use of personal protective equipment and preparation of chlorine solution for hand washing. Additionally, screeners began using noncontact infrared thermometers to identify travelers with high temperatures (≥38°C).
Between August 10 and the end of September, after establishing public health screening for travelers entering Uganda through formal points of entry, point-of-entry staff and volunteers screened more than 5 million people crossing into Uganda from the DRC. The screeners identified 102 travelers with fever or other signs or symptoms compatible with EVD and used the newly developed standard operating procedures to manage and refer those travelers. None of the 102 symptomatic travelers was diagnosed with EVD.
Logistical Support
The national task force enhanced laboratory testing capacity by providing 500 EVD rapid diagnostic test kits and more than 150 triple-layered packaging kits to 5 hospital laboratories in western Uganda. The national task force supported district rapid response teams to set up isolation rooms, construct Ebola treatment units, and prepare burial grounds at the same 5 major hospitals. The national rapid response team provided printed standard operating procedures for detecting signs or symptoms compatible with EVD, personal protective equipment, and other infection prevention and control supplies to the 5 hospitals and more than 60 other health facilities.
The national task force procured 160 infrared, handheld, noncontact thermometers for fever screening in various parts of the country and thermal scanners for the Mpondwe ground crossing in Kasese District and the Entebbe International Airport. The national task force provided to the hospitals with an Ebola treatment unit a total of 6 ambulances for patient transportation and 8 standby vehicles and 10 motorcycles for quick specimen transfer to the Uganda Virus Research Institute reference laboratory in Entebbe.
In addition, the national rapid response team trained 19 laboratory technicians at Uganda Virus Research Institute and the Central Public Health Laboratory to increase EVD sample testing capacity. Stemming from these collective efforts, more than 400 samples were transported to Uganda Virus Research Institute for quick laboratory diagnosis in August, up from an average of 10 to 20 samples per month before the outbreak was declared in the DRC. This increased laboratory capacity helped reduce the length of isolation and hospital stay for patients with suspected EVD who tested negative for the virus.
Public Awareness and Community Engagement
Recognizing the variety of languages spoken in all 30 category 1 and 2 districts, EVD messages and information, education, and communication materials were translated into 15 predominant languages to reach more than 2.3 million people. District task forces distributed the messages in the 12 priority districts. To ensure widespread distribution, the materials were disseminated regularly in the communities through local newspapers, radio, television, and posters. In addition, the district task force teams disseminated messages through regular radio talk shows and spot messages on more than 20 local and international radio stations. The district task force teams trained community volunteers to share the information through communal and door-to-door EVD health education in the places with most connectivity to the DRC.
EVD Vaccination
After the national task force received ethics and institutional approval for vaccine delivery,, the ministry of health, with support from WHO, secured 5,537 rVSV-ZEBOV vaccine doses for prophylactic use to protect frontline health and non-health workers. The ministry of health used results from the PopCAB risk mapping to help prioritize more than 150 health facilities and 15 points of entry during the initial EVD vaccination campaign implemented in November 2018.
Discussion
After the declaration of the tenth EVD outbreak in the DRC on August 1, 2018, the Uganda Ministry of Hhealth activated plans and strategies for EVD preparedness and response. With technical assistance from WHO and CDC, Uganda organized a quick, proactive assessment and risk mapping initiative in 12 priority category 1 districts bordering the DRC’s North Kivu and Ituri provinces to guide development of a national contingency plan to detect and respond to EVD cases. The efforts in Western Uganda served as an opportunity to reveal gaps in the country’s readiness to detect and respond to an EVD case eventuality. In 2014, the Netherlands’ robust infrastructure for planning and infection prevention in health systems enhanced the response to the Ebola outbreak through collaboration and coordination.9,10 The ministry of health has established a strong national coordination mechanism through the public health emergency operations center by taking the lead in strategic management of information and resources for EVD preparedness and response. National coordination between various public sectors and regions is necessary to strengthen preparedness for emerging infectious diseases.
During this EVD outbreak in DRC, there is a significant risk of the disease spreading to neighboring countries. WHO recommended that all neighboring countries, with an emphasis on those with a border near the outbreak center, implement public health measures to respond to suspected and confirmed EVD cases.7 An article about the evolution of EVD outbreaks highlights that “knowledge about the past outbreaks can generate crucial information which may be useful for future prevention.”11 It states that “leveraging on eexisting expertise of health systems is essential when faced with emerging infectious diseases.” In Malaysia, experience in past outbreak control enabled the ministry of health to quickly establish preparedness and response plans to abate an Ebola outbreak.12 This is supported by evidence from the 2001 Gulu District and 2007 Bundibugyo District EVD outbreaks, whose substantial experience seemed to have enhanced operational readiness for and response to EVD. Building on this experience, the ministry of health rapidly activated the public health emergency operations center and an EVD national task force that initiated a national incident management system. The national task force employed a multifaceted approach in developing an action plan that responded to existing preparedness and response capacity to the risk of EVD importation.
Most category 1 districts were less than 50% prepared for EVD detection and response based on WHO’s recommended status of 11 core capacities. These findings are similar to WHO assessments completed across countries at high EVD risk neighboring the DRC during the ninth EVD outbreak and results from the 2015 EVD preparedness assessment for West African countries.9 Two districts stood out with preparedness scores greater than 50%, perhaps because they host those refugee settlements that, with the support of the United Nations High Commissioner for Refugees, the International Organization for Migration, and Medical Teams International, have active EVD screening and enhanced surveillance. Of note, Kampala district, which includes the capital city, and Wakiso district, the largest hub for business and travelers, were not among the 12 priority districts because they lack a land border with the DRC.
Results from the checklist, the CDC border health capacity guide, and the PoPCAB guided the ministry of health in developing the national and district rapid response plans. The ministry of health tailored EVD training modules for healthcare staff and point-of-entry officials based on the stakeholder groups that visited specific locations. Community health volunteers from these locations were also selected to undergo community-based surveillance training to increase awareness areas with high cross-border connectivity.
The ministry of health also established training schedules for multisectoral staff and increased access to training materials in various languages. The assessment and mapping results further guided planning, resource mobilization, and allocation for early strengthening of EVD preparedness in priority areas. Similar methods have been used to address priority public health events in other African countries. For instance, in the 2014 West African EVD outbreak, preparedness activities—including training, developing guidelines, assessing Ebola preparedness, and facilitating emergency operations center establishment in 7 West African countries—improved the capacity to rapidly detect and contain imported EVD cases.13 The EVD preparedness assessment and risk mapping enabled identification of the strengths and weaknesses of the health system as specified at the national and district levels. The ministry of health national task force used the gaps identified in EVD preparedness core capacities to develop the contingency plan and resource mobilization for national EVD preparedness. The DRC population movement patterns and hot community activity spots identified in the risk mapping exercise generated the focus for community engagement and risk communication activities. Without these specifications, efforts for EVD preparedness would have been mistargeted and most likely missed the priority locations such as the unofficial points of entry for DRC land population crossings. This would probably have been major entries for importation of EVD cases from the DRC.
One limitation of the assessments and risk mapping was the reliance on respondent or participant opinion, experience, or knowledge, which may not be representative of a wider population. The team tried to address this consideration by inviting a range of stakeholders and leaders at various levels to participate in the data collection activities. This multisectoral approach may also have contributed to reduced personal bias in subsequent district task force team discussions about which locations or capacities to prioritize for interventions. However, the use of a multi-pronged approach to EVD preparedness with the 3 tools mentioned directed efforts to support capacity, equipment, and risk communication at national, district, and community levels. These efforts elicited support from several international organizations. Similar efforts could be adapted for other health events of international concern to prevent and prepare emergency response for diseases and disasters of international concern.
Conclusions
Through the multi-pronged approach of border health preparedness assessments and risk mapping, the Uganda Ministry of Health developed EVD preparedness strategies tailored to address its unique multisectoral public health system and complex community connections with the DRC. The results from the assessments helped to streamline response efforts and target resource allocation to newly identified capacity gaps. These methods can be adapted to address other priority public health events in Uganda and similar areas to better integrate border health considerations in preparedness and response initiatives, especially where complex cross-border and community connectivity thrives. We recommend that ministries of health reassess their country’s preparedness using the checklist and adapted guides to evaluate the national and district preparedness capacity to respond to EVD.
Acknowledgments
The data sets and the reports that supported this write-up belong to the Uganda Ministry of Health. For confidentiality reasons, the data sets and reports are not publicly available. However, the data sets and the reports can be provided upon reasonable request with permission from the Uganda Ministry of Health. The described EVD preparedness assessment and risk mapping activities were supported by the Uganda Ministry of Health, WHO, and the President’s Emergency Plan for AIDS Relief (PEPFAR) through US CDC Cooperative Agreement number GH001353–01 through Makerere University School of Public Health to the Uganda Public Health Fellowship Program, Ministry of Health, and several partner agencies. The findings and conclusions of this report are those of the authors and do not represent the official position of the CDC, the Uganda Ministry of Health, or participating partner agencies.
We would like to acknowledge the efforts of the Uganda Ministry of Health and national task force, which planned, coordinated, and implemented preparedness activities. We thank all international agencies and development and implementing partners that supported the EVD preparedness exercise: WHO, UNICEF, UNDP, UNHCR, WFP, IOM, FAO, US CDC, China CDC, Africa CDC, KOICA, JICA, UK Aid, USAID, Samaritan’s Purse, DFID, URCS, AFENET, MSF, MUWRP, JMEDDIC, UVRI, ECHO, IDI, WFP, World Vision, Save the Children, and RESOLVE. We would like to thank the district local governments of the high-risk districts for their collaboration, which enabled this exercise to be a success. We wish to thank Elvira McIntyre for creating figures for this article and Dr Bao-Ping Zhu for technical guidance in data collection and input into this manuscript.
References
- 1.Malvy D, McElroy AK, de Clerck H, Günther S, van Griensven J. Ebola virus disease. Lancet 2019;393(10174):936–948. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Ebola virus disease distribution map: cases of Ebola virus disease in Africa since 1976. Reviewed June 19, 2019. https://www.cdc.gov/vhf/ebola/history/distribution-map.html. Accessed March 10, 2020.
- 3.World Health Organization. Cluster of presumptive Ebola cases in North Kivu in the Democratic Republic of the Congo [news release]. August 1, 2018. https://www.who.int/news-room/detail/01-08-2018-cluster-of-presumptive-ebola-cases-in-north-kivu-in-the-democratic-republic-of-the-congo. Accessed March 10, 2020.
- 4.UNICEF. Regional Ebola Preparedness: Overview of Needs and Requirements. July-December 2019. https://www.who.int/ebola/preparedness/regional-ebola-preparedness-overview-june-dec2019.pdf. Accessed March 10, 2020.
- 5.International Federation of Red Cross and Red Crescent Societies. Uganda: Ebola preparedness emergency plan of action (EPoA) - DREF Operation n° MDRUG041 update n° 02. December 24, 2018. https://reliefweb.int/report/uganda/uganda-ebola-preparedness-emergency-plan-action-epoa-dref-operation-n-mdrug041-0. Accessed March 10, 2020.
- 6.World Health Organization. Consolidated Ebola virus disease preparedness checklist. January 2015. https://www.who.int/csr/resources/publications/ebola/ebola-preparedness-checklist/en/. Accessed March 10, 2020.
- 7.World Health Organization. WHO regional strategic plan for EVD operational readiness and preparedness in countries neighboring the Democratic Republic of the Congo. June 2018-Febraury 2019. https://www.who.int/csr/resources/publications/ebola/preparedness/WHO-regional-strategic-EVD-operational-readiness.pdf?ua=1. Accessed March 10, 2020.
- 8.Merrill RD, Rogers K, Ward S, et al. Responding to communicable diseases in internationally mobile populations at points of entry and along porous borders, Nigeria, Benin, and Togo. Emerg Infect Dis 2017;23(Suppl 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leonhardt KK, Keuler M, Safdar N, Hunter P. Ebola preparedness planning and collaboration by two health systems in Wisconsin, September to December 2014. Disaster Med Public Health Prep 2016;10(4):691–697. [DOI] [PubMed] [Google Scholar]
- 10.Swaan CM,Öry AV, Schol LGC, Jacobi A, Richardus JH, Timen A. Ebola preparedness in the Netherlands: the need for coordination between the public health and the curative sector. J Public Health Manag Pract 2018;24(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gałas A. The evolution of Ebola virus disease outbreaks. Folia Med Cracov 2014;54(3):27–32. [PubMed] [Google Scholar]
- 12.Wan Mohamed Noor WN, Sandhu SS, Ahmad Mahir HM, et al. Responding to the potential of Ebola virus disease (EVD) importation into Malaysia. Malays J Med Sci 2014; 21(6):3–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Breakwell L, Gerber AR, Greiner AL, et al. Early identification and prevention of the spread of Ebola in high-risk African countries. MMWR Suppl 2016;65(3):21–27. [DOI] [PubMed] [Google Scholar]


