Abstract
Background
Young children, 6 months to 4 years of age, were the last population for whom the COVID-19 vaccines became available and remain the group with the lowest uptake. Scarce information exists on drivers of vaccine uptake in young children. The relationship between parental perceived risk of infection and child COVID-19 vaccination is unknown.
Objective
Examine the association between perceived risk of infection and early childhood vaccination.
Methods
In June 2020, perinatal women in Vermont were enrolled in a longitudinal survey study assessing life changes during the pandemic. Surveys included worry of infection, Parents Attitude about Childhood Vaccines (PACV), intention to vaccinate children with the COVID-19 vaccine, and masking behaviors. Once vaccines became available, surveys also included child vaccination status. A demographic-adjusted stepwise logistic regression was conducted to assess the relationship of worry of infection and vaccine hesitancy on child vaccination status.
Results
85 women completed baseline and follow up surveys. Participants were highly adherent to adult COVID vaccines with 93 % at least partially vaccinated and only 3 % demonstrated general childhood vaccine hesitancy on the PACV. However, in this highly adherent population, only 61 % of young children are vaccinated. In univariate [OR = 7.35 95 % CI (2.70 to 20.02)] and demographic adjusted [OR = 6.03 95 % CI (1.30 to 27.90)] models, current worry about child infection was associated with higher odds of child vaccination. Previously established predictors, vaccine hesitancy [OR = 0.91 95 % CI (0.84 to 0.99)] and younger maternal age [OR = 1.33 95 % CI (1.07 to 1.65)] were again associated lower odds of child vaccination.
Conclusion
Among vaccine adherent parents, worry of infection was a strong predictor of vaccine uptake. Continued efforts to articulate the potential morbidity of COVID in young children, along with established methods to address general vaccine hesitancy may aid in COVID vaccine uptake in this population.
Keywords: COVID-19, Vaccine uptake, Vaccine hesitancy, Childhood vaccination, COVID-19 vaccine
Introduction
SARS CoV-2 (COVID-19) is a highly transmissible and pathogenic respiratory virus. In some patients, especially those with severe infection, COVID-19 can lead to devastating complications such as acute respiratory distress syndrome or organ failure affecting the kidneys or the heart. Since the beginning of the pandemic, more than 15 million cases of COVID-19 in children have been reported in the United States [1]. Though the effects of COVID-19 in children are not fully understood, young children (0–4 years) with COVID-19 infection have required hospitalization more frequently than older children [2]. Vaccination against COVID-19 has been associated with decreased risk of hospitalization in adolescents and school aged children [3], [4]. Lack of eligibility for COVID-19 vaccines correlated with disparate increases in hospitalization rates in young children during the Omicron surge in early 2022 [4], [5]. On June 17th, 2022, the FDA authorized the Moderna and Pfizer-BioNTech COVID-19 vaccines for children 6 months – 5 years of age. Despite evidence that the benefits of the COVID-19 vaccination in children outweigh the risks, uptake of vaccines in this population has been low [6]. In December 2023, rates of young children having received at least one COVID-19 vaccination were 10 % nationally with significant state to state variability (2.1 %–36.1 %) National vaccine uptake in this youngest population has been slower than that seen in school aged children. [8] There remains a gap in understanding what factors contribute to low childhood COVID-19 vaccine uptake, as well as factors that predict vaccine uptake in young children.
Studies of COVID-19 vaccines, and other infection prevention behaviors in adults reveal several variables may have particular importance in the current climate. In adults, perceived risk of infection has been associated with level of participation in COVID-19 preventative efforts such as handwashing, social distancing and vaccination [9], [10]. Predictors of vaccine hesitancy include, lower level of institutional trust, not being vaccinated against influenza, and perceived safety concerns with vaccinations [11]. In addition, demographic differences including female sex, age < 50 and lower educational attainment have been associated with increased vaccine hesitancy [11], [12]. However, previous experience with emerging pandemics demonstrate that parents may have different priorities and concerns regarding childhood vaccination than the general adult population. For example, during the H1N1 Influenza pandemic, 56 % of parents abstained from having their children vaccinated with the H1N1 vaccine and indicated safety concerns about the vaccine as a major factor in their decision. This is substantially lower than the 35 % of adult abstainers who indicated this was a major driver. Further the proportion of parents who indicated they did not feel public health officials would be forthcoming and honest about vaccine side effects was significantly higher than adults who did not receive the H1N1 flu vaccine (31 % vs 19 %; p < 0.05) [13]. Additionally, during this pandemic, perceived risk of H1N1 infection was not a significant predictor of vaccine uptake among parents when accounting for other social “cues to action” such as affirming messages from role models or celebrities [14].
Factors that influence intention to vaccinate children against COVID-19 have also been explored and reveal parents continue to be substantially concerned about vaccine side effects in the current climate. For instance, Szilagyi et al report a survey of 3759 parent–child pairs conducted between April 2020 and February 2021, including 884 children <5. They report parental concerns about vaccinating their children center around safety and side effects of the vaccine. [15] This is consistent with others who have evaluated reasons for parental hesitancy toward the COVID-19 vaccine. [16], [17], [18] Szilagyi also found parents who had older children, had received the adult COVID-19 vaccine, and who had a bachelor’s degree or higher were more likely to indicate they were “very likely” or “likely” to get a COVID-19 vaccine for their child. Lastly, 20 % of parents of children <5 indicated they would get the COVID-19 vaccine for their young child “as soon as possible.” [15] This is drastically different than the previously mentioned low rates of uptake seen now that the vaccine is available. Moreover, multiple reports indicate COVID-19 vaccine hesitancy is persistent even among those adherent to other childhood vaccines. For instance, Rane et al report only 10 % of vaccine adherent parents indicate they would not immediately vaccinate their child [18]. Similarly, the cohort described in this study consisted of highly vaccine adherent participants, yet only 50 % of whom reported of intention to vaccinate their young children [17]. Thus, an understanding of the correlations between intention to have children vaccinated and actual vaccine uptake, as well as predictors of uptake has potential to guide future public health messaging and elucidate opportunities to increase COVID-19 vaccine acceptance.
Materials and methods
Study population
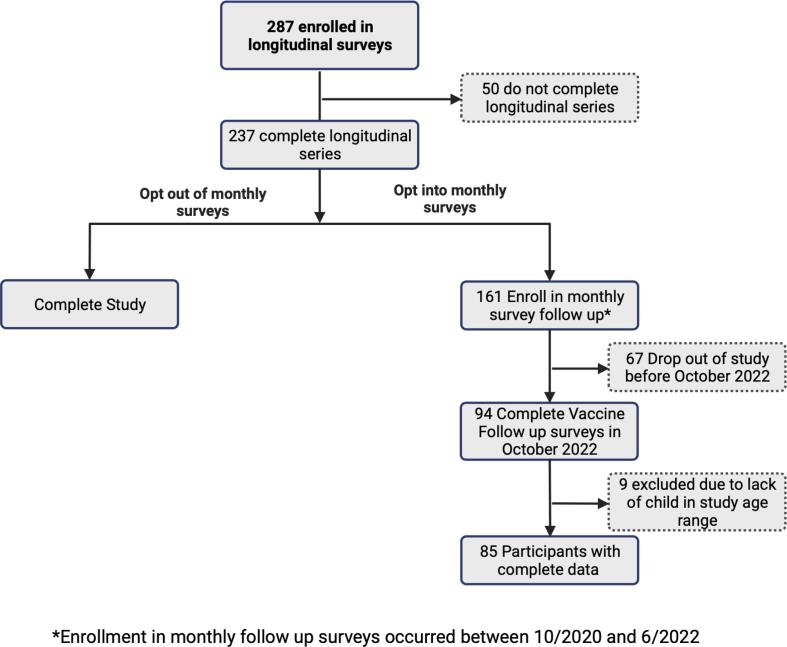
In June 2020, perinatal women receiving obstetric care at University of Vermont Medical Center were enrolled in a longitudinal study assessing the effects of COVID-19 on women and their children. Eligible women were 18 or older, pregnant, or had an infant 6 months old or younger. Participants were recruited if they indicated interest in research studies or if they met inclusion criteria by medical record review. Potential participants were emailed a study description and link to consent information. Overall enrollment rate for this convenience sample was approximately 10 %. Upon enrollment participants completed longitudinal questionnaires every 2 weeks for a total of 12 weeks that included demographic information, and questions about how the COVID pandemic had impacted their lives. A total of 287 participants completed enrollment, 83 % of whom completed the entire 12 week series. Following this longitudinal set of surveys, participants were given the choice to continue completing an additional 30 months of monthly surveys that assess life changes related to the pandemic including social distancing and masking behaviors, mental health symptoms, access to social supports among others. At time of this analysis all participants have completed the initial longitudinal series; 177 opted into the monthly follow up surveys. In January 2021, additional surveys were implemented to assess attitudes and behaviors regarding the COVID-19 vaccines. These included the Parents Attitude about Childhood Vaccines (PACV), maternal vaccination status, and whether women were worried about their children contracting COVID-19. In October 2022, surveys were updated to include child vaccination status. Fig. 1 depicts the flow of participants through the sequential studies from which our sample was obtained.
Fig. 1.
Study flow diagram from parent study to sample included in the current analysis.
Measures
Vaccine hesitancy was measured with the Parent Attitudes about Childhood Vaccines (PACV). The PACV is a validated instrument used to assess parental vaccine hesitancy related to standard childhood immunizations [19], [20]. It includes 15 questions assessing parental beliefs about vaccines including safety and efficacy, general attitude, and vaccine behaviors. Scores were summed and normalized as is standard for this measure. Participants with a PACV score > 50 are considered vaccine hesitant. Primipara women were excluded from the PACV questionnaires as they would not have been able to answer questions such as “Have you ever delayed having your child get a shot for reasons other than illness or allergy?”
Masking behaviors were measured with the question “In the past 2 weeks how often have you worn a mask or face covering when in a store or other business?” Response options included “Always,” “Most of the time,” “Some of the time,” “Hardly Ever,” and “Never.”
Intention to vaccinate children was measured with the question “Which of the following applies to your plans about the COVID-19 vaccine for your child(ren)?” Response options included “I do not plan on getting the vaccination for my child”, “I plan on getting the vaccination for my child after other children have gotten it,” and “I plan on getting the vaccination for my child as soon as it’s available to them.”
To assess worry of children contracting COVID-19 participants were asked “How often do you worry about your child(ren) getting COVID” and this was measured on a 5-point Likert scale with options: “never” “rarely” “sometimes” “often” “always.” Worry of children contracting COVID-19 was assessed at baseline and with each monthly survey.
Covariates
Predictors were assessed within the context of the following covariates. Maternal age, Child’s age, parental education level, combined annual family income, and maternal vaccination status. Race was not included in models. Parental education was considered as a categorical variable with the following categories: < 4 year degree; 4 year college degree; > 4 year degree. Additionally combined family income was assessed in 4 categories: <$50,000; $50,001-$100,000; $100,001-$180,000; >$180,000. A measure of medical complexity was assessed with participant perception of their child’s susceptibility to COVID compared to other children their age. Single answer options included “much lower,” “lower,” “similar,” “higher,” “much higher.” Lastly, Maternal COVID-19 vaccination status was asked monthly. Participants who reported they were partially or fully vaccinated were considered “vaccinated,” those who never received a COVID-19 vaccine were considered “unvaccinated.”.
Statistical analysis
Statistical analyses were performed using Stata 17.0 (StataCorps LLC, College Station, Texas). Current worry of infection was collapsed into a dichotomous variable for regression analyses with those who indicated they worried about infection sometimes or more often categorized as “Worried.” Masking behavior was also dichotomized with those who reported wearing a mask at least some of the time considered “masking.”
Univariate analyses of predictor variables including, intention to have children vaccinated in Jan 2021, maternal vaccination status, worry about child infection (at baseline and follow up), and PACV scores were conducted to assess individual associations with child vaccination status, and masking behaviors. Subsequently, a demographic-adjusted (maternal age, income, and education), stepwise logistic regression of predictors and covariates was conducted to generate the best fit model. Significance level for inclusion was set at 0.05 [21]. Stepwise regression was chosen given the lack of current understanding of the relationship between variables such as worry about contracting COVID and historical vaccine hesitancy on likelihood to have young children vaccinated. The benefit of the stepwise approach is that it allows to control for confounding variables with unknown relationships to better understand the individual correlations between predictive variables and outcomes.
Results
85 women completed baseline and follow up surveys. The mean maternal age was 33 years old; most women had received a college education with 82 % having at least a 4-year degree, and 43 % had a family income >$100,001 per year (Table 1). Mothers in our population were highly adherent to adult COVID-19 vaccines with 93 % of women at least partially vaccinated or fully vaccinated. Only 3 % demonstrated general childhood vaccine hesitancy on the PACV. The mean PACV score was 10. At the time of the baseline survey, 86 % of women reported worrying at least sometimes about their child contracting COVID-19. This proportion decreased to 66 % reporting worry about infection in October 2022. 61 % of children had been vaccinated with at least one COVID-19 vaccine in October 2022. 40 % of participants were wearing masks while going to the store.
Table 1.
Characteristics of the study population.
| Characteristics | Mean or N | SD or % |
|---|---|---|
| Maternal Age (years) | 33 | 5.7 |
| Child Age (months) | 20 | 9.7 |
| Income | ||
| <$50,000 | 14 | 17 % |
| $50,001-$100,000 | 36 | 42 % |
| $100,001 to $180,000 | 28 | 33 % |
| >$180,000 | 7 | 8 % |
| Education | ||
| <4 year degree | 16 | 19 % |
| 4 year degree | 33 | 39 % |
| >4 year degree | 36 | 42 % |
| PACV scores | 10 | 15.7 |
| Worry about child contracting COVID (Baseline) | ||
| Not worried | 13 | 15 % |
| Worried | 72 | 85 % |
| Worry about child contracting COVID (Follow up) | ||
| Not worried | 29 | 34 % |
| Worried | 56 | 66 % |
| Parental perception of their child’s susceptibility to COVID compared to other kids their age | ||
| Much lower | 9 | 11 % |
| Lower | 27 | 32 % |
| Similar | 43 | 51 % |
| Higher | 4 | 5 % |
| Much Higher | 1 | 1 % |
| Maternal COVID Vaccination Status | ||
| Partially or fully vaccinated | 79 | 93 % |
| Unvaccinated | 6 | 7 % |
| Child COVID Vaccination Status | ||
| Partially or fully vaccinated | 52 | 61 % |
| Unvaccinated | 33 | 39 % |
| Masking Behavior | ||
| Masking in public | 33 | 40 % |
| Not masking in public | 52 | 60 % |
Maternal vaccination status
All participants who were not vaccinated themselves did not vaccinate their children. Given the lack of variability in maternal vaccine status it was not included in the regression analyses.
Vaccine hesitancy
The few participants who were vaccine hesitant (PACV > 50) did not vaccinate their infants when the vaccine became available. PACV scores were significantly associated with higher odds of child vaccination in both the univariate (OR = 0.920, p = 0.001) and multivariate analyses (OR = 0.909, p = 0.014). PACV scores were also significantly associated with masking behaviors in univariate analyses with increased scores being associated with lower likelihood of masking (OR = 0.937 (0.89–0.99); p = 0.02). In multivariable analyses inclusion of PACV scores improved the model predicting masking behaviors but was not itself a statistically significant predictor (Table 3).
Table 3.
Odds ratios of univariate relationships between participant characteristics and outcomes.
| Characteristics | Vaccination Status OR (95 %CI) |
Masking Behavior OR (95 %CI) |
|---|---|---|
| Maternal Age (years) | 1.37 (1.17–1.60) | 1.04 (0.95–1.14) |
| Child Age (months) | 0.999 (0.998–1.001) | 0.999 (0.998–1.001) |
| Income | ||
| <$50,000 | Base | Base |
| $50,001-$100,000 | 2.25 (0.63–8.06) | 1.33 (0.34–5.19) |
| $100,001 to $180,000 | 6.60 (1.60–27.2) | 1.46 (0.36–5.91) |
| >$180,000 | 4.50 (0.63–32.3) | 5.625 (0.75–42.4) |
| Education | ||
| <4 year degree | Base | Base |
| 4 year degree | 5.88 (1.40–24.6) | 2.10 (0.49–9.03) |
| >4 year degree | 21.7 (4.69–100.2) | 3.67 (0.87–15.4) |
| PACV scores | 0.92 (0.87–0.97) | 0.94 (0.89–0.99) |
| Worry about child contracting COVID (Baseline) | ||
| Not worried | Base | Base |
| Worried | 3.13 (0.92–10.6) | 2.56 (0.65–10.1) |
| Worry about child contracting COVID (Follow up) | ||
| Not worried | Base | Base |
| Worried | 7.35 (2.70–20.0) | 6.69 (2.05–21.9) |
| Parental perception of their child’s susceptibility to COVID compared to other kids their age | ||
| Much lower | 0.52 (0.12–2.23) | 1.08 (0.23–5.16) |
| Lower | 1.55 (0.56–4.34) | 2.25 (0.84–6.04) |
| Similar | Base | Base |
| Higher | 0.65 (0.08–5.09) | * |
| Much Higher | * | * |
*Too few observations to calculate.
Intention
Of participants who reported they intended to vaccinate their children at baseline, 67 % were subsequently vaccinated (Table 2). In univariate analyses, those who reported they did not intend to vaccinate their child were significantly less likely to have a vaccinated child OR 0.03 95 % CI (0.004–0.27), however there was not a significant difference between those who planned to get their child vaccinated as soon as it was available and those who intended to wait until other children had received the COVID-19 vaccine OR 0.46 95 % CI (0.16–1.27). Intention to vaccinate was not significantly associated with masking behavior in univariate analyses and did not improve the multivariate model for vaccination status nor masking behavior.
Table 2.
Intention to vaccinated at baseline compared to child vaccine status in October 2022.
| Vaccine intention at baseline | Vaccination status in Oct 2022 |
|
|---|---|---|
| Unvaccinated (%) | Vaccinated (%) | |
| Vaccinate child as soon as the vaccine is available | 11 (24 %) | 35 (76 %) |
| Vaccinate child after other children have received the vaccine | 11 (41 %) | 16 (59 %) |
| Does Not Plan to Vaccinate | 10 (91 %) | 1 (9 %) |
Chi Square test for statistical difference = 17.0, p < 0.001.
Worry of children contracting COVID-19
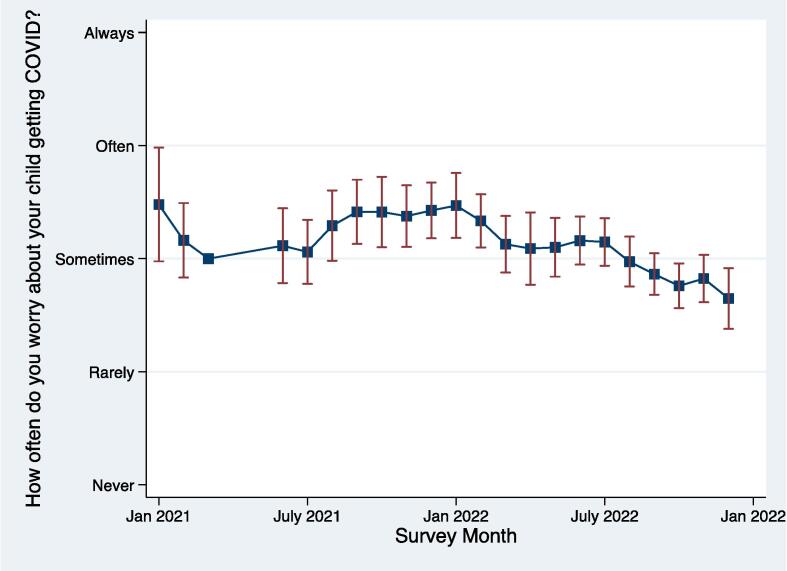
Worry of COVID-19 at baseline, prior to access to vaccinations, was not a predictor of future infant vaccination status [p = 0.067]. However, worry of COVID-19 infection in October 2022 was a predictor of infant vaccination status. In mothers who identified as worried at the follow up timepoint, 77 % of infants were vaccinated. Worry of COVID-19 has varied over time and the average of worry of COVID-19 infection in our population is decreasing (Fig. 2). Across the baseline and follow up time points, worry has decreased significantly (Chi Square 8.9; p 0.003).
Fig. 2.
Mean rating of participants level of worry about their children contracting COVID-19 over time is represented with the line and markers, bars represent the standard deviations. A 3 month gap exists between the earliest baseline vaccine assessments and implementation of the monthly follow up assessments.
In univariate [OR = 7.35 95 % CI (2.70 to 20.02)] and demographic adjusted for maternal age, income, and education level [OR = 6.03 95 % CI (1.30 to 27.90)] models, current worry about child infection was associated with higher odds of child vaccination (Table 4). More frequent worry about COVID-19 was associated with similarly increased odds of masking in public. The odds in the univariate analysis [OR = 6.69 95 % CI (2.05 to 21.86)] remained significant in the full model [OR = 4.87 95 % CI (1.26 to 18.8)] Vaccine hesitancy (PACV score > 50) [OR = 0.91 95 % CI (0.84 to 0.99)] and younger maternal age [OR = 1.33 95 % CI (1.07 to 1.65)] were associated lower odds of child vaccination (Table 4). For models of masking behaviors, only current worry was associated with a significantly increased odds of masking.
Table 4.
Demographic adjusted odds ratios of variables associated with child vaccine uptake and masking behaviors.
| Predictors | Vaccine uptake |
Masking behaviors |
||
|---|---|---|---|---|
| Odds ratio | 95 % CI | Odds ratio | 95 % CI | |
| COVID-19 Worry | 6.0 | (1.30–27.9) | 4.87 | (1.26–18.8) |
| Maternal Age | 1.33 | (1.07–1.65) | 0.99 | (0.90–1.1) |
| PACV score | 0.91 | (0.84–0.99) | Did not meet inclusion | |
Income and Education were included in the models but were not significant predictors in either model. Bolded odds ratios indicate p < 0.05.
Discussion
This study adds to the understanding of factors that influence beliefs and behaviors surrounding vaccination of young children against COVID-19. To our knowledge, this study represents the first longitudinal prospective assessment of caregiver COVID-19 vaccine intentions and behaviors. Second, the results indicate that caregiver worry about their child contracting COVID-19 is strongly associated with child vaccination status. These results suggest that there may be important opportunities to encourage vaccine uptake in families of young children. Lastly, this study suggests that general hesitancy toward childhood vaccinations is associated with lower odds of vaccinating children against COVID-19.
With any study related to COVID-19, context is key. This study takes place in Vermont. A state with some of the highest rates of COVID-19 vaccination across the United States and with low rates of infection [22]. Additionally, when initial COVID-19 vaccinations became available, the Vermont State Governor implemented a vaccination roll-out plan and encouraged all Vermont residents to become vaccinated. Large scale vaccination clinics made the vaccines accessible and were open throughout the state at the start of the pandemic and closed in May 2023 [23]. Vermonters were early adopters of the COVID-19 vaccine for the youngest populations with 32 % of eligible children 6 months to 4 years receiving at least one dose of the vaccine in the first 6 months it was available [7]. For these reasons, we believe that rather than offering the ability to generalize our findings, these participants represent those most likely to accept the COVID-19 vaccine for their children. It is with this lens that we interpret the results described above.
While several studies have investigated factors influencing parents’ intentions to vaccinate their children against COVID-19, little is known about how intention translates into behavior. We have previously reported readiness to have young children vaccinated against COVID-19 within this study population substantially fluctuated over time [17]. Even so, caregiver intention to vaccinate young children, prior to vaccine availability, was predictive of young children being vaccinated. Alternatively, caregivers who indicated they did not intend to vaccinate their children did not pursue the COVID-19 vaccine when it was available. Factors previously demonstrated to influence intention to vaccinate consistently include age, education level, higher income, and vaccine hesitancy [24], [25]. However, many of these variables are fixed, making intention to vaccinate difficult to target with intervention efforts. Thus, evaluating modifiable factors influencing vaccine intention and subsequent uptake may prove useful to changing vaccine behaviors.
Vaccine hesitancy is not unique to the COVID-19 vaccine. Historical evidence of factors influencing childhood influenza vaccination may shed light on factors influencing the acceptance of the COVID-19 vaccine. The childhood influenza vaccine is less frequently accepted by parents than routine childhood vaccination. Kempe et al. reported that 1 in 15 US parents are hesitant about routine childhood vaccines, while 1 in 4 are hesitant about the influenza vaccine. Further, they report vaccine efficacy and safety are the most common parental concerns about receiving the annual flu vaccine [26]. Factors that result in vaccine hesitancy and vaccine acceptance are important in informing public health interventions.
The findings we report are consistent with the limited literature associating concern about influenza infection with vaccine intention and behavior. Liao et al. identified that worry about one’s child becoming infected with influenza is the most common reason for pursuing vaccination [27]. However, others reported that worry about influenza infection was not a statistically significant association of intent to vaccinate against influenza [28], [29]. Therefore, it is possible that worry of infection influences behaviors more than intention. The association between increased worry about COVID-19 infection and increased frequency of masking in public supports the hypothesis that concern about infection is a driver of protective behaviors.
It is also worth noting that in univariate analyses parental education and income have significant associations with COVID vaccination. This does not persist in the full models after accounting for worry about COVID infection in one’s child. The large OR associated with worry about infection and the lack of association between these socioeconomic variables suggest that worry about COVID is a stronger driver of vaccine uptake in our population. Furthermore, the lack of association between vaccination and masking behaviors and age of the child is somewhat unexpected as rates of vaccinations against other respiratory viruses is higher in those under 2 years [30]. That said, in diseases such as influenza the youngest age groups have consistently had the broadest coverage in the United States for a number of years leading up to the COVID pandemic. [30].
Some might take these results to indicate that public health messaging should increase fear of infection to improve childhood vaccination coverage. Indeed, early messaging about COVID-19 infection and information provided via social media has been criticized for sensationalism and emphasis on the threat of COVID-19 without equal attention to actionable steps to mitigate risk [31], [32], [33]. Fear based public health messaging is most effective when the focus is on the desired behaviors and next steps [32]. Therefore, while we would not promote implementation of widespread fear-based campaigns, our data suggest it is important to continue to relay the accurate risks of childhood infection, and that childhood vaccination is safe and decreases risk of disease.
There are many similarities between factors influencing parental acceptance of childhood influenza vaccination and COVID-19 vaccination. This suggests interventions which target flu vaccine uptake make have similar efficacy in increasing COVID-19 vaccine uptake[34]. As such, one example of an opportunity to capitalize on parental concern would be to encourage COVID-19 vaccines while children are hospitalized for other viral illnesses and incorporate COVID-19 vaccine efforts into discharge planning.
Our study has important limitations to consider. First, the regional context as has been described is critical to frame the results. Additionally, the study design is that of convenience sampling. Thus, those answering the survey questions have willingly opted into this research project. That said, the breadth of the parent study aims, to understand the impact of COVID on perinatal individuals and their children, lacked a specific focus on vaccine behaviors that may have otherwise dissuaded those with significant vaccine hesitation specifically. Additionally, there was significant drop off in the study from time of enrollment to time of follow up vaccine questionnaires. We compared the population of participants who enrolled in the parent study to those in this specific study and found no differences in demographics, baseline vaccine hesitancy, intention to vaccinate their children, perceived susceptibility to COVID or concern about children becoming infected. Lastly, the sample size is modest making it more difficult to identify relationships with smaller effect size. Although this may have decreased or ability to identify covariates with smaller impacts, it does suggest that worry about COVID infection is indeed a strong predictor to protective behaviors. Acknowledging these limitations, we believe our data represent an important longitudinal study of vaccine behaviors that may prompt further investigation of these behavioral drivers.
In sum, this study demonstrates moderate uptake of COVID-19 vaccination for young children among vaccine adherent parents. Furthermore, the data indicates that worry about children becoming infected with COVID-19 is strongly correlated with protective behaviors. Similar studies are needed across different populations to test generalizability, but these results are consistent with generalized drivers of childhood influenza vaccination.
Funding ources
This work was supported by the National Institutes of Health: [grant number: R34DA050283-01S], and The Children’s Miracle Network.
CRediT authorship contribution statement
Kristen Keene: Conceptualization, Formal analysis, Writing – original draft. Anupama Balasubramanian: Conceptualization, Writing – original draft. Alexandra Potter: Funding acquisition, Investigation, Supervision, Writing – review & editing. Leigh-Anne Cioffredi: Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Leigh-Anne Cioffredi reports financial support was provided by National Institutes of Health. Leigh-Anne Cioffredi reports financial support was provided by Children’s Miracle Network Hospitals.
Data availability
Data will be made available on request.
References
- 1.Pediatrics. AAo. Children and COVID-19 State Data Report. 2023. Accessed April 20, 2023. https://downloads.aap.org/AAP/PDF/AAP%20COVID-19%20State%20Data%20Report%204.13.23%20FINAL.pdf?_ga=2.129443084.1204634337.1681923420-1183351689.1662644287.
- 2.Kim T.Y., Kim E.C., Agudelo A.Z., Friedman L. COVID-19 hospitalization rate in children across a private hospital network in the United States: COVID-19 hospitalization rate in children. Arch Pediatr. Oct 2021;28(7):530–532. doi: 10.1016/j.arcped.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi D.S., Whitaker M., Marks K.J., et al. Hospitalizations of Children Aged 5–11 Years with Laboratory-Confirmed COVID-19 - COVID-NET, 14 States, March 2020-February 2022. MMWR Morb Mortal Wkly Rep. 2022;71(16):574–581. doi: 10.15585/mmwr.mm7116e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marks K.J., Whitaker M., Anglin O., et al. Hospitalizations of Children and Adolescents with Laboratory-Confirmed COVID-19 - COVID-NET, 14 States, July 2021-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(7):271–278. doi: 10.15585/mmwr.mm7107e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamid S, Woodworth K, Pham H, et al. COVID-19-Associated Hospitalizations Among U.S. Infants Aged <6 Months - COVID-NET, 13 States, June 2021-August 2022. MMWR Morb Mortal Wkly Rep. Nov 11 2022;71(45):1442-1448. doi: 10.15585/mmwr.mm7145a3. [DOI] [PMC free article] [PubMed]
- 6.Fleming-Dutra K.E., Wallace M., Moulia D.L., et al. Interim Recommendations of the Advisory Committee on Immunization Practices for Use of Moderna and Pfizer-BioNTech COVID-19 Vaccines in Children Aged 6 Months-5 Years - United States, June 2022. MMWR Morb Mortal Wkly Rep. 2022;71(26):859–868. doi: 10.15585/mmwr.mm7126e2. [DOI] [PubMed] [Google Scholar]
- 7.Murthy B.P., Fast H.E., Zell E., et al. COVID-19 Vaccination Coverage and Demographic Characteristics of Infants and Children Aged 6 Months-4 Years - United States, June 20-December 31, 2022. MMWR Morb Mortal Wkly Rep. 2023;72(7):183–189. doi: 10.15585/mmwr.mm7207a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sparks G., Lopes L., Hamel L., Montero A., Presiado M., Brodie M. Kaiser Family Foundation; 2September 2022. KFF COVID-19 vaccine monitor. [Google Scholar]
- 9.Dryhurst S., Schneider C.R., Kerr J., et al. Risk perceptions of COVID-19 around the world. J Risk Res. 2020;23(7–8):994–1006. [Google Scholar]
- 10.Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Heal Addict. 2021;19:1875–1888. doi: 10.1007/s11469-020-00281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pires C. Global Predictors of COVID-19 Vaccine Hesitancy: A Systematic Review. Vaccines (Basel). Aug 18 2022;10(8). doi: 10.3390/vaccines10081349. [DOI] [PMC free article] [PubMed]
- 12.Fajar JK, Sallam M, Soegiarto G, et al. Global Prevalence and Potential Influencing Factors of COVID-19 Vaccination Hesitancy: A Meta-Analysis. Vaccines (Basel). Aug 19 2022;10(8). doi: 10.3390/vaccines10081356. [DOI] [PMC free article] [PubMed]
- 13.SteelFisher GK, Blendon RJ, Bekheit MM, Lubell K. The public's response to the 2009 H1N1 influenza pandemic. N Engl J Med. Jun 3 2010;362(22):e65. doi:10.1056/NEJMp1005102. [DOI] [PubMed]
- 14.Hilyard K.M., Quinn S.C., Kim K.H., Musa D., Freimuth V.S. Determinants of Parental Acceptance of the H1N1 Vaccine. Health Educ Behav. Jun 2014;41(3):307–314. doi: 10.1177/1090198113515244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szilagyi PG, Shah MD, Delgado JR, et al. Parents' Intentions and Perceptions About COVID-19 Vaccination for Their Children: Results From a National Survey. Pediatrics. Oct 2021;148(4)doi:10.1542/peds.2021-052335. [DOI] [PMC free article] [PubMed]
- 16.Ruggiero K.M., Wong J., Sweeney C.F., et al. Parents' Intentions to Vaccinate Their Children Against COVID-19. J Pediatr Health Care. 2021;35(5):509–517. doi: 10.1016/j.pedhc.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cioffredi L.A., Kohlasch K.L., Thomas E., Potter A.S. Persistently low readiness to vaccinate young children against COVID among vaccine adherent mothers in Vermont, USA. Prev Med Rep. Aug 2022;28 doi: 10.1016/j.pmedr.2022.101841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rane M.S., Robertson M.M., Westmoreland D.A., Teasdale C.A., Grov C., Nash D. Intention to Vaccinate Children Against COVID-19 Among Vaccinated and Unvaccinated US Parents. JAMA Pediatr. 2022;176(2):201–203. doi: 10.1001/jamapediatrics.2021.5153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Opel D.J., Mangione-Smith R., Taylor J.A., et al. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin. Apr 2011;7(4):419–425. doi: 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Opel D.J., Taylor J.A., Mangione-Smith R., et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–6605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- 21.Bose S. Inference and Prediction; JSTOR: 2003. The Elements of Statistical Learning: Data Mining. [Google Scholar]
- 22.Bollyky T.J., Castro E., Aravkin A.Y., et al. Assessing COVID-19 pandemic policies and behaviours and their economic and educational trade-offs across US states from Jan 1, 2020, to July 31, 2022: an observational analysis. Lancet. 2023;401(10385):1341–1360. doi: 10.1016/S0140-6736(23)00461-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.State of Vermont Office of Governor Phil Scott. Novel Coronavirus (COVID-19): Vermont State Response & Resources. State of Vermont. Updated June 14, 2021. 2023. https://governor.vermont.gov/covid19response#.
- 24.Walker K.K., Head K.J., Owens H., Zimet G.D. A qualitative study exploring the relationship between mothers' vaccine hesitancy and health beliefs with COVID-19 vaccination intention and prevention during the early pandemic months. Hum Vaccin Immunother. 2021;17(10):3355–3364. doi: 10.1080/21645515.2021.1942713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: Results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kempe A, Saville AW, Albertin C, et al. Parental Hesitancy About Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics. Jul 2020;146(1). doi: 10.1542/peds.2019-3852. [DOI] [PMC free article] [PubMed]
- 27.Liao Q, Lam WWT, Cowling BJ, Fielding R. Psychosocial Influences on Parental Decision-Making Regarding Vaccination Against Seasonal Influenza for Young Children in Hong Kong: a Longitudinal Study, 2012–2013. Int J Behav Med. 2016/10/01 2016;23(5):621-634. doi: 10.1007/s12529-016-9551-1. [DOI] [PubMed]
- 28.He L., Liao Q.-Y., Huang Y.-Q., Feng S., Zhuang X.-M. Parents’ perception and their decision on their children’s vaccination against seasonal influenza in Guangzhou. Chin Med J (Engl) 2015;128(03):327–341. doi: 10.4103/0366-6999.150099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wagner A.L., Gordon A., Tallo V.L., et al. Intent to obtain pediatric influenza vaccine among mothers in four middle income countries. Vaccine. 2020;38(27):4325–4335. doi: 10.1016/j.vaccine.2020.04.028. [DOI] [PubMed] [Google Scholar]
- 30.Lin J., Li C., He W. Trends in influenza vaccine uptake before and during the COVID-19 pandemic in the USA. Public Health. Dec 2023;225:291–298. doi: 10.1016/j.puhe.2023.10.028. [DOI] [PubMed] [Google Scholar]
- 31.Ng YMM. A Cross-National Study of Fear Appeal Messages in YouTube Trending Videos About COVID-19. American Behavioral Scientist. 0(0):00027642231155363. doi:10.1177/00027642231155363.
- 32.Stolow J.A., Moses L.M., Lederer A.M., Carter R. How fear appeal approaches in COVID-19 health communication may be harming the global community. Health Educ Behav. 2020;47(4):531–535. doi: 10.1177/1090198120935073. [DOI] [PubMed] [Google Scholar]
- 33.Swami M.K., Gupta T. Psychological impact of fear-based messages in context of COVID 19. Int J Soc Psychiatry. 2021;67(8):1081–1082. doi: 10.1177/0020764020980773. [DOI] [PubMed] [Google Scholar]
- 34.Orenstein EW, ElSayed-Ali O, Kandaswamy S, et al. Evaluation of a Clinical Decision Support Strategy to Increase Seasonal Influenza Vaccination Among Hospitalized Children Before Inpatient Discharge. JAMA Netw Open. Jul 1 2021;4(7):e2117809. doi:10.1001/jamanetworkopen.2021.17809. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.