Paget`s Disease of bone is a chronic condition characterized by altered bone resorption, bone formation, and bone remodeling, which leads to distorted bony anatomy and aberrations in normal joint mechanics, with possible subsequent degenerative changes of the affected joints.17,34 Since its first description in 1877, various infectious, genetic and environmental8,9,18,21,24,29,42 theories have been proposed as the source of the disease, yet the true pathogenesis remains unclear. After osteoporosis, Paget`s disease of bone is the second most common disease associated with bone remodeling.5 Although rarely found in patients younger the 40 years, the incidence drastically increases to 1.5%-3% in patients older than 60 years in the United States.17 However, pharmacological management is commonly sufficient to relief symptoms and control osteolytic lesions, and only few patients require surgical management. While common manifestations are found in the pelvis, lumbosacral spine, the tibia and the femur, involvement of the upper extremity is rare.33 Consequently, there is a larger number of reports concerning total hip arthroplasty10,11,25,26,37,44 and total knee arthroplasty4,20,26,38 in patients with Paget`s disease, and the collective experience in arthroplasty of the joints of the upper extremity in patients with Paget`s disease is very limited. Specifically, currently only 2 case reports exist regarding total shoulder arthroplasty in patients suffering from shoulder osteoarthritis due to Paget`s disease.13,33
To our knowledge, however, there has not been a description of the surgical management of end-staged elbow osteoarthritis associated with Paget`s disease. The purpose for this report is to demonstrate a successful elbow joint replacement in a patient with Paget’s disease and provide recommendations for similar orthopedic issues in the future, considering the existing literature and our personal experience.
Case presentation
Patient history
The patient is a 67-year-old Caucasian male who first presented to a local orthopedist due to right shoulder pain, which was treated with a subacromial corticosteroid injection. On the follow-up visit, the patient declared no improvement of his shoulder pain, yet mentioned a recently discovered deformity of his right elbow with progressive extension deficit and a repetitive dysesthesia of the right forearm and hand. Elbow pain was denied at that time. On physical examination, the patient could flex the elbow to 130° with an extension deficit of 30°. Furthermore, a positive Tinel`s sign was found in the region of the ulnar sulcus.
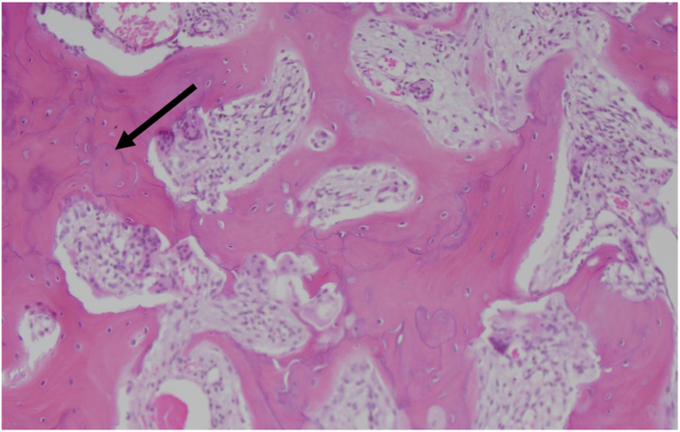
Plain radiographs of the elbow showed distension of the distal humerus with inhomogeneous osteolytic structures, the aspect of a thickened cortical bone and early signs of humeroradial and humeroulnar arthrosis. Magnetic resonance imaging presented abnormal cancellous bone, yet was not conclusive for a malignant tumor. Skeletal scintigraphy demonstrated isolated involvement of the right humerus. To rule out sarcomatous transformation, the tumoral mass in the distal humerus was biopsied. Histologically, the bone appeared in a mosaic pattern, with multiple cement lines that demarcated randomly oriented lamellar bone, consistent with Paget’s Disease of bone (Fig. 1). Considering the paucity of bone manifestation in the bone scan other than the elbow, the presence of a monostotic Morbus Paget of the elbow was concluded. Due to the oligosymptomatic presentation of the patient and only mild osteoarthritic changes, a conservative treatment with bisphosphonate therapy was recommended. Unfortunately, the patient did not appear to any subsequent follow-up visits at the treating orthopedic surgeon, thus the mentioned treatment could never be initiated.
Figure 1.
Cylindrical bone biopsy of the distal right humerus revealing bony mosaic pattern with thick cement lines ( ) that demarcate randomly oriented lamellar bone.
) that demarcate randomly oriented lamellar bone.
Preoperative evaluation
Ten years later, the patient was referred to our clinic by his family physician. He reported progressive motion deficit and pain that was worsened by manual activities. Additionally, the patient mentioned hypesthesia in his ulnar, right hand. On physical examination, obvious deformity at the distal humerus especially at the medial epicondyle was present. The patient could flex the elbow to 90°, with an extension deficit of 40°. Active and passive flexion and extension about the elbow inflicted pain, especially at the end of range of motion. Pronation and supination were not limited. Furthermore, hypothenar atrophy, hyposensitivity in the ulnar territory of the hand as well as a positive Froment-sign concluded the presence of a sensomotoric ulnar nerve damage, which later was confirmed with electrodiagnostic studies.
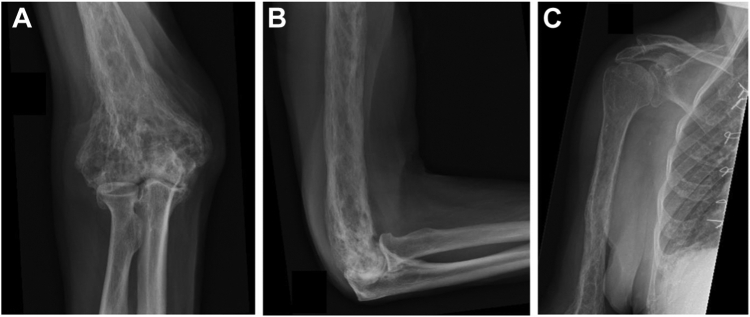
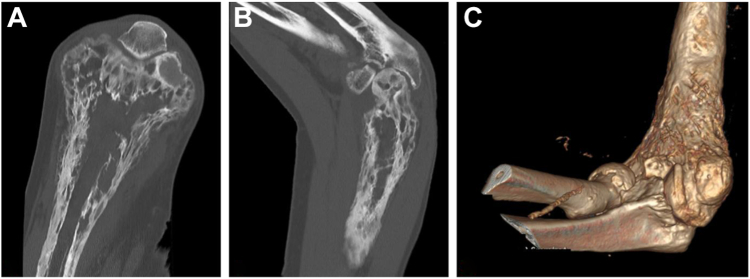
Plain radiographs showed characteristic findings of monostotic Paget’s disease of the humeral epiphysis and metaphysis up to the proximal third of the humeral shaft with sclerotic changes in a trabecular pattern, as well as advanced degenerative joint disease of the elbow (Fig. 2). A computed tomography (CT) scan showed typical cortical infraction sites with intensive osteolysis and osteosclerosis, leading to deformation of the medial epicondyle and the ulnar nerve sulcus. No evidence was apparent for a novel malignant transformation (Fig. 3). Laboratory values for alkaline phosphate were unremarkable, indicating an inactive disease state at the time of planned surgery.
Figure 2.
Anteroposterior (A) and lateral (B) view of the right elbow, as well as anteroposterior view of the right shoulder (C), demonstrating Paget’s disease involvement of the humerus up to its proximal third of the shaft as well as advanced humeroradial and humeroulnar arthrosis.
Figure 3.
CT scan images of the right elbow demonstrating local changes of anatomy and altered bone quality with multiple osteolytic lesions in the distal humerus as part of preoperative planning (coronal (A), sagittal (B) and 3D-reconstruction (C)). CT, computed tomography.
After discussion of the case at the annual Mayo Clinic elbow meeting in 2019, the decision was made to treat the patient with a total elbow arthroplasty in combination with decompression and translocation of the ulnar nerve.
Preoperative surgical planning
Before surgery, plane radiographs of the whole affected bone as well as CT scans of the affected area were investigated to assess the extent of Paget`s Disease, screen for areas of bony defects, dense osteosclerosis and hypertrophic bone formation as well as distorted alignment of the joint and adjacent diaphysis. Profound osteolysis should either be grafted or bypassed by a long stem to reduce the risk of periprosthetic fractures, thus sufficiently long stems should be available at the time of surgery. In case of alignment distortion, corrective osteotomies might be necessary to use sufficiently long stems, which must be anticipated during preoperative planning. On the other hand, dense intramedullary osteosclerosis might complicate canal preparation, thus fluoroscopy, burrs, power drills, and cannulated reamers should be available during the procedure, although care should be taken to avoid canal penetration with subsequent cement leakage. Finally, surgeons should be prepared to resect any hypertrophic bone formation to avoid implant malpositioning and component impingement.
Surgery
After general anesthesia was induced, the patient was placed in a supine position on the operating table. Preoperative antibiotics were administered before skin incision and for 24 hours postoperatively. Packed red blood cells and an intraoperative blood salvage system were available at the start of the case. The right upper extremity was prepped and draped in a usual sterile manner. Finally, a sterile tourniquet was applied before skin incision.
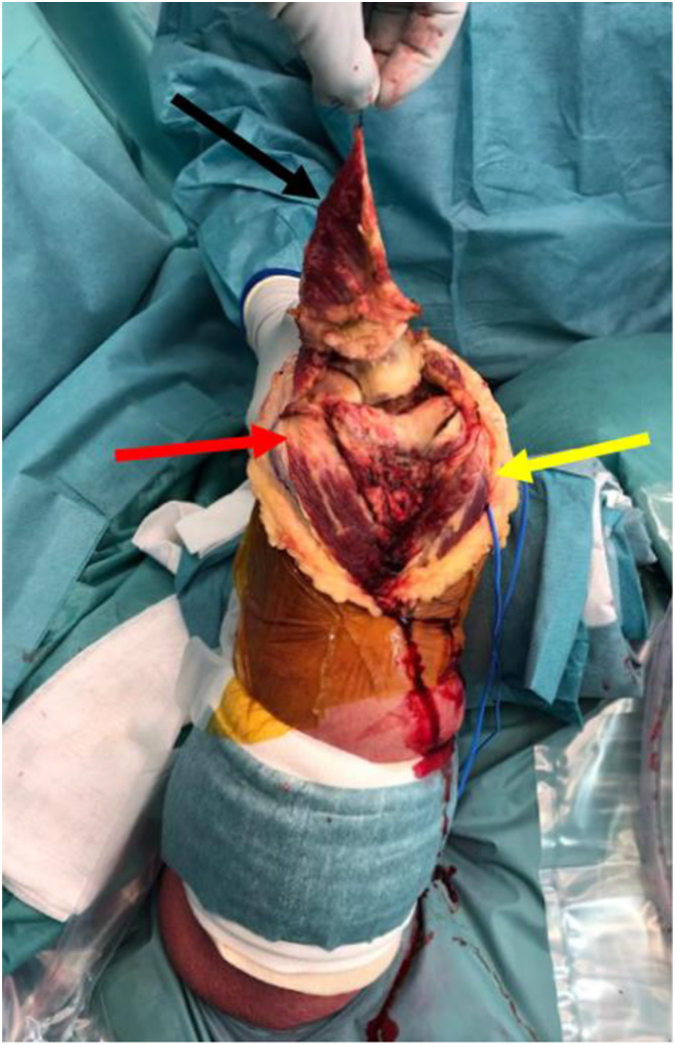
To approach the elbow joint, a diamond popup approach, as introduced by Professor Shawn W. O`Driscoll, was utilized. Exposition and decompression of the ulnar nerve was performed after mobilization of skin flaps. Starting approximately 5-7 cm distal to the tip of the olecranon, the fascia of the forearm was opened up and the incision was advanced proximally on the medial and lateral boarder of the ulna around the tip of the olecranon, leaving a small cuff of tissue on each side for later refixation. The fascial incisions were then continued proximally along the musculotendinous junction of the triceps, and finally met at point about 5-7 cm proximal to the tip of the olecranon, thereby creating a diamond-shaped incision. The main triceps tendon was then dissected from the deep triceps muscle and mobilized to its insertion on the olecranon. An elliptical arthrotomy around the tip of the olecranon trough the posterior capsule and the deep triceps was performed, and the deep triceps was split in line with its fibers proximally. The posterior capsule was then released from the humeral shaft, thereby exposing the posterior joint. Thereafter, the radial collateral ligament together with the anconeus muscle and the ulnar collateral ligament together with the flexor carpi ulnaris muscle were peeled off subperiostally from the proximal ulna, leaving the collateral ligament and muscular insertion on the humerus untouched. After this release, the elbow joint can be dislocated by popping up the radius and ulna as a unit by hyperflexing the joint (Fig. 4). After debulking and resection of hypertrophic bone as well as part of the articular capsule, the trochlea was resected. The humeral canal was thereafter opened, reamed and rasped up to the planned size of the implant. To definitely exclude sarcoid transformation of the Paget disease, the extracted tissues were analyzed histologically. No malignancy could be found later on. Having the humeral component adjusted, the ulna was prepared in a similar fashion. To allow for optimal articulation, adequate clearance around the sigmoid notch has been ensured. Due to sufficient bone quality and the absence of larger osteolytic lesions in the humeral canal intraoperatively and on preoperative CT scan, it was decided to proceed with cemented component implantation only without impaction bone grafting according to the Ling technique.13 Furthermore, only a regular stem length was used, as bypassing the whole affected bone seemed not to be necessary due to the stable bone quality, and usage of longer stem would have been complicated by the altered alignment of the humeral diaphysis with an increased risk of canal perforation and component malpositioning due to the flexion deformity of the humerus.
Figure 4.
Intraoperative view on the dislocated elbow joint through a diamond popup approach. Black arrow ( ) indicates the reflected triceps tendon attached to the Olecranon. The
) indicates the reflected triceps tendon attached to the Olecranon. The  points out the distal humerus with osteoarthritic changes of the trochlea and the capitellum. The
points out the distal humerus with osteoarthritic changes of the trochlea and the capitellum. The  indicates the exposed ulnar nerve with a vessel-loop around it.
indicates the exposed ulnar nerve with a vessel-loop around it.
After copious irrigation and insertion of a cement restrictor in the humeral canal, antibiotic-loaded cement was injected into the humeral canal. Due to far proximal progression of the disease on the humerus, a long humeral stem (Zimmer NEXEL Total Elbow prothesis humeral component size 5/150 mm right; Zimmer Biomet, Warsaw, IN, USA) was inserted into the humerus and advanced to the appropriate depth. The ulnar canal was irrigated and the ulnar component (Zimmer NEXEL Total Elbow prothesis, ulnar component size 5/75 mm right; Zimmer Biomet, Warsaw, IN, USA) was cemented without the use of a cement restrictor. After cement hardening, remaining osteophytes were removed and the elbow was reduced. The elbow was taken through range of motion and found to be stable without evidence of impingement. To finally release the ulnar nerve from its entrapment causing the above-mentioned symptoms, it was transpositioned submuscularly. The diamond popup approach was then closed stepwise by reattaching the deep portion of the triceps to the olecranon and then repair the main tendon of the triceps with nonabsorbable sutures. The surgical wound was covered with a sterile dressing and the arm was placed in a brace.
Postoperative course
Postoperatively, the patient immediately began with functional aftercare of the elbow with actively assisted movements out of a sling and no restriction in range of motion. After an uneventful initial postoperative course, he was discharged on the third postoperative day. Unfortunately, he was readmitted to the clinic 2 days after discharge due to an ascending urinary tract infection as well as an accompanying acute cardiac decompensation aground subsegmental pulmonary embolism and a type II myocardial infarction in the context of a newly diagnosed atrial fibrillation and postoperative anemia. The further course was uneventful regarding the elbow and the patient was discharged again 3 weeks after surgery.
After 6 weeks, slight strengthening exercise was implemented with formal physical therapy. Three months postoperatively, the patient was able to return to all his daily activities. At his 2-year follow-up, the patient reported no pain in the elbow at rest or motion. There were no residual sensomotoric losses attributed to the former sensomotoric neuropathy of the ulnar nerve. His active range of motion had increased to 130 degrees of flexion with a remaining extension deficit of 30° (Fig. 5, A). Pronation and supination were unrestricted and possible up to 80°, respectively. His Mayo Elbow Performance index was 95 of 100. Radiographs demonstrated an intact cement mantle on the humeral and ulnar side and no evidence of component loosening. However, the ulnar component appeared to be implanted slightly to shallow, which might be a reason for the remaining extension deficit (Fig. 5, B).
Figure 5.
Two-year postoperative anteroposterior and lateral radiographs of the elbow demonstrating an intact cement mantel about the humeral and ulnar stem and no evidence of component loosening. Clinically, flexion was possible up to 130° with a remaining extension deficit of 30°.
Discussion
Paget’s disease of bone is a chronic condition of unknown etiology that rarely involves the upper extremity. Accordingly, while various authors have reported on their experience with endoprosthetic treatment in patients suffering from hip and knee disease,4,10,11,20,25,26,37,38,44 there is a paucity of literature regarding treatment of upper extremity Paget’s Disease with only 2 reports of total shoulder arthroplasty being performed in patients with end-stage degenerative glenohumeral joint disease in the setting monostotic humeral Paget’s Disease.13,33 To our knowledge, this is the first report of a total elbow arthroplasty being performed for degenerative joint disease of the elbow in the setting of a monostotic humeral Paget’s Disease, demonstrating good clinical results at a 2-year follow-up.
In many patients with Paget’s Disease, nonoperative management including bisphosphonate medications will be sufficient to control bone pain and suppress metabolic activity in asymptomatic patients.39 If nonoperative management provides insufficient pain relief, the source of pain must be evaluated carefully, as the disease can generate pain in miscellaneous ways, such as pain from the pathologic process itself, malignant transformation to Paget’s Sarcoma,3,27 occult fractures through abnormal bone, bone deformity with altered joint loading, and subsequent degenerative joint disease.33 Alkaline phosphatase levels can be used as a marker for disease activity and to monitor treatment.30,31 However, some authors reported only weak correlation between bone pain and metabolic activity reflected by elevated alkaline phosphatase levels levels.19,40 In case of inconclusive clinical findings in the setting of degenerative joint disease with concomitant Paget’s Disease, pain relief from diagnostic intraarticular injection might reinforce the suspicion of an intraarticular cause of pain.
Before any surgical intervention, a thorough medical check-up of the patient is recommended. Patients should be screened by a cardiologist, as the often hypovascularized bone in Paget’s disease can lead to increased cardiac output with impaired cardiac function,2,17,36 which might be even aggravated due to the frequently observed excessive blood loss during surgery in patients suffering from Paget’s Disease.15,16 To reduce the risk of excessive blood loss during surgery, some authors advocated the use of anti-Pagetic treatment such as bisphosphonates and calcitonin before elective surgery,14, 15, 16, 17,35,41 although there is currently insufficient evidence to support this recommendation.39 In any way, surgeons should be prepared to react to increased blood loss with the use of a cell saver system and blood products readily available on standby.17,33
Currently, 2-dimensional anteroposterior and lateral plain radiographs are commonly used for preoperative planning of total elbow arthropalsty, which is especially important in cases with gross deformities frequently observed in patients with Paget`s disease of bone. Although no commercial 3-dimensional planning software for total elbow arthroplasty is currently available, the usefulness of 3-dimensional templating regarding implant positioning and stem size prediction compared to 2-dimensional planning has already been demonstrated in an experimental study.12 Such templating tools might further facilitate the evaluation of distorted alignment and its impact on implant positioning, thus should be used in these cases as soon as available.
Intraoperatively, the surgeon should be prepared to address any kind of deformity related to Paget’s disease, which can be extensive in some cases and even require corrective osteotomies, to restore physiological alignment.7,17,35 Furthermore, hypertrophic bone, which is regularly observed in patients with Paget’s Disease, poses the risk of implant malpositioning and component impingement and should thus be resected to reapproximate the patient’s normal anatomy before implant insertion.33 To achieve adequate exposure of the elbow joint, allowing for sufficient release and debulking of any abundant bone mass as well as adequate canal preparation, the authors decided to use a diamond popup approach. This triceps-off approach was first introduced in 2018 by Professor Shawn W. O`Driscoll. Similarly to the Van Gorder approach,43 a tongue-shaped triceps fascial flap is created without detaching its insertion on the olecranon, followed by splitting the deep part of the triceps. However, conversely to the aforementioned approach, the collateral ligaments are not released from the distal humerus but peeled off from the ulna together with the anconeus and flexor carpi ulnaris muscles. Doing so, the elbow joint is splinted after reduction by a sleeve of tissue that is still attached to the distal humerus and inserts to the ulna further distally, thereby providing greater stability compared to approaches which include release of the collateral ligaments from the distal humerus.
Other frequently observed bony alterations in Paget’s Disease comprise both ectatic and obliterative intramedullary deformities.13,33 Ectatic deformities pose the risk for inadequate fixation of stemmed components with subsequent subsidence, as time zero-stability might be diminished.13 To improve this time zero-stability, the Ling technique, which comprises a combination of impaction bone grafting of allograft and cemented stem fixation has been proposed23 and successfully used in patients with Paget’s Disease of bone.13,22 However, other authors have demonstrated excellent results with a low rate of component loosening during the first decade after uncemented total hip arthroplasty in patients with Paget’s Disease,37 thus the use of cemented implants is not mandatory. Canal obliteration and thinned cortices on the other hand increase the risk for intraoperative fractures during canal preparation and stem insertion, which might be even higher in case of impaction bone grafting, thus the Ling technique should only be used with caution during endoprosthetic treatment in patients with Paget’s disease and must be considered depending on the patient`s situation. If used, prophylactic cerclage tapes or wires can be applied,13 and intraoperative imaging can be used to guide intramedullary instrumentation33 to mitigate the risk of fractures. In our case, there was no excessive ectasia of the humeral canal, thus we decided to use cemented components without impaction bone grafting, thereby achieving adequate stem fixation. Table I provides a summary of recommendations for patients with Paget’s disease undergoing endoprosthetic treatment.
Table I.
Pearls and pitfalls in surgical management of patients with Paget’s Disease.
| Preoperative | Intraoperative |
|---|---|
| Precisely identify source of pain before surgery |
|
| Exclude Paget’s sarcroma |
|
| Screen for cardiac abnormalities |
|
|
Finally, surgical treatment in patients with Paget’s Disease comprises an increased risk of heterotopic ossification,28,37 thus various authors have recommended heterotopic ossification prophylaxis either through radiation or pharmacological treatment.6,28,32 However, analogous to our experience, heterotopic ossification has not yet been reported in endoprosthetic treatment of patients with Paget’s Disease of the upper extremity13,33 despite the lack of heterotopic ossification prophylaxis, thus we do not routinely recommend the use of such a prophylaxis.
In summary, this case report demonstrates total elbow arthroplasty to be a credible treatment option for patients suffering from elbow arthritis related to a monostotic humeral Paget’s Disease. Although a 2-year follow-up after total joint replacement is short, the rare entity of the presented case makes its description of value. Furthermore, a recent systematic review investigating 10,018 patients undergoing total hip and total knee arthroplasty for Paget`s disease of bone demonstrated similar implant longevity compared to joint replacement in patients without Paget`s disease, with a pooled revision rate of 4.4% at a mean follow-up of 7.2 years (range: 0-20) following total hip replacement and 2.2% at a mean follow-up of 7.4 years (range: 2-20 years) following total knee replacement, respectively.1 However, although these data demonstrate good outcomes of joint replacements in patients with Paget’s disease at a at long-term follow-up, the applicability on total elbow arthroplasty remains unknown.
Conclusion
This case report describes a patient with elbow arthritis related to a monostotic humeral Paget’s Disease, who successfully underwent cemented total elbow arthroplasty performed through a diamond popup approach. At a follow-up of 2 years, excellent clinical and radiographic outcomes could be demonstrated. To reduce risk of complications, a through preoperative medical evaluation and optimization of the patient is recommended, and special care should be taken during surgery to avoid intraoperative fractures and to achieve stable implant fixation. Based on this case, we believe that total elbow arthroplasty is a valuable treatment option in patients with Paget’s Disease of the elbow and concomitant degenerative joint disease.
Disclaimers:
Funding: The authors received no financial support for the authorship and/or publication of this article.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Patient consent: Obtained.
Footnotes
Institutional review board approval was not required for this case report.
References
- 1.Arif M., Makaram N.S., Macpherson G.J., Ralston S.H. Outcomes following total hip and knee arthroplasty in patients who have Paget's disease of bone: a systematic review. J Arthroplasty. 2023;38:1400–1408. doi: 10.1016/j.arth.2023.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Arnalich F., Plaza I., Sobrino J.A., Oliver J., Barbado J., Pena J.M., et al. Cardiac size and function in Paget's disease of bone. Int J Cardiol. 1984;5:491–505. doi: 10.1016/0167-5273(84)90085-8. [DOI] [PubMed] [Google Scholar]
- 3.Brandolini F., Bacchini P., Moscato M., Bertoni F. Chondrosarcoma as a complicating factor in Paget's disease of bone. Skeletal Radiol. 1997;26:497–500. doi: 10.1007/s002560050273. [DOI] [PubMed] [Google Scholar]
- 4.Broberg M.A., Cass J.R. Total knee arthroplasty in Paget's disease of the knee. J Arthroplasty. 1986;1:139–142. doi: 10.1016/s0883-5403(86)80052-3. [DOI] [PubMed] [Google Scholar]
- 5.Corral-Gudino L., Borao-Cengotita-Bengoa M., Del Pino-Montes J., Ralston S. Epidemiology of Paget's disease of bone: a systematic review and meta-analysis of secular changes. Bone. 2013;55:347–352. doi: 10.1016/j.bone.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson D.J., Itonaga I., Maki M., McNally E., Gundle R., Athanasou N.A. Heterotopic bone formation following hip arthroplasty in Paget's disease. Bone. 2004;34:1078–1083. doi: 10.1016/j.bone.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 7.Frankle M., Tiegs R.D., Sim F.H. A review of corrective osteotomies for deformity in Paget's disease. Semin Arthritis Rheum. 1994;23:253. doi: 10.1016/0049-0172(94)90050-7. [DOI] [PubMed] [Google Scholar]
- 8.Gordon M.T., Mee A.P., Anderson D.C., Sharpe P.T. Canine distemper virus transcripts sequenced from pagetic bone. Bone Miner. 1992;19:159–174. doi: 10.1016/0169-6009(92)90923-2. [DOI] [PubMed] [Google Scholar]
- 9.Helfrich M.H., Hobson R.P., Grabowski P.S., Zurbriggen A., Cosby S.L., Dickson G.R., et al. A negative search for a paramyxoviral etiology of Paget's disease of bone: molecular, immunological, and ultrastructural studies in UK patients. J Bone Miner Res. 2000;15:2315–2329. doi: 10.1359/jbmr.2000.15.12.2315. [DOI] [PubMed] [Google Scholar]
- 10.Hozack W.J., Rushton S.A., Carey C., Sakalkale D., Rothman R.H. Uncemented total hip arthroplasty in Paget's disease of the hip: a report of 5 cases with 5-year follow-up. J Arthroplasty. 1999;14:872–876. doi: 10.1016/s0883-5403(99)90041-4. [DOI] [PubMed] [Google Scholar]
- 11.Imbuldeniya A.M., Tai S.M., Aboelmagd T., Walter W.L., Walter W.K., Zicat B.A. Cementless hip arthroplasty in Paget's disease at long-term follow-up (average of 12.3 years) J Arthroplasty. 2014;29:1063–1066. doi: 10.1016/j.arth.2013.10.015. [DOI] [PubMed] [Google Scholar]
- 12.Iwamoto T., Suzuki T., Oki S., Matsumura N., Nakamura M., Matsumoto M., et al. Computed tomography-based 3-dimensional preoperative planning for unlinked total elbow arthroplasty. J Shoulder Elbow Surg. 2018;27:1792–1799. doi: 10.1016/j.jse.2018.04.013. [DOI] [PubMed] [Google Scholar]
- 13.Jensen A.R., Sperling J.W. Reverse shoulder arthroplasty in a patient with Paget’s disease using the modified Ling technique. JSES Rev Rep Tech. 2021;1:55–59. doi: 10.1016/j.xrrt.2020.100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jorge-Mora A., Amhaz-Escanlar S., Lois-Iglesias A., Leborans-Eiris S., Pino-Minguez J. Surgical treatment in spine Paget's disease: a systematic review. Eur J Orthop Surg Traumatol. 2016;26:27–30. doi: 10.1007/s00590-015-1659-5. [DOI] [PubMed] [Google Scholar]
- 15.Kaplan F.S. Severe orthopaedic complications of Paget's disease. Bone. 1999;24:43S–436S. doi: 10.1016/s8756-3282(99)00048-4. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan F.S. Paget's disease of bone: orthopedic complications. Semin Arthritis Rheum. 1994;23:250–252. doi: 10.1016/0049-0172(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 17.Klein G.R., Parvizi J. Surgical manifestations of Paget's disease. J Am Acad Orthop Surg. 2006;14:577–586. doi: 10.5435/00124635-200611000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Kurihara N., Zhou H., Reddy S.V., Garcia Palacios V., Subler M.A., Dempster D.W., et al. Experimental models of Paget's disease. J Bone Miner Res. 2006;21 Suppl 2:P55–P57. doi: 10.1359/jbmr.06s210. [DOI] [PubMed] [Google Scholar]
- 19.Langston A.L., Campbell M.K., Fraser W.D., MacLennan G.S., Selby P.L., Ralston S.H., et al. Randomized trial of intensive bisphosphonate treatment versus symptomatic management in Paget's disease of bone. J Bone Miner Res. 2010;25:20–31. doi: 10.1359/jbmr.090709. [DOI] [PubMed] [Google Scholar]
- 20.Lee G.C., Sanchez-Sotelo J., Berry D.J. Total knee arthroplasty in patients with Paget's disease of bone at the knee. J Arthroplasty. 2005;20:689–693. doi: 10.1016/j.arth.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Lever J.H. Paget's disease of bone in lancashire and arsenic pesticide in cotton mill wastewater: a speculative hypothesis. Bone. 2002;31:434–436. doi: 10.1016/s8756-3282(02)00833-5. [DOI] [PubMed] [Google Scholar]
- 22.Lewallen D.G. Hip arthroplasty in patients with Paget's disease. Clin Orthop Relat Res. 1999:243–250. doi: 10.1097/00003086-199912000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Ling R.S. Femoral component revision using impacted morsellised cancellous graft. J Bone Joint Surg Br. 1997;79:874–875. doi: 10.1302/0301-620x.79b5.8078. [DOI] [PubMed] [Google Scholar]
- 24.Lopez-Abente G., Morales-Piga A., Elena-Ibanez A., Rey-Rey J.S., Corres-Gonzalez J. Cattle, pets, and Paget's disease of bone. Epidemiology. 1997;8:247–251. doi: 10.1097/00001648-199705000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Lusty P.J., Walter W.L., Walter W.K., Zicat B. Cementless hip arthroplasty in Paget's disease at medium-term follow-up (average of 6.7 years) J Arthroplasty. 2007;22:692–696. doi: 10.1016/j.arth.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 26.Makaram N., Woods L., Beattie N., Roberts S.B., Macpherson G.J. Long-term outcomes following total hip and total knee arthroplasty in patients with Paget's disease of bone (PDB) - a national study. Surgeon. 2020;18:335–343. doi: 10.1016/j.surge.2019.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Mankin H.J., Hornicek F.J. Paget's sarcoma: a historical and outcome review. Clin Orthop Relat Res. 2005;438:97–102. doi: 10.1097/01.blo.0000180053.99840.27. [DOI] [PubMed] [Google Scholar]
- 28.McDonald D.J., Sim F.H. Total hip arthroplasty in Paget's disease. A follow-up note. J Bone Joint Surg Am. 1987;69:766–772. [PubMed] [Google Scholar]
- 29.Mee A.P. Paramyxoviruses and Paget's disease: the affirmative view. Bone. 1999;24(5 Suppl):19S–21S. doi: 10.1016/s8756-3282(99)00033-2. [DOI] [PubMed] [Google Scholar]
- 30.Merkow R.L., Lane J.M. Current concepts of Paget's disease of bone. Orthop Clin North Am. 1984;15:747–763. [PubMed] [Google Scholar]
- 31.Merkow R.L., Lane J.M. Paget's disease of bone. Endocrinol Metab Clin North Am. 1990;19:177–204. [PubMed] [Google Scholar]
- 32.Merkow R.L., Pellicci P.M., Hely D.P., Salvati E.A. Total hip replacement for Paget's disease of the hip. J Bone Joint Surg Am. 1984;66:752–758. [PubMed] [Google Scholar]
- 33.Moen T.C., Yin B., Ahmad C.S. Total shoulder arthroplasty in a patient with Paget's disease: case report and review of the literature. J Shoulder Elbow Surg. 2011;20:e11–e17. doi: 10.1016/j.jse.2011.01.028. [DOI] [PubMed] [Google Scholar]
- 34.Paget J. On a form of chronic inflammation of bones (Osteitis deformans) Clin Orthop Relat Res. 1966;49:3–16. [PubMed] [Google Scholar]
- 35.Parvizi J., Frankle M.A., Tiegs R.D., Sim F.H. Corrective osteotomy for deformity in Paget disease. J Bone Joint Surg Am. 2003;85:697–702. doi: 10.2106/00004623-200304000-00017. [DOI] [PubMed] [Google Scholar]
- 36.Parvizi J., Klein G.R., Sim F.H. Surgical management of Paget's disease of bone. J Bone Miner Res. 2006;21:P75–P82. doi: 10.1359/jbmr.06s214. [DOI] [PubMed] [Google Scholar]
- 37.Parvizi J., Schall D.M., Lewallen D.G., Sim F.H. Outcome of uncemented hip arthroplasty components in patients with Paget's disease. Clin Orthop Relat Res. 2002:127–134. doi: 10.1097/00003086-200210000-00020. [DOI] [PubMed] [Google Scholar]
- 38.Popat R., Tsitskaris K., Millington S., Dawson-Bowling S., Hanna S.A. Total knee arthroplasty in patients with Paget's disease of bone: a systematic review. World J Orthop. 2018;9:229–234. doi: 10.5312/wjo.v9.i10.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ralston S.H., Corral-Gudino L., Cooper C., Francis R.M., Fraser W.D., Gennari L., et al. Diagnosis and management of Paget's disease of bone in adults: a clinical guideline. J Bone Miner Res. 2019;34:579–604. doi: 10.1002/jbmr.3657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reid I.R., Nicholson G.C., Weinstein R.S., Hosking D.J., Cundy T., Kotowicz M.A., et al. Biochemical and radiologic improvement in Paget's disease of bone treated with alendronate: a randomized, placebo-controlled trial. Am J Med. 1996;101:341–348. doi: 10.1016/s0002-9343(96)00227-6. [DOI] [PubMed] [Google Scholar]
- 41.Siris E.S. Perspectives: a practical guide to the use of pamidronate in the treatment of Paget's disease. J Bone Miner Res. 1994;9:303–304. doi: 10.1002/jbmr.5650090302. [DOI] [PubMed] [Google Scholar]
- 42.Tiegs R.D., Lohse C.M., Wollan P.C., Melton L.J. Long-term trends in the incidence of Paget's disease of bone. Bone. 2000;27:423–427. doi: 10.1016/s8756-3282(00)00333-1. [DOI] [PubMed] [Google Scholar]
- 43.Van Gorder G. Surgical approach in supracondylar ‘‘T’’ fractures of the humerus requiring open reduction. J Bone Joint Surg Am. 1940;22:278–292. [Google Scholar]
- 44.Wegrzyn J., Pibarot V., Chapurlat R., Carret J.P., Bejui-Hugues J., Guyen O. Cementless total hip arthroplasty in Paget's disease of bone: a retrospective review. Int Orthop. 2010;34:1103–1109. doi: 10.1007/s00264-009-0853-7. [DOI] [PMC free article] [PubMed] [Google Scholar]