Abstract
BACKGROUND:
and Objectives: Hypocalcemia is a commonly reported complication after thyroid surgery. Many possible risk factors have been identified. The purpose of this study is to analyze various risk factors possibly associated with development of postoperative hypocalcemia after thyroid surgery by dividing the sample population into postoperative hypocalcemia and normal calcium groups.
DESIGN:
Retrospective
SETTING:
Multiple centers in the Makkah region of Saudi Arabia
PATIENTS AND METHODS:
Risk factors for postoperative hypocalcemia that were obtained for analysis include patient factors, perioperative blood parameters factors, disease-related factors, and surgical factors. Postoperative hypocalcemia was defined as a reduction of the total calcium level to <8.0 mg/dL. Hypocalcemic and normocalcemic patients were compared by multivariate logistic regression.
MAIN OUTCOME MEASURES:
Distinguish independent risk factors for postoperative hypocalcemia after thyroidectomy.
SAMPLE SIZE:
215 patients.
RESULTS:
The incidence of hypocalcemia was 52.1% (112 of 215 patients). According to multivariate analysis, statistically significant risk factors for predicting postoperative hypocalcemia included postoperative parathyroid hormone level <10 pg/dL, inadvertent parathyroid gland resection, and neck dissection surgeries.
CONCLUSION:
The causes of postoperative hypocalcemia are multi-factorial. Because many of these factors are modifiable, they should be identified postoperatively to distinguish high-risk groups and implement early preventive measures.
LIMITATIONS:
Retrospective with a relatively small size. We encourage additional prospective studies with a larger sample size in multiple regions of the country, which might reveal further significant results.
INTRODUCTION
Postoperative hypoparathyroidism leading to hypocalcemia is caused mainly by impairment of the parathyroid gland.1–5 It can lead to severe morbidities affecting patient quality of life and requires serial laboratory test monitoring, prolonged hospitalization, and treatment.4 The incidence of hypocalcemia following surgery varies widely from 1.7% to 68%, though different definitions may be to blame for this variation.3, 6, 7 Hypocalcemia is defined by a total amount of calcium in the blood below the lower limit of the center-specific reference range. If there are signs or symptoms along with it, it is called clinical hypocalcemia.8 Postoperative hypocalcemia is often transient and may be caused by an imbalance between electrolyte levels and hydration, in addition to hypoparathyroidism; however, approximately 10% of patients may develop permanent hypocalcemia.1, 5, 8 Biochemical hypoparathyroidism is defined as a decrease in parathyroid hormone (PTH) level below the minimal normal limit of the laboratory standard (usually 12 pg/mL) along with hypocalcemia.8 Transient or temporary hypoparathyroidism may last up to 6 months after surgery, while permanent or persistent hypoparathyroidism exceeds 6 months.8, 9 The mechanism of hypoparathyroidism depends on the extent of dissection of parathyroid glands or their vascular supply, which is attributed to thermal injury, mechanical injury, or surgical removal. Surgical removal of the parathyroid glands can be intentional or inadvertent.5, 8, 10 The risk for postoperative hypoparathyroidism is associated with extensive bilateral thyroid procedures, central neck dissection, retrosternal goiter, autoimmune thyroid disease, inexperienced surgeon(s), revision surgeries, and malignancy because it tends to be treated aggressively.5, 10–13
Clinical manifestations of hypocalcemia mainly include neurological and cardiac sequelae, which can range from perioral and peripheral paresthesia to muscle cramps, tetany, seizures, prolonged Q-T syndrome, and confusion.13, 14 The purpose of this study was to analyze various risk factors possibly associated with the development of postoperative hypocalcemia after thyroid surgery by dividing the sample population into postoperative hypocalcemia and normal calcium groups.
PATIENTS AND METHODS
This retrospective statistical analysis was performed on patients who underwent total thyroidectomy and completion thyroidectomy in our centers, located in the Makkah region of Saudi Arabia, between 2009 and 2020. The Institutional Review Board of King Abdullah Medical City (KAMC), Makkah, Saudi Arabia, and the National Biomedical Ethics Committee, King Abdulaziz City for Science and Technology (Protocol Number 14-07-1433, Registration Number H-02-K-001) approved this study. Patients requiring unilateral lobectomy or subtotal thyroidectomy were excluded, and only those who underwent total or complete thyroidectomy were enrolled in the study. The protocol for this study required hospitalization of all patients for a minimum of 1 day after surgery to evaluate signs and/or symptoms of hypocalcemia and to perform the required blood tests. Demographic and clinical information, including age, sex, type of surgery, and pathology, were obtained. Biochemical parameters, including pre- and postoperative PTH, pre- and postoperative total calcium, preoperative vitamin D, and preoperative albumin, phosphorus, and magnesium levels, were also measured. Postoperative PTH and calcium were sent twice, at 6 and 12 hours after surgery, and the lowest readings were used in the analysis. The occurrence of any hypocalcemic symptoms and the need for intravenous calcium management after surgery were documented. In this study, biochemical hypocalcemia was defined as a total calcium level <8.0 mg/dL obtained from the lowest reading during the hospital stay; total calcium measurements were all corrected according to albumin. Hypoparathyroidism was defined as a PTH level <10 pg/dL, which was measured at 6 and 12 hours after surgery, and the lowest reading was recorded and included in the study. Patients returned 6 months after surgery, at which time serum calcium and PTH levels were measured. Patients were diagnosed with permanent hypocalcemia when their calcium level persisted to be less than 8 mg/dL at 6 months after surgery. Risk factors were classified and examined according to patient factors, pre- and postoperative biochemical parameters, surgical factors, and disease-related factors.
The data were analyzed using IBM SPSS version 25 (IBM Corporation, Armonk, NY, USA). Discrete variables are displayed as count and percentage, while continuous variables are expressed as mean and standard deviation (SD) when the data were normally distributed by observation of histograms. Percentages were applied for categorical variables as well. Comparisons between hypocalcemic and normocalcemic groups were performed using the Student's t-test, analysis of variance, Kruskal-Wallis test, or Mann-Whitney test according to the data distribution and the number of both groups compared. All variables that were considered risk factors for postoperative hypocalcemia were integrated into a univariate binary logistic regression analysis to identify relative significant risk factors. Then, all significant risk factors associated with postoperative hypocalcemia were integrated into a multivariate logistic regression analysis to distinguish independent risk factors for postoperative hypocalcemia. Using the backward likelihood ratio test, multivariate logistic regression analysis was used to remove variables with P values >0.1. Odds ratios for statistically significant predictors are reported with corresponding 95% confidence intervals.4, 15 Differences with P values <.05 were statistically significant.
RESULTS
Of the 215 patients, 160 (74.7%) were female and 55 (25.6%) were male, with a median (minimum-maximum) age of 45 (13-90) years, and most (74.4%) were <55 years of age. In this study, all patients underwent total removal of the thyroid glands; 190 (88.4%) underwent total thyroidectomy in the same setting, and 25 (11.6%) underwent completion of thyroidectomy (two stages of thyroidectomy). According to the data, postoperative biochemical hypocalcemia (calcium level <8 mg/dL) developed in 112 (52.1%) patients. In the postoperative hypocalcemia group, 66 (58.9%) patients had symptoms of hypocalcemia and were diagnosed with clinical hypocalcemia. Only 4 (3.9%) patients in the normal calcium group had symptoms of hypocalcemia (P<.001) (Table 1).
Table 1.
Postoperative hypocalcemia group and normal calcium level after thyroidectomy.
| Variable | Hypocalcemia (level <8 mg/dL) (n=112, 52.1%) | No hypocalcemia (level ≥8 mg/dL) (n=103, 47.9%) | P value |
|---|---|---|---|
| Age | |||
| <55 years | 87 (77.7) | 73 (70.9) | .253 |
| ≥55 years | 25 (22.3) | 30 (29.1) | |
| Gender | .673 | ||
| Female | 82 (73.2) | 78 (75.7) | |
| Male | 30 (26.8) | 25 (24.3) | |
| Compression symptoms | |||
| Yes | 30 (26.8) | 18 (17.5) | .244 |
| No | 76 (67.9) | 80 (77.7) | |
| PTH (preoperative) | |||
| <10 pg/dL | 1 (.9) | 3 (2.9) | .274 |
| ≥10 pg/dL | 111 (99.1) | 100 (97.1) | |
| Vitamin D level (preoperative) | |||
| <25 ng/dL | 86 (76.8) | 68 (66) | .080 |
| ≥25 ng/dL | 26 (23.2) | 35 (34) | |
| Completion thyroidectomy | |||
| Yes | 8 (7.1) | 17 (16.5) | .032 |
| No | 104 (92.9) | 86 (83.5) | |
| Total thyroidectomy | |||
| Yes | 104 (92.9) | 86 (83.5) | .032 |
| No | 8 (7.1) | 17 (16.5) | |
| Bilateral neck dissection | |||
| Yes | 12 (10.7) | 3 (2.9) | .025 |
| No | 100 (89.3) | 100 (97.1) | |
| Left side neck dissection | |||
| Yes | 5 (4.5) | 2 (1.9) | .298 |
| No | 107 (95.5) | 101 (98.1) | |
| Right side neck dissection | |||
| Yes | 7 (6.3) | 3 (2.9) | .246 |
| No | 105 (93.8) | 100 (97.1) | |
| Malignancy | |||
| Yes | 64 (57.1) | 52 (50.5) | .328 |
| No | 48 (42.9) | 51 (49.5) | |
| Lymphovascular invasion | |||
| Yes | 25 (22.3) | 14 (13.6) | .257 |
| No | 39 (34.8) | 37 (35.9) | |
| Not applicable | 47 (42) | 52 (50.5) | |
| Inadvertent parathyroidectomy | |||
| Yes | 39 (34.8) | 8 (7.8) | .001 |
| No | 73 (65.2) | 95 (92.2) | |
| PTH (Postoperative) | |||
| <10 pg/dL | 77 (68.8) | 24 (23.3) | .001 |
| ≥10 pg/dL | 35 (31.3) | 79 (76.7) | |
| PTH (after 6 months) | |||
| <10 pg/dL (Permanent) | 23 (20.5) | 5 (4.9) | .001 |
| ≥10 pg/dL (Transient) | 89 (79.5) | 98 (95.1) | |
| Calcium (after 6 months) | |||
| <8 mg/dL (Permanent) | 13 (11.6) | 4 (3.9) | .036 |
| ≥8 mg/dL (Transient) | 99 (88.4) | 99 (96.1) | |
| Symptoms of hypocalcemia | |||
| Yes | 66 (58.9) | 4 (3.9) | .001 |
| No | 46 (41.1) | 99 (96.1) | |
| Revision surgery | |||
| Neck dissection | 3 (2.7) | 2 (1.9) | .690 |
| Not applicable | 47 (42) | 49 (47.6) | |
| Not done | 62 (55.4) | 52 (50.5) | |
| Need IV Calcium | |||
| Yes | 24 (21.4) | 2 (1.9) | .001 |
| No | 88 (78.6) | 101 (98.1) | |
| Retrosternal thyroid extension | |||
| Yes | 13 (11.6) | 9 (8.7) | .488 |
| No | 99 (88.4) | 94 (91.3) | |
| Number of parathyroid glands resected | |||
| 0 | 80 (71.4) | 88 (85.4) | .020 |
| 1 | 25 (78.1) | 8 (53.3) | |
| 2 | 7 (21.9) | 6 (40) | |
| 3 | 0 | 1 (6.7) | |
Data are number (percentage).
Most patients were younger than 55 years of age in both groups, and the median age (minimum-maximum) was significantly lower in the hypocalcemia group than in the normal calcium group (Table 2) (P=.025). The number of female patients in each group was similar, which indicates the female gender had no significant effect on postoperative hypocalcemia in the present study.
Table 2.
Postoperative hypocalcemia group versus normal calcium level after thyroidectomy.
| Variables | Hypocalcemia (level <8 mg/dL) n=112 (52.1%) | No hypocalcemia (level ≥8 mg/dL) n=103 (47.9%) | P value |
|---|---|---|---|
| Age | 41 (32–52.7) | 48 (35–55) | .025 |
| Calcium (preoperative) (mg/dL) | 9.0 (8.8–9.4) | 9 (8.7–9.4) | .525 |
| Albumin (preoperative) (gm/dl) | 4 (3.6–4) | 3.7 (3.5–4.0) | .012 |
| PTH (preoperative) (pg/dL) | 55 (34.4–71.7) | 45.50 (32.5–68) | .213 |
| Vitamin D (preoperative) (ng/mL) | 15.8 (11–24) | 17 (11–29.60) | .322 |
| Phosphorus (preoperative) (mg/dL) | 3.6 (2–4.4) | 3.6 (3.1–4.2) | .780 |
| Magnesium (preoperative) (mg/dL) | 0.8 (.7–1.7) | 1.8 (0.8–2.0) | .001 |
| PTH (postoperative) (pg/dL) | 5 (2.0–12.0) | 26 (10–49.8) | .001 |
| PTH (After 6 months) (pg/dL) | 31 (11.3–55.5) | 47 (33.7–68.2) | .005 |
| Calcium (After 6 months) (mg/dL) | 8.7 (8.3–9.0) | 9.10 (8.8–9.4) | .001 |
Data are median (25th–75th percentiles).
In terms of the biochemical blood test results before surgery, patients in the hypocalcemia group had significantly lower median (range) levels of magnesium and higher levels of albumin (Table 2). Preoperative vitamin D levels were similar in both groups, with 71.6% of all patients exhibiting levels suggesting severe deficiency (<25 ng/mL). Of the preoperative PTH estimates, most patients in both groups had normal PTH levels, with no significant difference. Postoperative hypocalcemia patients showed a significant reduction in the median value of postoperative PTH compared to the normal calcium group (Figure 1) and the majority of PTH readings (68.8%) in the hypocalcemia group were less than 10 pg/dL. The median value of preoperative calcium was the same in both groups and did not reveal any significant relation to postoperative hypocalcemia (P=.525).
Figure 1.
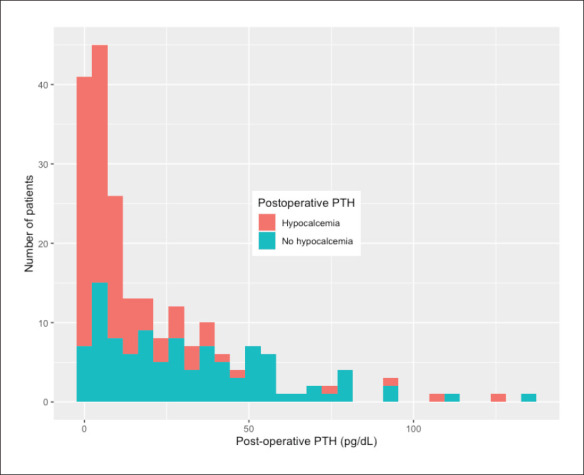
Postoperative PTH patients with and without hypocalcemia.
Regarding surgical factors, patients with low calcium levels after surgery exhibited a higher incidence of parathyroid tissue identified in their pathology report in 39 cases (34.8%; P<.001), suggesting inadvertent removal of parathyroid tissue (Table 1). Most patients who had an inadvertent parathyroidectomy in both groups reported the removal of one parathyroid gland. A significant percentage of patients in the postoperative hypocalcemia group underwent bilateral or unilateral neck dissections (P=.025). The majority of patients underwent total thyroidectomy and showed statistically significant risk for hypocalcemia compared to completion thyroidectomy (P=.032). The frequency of revision surgeries in both groups was low, and the difference was not statistically significant. Disease-related factors, including retrosternal extension (P=.48), compression symptoms (P=.24), lymphovascular invasion (P=.25), and malignancy (P=.32), did not demonstrate an increased risk for postoperative hypocalcemia.
Patients who developed clinical symptoms of hypocalcemia were compared to asymptomatic patients. There were 70 symptomatic patients out of 215, and 94.3% were confirmed to have postoperative biochemical hypocalcemia; the mean of calcium was 7.4 (0.4) mg/dL, P=.001. Postoperative PTH levels were lower in the symptomatic group (6.3 ppg/dL vs. 11.5) and their mean age was younger (41.84 vs. 14.0 years; P=.057]. After 6 months, calcium levels were checked again, and 7.9% of the patients in the whole study developed permanent hypocalcemia. Eleven (15.7%) of those patients were in the symptomatic group and six (4.1%) were in the asymptomatic group. In the temporary postoperative hypocalcemia group, 13 patients (11.6%) developed permanent hypocalcemia, compared to 4 patients (3.9%) in the postoperative normal calcium group. Overall, 26 (12.1%) patients received intravenous calcium for worsening biochemical hypocalcemia, with symptomatic patients more likely to require intravenous calcium (24% versus 6%; P<.001).
Multivariate analysis revealed that postoperative PTH level <10 pg/dL was an independent risk factor for predicting hypocalcemia (OR 5.61 [95% CI 1.76–17.86]; P=.003), the presence of parathyroid glands in the pathology report (OR 0.077 [95% CI 0.008–0.69]; P=.023), and if bilateral neck dissection was performed (OR 0.87 [95% CI 0.099–0.824]; P=.033). Age, gender, malignancy, preoperative vitamin D deficiency, preoperative calcium level <8 mg/dL, preoperative PTH <10 pg/dL, magnesium, and the remainder of the variables were not independently significant in the multivariate analysis (Table 3).
Table 3.
Associations between patient clinical characteristics and postoperative hypocalcemia (dependent variable) by multivariate logistic regression model.
| Variables | OR (95% CI) | P value |
|---|---|---|
| PTH < 10 pg/dL (preoperative) | .000 | .999 |
| PTH < 10 pg/dl (postoperative) | 5.61 (1.76–17.86) | .003 |
| Bilateral neck dissection | .087 (.099–.824) | .033 |
| Inadvertent parathyroidectomy | .077 (.008–.697) | .023 |
| Symptomatic hypocalcaemia | .318 (.080–1.26) | .104 |
DISCUSSION
Despite the precise identification and preservation of the parathyroid glands during thyroidectomy, the most common postoperative complication after thyroid surgery is hypocalcemia. In many studies, post-total thyroidectomy and transient hypocalcemia reached 50%–68%.16, 17 The percentage of temporary biochemical postoperative hypocalcemia in our study was 52%, and permanent hypocalcemia after 6 months was 7.9%. In some studies, postoperative hypocalcemia was classified according to serum calcium level as mild biochemical hypocalcemia (<8.4 and >8.0 mg/dL) or significant hypocalcemia (<8.0 mg/dL or symptomatic).9, 18 In our study, biochemical hypocalcemia was defined as a postoperative serum calcium level <8.0 mg/dL on at least one reading during hospital admission.
Identifying patients in jeopardy for hypocalcemia would enable prophylactic treatment, which would avoid the development of symptomatic hypocalcemia. Thus, for patients who are not in jeopardy, repeated bloodwork can be spared, and the patients can be discharged early without suspicion of developing hypocalcemia. The development of hypocalcemia is associated with hypoparathyroidism and has been considered a predictive factor. Nevertheless, the PTH assay, timing of measurement, and cut-off levels across studies have varied.19 Early postoperative calcium measurement alone is not sufficient to predict the severity of hypocalcemia and the development of permanent hypocalcemia due to the unsynchronized occurrence between hyposecretion of PTH and the subsequent development of biochemical or symptomatic hypocalcemia.8 This results in a delay in the onset of signs and symptoms of hypocalcemia from hours to several days after surgery, and patients may have been discharged from the hospital before finding out that their serum calcium is declining further.1,5,8,18 Multiple studies in the literature have encouraged prophylactic pharmacological support with oral calcium, calcitriol, and magnesium supplements, which can potentially maintain normal levels of calcium in high-risk and asymptomatic patients to prevent postoperative hypocalcemia crisis, thereby avoiding morbidities.1,5,8,19,20
Our data showed that advanced age and gender did not affect postoperative hypocalcemia. Most of the patients in each of the postoperative hypocalcium groups were younger than 55 years old, and the median age of the hypocalcemia group was lower than that of the normal calcium group. A previous study involving 130 patients reported that advanced age was a risk factor for hypocalcemia.21 In a study involving 6519 patients, Torabi et al reported that obesity and older age were remarkably linked with lower rates of hypocalcemia after total thyroidectomy, while female gender was associated with hypocalcemia.22
Our results showed that there was no increased risk for postoperative hypocalcemia in patients with a low preoperative PTH level <10 pg/ml (P=.276) or low preoperative calcium level <8 mg/dL (P=.582). Multiple studies have found that postoperative temporary hypocalcemia develops more often in patients exhibiting a significantly decreased calcium level before surgery.23–25 A meta-analysis of six studies, including 2493 patients, did not show a statistically reliable association between calcium level prior to surgery and the frequency of temporary hypocalcemia.7
PTH measurements taken intraoperatively are frequently recommended for early detection, treatment, and the potential for early discharge. Pattou et al mentioned that an early postoperative PTH level ≤12 pg/mL during a 2-day follow-up was a predictor of hypocalcemia, but did not specify the actual timing when PTH levels were measured after surgery.26 Lombardi et al established better accuracy with measurements performed at 4 hours and 6 hours, with an overall accuracy of 98%.27 Lam and Kerr reported that all patients with a PTH level <8 pg/mL measured 1 hour after the surgery became hypocalcemic, and patients with a PTH level ≥9 pg/mL stayed normal.28 AlQahtani et al demonstrated that PTH assays at 1, 6, and 24 hours postoperatively were good predictors of hypocalcemia, and a decrease in PTH level 1 hour after surgery alone was the earliest predictor of symptomatic hypocalcemia, with a sensitivity of 89% and a negative predictive value of 97%.20 Different low PTH values and time intervals after surgery have been acknowledged depending on the assay and institutions. A systematic overview and meta-analysis by Edafe et al revealed that patients with a decrease in postoperative PTH level from 6 to 35 pg/mL, 1 hour to 1 day following surgery, had a 69% to 100% chance of developing temporary hypocalcemia.7 The American Thyroid Association guidelines adopted a postoperative PTH level of <15 pg/ml, serum calcium level <8.5 mg/dL, or ionized calcium <1.1 mmol/L to be a sign of acute hypoparathyroidism and advised immediate management with oral calcium and calcitriol and serial serum calcium measurements until calcium stability is confirmed.8
Vitamin D deficiency is considered an independent predictor of temporary hypocalcemia despite uncertainty regarding the precision of reported estimates.21, 30, 31 Generally, routine preoperative vitamin D measurement is recommended, especially in high-risk groups such as those with malabsorption, advanced age, obesity and darker skin tones.33 Similar to the results of our study, Ravikumar et al and Chia et al reported that preoperative vitamin D levels were not correlated with postoperative calcium levels, and did not help predict postoperative hypocalcemia; however, Erbil et al reported that preoperative vitamin D levels are a significant predictor of post-thyroidectomy hypocalcemia.21, 32, 33 A meta-analysis by Alhefdhi et al revealed a decline in the rate of symptomatic hypocalcemia in groups treated with vitamin D and calcium supplements compared with no prophylaxis or calcium alone. 34 In cases of elective bilateral thyroid surgery, it may be prudent to delay surgery to correct severe vitamin D deficiency.8
Magnesium plays a necessary role in the secretion of PTH, and its release would be impaired by magnesium deficiency. In a retrospective study of 201 patients, Garrahy et al showed that low postoperative magnesium level was an independent predictor of biochemical hypocalcemia.35 However, a study by Cherian et al showed that there was an association between severe hypocalcemia and hypomagnesemia, but hypomagnesemia (<1.8 mg/dL) was not a risk factor for postoperative hypocalcemia in a prospective analysis of 50 patients who underwent total thyroidectomy.36 In our study, postoperative hypocalcemia patients had lower readings of magnesium compared to normal calcium patients (P<.01) but in the multivariate analysis, magnesium was not a predictive factor for hypocalcemia. Evaluating for hypomagnesemia is recommended and magnesium supplementation with 400 mg of magnesium oxide once or twice daily if serum magnesium level is <1.6 mg/dL in patients with normal renal function should be given, thus facilitating recovery from hypocalcemia.8
Protecting all parathyroid glands during a total thyroidectomy is very important. This can be hard to do because of how bad the thyroid disease is, the need for aggressive treatments, the fact that parathyroid glands are located in different parts of the body, their blood supply, and their general resemblance to other tissues in the neck like thyroid, fat, and lymph nodes.8 Thomusch et al indicated that the greater the number of parathyroid glands found and preserved during surgery, the lower the risk for hypocalcemia.37 In their study, permanent postoperative hypocalcemia was more likely to develop if fewer than two parathyroid glands were identified and preserved during surgery, supporting routine search and identification of parathyroid glands to ensure preservation.37 However, a study by Sheahan et al reported that identification of parathyroid glands during thyroid surgery routinely is not needed. Their results indicate that less than two parathyroid glands identified during thyroidectomy are significantly associated with lower incidence of clinical hypocalcemia compared to three or four parathyroid glands identified, and differences in biochemical hypocalcemia were not significant; moreover, the incidence of inadvertent parathyroidectomy was similar in both groups.38 Factors that would lead to inadvertent parathyroidectomy include extrathyroidal extension of the tumor and central neck dissection.39 According to our data, the incidence of inadvertent resection of parathyroid glands was frequent in the postoperative hypocalcemia group and is considered an independent risk factor.
In many studies, operative factors, such as extensive thyroid surgery and increased operative duration, have demonstrated a significant correlation with postoperative hypoparathyroidism compared with less extensive thyroid procedures.38, 41–43 Longer operative duration usually implies a more complicated procedure, and central neck dissection is commonly associated with advanced thyroid cancer.43 A previous partial thyroid operation creates a potentially increased risk for hypoparathyroidism and hypocalcemia during complete thyroidectomy due to unknown status (presence or viability) of the parathyroid glands in the previously operated neck and the effect of fibrosis and adhesions.8 Sousa et al found that neck dissection was significantly predictive of hypocalcemia but not definitive hypoparathyroidism.44–46 Our data revealed that neck dissection and total thyroidectomy operations were significantly associated with postoperative biochemical and clinical hypocalcemia, and bilateral neck dissection alone was an independent risk factor according to the multivariate analysis. However, revision surgery was not associated with hypocalcemia.
Malignancy has been reported to be a risk factor for hypocalcemia during thyroidectomy.18 In contrast, a study conducted by Eismontas et al found that in cases of malignancy, an increased risk for postoperative hypocalcemia was not demonstrated.19 Our data revealed no similar frequencies of hypocalcemia between benign and malignant pathologies.
In conclusion, a multivariate analysis revealed that inadvertent parathyroid gland excision confirmed by histopathology, bilateral neck dissection, and postoperative hypoparathyroidism <10 pg/dL were statistically significant risk factors and postoperative PTH was the strongest risk factor for postoperative biochemical hypocalcemia. The present study did not reveal a statistical association between preoperative biochemical parameters, including calcium, parathyroid hormone, vitamin D, magnesium and the risk for postoperative hypocalcemia. However, we emphasize the need to diagnose preoperative hypocalcemia, hypomagnesemia and vitamin D deficiency in all patients and initiate appropriate corrective supplementation before surgery. The incidence of hypocalcemia did not increase in association with patient- or disease-related factors. The predictors for postoperative hypocalcemia are multi-factorial and need to be addressed to identify high-risk patients to implement early intervention and prevention of adverse outcomes.
Our study was retrospective, and we encourage further prospective studies in the future with larger sample sizes, and in multiple regions of the country included in the database, which might reveal further significant results.
ACKNOWLEDGMENT
We sincerely acknowledge Ms. Doaa Mohorjy for statistical analysis, and Editage (www.editage.com) for English language.
Funding Statement
Funding: Institute of Consulting Research & Studies, Umm Al-Qura University, Makkah, Saudi Arabia
Footnotes
CONFLICT OF INTEREST: None.
AUTHOR DECLARATION
We declare that this manuscript is original, have never been published, or under the consideration for publication elsewhere (in part or in whole). We also declare that the corresponding author and all the co-authors have actively participated in this manuscript. No Arabic abstract and Arabic article for this manuscript.
ETHICS APPROVAL
The Institutional Review Board of King Abdullah Medical City (KAMC), Makkah, Saudi Arabia, and the National Biomedical Ethics Committee, King Abdulaziz City for Science and Technology (Protocol Number 14-07-1433, Registration Number H-02-K-001) approved this study.
REFERENCES
- 1.Roh JL, Park CI.. Routine oral calcium and vitamin D supplements for prevention of hypocalcemia after total thyroidectomy. Am J Surg. 2006;192(5):675–8. doi: 10.1016/j.amjsurg.2006.03.010 PubMed PMID: 17071205. [DOI] [PubMed] [Google Scholar]
- 2.Wang W, Xia F, Meng C, Zhang Z, Bai N, Li X.. Prediction of permanent hypoparathyroidism by parathyroid hormone and serum calcium 24h after thyroidectomy. Am J Otolaryngol. 2018;39(6):746–50. Epub 2018/09/11. doi: 10.1016/j.amjoto.2018.08.005 PubMed PMID: 30197157. [DOI] [PubMed] [Google Scholar]
- 3.Cannizzaro MA, Okatyeva V, Lo Bianco S, Caruso V, Buffone A.. Hypocalcemia after thyroidectomy: iPTH levels and iPTH decline are predictive? Retrospective cohort study. Ann Med Surg (Lond). 2018;30:42–5. Epub 20180503. doi: 10.1016/j.amsu.2018.04.032 PubMed PMID: 29946457; PubMed Central PMCID: PMC6016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Falch C, Hornig J, Senne M, Braun M, Konigsrainer A, Kirschniak A, et al. Factors predicting hypocalcemia after total thyroidectomy- A retrospective cohort analysis. Int J Surg. 2018;55:46–50. Epub 20180516. doi: 10.1016/j.ijsu.2018.05.014 PubMed PMID: 29777882. [DOI] [PubMed] [Google Scholar]
- 5.Mazotas IG, Yen TWF, Park J, Liu Y, Eastwood DC, Carr AA, et al. A postoperative parathyroid hormone-based algorithm to reduce symptomatic hypocalcemia following completion/total thyroidectomy: A retrospective analysis of 591 patients. Surgery. 2018;164(4):746–53. Epub 20180730. doi: 10.1016/j.surg.2018.04.040 PubMed PMID: 30072256. [DOI] [PubMed] [Google Scholar]
- 6.Wu J, Harrison B.. Hypocalcemia after Thyroidectomy: The Need for Improved Definitions. World Journal of Endocrine Surgery. 2010;2:17–20. doi: doi: 10.5005/jp-journals-10002-1015. [DOI] [Google Scholar]
- 7.Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP.. Systematic review and meta-analysis of predictors of postthyroidectomy hypocalcaemia. Br J Surg. 2014;101(4):307–20. Epub 2014/01/10. doi: 10.1002/bjs.9384 PubMed PMID: 24402815. [DOI] [PubMed] [Google Scholar]
- 8.Orloff LA, Wiseman SM, Bernet VJ, Fahey TJ, 3rd, Shaha AR, Shindo ML, et al. American Thyroid Association Statement on Postoperative Hypoparathyroidism: Diagnosis, Prevention, and Management in Adults. Thyroid. 2018;28(7):830–41. Epub 2018/06/01. doi: 10.1089/thy.2017.0309 PubMed PMID: 29848235. [DOI] [PubMed] [Google Scholar]
- 9.Shoback DM, Bilezikian JP, Costa AG, Dempster D, Dralle H, Khan AA, et al. Presentation of Hypoparathyroidism: Etiologies and Clinical Features. J Clin Endocrinol Metab. 2016;101(6):2300–12. Epub 2016/03/05. doi: 10.1210/jc.2015-3909 PubMed PMID: 26943721. [DOI] [PubMed] [Google Scholar]
- 10.Pesce CE, Shiue Z, Tsai HL, Umbricht CB, Tufano RP, Dackiw AP, et al. Postoperative hypocalcemia after thyroidectomy for Graves' disease. Thyroid. 2010;20(11):1279–83. Epub 2010/10/19. doi: 10.1089/thy.2010.0047 PubMed PMID: 20950255. [DOI] [PubMed] [Google Scholar]
- 11.Shaha AR, Jaffe BM.. Parathyroid preservation during thyroid surgery. Am J Otolaryngol. 1998;19(2):113–7. Epub 1998/04/29. doi: 10.1016/s0196-0709(98)90106-5 PubMed PMID: 9550443. [DOI] [PubMed] [Google Scholar]
- 12.Olson JA, Jr., DeBenedetti MK, Baumann DS, Wells SA, Jr.. Parathyroid autotransplantation during thyroidectomy. Results of longterm follow-up. Ann Surg. 1996;223(5):472–8; discussion 8–80. Epub 1996/05/01. doi: 10.1097/00000658-199605000-00003 PubMed PMID: 8651738; PubMed Central PMCID: PMC1235165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baldassarre RL, Chang DC, Brumund KT, Bouvet M.. Predictors of hypocalcemia after thyroidectomy: results from the nationwide inpatient sample. ISRN Surg. 2012;2012:838614. Epub 2012/07/31. doi: 10.5402/2012/838614 PubMed PMID: 22844618; PubMed Central PMCID: PMC3403163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazotas IG, Wang TS.. The role and timing of parathyroid hormone determination after total thyroidectomy. Gland Surg. 2017;6(Suppl 1):S38–S48. Epub 2018/01/13. doi: 10.21037/gs.2017.09.06 PubMed PMID: 29322021; PubMed Central PMCID: PMC5756748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eismontas V, Slepavicius A, Janusonis V, Zeromskas P, Beisa V, Strupas K, et al. Predictors of postoperative hypocalcemia occurring after a total thyroidectomy: results of prospective multicenter study. BMC Surgery. 2018;18(1):55. doi: doi: 10.1186/s12893-018-0387-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson RB, Erskine C, Crowe PJ.. Hypomagnesemia and hypocalcemia after thyroidectomy: prospective study. World J Surg. 2000;24(6):722–6. Epub 2000/04/25. doi: 10.1007/s002689910116 PubMed PMID: 10773126. [DOI] [PubMed] [Google Scholar]
- 17.Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28(3):271–6. Epub 2004/02/13. doi: 10.1007/s00268-003-6903-1 PubMed PMID: 14961204. [DOI] [PubMed] [Google Scholar]
- 18.Noureldine SI, Genther DJ, Lopez M, Agrawal N, Tufano RP.. Early predictors of hypocalcemia after total thyroidectomy: an analysis of 304 patients using a short-stay monitoring protocol. JAMA Otolaryngol Head Neck Surg. 2014;140(11):1006–13. Epub 2014/10/17. doi: 10.1001/jamaoto.2014.2435 PubMed PMID: 25321339; PubMed Central PMCID: PMC4316663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eismontas V, Slepavicius A, Janusonis V, Zeromskas P, Beisa V, Strupas K, et al. Predictors of postoperative hypocalcemia occurring after a total thyroidectomy: results of prospective multicenter study. BMC Surg. 2018;18(1):55. Epub 2018/08/11. doi: 10.1186/s12893-018-0387-2 PubMed PMID: 30092793; PubMed Central PMCID: PMC6085643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.AlQahtani A, Parsyan A, Payne R, Tabah R.. Parathyroid hormone levels 1 hour after thyroidectomy: an early predictor of postoperative hypocalcemia. Can J Surg. 2014;57(4):237–40. Epub 2014/08/01. doi: 10.1503/cjs.008013 PubMed PMID: 25078927; PubMed Central PMCID: PMC4119114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Erbil Y, Bozbora A, Ozbey N, Issever H, Aral F, Ozarmagan S, et al. Predictive value of age and serum parathormone and vitamin d3 levels for postoperative hypocalcemia after total thyroidectomy for nontoxic multinodular goiter. Arch Surg. 2007;142(12):1182–7. Epub 2007/12/19. doi: 10.1001/archsurg.142.12.1182 PubMed PMID: 18086985. [DOI] [PubMed] [Google Scholar]
- 22.Torabi SJ, Avery JM, Salehi PP, Lee Y.. Risk factors and effects of hypocalcemia prior to discharge following thyroidectomy. Am J Otolaryngol. 2020;41(3):102420. Epub 2020/03/07. doi: 10.1016/j.amjoto.2020.102420 PubMed PMID: 32139087. [DOI] [PubMed] [Google Scholar]
- 23.Lang BH, Yih PC, Ng KK.. A prospective evaluation of quick intraoperative parathyroid hormone assay at the time of skin closure in predicting clinically relevant hypocalcemia after thyroidectomy. World J Surg. 2012;36(6):1300–6. Epub 2012/03/09. doi: 10.1007/s00268-012-1561-9 PubMed PMID: 22399155; PubMed Central PMCID: PMC3348470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sitges-Serra A, Ruiz S, Girvent M, Manjon H, Duenas JP, Sancho JJ.. Outcome of protracted hypoparathyroidism after total thyroidectomy. Br J Surg. 2010;97(11):1687–95. Epub 2010/08/24. doi: 10.1002/bjs.7219 PubMed PMID: 20730856. [DOI] [PubMed] [Google Scholar]
- 25.Moriyama T, Yamashita H, Noguchi S, Takamatsu Y, Ogawa T, Watanabe S, et al. Intraoperative parathyroid hormone assay in patients with Graves' disease for prediction of postoperative tetany. World J Surg. 2005;29(10):1282–7. Epub 2005/09/10. doi: 10.1007/s00268-005-7880-3 PubMed PMID: 16151665. [DOI] [PubMed] [Google Scholar]
- 26.Pattou F, Combemale F, Fabre S, Carnaille B, Decoulx M, Wemeau JL, et al. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg. 1998;22(7):718–24. Epub 1998/06/20. doi: 10.1007/s002689900459 PubMed PMID: 9606288. [DOI] [PubMed] [Google Scholar]
- 27.Lombardi CP, Raffaelli M, Princi P, Santini S, Boscherini M, De Crea C, et al. Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery. 2004;136(6):1236–41. Epub 2005/01/20. doi: 10.1016/j.surg.2004.06.053 PubMed PMID: 15657581. [DOI] [PubMed] [Google Scholar]
- 28.Lam A, Kerr PD.. Parathyroid hormone: an early predictor of postthyroidectomy hypocalcemia. Laryngoscope. 2003;113(12):2196–200. Epub 2003/12/09. doi: 10.1097/00005537-200312000-00029 PubMed PMID: 14660927. [DOI] [PubMed] [Google Scholar]
- 29.Erbil Y, Barbaros U, Temel B, Turkoglu U, Issever H, Bozbora A, et al. The impact of age, vitamin D(3) level, and incidental parathyroidectomy on postoperative hypocalcemia after total or near total thyroidectomy. Am J Surg. 2009;197(4):439–46. Epub 2009/03/28. doi: 10.1016/j.amjsurg.2008.01.032 PubMed PMID: 19324110. [DOI] [PubMed] [Google Scholar]
- 30.Erbil Y, Ozbey NC, Sari S, Unalp HR, Agcaoglu O, Ersoz F, et al. Determinants of postoperative hypocalcemia in vitamin D-deficient Graves' patients after total thyroidectomy. Am J Surg. 2011;201(5):685–91. Epub 2011/05/07. doi: 10.1016/j.amjsurg.2010.04.030 PubMed PMID: 21545922. [DOI] [PubMed] [Google Scholar]
- 31.Pearce SH, Cheetham TD.. Diagnosis and management of vitamin D deficiency. BMJ. 2010;340:b5664. Epub 2010/01/13. doi: 10.1136/bmj.b5664 PubMed PMID: 20064851. [DOI] [PubMed] [Google Scholar]
- 32.Ravikumar K, Sadacharan D, Muthukumar S, Sundarram T, Periyasamy S, Suresh RV.. A Prospective Study on Role of Supplemental Oral Calcium and Vitamin D in Prevention of Postthyroidectomy Hypocalcemia. Indian J Endocrinol Metab. 2017;21(4):498–503. Epub 2017/07/04. doi: 10.4103/ijem.IJEM_402_16 PubMed PMID: 28670529; PubMed Central PMCID: PMC5477433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chia SH, Weisman RA, Tieu D, Kelly C, Dillmann WH, Orloff LA.. Prospective study of perioperative factors predicting hypocalcemia after thyroid and parathyroid surgery. Arch Otolaryngol Head Neck Surg. 2006;132(1):41–5. Epub 2006/01/18. doi: 10.1001/archotol.132.1.41 PubMed PMID: 16415428. [DOI] [PubMed] [Google Scholar]
- 34.Alhefdhi A, Mazeh H, Chen H.. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: a systematic review and meta-analysis. Oncologist. 2013;18(5):533–42. Epub 2013/05/03. doi: 10.1634/theoncologist.2012-0283 PubMed PMID: 23635556; PubMed Central PMCID: PMC3662844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garrahy A, Murphy MS, Sheahan P.. Impact of postoperative magnesium levels on early hypocalcemia and permanent hypoparathyroidism after thyroidectomy. Head Neck. 2016;38(4):613–9. Epub 2014/12/11. doi: 10.1002/hed.23937 PubMed PMID: 25491348. [DOI] [PubMed] [Google Scholar]
- 36.Cherian AJ, Gowri M, Ramakant P, Paul TV, Abraham DT, Paul MJ.. The Role of Magnesium in Post-thyroidectomy Hypocalcemia. World J Surg. 2016;40(4):881–8. Epub 2015/11/19. doi: 10.1007/s00268-015-3347-3 PubMed PMID: 26578317. [DOI] [PubMed] [Google Scholar]
- 37.Thomusch O, Machens A, Sekulla C, Ukkat J, Brauckhoff M, Dralle H.. The impact of surgical technique on postoperative hypoparathyroidism in bilateral thyroid surgery: a multivariate analysis of 5846 consecutive patients. Surgery. 2003;133(2):180–5. Epub 2003/02/28. doi: 10.1067/msy.2003.61 PubMed PMID: 12605179. [DOI] [PubMed] [Google Scholar]
- 38.Sheahan P, Mehanna R, Basheeth N, Murphy MS.. Is systematic identification of all four parathyroid glands necessary during total thyroidectomy?: a prospective study. Laryngoscope. 2013;123(9):2324–8. Epub 2013/06/05. doi: 10.1002/lary.23954 PubMed PMID: 23733535. [DOI] [PubMed] [Google Scholar]
- 39.Sitges-Serra A, Gallego-Otaegui L, Suarez S, Lorente-Poch L, Munne A, Sancho JJ.. Inadvertent parathyroidectomy during total thyroidectomy and central neck dissection for papillary thyroid carcinoma. Surgery. 2017;161(3):712–9. Epub 2016/10/17. doi: 10.1016/j.surg.2016.08.021 PubMed PMID: 27743717. [DOI] [PubMed] [Google Scholar]
- 40.Thompson NW, Olsen WR, Hoffman GL.. The continuing development of the technique of thyroidectomy. Surgery. 1973;73(6):913–27. Epub 1973/06/01. PubMed PMID: 4703492. [PubMed] [Google Scholar]
- 41.Raja M, Natesan M.. Hypocalcemia and its Risk Factors in Post Thyroidectomy – A Prospective Study. International Journal of Contemporary Medicine, Surgery and Radiology. 2019;4. doi: doi: 10.21276/ijcmsr.2019.4.3.21. [DOI]
- 42.Demeester-Mirkine N, Hooghe L, Van Geertruyden J, De Maertelaer V.. Hypocalcemia after thyroidectomy. Arch Surg. 1992;127(7):854–8. Epub 1992/07/01. doi: 10.1001/archsurg.1992.01420070118021 PubMed PMID: 1524486. [DOI] [PubMed] [Google Scholar]
- 43.Friedman M, Kelley K, Maley A.. Central neck dissection. Operative Techniques in Otolaryngology-Head and Neck Surgery. 2011;22(2):169–72. doi: doi: 10.1016/j.otot.2011.04.001. [DOI] [Google Scholar]
- 44.Sousa Ade A, Salles JM, Soares JM, Moraes GM, Carvalho JR, Savassi-Rocha PR.. Predictors factors for post-thyroidectomy hypocalcaemia. Rev Col Bras Cir. 2012;39(6):476–82. Epub 2013/01/26. doi: 10.1590/s0100-69912012000600006 PubMed PMID: 23348643. [DOI] [PubMed] [Google Scholar]
- 45.Alkaff HH, Besharah BO, Bukhari DH, Sayed SI, Alessa MA, Abdelmonim SK, et al. Thyroid neoplasm in Makkah region, Saudi Arabia. A retrospective epidemiological study. Saudi Med J. 2020;41(12):1330–5. doi: 10.15537/smj.2020.12.25575 PubMed PMID: 33294891; PubMed Central PMCID: PMC7841587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al-Herabi AZ. Head and neck oncology experience in Makkah, Saudi Arabia. Saudi Med J. 2009;30(10):1316–22. PubMed PMID: 19838441. [PubMed] [Google Scholar]


