Abstract
Standfirst:
Hopelessness and despair threaten health and longevity. We urgently need strategies to counteract these effects and improve population health. Prosociality contributes to better mental and physical health for individuals, and for the communities in which they live. We propose that prosociality should be a public health priority.
Comment:
The COVID-19 pandemic produced high levels of stress, loneliness, and mental health problems, magnifying global trends in health disparities.1 Hopelessness and despair are growing problems particularly in the U.S. The sharp increase in rates of poor mental health is problematic in its own right, but poor mental health also contributes to greater morbidity and mortality. Without action, we will see steep declines in global population health and related costs to society. An approach that is “more of the same” is insufficient to stem the cascading effects of emotional ill-being. Something new is desperately needed.
To this point, recent work called on the discipline of psychiatry to contribute more meaningfully to the deaths of despair framework (i.e., conceptualizing rises in suicide, drug poisoning and alcoholic liver disease as due to misery of difficult social and economic circumstances).2 Recognizing that simply expanding mental health services cannot address the problem, the authors noted the importance of population-level prevention and targeting macro-level causes for intervention. This requires identifying upstream factors causally related to these deaths. However, factors explaining population health trends are poorly delineated and focus on risks and deficits (e.g., adverse childhood experiences, unemployment). A ‘deficit-based’ approach has limits as the absence of a risk factor does not inevitably indicate presence of a protective asset; we also need an ‘asset-based’ approach to understanding more comprehensively the forces that shape good health and buffer harmful effects of stress and adversity.
Prosociality for Population Health
The COVID-19 pandemic sharply reminds us of the importance of prosociality for population and community health. Prosociality, defined as positive other-regarding behaviors and beliefs, encompasses numerous facets such as altruism, trust, reciprocity, compassion, and empathy. Recent research documents links of higher prosociality with intentions to receive a COVID-19 vaccination and engaging in preventive behaviors like masking.3 Prior work also shows linkages between prosocial behaviors (e.g., compassionate acts, volunteering) and greater well-being,4 although such research has not yet reached a broad audience. Though limited, work examining prosociality in relation to physical health suggests it is a health asset.4 Sociological and other work on resilience further indicate prosociality contributes to maintaining health not only for individuals practicing the behaviors, but also for the communities and societies in which they live.5 In fact, a key finding from a Lancet Commission on lessons from the COVID-19 pandemic was the low population levels of prosociality and how this contributed to global failure to successfully implement epidemic control.3 The Commission defined prosociality as ‘the orientation of individuals and government regulations to the needs of society as a whole, rather than to narrow individual interests’ and urgently called for public health systems to invest in promoting prosocial behaviour to prepare for future pandemics. We echo this call but suggest the Commission’s view of prosociality is too narrow. The potential reach of prosociality for improving population health goes well beyond managing emerging infectious diseases. Because prosociality substantially contributes to individual and community health, it provides a novel target for improving population health across many public health spheres, and may be especially important in the context of climate change. Of note, the UN’s sustainable development goals (SDG’s) are also rooted in the universal values of prosociality, compassion and equity.6 As a result, understanding the antecdents and consequences of prosociality should be a public health priority worthy of resources.
Initial evidence suggests changes in prosocial behavior reliably lead to downstream physical health improvements. Some studies show meditation-based interventions that cultivate compassion and kindness and other methods of modifying prosocial behaviors have positive effects on major health outcomes including cardiovascular disease.7,8 Such interventions can be labor-intensive and generally focus on modifying prosociality at the individual level, but may be modifiable to have greater reach. For example, recent randomized trials show highly scalable digital mobile interventions decrease distress and loneliness and improve social connectedness.9 Also promising are interventions that can be implemented at scale in schools, communities, and organizations to provide greater reach. For example, a randomized trial of adolescents examined effects of volunteering weekly (versus not) on risk markers for cardiovascular disease and found lower systemic inflammation, and healthier cholesterol levels and body weight in the intervention group four months later.8 Taken together, the experimental and epidemiologic evidence points to a moderate but consistently protective association of prosociality with physical health. Randomized trials of prosocial behavior that can follow participants for long enough to observe meaningful health changes and rigorous longitudinal studies will enhance the evidence base.
A deeper understanding of biospsychosocial mechanisms underlying the prosociality-health relationship will help guide more effective strategies for scaling up interventions to the population level. Mechanistic studies suggest prosociality leads to better health not only via behavioral and social pathways but also through direct biological effects. Volunteering is linked to healthier cognition in later life, and also with slowing or reversing declines in brain volume of areas implicated in dementia pathology.10 Interventions that teach simple meditation practices designed to nurture kindness and compassion lead to increases in prosociality and to changes in brain circuits implicated in effectively regulating emotions. Prosociality may also impact health by decreasing stress and stress reactivity, and promoting social connectedness.4
Of note, other positive qualities have been identified as potential health assets, including hope, optimism, self-regulation, and resilience. In contrast to prosociality, these factors are non-social. While positive non-social and social factors are correlated, they also have distinct effects. For example, non-social factors may be less likely to benefit the health of community members. Importantly, the inter-relationships between these factors and health requires future research.
A New Epidemiology of Prosociality
We propose prosociality as a novel strategy for improving population health. To develop and implement this strategy, first, we recommend developing an epidemiology of prosociality, with research designed to identify the antecedents and consequences of prosociality in the context of health. This will include gaining more granularity on when and how prosocial behaviors influence health, the range of outcomes affected, and if relationships are similar across diverse groups. It will be important to consider outcomes at both the individual and societal levels. An example is a global study of 31 nations and regions that documented associations between national prosociality levels and each country’s performance on environmental protection, which also benefits human health.11
Leveraging prior work on social and moral determinants of health,12 Figure 1 provides a conceptual model. Refining the model will require identifying characteristics of communities and organizations that promote prosocial values and behaviors, structural factors that work against or promote prosocial behaviors (e.g., school or workplace policies that promote competition versus collaboration), and specific pathways linking prosociality to individual and community health.
Figure 1.
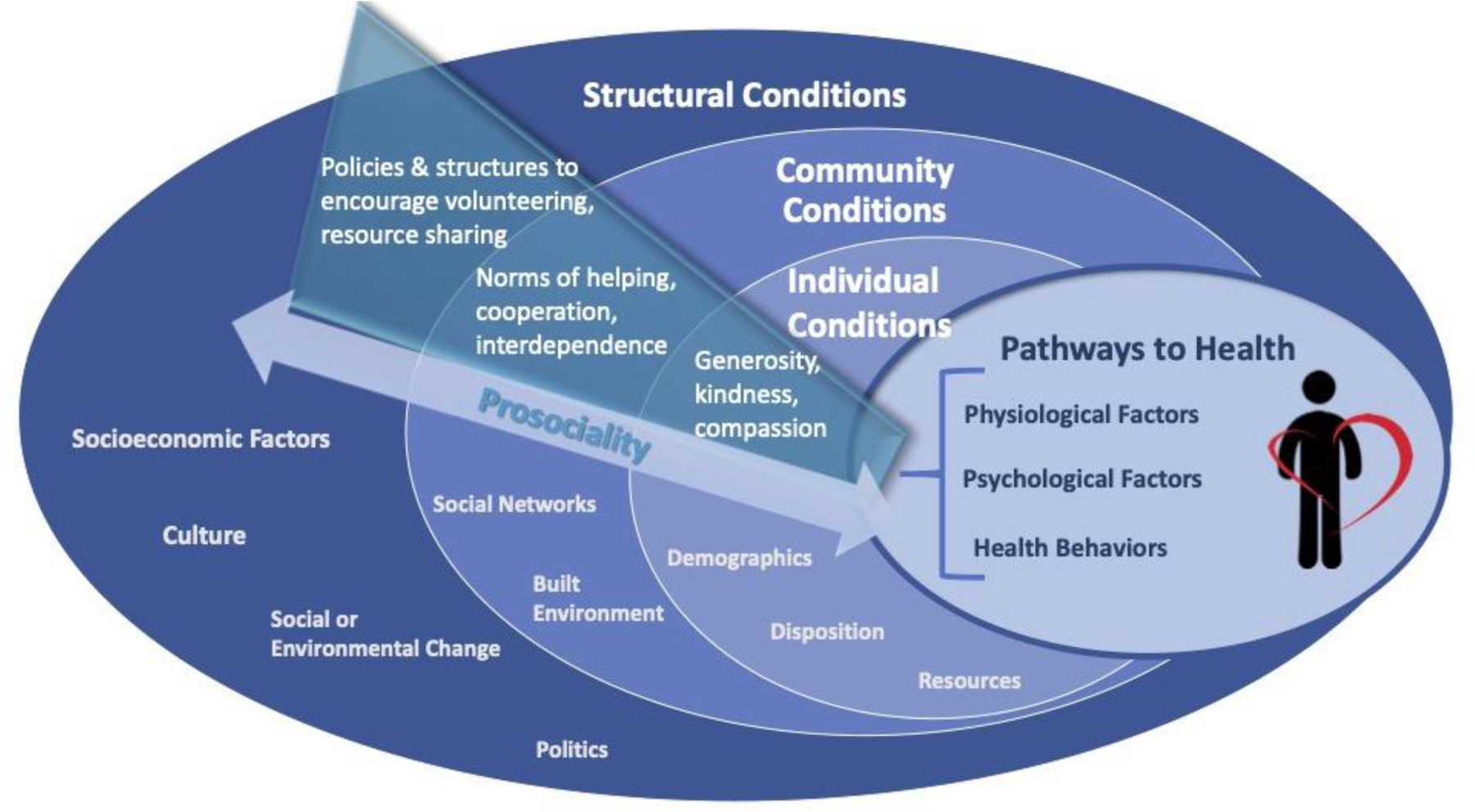
A Conceptual Model of Prosociality and Population Health
The model describes upstream macro- and individual-level factors that shape the distribution of prosociality (either by promoting or impeding levels) among individuals in the population and the downstream effects of prosociality on health-relevant processes that influence morbidity and mortality over the life course. Note that structural, community, and individual conditions all interact with each other and have direct and indirect effects on pathways to health. The inset provides more specific examples of ways structural, community, and individual conditions could promote higher prevalence of prosociality in the population. This model is not designed to include all relevant factors in each category but rather to provide examples for each. Also, in this model dispositional factors include individual level factors that promote prosocial behaviors, whereas psychological factors refer solely to downstream individual-level factors that are influenced by prosociality and also affect health-related processes. Examples of each element in the model are as follows. Structural conditions: socioeconomic factors – inequality, social welfare, systemic racism; culture – norms, values, competition/cooperation, independence/interdependence; social/environmental change – war/civil unrest, climate change; politics – laws/public policy, level of trust in leaders, human rights. Community conditions: social networks – size, density, diversity; built environment – safe communal spaces, barriers to integration. Individual conditions: disposition – motivation, compassion; demographics – sex, majority group status; resources – time, money. Pathways to health: physiological factors – immune function, brain neuroplasticity; psychological factors – stress buffering, sense of purpose; health behaviors – exercise, smoking.
While prosociality interventions at the individual level have received more attention, given prosociality is embedded in cultural values and social norms that shape behavior, efforts to modify prosociality must occur at multiple levels. Research on upstream structural factors that affect population levels of prosociality and how they may be modified is urgently needed. Such work can build on findings linking economic (e.g., income inequality, economic hardship) and other social conditions (e.g., market forces, racial segregation) to prosociality levels (e.g., volunteerism rates), and on promising community level interventions.13 For example, the Experience Corps, which pairs high-risk retirees with underprivileged youth through a tutoring program, has demonstrated effects on prosociality.10 Such interventions could be considered for expansion. We can also learn from prior successful public health campaigns targeting smoking, and physical exercise, and use similar strategies such as leveraging the social influence of celebrities, medical influencers, public health messaging and advertising. Efforts to develop a coordinated campaign for promoting prosocial behavior should be informed by key design principles that contribute to (or impair) campaign effectiveness. Moreover, research on individual-level interventions can be leveraged to assess scalability and durability of effects. For example, micro-interventions (e.g., simple kindness and compassion meditation practices, short in duration) have demonstrated impact on prosocial behavior in the moment and over time with repeated practice. Critical next steps include evaluating if such interventions can promote prosociality at scale, impact community norms and culture (e.g., by creating a culture of caring), and ultimately affect population health, and considering potential synergistic effects of interventions targeting structural factors and individual-level components. Beyond issues of scalability, timing and dose of interventions at any level should consider sensitive periods of development and change. Prior work suggests critical developmental influences on and stability in prosocial behavior over time, whereby interventions administered as early as pre-school effectively promoted higher prosociality.14 Other work suggests older adulthood is a critical etiologic window; enhancing prosociality in this period could provide health benefits when individuals are particularly vulnerable.10
The way forward
We call for researchers to apply a public health lens to prosociality. We must consider its potential as a promising health asset beyond preparing for the next pandemic. A major obstacle to developing strategies that promote health assets is the belief that such efforts are a luxury, not a necessity -- that we must focus on mitigating deficits and disease. Given increasing evidence that promoting health assets can effectively and independently improve emotional well-being, quality of life, and health, we should ensure such efforts become a front line treatment in clinical populations and a critical focus for population-based interventions. Rather than being a secondary treatment if resources allow, efforts to enhance assets must be a priority. In perhaps the clearest demonstration to date, the pandemic has shown that prosociality is an absolutely necessary health asset.3 As such, public health researchers and practitioners should invest resources in understanding both its antecedents and downstream effects.
Research on upstream determinants faces significant challenges. Individual-level interventions are easier to evaluate and recommend. Complex multifactorial causal pathways can be difficult to test with randomized experiments, and isolating effects of macro-level determinants can be problematic. However, natural experiments derived from policy changes and related examination of practice-based evidence could provide critical insights.15 Research funding is often siloed by disease endpoints rather than supporting work on causal psychosocial factors. Further, changes at the macro-level require political will. However, such problems are insurmountable only if scholars and funders do not engage with them.
We invite multidisciplinary collaborations to build the science around prosociality and request commitment from all relevant funding agencies and organizations to support this work. We ask researchers from public health, medicine and the social sciences to commit to examining social and structural factors that promote prosociality across diverse populations and how prosociality is linked to population mental and physical health. We also need to identify interventions that promote prosociality and assess if they improve health. It is time to go beyond an individual-level orientation to well-being; we must identify factors that promote both individual and societal health. In this time of high economic uncertainty with countless societal stressors imposing significant burden on mental and physical health, such efforts are particularly urgent. There is much work to be done.
Acknowledgements:
The authors would like to thank Justin Feldman for his invaluable assistance with reviewing and synthesizing relevant literature.
Footnotes
Competing Interests
Richard Davidson is the founder and President of the non-profit corporation Healthy Minds Innovations.
Authors have no other competing interests to declare.
References
- 1.Maffly-Kipp J, Eisenbeck N, Carreno DF & Hicks J Mental health inequalities increase as a function of COVID-19 pandemic severity levels. Soc Sci Med 285, 114275 (2021). 10.1016/j.socscimed.2021.114275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shanahan L & Copeland WE Psychiatry and Deaths of Despair. JAMA psychiatry (2021). 10.1001/jamapsychiatry.2021.0256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sachs JD et al. The Lancet Commission on lessons for the future from the COVID-19 pandemic. Lancet 400, 1224–1280 (2022). 10.1016/S0140-6736(22)01585-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hui BPH, Ng JCK, Berzaghi E, Cunningham-Amos LA & Kogan A Rewards of kindness? A meta-analysis of the link between prosociality and well-being. Psychological Bulletin, 1084–1116 (2020). 10.1037/bul0000298 [DOI] [PubMed] [Google Scholar]
- 5.Lamont M From ‘having’ to ‘being’: self-worth and the current crisis of American society. The British journal of sociology 70, 660–707 (2019). 10.1111/1468-4446.12667 [DOI] [PubMed] [Google Scholar]
- 6.UN DESA, N. Y., USA: UN DESA.. The Sustainable Development Goals Report 2022 - July 2022 (UN DESA, New York, USA, 2022). [Google Scholar]
- 7.Levine GN et al. Meditation and Cardiovascular Risk Reduction: A Scientific Statement From the American Heart Association. J Am Heart Assoc 6 (2017). 10.1161/JAHA.117.002218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schreier HMC, Schonert-Reichl KA & Chen E Effect of Volunteering on Risk Factors for Cardiovascular Disease in Adolescents: A Randomized Controlled Trial. JAMA Pediatr 167, 327–332 (2013). 10.1001/jamapediatrics.2013.1100 [DOI] [PubMed] [Google Scholar]
- 9.Hirshberg MJ et al. A randomized controlled trial of a smartphone-based well-being training in public school system employees during the COVID-19 pandemic. Journal of Educational Psychology 114, 1895–1911 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson MC et al. Impact of the Baltimore Experience Corps Trial on cortical and hippocampal volumes. Alzheimer’s & dementia : the journal of the Alzheimer’s Association 11, 1340–1348 (2015). 10.1016/j.jalz.2014.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Doesum NJ et al. Social mindfulness and prosociality vary across the globe. Proc Natl Acad Sci U S A 118 (2021). 10.1073/pnas.2023846118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berwick DM The Moral Determinants of Health. JAMA 324, 225–226 (2020). 10.1001/jama.2020.11129 [DOI] [PubMed] [Google Scholar]
- 13.Paarlberg LE, Nesbit R, Choi SY & Moss R The Rural/Urban Volunteering Divide. VOLUNTAS: International Journal of Voluntary and Nonprofit Organizations 33, 1–7-20 (2022). [Google Scholar]
- 14.Flook L, Goldberg SB, Pinger L & Davidson RJ Promoting prosocial behavior and self-regulatory skills in preschool children through a mindfulness-based Kindness Curriculum. Dev Psychol 51, 44–51 (2015). 10.1037/a0038256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ogilvie D et al. Using natural experimental studies to guide public health action: turning the evidence-based medicine paradigm on its head. J Epidemiol Community Health 74, 203–208 (2020). 10.1136/jech-2019-213085 [DOI] [PMC free article] [PubMed] [Google Scholar]


