Abstract
Background
Kasai procedure and liver transplantation are effective ways to save the life of children with biliary atresia (BA). However, with the gradual development of liver transplantation technology, scholars have questioned the necessity of the Kasai procedure. Therefore, we conducted a meta-analysis to evaluate the effect of previous Kasai procedures on liver transplantation in children with BA.
Methods
Seven databases were searched and screened from the establishment of the database to May 3, 2023. The data in the included literature were extracted for meta-analysis to compare the differences between the Kasai group and the non-Kasai group. Finally, a publication bias test, sensitivity analysis, subgroup analysis, and systematic review were performed.
Results
A total of 26 studies were included in which 6,522 children with BA underwent liver transplantation, including 4,989 in the Kasai group. Compared with the non-Kasai group, the Kasai group had older age [standardized mean difference (SMD) =0.64; 95% confidence interval (CI): 0.46, 0.82; P<0.001] (I2=78.6%), heavier weight (SMD =0.41; 95% CI: 0.33, 0.48; P<0.001) (after sensitivity analysis, I2=0.0%), lower pediatric end-stage liver disease (PELD) (SMD =−0.41; 95% CI: −0.48, −0.35; P<0.001) (I2=20.1%), longer operation time (SMD =0.33; 95% CI: 0.01, 0.65; P<0.001) (I2=83.2%), more intraoperative blood loss (SMD =0.26; 95% CI: 0.06, 0.46; P=0.012) (I2=19.1%), shorter intensive care unit (ICU) stay (SMD =−0.09; 95% CI: −0.34, 0.15; P=0.027) (I2=68.6%) and higher incidence of intestinal perforation [odds ratio (OR) =1.96; 95% CI: 1.20, 3.18; P=0.007] (I2=7.4%) and biliary complications (OR =1.41; 95% CI: 1.05, 1.89; P=0.024) (I2=31.4%). In the “Asia” subgroup, the Kasai group was older (SMD =0.68; 95% CI: 0.52, 0.84; P<0.001) (I2=28.2%). In the “Cases since 2000” subgroup, there was no significant difference in operation time between the two groups (I2=28.5%). In the “Other” and the “non-Asia” subgroup, there was no significant difference in length of intensive care unit (ICU) stay between the two groups (I2=0.0%). However, there were no significant differences in other postoperative complications and prognostic indicators between the two groups.
Conclusions
For children with BA undergoing liver transplantation, although previous Kasai procedure may increase the risk of intraoperative bleeding, biliary complications, and intestinal perforation, it does not affect the main clinical outcomes, and can even delay the timing of liver transplantation and improve the preoperative status of children. Therefore, when BA children have no obvious contraindications to Kasai procedure, the sequential treatment of Kasai procedure-liver transplantation should be supported first.
Keywords: Biliary atresia (BA), Kasai procedure, liver transplantation, meta-analysis, review
Highlight box.
Key findings
• For liver transplantation in children with biliary atresia (BA), the previous Kasai procedure may increase the risk of intraoperative bleeding, biliary complications, and intestinal perforation, but it does not affect the main clinical outcomes.
• Previous Kasai procedure can delay the timing of liver transplantation and improve the preoperative condition of patients.
What is known and what is new?
• Previous Kasai procedure did not influence the primary outcome of liver transplantation.
• Compared with previous studies, we included more studies (n=26), collected more comprehensive data, used more appropriate analysis methods, and reached slightly different conclusions.
What is the implication, and what should change now?
• It is recommended that the sequential treatment of the Kasai procedure-liver transplantation is the first choice for BA children in the absence of contraindications to the Kasai procedure, and the Kasai procedure should be standardized.
Introduction
Biliary atresia (BA) is a progressive, inflammatory, and fibrosclerosing disease of the bile ducts. It occurs predominantly during the neonatal period, and surgical treatment is the only effective way to save lives. Without treatment, most patients will die in the first two years of life (1). The current surgical methods include Kasai procedure and liver transplantation. According to various countries, the 5-year survival rate of the native liver after the Kasai procedure in children with BA is about 50% (2-4). Intestinal adhesions caused by previous Kasai procedures are a major concern for surgeons during liver resection in recipients (5). With the development of pediatric liver transplantation, the efficacy of BA liver transplantation has been significantly improved, and scholars have begun to rethink the role of Kasai procedure in the treatment of BA. However, liver transplantation is also not perfect, and long-term use of immunosuppressive drugs after liver transplantation may increase the risk of infection and malignant tumors. Therefore, we systematically reviewed the literature and performed a meta-analysis to evaluate the effect of previous Kasai procedure on liver transplantation in children with BA. This may contribute to the selection of clinical treatment options and the resolution of academic controversies on this issue. The researchers followed the PRISMA reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-504/rc) (6).
Methods
The study followed a protocol registered with the international review registration platform PROSPERO (International Prospective Register of Systematic Reviews) with PROSPERO ID: CRD42023423232.
Search strategy
PubMed, Embase, Web of Science, Cochrane, China National Knowledge Infrastructure (CNKI), China Biology Medicine (CBM), and Wanfang Database were searched from the establishment of the database to May 3, 2023. The MeSH keywords were “Biliary Atresia”, “Portoenterostomy, Hepatic” and “Liver Transplantation”, and the corresponding free words were searched. We used the Boolean operator “OR” to connect the subject words with the free words to extend the search criteria, and then the individual subject words were connected through the Boolean operator “AND” to exact the search range. The search strategy for the seven databases is available at https://cdn.amegroups.cn/static/public/TP-23-504-1.docx. There were no restrictions on the language and publication status of the papers.
Literature searches
The inclusion and exclusion criteria were prespecified according to PRISMA, and the PICOS approach was used to define study eligibility. Studies selected in our meta-analysis must meet all the following inclusion criteria: Inclusion criteria: (I) clinical studies involving BA patients undergoing liver transplantation. (II) Patients with or without previous Kasai procedure were included. (III) Any one of these indicators was reported: age at surgery, weight at surgery, pediatric end-stage liver disease (PELD) score, operation time, intraoperative blood loss, intraoperative blood transfusion, length of hospital stay, length of intensive care unit (ICU) stay, infection, reoperation, retransplantation, hepatic artery complications, portal vein complications, hepatic vein complications, biliary complications, rejection, intestinal perforation, intestinal obstruction, bleeding, lymphatic fistula, survival of patients and grafts or other data available from the article. (IV) If there were studies with duplicate cases from the same center, the studies with larger number of cases, more recent publications, and complete data were preferentially included. Meanwhile, the criteria used to exclude studies were as follows: (I) lack of necessary information or obvious errors in the data. (II) Case reports, expert consensus, conference abstracts with no valid information, clinical trials, comments, questions and reflections, guidelines, reviews, letters, meta and systematic reviews, and proposals. (III) No comparisons were made between Kasai and non-Kasai groups. (IV) Non-BA or combined with other related diseases. (V) Non-human studies. (VI) Repeated data.
Study selection and definitions
All authors independently removed duplicate entries from the seven databases. Subsequently, each author independently screened the titles and abstracts of the retrieved results for relevance. Finally, the full text of the remaining results was assessed separately by two authors according to prespecified criteria, with discrepancies resolved by a third author. The final list of included articles was determined by careful discussion among the authors.
Data extraction
According to the inclusion criteria, all data were recorded independently by three authors, and discrepancies were resolved by discussion with the research team (raw data are available at https://cdn.amegroups.cn/static/public/TP-23-504-1.docx). A self-designed extraction table was used to extract the following information from the included literature:
Literature characteristics (first author’s name, publication year, country).
Baseline data of previous Kasai group and non-Kasai group (number, gender, liver source, study type, follow-up time).
Preoperative indicators of the two groups (age at surgery, weight at surgery, PELD score).
Perioperative data of the two groups (operation time, intraoperative blood loss, intraoperative blood transfusion, length of hospital stay, length of ICU stay).
Postoperative indicators of the two groups (infection, reoperation, retransplantation, hepatic artery complications, hepatic vein complications, portal vein complications, biliary complications, rejection, lymphatic fistula, bleeding, intestinal perforation, intestinal obstruction).
Survival data of patients and grafts in the two groups.
Validity assessment
The quality of the included studies was independently evaluated by two authors using the Newcastle-Ottawa Quality Assessment Scale. The checklist covered essential items on the quality of the included studies, including (I) patient selection. (II) Comparability of study groups. (III) Outcome assessment. Each item was assigned a score of one for meeting the criteria, and zero for not meeting the criteria or being unclear whether the criteria were met. Then a total score was calculated for each study, a score greater than five indicated a high-quality study. Discrepancies needed to be resolved by the third author.
Statistical analysis
Statistical analyses were performed with Review Manager 5.4 (Cochrane Collaboration, Oxford, UK) and STATA 16.0 (StataCorp LP, College Station, TX, USA). An odds ratio (OR) with a 95% confidence interval (CI) was used to compare binary variables. The standardized mean difference (SMD) and 95% CI were calculated for continuous outcomes. For all meta-analyses, the Cochrane Q P value and I2 statistic were applied to check heterogeneity. When P<0.05 or I2>50%, there was a significant heterogeneity, a random-effect model was used to merge the results. Otherwise, a fixed-effect model was used. P<0.05 was considered statistically significant. Egger’s test and funnel plot were used to assess publication bias, and P<0.05 was considered as the existence of publication bias. Sensitivity analysis (“leave-one-out” method) and subgroup analysis were used to find the sources of heterogeneity. The method of combining the mean and standard deviation of two or more groups of data can be referred to the study of Higgins et al. (7). In contrast, the method of transforming the interquartile range into the mean and standard deviation can be referred to the study of Shi et al. (8) and Wan et al. (9).
Results
Search process
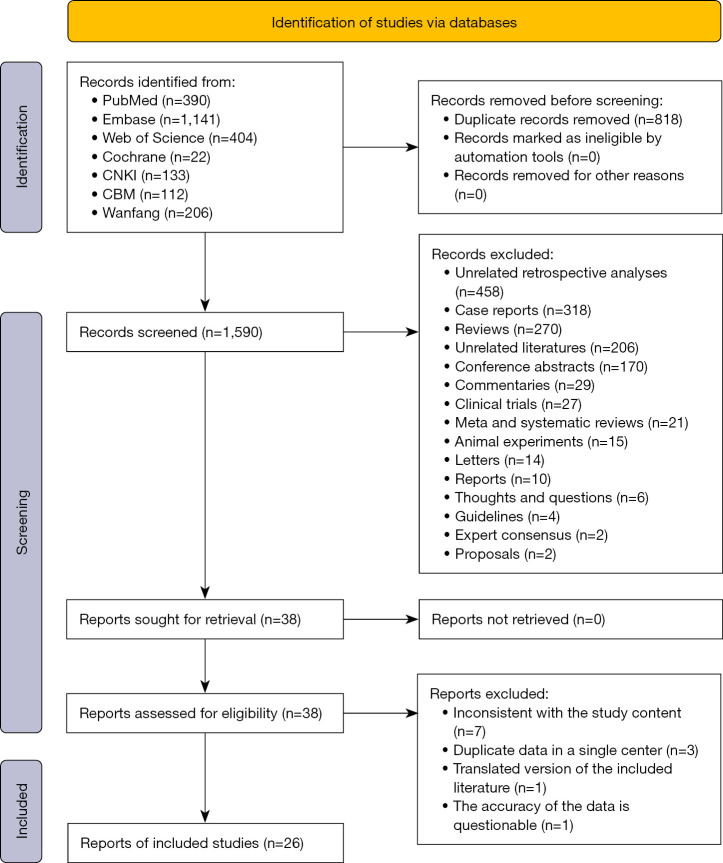
The literature screening flow chart is shown in Figure 1. Firstly, the first step identified 2,408 articles by database search, of which 818 duplicate articles existed. In the second step, we removed 1,552 articles based on reading the title and abstract of the articles, leaving only 38 articles. In the third step, we conducted a close reading of the full text of 38 articles and removed 12 of them. In the fourth step, the remaining 26 studies were included, and subsequent data extraction and meta-analysis were performed. Among 26 studies, five studies (10-14) were published before 2000, and 21 studies (15-35) were published after 2000.
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases only. CNKI, China National Knowledge Infrastructure; CBM, China Biology Medicine.
Quality assessment of studies included in the meta-analysis
The quality of the 26 included studies was evaluated based on the Newcastle-Ottawa quality assessment scale (Table S1). Four studies had a score of nine, six studies had a score of eight, 12 studies had a score of seven, and four studies had a score of six.
Study baseline data
The 26 included studies were all retrospective studies, 22 studies were published in English and four studies were published in Chinese (Table 1). Among them, the study population included China (n=10), USA (n=8), Belgium (n=2), India (n=2), Canada (n=1), France (n=1), Turkey (n=1), Brazil (n=1). A total of 6,522 children with BA were included in the meta-analysis, and 4,989 of them had undergone the Kasai procedure. In the studies with gender information, boys accounted for 42.8% (1,988/4,643) and girls accounted for 57.2% (2,655/4,643). Among the studies with available liver source information, 64.8% (1,283/1,980) received living donor (LD) liver and 35.2% (697/1,980) received deceased donor (DD) liver. Table S2 provides data summary information on the indications for transplantation in children from each study.
Table 1. Baseline data from 26 studies.
| First author | Year | Country | Data coverage time | Kasai | N | Gender (male:female) | LT type (LD:DD)† | Follow-up (months) | Type of study |
|---|---|---|---|---|---|---|---|---|---|
| Millis (10) | 1988 | USA | 1984–1987 | Yes | 28 | – | 0:28 | – | Retrospective study |
| No | 8 | – | 0:8 | – | |||||
| Wood (11) | 1990 | USA | 1985–1989 | Yes | 46 | – | – | – | Retrospective study |
| No | 2 | – | – | – | |||||
| Meister (12) | 1993 | USA | 1988–1991 | Yes | 32 | – | 0:32 | – | Retrospective study |
| No | 7 | – | 0:7 | – | |||||
| Sandler (13) | 1997 | Canada | 1986–1996 | Yes | 49 | 24:25 | 0:49 | – | Retrospective study |
| No | 8 | 3:5 | 0:8 | – | |||||
| Chardot (14) | 1999 | France | 1986–1996 | Yes | 208 | – | – | – | Retrospective study |
| No | 17 | – | – | – | |||||
| Diem (15) | 2003 | Belgium | 1984–2000 | Yes | 285 | – | – | – | Retrospective study |
| No | 43 | – | – | – | |||||
| Visser (16) | 2004 | USA | 1988–2002 | Yes | 42 | – | 22:20 | – | Retrospective study |
| No | 13 | – | 7:6 | – | |||||
| Cowles (17) | 2008 | USA | 1998–2006 | Yes | 61 | – | – | 58.00 (6.00–111.00)‡ | Retrospective study |
| No | 10 | – | – | 58.00 (6.00–111.00)‡ | |||||
| Tiao (18) | 2008 | China | 1996–2004 | Yes | 60 | – | – | – | Retrospective study |
| No | 46 | – | – | – | |||||
| Guo (19) | 2010 | China | 2006–2009 | Yes | 9 | – | 9:0 | 18.50 (1.00–36.00)‡ | Retrospective study |
| No | 13 | – | 13:0 | 18.50 (1.00–36.00)‡ | |||||
| Alexopoulos (20) | 2012 | USA | 1995–2008 | Yes | 112 | – | – | – | Retrospective study |
| No | 22 | – | – | – | |||||
| Wang (21) | 2013 | China | 2008–2011 | Yes | 10 | 2:8 | 10:0 | 31.00 (12.00–44.50)‡ | Retrospective study |
| No | 18 | 10:8 | 18:0 | 31.00 (12.00–44.50)‡ | |||||
| Celik (22) | 2014 | Turkey | 2006–2013 | Yes | 28 | – | – | – | Retrospective study |
| No | 12 | – | – | – | |||||
| Neto (23) | 2015 | Brazil | 1995–2013 | Yes | 209 | 90:119 | 189:20 | – | Retrospective study |
| No | 138 | 51:87 | 120:18 | – | |||||
| Chung (24) | 2015 | China | 1993–2015 | Yes | 74 | – | – | – | Retrospective study |
| No | 7 | – | – | – | |||||
| Safwan (25) | 2016 | India | 2010–2015 | Yes | 33 | – | – | 18.00 (3.00–61.00)‡ | Retrospective study |
| No | 25 | – | – | 18.00 (3.00–61.00)‡ | |||||
| Mohan (26) | 2016 | India | 2004–2015 | Yes | 38 | 20:18 | – | 45.12§ | Retrospective study |
| No | 20 | – | – | 45.12§ | |||||
| Yang (27) | 2018 | China | 2014–2015 | Yes | 58 | 24:34 | 40:18 | – | Retrospective study |
| No | 45 | 24:21 | 34:11 | – | |||||
| Li (28) | 2019 | China | 2006–2014 | Yes | 89 | 53:36 | – | 19.70§ | Retrospective study |
| No | 61 | 38:23 | – | 14.60§ | |||||
| Chang (29) | 2021 | China | 2010–2016 | Yes | 38 | – | – | 36.00§ | Retrospective study |
| No | 36 | – | – | 36.00§ | |||||
| Tambucci (30) | 2021 | Belgium | 1993–2018 | Yes | 296 | – | – | – | Retrospective study |
| No | 97 | – | – | – | |||||
| Li (31) | 2022 | China | 2013–2020 | Yes | 51 | 31:20 | 14:37 | 22.00 (1.00–88.00)‡ | Retrospective study |
| No | 54 | 30:24 | 25:29 | 22.00 (1.00–88.00)‡ | |||||
| Zhang (32) | 2022 | China | 2014–2019 | Yes | 542 | 245:297 | 334:208 | 38.00 (26.90, 55.40)¶ | Retrospective study |
| No | 338 | 149:189 | 251:87 | 38.00 (26.90, 55.40)¶ | |||||
| Lemoine (33) | 2022 | USA | 1997–2020 | Yes | 97 | – | 39:58 | – | Retrospective study |
| No | 14 | – | 4:10 | – | |||||
| Yoeli (34) | 2022 | USA | 2002–2021 | Yes | 2,340 | 963:1,377 | – | 12.57±7.84†† | Retrospective study |
| No | 436 | 151:285 | – | 8.26±2.97†† | |||||
| Liu (35) | 2022 | China | 2017–2019 | Yes | 154 | 81:73 | 117:37 | – | Retrospective study |
| No | 43 | 19:24 | 37:6 | – |
†, LD:DD = living donor:deceased donor; ‡, median (minimum–maximum); §, median; ¶, median (P25, P75); ††, mean ± standard deviation.
Preoperative indicators
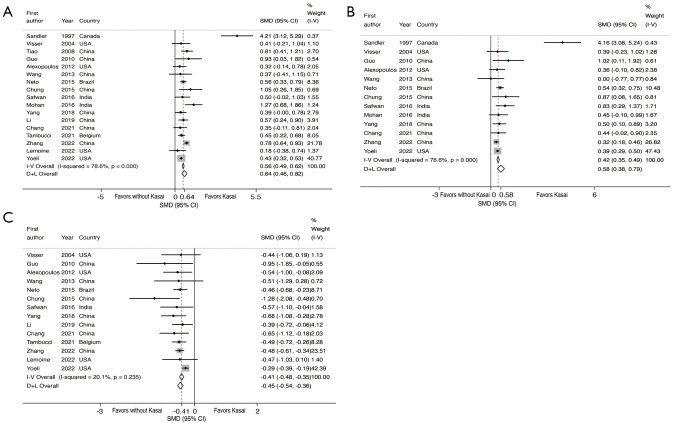
There was large heterogeneity in the age at surgery between the 17 studies (I2=78.6%, P<0.001), so the random effect model was used. The results of the meta-analysis showed that the age at surgery in the Kasai group was older, and the difference was statistically significant (SMD =0.64; 95% CI: 0.46, 0.82; P<0.001) (Figure 2A).
Figure 2.
Forest plot of the meta-analysis of preoperative indicators. (A) Age at surgery. (B) Weight at surgery. (C) PELD score. Fixed effects model: I-V overall, random effects model: D + L overall. SMD, standardized mean difference; CI, confidence interval; I-V, Inverse-Variance; D + L, DerSimonian and Laird; PELD, pediatric end-stage liver disease.
There was large heterogeneity in the weight at surgery between the 13 studies (I2=78.6%, P<0.001), so the random effect model was used. The results of the meta-analysis showed that the weight at surgery of the Kasai group was heavier. The difference was statistically significant (SMD =0.58; 95% CI: 0.38, 0.79; P<0.001) (Figure 2B).
There was no significant heterogeneity in the PELD score between the 14 studies (I2=20.1%, P=0.235), so the fixed effect model was used. The results of the meta-analysis showed that the PELD score of the Kasai group was lower, and the difference was statistically significant (SMD =−0.41; 95% CI: −0.48, −0.35; P<0.001) (Figure 2C).
Perioperative indicators
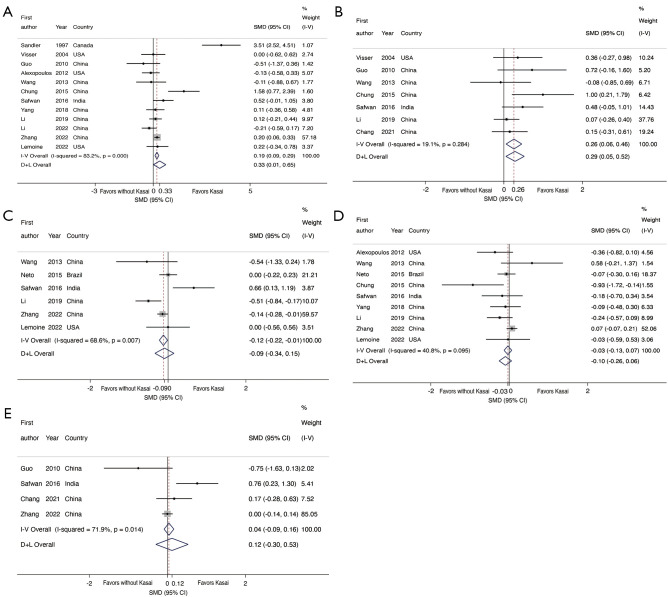
There was large heterogeneity in the operation time between the 12 studies (I2=83.2%, P<0.001), so the random effect model was used. The results of the meta-analysis showed that the operation time of the Kasai group was longer, and the difference was statistically significant (SMD =0.33; 95% CI: 0.01, 0.65; P<0.001) (Figure 3A).
Figure 3.
Forest plot of the meta-analysis of perioperative indicators. (A) Operation time. (B) Intraoperative blood loss. (C) Length of ICU stay. (D) Length of hospital stay. (E) Intraoperative blood transfusion. Fixed effects model: I-V overall, random effects model: D + L overall. SMD, standardized mean difference; CI, confidence interval; I-V, Inverse-Variance; D + L, DerSimonian and Laird; ICU, intensive care unit.
There was no significant heterogeneity in intraoperative blood loss between the seven studies (I2=19.1%, P=0.284), so the fixed effect model was used. The results of the meta-analysis showed that the Kasai group had more intraoperative blood loss, and the difference was statistically significant (SMD =0.26; 95% CI: 0.06, 0.46; P=0.012) (Figure 3B).
There was large heterogeneity in the length of ICU stay between the six studies (I2=68.6%, P=0.007), so the random effects model was used. The results of the meta-analysis showed that the length of ICU stay of the Kasai group was shorter. The difference was statistically significant (SMD =−0.09; 95% CI: −0.34, 0.15; P=0.027) (Figure 3C).
There was no significant heterogeneity in the length of hospital stay between the nine studies (I2=40.8%, P=0.095), so a fixed effect model was used. The results of the meta-analysis showed that there was no significant difference in the length of hospital stay between the two groups (SMD =−0.03, 95% CI: −0.13, 0.07; P=0.514) (Figure 3D).
There was large heterogeneity in the intraoperative blood transfusion between the four studies (I2=71.9%, P=0.014). The results of the meta-analysis showed that there was no significant difference in intraoperative blood transfusion between the two groups (SMD =0.12; 95% CI: −0.30, 0.53; P=0.536) (Figure 3E).
Postoperative indicators
The results of the meta-analysis showed that the incidence of intestinal perforation and biliary complications in the Kasai group was higher than that in the non-Kasai group, and the differences were statistically significant. However, there were no significant differences in postoperative infection, reoperation, retransplantation, hepatic artery complications, portal vein complications, hepatic vein complications, bleeding, intestinal obstruction, rejection, and lymphatic fistula between the two groups (Table 2, Figures S1,S2).
Table 2. The meta-analysis of postoperative indicators.
| Postoperative indicators | Number of studies | Test of heterogeneity | Model of effect | OR (95% CI) | P value | |
|---|---|---|---|---|---|---|
| I2 | P value | |||||
| Infection | 8 | 6.0% | 0.384 | Fixed | 1.63 (0.97, 2.74) | 0.066 |
| Reoperation | 11 | 20.4% | 0.255 | Fixed | 0.92 (0.66, 1.29) | 0.636 |
| Retransplantation | 8 | 0.0% | 0.522 | Fixed | 1.12 (0.53, 2.38) | 0.769 |
| Hepatic artery complications | 14 | 0.0% | 0.900 | Fixed | 0.92 (0.62, 1.36) | 0.659 |
| Hepatic vein complications | 3 | 0.0% | 0.571 | Fixed | 2.76 (0.67, 11.34) | 0.160 |
| Portal vein complications | 13 | 0.0% | 0.849 | Fixed | 1.27 (0.93, 1.73) | 0.130 |
| Biliary complications | 15 | 31.4% | 0.124 | Fixed | 1.41 (1.05, 1.89) | 0.024* |
| Rejection | 7 | 26.0% | 0.230 | Fixed | 1.22 (0.93, 1.58) | 0.146 |
| Lymphatic fistula | 3 | 11.6% | 0.323 | Fixed | 0.82 (0.63, 1.08) | 0.167 |
| Bleeding | 7 | 0.0% | 0.954 | Fixed | 1.36 (0.69, 2.68) | 0.376 |
| Intestinal perforation | 12 | 7.4% | 0.373 | Fixed | 1.96 (1.20, 3.18) | 0.007** |
| Intestinal obstruction | 5 | 0.0% | 0.441 | Fixed | 0.73 (0.45, 1.19) | 0.210 |
*, P<0.05; **, P<0.01. OR, odds ratio; CI, confidence interval.
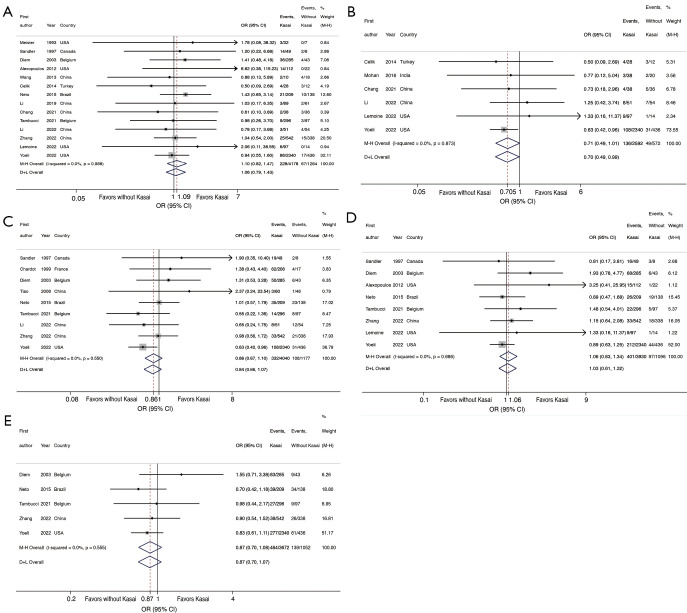
Patient survival rate
There was no significant heterogeneity in the 1-year survival between the 14 studies (I2=0.0%, P=0.988), so the fixed effect model was used. The results of the meta-analysis showed that the difference was not statistically significant (OR =1.10; 95% CI: 0.82, 1.47; P=0.546) (Figure 4A).
Figure 4.
Forest plot of the meta-analysis of survival information. (A) 1-year survival rate. (B) 3-year survival rate. (C) 5-year survival rate. (D) 1-year graft survival rate. (E) 5-year graft survival rate. Fixed effects model: M-H overall, random effects model: D + L overall. OR, odds ratio; CI, confidence interval; M-H, Mantel-Haenszel; D + L, DerSimonian and Laird.
There was no significant heterogeneity in the 3-year survival between the six studies (I2=0.0%, P=0.873), so the fixed effect model was used. The results of the meta-analysis showed that the difference was not statistically significant (OR =0.71; 95% CI: 0.49, 1.01; P=0.053) (Figure 4B).
There was no significant heterogeneity in the 5-year survival between the nine studies (I2=0.0%, P=0.550), so the fixed effect model was used. The results of the meta-analysis showed that the difference was not statistically significant (OR =0.86; 95% CI: 0.67, 1.10; P=0.219) (Figure 4C).
Graft survival rate
There was no significant heterogeneity in 1-year graft survival between the eight studies (I2=0.0%, P=0.686), so a fixed effect model was used. The results of the meta-analysis showed that there was no statistically significant difference (OR =1.06; 95% CI: 0.83, 1.34; P=0.660) (Figure 4D).
There was no significant heterogeneity in 5-year graft survival between the five studies (I2=0.0%, P=0.555), so the fixed effect model was used. The results of the meta-analysis showed that there was no statistically significant difference (OR =0.87; 95% CI: 0.70, 1.08; P=0.207) (Figure 4E).
Publication bias
To make the included studies more persuasive, we used the funnel plot and Egger’s test to detect publication bias. When the funnel plot is used to detect publication bias, the number of studies in the meta-analysis should be at least 10, and if the number of studies is too small, it is difficult to detect the cause of asymmetry (36). The results showed that the Egger’s test of PELD score was less than 0.05, indicating that there may be publication bias, and the reliability of its conclusions still needs to be confirmed by more studies (Table 3, Figure S3).
Table 3. Publication bias.
| Indicators | Number of studies | P value for Egger’s test |
|---|---|---|
| Preoperative indicators | ||
| Age at surgery | 17 | 0.215 |
| Weight at surgery | 13 | 0.125 |
| PELD score | 14 | 0.003** |
| Perioperative indicators | ||
| Operation time | 12 | 0.411 |
| Intraoperative blood loss | 7 | 0.114 |
| Intraoperative blood transfusion | 4 | 0.779 |
| Length of hospital stay | 9 | 0.162 |
| Length of ICU stay | 6 | 0.817 |
| Postoperative complications | ||
| Infection | 8 | 0.154 |
| Reoperation | 11 | 0.939 |
| Retransplantation | 8 | 0.686 |
| Hepatic artery complications | 14 | 0.353 |
| Hepatic vein complications | 3 | 0.659 |
| Portal vein complications | 13 | 0.434 |
| Biliary complications | 15 | 0.310 |
| Rejection | 7 | 0.650 |
| Lymphatic fistula | 3 | 0.449 |
| Bleeding | 7 | 0.083 |
| Intestinal perforation | 12 | 0.210 |
| Intestinal obstruction | 5 | 0.794 |
| Survival | ||
| 1-year survival rate | 14 | 0.509 |
| 3-year survival rate | 6 | 0.311 |
| 5-year survival rate | 9 | 0.091 |
| 1-year graft survival rate | 8 | 0.084 |
| 5-year graft survival rate | 5 | 0.297 |
**, P<0.01. PELD, pediatric end-stage liver disease; ICU, intensive care unit.
Sensitivity analysis
To determine the source of heterogeneity, we performed a sensitivity analysis of studies in which heterogeneity was present, including age at surgery, weight at surgery, operation time, intraoperative blood transfusion, and length of ICU stay. Excluding any one study under each indicator, the results showed that the study of Sandler et al. (13) was the main source of heterogeneity in the weight at surgery (Figure S4A). After exclusion, there was no significant heterogeneity among the remaining 12 studies (I2=0.0%, P=0.563), so the fixed effect model was used. The results of the meta-analysis showed that the weight at surgery of the Kasai group was heavier. The difference was statistically significant (SMD =0.41; 95% CI: 0.33, 0.48; P<0.001) (Figure S4B,S4C). However, the exclusion of any study in the other indicators did not have a significant effect on heterogeneity, and further search for the source of heterogeneity is needed (Figure S4D-S4G).
Subgroup analysis
To further search for sources of heterogeneity, subgroup analyses were performed. All studies were divided into “Asia” and “non-Asia” groups according to region. According to the time of case reporting, the Cases after 2000 were divided into the “Cases since 2000” group, and the studies involving cases before 2000 were divided into the “Other” group.
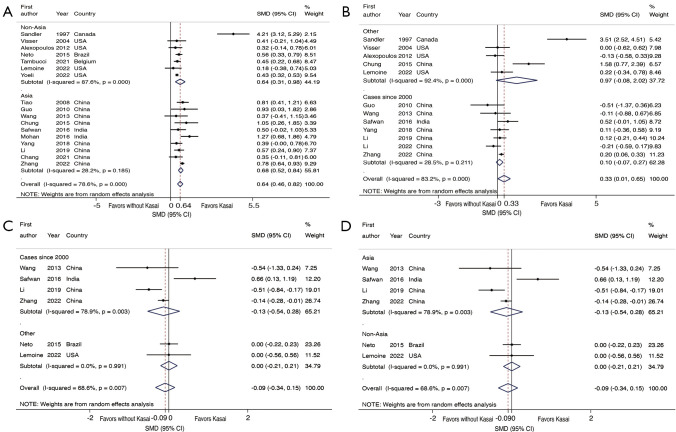
In the “Asia” subgroup, the age at surgery of Kasai group was older, the difference was statistically significant (SMD =0.68; 95% CI: 0.52, 0.84; P<0.001] (I2=28.2%, P=0.185); The “non-Asia” subgroup Kasai group was older, and the difference was statistically significant (SMD =0.64; 95% CI: 0.31, 0.98; P<0.001) (I2=87.6%, P<0.001) (Figure 5A).
Figure 5.
Subgroup analysis. (A) Age at surgery was analyzed according to the subgroups of region. (B) The operation time was analyzed according to the subgroups of case time. (C) The length of ICU stay was divided into subgroups according to patient time. (D) The length of ICU stay was analyzed according to the subgroups of region. SMD, standardized mean difference; CI, confidence interval; ICU, intensive care unit.
In the “Cases since 2000” subgroup, there was no significant difference in operation time between the two groups (P=0.241) (I2=28.5%, P=0.211). In the “Other” subgroup, there was no significant difference in operation time between the two groups (P=0.069) (I2=92.4%, P<0.001) (Figure 5B).
The studies included in the “Cases since 2000” subgroup coincided with the studies included in the “Asia” subgroup, and both showed no significant difference in ICU length of stay between the two groups (P=0.528) (I2=78.9%, P=0.003) (Figure 5C). The studies included in the “Other” subgroup coincided with those in the “non-Asia” subgroup, both of which showed no statistically significant difference in the length of ICU stay between the two groups (P=0.977) (I2=0.0%, P=0.991) (Figure 5D).
The intraoperative blood transfusion could not be analyzed by subgroup analysis because there was only one group under the two grouping methods.
Discussion
BA is a severe cholestatic disease involving intrahepatic and extrahepatic bile ducts, which can rapidly develop into cirrhosis if surgical treatment is not performed in time. Among them, the pros and cons of Kasai procedure and liver transplantation for BA have been controversial. The advantages and disadvantages of the two surgical methods in the treatment of BA are shown in Table 4 (37,38). Of the 26 studies included in this study, 15 studies were more supportive of the Kasai procedure as the first step in the treatment of BA, five studies were more supportive of direct liver transplantation, and six studies had relatively neutral views.
Table 4. Comparison of the advantages and disadvantages of Kasai procedure and liver transplantation.
| Surgical methods | Advantages | Disadvantages |
|---|---|---|
| Kasai procedure | (I) It can prolong the survival time of native liver to a certain extent, and even some patients can survive for a long time without liver transplantation | (I) The long-term survival is not satisfactory, which may be hit by the second operation |
| (II) Improve the preoperative status of liver transplant recipients | (II) Cause abdominal adhesion and scar formation, which will increase the difficulty of liver transplantation and the complications after transplantation | |
| (III) Relieve the tension of insufficient donor liver | (III) Maybe affect the growth and development of patients in childhood and adolescence, leading to malnutrition and growth and development disorders | |
| (IV) Liver transplantation can be postponed to a better age when the basic conditions of BA patients such as body weight, hepatic vessel diameter, and upper abdominal cavity volume are better (37) | ||
| (V) The Roux-en-Y anastomosis established in the Kasai procedure can be used for liver transplantation, which helps save time | ||
| (VI) The abdominal adhesions were mostly membranous, and the separation was not very difficult | ||
| Liver transplantation | (I) Low cost (some countries will provide social support) | (I) Losing the chance of native liver survival |
| (II) High survival rate | (II) Young age will inevitably increase the difficulty of surgery and the probability of postoperative complications | |
| (III) The long-term use of immunosuppressants also increases the probability of infection and cancer | ||
| (IV) If the number of grafts is not proportional to the supply, survival can be affected | ||
| (V) In some countries, liver transplantation is more expensive than Kasai procedure (38) |
BA, biliary atresia.
Explanations of findings
The meta-analysis of the present study confirmed that Kasai procedure can prolong the age at the time of liver transplantation in children with BA, increase body weight, and reduce PELD scores. A lower PELD score predicts lower mortality while waiting for transplantation (39). These results indicate that Kasai procedure can not only reduce the potential surgical risk caused by younger age, but also improve preoperative status.
The results showed that the heterogeneity could be well eliminated when the age at surgery was analyzed in the “Asia” group (I2=28.2%), and the results were not affected and were still being statistically significant. Therefore, we believe that the inference of “the age at surgery of children in the Kasai group is older” is more convincing when applied to the Asian population.
Intestinal adhesion after Kasai procedure will increase the difficulty of liver transplantation. Our preliminary results also showed that children in the Kasai group had longer operation time and more blood loss during transplantation. However, there was no significant difference in intraoperative blood transfusion and hospital stay between the two groups, and the length of ICU stay was even shorter in the Kasai group. Further analysis showed that there was no significant difference in the operation time between the two groups in the “Cases since 2000” subgroup (I2=28.5%), and there was no significant difference in the length of ICU stay between the two groups in the “Other” subgroup and the “non-Asia” subgroup (I2=0.0%). This may indicate that with the gradual development of Kasai procedure, it does not affect the operation time and postoperative recovery of liver transplantation, but the increase of intraoperative blood loss is inevitable.
The incidence of biliary complications and intestinal perforation was higher in children who had undergone the Kasai procedure, which may be due to the easy injury of the intestinal tract and bile duct when the anastomosis between the hepatic hilum and jejunum was separated during liver transplantation. However, there were no significant differences in other postoperative indicators (including infection, reoperation, retransplantation, hepatic artery complications, portal vein complications, hepatic vein complications, rejection, bleeding, lymphatic fistula, and intestinal obstruction) and prognostic survival (including 1-/3-/5-year patient survival rate and 1-/5-year graft survival rate) between the two groups. This may be due to the advancement of surgical techniques and postoperative management, so that biliary complications (biliary fistula and biliary stricture) and intestinal perforation can be timely and effectively prevented and controlled, without affecting the survival of patients and grafts.
In addition, four studies subdivided the Kasai group of patients into two groups: early failure (patients who eventually received a transplant within the first year after Kasai) and late failure (patients who required a transplant after the first year) (20,23,34,35). Alexopoulos et al. (20) showed that patients with early failure had a higher risk of infection than those with late failure and non-Kasai. Neto et al. (23) showed that the late failure group had the highest patient survival and graft survival, while the early failure group had no significant difference in patient survival and graft survival compared with the non-Kasai group. Yoeli et al. (34) showed that outcomes in the early failure group were not significantly different from those in the non-Kasai group, whereas the waiting list and graft survival were higher in the late failure group. Liu et al. (35) showed that the survival difference in the early (<1 year), middle (1–5 years), and late (>5 years) failed groups and no Kasai group was not significant. Although the prognosis of early failure was not better than that of the primary transplantation group, current technical means cannot predict BA children with early failure. However, the timing of the Kasai procedure can affect the survival rate of the autologous liver. Yang et al. (40) showed that the prognosis was good when the age of surgery was about 60 days. When the age of surgery was more than 90 days, the survival time of autologous liver shortened with the increase of the age of surgery, and the probability of early failure also increased.
Strengths and limitations
The strengths of this study are as follows: (I) a total of 26 studies were included in the meta-analysis, which makes the results highly convincing. (II) Indicators from each study were collected as comprehensively as possible during data extraction. (III) To find the source of heterogeneity, subgroup analysis and sensitivity analysis were conducted. The limitations of this study include: (I) all studies are retrospective and lack of data from prospective studies. (II) The disease of some patients with BA progressed too fast and the liver was in the decompensated stage, so they can only choose liver transplantation, which was an inevitable selection bias. (III) Confounding by unknown or no measurable factors cannot be completely ruled out, and any inherent limitations in the included studies could have biased our results.
Conclusions
For children with BA undergoing liver transplantation, although previous Kasai procedure may increase the risk of intraoperative bleeding, biliary complications, and intestinal perforation, it does not affect the main clinical outcomes and can even delay the timing of liver transplantation and improve the preoperative status of children. In this sense, the failed Kasai procedure is also of some significance. It has been shown that 20–40% of patients can achieve long-term native liver survival (≥10 years) after Kasai procedure (35). Therefore, in the treatment of BA children, when there is no obvious contraindication to Kasai procedure, the sequential treatment of Kasai procedure-liver transplantation should be supported first.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: We acknowledge the Tianjin Science and Technology Program (No. 21ZXGWSY00070) and the Tianjin Applied Basic Research Project (No. 22JCZDJC00290) for the support of the research.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-504/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-504/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-504/coif). The authors have no conflicts of interest to declare.
References
- 1.Bezerra JA, Wells RG, Mack CL, et al. Biliary Atresia: Clinical and Research Challenges for the Twenty-First Century. Hepatology 2018;68:1163-73. 10.1002/hep.29905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pakarinen MP, Johansen LS, Svensson JF, et al. Outcomes of biliary atresia in the Nordic countries – a multicenter study of 158 patients during 2005-2016. J Pediatr Surg 2018;53:1509-15. 10.1016/j.jpedsurg.2017.08.048 [DOI] [PubMed] [Google Scholar]
- 3.Saito T, Terui K, Mitsunaga T, et al. Significance and indications for reoperative portoenterostomy in biliary atresia in light of long-term outcome. J Hepatobiliary Pancreat Sci 2018;25:275-80. 10.1002/jhbp.548 [DOI] [PubMed] [Google Scholar]
- 4.Wang Z, Chen Y, Peng C, et al. Five-year native liver survival analysis in biliary atresia from a single large Chinese center: The death/liver transplantation hazard change and the importance of rapid early clearance of jaundice. J Pediatr Surg 2019;54:1680-5. 10.1016/j.jpedsurg.2018.09.025 [DOI] [PubMed] [Google Scholar]
- 5.LeeVan E , Matsuoka L, Cao S, et al. Biliary-Enteric Drainage vs Primary Liver Transplant as Initial Treatment for Children With Biliary Atresia. JAMA Surg 2019;154:26-32. 10.1001/jamasurg.2018.3180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins JPT, Li T, Deeks JJ. Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, et al. editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023. Available online: https://training.cochrane.org/handbook [Google Scholar]
- 8.Shi J, Luo D, Wan X, et al. Detecting the skewness of data from the five-number summary and its application in meta-analysis. Stat Methods Med Res 2023;32:1338-60. 10.1177/09622802231172043 [DOI] [PubMed] [Google Scholar]
- 9.Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Millis JM, Brems JJ, Hiatt JR, et al. Orthotopic liver transplantation for biliary atresia. Evolution of management. Arch Surg 1988;123:1237-9. 10.1001/archsurg.1988.01400340063011 [DOI] [PubMed] [Google Scholar]
- 11.Wood RP, Langnas AN, Stratta RJ, et al. Optimal therapy for patients with biliary atresia: portoenterostomy (“Kasai” procedures) versus primary transplantation. J Pediatr Surg 1990;25:153-62. 10.1016/s0022-3468(05)80183-6 [DOI] [PubMed] [Google Scholar]
- 12.Meister RK, Esquivel CO, Cox KL, et al. The influence of portoenterostomy with stoma on morbidity in pediatric patients with biliary atresia undergoing orthotopic liver transplantation. J Pediatr Surg 1993;28:387-90. 10.1016/0022-3468(93)90237-f [DOI] [PubMed] [Google Scholar]
- 13.Sandler AD, Azarow KS, Superina RA. The impact of a previous Kasai procedure on liver transplantation for biliary atresia. J Pediatr Surg 1997;32:416-9. 10.1016/s0022-3468(97)90594-7 [DOI] [PubMed] [Google Scholar]
- 14.Chardot C, Carton M, Spire-Bendelac N, et al. Prognosis of biliary atresia in the era of liver transplantation: French national study from 1986 to 1996. Hepatology 1999;30:606-11. 10.1002/hep.510300330 [DOI] [PubMed] [Google Scholar]
- 15.Diem HV, Evrard V, Vinh HT, et al. Pediatric liver transplantation for biliary atresia: results of primary grafts in 328 recipients. Transplantation 2003;75:1692-7. 10.1097/01.TP.0000062570.83203.A3 [DOI] [PubMed] [Google Scholar]
- 16.Visser BC, Suh I, Hirose S, et al. The influence of portoenterostomy on transplantation for biliary atresia. Liver Transpl 2004;10:1279-86. 10.1002/lt.20234 [DOI] [PubMed] [Google Scholar]
- 17.Cowles RA, Lobritto SJ, Ventura KA, et al. Timing of liver transplantation in biliary atresia-results in 71 children managed by a multidisciplinary team. J Pediatr Surg 2008;43:1605-9. 10.1016/j.jpedsurg.2008.04.012 [DOI] [PubMed] [Google Scholar]
- 18.Tiao MM, Yang CY, Tsai SS, et al. Liver transplantation for biliary atresia in Taiwan: a national study. Transplant Proc 2008;40:3569-70. 10.1016/j.transproceed.2008.07.136 [DOI] [PubMed] [Google Scholar]
- 19.Guo C, Zhang M, Deng Y, et al. Twenty two living related liver transplantation in children suffering from biliary atresia: a single centre experience. Chin J Pediatr Surg 2010;31:416-20. [Google Scholar]
- 20.Alexopoulos SP, Merrill M, Kin C, et al. The impact of hepatic portoenterostomy on liver transplantation for the treatment of biliary atresia: early failure adversely affects outcome. Pediatr Transplant 2012;16:373-8. 10.1111/j.1399-3046.2012.01677.x [DOI] [PubMed] [Google Scholar]
- 21.Wang Q, Yan LN, Zhang MM, et al. The pre-Kasai procedure in living donor liver transplantation for children with biliary atresia. Hepatobiliary Pancreat Dis Int 2013;12:47-53. 10.1016/s1499-3872(13)60005-3 [DOI] [PubMed] [Google Scholar]
- 22.Celik N, Yankol Y, Aydogdu B. Pediatric Liver Transplantation in Biliary Atresia Patients: One Center Experience. Transplantation 2014;98:722. [Google Scholar]
- 23.Neto JS, Feier FH, Bierrenbach AL, et al. Impact of Kasai portoenterostomy on liver transplantation outcomes: A retrospective cohort study of 347 children with biliary atresia. Liver Transpl 2015;21:922-7. 10.1002/lt.24132 [DOI] [PubMed] [Google Scholar]
- 24.Chung PH, Wong KK, Chan SC, et al. Liver transplant for biliary atresia is associated with a worse outcome – Myth or fact? J Pediatr Surg 2015;50:2134-6. 10.1016/j.jpedsurg.2015.08.042 [DOI] [PubMed] [Google Scholar]
- 25.Safwan M, Ramachandran P, Reddy MS, et al. Living donor liver transplantation for biliary atresia – An Indian experience. Pediatr Transplant 2016;20:1045-50. 10.1111/petr.12749 [DOI] [PubMed] [Google Scholar]
- 26.Mohan N, Karkra S, Kumari C. Does Outcome of Liver Transplantation in Post Kasai Biliary Atresia (BA) Differ from Non Operated BA Cases? Transplantation 2016;100:5(S109):Supplement 1.
- 27.Yang J, Gao W, Zhan J, et al. Kasai procedure improves nutritional status and decreases transplantation-associated complications. Pediatr Surg Int 2018;34:387-93. 10.1007/s00383-018-4228-2 [DOI] [PubMed] [Google Scholar]
- 28.Li S, Ma N, Meng X, et al. The effects of Kasai procedure on living donor liver transplantation for children with biliary atresia. J Pediatr Surg 2019;54:1436-9. 10.1016/j.jpedsurg.2018.07.022 [DOI] [PubMed] [Google Scholar]
- 29.Chang Q, Wang J, Song C. Clinical efficacy of living donor liver transplantation in children with biliary atresia. Journal of Practical Hepatology 2021;24:431-4. [Google Scholar]
- 30.Tambucci R, de Magnée C, Szabo M, et al. Sequential Treatment of Biliary Atresia With Kasai Hepatoportoenterostomy and Liver Transplantation: Benefits, Risks, and Outcome in 393 Children. Front Pediatr 2021;9:697581. 10.3389/fped.2021.697581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li X, Feng X, Xie Y, et al. Effect of Kasai operation on clinical efficacy of liver transplantation in children with biliary atresia. Chinese Journal of Hepatic Surgery (Electronic Edition) 2022;11:149-53. [Google Scholar]
- 32.Zhang Z, Dong C, Sun C, et al. The effects of Kasai procedure on the liver transplantation for children with biliary atresia. Tianjin Medical Journal 2022;50:20-4. [Google Scholar]
- 33.Lemoine CP, LeShock JP, Brandt KA, et al. Primary Liver Transplantation vs. Transplant after Kasai Portoenterostomy for Infants with Biliary Atresia. J Clin Med 2022;11:3012. 10.3390/jcm11113012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoeli D, Choudhury RA, Sundaram SS, et al. Primary vs. salvage liver transplantation for biliary atresia: A retrospective cohort study. J Pediatr Surg 2022;57:407-13. 10.1016/j.jpedsurg.2021.12.027 [DOI] [PubMed] [Google Scholar]
- 35.Liu L, Wei L, Qu W, et al. Impact of the Kasai Procedure and the Length of Native Liver Survival Time on Outcomes of Liver Transplantation for Biliary Atresia. Liver Transpl 2022;28:224-35. 10.1002/lt.26287 [DOI] [PubMed] [Google Scholar]
- 36.Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of andomized controlled trials. BMJ 2011;343:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 37.Arnon R, Annunziato RA, D’Amelio G, et al. Liver Transplantation for Biliary Atresia: Is There a Difference in Outcome for Infants? J Pediatr Gastroenterol Nutr 2016;62:220-5. 10.1097/MPG.0000000000000986 [DOI] [PubMed] [Google Scholar]
- 38.Raghu VK, Squires JE, Mogul DB, et al. Cost-Effectiveness of Primary Liver Transplantation Versus Hepatoportoenterostomy in the Management of Biliary Atresia in the United States. Liver Transpl 2021;27:711-8. 10.1002/lt.25984 [DOI] [PubMed] [Google Scholar]
- 39.Chang CH, Bryce CL, Shneider BL, et al. Accuracy of the Pediatric End-stage Liver Disease Score in Estimating Pretransplant Mortality Among Pediatric Liver Transplant Candidates. JAMA Pediatr 2018;172:1070-7. 10.1001/jamapediatrics.2018.2541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang C, Ke M, Zhou Y, et al. Impact of early Kasai portoenterostomy on short-term outcomes of biliary atresia: A systematic review and meta-analysis. Front Surg 2022;9:924506. 10.3389/fsurg.2022.924506 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as