Abstract
Objective
To investigate whether the clinical and radiographical outcomes are affected when four or six implants support the maxillary fixed complete denture (FCD).
Materials and methods
This study was registered on PROSPERO (CRD42021226432) and followed the PRISMA guidelines. The focused PICO question was, "For an edentulous maxillary patient rehabilitated with an implant-supported fixed prosthesis, do the clinical and radiographical outcomes differ when four or six implants support the prosthesis ". A thorough search of the relevant studies was designed and performed electronically. The survival rate of implant and prosthesis, marginal bone loss, and complications (mechanical and biological) were the primary outcomes, whereas implant distribution and using the surgical guide, follow-up, and framework material were evaluated as secondary outcomes.
Results
Out of 1099 articles initially retrieved, 53 clearly stated the outcomes of interest and were included in this study. There were no significant differences in implant and prosthesis survival, technical/mechanical complications, and biological complications between the 4-implant group (4-IG) and the 6-implant group (6-IG). However, marginal bone loss (MBL) was significantly higher in the 4-IG (p < 0.01). The surgical guide and follow-up period did not significantly affect implant/prosthesis survival. Additionally, using the CAD/CAM milled framework and anteroposterior implant distribution were associated with significantly higher implant survival in the 6-IG (p < 0.01).
Conclusion
The findings of this study indicated that having a greater number of implants, as seen in the 6-implant group, can lead to a decrease in technical and biological complications and reduce marginal bone loss. It is worth noting that factors such as using CAD/CAM frameworks and the anteroposterior distribution of implants were recognized as important in improving implant survival rates when more implants are present.
Keywords: Maxilla, Edentulous, Fixed prosthesis, Dental implants, Complications
1. Introduction
The continuous evolution of surgical and restorative protocols in implant dentistry allowed early predictability and immediate treatments for patients with a growing scientific background [[1], [2], [3]]. However, the consensus regarding the optimal number of implants per edentulous arch remains absent in the literature [[4], [5], [6], [7]]. In the maxilla, due to poor bone quality, inadequate bone volume, and maxillary sinus pneumatization, placing an adequate number of implants in the ideal location to support a fixed complete denture (FCD) is more challenging [8]. As a result, numerous techniques have been developed to address the challenges in atrophic maxilla, including using tilted implants and distal cantilevers to optimize the use of existing bone and minimize patient morbidity by avoiding bone grafting [9,10]. Using short implants also appears to be a reliable and safe procedure when done under tight clinical guidelines [11]. Placing implants in anatomical locations such as the tuberosity, pterygomaxillary, and zygoma has emerged as an alternative approach [12,13]. However, this necessitates complex surgical and prosthetic procedures and carries a higher risk of morbidity and soft-tissue complications [14]. Additionally, maxillary sinus floor augmentation (MSFA) has proven to be a successful and predictable procedure for facilitating implant placement in the posterior atrophic maxilla without compromising the inter-arch distance, with success rates exceeding 90% [[15], [16], [17]].
A significant discrepancy in the literature exists regarding the optimal number of implants for full-arch maxillary prosthesis, with some sources recommending six to ten implants [18], others advocating for eight implants in segmented full-arch restorations [19], or six implants arranged in a parallel configuration [20], while some argue that as few as four implants are sufficient [21].
The influence of the number of implants on marginal bone loss (MBL) has been rarely discussed in the literature. Passoni et al. [22] observed more significant bone loss and the prevalence of peri-implantitis for implant-supported fixed complete denture prosthesis (ISFCDP) in the group of >5 implants compared to the group of ≤5 implants. On the other hand, de Luna Gomes et al. [7] did not find a clinically significant difference in MBL between >4 and <5 implant groups per jaw. To the author's knowledge, only two randomized clinical trials (RCTs) compared the MBL between 4 and 6 implant groups in maxillary FCDs [23,24], and both trials reported no statistical difference between groups. The anteroposterior distribution of the implants could play a role in implant and prosthesis survival and technical complications [4,5,25]. However, according to Daudt Polido et al. [6],there is no significant difference in implant and prosthesis survival between the different implant distributions.
In complete-arch prostheses, when a fewer number of supporting implants (less than 5 implants) is adopted, the presence of distal cantilevers of different lengths (>15 mm in the mandible and >10 mm in the maxilla), depending on the distribution of implants, may be inevitable [26]. Some clinical and biomechanical studies reported that the presence of a distal cantilever could increase the risk of mechanical complications in the prostheses [26,27]; however, recent studies did not find a relationship between the length of the cantilever and the number of implants, MBL, or prosthesis-related complications [23,28,29]. The incidence of biological and technical complications concerning the number of implants in ISFCDPs were addressed in two studies [5,7]. de Luna Gomes et al. [7] reported a lower complication rate in the <5 implants group than the >4 implants group with no significant difference. On the other hand, Heydecke et al. [5] found that most of the studies they reviewed showed survival and complication rates for full arch fixed dental prostheses (FAFDPs) supported by four to six implants without discussing the distribution of implants or the number of reconstructions supported by four, five, or six implants.
The ideal number of implants for maxillary rehabilitation with fixed prostheses remains a topic of debate in the literature [[5], [6], [7]]. Some studies advocate using six implants, believing it improves prosthesis support and overall success [[30], [31], [32], [33], [34]]. Conversely, others argue that four implants are sufficient to avoid potential challenges in maintaining oral health and prevent complications [[35], [36], [37], [38]]. However, literature comparing the effects of using four or six implants on peri-implant health and prosthetic complications in the edentulous maxilla is scarce, with a lack of systematic reviews directly comparing these approaches. Thus, the primary goal of this systematic review and meta-analysis was to evaluate the implant and prosthesis survival, MBL, and the incidence of technical/mechanical and biological complications in maxillary FCDs supported by four implants (4-IG) compared with six implants (6-IG). The secondary goal was to analyze the effect of the follow-up period, surgical guide, framework design, and anteroposterior implant distribution on implant/prosthesis survival in both groups (4-IG and 6-IG). The research hypothesis was that clinical and radiographical outcomes are not affected whether four or six implants support the maxillary fixed complete denture prosthesis.
2. Materials and methods
The review was performed according to the PRISMA 2020 guidelines [39] (Appendix 1). The protocol of this systematic review was registered on PROSPERO (CRD42022322074).
2.1. PICOS question
The focused question was formatted according to the PICOS [40] framework: "For the maxillary edentulous patient rehabilitated with an implant-supported fixed complete prosthesis, do clinical and radiographical outcomes differ between four compared with six supporting implants."
-
•
Population (P): Maxillary edentulous patient.
-
•
Intervention (I): Four or six implant-supported fixed complete prosthesis.
-
•
Comparison (C): Four versus six implants
-
•
Outcomes (O): Clinical and radiographical outcomes.
-
•
Study design (S): Randomized clinical trials (RCTs) and nonRCTs (NRCTs). There were no restrictions to the type of study.
The primary outcomes measured were the survival rate of implant and prosthesis, marginal bone loss, and complications (mechanical and biological). In contrast, the distribution of implants and use of the surgical guide, follow-up period, and framework material were evaluated as secondary outcomes.
2.2. Eligibility criteria
Inclusion and exclusion criteria.
-
1.
Studies on healthy individuals with the completely edentulous maxilla rehabilitated by four or six implants.
-
2.
Clearly state four or six implants in the maxilla.
-
3.
Studies with ten patients (at least) with a minimum follow-up period of one year.
-
4.
Studies provide at least information on implant/prosthesis survival and other outcomes: radiographic marginal bone level and implant/prosthetic complication.
Tilted implants, graft cases, randomized clinical trials, and prospective and retrospective studies were included as long as they fulfilled the abovementioned criteria.
There is no limitation regarding prosthesis type or loading protocol (immediate, early, or delayed). Zygomatic implants, animal, in vitro studies, and single case reports were excluded, and the results were limited to English.
2.3. Search strategy
An electronic search for literature was conducted using MEDLINE (PubMed), Embase, Cochrane Library, and Web of Science databases. The search was updated on February 14. 2022, and the articles published in English - from each database inception date were identified (Appendix 2). The electronic search was further supplemented by a manual search of the last five years of relevant dental journals (Journal of Prosthodontics, Journal of Prosthetic Dentistry, International Journal of Oral & Maxillofacial Implants, International Journal of Prosthodontics, Implant Dentistry, Clinical Implant Dentistry and Related Research and Clinical Oral Implants Research) and bibliographies of the relevant studies.
2.4. Data extraction
The two reviewers (M.A.Sh., S.W.) independently screened the title and abstract and performed a full-text assessment. The data were extracted and tabled based on first author, year of publication, study design, number of maxillary arches, the total number of implants, the position of implants per arch, type of implants (manufacturer), mean follow-up, survival of implants, survival of prosthesis, using of surgical guide, marginal bone loss, technical/mechanical complication, and biological complications. The data for the included implants (four or six) in the maxilla were extracted from each study. In case of disagreement, the third author (M.A.M.) was consulted.
2.5. Risk of bias assessment
The risk of bias assessment for the included RCTs was assessed through the Cochrane Risk of Bias Tool [41]. For non-RCTs (retrospective and prospective studies), the risk of assessment was assessed using RoB-1 Tool [42]. The two reviewers assessed the risk of bias (M.A.Sh., O.H.).
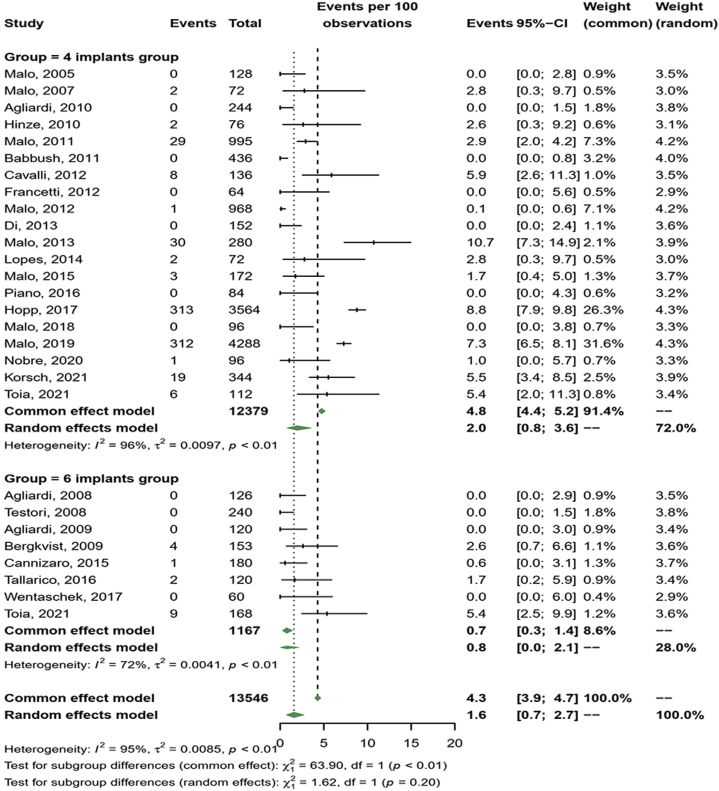
2.6. Statistical analysis
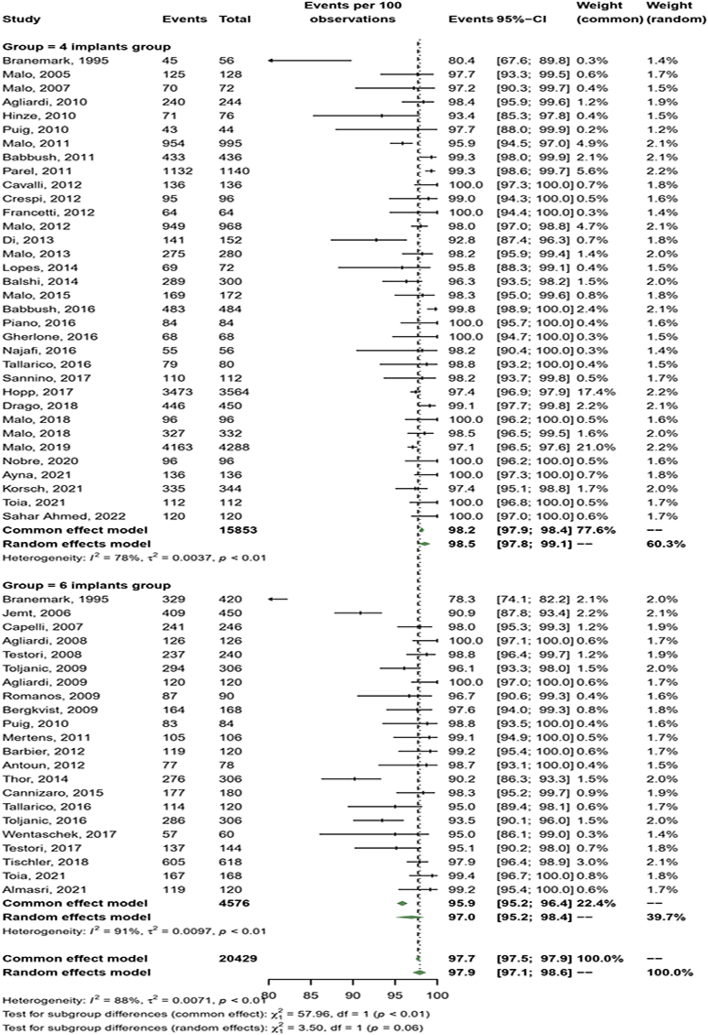
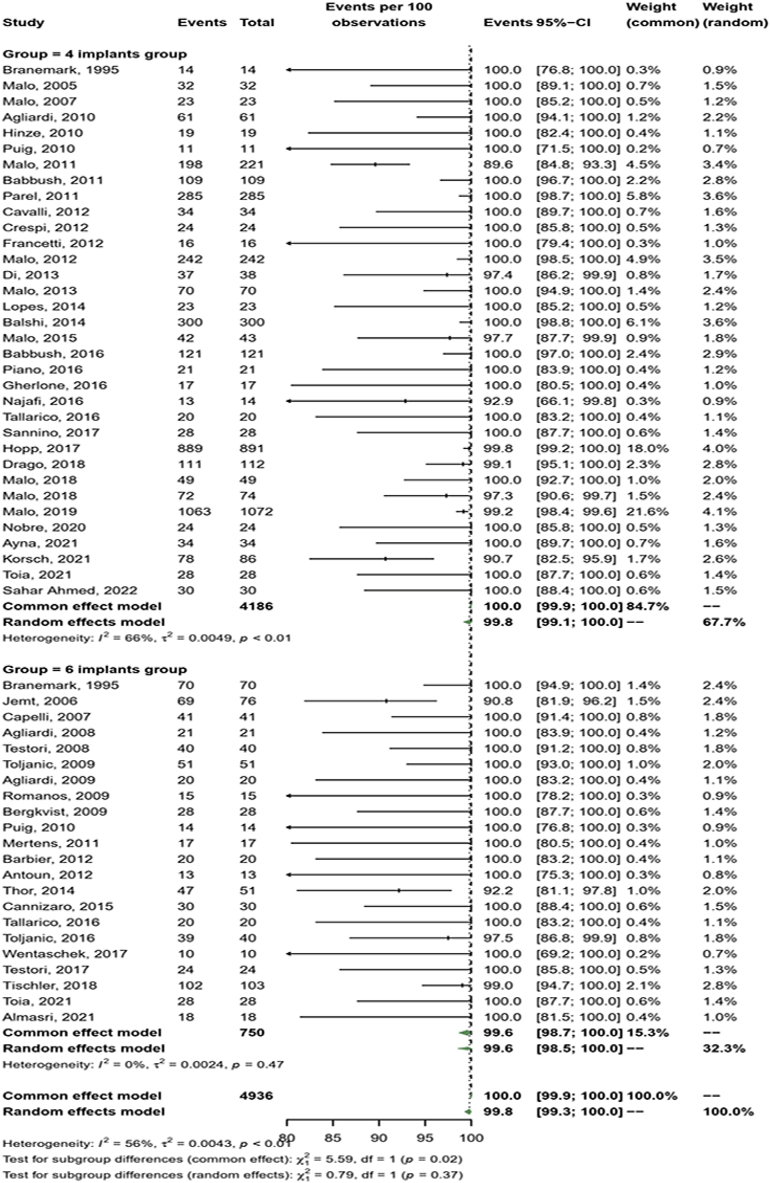
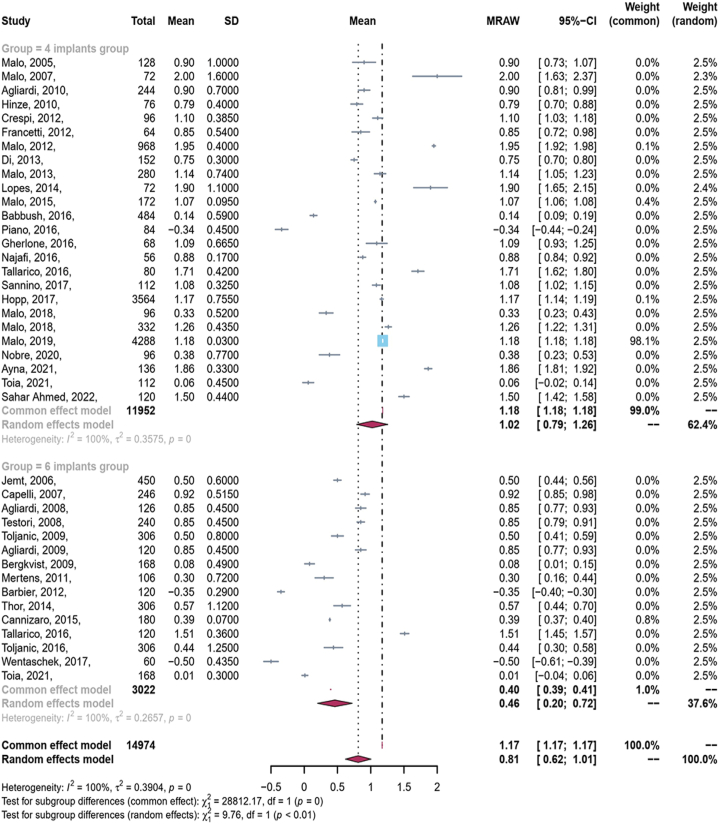
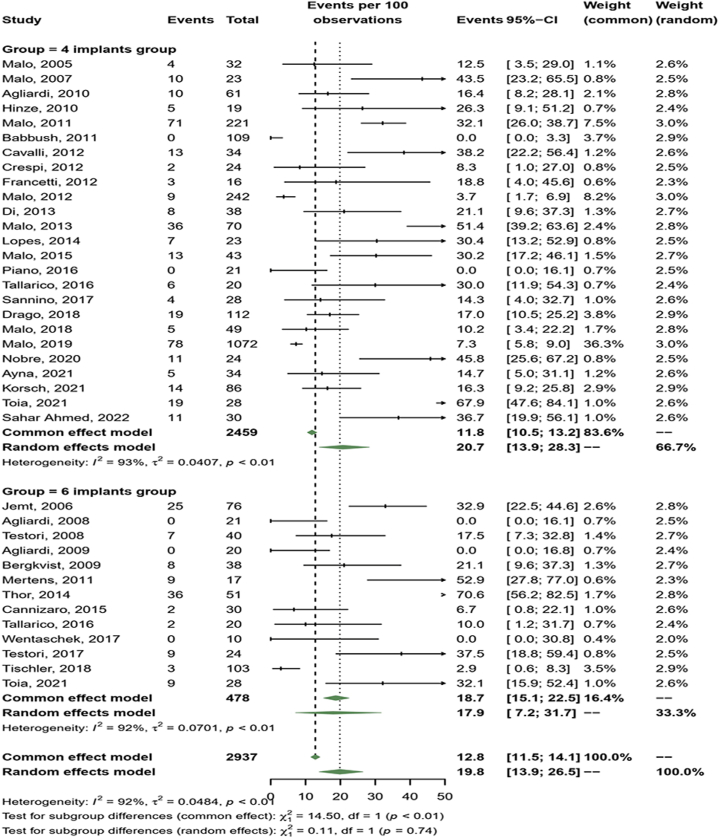
Each study's outcomes were divided by the total number of implants. The event occurrence rate (implant survival, prosthesis survival, biological complication, and mechanical complication; dichotomous outcomes) was calculated with a 95% confidence interval utilizing a computer program metaprop (R version 4.2.1, meta). The marginal bone loss (continuous variables) difference was calculated using meta mean with a 95 % confidence interval (R version 4.2.1; metaphor). Cochran's Q-statistic and the I2 statistic model were performed to assess the heterogeneity. The random-effects model was adopted considering the high heterogeneity of the selected studies (I2 >50 %). Forest plots were generated for visualization (R version 4.2.1, metaphor), with P values < 0.05 considered a significant difference (Fig. 2, Fig. 3, Fig. 4, Fig. 5). In addition, Subgroup analysis was performed to assess intra-group differences concerning follow-up years, use of a surgical guide, framework (Milled or casted), and implant distribution utilizing metaprop (R version 4.2.1, meta). The results were documented, with P values < 0.05 considered a significant difference.
Fig. 2.
Meta-analysis forest plot—implants survival 4-IG & 6-IG.
Fig. 3.
Meta-analysis forest plot—prosthesis survival 4-IG & 6-IG.
Fig. 4.
Meta-analysis forest plot— marginal bone loss 4-IG & 6-IG.
Fig. 5.
Meta-analysis forest plot— Technical/mechanical complications 4-IG & 6-IG.
3. Results
3.1. Search strategy
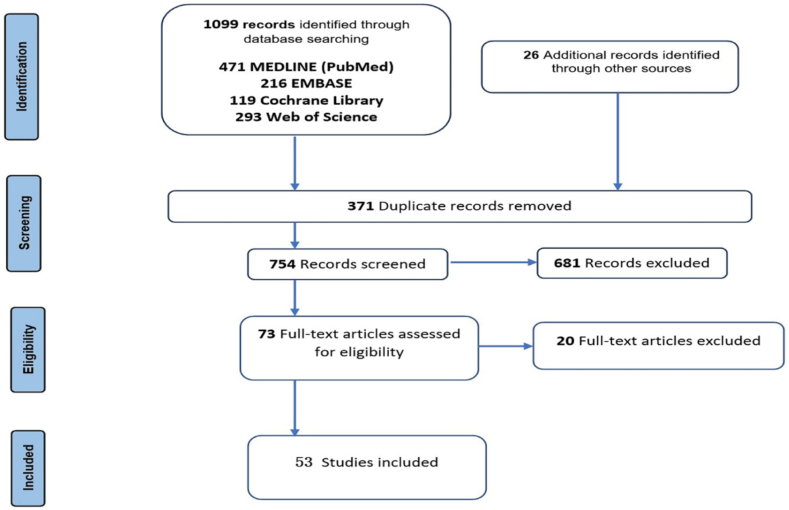
A comprehensive search across various databases yielded a total of 1099 articles, with 471 from MEDLINE (PubMed), 216 from EMBASE, 119 from the Cochrane Library, and 293 from Web of Science. Additionally, 26 articles were identified through relevant bibliography and other sources. After removing duplicates, a total of 754 titles and abstracts underwent screening, resulting in the exclusion of 681 articles. Consequently, 73 studies were eligible for full-text assessment. Following the application of inclusion and exclusion criteria, 53 articles were deemed suitable for inclusion (Fig. 1). The majority of exclusions during the initial screening of titles and abstracts were attributed to various reasons, such as partial edentulism, study sample sizes of fewer than 10 patients, overdenture, the use of zygomatic implants, and a focus on reporting outcomes exclusively for mandibular implant. Simultaneously, the primary reason for excluding studies during full-text assessment was the failure to report outcomes separately for four and/or six implants, with these studies presenting results for the total number of included implants.
Fig. 1.
PRISMA flowchart.
3.2. Risk of bias of selected studies
The three included RCTs were assessed with a low risk of bias (Table 1). Two RCTs compared groups with four versus six implants in the maxilla [23,24], while the third included six implants in the maxilla and four in the mandible [43]. The risk of bias assessment for the remaining non-RCTs (29 retrospective and 21 prospective) is detailed in Table 2. Five studies were assessed with low risk, 38 with moderate risk, and six with a serious risk of bias.
Table 1.
The risk of bise assessment for the included RCTs (COCHRANE Tool).
| First author (year) | Random sequence generation (Selection bias) | Blinding of participants and personnel (Performance bias) | Blinding of outcome assessment (Detection bias) | Incomplete outcome data (Attrition bias) | Selective reporting (Reporting bias) | Other sources of bias | Overall risk of bias |
|---|---|---|---|---|---|---|---|
| Cannizaro 2015 | low | low | low | low | unclear | NI | low |
| Tallarico 2016 | low | low | low | low | low | NI | low |
| Toia 2021 | low | low | low | low | unclear | NI | low |
NI: No information.
Table 2.
The risk of bise assessment for the included non-RCTs (RoB-1 Tool).
| First author (year) | Confounding | Selection of participants | Classification of interventions | Deviation from intended interventions | Missing data | Measurements of outcomes | Selection of reported results | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|
| Drago 2018 | M | M | M | M | M | M | M | M |
| Babbush 2016 | M | M | M | L | L | M | M | M |
| Lopes 2016 | M | M | M | L | M | M | M | M |
| Maló 2011 | M | M | M | M | M | M | M | M |
| Balshi 2014 | M | M | M | M | M | M | M | M |
| Piano 2016 | M | M | M | M | M | M | M | M |
| Ayna 2021 | M | M | M | M | M | M | M | M |
| Maló 2018 | M | M | M | M | M | M | M | M |
| Cavalli 2012 | M | M | M | M | M | M | M | M |
| Malo 2007 | M | M | M | M | M | M | M | M |
| Crespi 2012 | M | S | M | M | S | S | S | S |
| Babbush 2011 | M | M | M | M | M | M | M | M |
| Sannino 2017 | M | M | M | M | M | M | M | M |
| Di 2013 | M | M | M | M | M | M | M | M |
| Maló 2005 | M | M | M | M | M | M | M | M |
| Francetti 2012 | M | M | M | M | M | M | M | M |
| Maló 2019 | M | M | M | M | M | M | M | M |
| Agliardi 2010 | M | M | L | L | L | L | M | L |
| S. Ahmed 2022 | M | M | M | M | M | M | M | M |
| Hopp 2017 | M | M | M | M | M | M | M | M |
| Malo 2013 | M | M | M | M | M | M | M | M |
| Malo 2018 | M | M | L | L | L | L | L | L |
| Nobre 2020 | M | S | M | M | S | M | M | S |
| Hinze 2010 | M | M | M | M | M | M | M | M |
| Korsch 2021 | M | M | M | M | M | M | M | M |
| Maló 2012 | M | M | M | M | M | M | M | M |
| Malo 2015 | M | M | M | M | M | M | M | M |
| Parel 2011 | M | M | M | M | M | M | M | M |
| Gherlone 2016 | S | M | M | M | M | S | S | S |
| Najafi 2016 | M | M | S | M | S | S | S | S |
|---|---|---|---|---|---|---|---|---|
| Brånemark 1995 | M | S | M | M | M | M | S | M |
| Puig 2010 | M | M | M | M | M | M | M | M |
| Toljanic 2016 | M | M | M | M | M | M | M | M |
| Mertens 2011 | M | M | M | M | M | M | M | M |
| Barbier 2012 | M | M | L | M | M | M | M | M |
| Tischler 2018 | M | M | M | M | M | M | M | M |
| Wentaschek 2017 | M | M | L | L | L | L | M | L |
| Thor 2014 | M | M | M | M | M | M | M | M |
| Almasri 2021 | M | M | M | M | M | M | M | M |
| Testori 2017 | M | M | M | M | M | M | M | M |
| Jemt 2006 | S | S | S | M | S | M | M | S |
| Agliardi 2008 | M | M | M | L | L | M | M | M |
| Agliardi 2009 | M | M | L | L | M | M | L | M |
| Capelli 2007 | M | M | M | S | M | M | M | S |
| Testori 2008 | M | M | M | M | M | M | M | M |
| Antoun 2012 | M | M | L | L | L | M | M | L |
| Romanos 2009 | M | M | M | M | M | M | S | M |
| Bergkvist 2009 | M | M | L | L | M | L | L | L |
| Toljanic 2016 | M | M | M | M | M | M | M | M |
| Mertens 2012 | M | M | M | M | M | M | M | M |
L: Low Risk, M: Medium Risk, S: serious Risk.
3.3. Study characteristics
The data extracted from the studies are summarized in Table 3. A total of 57 groups of patients were identified from 53 studies. Thirty studies provided information on four implants [21,27,28,[35], [36], [37], [38],[44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66]], with 17 involving both arches [28,44,47,50,51,53,[55], [56], [57],[59], [60], [61], [62], [63],66] and 13 focusing on the maxilla [21,27,[35], [36], [37], [38],48,49,52,54,58,64,65]). Nineteen studies reported outcomes for six implants [[30], [31], [32],34,43,[67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80]], including five in both arches [32,43,68,77,80] and 14 in maxilla [31,32,34,67,[69], [70], [71], [72], [73], [74], [75], [76],79,80]). Additionally, four studies reported outcomes for both four and six implants [20,23,24,81].
Table 3.
Data extracted from the studies.
| First author | Year | Study design | No. of Impt./max. | No. of max. arches | Total No. of Impt. | Position of Impt. per arch |
Implant system | Mean Follow up (y) | Surgical guide using |
Impt. Surv. (No.) | Impt. Surv. (%) | Prosth. Surv. (No.) |
Prosth. Surv. (%) |
Mean MBL (mm) | Fram. | Tech. & mech. Comp./Prosth. No. | Bio. Comp./Impt. No. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brånemark [20] | 1995 | Retro | 4 | 14 | 56 | Parallel | Brånemark | 10 | NR | 45 | 80.30 | 14 | 100 | NR | NR | NR | NR |
| Maló [9] | 2005 | Retro | 4 | 32 | 128 | 2 Ant. axial/2 Post. tilted | Nobel MKIII/MKIV TiUnite | 1 | No | 125 | 97.60 | 32 | 100 | 0.9 ± 1.0 | NR | 4/32 | 0/128 |
| Malo [45] | 2007 | Retro | 4 | 18 | 72 | 2 Ant. axial/2 Post. tilted | NobelSpeedy | 1.1 | Yes | 70 | 97.20 | 23 | 100 | 2.0 ± 1.6 | Cast | 10/23 | 3/72 |
| Agliardi [46] | 2010 | Pros | 4 | 61 | 244 | 2 Ant. axial/2 Post. tilted | Nobel MKIV/Groovy | 2.6 | No | 240 | 98.36 | 61 | 100 | 0.9 ± 0.7 | Milled | 10/61 | 0/244 |
| Hinze [47] | 2010 | Pros | 4 | 19 | 76 | 2 Ant. axial/2 Post. tilted | Nanotite Tapered (Biomet 3i) | 1 | No | 71 | 96.60 | 19 | 100 | 0.79 ± 0.4 | Cast | 5/19 | 2/76 |
| Puig [82] | 2010 | Retro | 4 | 11 | 44 | 2 Ant. axial/2 Post. tilted | Nobel Speedy Groovy/MK III Groovy | 1 | Yes | 11 | 78.30 | 43 | 98.50 | NR | Milled | 8/30 | 3/30 |
| Maló [27] | 2011 | Pros | 4 | 221 | 995 | 2 Ant. axial/2 Post. tilted | Nobel Biocare | 5 | Yes | 954 | 95.80 | 198 | 98.60 | NR | Milled | 71/221 | 29/995 |
| Babbush [48] | 2011 | Retro | 4 | 109 | 436 | 2 Ant. axial/2 Post. tilted | NobelActive | 1 | Yes | 433 | 99.30 | 109 | 100 | NR | Milled | 0/109 | 0/436 |
| Parel [49] | 2011 | Retro | 4 | 285 | 1140 | 2 Ant. axial/2 Post. tilted | Nobel Active | 2.7 | No | 1132 | 99.30 | 285 | 100 | NR | NR | NR | NR |
| Cavalli [50] | 2012 | Retro | 4 | 34 | 136 | 2 Ant. axial/2 Post. tilted | Nobel MKIV/Groovy | 3.2 | No | 136 | 100 | 34 | 100 | NR | Milled | 13/34 | 8/136 |
| Crespi [51] | 2012 | Pros | 4 | 24 | 96 | 2 Ant. axial/2 Post. tilted | PAD Sweden-Martina | 3 | No | 95 | 98.96 | 24 | 100 | 1.10 ± 0.39 | Cast | 2/26 | NR |
| Francetti [52] | 2012 | Pros | 4 | 16 | 64 | 2 Ant. axial/2 Post. tilted | Brånemark MK IV, NobelSpeedy Groovy | 2.8 | Yes | 64 | 100 | 16 | 100 | 0.85 ± 0.54 | Milled | 3/16 | 0/64 |
| Maló [53] | 2012 | Retro | 4 | 242 | 698 | 2 Ant. axial/2 Post. tilted | Brånemark/Nobel Speedy Groovy | 6.6 | Yes | 949 | 98 | 242 | 100 | 1.95 ± 0.4 | Milled | 9/242 | 1/698 |
| Di [54] | 2013 | Retro | 4 | 38 | 152 | 2 Ant. axial/2 Post. tilted | Brånemark/Nobel Speedy Groovy | 2.8 | No | 141 | 92.80 | 37 | 96.50 | 0.75 ± 0.30 | Cast | 8/68 | 0/152 |
| Malo [55] | 2013 | Retro | 4 | 70 | 280 | 2 Ant. axial/2 Post. tilted | Nobel- Speedy Replace | 3 | No | 275 | 98.21 | 70 | 100 | 1.14 ± 0.74 | Milled | 36/70 | 30/280 |
| Lopes [56] | 2014 | Pros | 4 | 18 | 72 | 2 Ant. axial/2 Post. tilted | NobelSpeedy Groovy | 5 | Yes | 69 | 96.60 | 23 | 100 | 1.9 ± 1.1 | Milled | 7/23 | 2/27 |
| Balshi [57] | 2014 | Retro | 4 | 75 | 300 | 2 Ant. axial/2 Post. tilted | Nobel | 2.2 | NR | 289 | 96.30 | 300 | 100 | NR | Milled | NR | NR |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Malo [35] | 2015 | Retro | 4 | 43 | 172 | 2 Ant. axial/2 Post. tilted | Nobel Speedy Groovy/Shorty | 3 | No | 169 | 95.70 | 42 | 97.70 | 1.07 ± 0.09 | Milled | 13/43 | 3/172 |
| Babbush [58] | 2016 | Retro | 4 | 121 | 484 | 2 Ant. axial/2 Post. tilted | Nobel Active | 1.3 | Yes | 483 | 99.80 | 121 | 100 | 0.14 ± 0.59 | Milled | NR | NR |
| Piano [59] | 2016 | Pros | 4 | 21 | 84 | 2 Ant. axial/2 Post. tilted | Straumann SLActive Bone-Level | 2 | Yes | 84 | 100 | 21 | 100 | −0.34 ± −0.45 | Milled | 0/21 | 0/84 |
| Gherlone [60] | 2016 | Pros | 4 | 17 | 68 | 2 Ant. axial/2 Post. tilted | IDI Evolution | 1 | No | 68 | 100 | 17 | 100 | 1.09 ± 0.66 | Milled | NR | NR |
| Najafi [61] | 2016 | Pros | 4 | 14 | 56 | 2 axial, 2 tilted | Nobel | 3 | No | 55 | 98.21 | 13 | 92.86 | 0.88 ± 0.17 | Cast | NR | NR |
| Tallarico [24] | 2016 | RCT | 4 | 20 | 80 | 2 Ant. axial/2 Post. tilted | NobelSpeedy Groovy implants | 5.3 | Yes | 79 | 98.75 | 20 | 100 | 1.71 ± 0.42 | NR | 6/20 | 3/80 |
| Sannino [62] | 2017 | Retro | 4 | 28 | 112 | 2 Ant. axial/2 Post. tilted | TTx, WINSIX, Biosafin | 2 | Yes | 110 | 99.19 | 28 | 100 | 1.08 ± 0.33 | Milled | 4/28 | NR |
| Hopp [36] | 2017 | Retro | 4 | 891 | 3564 | 2 Ant. axial/2 Post. tilted | NobeSpeedy groovy/Brånemark Mk | 5 | Yes | 3473 | 96 | 889 | 99.80 | 1.17 ± 0.75 | Milled | NR | 313/3564 |
| Drago [28] | 2018 | Retro | 4 | 112 | 448 | 2 Ant. axial/2 Post. tilted | NobelActive | 4 | NP | 446 | 99.10 | 111 | 99 | NR | Milled | 18/111 | NR |
| Maló [37] | 2018 | Pros | 4 | 24 | 96 | 2 Ant. axial/2 Post. tilted | Nobelspeedy | 1 | NR | 196 | 100 | 49 | 100 | 0.33 ± 0.52 | NR | 5/49 | 0/96 |
| Malo [63] | 2018 | Retro | 4 | 83 | 332 | 2 Ant. axial/2 Post. tilted | NobelSpeedy Groovy | 2.5 | Yes | 227 | 97.80 | 72 | 97.60 | 1.26 ± 0.43 | Cast | NR | NR |
| Maló [38] | 2019 | Retro | 4 | 1072 | 4288 | 2 Ant. axial/2 Post. tilted | Brånemark MKIII, IV/Nobel Groovy | 13 | Yes | 4163 | 94.70 | 1063 | 99.20 | 1.18 ± 0.03 | Milled | 78/1072 | 312/4288 |
| Nobre [64] | 2020 | Pros | 4 | 24 | 96 | 2 Ant. axial/2 Post. tilted | Nobelspeedy | 3 | NR | 96 | 100 | 24 | 100 | 0.38 ± 0.77 | NA | 11/24 | 1/69 |
| Ayna [65] | 2021 | Retro | 4 | 34 | 136 | 2 Ant. axial/2 Post. tilted | Nobel | 6 | Yes | 136 | 100 | 34 | 100 | 1.86 ± 0.33 | Milled | 5/34 | NR |
| Korsch [66] | 2021 | Retro cohort study | 4 | 86 | 344 | 2 Ant. axial/2 Post. tilted | Nobel Biocare Active | 2 | Yes | 335 | 97.38 | 78 | 90.70 | NR | Milled | 14/86 | 19/344 |
| Toia [23] | 2021 | RCT | 4 | 28 | 112 | 2 Ant. axial/2 Post. tilted | Astra OsseoSpeed | 3 | No | 112 | 100 | 28 | 100 | 0.06 ± 0.45 | Milled | 19/28 | 6/112 |
| Sahar Ahmed [66] | 2022 | Pros | 4 | 30 | 120 | 2 Ant. axial/2 Post. tilted | Dentaurum | 3 | Yes | 120 | 100 | 30 | 100 | 1.50 ± 0.44 | Cast | 11/30 | NR |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brånemark [20] | 1995 | Retro | 6 | 70 | 420 | Parallel | Brånemark | 10 | NR | 329 | 78.30 | 70 | 100 | NR | NR | NR | NR |
| Jemt [67] | 2006 | Retro | 6 | 76 | 450 | Parallel | Brånemark | 15 | No | 409 | 90.90 | 69 | 90.60 | 0.50 ± 0.60 | NR | 25/76 | 6/76 max, mand. |
| Capelli [68] | 2007 | Retro | 6 | 41 | 246 | 4 Ant. axial/2 Post. tilted | 3i Osseotite NT | 1.8 | No | 241 | 97.59 | 41 | 100 | 0.92 ± 0.52 | Cast | NR | NR |
| Agliardi [96] | 2008 | Pros | 6 | 21 | 126 | Tilted V-II-V | Nobel MKIV/Groovy | 1.6 | NR | 121 | 100 | 21 | 100 | 0.85 ± 0.45 | NR | 0/21 | 0/126 |
| Testori [70] | 2008 | Pros | 6 | 40 | 240 | 4 Ant. axial/2 Post. tilted | 3i Osseotite NT | 1 | No | 237 | 98.80 | 40 | 100 | 0.85 ± 0.45 | Cast | 7/40 | 0/240 |
| Toljanic [71] | 2009 | Pros | 6 | 51 | 306 | 4 Ant. axial/2 Post. tilted | Astra OsseoSpeed | 1 | No | 294 | 96 | 51 | 100 | 0.50 ± 0.80 | Cast | NR | NR |
| Agliardi [72] | 2009 | Pros | 6 | 20 | 120 | Tilted V-II-V | Nobel MKIV/Groovy | 2.3 | No | 120 | 100 | 20 | 100 | 0.85 ± 0.45 | Milled | 0/20 | 0/120 |
| Romanos [73] | 2009 | Retro | 6 | 15 | 90 | Parallel | Ankylos | 3.6 | Yes | 87 | 96.67 | 15 | 100 | NR | Cast | NR | NR |
| Bergkvist [74] | 2009 | Pros | 6 | 28 | 168 | Parallel | Straumann STL | 2.6 | No | 150 | 98.04 | 38 | 100 | 0.08 ± 0.49 | NR | 8/38 | 4/168 |
| Puig [84] | 2010 | Retro | 6 | 14 | 84 | 4 Ant. axial/2 Post. tilted | Nobel Speedy Groovy/MK III Groovy | 1 | Yes | 82 | 98.50 | 14 | 100 | NR | Milled | 8/30 | 8/30 |
| Mertens [75] | 2011 | Pros | 6 | 17 | 106 | Parallel | Astra Tech | 8 | No | 105 | 99 | 17 | 100 | 0.30 ± 0.72 | Cast | 9/17 | NR |
| Barbier [76] | 2012 | Pros | 6 | 20 | 120 | Parallel | Astra Osseospeed | 1 | Yes | 119 | 99.30 | 20 | 100 | −0.35 ± 0.29 | Milled | NR | NR |
| Antoun [77] | 2012 | Retro | 6 | 13 | 78 | Parallel | Nobel | 1.5 | No | 78 | 98.50 | 13 | 97.70 | NR | NR | 12/44 | NR |
| Merten [78] | 2012 | Pros | 6 | 15 | 94 | Parallel | AstraTech | 11.3 | NR | 92 | 98.50 | 15 | 100 | NR | NR | 12/15 | NR |
| Thor [30] | 2014 | Pros | 6 | 51 | 306 | Parallel | Astra Osseospeed | 3 | Yes | 276 | 96 | 47 | 92.50 | 0.57 ± 1.12 | Cast | 36/51 | NR |
| Cannizaro [43] | 2015 | RCT | 6 | 30 | 180 | Parallel | 3i | 1 | No | 177 | 98.50 | 30 | 100 | 0.39 ± 0.07 | Cast | 3/30 | 1/30 |
| Toljanic [31] | 2016 | Pros | 6 | 51 | 306 | 4 Ant. axial/2 Post. tilted | Astra Osseospeed | 5 | No | 286 | 93.46 | 39 | 97.50 | 0.44 ± 1.25 | Cast | NR | NR |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tallarico [24] | 2016 | RCT | 6 | 20 | 120 | Parallel | NobelSpeedy Groovy | 5.3 | Yes | 114 | 95 | 20 | 100 | 1.51 ± 0.36 | NR | 2/20 | 2/120 |
| Wentaschek [79] | 2017 | Retro | 6 | 10 | 60 | 4 Ant. axial/2 Post. tilted | Bredent BlueSky | 5.3 | Yes | 75 | 95 | 10 | 100 | −0.50 ± 0.43 | Cast | 0/10 | 0/60 |
| Testori [34] | 2017 | Retro | 6 | 24 | 144 | 4 Ant. axial/2 Post. tilted | Biomet/3i | 10 | No | 137 | 95.10 | 24 | 100 | NR | Cast | 9/24 | NR |
| Tischler [32] | 2018 | Retro | 6 | 103 | 618 | 4 Ant. axial/2 Post. tilted | Tapered Internal; Biohorizons | 4 | No | 605 | 97.60 | 102 | 99.40 | NR | NR | 3/103 | NR |
| Almasri [80] | 2021 | Retro | 6 | 20 | 120 | Probably Parallel | Astratech/Nobel-Replace | 5 | NR | 119 | 99 | 18 | 100 | NR | Cast | NR | NR |
| Toia [23] | 2021 | RCT | 6 | 28 | 168 | 4 Ant. axial/2 Post. tilted | Astra OsseoSpeed | 3 | No | 167 | 99.40 | 28 | 100 | 0.01 ± 0.30 | Milled | 9/28 | 9/168 |
Retro; Retrospective, Pros; Prospective, RCT; Randomized clinical trial, Impt.; Implants, max.; maxilla, mand.; mandible, Ant.; Anterior, post.; posterior, Surv.; survival, Prosth.; prosthesis, MBL; marginal bone loss, Fram.; Framework, Tech. & mech. Comp./Prosth.; Technical and mechanical Complications per prosthesis number; complications, Bio. Comp./Impt. No.; Biological complications per implants number, NR; Not reported.
Among the included studies, 29 were retrospective, 21 were prospective, and three were RCTs. A total of 20251 implants were placed in 4713 maxillary aches, distributed into 15581 implants in 3935 arches (4-IG) and 4670 implants in 778 arches (6-IG), with a mean follow-up of 3.8 years. The final restoration reports indicated screw-trained fixed prostheses, with cast metal frames in 18 reports and CAD/CAM milled frames in 23 reports. Surgical guides were employed in 21 studies, MBL was reported in 38 studies, and technical and biological complications were extracted from 35 studies (Table 3).
3.4. Implant and prosthesis survival rates
The overall mean survival rate of implants and prostheses over a 3.8-year follow-up period was 97.9 % and 99.8 %, respectively. The mean implant survival rate was 98.5 % in 4-IG (95 % CI: 97.8; 99.1), slightly higher than the reported 97 % (95 % CI: 95.2; 98.4 %) in 6-IG. However, this difference was not statistically significant (p = 0.06) (Fig. 2). For prosthesis survival rates, the mean in 4-IG was 99.8 % (95 % CI: 99.1; 100.0), compared to 99.6 % (95 % CI: 99.3; 100.0) in 6-IG with no statistically significant difference (p = 0.37) (Fig. 3).
3.5. Marginal bone loss
The overall mane MBL around implants at an average follow-up of 3.8 years was 0.81 mm (95 % CI: 0.62; 1.01). Notably, increased MBL was observed in 4-IG at 1.02 mm (95 % CI: 0.79; 1.26) compared to 6-IG at 0.46 mm (95 % CI: 0.20; 0.72), and this difference was statistically significant (p < 0.01) (Fig. 4).
3.6. Technical/mechanical and biological complications
The estimated technical/mechanical complication rate per 100 prostheses was 19.8 %. Despite that more complications were reported in 4-IG (20.7, 95 % CI: 13.9; 28.3) compared to 6-IG (17.9, 95 % CI: 7.2; 31.71), the difference between groups was not statistically significant (p = 0.74) (Fig. 5). Technical complications were addressed in 37 studies, with 24 in 4-IG [21,23,24,27,28,35,37,38,[44], [45], [46],[49], [50], [51], [52], [53], [54], [55],58,61,[63], [64], [65], [66],81] and 13 in 6-IG [23,24,30,32,34,43,67,71,74,75,77,78,81]. Specific technical/mechanical complications in 4-IG per included studies were denture tooth fracture/debonding (5/24), detachment of the veneering material (6/24), screw loosening (14/24), fracture of the acrylic prosthesis (11/24), abutment fracture (1/24), screw fracture (3/24), prosthetic wear (1/24), and framework fracture (1/24, PEEK framework). In 6-IG, complications per included studies were denture tooth fracture/debonding (4/13), detachment of the veneering material (7/13), screw loosening (7/13), fracture of the acrylic prosthesis (5/13), abutment fracture (4/13), screw fracture (3/13), framework fracture (2/13), welded titanium framework), and aging of the acrylic base (2/13).
The estimated biological complication rate per 100 prostheses was 6.3 % (95 % CI: 2.7; 11.21). The recorded biological complication for 4-IG was higher at 2.0 % (95 % CI: 0.8; 3.6) compared to 6-IG at 0.8 % (95 % CI: 0.0; 2.1), with no statistically significant difference (p = 0.20) (Fig. 6). Biological complications were reported in 21 studies, with 15 in 4-IG [23,24,27,35,36,38,44,46,49,52,54,55,63,65,81] and 6 in 6-IG [23,24,43,67,74,81]. Reported biological complications in 4-IG per studies were probing pocket depths (5/15), bleeding on probing (6/15), peri-implantitis/excessive marginal bone loss (6/13), swelling (2/15), fistula (2/15), abscess (2/15), and infection (2/15). In 6-IG, biological complications per studies were bleeding on probing (4/6), peri-implantitis/excessive marginal bone loss (2/6), swelling (2/6), infection (1/6), plaque accumulation (2/6), and hyperplasia (2/6). Detailed technical/mechanical and biological complications are listed in Appendix 3.
Fig. 6.
Meta-analysis forest plot— Biological complications 4-IG & 6-IG.
3.7. Subgroup analysis
Data pertaining to the follow-up period, use of surgical guide, type of metal framework, and implant distribution were extracted for 4-IG and 6-IG, with the meta-analysis results presented in Appendix 4. The overall mean follow-up was 3.8 years, with 3.4 years in 4-IG and 4.5 years in 6IG. Studies were categorized into three groups according to the follow-up period (≤3, 3–5, and ≥5 years). No statistically significant difference in implant survival was observed for the different follow-up periods in 4-IG (p = 0.57) or 6-IG (p = 0.06).
The use of surgical guide was reported in 17 studies for 4-IG and 6 studies for 6-IG. Implant survival did not significantly differ when comparing the use of surgical guide to the freehand technique in either 6-IG (p = 0.32) or 4-IG (p = 0.89). CAD/CAM milled frameworks were reported in 25 studies (21 in 4-IG and 4 in 6-IG), while cast metal frameworks were addressed in 18 studies (7 in 4-IG and 11 in 6-IG) (Table 3). No significant difference in implant survival was found between cast and milled subgroups in 4-IG (p = 0.86). In 6-IG, a high implant survival 97.6 % (95 % CI: 96.1; 98.7) was observed in CAD/CAM milled framework subgroup compared to the casted subgroups with a rate of 96.9 % (95 % CI: 94.9; 98.1). The difference between subgroups was statistically significant (p ﹤0.01).
Regarding implant distribution, in 4-IG, all studies adopted a "2 axial, 2 tilted" configuration, except for one study that used the parallel configuration [20]. In 6-GI, implant distribution varied with "parallel" in nine studies, showing an implant survival rate of 95.7 % (95 % CI: 92.2; 98.3), "4 Anterior axial/2 Posterior Tilted" in nine studies with an implant survival rate of 97.3 % (95 % CI: 95.8; 98.5), and "V-II-V" (2 anterior parallel, two anteriorly tilted mesially, and two posteriorly tilted distally) in two studies with an implant survival rate of 100 % (95 % CI: 95.2; 98.4). Implant survival was significantly affected by different implant distributions in 6-IG (p < 0.01) (Appendix 4).
4. Discussion
4.1. Summary of evidence
The study's hypothesis was partially validated, as clinical and radiographical outcomes were comparable to whether a maxillary fixed complete denture prosthesis was supported by four or six implants. The meta-analysis indicated high implant and prosthesis survival rates, with no statistically significant differences between the two groups. However, the 4-implant group exhibited a higher incidence of technical and biological complications, although the disparity was not significant. Notably, there was a significantly greater marginal bone loss observed in the 4-implant group compared to the 6-implant group (p < 0.01).
The overall mean survival rate of implants at 3.8 years (mean follow-up) was 97.9 %, mirroring Heydecke et al. [5] findings of a 97.5 % survival rate (95 % CI: 94.1–98.9 %) for FAFDPs on four to six implants after 5 years. In this systematic review, the implant survival rate was 98.5 % in 4-IG and 97.0 % in 6-IG over 3.4 and 4.5 years of mean follow-up, respectively. These results slightly exceeded those reported by Daudt Polido et al. [6], who documented a 97% implant survival rate for 4-IG and 95 % for 6-IG in longer follow-up periods. De Luna Gomes et al. [7] reported a 99% implant survival for <5 implants, consistent with our findings. However, the survival rate for ≥5 implants was 95%, slightly lower than our review.
The prosthesis survival rate in the present systematic review was 99.8 % in 4-IG and 99.6 % in 6-IG, aligning with Daudt Polido et al. [6] report of 99 % restoration survival for 4-IG and 98.5 % for 6-IG. In contrast, De Luna Gomes et al. [7] reported a 100 % survival rate for complete arches with <5 implants and 89.62 % for those with >4 implants in the maxilla, respectively. The author declared that the higher failure rates for the >4 implants group could be attributed to a longer average, contrary to the present review, which did not find a significant effect of follow-up duration on implant/prosthesis survival rate.
The pooled MBL was significantly higher in 4-IG (1.02 mm) compared with 6-IG (0.46 mm) (p < 0.01). These results are consistent with those reported by Patzelt et al. [82], who recorded a mean MBL of 1.0 ± 0.5 mm, 0.8 ± 0.4 mm, and 1.3 ± 0.5 mm in the maxilla within 12, 24, and 36 months, respectively. However, De Luna Gomes et al. [7] reported a higher MBL in the group with five or more implants (1.46 ± 0.46 mm) compared to the group with less than five implants (1.22 ± 0.49 mm), diverging from our findings. The increased MBL in 4-IG compared to 6-IG in our review may be attributed to the presence of a distal cantilever in the former group. Biomechanical studies suggested that lengthening the cantilever raises stress levels, potentially leading to increased bone resorption around the implant [83]. Conversely, other biomechanical research indicated that increasing the number of implants, as in the All-on-6 concept, improves force distribution and may decrease stress on bone tissue [84].
The incidence of mechanical, technical, and biological complications per 100 prostheses per year was higher in 4-IG compared with 6-IG. To the authors' knowledge, there is a lack of systematic reviews comparing the incidence of technical/biological complications in FCDs supported by four versus six implants. Consequently, drawing direct comparisons between the current study's findings and those of other reviews proved challenging. It's worth mentioning that more prosthetic complications were reported in the <5 implant group (7.85 with a pooled weighted event rate of 19.9 %, I2 = 93.5 %, P < 0.001) compared with the ≥5 implant group (5.76 with a pooled weighted event rate of 24.5 %, I2 = 88.89, P < 0.001) in a previous study [7]. However, it's crucial to acknowledge that the present systematic review reported pooled complication rates for both jaws collectively.
Among the included studies in this review, the most frequently reported technical complication was screw loosening (21/37), while bleeding on probing (9/21) and excessive marginal bone loss (8/21) were the most commonly reported biological complications. These findings align with those reported by Papaspyridakos P et al. [25], who conducted a systematic review on biological and technical complications with fixed implant rehabilitations for edentulous patients. In their study, abutment/occlusal screw loosening and veneering material chipping/fracture were the most common implant/prosthetic technical complications. Excessive peri-implant crestal bone loss exceeding 2 mm and hypertrophy/hyperplasia of the soft tissue were the predominant biological complications. Denture fractures, primarily observed in provisional prostheses, were attributed to the shift in individuals' masticatory behavior from soft to harder foods after regaining the ability to chew [45]. Biomechanical studies suggest that the All-on-6 concept induces lower stress and exhibits more favourable biomechanical behaviour compared to the All-on-4. Moreover, anteroposterior distribution of implants has been linked to implant survival and technical complications [5,25]. These factors could contribute to the lower complication rates observed in 6-IG compared with 4-IG.
Subgroup analysis did not reveal a significant effect of the follow-up period on implant/prosthesis survival between 4I-G and 6I-G. Similarly, using a surgical guide or freehand technique did not significantly impact the survival rate of both groups, aligning with findings from previous systematic reviews [85,86]. However, these results contradict Abdelhay et al.’s [87] conclusion that implant failure rates were nearly three times higher in freehand than in guided placement.
Regarding the framework, subgroup analysis found significantly higher implant survival in 6I-G when the CAD/CAM milled metal framework was used compared with the cast metal framework (p ﹤0.01). However, there was no significant effect of the type of framework used in 4-IG (p = 0.86). Increasing the number of implants, as in the case of six implants, can introduce complexity to prosthesis construction, particularly in the face of implant malposition [19]. This complexity could be more pronounced when constructing a conventional cast metal framework, highlighting the demand for a precise framework with good marginal fitness when the number of implants increases.
Implant distribution was found to significantly affect implant survival, with the "V-II-V″ distribution exhibiting the highest survival rate (100 %), followed by "4 Anterior axial/2 Posterior Tilted" (79.3%), and "parallel" configuration (95.5 %). This observation is consistent with those in the previous studies. [4,5,25], indicating that implant distribution directly influences implant survival and technical complications.
While the meta-analysis conducted in this review indicates minimal variation in outcomes between the use of 4-IG and 6-IG, it is essential to consider factors such as complications that can influence the overall treatment expenses. These complications can potentially compromise both short and long-term treatment goals, posing challenges to both the dental clinic and patients' satisfaction. Therefore, a comprehensive consideration of all relevant factors is crucial for ensuring the best possible treatment outcome [88].
Occlusion plays a pivotal role in planning implant-supported teeth, significantly affects the long-term success, stability, and functionality of both implants and prosthesis [89,90]. Factors such as the number and position of implants, available implant surfaces for load transmission on the jaw bone, the relationship of superstructure length to the implant body, and establishment of proper occlusion are all critical considerations in implant placement and fabrication of implant-supported complete dentures [91]. Effective occlusion management is vital for preserving surrounding bone and soft tissues supporting dental implants. Proper force distribution through occlusion stimulates adjacent bone, maintaining its health and preventing bone loss [92]. Skeletal relations, maxillary and mandibular ridge relationships (Anterior-Posterior, Buccal-Lingual), esthetic demands, temporomandibular symptoms, vertical dimension of occlusion, planned implant positions, occlusal and periodontal examinations of remaining teeth, and parafunctional habits must all be evaluated before treatments [89]. Thorough assessments utilizing diagnostic techniques such as digital imaging, intraoral scanners, and occlusal analysis equipment enable the dental team to devise a treatment plan addressing occlusal concerns, thereby supporting the long-term success of implant-supported teeth.
The success of implant therapy relies significantly on proper patient selection, akin to any surgical procedure [93,94]. In fully edentulous patients, older age does not impact implant survival in the short term (1–5 years of follow-up), but health status considerations are crucial. Comprehensive medical history registration, in particular systemic diseases and concomitant polypharmacy, and assessment of the involved surgical site are essential [95]. Various systemic conditions have been identified as potential complicating factors or contraindications for implant surgery [96,97], necessitating careful considerations. Understanding the impact of systemic disease (and accompanying drugs) on the surgical procedure and final treatment outcome is critical [98].
In contemporary practice, a digital workflow is employed for fabricating full-mouth fixed implant rehabilitation, serving as an alternative or supplement to conventional approaches. This workflow encompasses interconnected stages including three-dimensional (3D) imaging, digital planning, template-guided surgery, digital scans, and CAD/CAM prosthetics [3,[99], [100], [101]]. An integral element of this digital process is the implementation of an intraoral scanner (IOS), crucial for generating Standard Tessellation Language (STL) files instrumental in fabricating definitive FCDs [101,102]. The digital workflow is anticipated to contribute to more precise and less invasive surgical procedures, superior prosthetic fitting, and potentially improved patient outcomes.
4.2. Methodological quality assessment
In this systematic review, the majority of included studies were prospective and retrospective studies. Therefore, strict selection criteria were employed to minimize expected heterogeneity and enhance the overall search quality. Nevertheless, notable heterogeneity amongst the included studies was observed, stemming from variations in several key aspects: (1) Patient selection criteria: Differences in patient demographics, medical history, and oral health status contributed to the heterogeneity. (2) Implant type and design: Variances in implant shape, size, material, and surface characteristics influenced clinical outcomes. (3) Surgical technique: Disparities in surgical techniques, such as flapless versus flap surgery, immediate versus delayed implant placement, or one-stage versus two-stage surgery. (4) Follow-up period: Variations in the duration of follow-up periods impacted the report implant success rate. (5) Outcome measures: Differences in outcome measures, such as implant survival, implant success, or peri-implantitis rate, introduced variability. (6) Study design: Variability in study designs, with retrospective studies potentially exhibiting higher heterogeneity compared to randomized controlled trials. (7) Operator experience: The skill and experience of operators, which varied across studies, contributed to potential heterogeneity.
Despite employing rigorous selection criteria, the findings of the present systematic review should be interpreted with caution due to several limitations. The lack of RCTs in the majority of the included studies and the inherent heterogeneity underscore the need for further research.
4.3. Limitations
The high heterogeneity observed among the included studies is a significant limitation of our study, but it aligns with the nature of proportional meta-analysis; as highlighted by Barker et al. [103], the elevated I2 in the context of proportional meta-analysis does not necessarily indicate inconsistency or lack of generalization. Notably, most of the included studies were retrospective and prospective, and a strength of the study lies in its focused evaluation and comparison of reports specifically involving four or six implants for rehabilitating the edentulous maxilla. However, to enhance the robustness of outcome assessment, future research should prioritize RCTs with extended follow-up periods, direct comparing the efficacy of four and six implants in supporting maxillary FCDPs.
5. Conclusion
The findings of this study suggest that increasing the number of implants, as observed in the 6-implant group, can contribute to a reduction in technical and biological complications, along with mitigating marginal bone loss. Notably, factors such as the utilization of CAD/CAM frameworks and the anteroposterior distribution of implants were identified as influential in enhancing implant survival rates with an increased number of implants. To bolster the evidence base, it is imperative to conduct further RCTs directly comparing the efficacy of using 4 versus 6 implants. Furthermore, a comprehensive exploration of other potential factors impacting implant survival, including implant type and design, the integration of digital technology, and the application of bone grafts, warrants further investigation. Such investigations will contribute to a more nuanced understanding of optimal strategies for successful implant-supported maxillary fixed complete denture prostheses.
Funding statement
This study was supported by grants from the National Natural Science Foundation of China (No. 82271026) and the Key Research and Development Program of Science and Technology Department of Zhejiang Province (No. 2019C03081).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author.
CRediT authorship contribution statement
Mufeed Ahmed Sharaf: Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Siyuan Wang: Writing – original draft, Methodology, Investigation, Formal analysis. Mubarak Ahmed Mashrah: Writing – review & editing, Methodology, Investigation. Yangbo Xu: Writing – review & editing, Formal analysis, Data curation. Ohood Haider: Writing – review & editing, Formal analysis, Data curation. Fuming He: Writing – review & editing, Supervision, Project administration, Methodology, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:He Fuming reports financial support was provided by This study was supported by grants from the National Natural Science Foundation of China (No. 82271026) and the Key Research and Development Program of Science and Technology Department of Zhejiang Province (No. 2019C03081). If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors thank Xiangrong Gao for her assistance with the statistical analysis.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e24365.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Lee S.J., Gallucci G.O. Digital vs. conventional implant impressions: efficiency outcomes. Clin. Oral Implants Res. 2013;24(1):111–115. doi: 10.1111/j.1600-0501.2012.02430.x. [DOI] [PubMed] [Google Scholar]
- 2.Maló P., et al. Retrievable metal ceramic implant-supported fixed prostheses with milled titanium frameworks and all-ceramic crowns: retrospective clinical study with up to 10 years of follow-up. J. Prosthodont. 2012;21(4):256–264. doi: 10.1111/j.1532-849X.2011.00824.x. [DOI] [PubMed] [Google Scholar]
- 3.Papaspyridakos P., et al. Digital workflow for fixed implant rehabilitation of an Extremely atrophic edentulous mandible in three Appointments. J Esthet Restor Dent. 2017;29(3):178–188. doi: 10.1111/jerd.12290. [DOI] [PubMed] [Google Scholar]
- 4.Lambert F.E., et al. Descriptive analysis of implant and prosthodontic survival rates with fixed implant-supported rehabilitations in the edentulous maxilla. J. Periodontol. 2009;80(8):1220–1230. doi: 10.1902/jop.2009.090109. [DOI] [PubMed] [Google Scholar]
- 5.Heydecke G., et al. What is the optimal number of implants for fixed reconstructions: a systematic review. Clin. Oral Implants Res. 2012;23(Suppl 6):217–228. doi: 10.1111/j.1600-0501.2012.02548.x. [DOI] [PubMed] [Google Scholar]
- 6.Daudt Polido W., et al. Number of implants placed for complete-arch fixed prostheses: a systematic review and meta-analysis. Clin. Oral Implants Res. 2018;29(Suppl 16):154–183. doi: 10.1111/clr.13312. [DOI] [PubMed] [Google Scholar]
- 7.de Luna Gomes J.M., et al. Optimal number of implants for complete-arch implant-supported prostheses with a follow-up of at least 5 years: a systematic review and meta-analysis. J. Prosthet. Dent. 2019;121(5):766–+. doi: 10.1016/j.prosdent.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Morand M., Irinakis T. The challenge of implant therapy in the posterior maxilla: Providing a Rationale for the Use of short implants. J. Oral Implantol. 2007;33(5):257–266. doi: 10.1563/1548-1336(2007)33[257:Tcoiti]2.0.Co;2. [DOI] [PubMed] [Google Scholar]
- 9.Maló P., Rangert B., Nobre M. All-on-4 immediate-function concept with Brånemark System® implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin. Implant Dent. Relat. Res. 2005;7(SUPPL. 1):S88–S94. doi: 10.1111/j.1708-8208.2005.tb00080.x. [DOI] [PubMed] [Google Scholar]
- 10.Babbush C.A., et al. Patient-related and financial outcomes analysis of conventional full-arch rehabilitation versus the All-on-4 concept: a cohort study. Implant Dent. 2014;23(2):218–224. doi: 10.1097/id.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 11.Esfahrood Z.R., et al. Short dental implants in the posterior maxilla: a review of the literature. J Korean Assoc Oral Maxillofac Surg. 2017;43(2):70–76. doi: 10.5125/jkaoms.2017.43.2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Araujo R.Z., et al. Clinical outcomes of pterygoid implants: systematic review and meta-analysis. J. Cranio-Maxillo-Fac. Surg. 2019;47(4):651–660. doi: 10.1016/j.jcms.2019.01.030. [DOI] [PubMed] [Google Scholar]
- 13.Lopes L.F., et al. Placement of dental implants in the maxillary tuberosity: a systematic review. Int. J. Oral Maxillofac. Surg. 2015;44(2):229–238. doi: 10.1016/j.ijom.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Chrcanovic B.R., Albrektsson T., Wennerberg A. Survival and complications of zygomatic implants: an updated systematic review. J. Oral Maxillofac. Surg. 2016;74(10):1949–1964. doi: 10.1016/j.joms.2016.06.166. [DOI] [PubMed] [Google Scholar]
- 15.Raghoebar G.M., et al. Long-term effectiveness of maxillary sinus floor augmentation: a systematic review and meta-analysis. J. Clin. Periodontol. 2019;46(Suppl 21):307–318. doi: 10.1111/jcpe.13055. [DOI] [PubMed] [Google Scholar]
- 16.Danesh-Sani S.A., Loomer P.M., Wallace S.S. A comprehensive clinical review of maxillary sinus floor elevation: anatomy, techniques, biomaterials and complications. Br. J. Oral Maxillofac. Surg. 2016;54(7):724–730. doi: 10.1016/j.bjoms.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 17.Starch-Jensen T., Jensen J.D. Maxillary sinus floor augmentation: a review of selected treatment Modalities. J. Oral Maxillofac. Res. 2017;8(3):e3. doi: 10.5037/jomr.2017.8303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zarb G.A., Schmitt A. The longitudinal clinical effectiveness of osseointegrated dental implants: the Toronto study. Part I: surgical results. J. Prosthet. Dent. 1990;63(4):451–457. doi: 10.1016/0022-3913(90)90237-7. [DOI] [PubMed] [Google Scholar]
- 19.Gallucci G.O., et al. Maxillary implant-supported fixed prosthesis: a Survey of reviews and key variables for treatment planning. Int. J. Oral Maxillofac. Implants. 2016;31(Suppl):s192–s197. doi: 10.11607/jomi.16suppl.g5.3. [DOI] [PubMed] [Google Scholar]
- 20.Brånemark P.-I., Svensson B., Van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Brånemark in full edentulism. Clin. Oral Implants Res. 1995;6(4):227–231. doi: 10.1034/j.1600-0501.1995.060405.x. [DOI] [PubMed] [Google Scholar]
- 21.Malo P., Rangert B., Nobre M. All-on-4 immediate-function concept with Branemark System (R) implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin. Implant Dent. Relat. Res. 2005;7:S88–S94. doi: 10.1111/j.1708-8208.2005.tb00080.x. [DOI] [PubMed] [Google Scholar]
- 22.Passoni B.B., et al. Does the number of implants have any relation with peri-implant disease? J. Appl. Oral Sci. 2014;22(5):403–408. doi: 10.1590/1678-775720140055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toia M., et al. Fixed full-arch maxillary prostheses supported by four versus six implants with a titanium CAD/CAM milled framework: 3-year multicentre RCT. Clin. Oral Implants Res. 2021;32(1):44–59. doi: 10.1111/clr.13679. [DOI] [PubMed] [Google Scholar]
- 24.Tallarico M., et al. Five-year results of a randomized controlled trial comparing patients rehabilitated with immediately loaded maxillary cross-arch fixed dental prosthesis supported by four or six implants placed using guided surgery. Clin. Implant Dent. Relat. Res. 2016;18(5):965–972. doi: 10.1111/cid.12380. [DOI] [PubMed] [Google Scholar]
- 25.Papaspyridakos P., et al. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int. J. Oral Maxillofac. Implants. 2012;27(1):102–110. [PubMed] [Google Scholar]
- 26.Shackleton J.L., et al. Survival of fixed implant-supported prostheses related to cantilever lengths. J. Prosthet. Dent. 1994;71(1):23–26. doi: 10.1016/0022-3913(94)90250-x. [DOI] [PubMed] [Google Scholar]
- 27.Maló P., Nobre M., Lopes A. The rehabilitation of completely edentulous maxillae with different degrees of resorption with four or more immediately loaded implants: a 5-year retrospective study and a new classification. Eur J Oral Implantol. 2011;4(3):227–243. [PubMed] [Google Scholar]
- 28.Drago C. Ratios of cantilever lengths and anterior-posterior Spreads of definitive hybrid full-arch, screw-retained prostheses: results of a clinical study. J. Prosthodont. 2018;27(5):402–408. doi: 10.1111/jopr.12519. [DOI] [PubMed] [Google Scholar]
- 29.Krennmair G., et al. Clinical outcome and peri-implant findings of four-implant-supported distal cantilevered fixed mandibular prostheses: five-year results. Int. J. Oral Maxillofac. Implants. 2013;28(3):831–840. doi: 10.11607/jomi.3024. [DOI] [PubMed] [Google Scholar]
- 30.Thor A., et al. Three-year follow-up of immediately loaded implants in the edentulous atrophic maxilla: a study in patients with poor bone quantity and quality. Int. J. Oral Maxillofac. Implants. 2014;29(3):642–649. doi: 10.11607/jomi.3163. [DOI] [PubMed] [Google Scholar]
- 31.Toljanic J.A., et al. Immediate loading of implants in the edentulous maxilla with a fixed provisional restoration without bone augmentation: a report on 5-year outcomes data Obtained from a prospective clinical trial. Int. J. Oral Maxillofac. Implants. 2016;31(5):1164–1170. doi: 10.11607/jomi.4364. [DOI] [PubMed] [Google Scholar]
- 32.Tischler M., Patch C., Bidra A.S. Rehabilitation of edentulous jaws with zirconia complete-arch fixed implant-supported prostheses: an up to 4-year retrospective clinical study. J. Prosthet. Dent. 2018;120(2):204–209. doi: 10.1016/j.prosdent.2017.12.010. [DOI] [PubMed] [Google Scholar]
- 33.Sharaf M.A., et al. Clinical and patient-centered outcomes following rehabilitation of atrophic edentulous maxilla using six implants placed simultaneously with bilateral maxillary sinus augmentation: a retrospective case series. J Stomatol Oral Maxillofac Surg. 2023 doi: 10.1016/j.jormas.2023.101480. [DOI] [PubMed] [Google Scholar]
- 34.Testori T., et al. Assessment of long-term survival of immediately loaded tilted implants supporting a maxillary full-arch fixed prosthesis. Int. J. Oral Maxillofac. Implants. 2017;32(4):904–911. doi: 10.11607/jomi.5578. [DOI] [PubMed] [Google Scholar]
- 35.Maló P., et al. Immediate loading short implants inserted on low bone quantity for the rehabilitation of the edentulous maxilla using an All-on-4 design. J. Oral Rehabil. 2015;42(8):615–623. doi: 10.1111/joor.12291. [DOI] [PubMed] [Google Scholar]
- 36.Hopp M., de Araújo Nobre M., Maló P. Comparison of marginal bone loss and implant success between axial and tilted implants in maxillary All-on-4 treatment concept rehabilitations after 5 years of follow-up. Clin. Implant Dent. Relat. Res. 2017;19(5):849–859. doi: 10.1111/cid.12526. [DOI] [PubMed] [Google Scholar]
- 37.Malo P., et al. Immediate function dental implants inserted with less than 30 N.cm of torque in full-arch maxillary rehabilitations using the All-on-4 concept: retrospective study. Int. J. Oral Maxillofac. Surg. 2018;47(8):1079–1085. doi: 10.1016/j.ijom.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 38.Maló P., et al. The All-on-4 concept for full-arch rehabilitation of the edentulous maxillae: a longitudinal study with 5-13 years of follow-up. Clin. Implant Dent. Relat. Res. 2019;21(4):538–549. doi: 10.1111/cid.12771. [DOI] [PubMed] [Google Scholar]
- 39.Page M.J., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miller S.A., Forrest J.L. Enhancing your practice through evidence-based decision making: PICO, learning how to ask good questions. J. Evid. Base Dent. Pract. 2001;1(2):136–141. doi: 10.1016/S1532-3382(01)70024-3. [DOI] [Google Scholar]
- 41.Higgins J.P., et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Bmj. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sterne J.A., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Bmj. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cannizzaro G., et al. Immediate loading of fixed cross-arch prostheses supported by flapless-placed supershort or long implants: 1-year results from a randomised controlled trial. Eur J Oral Implantol. 2015;8(1):27–36. [PubMed] [Google Scholar]
- 44.Malo P., de Araujo Nobre M., Lopes A. The use of computer-guided flapless implant surgery and four implants placed in immediate function to support a fixed denture: preliminary results after a mean follow-up period of thirteen months. J. Prosthet. Dent. 2007;97(6 Suppl):S26–S34. doi: 10.1016/s0022-3913(07)60005-5. [DOI] [PubMed] [Google Scholar]
- 45.Agliardi E., et al. Immediate rehabilitation of the edentulous jaws with full fixed prostheses supported by four implants: interim results of a single cohort prospective study. Clin. Oral Implants Res. 2010;21(5):459–465. doi: 10.1111/j.1600-0501.2009.01852.x. [DOI] [PubMed] [Google Scholar]
- 46.Hinze M., et al. Immediate loading of fixed provisional prostheses using four implants for the rehabilitation of the edentulous arch: a prospective clinical study. Int. J. Oral Maxillofac. Implants. 2010;25(5):1011–1018. [PubMed] [Google Scholar]
- 47.Babbush C.A., Kutsko G.T., Brokloff J. The all-on-four immediate function treatment concept with NobelActive implants: a retrospective study. J. Oral Implantol. 2011;37(4):431–445. doi: 10.1563/aaid-joi-d-10-00133. [DOI] [PubMed] [Google Scholar]
- 48.Parel S.M., Phillips W.R. A risk assessment treatment planning protocol for the four implant immediately loaded maxilla: preliminary findings. J. Prosthet. Dent. 2011;106(6):359–366. doi: 10.1016/s0022-3913(11)60147-9. [DOI] [PubMed] [Google Scholar]
- 49.Cavalli N., et al. Tilted implants for full-arch rehabilitations in completely edentulous maxilla: a retrospective study. Int J Dent. 2012;2012 doi: 10.1155/2012/180379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crespi R., et al. A clinical study of edentulous patients rehabilitated according to the "all on four" immediate function protocol. Int. J. Oral Maxillofac. Implants. 2012;27(2):428–434. [PubMed] [Google Scholar]
- 51.Francetti L., et al. Bone level changes around axial and tilted implants in full-arch fixed immediate restorations. Interim results of a prospective study. Clin. Implant Dent. Relat. Res. 2012;14(5):646–654. doi: 10.1111/j.1708-8208.2010.00304.x. [DOI] [PubMed] [Google Scholar]
- 52.Maló P., et al. "All-on-4" immediate-function concept for completely edentulous maxillae: a clinical report on the medium (3 years) and long-term (5 years) outcomes. Clin. Implant Dent. Relat. Res. 2012;14(Suppl 1):e139–e150. doi: 10.1111/j.1708-8208.2011.00395.x. [DOI] [PubMed] [Google Scholar]
- 53.Di P., et al. The All-on-Four implant therapy protocol in the management of edentulous Chinese patients. Int. J. Prosthodont. (IJP) 2013;26(6):509–516. doi: 10.11607/ijp.3602. [DOI] [PubMed] [Google Scholar]
- 54.Maló P., Nobre M., Lopes A. Immediate loading of 'All-on-4' maxillary prostheses using trans-sinus tilted implants without sinus bone grafting: a retrospective study reporting the 3-year outcome. Eur J Oral Implantol. 2013;6(3):273–283. [PubMed] [Google Scholar]
- 55.Lopes A., et al. The NobelGuide® all-on-4® treatment concept for rehabilitation of edentulous jaws: a prospective report on medium- and long-term outcomes. Clin. Implant Dent. Relat. Res. 2015;17(Suppl 2):e406–e416. doi: 10.1111/cid.12260. [DOI] [PubMed] [Google Scholar]
- 56.Balshi T.J., et al. A retrospective analysis of 800 Brånemark System implants following the All-on-Four™ protocol. J. Prosthodont. 2014;23(2):83–88. doi: 10.1111/jopr.12089. [DOI] [PubMed] [Google Scholar]
- 57.Babbush C.A., Kanawati A., Kotsakis G.A. Marginal bone stability around Tapered, platform-Shifted implants placed with an immediately loaded four-implant-supported fixed prosthetic concept: a cohort study. Int. J. Oral Maxillofac. Implants. 2016;31(3):643–650. doi: 10.11607/jomi.4354. [DOI] [PubMed] [Google Scholar]
- 58.Piano S., et al. Simplified procedure for the immediate loading of a complete fixed prosthesis supported by four implants in the maxillary jaw: a 2-year prospective study. Clin. Oral Implants Res. 2016;27(12):e154–e160. doi: 10.1111/clr.12580. [DOI] [PubMed] [Google Scholar]
- 59.Gherlone E., et al. Conventional versus digital impressions for "All-on-Four" restorations. Int. J. Oral Maxillofac. Implants. 2016;31(2):324–330. doi: 10.11607/jomi.3900. [DOI] [PubMed] [Google Scholar]
- 60.Najafi H., et al. Effects of immediate and delayed loading on the outcomes of all-on-4 treatment: a prospective study. J. Dent. 2016;13(6):415–422. [PMC free article] [PubMed] [Google Scholar]
- 61.Sannino G., et al. A retrospective 2-year clinical study of immediate prosthetic rehabilitation of edentulous jaws with four implants and Prefabricated Bars. J. Prosthodont. 2017;26(5):387–394. doi: 10.1111/jopr.12406. [DOI] [PubMed] [Google Scholar]
- 62.Maló P., et al. Short-term report of an ongoing prospective cohort study evaluating the outcome of full-arch implant-supported fixed hybrid polyetheretherketone-acrylic resin prostheses and the All-on-Four concept. Clin. Implant Dent. Relat. Res. 2018;20(5):692–702. doi: 10.1111/cid.12662. [DOI] [PubMed] [Google Scholar]
- 63.de Araújo Nobre M., et al. Hybrid polyetheretherketone (PEEK)–Acrylic resin prostheses and the all-on-4 concept: a full-arch implant-supported fixed Solution with 3 Years of follow-up. J. Clin. Med. 2020;9(7):2187. doi: 10.3390/jcm9072187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ayna M., et al. Six-year clinical outcomes of implant-supported acrylic vs. ceramic superstructures according to the All-on-4 treatment concept for the rehabilitation of the edentulous maxilla. Odontology. 2021;109(4):930–940. doi: 10.1007/s10266-021-00605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Korsch M., et al. Evaluation of the surgical and prosthetic success of All-on-4 restorations: a retrospective cohort study of provisional vs. definitive immediate restorations. Int. J. Implant Dent. 2021;7(1):48. doi: 10.1186/s40729-021-00330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kortam S.A., et al. Metal-Ceramic and polyether ether ketone-composite maxillary fixed prosthesis supported by four implants and opposed by removable distal extension partial dentures: a comparative study of clinical and prosthetic outcomes. Int. J. Oral Maxillofac. Implants. 2022;37(1):181–189. doi: 10.11607/jomi.9189. [DOI] [PubMed] [Google Scholar]
- 67.Jemt T., Johansson J. Implant treatment in the edentulous maxillae: a 15-year follow-up study on 76 consecutive patients provided with fixed prostheses. Clin. Implant Dent. Relat. Res. 2006;8(2):61–69. doi: 10.1111/j.1708-8208.2006.00003.x. [DOI] [PubMed] [Google Scholar]
- 68.Capelli M., et al. Immediate rehabilitation of the completely edentulous jaw with fixed prostheses supported by either upright or tilted implants: a multicenter clinical study. Int. J. Oral Maxillofac. Implants. 2007;22(4):639–644. [PubMed] [Google Scholar]
- 69.Agliardi E.L., et al. Immediate loading in the fully edentulous maxilla without bone grafting: the V-II-V technique. Minerva Stomatol. 2008;57(5):251–259. 259-263. [PubMed] [Google Scholar]
- 70.Testori T., et al. Immediate occlusal loading and tilted implants for the rehabilitation of the atrophic edentulous maxilla: 1-year interim results of a multicenter prospective study. Clin. Oral Implants Res. 2008;19(3):227–232. doi: 10.1111/j.1600-0501.2007.01472.x. [DOI] [PubMed] [Google Scholar]
- 71.Toljanic J.A., et al. Implant rehabilitation of the atrophic edentulous maxilla including immediate fixed provisional restoration without the use of bone grafting: a review of 1-year outcome data from a long-term prospective clinical trial. Int. J. Oral Maxillofac. Implants. 2009;24(3):518–526. [PubMed] [Google Scholar]
- 72.Agliardi E.L., et al. Immediate rehabilitation of the edentulous maxilla: preliminary results of a single-cohort prospective study. Int. J. Oral Maxillofac. Implants. 2009;24(5):887–895. [PubMed] [Google Scholar]
- 73.Romanos G.E., Nentwig G.H. Immediate functional loading in the maxilla using implants with platform switching: five-year results. Int. J. Oral Maxillofac. Implants. 2009;24(6):1106–1112. [PubMed] [Google Scholar]
- 74.Bergkvist G., et al. Immediate loading of implants in the edentulous maxilla: use of an interim fixed prosthesis followed by a permanent fixed prosthesis: a 32-month prospective radiological and clinical study. Clin. Implant Dent. Relat. Res. 2009;11(1):1–10. doi: 10.1111/j.1708-8208.2008.00094.x. [DOI] [PubMed] [Google Scholar]
- 75.Mertens C., Steveling H.G. Implant-supported fixed prostheses in the edentulous maxilla: 8-year prospective results. Clin. Oral Implants Res. 2011;22(5):464–472. doi: 10.1111/j.1600-0501.2010.02028.x. [DOI] [PubMed] [Google Scholar]
- 76.Barbier L., et al. Peri-implant bone changes following tooth extraction, immediate placement and loading of implants in the edentulous maxilla. Clin Oral Investig. 2012;16(4):1061–1070. doi: 10.1007/s00784-011-0617-9. [DOI] [PubMed] [Google Scholar]
- 77.Antoun H., et al. Immediate loading of four or six implants in completely edentulous patients. Int J Periodontics Restorative Dent. 2012;32(1):e1–e9. [PubMed] [Google Scholar]
- 78.Mertens C., et al. Fixed implant-retained rehabilitation of the edentulous maxilla: 11-year results of a prospective study. Clin. Implant Dent. Relat. Res. 2012;14(6):816–827. doi: 10.1111/j.1708-8208.2011.00434.x. [DOI] [PubMed] [Google Scholar]
- 79.Wentaschek S., et al. Six-implant-supported immediate fixed rehabilitation of atrophic edentulous maxillae with tilted distal implants. Int. J. Implant Dent. 2017;3 doi: 10.1186/s40729-017-0096-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Almasri M.A. A 5-year satisfaction outcome study of patients receiving six-implant-supported fixed prosthesis. Clinics and Practice. 2021;11(4):827–834. doi: 10.3390/clinpract11040097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pomares C. A retrospective study of edentulous patients rehabilitated according to the 'all-on-four' or the 'all-on-six' immediate function concept using flapless computer-guided implant surgery. Eur J Oral Implantol. 2010;3(2):155–163. [PubMed] [Google Scholar]
- 82.Patzelt S.B., et al. The all-on-four treatment concept: a systematic review. Clin. Implant Dent. Relat. Res. 2014;16(6):836–855. doi: 10.1111/cid.12068. [DOI] [PubMed] [Google Scholar]
- 83.Bozini T., et al. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int. J. Oral Maxillofac. Implants. 2011;26(2):304–318. [PubMed] [Google Scholar]
- 84.Bhering C.L., et al. Comparison between all-on-four and all-on-six treatment concepts and framework material on stress distribution in atrophic maxilla: a prototyping guided 3D-FEA study. Mater Sci Eng C Mater Biol Appl. 2016;69:715–725. doi: 10.1016/j.msec.2016.07.059. [DOI] [PubMed] [Google Scholar]
- 85.Yogui F.C., et al. Comparison between computer-guided and freehand dental implant placement surgery: a systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2021;50(2):242–250. doi: 10.1016/j.ijom.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 86.Walker-Finch K., Ucer C. Five-year survival rates for implants placed using digitally-designed static surgical guides: a systematic review. Br. J. Oral Maxillofac. Surg. 2020;58(3):268–276. doi: 10.1016/j.bjoms.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 87.Abdelhay N., Prasad S., Gibson M.P. Failure rates associated with guided versus non-guided dental implant placement: a systematic review and meta-analysis. BDJ Open. 2021;7(1):31. doi: 10.1038/s41405-021-00086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Walton J.N., MacEntee M.I. A prospective study on the maintenance of implant prostheses in private practice. Int. J. Prosthodont. (IJP) 1997;10(5):453–458. [PubMed] [Google Scholar]
- 89.Yoon D., et al. Occlusal considerations for full-arch implant-supported prostheses: a guideline. Dentistry Review. 2022;2(2) doi: 10.1016/j.dentre.2022.100042. [DOI] [Google Scholar]
- 90.Isidor F. Histological evaluation of peri-implant bone at implants subjected to occlusal overload or plaque accumulation. Clin. Oral Implants Res. 1997;8(1):1–9. doi: 10.1111/j.1600-0501.1997.tb00001.x. [DOI] [PubMed] [Google Scholar]
- 91.Engelman M.J., Sorensen J.A., Moy P. Optimum placement of osseointegrated implants. J. Prosthet. Dent. 1988;59(4):467–473. doi: 10.1016/0022-3913(88)90044-3. [DOI] [PubMed] [Google Scholar]
- 92.Graves C.V., et al. The role of occlusion in the dental implant and peri-implant condition: a review. Open Dent. J. 2016;10:594–601. doi: 10.2174/1874210601610010594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Alsaadi G., et al. Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. J. Clin. Periodontol. 2007;34(7):610–617. doi: 10.1111/j.1600-051X.2007.01077.x. [DOI] [PubMed] [Google Scholar]
- 94.Liddelow G., Klineberg I. Patient-related risk factors for implant therapy. A critique of pertinent literature. Aust. Dent. J. 2011;56(4):417–426. doi: 10.1111/j.1834-7819.2011.01367.x. quiz 441. [DOI] [PubMed] [Google Scholar]
- 95.Heitz-Mayfield L.J., et al. Consensus statements and clinical recommendations for prevention and management of biologic and technical implant complications. Int. J. Oral Maxillofac. Implants. 2014;29(Suppl):346–350. doi: 10.11607/jomi.2013.g5. [DOI] [PubMed] [Google Scholar]
- 96.Beikler T., Flemmig T.F. Implants in the medically compromised patient. Crit. Rev. Oral Biol. Med. 2003;14(4):305–316. doi: 10.1177/154411130301400407. [DOI] [PubMed] [Google Scholar]
- 97.Diz P., Scully C., Sanz M. Dental implants in the medically compromised patient. J. Dent. 2013;41(3):195–206. doi: 10.1016/j.jdent.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 98.Donos N., Calciolari E. Dental implants in patients affected by systemic diseases. Br. Dent. J. 2014;217(8):425–430. doi: 10.1038/sj.bdj.2014.911. [DOI] [PubMed] [Google Scholar]
- 99.Chochlidakis K.M., et al. Digital versus conventional impressions for fixed prosthodontics: a systematic review and meta-analysis. J. Prosthet. Dent. 2016;116(2):184–190.e12. doi: 10.1016/j.prosdent.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 100.Papaspyridakos P., et al. Complete digital workflow in prosthesis prototype fabrication for complete-arch implant rehabilitation: a technique. J. Prosthet. Dent. 2019;122(3):189–192. doi: 10.1016/j.prosdent.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 101.Vandeweghe S., et al. Accuracy of digital impressions of multiple dental implants: an in vitro study. Clin. Oral Implants Res. 2017;28(6):648–653. doi: 10.1111/clr.12853. [DOI] [PubMed] [Google Scholar]
- 102.Pesce P., et al. Precision and accuracy of a digital impression scanner in full-arch implant rehabilitation. Int. J. Prosthodont. (IJP) 2018;31(2):171–175. doi: 10.11607/ijp.5535. [DOI] [PubMed] [Google Scholar]
- 103.Barker T.H., et al. Conducting proportional meta-analysis in different types of systematic reviews: a guide for synthesisers of evidence. BMC Med. Res. Methodol. 2021;21(1):189. doi: 10.1186/s12874-021-01381-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.