Abstract
This pilot randomized controlled trial evaluated a previously developed manualized telephone based cognitive behavioral therapy (T-CBT) intervention compared to face-to-face (f2f) therapy among low-income, urban dwelling HIV infected depressed individuals. The primary outcome was the reduction of depressive symptoms as measured by the Hamliton rating scale for depression scale. The secondary outcome was adherence to HAART as measured by random telephone based pill counts. Outcome measures were collected by trained research assistants masked to treatment allocation. Analysis was based on intention-to-treat. Thirty-four participants met eligibility criteria and were randomly assigned to receive T-CBT (n = 16) or f2f (n = 18). There was no statistically significant difference in depression treatment outcomes comparing f2f to T-CBT. Within group evaluation demonstrated that both the T-CBT and the f2f psychotherapy groups resulted in significant reductions in depressive symptoms. Those who received the T-CBT were significantly more likely to maintain their adherence to antiretroviral medication compared to the f2f treatment. None of the participants discontinued treatment due to adverse events. T-CBT can be delivered to low-income, urban dwelling HIV infected depressed individuals resulting in significant reductions in depression symptoms and improved adherence to antiretroviral medication. Trial Registry: Clinical Trial.gov identifier: NCT01055158.
Keywords: HIV, Depression, CBT, Telephone
Introduction
Depressive disorders are highly prevalent among those infected with HIV [1]. Individuals with HIV and depressive disorders, compared to those with HIV alone, have worse adherence to taking antiretroviral medication, increased HIV related morbidity [2–5] and a higher mortality [6, 7]. Although mental health interventions may lead to improved depressive and HIV related outcomes among whites [8, 9], studies in the United States suggest that HIV infected people who identify as being part of an ethnic minority group may have more difficulty accessing mental health care [10]. Additionally, people who identify as being part of an ethnic minority group who have depression are also reported to be less likely to access [11] and benefit from standard mental health services compared to whites [12]. Furthermore as systematic reviews and meta-analyses have consistently shown that depression is strongly associated with sub-optimal antiretroviral adherence [13, 14], it is important to evaluate whether or not improvement of depression is associated with improvement of antiretroviral adherence.
Psychotherapeutic interventions may be particularly well suited to address the psychosocial and interpersonal difficulties as well as the distress associated with HIV [9]. Of note, telephone based cognitive behavioral therapy (T-CBT) has emerged as a feasible, acceptable and efficacious treatment for major depression [15–17]. Advantages of telephone based psychotherapy include the use of flexible scheduling, use of patient preferred locations which may help alleviate concerns about stigma, as well as ease of utilization [18]. These advantages may be particularly important for low income HIV infected people living in urban environments who may have difficulties with transportation, financial problems, multiple and conflicting medical appointments, and concerns about stigma [19]. With this in mind we developed an 11-session telephone based cognitive behavioral intervention to target low-income, urban dwelling HIV infected depressed individuals receiving HIV care in a medical setting. We previously reported that this T-CBT intervention was feasible, acceptable and resulted in a large and clinically meaningful reduction in depressive symptoms [20]. Building on the results of this feasibility study, we conducted a pilot randomized controlled study. We hypothesized that T-CBT would significantly improve depression outcomes and improve adherence to antiretroviral medication among a sample of low-income, urban dwelling HIV infected depressed individuals receiving HIV care in urban HIV clinics.
Methods
Study Design
This pilot randomized controlled trial evaluated a previously developed 11-session manualized T-CBT intervention compared to face to face (f2f) psychotherapy targeting low-income, urban dwelling HIV infected depressed individuals attending one of two urban HIV clinics affiliated with a large urban Medical Center. f2f therapy was chosen as the control condition in order to control for time and attention as well as provide an ethical and active treatment for major depression [21]. Our primary outcome was the reduction of depressive symptoms as measured by the Hamilton rating scale for depression scale (HAM-D) and the quick inventory of depression-self report (QID-SR). Our secondary outcome was adherence to HAART as measured by random telephone based pill counts.
Study Sample and Consent
As part of routine clinical care, clients attending the HIV clinic were screened for depression using the patient health questionnaire (PHQ-9) [22]. Patients who endorsed suicidal ideation on the PHQ-9 were evaluated by the appropriate clinical staff at the HIV clinic at the time of their appointment and were not eligible to participate in the study. Clients who endorsed anhedonia and/or depressed mood without endorsing suicidal symptoms and scored a 12 or higher on the PHQ-9 were referred to meet with a research assistant to discuss the study and consent procedures. Inclusion criteria included English speaking adults who had access to a working telephone, were able to read at a 4th grade reading level determined by the wide range achievement test-fourth edition (WRAT-4) [23] or self-report, and met criteria for major depressive episode based on the Mini International Neuropsychiatric Interview (MINI) [24]. Exclusion criteria included receiving concurrent psychotherapy, life expectancy <6 months as determined by their HIV clinician, having HIV related dementia as determined by the HIV dementia scale [25], initiating antidepressant treatment targeting depression or having an antidepressant medication dose change within 6 weeks of the consent process, and/or having current drug or alcohol dependence. The MINI was also used to rule out anyone with more severe psychiatric pathology (e.g., schizophrenia, bipolar affective disorder) for whom participation in the study might be considered dangerous or unethical.
Eligible clients were randomized within therapist using permuted blocks of varying sizes on a 1:1 ratio by the study statistician (DM). Therapists provided both telephone and f2f therapy. There was equal distribution of patients seen in each condition within therapist. Clients who were ineligible for the study were referred to mental health clinicians at their HIV clinic for follow-up. Clients were recruited from April 2010 to December 2011. The study was approved by the University of Maryland Institutional Review Board and all participants provided written informed consent.
Telephone Based Cognitive Behavioral Intervention
The telephone intervention used in this study was an 11-session manualized telephone CBT intervention targeting depression [20]. The intervention included one initial evaluation session, five sessions of behavioral activation and five sessions of cognitive restructuring delivered over a 14-week period. A 14-week period was chosen to provide up to three additional weeks for missed sessions to be made up or rescheduled. The intervention included a patient workbook and a linked therapist manual.
Therapist Training
The intervention was delivered by two master’s level therapists experienced in delivering cognitive-behavioral interventions. Each therapist received 12 h of didactic training and subsequently completed one supervised case using the adapted T-CBT intervention. Prior to being assigned trial participants, the therapist demonstrated high fidelity to the intervention and scored a mean score of 4 or greater on the cognitive therapy adherence and competence scale (CTACS) [26]. All supervision and training were training were conducted by the study principal investigator (SH). Supervision occurred on an approximately weekly basis. F2F therapy sessions were not audio recorded. All telephone based therapy sessions were audiotaped. CTACS ratings (SH) were performed on a 25 % random sample of therapy sessions at the end of the study to ensure fidelity.
Study Procedures
Intervention Condition
Participants were given a study workbook and were given the name and telephone number of their therapist. The therapist contacted the participant to set up the first session. Participants were reminded to choose a private and confidential location (e.g., in a private room behind a closed door) when participating in a therapy phone call. Each subsequent T-CBT session was scheduled in advance and lasted approximately 45 min. In the case of a psychiatric emergency participants would be directed by their therapist to an urgent care facility and the study psychiatrist would be contacted to facilitate the participant’s access to care. None of the study participants required this level of care.
Control Condition
The control condition was intended to be treatment-as-usual within the HIV clinic and therefore consisted of a non-manualized 11 sessions of CBT provided by clinic therapist without study supervision. Participants were scheduled for an appointment with a psychotherapist at their HIV clinic. The psychotherapy was conducted in accordance with psychotherapy treatment provided at the clinic. Sessions were scheduled for 60-min blocks. As both HIV clinics had on-site mental health teams, therapy appointments were set up using the existing administrative and clinical procedures employed by the clinic when scheduling a mental health appointment. In the case of a psychiatric emergency, the therapists were instructed to contact an on-site psychiatrist. None of the study participants required this level of care. In order to keep as close to usual clinical practice as possible, the number of appointments was left to the judgment of the therapist and based on clinical need.
Schedule of Assessment and Outcome Measures
All assessments were completed by interview with a trained research assessor. Research assessments were conducted at baseline, midpoint (week 7) and at the conclusion of the intervention (week 14). All baseline interviews were conducted in person. Follow-up interviews could be conducted either in person or on the phone. Participants were paid $10.00 for their first assessment, $40.00 for their midpoint assessment and $50.00 for their final assessment. All research assessors were trained to provide all outcome measures and were masked to treatment allocation. To assess the primary outcome of depression, the Hamilton depression rating scale (HAM-D) [27, 28] and the quick inventory of depressive symptomology (QIDS-SR) [29] were used. To assess the therapeutic process between the participant and therapist we used the working alliance inventory (WAI) [30]. To assess satisfaction, we used the satisfaction index-mental health (SIMH) [31]. To assess adherence to antiretroviral medication we used a validated telephone based pill counting method [32]. All participants receiving HAART at their baseline visit were trained how to count their pills. This training included teaching them how to: (i) prepare a comfortable, flat surface that is near the phone; (ii)sort their medications if necessary; (iii) select a medication, report the prescription number, refill date and dispensed quantity; and (iv) use a pharmacist tray and cup (provided by the study) to double count their medication. Participants were also informed that they would be asked to specify whether they had lost or gained any pills since the previous phone contact and whether they had taken any medication that day. An unannounced telephone pill count occurred three times during the study. The first time to determine the amount of pills they had at home occurred 7–12 days after being taught how to count their pills. Unannounced pill count calls then occurred two more times, once approximately 1 month after first pill count and again approximately 2 months after the first pill count. A masked research assistant trained to carry out the unannounced telephone based pill count contacted the participants. These telephone contacts occurred separately from the telephone based intervention. Adherence was calculated as the difference between pills counted at the two times divided by the pills prescribed, taking into account the number of pills dispensed, pills lost, gained and taken that day.
Analysis
Univariate distributions included percentages for bivariate and categorical variables and means and medians for continuous variables. General linear mixed models (SAS, v9.2, Proc Mixed) were used to assess change over time for the two depression measures. We used intent to treat analysis such that all data from the randomized subjects were included in the models. The predictors were treatment condition, time and the treatment by time interaction. To aid in interpretation of findings effect sizes were calculated for each outcome. Although there was no formal data imputation strategy, the use of Proc Mixed allowed for the use of all available data from each subject. Significance was based on p < 0.05, two tailed.
Results
Participants
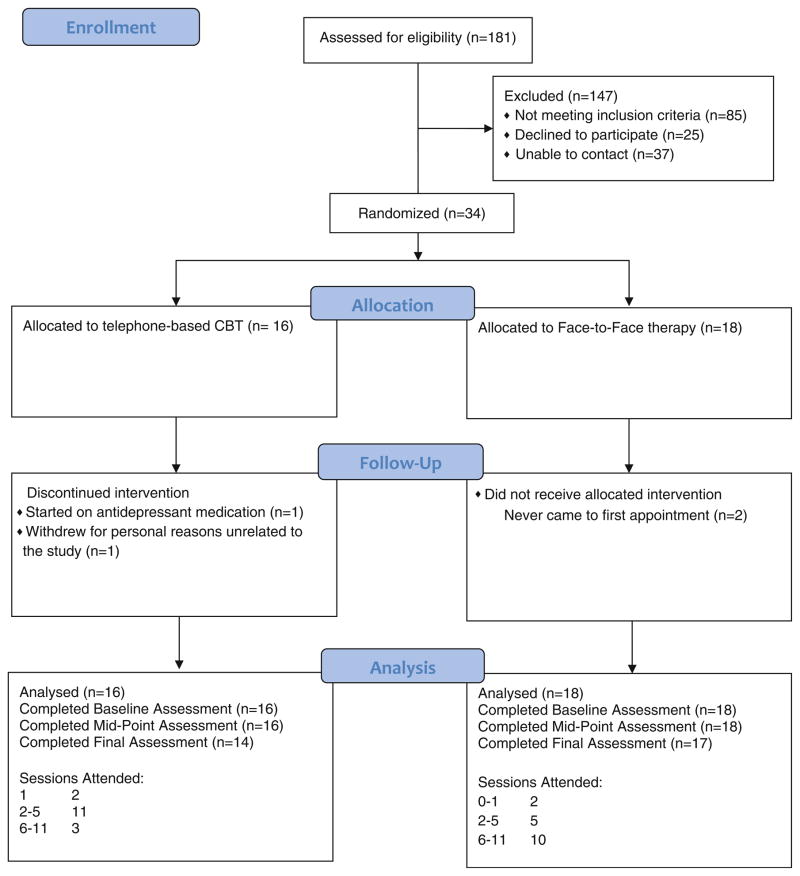
One hundred nineteen of the 181 individuals eligible for study screening (based on their PHQ-9 scores) were screened. The flow of patients, resulting in 35 participants is displayed in Fig. 1. Eighty-five did not meet eligibility criteria. Reasons for not meeting eligibility criteria included: 18 (21 %) did not meet criteria for depression, 8 (9.4 %) people had hypomania or psychosis, 8 (9.4 %) could not pass the WRAT, 5 (5.8 %) had suicidal symptoms, 4 (4.7 %) did not have a phone. The remainder had multiple exclusion issues 42(49.4 %).
Fig. 1.
CONSORT 2010 flow diagram
Of the 62 who did not participate in the screening part of the study—25 actively refused to participate and 37 could not be contacted (i.e., telephone not in service). Those who actively refused to participate in the study were not statistically different from those who consented to participate in the screening part of the study as assessed on the variables of age, gender and race.
Of the 34 enrolled participants, 16 were randomized to T-CBT intervention and 18 to f2f psychotherapeutic treatment. Four individuals were withdrawn from the study. Two individuals randomized to receive the f2f treatment never received allocated treatment. One individual randomized to receive T-CBT was withdrawn from the study after being prescribed antidepressant treatment in violation of the protocol and one person randomized to receive T-CBT self-withdrew or reasons not related to the study or treatment received (Fig. 1). All were included in the final analysis.
Demographic Characteristics
On average participants were aged 45.1 (SD ± 8.3) years, self described their race as black (94.1 %) and were female (73.5 %). The majority had completed high school (64.7 %), reported earnings of <$10,000 per year (70.6 %). The majority also had a history of substance dependence (55.8 %). About half were prescribed HAART (n = 18). There were no differences in the total number of pills taken per day comparing the f2f group (mean 2.5 pills) to the telephone psychotherapy group (mean 2.4 pills).
The average HAM-D depression score at baseline was 23.6 ± 5.2 and the average QIDS-SR score at baseline was 16.7 ± 3.7. Both these scores represent severe depressive symptoms. There were no statistically significant differences on baseline demographic characteristics or depression rating scales results comparing those randomized to T-CBT to those randomized to f2f therapy (Table 1).
Table 1.
Sample Characteristics
| Variable | Total sample (n = 34) | Telephone based CBT (n = 16) | Face-to-face psychotherapy (n = 18) | p Value |
|---|---|---|---|---|
| Demographics | ||||
| Age | 45.12 ± 8.33 | 42.47 ± 7.95 | 46.78 ± 8.87 | 0.141a |
| Female | 25 (73.5 %) | 12 (70.6 %) | 13 (72.2 %) | 1.000b |
| Race | 0.229b | |||
| Black | 32 (94.1 %) | 15 (88.2 %) | 18 (100.0 %) | |
| American Indian | 1 (2.9 %) | 1 (5.9 %) | 0 (0.0 %) | |
| Other | 1 (2.9 %) | 1 (5.9 %) | 0 (0.0 %) | |
| Ethnicity | 0.229b | |||
| Hispanic | 2 (5.7 %) | 2 (11.8 %) | 0 (0.0 %) | |
| Education | 0.811b | |||
| 8th grade or below | 3 (8.6 %) | 1 (5.9 %) | 2 (11.1 %) | |
| Some high school | 9 (26.5 %) | 5 (29.4 %) | 4 (22.2 %) | |
| High school/GED | 11 (32.3 %) | 7 (41.2 %) | 5 (27.8 %) | |
| Some college | 10 (29.4 %) | 4 (23.5 %) | 6 (33.3 %) | |
| College or higher | 1 (2.9 %) | 0 (0.0 %) | 1 (5.6 %) | |
| Income | 0.521b | |||
| Less than $10,000 | 24 (70.6 %) | 11 (64.7 %) | 14 (77.8 %) | |
| $10,000–$30,000 | 8 (23.5 %) | 4 (23.5 %) | 4 (22.2 %) | |
| $30,000–$50,000 | 2 (5.9 %) | 2 (11.8 %) | 0 (0.0 %) | |
| History of drug dependence | 19 (55.8 %) | 9 (56.2 %) | 10 (55.5 %) | 0.93b |
| Depression score | ||||
| HAM-D score | 23.65 ± 5.25 | 22.71 ± 5.03 | 24.56 ± 5.28 | 0.297a |
| QIDS-score | 16.68 ± 3.72 | 16.76 ± 4.37 | 17 ± 3.46 | 0.860a |
T test
Fisher exact test
Depression Outcome
There were no statistically significant differences in depression treatment outcomes comparing f2f psychotherapy to T-CBT whether evaluating outcomes on the HAM-D (15.9 ± 7.2 vs. 16.3 ± 8.6; p = 0.32) or on the QID-SR (9.2 ± 3.7 vs. 10.8 ± 5.5; p = 0.28) (Table 2). Within group evaluation demonstrated that both the T-CBT and the f2f psychotherapy groups resulted in clinically meaningful, significant reductions in depressive symptoms as measured by the HAM-D (T-CBTd = −0.9, p = 0.04 and f2f psychotherapy, d = −1.2, p = 0.001) as well as the QIDS-SR (T-CBT d = −1.0, p = 0.02 and f2f psychotherapy, d = −1.5, p = 0.001). None of the participants discontinued treatment due to adverse events (Table 3).
Table 2.
Change in depression over time comparing T-CBT to f2f treatment
| Variable | Baseline
|
Midpoint
|
Post
|
Baseline Versus midpoint p value | Baseline versus post p value | |||
|---|---|---|---|---|---|---|---|---|
| T-CBT (n = 16) | f2f (n = 18) | T-CBT (n = 16) | f2f (n = 18) | T-CBT (n = 16) | f2f (n = 18) | |||
| HAM-D | 22.6 ± 5.2 | 24.6 ± 5.3 | 17.1 ± 4.8 | 17.6 ± 6.4 | 16.3 ± 8.6 | 15.9 ± 7.2 | 0.41 | 0.32 |
| QID-S | 16.3 ± 4.1 | 17.0 ± 3.5 | 13.1 ± 4.7 | 11.9 ± 5.6 | 10.8 ± 5.5 | 9.2 ± 3.7 | 0.34 | 0.21 |
Table 3.
Effect size associated with within group change in depression over time
| T-CBT | Baseline | Midpoint | Follow-up | Within group effect size
|
|
|---|---|---|---|---|---|
| Baseline versus midpoint | Baseline versus follow-up | ||||
| HAM-D | 22.6 ± 5.2 | 17.1 ± 4.8 | 16.3 ± 8.6 | −0.98 | −0.86 |
| QID-S | 16.3 ± 4.1 | 13.1 ± 4.7 | 10.8 ± 5.5 | −0.70 | −1.03 |
| f2f | |||||
| HAM-D | 24.6 ± 5.3 | 17.6 ± 6.4 | 15.9 ± 7.2 | −1.03 | −1.16 |
| QID-S | 17.0 ± 3.5 | 11.9 ± 5.6 | 9.2 ± 3.7 | −0.99 | −1.48 |
Number of Sessions
On average participants attended 5.2 ± 3.1 sessions. Those randomized to the T-CBT intervention attended 4.1 ± 2.7 sessions which was not statistically significantly different from those randomized to the f2f psychotherapy intervention who attended 6.3 ± 3.1 sessions (T-CBT vs. f2f, t = −1.30, p = 0.20).
Satisfaction and Working Alliance
Those randomized to T-CBT were not significantly different from the reported high levels of satisfaction reported by those randomized to receive f2f psychotherapy (63.0 ± 8.6 vs. 65.6 ± 5.7; t = −0.90, p = 0.38). Similarly, those randomized to T-CBT were not significantly different from the reported working alliance scores reported by those randomized to receive f2f psychotherapy (74.4 ± 4.7 vs. 74.0 ± 9.1; t = 0.90, p = 0.93).
HAART Adherence Outcome
At first assessment, those randomized to receive f2f therapy reported adherence to be 77 % which was not significantly different from the adherence reported by those randomized to T-CBT which was 82 % (0.77 ± 0.33 vs. 0.82 ± 0.23; t = 0.59, p = 0.56) At study conclusion, those who received the T-CBT were significantly more likely to maintain their adherence to antiretroviral medication (83 %) as compared to those randomized to receive f2f treatment whose adherence declined to 68 %. (0.83 ± 0.27 vs. 0.68 ± 0.21, t = 2.07; p = 0.04, effect size: 0.60).
Conclusions
This study is among the first to demonstrate that T-CBT is efficacious in the treatment of major depression among low income, urban dwelling minority patients. Our study found that T-CBT was feasible to deliver and resulted in levels of satisfaction and therapeutic alliance that are not significantly different from f2f therapy. Depressive symptoms were significantly reduced in both treatment arms and associated with large effect sizes (f2f (HAM-D, effect size = −1.2) and T-CBT (HAM-D, effect size = −0.90)). Our results build on previous studies that have demonstrated that T-CBT is a feasible, acceptable and efficacious treatment for major depression [15–17]. Our study also extends those previous findings by providing evidence that telephone based interventions can result in improvement in depression among economically disadvantaged individuals [33]. It is important to note that we did not provide telephones to participants nor did we incentivize attendance of therapy sessions. We believe this adds to the external validity of our findings and is an important strength of the study.
Two previous controlled trials have evaluated the use of telephone based individual interventions to improve depressive symptoms among those with HIV [34, 35]. These two studies had mixed results. The first study conducted by Stein et al. [35] evaluated the efficacy of a 12 session telephone support behavioral intervention compared to assessment only-control group among HIV positive patients with Beck depression inventory scores greater than 10. The authors concluded that the telephone support behavioral intervention was not associated with reductions in depression symptoms. It is important to note that this study was not designed to target nor treat patients with major depression and therefore may have lacked the specificity and potency necessary to properly evaluate a depression associated treatment effect. The second study conducted by Ransom et al. [34.] evaluated the preliminary efficacy of a 6 session telephone based interpersonal psychotherapy (IPT) intervention targeting depression among rural, white, HIV infected individuals (the majority of whom were male). The study found that telephone-delivered IPT resulted in a significant change in depressive symptoms that was superior to treatment as usual. However, both treatment and intervention groups remained in the moderate depressed range at the completion of the study. An important limitation of this study was the reported concomitant receipt of additional mental health interventions by a large number of participants in both treatment and control arms.
The positive results of our randomized controlled trial extends previous research from a previous single arm Phase I trial conducted by our group that found support for the T-CBT model in treating this population. Specifically, we found that the T-CBT model was feasible, acceptable and resulted in a large and clinically meaningful reduction in depressive symptoms [20]. The results of our study build on the findings of Ransom et al. and support the use of telephone based interventions in a more diverse sample of HIV infected people with major depression including women and ethnic minorities. This is particularly important as few studies have evaluated the efficacy of CBT targeting depression specifically among African–Americans [12]. The results of our study also extend previous research demonstrating the efficacy of cognitive behavioral interventions among those with HIV and depression. Safren et al. [36.] found that f2f CBT significantly improved depressive symptoms among a sample of HIV patients with major depression compared to wait list control. The intervention was associated with a large and clinically meaningful effect size (HAM-D, effect size = 0.90). Similar to the Safren et al. study, our study found very similar large effects in both the f2f (HAM-D, effect size = 1.2) and T-CBT (HAM-D, effect size = 0.90) arms. Like Safren et al., our treatment interventions did not produce a complete remission of depressive symptoms. We believe this was likely due to the complex nature of the somatic and psychiatric symptoms that we were evaluating in the context of HIV infection, some of which may not be uniquely related to depression (i.e., weight, energy level and somatization).
One randomized control trial found that among depressed, low income, African–American and Hispanic women, CBT was as likely to lead to reductions in depression compared to whites [37]. Similar to our findings, Miranda et al. [37] reported that the majority of participants received about half of the treatment sessions. A recent study evaluating the use of telephone based CBT targeting depression among Latino patients living in rural areas found similar significant reductions in depression with a little more than half of the treatment sessions being attended [38]. Again these findings were similar to ours suggesting that limited session attendance, although not as intended, can result in significant reductions in depressive symptoms. It is possible that for this sample reductions in depressive symptoms may occur early in treatment which may suggest that a shorter course of treatment may be warranted and may perhaps be preferred.
An interesting and important finding of our study is that adherence to antiretroviral medication appeared to be significantly better in the T-CBT group compared to f2f treatment group. There are several possible reasons for this finding. First, it is possible the telephone psychotherapy sessions which occurred in close proximity to the place where individuals prefer to take their medication (i.e., home) may have served as an additional reminder to take their medication. Second, the decrease in depressive symptom in the context of these well-placed reminders may have led to improvements in adherence and may explain why the f2f treatment group had worse adherence even with improvements in their depressive symptoms. The intriguing possibility that telephone therapy may mediate the effect of depression treatment on improving adherence could be evaluated in the context of a future randomized control trial.
Our study does have several limitations. First, the focus of this study was on feasibility testing and not necessarily on hypothesis testing. Thus, while our findings are consistent with a recent large non-inferiority trial comparing T-CBT to f2f-CBT [33], it may be premature to draw any inferences regarding the equivalence of T-CBT and f2f in this population. Second, we did not collect long-term treatment assessments and therefore we were not able determine whether the improvement in depression or adherence were sustained over time. Third, participants had to agree to f2f treatment. Therefore, we may have excluded precisely those who would benefit most from T-CBT. Fourth, this is a small sample, and small samples can include biases that affect both internal and external validity. This may be an important limitation with respect to our adherence analysis as only about half of the participants were prescribed HAART. Nonetheless, meaningful information can be interpreted. The participants successfully completed the intervention and reported satisfaction with the therapy. The participants began the intervention with severe depression and their depression scores were significantly reduced at the final assessment. Fifth, although not statistically significantly, those randomized to the f2f treatment group had a larger effect size for the depression outcomes compared to those randomize to the T-CBT condition. Finally, the proportion of patients on HAART may seem low due to the reluctance of some providers to initiate HAART treatment when patients are depressed.
In summary our study found that low-income, urban dwelling HIV infected depressed individuals showed significant improvements in depression when treated with T-CBT. T-CBT was also found to improve adherence to HIV medication compared with f2f treatment. In order to meet the increasing demand for mental health care in the era of the Health Care Affordability Act, policy makers and insurance companies may increasingly turn to technologically mediated forms of treatment to provide ongoing access to care. Clearly telephone based care will be one important method of meeting this increase demand. As ownership of cell phones and smartphones continues to increase among minority and low income individuals, decreasing historical disparities in access to communications technologies [39, 40] the potential power and utility of using telephones to provide mental health treatment to disadvantaged communities increases. This may be particularly important to individuals with HIV and depression who may receive the additional benefit of improved adherence to HIV treatment. This study has demonstrated the feasibility of using the telephone to deliver care, underscoring the potential utility of future research examining the use of the telephone in extending and improving mental health treatment for potentially disenfranchised communities.
Acknowledgments
This project was supported by the National Institute of Mental Health (R34-MH80630)
Footnotes
Disclaimer The views expressed in this paper are those of the authors. No official endorsement by the National Institutes of Health is intended or should be inferred.
Contributor Information
Seth Himelhoch, Email: shimelho@psych.umaryland.edu, Department of Psychiatry, Division of Services Research, University of Maryland School of Medicine, 737 West Lombard St., Room 516, Baltimore, MD 21212, USA.
Deborah Medoff, Department of Psychiatry, Division of Services Research, University of Maryland School of Medicine, 737 West Lombard St., Room 516, Baltimore, MD 21212, USA.
Jennifer Maxfield, Mid-America Christian University College of Adult and Graduate Studies, Oklahoma City, OK, USA.
Sarah Dihmes, Baltimore, MD, USA.
Lisa Dixon, New York State Psychiatric Institute, New York, NY, USA.
Charles Robinson, Department of Psychiatry, Division of Services Research, University of Maryland School of Medicine, 737 West Lombard St., Room 516, Baltimore, MD 21212, USA.
Wendy Potts, Department of Psychiatry, Division of Services Research, University of Maryland School of Medicine, 737 West Lombard St., Room 516, Baltimore, MD 21212, USA.
David C. Mohr, Department of Preventive Medicine, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
References
- 1.Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–8. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 2.Fairfield KM, Libman H, Davis RB, Eisenberg DM. Delays in protease inhibitor use in clinical practice. J Gen Intern Med. 1999;14(7):395–401. doi: 10.1046/j.1525-1497.1999.08198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gordillo V, del Amo J, Soriano V, Gonzalez-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS. 1999;13(13):1763–9. doi: 10.1097/00002030-199909100-00021. [DOI] [PubMed] [Google Scholar]
- 4.Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, Perkins DO, et al. Progression to AIDS: the effects of stress, depressive symptoms, and social support. Psychosom Med. 1999;61(3):397–406. doi: 10.1097/00006842-199905000-00021. [DOI] [PubMed] [Google Scholar]
- 5.McDaniel JS, Fowlie E, Summerville MB, Farber EW, Cohen-Cole SA. An assessment of rates of psychiatric morbidity and functioning in HIV disease. Gen Hosp Psychiatry. 1995;17(5):346–52. doi: 10.1016/0163-8343(95)00066-z. [DOI] [PubMed] [Google Scholar]
- 6.Cook JA, Cohen MH, Burke J, Grey D, Anastos K, Kirstein L, et al. Effects of depressive symptoms and mental health quality of life on use of highly active antiretroviral therapy among HIV-seropositive women. J Acquir Immune Defic Syndr. 2002;30(4):401–9. doi: 10.1097/00042560-200208010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV epidemiology research study. JAMA. 2001;285(11):1466–74. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- 8.Himelhoch S, Medoff DR. Efficacy of antidepressant medication among HIV-positive individuals with depression: a systematic review and meta-analysis. AIDS Patient Care STDS. 2005;19(12):813–22. doi: 10.1089/apc.2005.19.813. [DOI] [PubMed] [Google Scholar]
- 9.Himelhoch S, Medoff DR, Oyeniyi G. Efficacy of group psychotherapy to reduce depressive symptoms among HIV-infected individuals: a systematic review and meta-analysis. AIDS Patient Care STDS. 2007;21(10):732–9. doi: 10.1089/apc.2007.0012. [DOI] [PubMed] [Google Scholar]
- 10.Himelhoch S, Josephs JS, Chander G, Korthuis PT, Gebo KA. Use of outpatient mental health services and psychotropic medications among HIV-infected patients in a multisite, multistate study. Gen Hosp Psychiatry. 2009;31(6):538–45. doi: 10.1016/j.genhosppsych.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the national Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 12.Voss Horrell SC. Effectiveness of cognitive-behavioral therapy with adult ethnic minority clients: A review. Prof Psychol ResPract. 2008;39(2):160–8. [Google Scholar]
- 13.Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry. 2001;158(5):725–30. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- 14.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 15.Mohr DC, Likosky W, Bertagnolli A, Goodkin DE, Van Der WJ, Dwyer P, et al. Telephone-administered cognitive-behavioral therapy for the treatment of depressive symptoms in multiple sclerosis. J Consult Clin Psychol. 2000;68(2):356–61. doi: 10.1037//0022-006x.68.2.356. [DOI] [PubMed] [Google Scholar]
- 16.Mohr DC, Hart SL, Julian L, Catledge C, Honos-Webb L, Vella L, et al. Telephone-administered psychotherapy for depression. Arch Gen Psychiatry. 2005;62(9):1007–14. doi: 10.1001/archpsyc.62.9.1007. [DOI] [PubMed] [Google Scholar]
- 17.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292(8):935–42. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 18.Mohr DC, Hart SL, Howard I, Julian L, Vella L, Catledge C, et al. Barriers to psychotherapy among depressed and nondepressed primary care patients. Ann Behav Med. 2006;32(3):254–8. doi: 10.1207/s15324796abm3203_12. [DOI] [PubMed] [Google Scholar]
- 19.Heckman TG, Somlai AM, Peters J, Walker J, Otto-Salaj L, Galdabini CA, et al. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10(3):365–75. doi: 10.1080/713612410. [DOI] [PubMed] [Google Scholar]
- 20.Himelhoch S, Mohr D, Maxfield J, Clayton S, Weber E, Medoff D, et al. Feasibility of telephone-based cognitive behavioral therapy targeting major depression among urban dwelling African–American people with co-occurring HIV. Psychol Health Med. 2011;16(2):156–65. doi: 10.1080/13548506.2010.534641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD, et al. The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom. 2009;78(5):275–84. doi: 10.1159/000228248. [DOI] [PubMed] [Google Scholar]
- 22.Spitzer R, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. J Am Med Assoc. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 23.Wilkinson GS, Robertson GJ, editors. WRAT4:Wide range achievement test professional manual. 4. Lutz: American Psychological Association; 2006. [Google Scholar]
- 24.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 25.Power C, Selnes OA, Grim JA, McArthur JC. HIV Dementia Scale: a rapid screening test. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;8(3):273–8. doi: 10.1097/00042560-199503010-00008. [DOI] [PubMed] [Google Scholar]
- 26.Barber JP, Liese BS, Abrams MJ. Development of the cognitive therapy adherence and competence scale. Psychother Res. 2003;13(2):205–21. [Google Scholar]
- 27.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williams JB, Kobak KA, Bech P, Engelhardt N, Evans K, Lipsitz J, et al. The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. Int Clin Psychopharmacol. 2008;23(3):120–9. doi: 10.1097/YIC.0b013e3282f948f5. [DOI] [PubMed] [Google Scholar]
- 29.Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–83. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 30.Horvath AO, Greenberg LS. Development of the working alliance inventory. J Couns Psychol. 1989;36:223–33. [Google Scholar]
- 31.Nabati L, Shea N, McBride L, Gavin C, Bauer MS. Adaptation of a simple patient satisfaction instrument to mental health: psychometric properties. Psychiatry Res. 1998;77(1):51–6. doi: 10.1016/s0165-1781(97)00122-4. [DOI] [PubMed] [Google Scholar]
- 32.Kalichman S, Amaral C, Stearns H, White D, Flanagan J, Pope H, et al. Adherence to antiretroviral therapy assessed by unannounced pill counts conducted by telephone. J Gen Intern Med. 2007;22(7):1003–6. doi: 10.1007/s11606-007-0171-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, et al. Effect of telephone-administered versus face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: a randomized trial. JAMA. 2012;307(21):2278–85. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ransom D, Heckman TG, Anderson T, Garske J, Holroyd K, Basta T. Telephone-delivered, interpersonal psychotherapy for HIV-infected rural persons with depression: a pilot trial. Psychiatr Serv. 2008;59(8):871–7. doi: 10.1176/ps.2008.59.8.871. [DOI] [PubMed] [Google Scholar]
- 35.Stein MD, Herman DS, Bishop D, Anderson BJ, Trisvan E, Lopez R, et al. A telephone-based intervention for depression in HIV patients: negative results from a randomized clinical trial. AIDS Behav. 2007;11(1):15–23. doi: 10.1007/s10461-006-9131-5. [DOI] [PubMed] [Google Scholar]
- 36.Safren SA, O’Cleirigh C, Tan JY, Raminani SR, Reilly LC, Otto MW, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28(1):1–10. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, et al. Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA. 2003;290(1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 38.Dwight-Johnson M, Aisenberg E, Golinelli D, Hong S, O’Brien M, Ludman E. Telephone-based cognitive-behavioral therapy for Latino patients living in rural areas: A randomized pilot study. Psychiatr Serv. 2011;62:936–42. doi: 10.1176/ps.62.8.pss6208_0936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lenhart A. Pew Research Center, editor. Cell Phones and American Adults. Sep 2, 2010. http://pewinternet.org/Reports/2010/Cell-Phones-and-American-Adults.aspx .
- 40.Smith A. Mobile Access 2010. Pew Internet and American Life Project; Jul 7, 2010. http://pewinternet.org/Reports/2010/Mobile-Access-2010.aspx . [Google Scholar]