Abstract
Background:
Opioid overdose continues to be a major cause of death in the United States. One effort to control opioid use has been to implement policies that enhance criminalization of opioid possession. Laws to further criminalize possession of fentanyl have been enacted or are under consideration across the country, including at the national level.
Objective:
Estimate the long-term effects on opioid death and incarceration resulting from increasingly strict fentanyl possession laws.
Design:
We built a Markov simulation model to explore the potential outcomes of a 2022 Colorado law which made possession of >1 gram of drug with any amount of fentanyl a Level 4 drug felony (and escalation of the previous law, where >4 grams of any drug with any amount of fentanyl in possession was considered a felony). The model simulates a cohort of people with fentanyl possession moving through the criminal justice system, exploring the probability of overdose and incarceration under different scenarios, including various fentanyl possession policies and potential interventions.
Setting:
Colorado
Participants:
A simulated cohort of people in possession of fentanyl.
Measurements:
Number of opioid overdose deaths, people incarcerated, and associated costs over 5 years.
Results:
When >4 grams of a drug containing any amount of fentanyl is considered a felony in Colorado, the model predicts 5,460 overdose deaths (95% CrI 410–9,260) and 2,740 incarcerations for fentanyl possession (95% CrI: 230–10,500) over 5 years. When the policy changes so that >1 gram possession of drug with fentanyl is considered a felony, opioid overdose deaths increase by 19% (95% CRI: 16%–38%) and incarcerations for possession increase by 98% (CrI: 85%–98%). Diversion programs and MOUD in prison help alleviate some of the increases in death and incarceration, but do not completely offset them.
Limitations:
The mathematical model is meant to offer broad assessment of the impact of these policies, not forecast specific and exact numerical outcomes.
Conclusions:
Our model shows that lowering thresholds for felony possession of fentanyl containing drugs can lead to more opioid overdose deaths and incarceration.
Keywords: simulation modeling, overdose, fentanyl, criminal justice
Introduction
Overdose deaths in the US have been steadily rising over the past several decades, with synthetic opioids including illicitly-manufactured fentanyl overtaking prescription opioids and heroin as the leading cause of opioid mortality (1). In 2021 in the US, fentanyl overdoses alone accounted for over 70,000 deaths (2). This a major concern for public health officials, other policy makers, and local and national leaders. There have been various efforts to curb this epidemic, including expanding access to treatment with medications for opioid use disorder (MOUD) (3–5), expanded distribution and availability of naloxone (6–8), and policies for more careful opioid prescribing (9, 10). While some of these interventions have proven effective, rates of overdoses continue to rise.
In addition to the interventions described above, some legislative bodies have passed laws aimed at enhancing penalties for opioid use and possession, though historically these criminalization efforts have not been shown to prevent or deter drug use (11–13). Multiple states have implemented severe penalties for fentanyl manufacturing and distribution (14), bringing fentanyl across state lines (15), or providing fentanyl to someone who then experiences a fatal overdose (16). In 2023, the US House of Representatives passed HR 467, add all fentanyl substances as a schedule 1 drug of the Controlled Substances Act, which can allow for harsher penalties in the criminal justice system (17). As of 2021, 18 states had classified possession of less than 4 grams of certain controlled substances, including fentanyl, as a felony (18). In 2022, Colorado became the 19th state to do this with the passage of House Bill 22–1326 (HB22–1326) (19). This bill made possession of greater than 1 gram of any drug containing any amount of fentanyl a Level 4 felony, which is punishable by a 6-month to 1-year prison sentence and/or fines of up to $100,000 (20). Punitive approaches to drugs have not decreased drug use (11–13), but they have led to racial profiling in drug arrests targeting the Black community, with concomitant large increases in the US prison population and spending on incarceration (21–23). Incarceration can lead to higher overdose risk upon release, with rates of overdose up to 40 times higher than in the general population within the first few weeks of release from prison (24).
In the setting where more people are being incarcerated for drug related offenses, MOUD can reduce the risk of death. MOUD during carceral stays has been shown to reduce the risk of overdose following release (25). Unfortunately, MOUD provision in the US is low with less than 10% of all correctional facilities offering MOUD. In Colorado, Denver County has had access to MOUD in correctional settings since 2018, but less than 10% of those with reported OUD in correctional settings have access to buprenorphine induction (26). While HB22–1326 provides $3 million in funding for Colorado jails to create policies on how they would provide MOUD to incarcerated people during their jail stays, the bill does not require MOUD in prison settings and for jails it is an unfunded mandate for providing medications (19). Additionally, several alternative to incarceration programs exist that have shown positive outcomes. These diversion programs attempt to keep people out of jail while holding them accountable for their crimes and, when appropriate, having them make restitution to their victims. Diversion programs more often work with misdemeanors and crimes with victims, but Colorado programs do accept those with drug felonies as well (27). In 2021, diversion programs kept 1,200 Coloradoans out of jail (27). HB22–1326 did not formally expand adult diversion programs. The sole focus on punishment may, therefore, have important short- and long-term implications for deaths, incarceration numbers, and the state budget.
Mathematical modeling is a useful tool that can simulate policies and estimate their effects, guiding decision-makers in real-time (28, 29). In particular, policy models, meant to address current policy issues with limited data availability while balancing precision and tractability, are useful in answering broad policy-related questions without attempting to perfectly represent a phenomenon (30). Herein, we developed a policy model to estimate the potential impact of the recent Colorado law enhancing penalties for fentanyl possession on population-level health and economic outcomes. In particular, we assess mortality and incarceration rates, compared to the previously existing threshold in the law, and include access to MOUD and diversion programs as additional interventions in our model.
Methods
Model Structure
We developed a closed cohort compartmental Markov model to examine the effect of changing criminal penalties for fentanyl possession. In this analysis, we used the model to estimate the impact of a new law reducing the threshold for felony status for fentanyl possession at the Colorado state level.
The model simulates a population of people with illicit opioid use who possess fentanyl. In the model, the population is divided into three groups: those who possess greater than 4 grams of drugs containing any amount of fentanyl, those who possess between 1 and 4 grams of drugs containing any amount of fentanyl, and those who possess less than one gram of drugs containing any amount fentanyl. We chose these cutoffs to specifically model the effects of Colorado law HB22–1326 (19).
Individuals in the population begin the simulation as alive and never incarcerated. The population progresses in monthly time steps and each month a proportion of the population dies of opioid overdoses, initiates treatment with medications for opioid use disorder (MOUD) modeled as buprenorphine, or is arrested for drug possession, which is followed by either incarceration or a diversion program (31, 32). In our analyses, we use data from the Colorado diversion programs on program completion and reduction in incarceration in the year following diversion (27). We assume that those in the diversion program and post-diversion to have the same risk of overdose as those not in the diversion program since MOUD is not uniformly part of diversion programs and data on reduction in overdoses in diversion programs is not available. Those who die from overdose are removed from the simulation and not replaced. We assume that the population who initiate MOUD are not at risk for fatal overdose or arrest for drug possession for the duration of the time they remain on MOUD. They do, however, have a probability of stopping MOUD and transitioning back into opioid use and possession.
The population of those arrested for fentanyl possession can take several potential paths in the model, reflecting variation in law enforcement practice among jurisdictions. First, depending on which version of laws described above is being simulated, some people do not possess a sufficient among of fentanyl-containing drug to constitute a felony. These individuals move back to the active drug use state. Second, those who do possess enough drug to constitute a felony are assigned a probability of avoiding incarceration and entering a diversion program as well as a probability of being incarcerated. Those who enter a diversion program have a lower risk of incarceration while in the program than they would existing in an active drug use state alone. Those who complete the requirements of diversion enter a post-diversion period during which arrest is also less likely than in the active drug use state.
Those who are incarcerated due to possession remain in the incarcerated state for a duration consistent with the data on sentencing in Colorado for these offenses. During incarceration, we conservatively assume that there is no risk of fatal overdose even though data suggest that overdoses in these settings do occur (33). Upon release from incarceration, this population experiences an elevated risk for overdose death in the first month and the first-year post-release and a permanently elevated risk of re-incarceration (24, 34).
We model MOUD such that it can be initiated in the community and/or during incarceration. We vary the proportion of the incarcerated population who begin MOUD during incarceration and the probability of linkage to outpatient MOUD following release. Linkage to MOUD post-release from incarceration lowers the risk of overdose mortality for those on treatment. Once released, those on MOUD can discontinue MOUD or be retained in substance use care.
Each state (incarceration, MOUD, diversion, and overdose) has costs associated with their occupancy.
Model parameterization
Table 1 includes a complete list of all parameter estimates. We parameterized a cohort of people with illicit opioid use in Colorado using a combination of estimates from the National Survey on Drug Use and Health (35) and Krawczyk et al (2022), which applied a multiplier based on reported drug poisoning and opioid deaths to account for underreporting. For the base case, we estimated that approximately 50% of the drug supply in Colorado contained fentanyl and, therefore, that approximately 50% of people with illicit opioid use possess fentanyl. This estimate was derived from data from the Denver Department of Public Health and Environment, which found that 50% of all fatal opioid overdoses in Colorado contained fentanyl (36). However, this estimate may change as the magnitude of fentanyl presence in the drug supply evolves. While our estimates here are an imperfect proxy for fentanyl possession, the online tool described later in the methods allows for users and decision-makers to explore different estimates of fentanyl presence in the context of possession to account for this uncertainty. Opioid mortality rates were calculated based on number of people with illicit opioid use and the number of fatal overdoses, as reported by the US Centers for Disease Control and Prevention (CDC) (2, 37). We assumed overdose mortality risk did not differ by amount of drug in possession. Other estimates on drug possession were obtained from published literature, which used criminal justice and arrest data to estimate amount of drug in possession, finding that over 60% of all those arrested for illicit drug possession (excluding marijuana) had less than 1 gram of drug on them, approximately half of the remaining population had less than 5 grams(38).
Table 1.
Model parameter values and ranges.
| Parameter | Estimate | Range Evaluated | Source |
|---|---|---|---|
| Population and drug possession | |||
| Adult population with opioid use disorder | 139,867 | 37,000–166,130 | NSDUH 2021 (35) Krawczyk et al. 2022(39) |
| Percent of drug supply with fentanyl | 50% | DDPHE, 2022 (36) based on drug fatality data from 2021 | |
| Amount of drug in possession | Kennedy et al. 2018(38) | ||
| >4 grams | 17% | ||
| 1–4 grams | 18% | ||
| <1 gram | 65% | ||
| MOUD treatment | |||
| Number on MOUD, annually | 9,105 | 4,553–13,700 | Krawczyk 2022(39) |
| Average duration of MOUD | 6 months | 3 months- 9 months | Morgan et al. 2018 (40) Morgan et al. 2021 (41) |
| Probability of MOUD while incarcerated | 1 | 0–1 | |
| Probability of linking to MOUD post-incarceration, if on MOUD in prison | 0.48 | 0.25–0.75 | Gordon et al. 2017 (49) Magura et al. 2009 (50) Gordon et al. 2014 (48) |
| Criminal justice | |||
| Annual arrest probability with drug possession | |||
| Standard | 0.13 | PEW Charitable Trusts (43) | |
| Calibrated to Colorado | 0.07 | Calibrated to Colorado drug arrest rate, 2021 (47) | |
| Low policing | 0.05 | Estimated | |
| High policing | 0.25 | Estimated | |
| Multiplier on likelihood of subsequent arrest given prior arrest | 2.43x | 1.22–3.65 | Langan et al. (2002) (42) Belenko et al. (2013)(34) |
| Diversion | |||
| Probability of diversion if felony possession | 0.1 | Colorado Judicial Department 2021 (27), Simulated estimate | |
| Duration of diversion | 12 months | Colorado Judicial Department 2021 (27) | |
| Probability of completing diversion program | 0.89 | Colorado Judicial Department 2021 (27) | |
| Probability of arrest within one year of diversion program completion | 0.07 | Colorado Judicial Department 2021 (27) | |
| Mortality | |||
| Annual overdose probability | 0.0142 | 0.0090–0.0405 | CDC NCHS 2021 (2, 37) Krawczyk 2022(39) National Center for Vital Statistics (54) |
| Overdose multiplier within first month of release from incarceration | 40x | 30x-51x | Ranapurwala et al. 2018(24) |
| Overdose multiplier within first year of release from incarceration | 10x | 9.5x-11.7x | Ranapurwala et al. 2018(24) |
| Costs | |||
| Cost of incarceration, 6 months | $19,700 | Vera, 2015 (44) | |
| Cost of diversion program, annual per-person | $500 | Colorado Judicial Department 2021 (27) | |
| Cost of overdose death | |||
| Healthcare costs only | $5,500 | Florence et al. 2021(45) | |
| Lost productivity costs only | $1.4 million | Florence et al. 2021(45) | |
| Value of a statistical life | $10 million | Florence et al. 2021(45) | |
| Cost of MOUD, annual per-person | $5,980 | NIDA, 2022 (1) |
MOUD treatment initiation was based on Colorado-specific MOUD rates from literature, assuming approximately 8% of those at risk were on MOUD (39). MOUD retention estimates were obtained from national sources in published literature assuming that these estimates would not differ by jurisdiction (40, 41). Estimates for criminal justice parameters including sentence duration and diversion program effectiveness and costs were obtained by a combination of Colorado-specific and national data (27, 34, 42, 43). We assumed that those in diversion programs had the same rate of MOUD initiation and fatal overdose as the general never-incarcerated population. Incarceration costs were calculated using estimates for average inmate costs by state (44). Opioid overdose mortality costs were estimated representing healthcare costs only and derived from the existing literature (45).
We calibrated the model to the number of fatal opioid overdoses in Colorado in 2021, as well as to the number of arrests for synthetic narcotics in Colorado in the same timeframe. The CDC reports 1,887 fatal opioid overdoses in 2021 (2, 37), and the National Center for Vital Statistics reports that nearly 1,000 of those were from synthetic opioids (46). Our model estimates approximately 970 fatal opioid overdoses over a 1-year period with the policy that was in place in Colorado in 2021. In addition, Colorado reports 784 arrests for possession of synthetic narcotics in 2021, though the number of arrests is trending up (47). Our model estimates 780 total arrests during a 1-year time period with the policy in place in 2021 in Colorado. It is important to note that our model cannot account for trends, as both arrests and overdoses from fentanyl in Colorado seem to be increasing, and estimates for fatal overdoses for 2022 are higher than for 2021. To account for uncertainty in arrests and overdoses from fentanyl in Colorado, we report credible intervals for all estimates.
Model Analyses
We modeled the following policy scenarios:
Policy Scenario A (Base Case): the fentanyl felony possession law in place prior to HB22–1326, where >4 grams of any drug with any amount fentanyl was considered a felony.
Policy Scenario B: modeling HB22–1326, where >1 grams of any drug with any amount fentanyl is considered a felony.
Policy Scenario C: a hypothetical scenario where any amount of drug with any amount fentanyl is considered a felony.
In addition, we also modeled 4 differrent intervention scenarios:
No additional interventions: no diversion program or MOUD in prison.
Diversion program: where 10% of all those arrested avoid incarceration and instead enter a diversion program. 10% is an estimate of the potential capacity for scale-up of diversion programs within this population.
MOUD in prisons: where 100% of those incarcerated are offered MOUD, nearly half (48%) link to continued care upon release (48–50).
MOUD in prisons and diversion program: combining the above scenarios, with 10% of all arrested entering a diversion program, and 100% of those incarcerated having access to MOUD in prison with 48% linking to continued care upon release (48–50).
The base case of the model considered Policy Scenario A with no additional interventions, and we compared outcomes between the base case and other policy and intervention scenarios.
We used the model to generate expected outcomes at 1-, 5-, and 10-year time horizons. Outcomes of interest included opioid overdose mortality, total incarcerations, and costs associated with deaths, incarcerations, and MOUD and diversion programs. Costs were estimated from a limited state perspective (with regard to incarceration costs) as well as a limited healthcare perspective (with regard to deaths and MOUD).
Sensitivity analysis
Due to the uncertainty of several parameter values, we performed a probabilistic sensitivity analysis (PSA) on key parameters of interest for the base case (with no diversion program or MOUD in prisons) including: population who use opioids in Colorado, population on MOUD in Colorado, proportion of fentanyl in the drug supply, average duration of MOUD treatment, likelihood of arrest for fentanyl possession, and increased likelihood of arrest and death given history of incarceration. The PSA consisted of 1,000 model runs. We generated a 95% credible interval (CrI) using PSAs. All parameter ranges included in the PSA can be found in Table 1. We also performed one-way sensitivity analyses on key parameters of interest for Policy Scenario A, to explore which parameters had the most effect on the outcomes of the model.
We also explored a series of multi-way deterministic sensitivity analyses evaluating key parameters through a range of values. In particular, we analyzed the thresholds of MOUD linkage post-incarceration, duration of MOUD post-incarceration, and risk of overdose mortality post-incarceration to find the values at which Policy Scenario B (HB 22–1326) might lead to fewer deaths than the base case. We ranged MOUD linkage post-incarceration from 0–100%, duration of MOUD post-incarceration from 1–26 months, and multiplier on risk of overdose mortality post-incarceration from 1 to 40 in the first month post-incarceration and 1 to 10 in the first year post-incarceration.
Our base case analyses assumed that at the start of simulation, all people started in the “never incarcerated” state and moved from there. In reality, some people in the population have a history of incarceration. To account for this, we conducted a sensitivity analysis where we assigned 10% of the population to incarcerated or previously incarcerated states (2% current incarcerated, 1% incarcerated in the past month, 2% incarcerated in the last year, and 5% incarcerated more than a year prior).
We performed an additional sensitivity analysis exploring what percentage of those in possession of fentanyl would have to discontinue opioid use in order to make Policy Scenario B preferrable to Policy Scenario A. We did this by varying the proportion of the “at-risk” population (all those with >1g of fentanyl in their possession) who might discontinue fentanyl use due to the new policy implementation.
Online tool
In addition to the analysis of the impact of Colorado state law, we developed an online companion tool which can be used by stakeholders and policymakers in other jurisdictions to analyze possible outcomes of fentanyl possession policies and with different parameter estimates in their own states. The tool allows users to select their state of interest (which determines the number of people with opioid use disorder as well as the cost of a month of incarceration and the prevalence of community MOUD treatment), penalty threshold (>4g, >1g, any amount), length of the simulation, proportion of drug supply that contains fentanyl, proportion of incarcerated individuals who initiate MOUD and link to care post-incarceration, the proportion of those who can enter a diversion program, and measures of policing and cost per death.
Funding Declaration
Funders had no role in design, conduct, or reporting of the work.
Results
In the 5-year base case (Policy Scenario A, >4 grams of any drug with any amount fentanyl was considered a felony) analysis, the model estimated 5,460 overdose deaths (95% CrI 410–9,260) and 2,740 incarcerations for felony possession (95% CrI: 230–10,500) (Figure 2, Table 2). Considering Policy Scenario B (>1 gram of any drug with any amount fentanyl was considered a felony) with no interventions, the model estimated 6,490 overdose deaths (95% CrI: 710–12,240), a 19% increase from the base case (95% CrI: 16%–38%), and 5,430 incarcerations for felony possession (95% CrI: 520–19,720), a 98% increase from the base case (95% CrI: 85%–98%). This means that almost one fifth of the deaths and half of incarcerations in Policy Scenario B could be attributed to changes represented by the new Colorado law. With Policy Scenario C (any amount of any drug with any amount fentanyl was considered a felony), the model estimated 9,990 overdose deaths (95% CrI: 950–21,360), an 83% increase from the base case (95% CrI: 67%–153%), and 13,560 incarcerations for felony possession (95% CrI: 1,000–43,620), a 395% increase from the base case (95% CrI: 276%–392%).
Figure 2. Model results for overdose deaths and incarceration for fentanyl possession in Colorado over 5 years, by Policy Scenario.
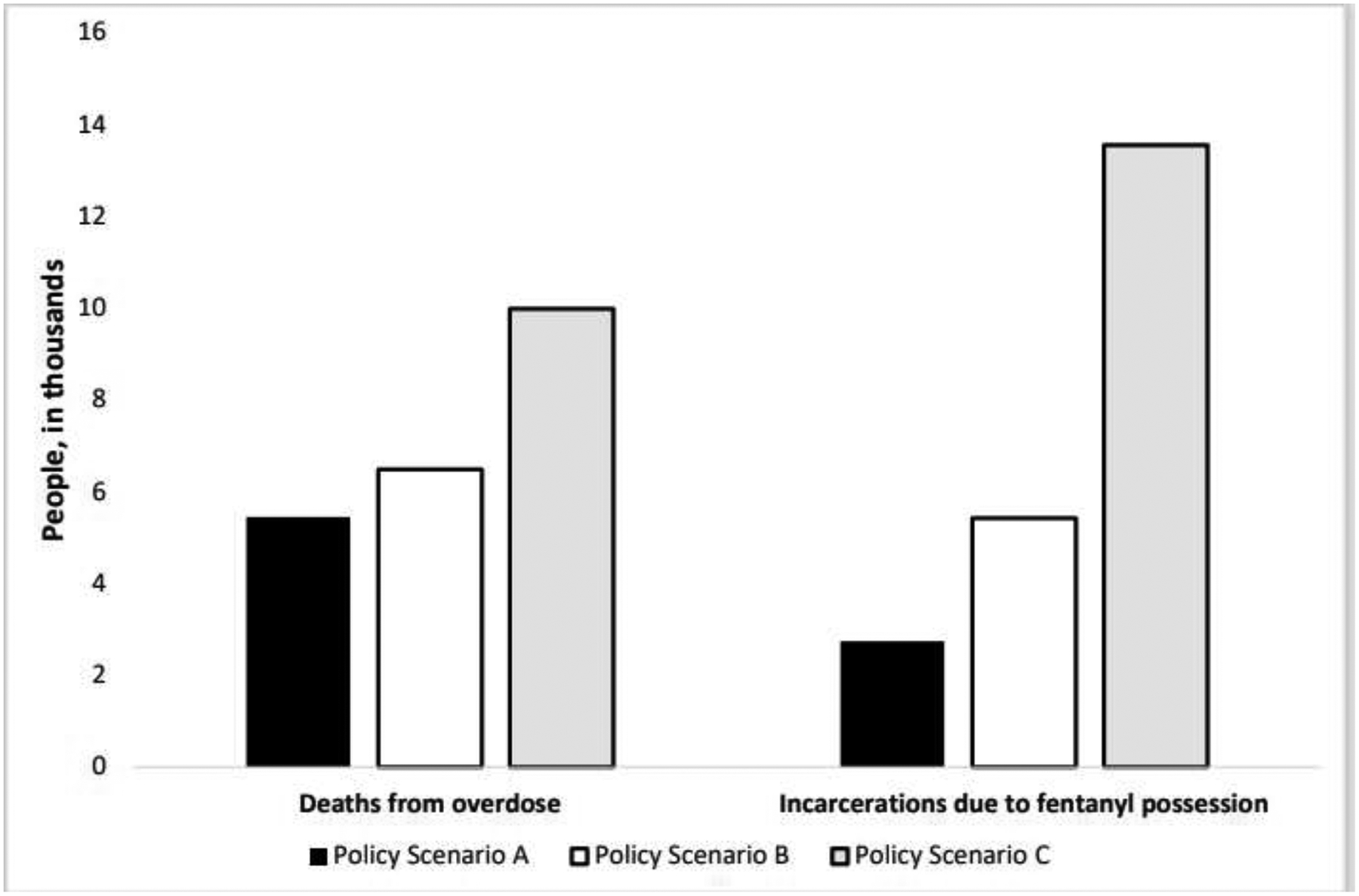
Assuming an estimated population with opioid use disorder of 139,000, annual community-level MOUD uptake of 8% with an average 6-month duration, and a 13% annual arrest rate for drug possession.
Table 2.
5-year model results with varying felony possession of fentanyl policies and interventions implemented.
| Total opioid overdose deaths | Total incarcerations | Total cost of incarcerations, millions | Total costs of death (healthcare costs only), millions | Total Cost | |||
|---|---|---|---|---|---|---|---|
| No intervention | Deaths | Percent Change | Incarcerations | Percent Change | |||
| Base Case (Policy Scenario A) | 5,460 (410–9,260) | 2,740 (230–10,500) | $74.11 ($7.39-$280.28) | $29.80 ($2.25-$50.60) | $163.90 ($14.06-$471.78) | ||
| Policy Scenario B | 6,490 (710–12,240) | 19% (16–38% | 5,430 (520–19,720) | 98% (85–98%) | $154.30 ($18.42-$576.62) | $35.43 ($3.89-$66.84) | $249.05 ($28.00-$790.04) |
| Policy Scenario C | 9,990 (930–21,360) | 83% (67–153%) | 13,560 (1,000–43,620) | 395% (276–392%) | $453.69 ($42.36-$1,792.83) | $54.57 ($5.09-$116.68) | $565.20 ($52.07-$2,038.11) |
| 100% MOUD in jails with 48% linkage post-incarceration | |||||||
| Policy Scenario A | 5,380 (390–9,120) | 2,630 (210–9,650) | $73.82 ($7.54-$275.87) | $29.38 ($2.14-$49.82) | $167.90 ($15.58-$477.84) | ||
| Policy Scenario B | 6,320 (540–11,580) | 18% | 5,200 (420–18,620) | 98% | $153.08 ($15.38-$576.47) | $34.54 ($2.93-$63.24) | $256.70 ($24.53-$806.66) |
| Policy Scenario C | 9,490 (790–19,650) | 76% | 12,880 (900–40,860) | 390% | $444.15 ($42.08-$1,695.20) | $51.83 ($4.34-$107.30) | $581.20 ($53.61-$2,028.79) |
| 10% move to diversion program | |||||||
| Policy Scenario A | 5,360 (460–9,010) | 2,490 (220–9,940) | $67.39 ($6.95-$260.82) | $29.30 ($2.52-$49.22) | $156.87 ($14.29-$448.37) | ||
| Policy Scenario B | 6,300 (520–11,810) | 17% | 4,950 (380–18,350) | 98% | $140.48 ($13.39-$541.85) | $34.43 ($2.85-$64.50) | $234.63 ($20.95-$750.45) |
| Policy Scenario C | 9,510 (1,010–19,680) | 77% | 12,450 (1,050–40,460) | 399% | $414.96 ($46.04-$1,555.31) | $51.94 ($5.51-$107.47) | $524.90 ($56.36-$1,793.60) |
| 10% move to diversion program, 100% MOUD in jails with 48% linkage post-incarceration | |||||||
| Policy Scenario A | 5,290 (530–8,710) | 2,390 (210–8,740) | $67.12 ($7.04-$245.01) | $28.92 ($2.90-$47.56) | $160.51 ($16.73-$446.35) | ||
| Policy Scenario B | 6,150 (570–10,980) | 16% | 4,740 (390–18,110) | 98% | $139.38 ($14.19-$539.41) | $33.61 ($3.12-$59.99) | $241.59 ($23.80-$768.32) |
| Policy Scenario C | 9,050 (850–19,850) | 71% | 11,820 (910–40,250) | 394% | $406.25 ($41.64-$1,596.35) | $49.43 ($4.64-$108.40) | $539.51 ($54.43-$1,924.38) |
In our scenario in which MOUD were offered to 100% of those incarcerated and 48% of those people linked to care, we found decreases in overdose deaths and incarcerations compared to the no intervention scenarios. The extent to which these outcomes changed were dependent on the policy scenario evaluated. In Policy Scenario B, overdose deaths decreased by nearly 200 (3% reduction) and in Policy Scenario C overdose deaths decreased by 500 (5% reduction) over 5 years (Figure 3, Table 2). Incarcerations decreased by 4–5% (Figure 3, Table 2).
Figure 3. Model results for overdose deaths and incarceration for fentanyl possession in Colorado over 5 years, assuming different levels of MOUD availability in prisons and diversion programs in the community.
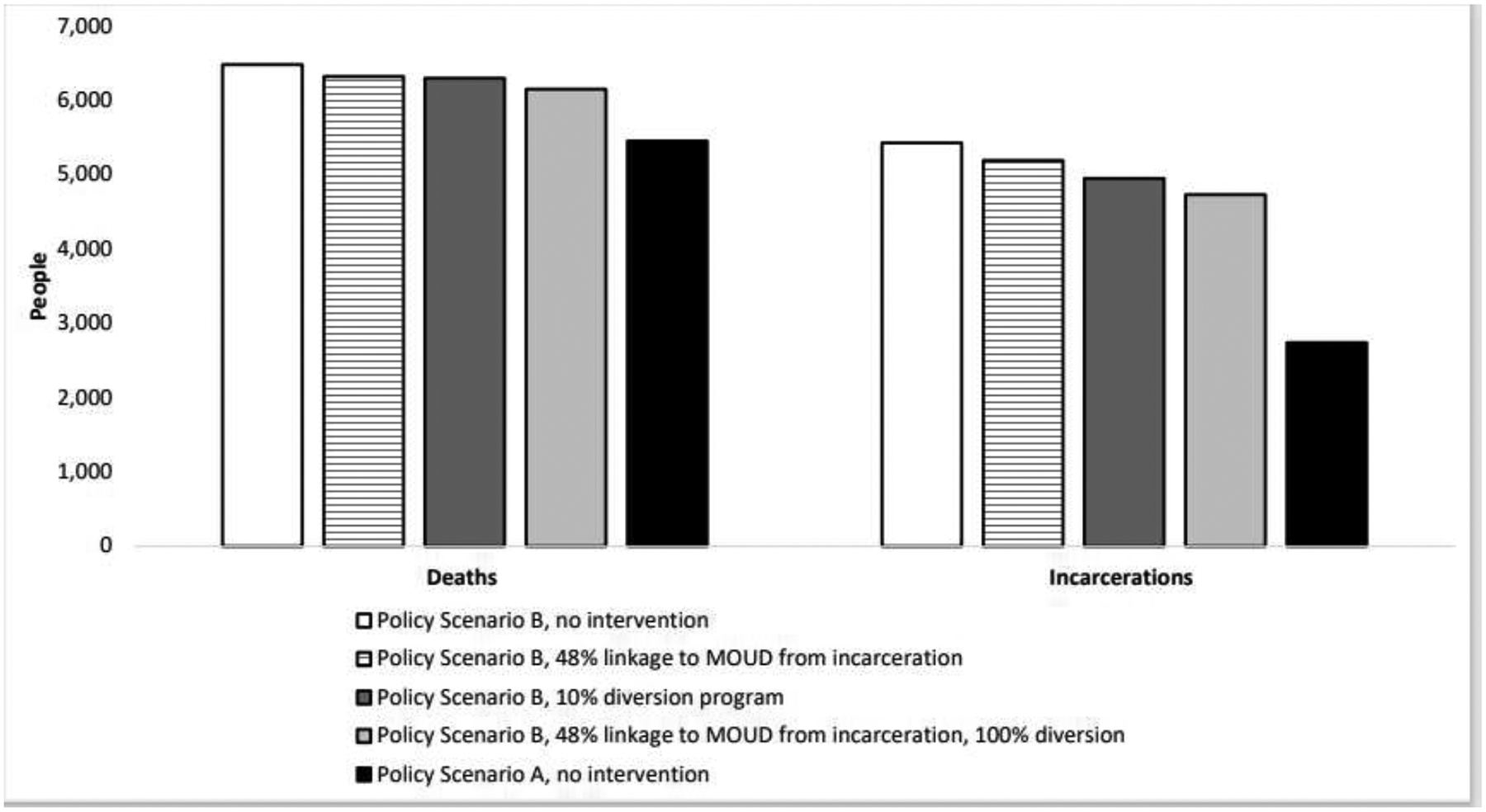
Assuming an estimated population with opioid use disorder of 139,000, annual community-level MOUD uptake of 8% with an average 6-month duration, and a 13% annual arrest rate for drug possession.
In our scenario in which a diversion program was offered to 10% of those arrested, overdose deaths decreased by approximately 150–500 (3–5% reduction) and incarcerations for fentanyl possession decreased by 400–1,300 (7–9% reduction) as compared to scenarios with no additional interventions (Figure 3, Table 2).
In our scenario where both MOUD and a diversion program were offered in prison, overdose deaths decreased by 170–940 (3–9%) and incarcerations for fentanyl possession decreased by 350–1,740 (13–14%), as compared to the scenario with no additional intervention (Figure 3, Table 2).
In each modeled scenario, there remained fewer overdose deaths and incarcerations with Policy Scenario A, regardless of additional interventions implemented (e.g., diversion, MOUD in jail). The base case was preferred over any other option where Policy Scenario B or Policy Scenario C were considered.
Finally, five-year costs for incarcerations and community MOUD were $164 million under the base case and increased to $249 million with Policy Scenario B and $565 million with Policy Scenario C (Figure 4, Table 2), assuming no additional intervention.
Figure 4. Model results for total costs from incarcerations for fentanyl possession, MOUD, and diversion program in Colorado over 5 years, assuming different levels of MOUD availability in prisons and diversion programs in the community.
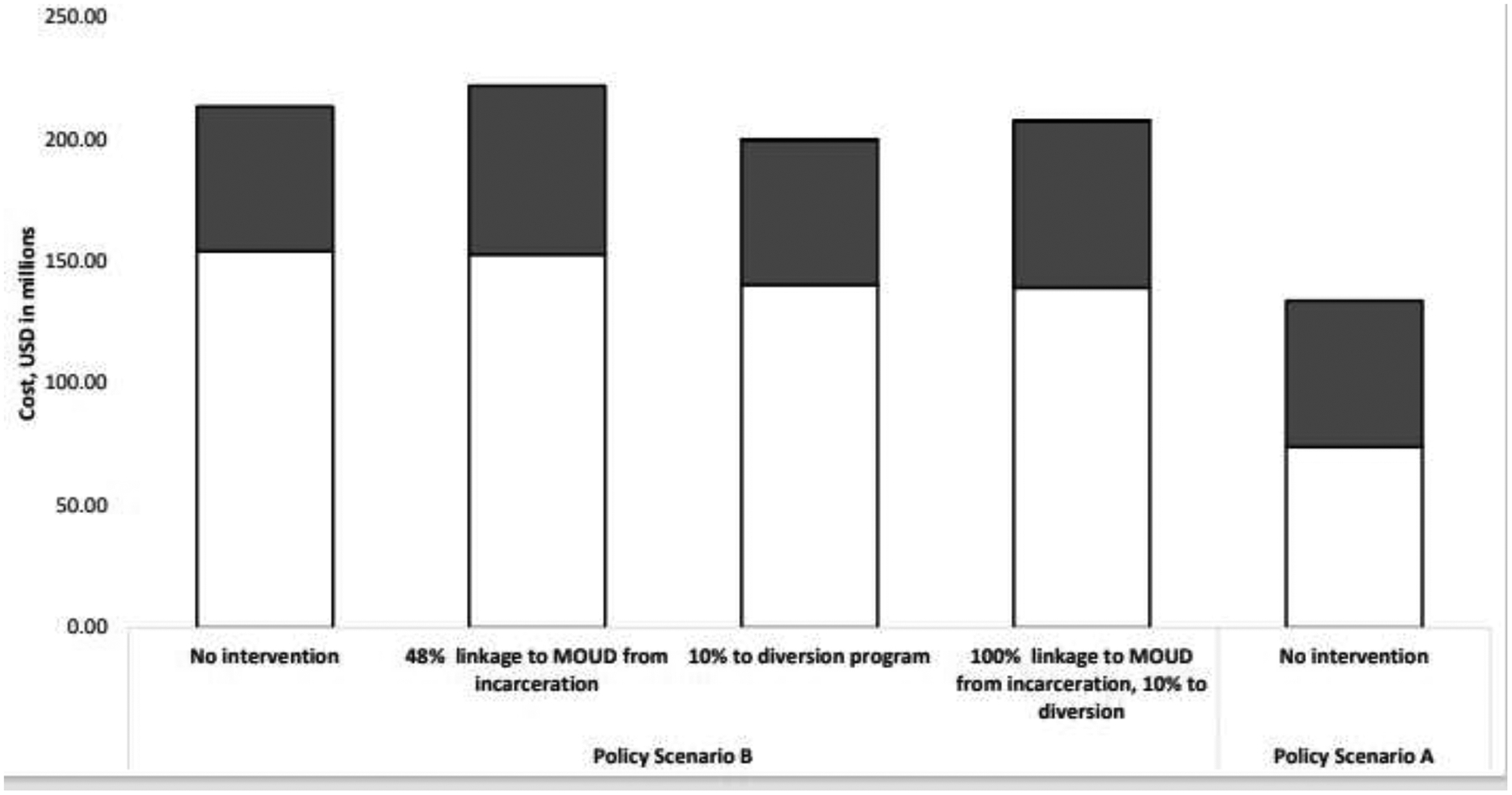
Assuming an estimated population with opioid use disorder of 139,000, annual community-level MOUD uptake of 8% with an average 6-month duration, and a 13% annual arrest rate for drug possession. Incarceration costs in white, MOUD costs in dark grey, diversion program costs in light grey.
When considering results from the PSA, wide credible intervals were obtained due to uncertainty of key parameters, including size of population with fentanyl possession. However, in every iteration of the PSA, Policy Scenario A predicted fewer deaths and fewer incarcerations than either Policy Scenario B or Policy Scenario C.
In one-way sensitivity analyses, the parameters with the most effect on both number of deaths and incarcerations were the size of the population in possession of fentanyl, fatal overdose rate, and proportion of the population with >4 grams of fentanyl in possession (for incarcerations only) (Supplemental Figure 1).
In a three-way deterministic sensitivity analysis evaluating percent of people linking to MOUD post-incarceration, duration on MOUD post-incarceration, and risk of overdose post-incarceration, our model found that more deaths were expected in Policy Scenario B unless at least 90% of people linked to MOUD post-incarceration with an average MOUD duration of 26 months, or 100% of people linked to MOUD post-incarceration with an average MOUD duration of 22 months. When risk of death post-incarceration was reduced to equal that without incarceration, Policy Scenario B shows fewer deaths than Policy Scenario A with no MOUD linkage from prison (likely due to prison acting as a protective factor since mortality is lower in the model during incarceration). Assuming risk of death multipliers for opioid overdose mortality post-incarceration of >1, 100% of people needed to link to MOUD post-incarceration with 16 months duration on MOUD, or over 70% of people needed to link to MOUD post-incarceration with 26 months duration on MOUD before Policy Scenario B showed fewer deaths than Policy Scenario A with no interventions (the base case).
When we assumed a 10% prevalence of current or previous incarceration in the model, 5-year mortality estimates for Policy Scenario A and Policy Scenario B increased by approximately 25% and incarceration estimates increased by approximately 80% to nearly 200%. Changes in fatal overdoses between Policy Scenario A and Policy Scenario B with increasingly strict fentanyl possession policies remained consistent with those in the base case analysis. However, incarcerations increased less dramatically (almost 100% in the base case, near 30% in the analysis considering previous incarceration). Though the magnitude of the increases were less extreme, conclusions of the analysis remained consistent with the initial analysis.
In the one-way sensitivity analysis examining the potential for stricter policies to lead to discontinuation of fentanyl use, we found that more than 50% of those possessing >1 gram of fentanyl would need to discontinue fentanyl use in order for deaths to not increase with implementation of Policy Scenario B. It is important to note that this meant full discontinuation of opioid use, as we do not capture non-fentanyl overdoses in the model.
Results were consistent at 1- and 10- year time periods (Supplemental Tables 1–2).
Discussion
In our analysis, we estimated the long-term implications of increasingly punitive drug possession policies for fentanyl possession in Colorado. Our analyses showed that more enhanced policies could lead to increased deaths from opioid overdose, increases in the number of people incarcerated, and substantially increased costs due to both. Even when allowing for wide uncertainty intervals for key parameter estimates in probabilistic sensitivity analyses, our model predicted increased deaths and incarceration over the base case 100% of the time. Interventions such as diversion programs and MOUD in jails and post-incarceration alleviate some of the impact of increased rates of incarceration, but even with these programs in place, our model showed net increases in both overdose deaths and incarceration for possession. Our two-way deterministic sensitivity analysis showed that over 90% of people would need to be linked directly to MOUD care services post-incarceration and would need to stay in care for almost around 2 years before Policy Scenario B led to fewer deaths than the base case. As the average duration of MOUD retention in the US is 6 months (40, 41) and linkage to MOUD post-incarceration has been estimated at around 48% (48–50), these are unrealistic assumptions and strengthen the credibility the of our primary conclusion in this paper.
In addition to increased deaths and incarceration, costs (combined for MOUD, incarceration, and diversion) were substantially higher as drug possession policies grew more punitive in our model. Shifting from the 4g policy to the 1g policy led to total cost increases from $100 million to $150 million over 5 years in Colorado. Moving from 1g policy to any amount policy increased spending by approximately another half a billion dollars over a 5-year period in this one state. Spending on the carceral system in the US is already higher than any other country, and a recent study shows that in most US cities spending on the carceral system overtakes spending on all health and services systems combined (51).
Finally, even when we accounted for MOUD during incarceration and diversion programs, mortality due to the enhanced penalties for fentanyl possession remained above 1,000 deaths over 5 years in the state. While these programs are valuable and should be standard of care, our models demonstrate that they are not a replacement for providing greater coverage of MOUD and strengthening linkage to care in the community in terms of deaths and incarcerations averted and costs saved.
We acknowledge that the stated goal of increased criminalization of drug possession is to ultimately reduce use and therefore associated risks, including overdose and incarceration. However, previous iterations of such policies, especially during the “War on Drugs” era, showed that this is rarely if ever the case, and data continues to support this. Unlike drug treatment and harm reduction efforts, (4, 39, 52) criminalization has not been proven to reduce drug use or its sequelae (11–13, 43). Given that the two parameters with the most effect on both death and incarceration in our model were the size of the population in possession of fentanyl and the fatal overdose rate, legislative efforts may be more effective if they focus on prevention of drug use and prevention of overdose. Addressing upstreams factors such as untreated mental illness, particularly in school aged children, and increasing naloxone and MOUD availability are likely to have the most positive impact on decrease fentanyl-related overdoses—not criminalization.
There are limitations to our study. The model is a simplified version of the impact of different penalties on possession of fentanyl-containing drugs under a number of various scenarios. For this reason, the results from the model should be seen as a broad assessment of effects these policy changes and not a precise numerical prediction of deaths and dollars associated with them. However, in our PSA and threshold analyses, under broad assumptions about parameter values, all analyses showed a benefit for Policy Scenario A (least criminalization of fentanyl possession) and a stark increase in deaths and costs with new, enhanced policies for possession, like those initiated in Colorado. We have provided a simple policy model looking at the effects of fentanyl felonization, but do not capture all the scenarios that may occur in this setting; for instance, we do not consider secondary effects the policy might have on likelihood of people to call emergency medical services for overdoses as penalties for drug possession rise. In addition, the model cannot account for additional policy changes or innovations that may take place within the length of time of our simulation. Due to this, we choose to focus on 5-year results rather than 10-year estimates, to minimize the changes that might occur over longer lengths of time. Much of the data surrounding illicit opioid use is uncertain, including the size of the population in possession of fentanyl or other opioids at any given time. Because of this, our parameters in this model incorporate broad ranges for each and include the online tool which can be used by decision-makers and stakeholders to evaluate policy implications under different data assumptions and scenarios. In addition, due to the uncertainty in parameters as well as future trends in opioid mortality and policy, we have chosen to include credible intervals, together with additional sensitivity analyses to assess the outcomes under each policy. Our model only considers those who possess fentanyl and also use fentanyl, and does not model those who only sell the drug and have no risk of overdose. It is possible that a response to stricter drug possession penalties based on amount of drug in possession might simply lead to people choosing to carry less fentanyl to avoid arrest while not changing their consumption, therefore, effectively, leading to no change in deaths or incarcerations. This seems unlikely given historical trends in alcohol and other drug use (e.g., crack, cocaine) following more prohibitive laws (22, 38, 53). We do not model mortality due to causes other than fatal opioid overdose in our model, though it is expected that a small proportion of the population will die of causes other than overdose. In addition, we assume that those on MOUD do not fatally overdose, though in reality people on MOUD can use opioids and overdose even while on treatment. This is a simplification made for the model which purposefully overestimates the effect of MOUD, strengthening our findings that even offering treatment to those incarcerated does not outweigh the risks that come with the incarceration. Lastly, we do not consider heterogeneity of fentanyl penetration or opioid use around the state, though likely differences exist between different counties as well as urban and rural areas.
In conclusion, our analysis suggests that increased criminalization of possession of fentanyl containing drugs may lead to increased deaths and incarceration, even with interventions to mitigate the impact of these measures in place. In addressing the opioid epidemic in the US, it is critical that policy makers understand the implications of potential new initiatives and legislation, and we hope we have demonstrated here the harmful effects of implementing new measures without investigating their human and economic costs.
Supplementary Material
Figure 1.
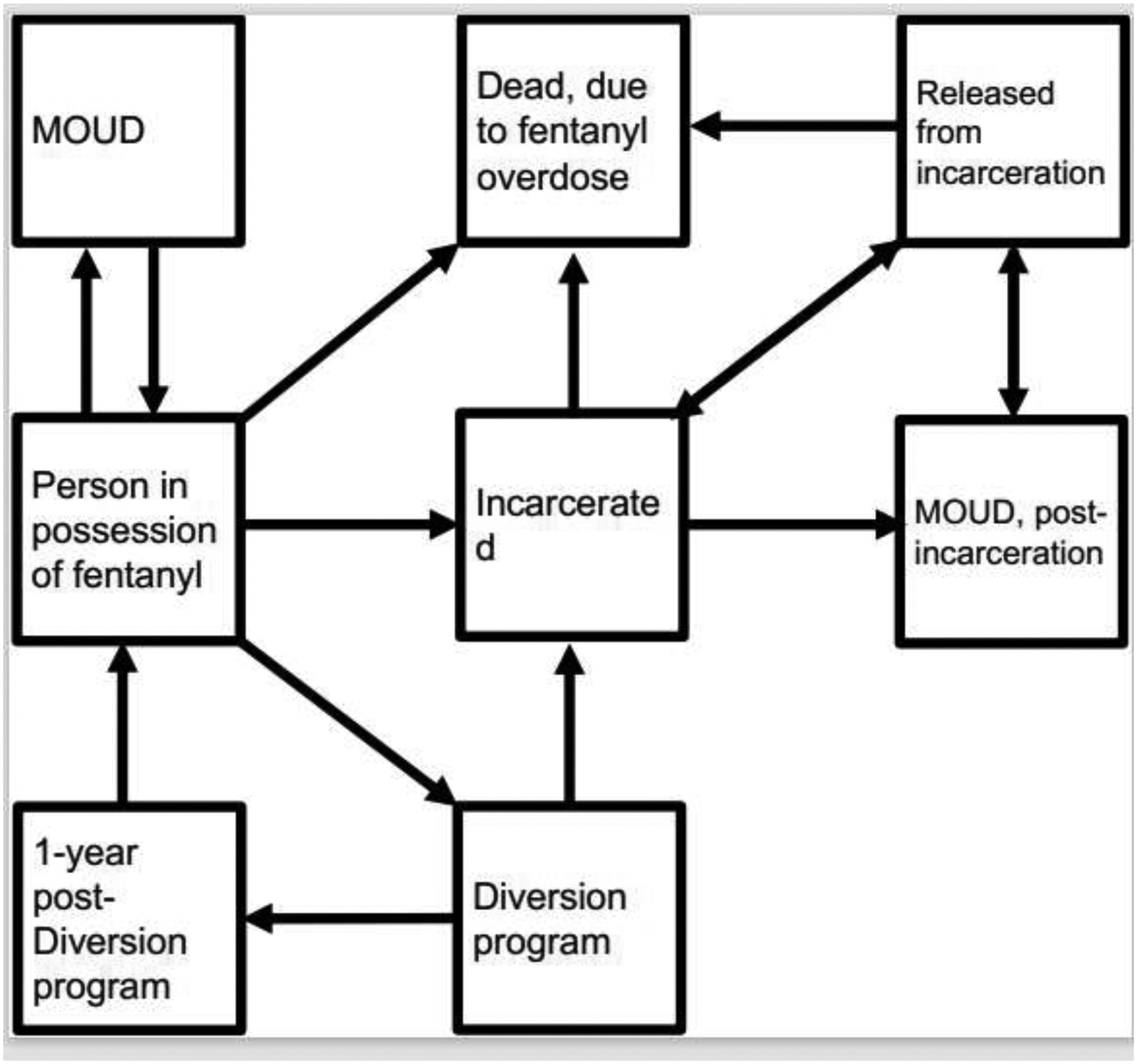
Model diagram.
Role of the Funding Source:
This study was funded by grants from the National Institute on Drug Abuse and the Colorado Department of Human Services, which had no direct role in the design, conduct, and analysis of the study or in the decision to submit the manuscript for publication.
All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding.
This work was supported by the National Institute on Drug Abuse (JAB: K01DA051684 & DP2DA051864; GG: DP2DA049282 & 5R37DA015612). This work was also supported by the Colorado Department of Human Services (JAB, CJ).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Ethics approval
The authors declare that they have obtained ethics approval from an appropriately constituted ethics committee/institutional review board where the research entailed animal or human participation.
Author CRediT Statement:
Alexandra Savinkina: Conceptualization, Methodology, Formal Analysis, Writing-Original Draft, Visualization
Cole Jurecka: Investigation, Resources, Conceptualization, Writing- Review and Editing
Gregg Gonsalves: Conceptualization, Writing-Review and Editing, Conceptualization
Josh Barocas: Conceptualization, Methodology, Supervision
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.NIDA 2022;Pages https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates on 12/7 2022.
- 2.CDC. U.S. Overdose Deaths In 2021 Increased Half as Much as in 2020 – But Are Still Up 15% 2022.
- 3.Hser YI, Ober AJ, Dopp AR, Lin C, Osterhage KP, Clingan SE, et al. Is telemedicine the answer to rural expansion of medication treatment for opioid use disorder? Early experiences in the feasibility study phase of a National Drug Abuse Treatment Clinical Trials Network Trial. Addict Sci Clin Pract. 2021;16(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nesoff ED, Marziali ME, Martins SS. The estimated impact of state-level support for expanded delivery of substance use disorder treatment during the COVID-19 pandemic. Addiction. 2022;117(6):1781–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson NL, Choi S, Herrera CN. Black clients in expansion states who used opioids were more likely to access medication for opioid use disorder after ACA implementation. J Subst Abuse Treat. 2022;133:108533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng Y, Freeman PR, Slade E, Sohn M, Talbert JC, Delcher C. Medicaid expansion and access to naloxone in metropolitan and nonmetropolitan areas. J Rural Health. 2022. [DOI] [PubMed] [Google Scholar]
- 7.Spector AL, Galletly CL, Christenson EA, Montaque HDG, Dickson-Gomez J. A qualitative examination of naloxone access in three states: Connecticut, Kentucky, and Wisconsin. BMC Public Health. 2022;22(1):1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Razaghizad A, Windle SB, Filion KB, Gore G, Kudrina I, Paraskevopoulos E, et al. The Effect of Overdose Education and Naloxone Distribution: An Umbrella Review of Systematic Reviews. Am J Public Health. 2021;111(8):e1–e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain - United States, 2022. MMWR Recomm Rep. 2022;71(3):1–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiang MV, Humphreys K, Cullen MR, Basu S. Opioid prescribing patterns among medical providers in the United States, 2003–17: retrospective, observational study. Bmj. 2020;368:l6968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volkow N Punishing Drug Use Heightens the Stigma of Addiction. In: National Institute on Drug Abuse, ed; 2021. [Google Scholar]
- 12.PEW Charitable Trusts 2018;Pages https://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2018/03/more-imprisonment-does-not-reduce-state-drug-problems on 2/9 2023.
- 13.PEW Charitable Trusts 2015;Pages https://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2015/08/federal-drug-sentencing-laws-bring-high-cost-low-return on 2/9 2023.
- 14.Wisconsin Legislature. 2021 Wisconsin Act 179. 2022.
- 15.Kentucky Legistature. House Bill 215. 2022.
- 16.Mississippi Legislature. House Bill 607. 2022.
- 17.US House of Representatives. H.R. 467 2023.
- 18.Alliance DP 2022;Pages https://drugpolicy.org/decrim/laws on 2/24 2023.
- 19.HB22–1326 Fentanyl Accountability and Prevention. In: Assembly CG, ed; 2022. [Google Scholar]
- 20.Paul SNJ. Here’s what’s in the Colorado fentanyl “accountability and prevention” bill just signed into law. The Colorado Sun; 2022. [Google Scholar]
- 21.Borden TR B; Goldman M; Smith WP 2016;Pages https://www.hrw.org/report/2016/10/12/every-25-seconds/human-toll-criminalizing-drug-use-united-states on 2/9 2023.
- 22.Pearl B Ending the War on Drugs: By the Numbers. Center for American Progress; 2018. [Google Scholar]
- 23.Langan PA. The racial disparity in US drug arrests. Bureau of Justice Statistics (BJS) and US Dept Justice and Office of Justice Programs and United States of America. 1995. [Google Scholar]
- 24.Ranapurwala SI, Shanahan ME, Alexandridis AA, Proescholdbell SK, Naumann RB, Edwards D Jr., et al. Opioid Overdose Mortality Among Former North Carolina Inmates: 2000–2015. Am J Public Health. 2018;108(9):1207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marsden J, Stillwell G, Jones H, Cooper A, Eastwood B, Farrell M, et al. Does exposure to opioid substitution treatment in prison reduce the risk of death after release? A national prospective observational study in England. Addiction. 2017;112(8):1408–18. [DOI] [PubMed] [Google Scholar]
- 26.Duncan A Opioid Use Disorder Treatment in Jails and Prisons. Pew Pew Charitable Trusts; 2020. [Google Scholar]
- 27.Colorado Judicial Department. Adult Diversion Program Annual Legislative Report Fiscal Year 2021. In: Department CJ, ed; 2021. [Google Scholar]
- 28.James LP, Salomon JA, Buckee CO, Menzies NA. The use and misuse of mathematical modeling for infectious disease policymaking: lessons for the COVID-19 pandemic. Medical Decision Making. 2021;41(4):379–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boden LA, McKendrick IJ. Model-based policymaking: A framework to promote ethical “good practice” in mathematical modeling for public health policymaking. Frontiers in public health. 2017:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gonsalves GS, Salomon JA, Thornhill T, Paltiel AD. Adventures in COVID-19 Policy Modeling: Education Edition. Curr HIV/AIDS Rep. 2022;19(1):94–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoff RA, Baranosky MV, Buchanan J, Zonana H, Rosenheck RA. The effects of a jail diversion program on incarceration: A retrospective cohort study. Journal of the American Academy of Psychiatry and the Law Online. 1999;27(3):377–86. [PubMed] [Google Scholar]
- 32.Schwalbe CS, Gearing RE, MacKenzie MJ, Brewer KB, Ibrahim R. A meta-analysis of experimental studies of diversion programs for juvenile offenders. Clinical psychology review. 2012;32(1):26–33. [DOI] [PubMed] [Google Scholar]
- 33.Kaplowitz E, Truong AQ, Macmadu A, Peterson M, Brinkley-Rubinstein L, Potter N, et al. Fentanyl-related overdose during incarceration: a comprehensive review. Health & justice. 2021;9(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Belenko S, Hiller M, Hamilton L. Treating substance use disorders in the criminal justice system. Curr Psychiatry Rep. 2013;15(11):414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abuse S. Mental Health Data Archive. Substance Abuse and Mental Health Services Administration (SAMHSA). National survey on drug use and health file NSDUH-2002–2019-DS0001. https://www.datafiles.samhsa.gov/study-dataset/nsduh-2002-2019-ds0001-nsduh-2002-2019-ds0001-nid19112. Accessed March. 2021;25.
- 36.DDPHE Issues Guidance Regarding Fentanyl in Denver: Be Cautious. In: Environment DDoPHa, ed. denvergov.org; 2022. [Google Scholar]
- 37.Centers for Disease Control and Prevention. Drug Overdose Mortality by State. 2022.
- 38.Kennedy JE, Unah I, Wahlers K. Sharks and minnows in the war on drugs: A study of quantity, race and drug type in drug arrests. UC Davis L. Rev 2018;52:729. [Google Scholar]
- 39.Krawczyk N, Rivera BD, Jent V, Keyes KM, Jones CM, Cerdá M. Has the treatment gap for opioid use disorder narrowed in the U.S.?: A yearly assessment from 2010 to 2019”. Int J Drug Policy. 2022:103786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morgan JR, Schackman BR, Leff JA, Linas BP, Walley AY. Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. J Subst Abuse Treat. 2018;85:90–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morgan JR, Walley AY, Murphy SM, Chatterjee A, Hadland SE, Barocas J, et al. Characterizing initiation, use, and discontinuation of extended-release buprenorphine in a nationally representative United States commercially insured cohort. Drug Alcohol Depend. 2021;225:108764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Langan PA, Levin DJ. Recidivism of prisoners released in 1994: US Department of Justice, Office of Justice Programs, Bureau of Justice; …; 2002. [Google Scholar]
- 43.PEW Charitable Trusts 2022;Pages https://www.pewtrusts.org/en/research-and-analysis/issue-briefs/2022/02/drug-arrests-stayed-high-even-as-imprisonment-fell-from-2009-to-2019 on 2/9 2023.
- 44.Vera 2015;Pages https://www.vera.org/publications/price-of-prisons-2015-state-spending-trends/price-of-prisons-2015-state-spending-trends/price-of-prisons-2015-state-spending-trends-prison-spending on 2/9 2023.
- 45.Florence C, Luo F, Rice K. The economic burden of opioid use disorder and fatal opioid overdose in the United States, 2017. Drug Alcohol Depend. 2021;218:108350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.George Brauchler MM, Steven Byers. Crime in Colorado in 2022: The Data on Colorado’s Increasing Crime Problem Common Sense Institute CO; 2022. [Google Scholar]
- 47.Alison Rosenthal JR. Public Safety and Substance Use. In: Safety CDoP, ed; 2022. [Google Scholar]
- 48.Gordon MS, Kinlock TW, Schwartz RP, Fitzgerald TT, O’Grady KE, Vocci FJ. A randomized controlled trial of prison-initiated buprenorphine: prison outcomes and community treatment entry. Drug Alcohol Depend. 2014;142:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gordon MS, Kinlock TW, Schwartz RP, O’Grady KE, Fitzgerald TT, Vocci FJ. A randomized clinical trial of buprenorphine for prisoners: Findings at 12-months post-release. Drug Alcohol Depend. 2017;172:34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Magura S, Lee JD, Hershberger J, Joseph H, Marsch L, Shropshire C, et al. Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug Alcohol Depend. 2009;99(1–3):222–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Skaathun B, Maviglia F, Vo A, McBride A, Seymour S, Mendez S, et al. Prioritization of carceral spending in U.S. cities: Development of the Carceral Resource Index (CRI) and the role of race and income inequality. PLoS One. 2022;17(12):e0276818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martin RA, Alexander-Scott N, Berk J, Carpenter RW, Kang A, Hoadley A, et al. Post-incarceration outcomes of a comprehensive statewide correctional MOUD program: a retrospective cohort study. Lancet Reg Health Am. 2023;18:100419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Burrus T The Hidden Costs of Drug Prohibition. CATO Institute; 2019. [Google Scholar]
- 54.Ahmad FB CJ, Rossen LA, Sutton P. Provisional drug overdose death counts. In: Statistics NCfH, ed; 2023. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


