Abstract
Background:
Hip fractures are costly and common in older adults, but there is limited understanding of how treatment patterns and outcomes might differ between countries.
Methods:
We performed a retrospective serial cross-sectional cohort study of adults aged ≥ 66 years hospitalized with hip fracture between 2011 and 2018 in the US, Canada, England, Netherlands, Taiwan, and Israel using population-representative administrative data. We examined mortality, hip fracture treatment approaches (total hip arthroplasty [THA], hemiarthroplasty [HA], internal fixation [IF], and non-operative), and health system performance measures, including hospital length of stay (LOS), 30-day readmission rates and time-to-surgery.
Results:
The total number of hip fracture admissions between 2011–2018 ranged from 23,941 in Israel to 1,219,696 in the US. In 2018, 30-day mortality varied from 3% (16% at 1-year) in Taiwan to 10% (27%) in the Netherlands. With regards to processes of care, the proportion of hip fractures treated with HA (range 23–45%) and THA (0.2–10%) differed widely across countries. For example, in 2018, THA was used to treat approximately 9% of patients in England and Israel but less than 1% in Taiwan. Overall, IF was the most common surgery performed in all countries (40–60% of patients). IF was used in approximately 60% of patients in the US and Israel but 40% in England. In 2018 rates of non-operative management ranged from 5% of patients in Taiwan to nearly 10% in England. Mean hospital LOS in 2018 ranged from 6.4 days (US) to 18.7 days (England). The 30-day readmission rate in 2018 ranged from 8% (Canada and Netherlands) to nearly 18% in England. The mean days to surgery in 2018 ranged from 0.5 days (Israel) to 1.6 days (Canada).
Conclusions:
We observed substantial between-country variation in mortality, surgical approaches, and health system performance measures. These findings underscore the need for further research to inform evidence-based surgical approaches.
Keywords: Hip fracture, Osteoporosis, Longevity, Healthcare policy, International comparison
INTRODUCTION
Hip fractures are costly and a common cause of morbidity and mortality in older patients, with an expected annual cost of $25.3 billion in the US ($1.25 billion in England).1–3 Despite improvements in surgical technique and postoperative management, mortality within one year of a hip fracture remains high (14%−36%), and survivors frequently do not return to their functional baseline.4–6 Moreover, the aging population in high-income countries portends future increases in the number of hip fractures.2
The vast majority of older adults hospitalized with hip fractures undergo surgical repair. However, a significant percentage (5%−15%) with limited functional status or advanced illness may receive non-operative management with palliation.7–10 There are three principal types of surgical repair approaches for hip fractures: total hip arthroplasty (THA); hemiarthroplasty (HA); and internal fixation (IF), with non-operative management an option for those who are particularly frail. With very few randomized trials to guide the choice of surgery, treatment often depends upon fracture type, surgeon preference, hospital capabilities (e.g., implant availability), and health system factors (e.g., regionalization, payment incentives for physicians and hospitals).11–14
Hip fracture provides an ideal condition for international comparisons of hospital-based care and outcomes because it is common, and virtually all patients require hospitalization, minimizing selection effects that might be present for conditions where hospitalization is discretionary. Studies comparing hip fracture treatment across high-income countries are limited. Some were not nationally representative,15,16 limited to a small number of countries,15,17–19 or relied upon aggregated data.2,20 Moreover, many studies have not evaluated between-country differences in the repair procedure used.16,21,22
In this study from the International Health Systems Research Collaborative (IHSRC: https://projects.iq.harvard.edu/ihsrc/people), we used nationally representative patient-level data from six high-income countries (US, Canada, England, Netherlands, Israel, and Taiwan) to identify older adults hospitalized with a hip fracture between 2011–2018.23,24 We compared countries with respect to surgical treatments (THA, HA, IF, non-operative), mortality, hospital length-of-stay (LOS), 30-day readmission, discharge disposition, and days from presentation to surgery and examined how rates changed over time.
METHODS
Data sources and study patients
In this retrospective serial cross-sectional cohort study, we identified patients aged 66 years and older who were hospitalized with a primary diagnosis of hip fracture between January 1, 2011 and December 31, 2018 (2013–18 for the Netherlands). In each consecutive year within the study period, we compared each nation separately, using administrative data that broadly represent the population (Supplementary S1). To identify patients hospitalized with hip fractures, we used established coding algorithms based upon relevant ICD-9 and ICD-10 codes (Supplementary S2).23 We allowed minor adaptations to the coding scheme to reflect differences between countries. We applied identical inclusion and exclusion criteria in the same order in each country, with slight country-specific exceptions.
We excluded high-energy hip fractures25 (e.g., falls from significant heights, vehicular trauma, etc.) and patients with hip fracture admission during the preceding 180-day period (to avoid counting readmissions as new admissions). We also excluded small numbers of patients with missing age or sex, residence outside the jurisdiction of admission, and patients with less than one year of pre-admission or post-admission follow-up data with the exception of those who died during follow-up (Supplementary S3). We also excluded US patients who were enrolled in Medicare Advantage insurance plans for two or more months during the year before or after hip fracture hospitalization because certain data elements may not be available. For patients transferred between hospitals, we evaluated the complete episode of care from initial admission to final hospital discharge. Comorbid conditions were identified from the index admission and prior hospitalizations in the year before the index admission using an adaptation of the Elixhauser comorbidity measures.26 In Israel, comorbid diagnoses included those given in primary care ambulatory settings, as medical record systems integrate both hospital and primary care visits.
Outcomes
First, we evaluated mortality within 30-days and one-year of index hospital admission. Second, we evaluated the percentage of patients with hip fractures receiving each type of treatment (THA, HA, IF, and non-operative). For patients with multiple procedures during the index admission, we assigned the most extensive repair type first (THA>HA>IF), and patients were only deemed non-operative if they lacked procedure codes for all surgical repair types. We also examined hospital length of stay (LOS) and readmission within 30 days of discharge among those discharged alive. We also examined discharge disposition (home versus not) and days from hospital admission to surgery (for those receiving surgery) in the four countries (US, Canada, Netherlands, and Israel) that could provide these data.
Statistical Analyses
We calculated the annual hip fracture rate as the number of hospitalizations per 1,000 population age ≥ 66 years for each country and calendar year and directly standardized to the age-sex distribution of the US age 66+ population in 2018.27 We similarly used direct standardization to compare the outcomes specified above. For simplicity, we report data from the first (2011) and last years (2018), with data for all years in the supplementary appendix. We did not adjust our outcomes for comorbid conditions because of the implausibly large between-country differences in the prevalence of comorbid conditions; these differences are less likely to reflect actual differences in the hip fracture populations across countries but rather differences in the financial incentives to code patient complexity.28,29 Furthermore, multiple studies have shown that comorbid conditions have a little overall impact on hip fracture outcomes above age and sex alone.30
To evaluate the robustness of our results among patients with greater and lesser frailty, we performed subgroup analysis among individuals greater-than and less-than 90-years of age using age as a proxy for frailty and underlying health status, again standardized to the US 2018 sex distribution of these strata. This study intends to draw attention to the differences in hip fracture care patterns between countries over time and is descriptive in nature. Moreover, given our large sample size, we chose not to conduct formal statistical testing (e.g., reporting p values), cognizant of the potential for such testing to overemphasize clinically inconsequential differences.31 Our analyses were conducted using SAS (US, Canada, Taiwan) and R (England, Israel, Netherlands). Analyses were conducted locally in each country, and ethics approval was obtained following local guidelines.
RESULTS
Patient populations
The number of hip fracture admissions across the study period ranged from 23,941 in Israel to 1,219,696 in the US (Table 1 and Supplementary S4). The mean age was 83–84 years in most countries, but slightly younger in Taiwan; females comprised 71%−75% of the population, but somewhat less (64%−67%) in Taiwan (Table 1). There were significant between-country differences in the recorded prevalence of comorbid conditions, including hypertension, diabetes, and hypothyroidism (Table 1). In 2018, the age and sex-standardized annual incidence of hip fracture was 4.6 per 1,000 population in the US but was somewhat higher in Taiwan (6.3) and lower in England (3.6) (Supplementary S5).
Table 1:
Socio-demographic characteristics and select comorbid conditions for patients hospitalized with hip fracture in 2011 and 2018 in the US, Canada (Ontario and Manitoba), England, Netherlands (2013 and 2018), Israel, and Taiwan
| 2011 | 2018 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Metric | US N=161,626 |
Canada 9,495 |
England 9,603 |
Netherlands 12,9452 |
Israel 2,628 |
Taiwan 15,792 |
US 143,329 |
Canada 11,006 |
England 7,531 |
Netherlands 15,170 |
Israel 3,298 |
Taiwan 17,917 |
| Female (%) | 73.7 | 73.4 | 74.9 | 74.0 | 70.6 | 63.6 | 71.2 | 70.8 | 71.5 | 71.1 | 67.2 | 67.3 |
| Age, mean | 84.2 | 83.9 | 84.8 | 83.9 | 82.8 | 80.9 | 83.7 | 83.9 | 84.4 | 83.4 | 83.0 | 81.9 |
| Comorbid conditions (%) | ||||||||||||
| CHF | 21.7 | 4.11 | 11.1 | 1.2 | 13.6 | 7.3 | 22.5 | 4.03 | 14.4 | 0.8 | 13.1 | 6.6 |
| Hypertension uncomplicated | 63.8 | 28.41 | 53.2 | 16.7 | 60.8 | 44.3 | 54.9 | 21.13 | 60.7 | 29.0 | 56.5 | 42.5 |
| Diabetes - uncomplicated | 20.5 | 6.51 | 15.2 | 12.9 | 31.5 | 29.2 | 13.2 | 6.33 | 17.4 | 16.6 | 32.0 | 23.8 |
| Hypothyroidism | 23.3 | N/A | 10.5 | 1.1 | 11.3 | 0.4 | 26.0 | N/A | 13.1 | 2.6 | 11.5 | 0.4 |
2011 and 2012 pooled due to small cell sizes.
2013 data shown; data unavailable for 2011–12
2017 and 2018 data were pooled due to small cell sizes.
Mortality
Age and sex standardized 30-day and 1-year mortality varied widely between countries (Figure 1 and Supplementary S6). In 2018, standardized 30-day mortality was lowest in Taiwan (3.0%) and highest in the Netherlands (10.3%). One-year mortality in 2018 was lowest in Taiwan (15.7%) and England (19.4%) and highest in the US (26.2%) and the Netherlands (27.5%). Between 2011 and 2018, 1-year mortality declined by between 0.4% and 1.5% in all countries except England (0.9% increase).
Figure 1:
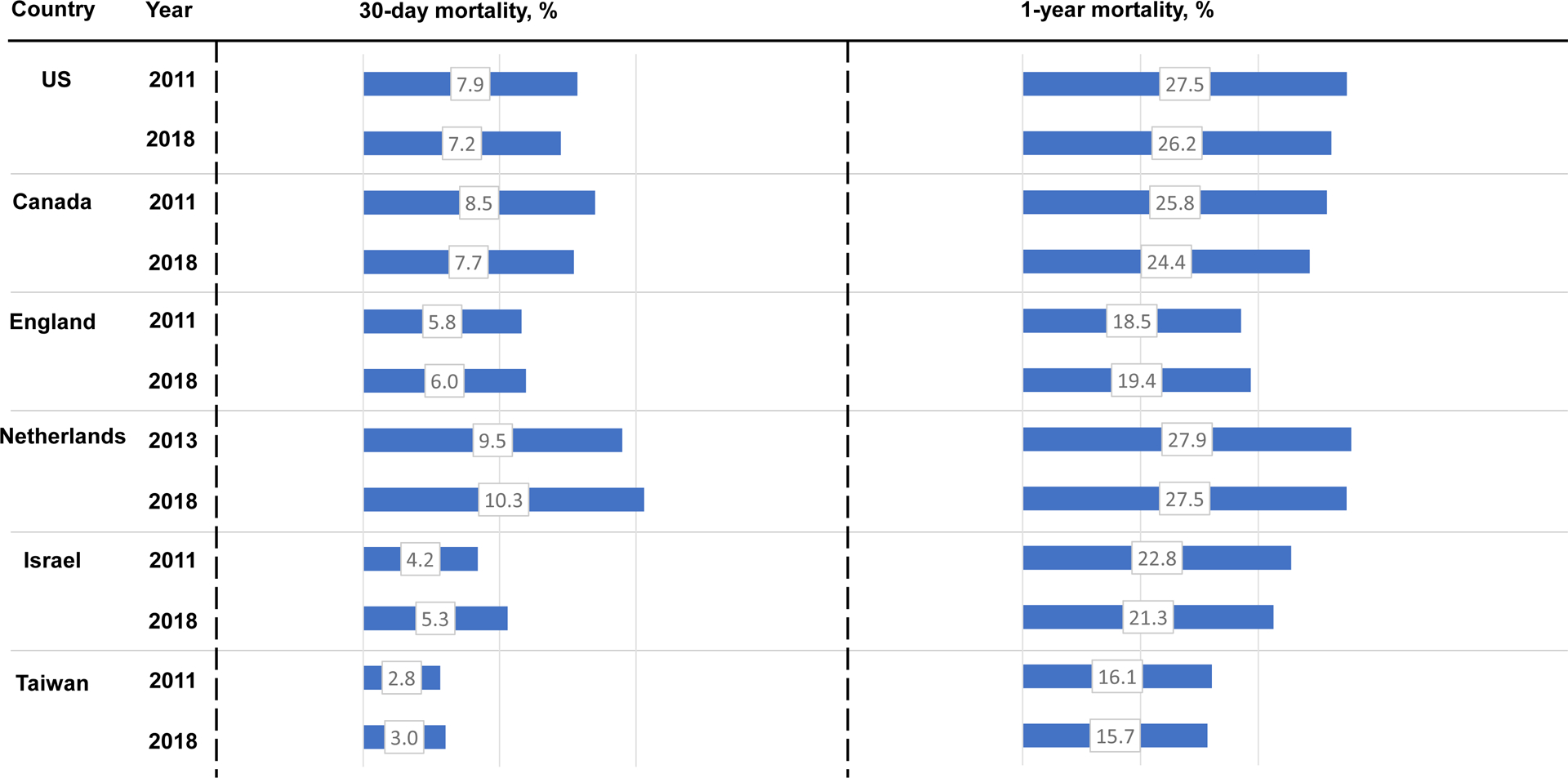
Age- and sex-standardized 30-day and 1-year mortality, 2011 and 2018.
Surgical Approach
There were vast between-country differences in the treatment practices of hip fractures (Figure 2 and Supplementary S7–8). For example, in 2018, THA was used to treat 9.4% of hip fractures in England, and 9.1% of hip fractures in Israel but just 0.7% in Taiwan. Similarly, in 2018 HA was used to treat 39.1% of hip fractures in England and Taiwan but 22.8% in Israel. In 2018 fixation was used to treat 50%−60% of hip fractures in most countries but just 42.2% in England. The percentage of patients treated non-operatively in 2018 ranged from 4.6% (Taiwan) to 9.7% in England. Rates of non-operative management decreased from 2011–2018 in England, Israel, and Taiwan (11.6% to 9.7% and 13.5% to 6.1%, 5.4% to 4.6%, respectively), but increased in the remaining countries.
Figure 2:
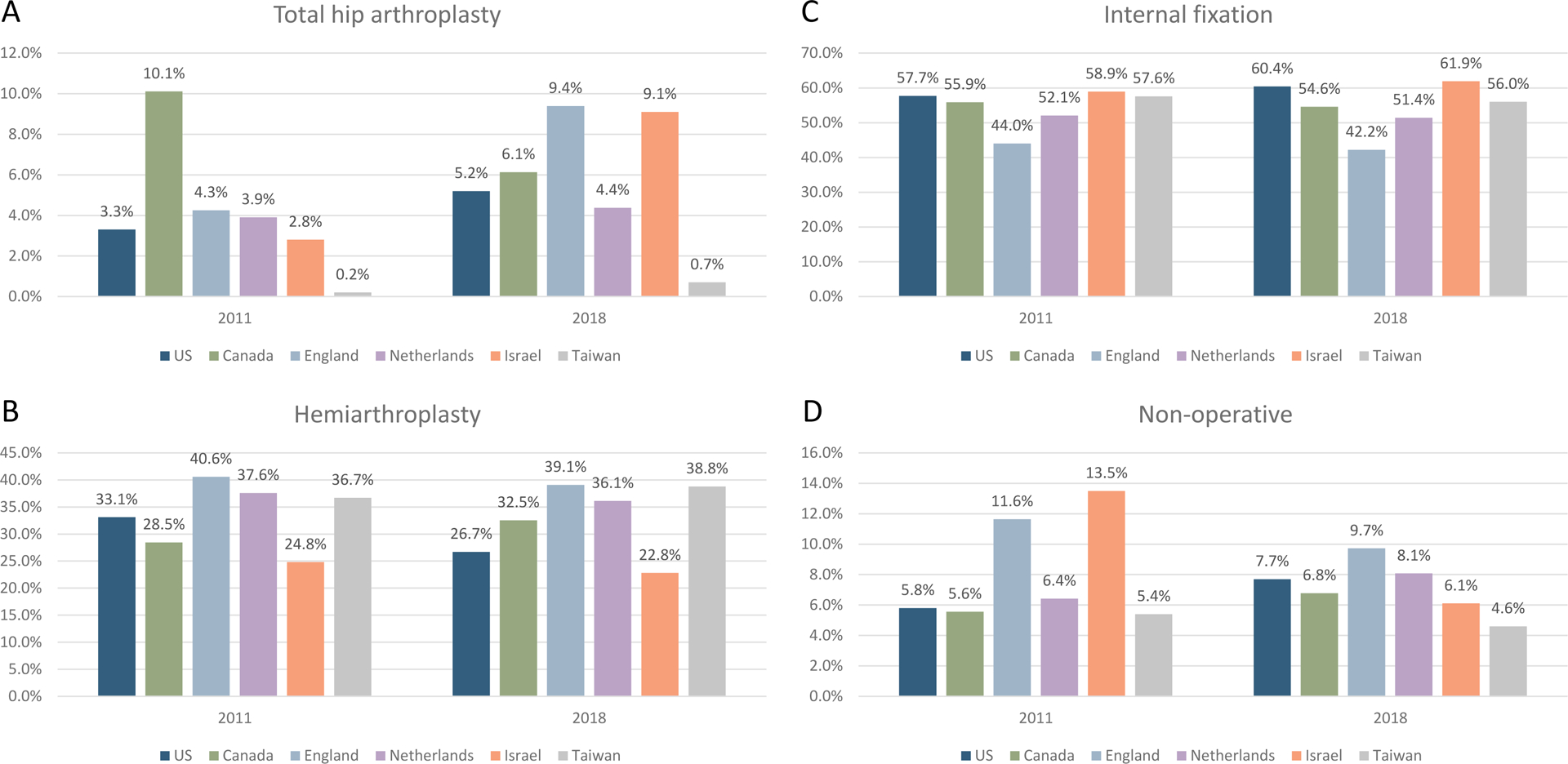
Age- and sex-standardized rates of total hip arthroplasty (THA), hemiarthroplasty (HA), internal fixation (IF), and non-operative management (non-op) after hospitalization for hip fracture, 2011 and 2018.
Health system performance factors
In 2018 hospital LOS was shortest in the US (6.4 days) and longest in Canada (14.0 days) and England (18.7 days) (Figure 3). Between 2011 and 2018 the mean LOS decreased by at least one day in all countries except the Netherlands, with a decrease of 3.6 days in England. The 2018 30-day hospital readmission rate was lowest in Canada (7.8%) and highest in England (17.6%). Between 2011 and 2018, the 30-day readmission rate declined in four countries but increased in two (England and Israel) (Figure 3). Among the four countries with available data, the mean days between hospital admission and surgical repair in 2018 ranged between 0.5 days (Israel) to 1.6 days in Canada (1.1 in the US and 1.5 in England). (Figure 4). The percentage of patients discharged home in 2018 was lowest in the US (9.6%) and highest in Israel (59.3%) (Figure 4).
Figure 3:
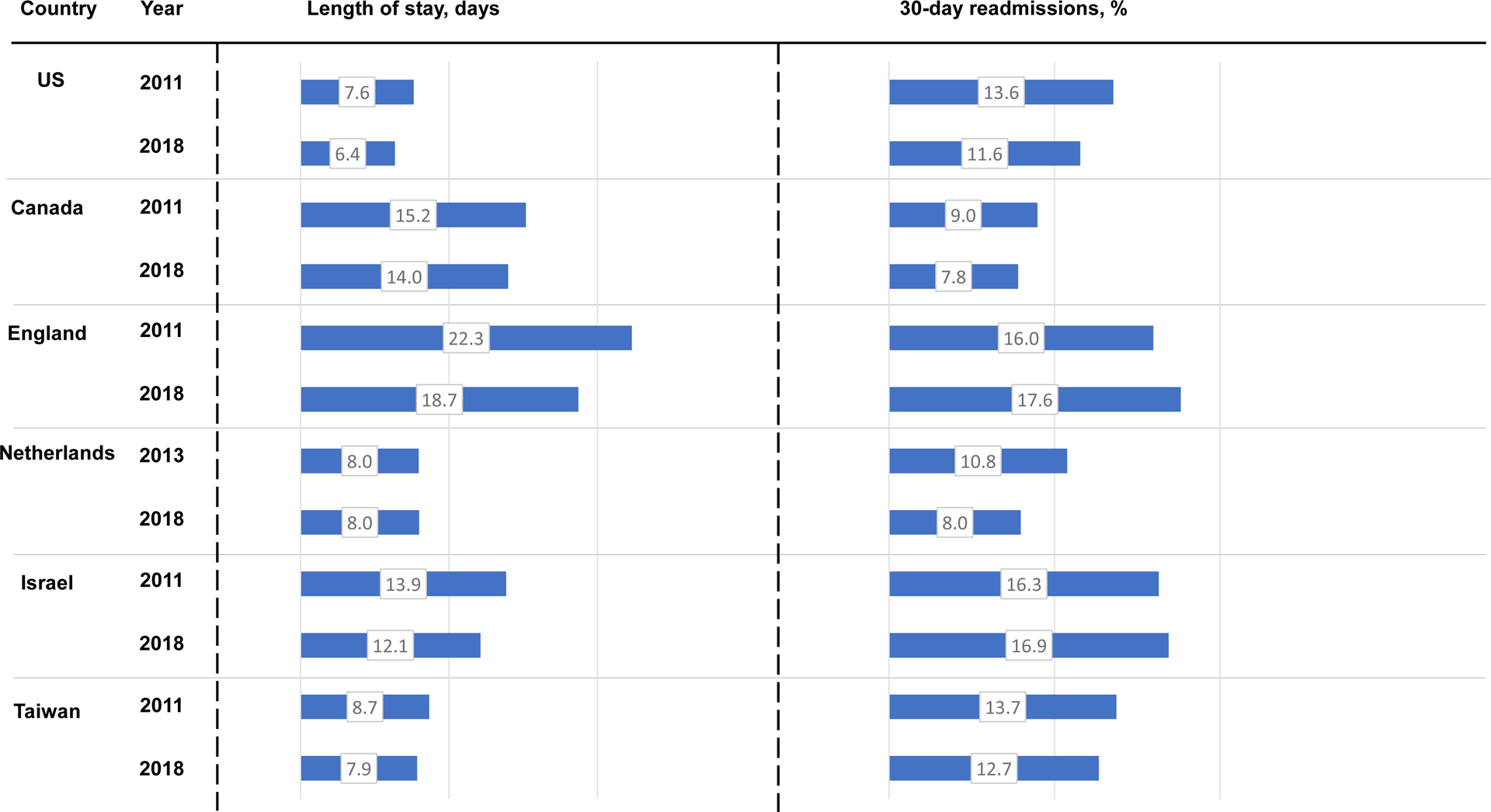
Age- and sex-standardized length of stay and 30-day readmissions rates, 2011 and 2018.
Figure 4:
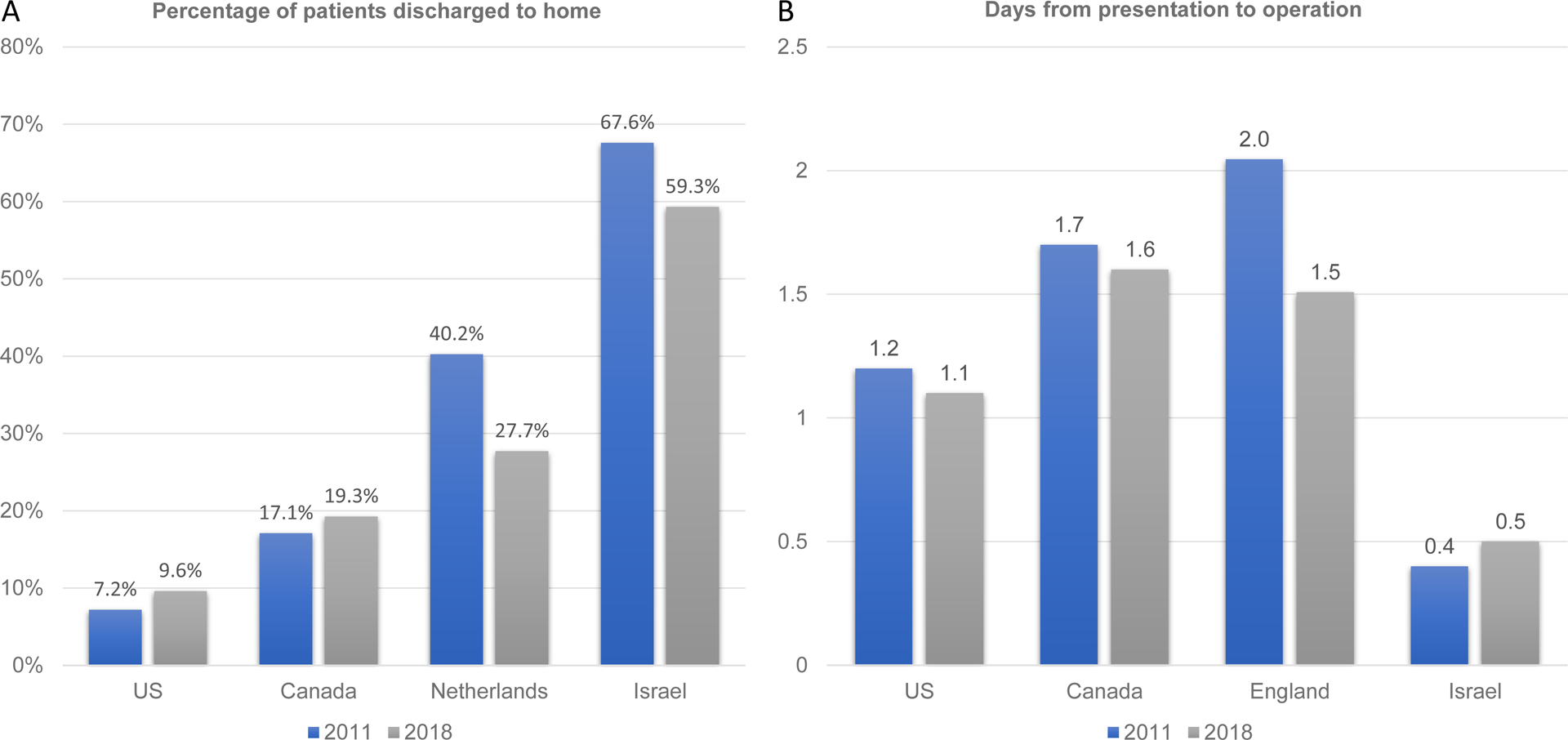
Age- and sex-standardized percentage of patients discharged to home and days from presentation to operation, 2011 and 2018.
Stratified Analysis by Age
Comparing patients aged below 90 and ≥ 90 years demonstrated several noteworthy findings (Supplementary S9–10). First, utilization of THA was 40%−70% lower among patients aged 90 and above than among patients younger than 90, but these findings showed substantial variation across countries. Second, the US showed the largest difference in the use of non-operative management across the age groups, increasing from ~3% in the <90 cohort to ~10% in those 90-and-older. In contrast, several of the countries showed relatively stable rates of non-operative management. For instance, rates of non-repair in the ≥90 versus <90 cohort in Canada and England showed a 2% or lower difference. Third, 30-day mortality rates were two times higher (or more) in the 90+ cohort versus those below 90 in all countries.
DISCUSSION
In this population-based study of patients hospitalized with acute hip fracture using health administrative data from six high-income countries, several findings are noteworthy. First, we observed substantial differences in both 30-day and one-year mortality across the countries, despite the similarities in the age and sex distribution of the populations. Second, there was marked between-country variation in the types of surgical repair used, and rates of non-operative treatment varied by up to a factor of two in the most recent year. Third, we observed significant between-country differences in hospital LOS, readmissions, the proportion of patients discharged home, and time from hospital presentation to surgery, suggesting substantial opportunities for countries to improve the efficiency of care provision.
Several findings deserve further discussion. First, the finding that one-year mortality in certain countries including the US and the Netherlands was 10% higher than in other countries is noteworthy. The finding of high mortality in the US is concerning in the context of other recent studies demonstrating that American patients hospitalized with other conditions also seem to have significantly higher mortality than their international peers.22,23 There is an urgent need to better understand the specific causes of this excess mortality in the US and to identify targets for intervention. The high mortality observed in the Netherlands is consistent with another recent study, but as in the US, we do not understand the underlying causes.32 In contrast, the low mortality observed in Taiwan is interesting and consistent with a recent study that found lower inpatient mortality for patients in Taiwan than in either Japan or Korea.19
Second, despite an estimated more than 2.6 million hip fractures annually worldwide by 2025, there remains substantial uncertainty about which type of surgical repair a given patient should receive.33 The choice of repair approach depends, in part, on the anatomy of the fracture (e.g., fixation for nondisplaced or intertrochanteric fractures versus THA or HA for displaced fractures of the femoral neck); age and functional status also are important considerations, with total hip arthroplasty generally reserved for younger, healthier patients.11,34 Though the HEALTH study found no appreciable benefit over two years for THA v. HA, we find wide variation in rates of THA and HA across the IHSRC countries. We also see rates of IF that vary by as much as 20%, which seems unlikely to be driven by differences in fracture epidemiology across countries. Thus, our study highlights the urgent need for more randomized and comparative effectiveness trials to better understand the optimal treatment approaches for hip fracture in older adults.11,12,35
In the context of the limited evidence to guide the choice of repair strategies, it is essential to consider how best to interpret the between-country variation we observed. We suspect that the large between country variation reflects differences in surgical team preferences and experience and health system financing and organization within each country. This pertains especially to patients for which several surgical options can be considered, as in the case of nondisplaced cervical fractures or the choice between THA and HA for displaced fractures.11,12 Looking at specific countries is particularly interesting; in 2018 England had the highest use of THA (9.4% of fractures), HA (39.1% of fractures), and non-operative management (9.7% of fractures) but far lower use of internal fixation (42.2%) than all other countries. Fixation is typically considered the least complex and least expensive surgical option, with HA being intermediate, and THA being the most complex, requiring significantly more time and more costly implants than the other options but potentially better outcomes for younger and healthier patients. Our results suggest a more treatment-intensive approach for most patients in England, paired with a higher rate of non-operative management, presumably reserved for the frailest patients. In contrast, in 2018, Taiwan had the lowest rate of both THA (0.7%) and non-operative management (4.6%) but higher use of both HA and fixation.
We doubt that these differences can be attributed to country-specific clinical factors such as differences in fracture anatomy or patient complexity, given our rigorous study protocol designed to capture the whole hip fracture population in each country. Furthermore, our surgical procedure rates were age and sex standardized to enhance comparability. Instead, we suspect that policy decisions, such as how care is organized, reimbursed, and incentivized play an important role. Since 2010, hospitals in England have been receiving a supplement for patient care that meets six clinical standards under the ‘Best Practice Tariff’ (BPT) program.36 These include a timed surgery within 36 hours, geriatric and rehabilitation specialist evaluation, and admission according to joint assessment protocol. Israel reduced non-operative rates by over half over the study period, possibly due to increased awareness of the importance of surgical repair and accompanying changes to direct payments for repair, particularly for THA, which tripled in rate.37,38 In contrast, the Taiwanese reimbursement system may not adequately incentivize surgeons and hospitals to perform THA and HA, resulting in higher rates of less complex fixation.19 In the US, modest rates of THA and higher rates of IF may well reflect discordance between the high amount of surgeon effort required to perform THA relative to reimbursement.39 In aggregate, the variation that we see likely reflects the more intentional design of hip fracture management programs and reimbursement models in certain countries combined with a lack of compelling data to generate strong international consensus on the best approaches. Moreover, it is essential to acknowledge that variations in non-operative rates are influenced by factors such as differing perspectives among surgeons, the availability of palliative care, and cultural and religious preferences surrounding end-of-life treatment.7 These factors likely contribute to the variation in non-operative management we observed and emphasize the need for future research to prioritize addressing them at a national level.
Third, it is important to consider health system performance measures. In 2018 mean hospital LOS ranged from 6.4 days in the US to 18.7 days in England, while 30-day readmissions ranged from 7.8% in Canada to 17.6% in England. The US (2018 LOS 6.0 days, readmission rate 11.6%) and the Netherlands (2018 LOS 8.0 days, readmission rate 8.0%) were both notable for short hospital LOS and low readmission rates. In the US, the short LOS is made possible by the high availability of skilled nursing facilities (SNFs). Alternatively, England’s combination of prolonged hospital LOS and high readmission rates is likely reflective of misaligned incentives for either hospitals or surgeons and suggest significant opportunities for improvement from a system perspective. It is noteworthy that there was no clear relationship between LOS and readmission rates across the countries. This suggests that other factors, such as post-discharge care arrangements or patient characteristics, may be more prominent in determining readmission rates. Our finding that certain countries commonly discharged patients to post-acute care while others discharged patients home is also important; in Israel, 59% of patients were discharged home compared to 10% in the US and 19% in Canada. These differences likely reflect each country’s availability of and funding for post-acute care and the expectations of patients and their families. In Israel, the high proportion of patients discharged home contributes to Israel’s achieving good health outcomes while simultaneously spending only 7.5% of gross domestic product (GDP) on healthcare. In contrast, patients in the US were rarely discharged home, which is consistent with a country that spends nearly 20% of its GDP on healthcare.40 Notably, decreases in the use of post-acute care under CMS’s Comprehensive Joint Replacement and Accountable Care Organization bundled payment programs suggest that misaligned incentives for hospitals contribute to high rates of use in the US.41,42
Finally, there is convincing evidence that timely surgical repair is associated with improved patient outcomes,5,43–50 and timely surgery is increasingly incentivized and monitored by payers and government regulators.44,51,52 Our finding that the time from hospital presentation to surgery in 2018 ranged between 0.5 days in Israel to 1.6 and 1.5 days in Canada and England, respectively, is noteworthy and suggests significant opportunities for improvement. In 2004 Israel introduced a payment model that rewarded hospitals for surgical repair completed within 48-hours, but penalized hospitals with unjustified delays.52 Interestingly, while both Canada and England have recommendations and guidelines advocating early repair,53,54 the financial incentives in both countries are less tangible and direct, which may explain the differences that we observed.
Our study has several limitations that should be acknowledged. First, our data are based on health administrative records; we lacked detailed clinical information on fracture subtype (i.e., cervical vs. intertrochanteric) as well as patient complexity and acuity that could influence treatment decisions. However, our large population-representative cohorts and detailed inclusion and exclusion criteria make it unlikely that widespread between-country differences in fracture subtype or patient complexity could explain our findings; moreover, we standardized for age and sex, thus adding further strength to our results. Second, although we use population-representative patient-level administrative data, we lacked data from 2011 and 2012 in the Netherlands and data about time-to-surgery and discharge disposition in England and Taiwan. Finally, we limited our study to hip fracture patients aged 66 years or older due to data availability in the US. However, most hip fractures occur in this age group.1 Thus, the findings may not be generalizable to younger patients or those covered by private insurance or Medicare-managed care in the US.
Conclusion
We discovered substantial between-country variation in mortality, in addition to similarly large differences in surgical approaches and health system performance measures. The study findings emphasize the need for further research that can provide objective evidence for the superiority of specific surgeries based on patient clinical conditions.
Supplementary Material
KEY POINTS.
There is substantial variation in mortality, surgical approaches, and health system performance for hip fracture care across six high-income countries.
The most common surgery performed was internal fixation, followed by hemiarthroplasty and total hip arthroplasty, but the rate of these and non-operative treatments varied substantially across countries.
The variation in surgical treatment highlights the need for additional research to determine the most effective surgical procedures based on individual patient and fracture characteristics.
Why does this matter?
The findings of this study have important implications for policymakers, healthcare providers, and researchers. By identifying the differences in hip fracture care across countries, this study provides insights into opportunities for improvement and shared learning. Additionally, the study highlights the need to identify optimal treatment strategies for hip fractures and investigate the factors contributing to higher mortality rates in certain countries. As the global population continues to age, hip fractures are expected to become more common, making it imperative to improve care and outcomes for this patient population.
ACKNOWLEDGMENTS
This work is supported by a grant from the US National Institute of Aging (R01AG058878) to (Landon/Cram PIs). Dr. Lix receives salary support from a Tier 1 Canada Research Chair. This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). Dr. Ko is supported by the Jack Tu Chair in Cardiovascular Outcomes, Sunnybrook Hospital, and the University of Toronto. ICES is an independent, non-profit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement. Ontario datasets were linked using unique encoded identifiers and analyzed at ICES. This work used data adapted from the Statistics Canada Postal Code Conversion File, which is based on data licensed from Canada Post Corporation, and/or data adapted from the MOH Postal Code Conversion File, which contains data copied under license from ©Canada Post Corporation and Statistics Canada. Parts of this material are based on data and/or information compiled and provided by the MOH and CIHI. The authors acknowledge the Manitoba Centre for Health Policy for using data in the Manitoba Population Research Data Repository under project #2019–056 (HIPC#2019/2020–38). Data used in this study are from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba, and were derived from data provided by Manitoba Health. The results for the Netherlands are based on calculations by Erasmus University using non-public microdata available from Statistics Netherlands. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Sponsor’s Role
The funders had no role in study design, data collection and analysis, the decision to publish, or the preparation of the manuscript.
Footnotes
Declaration of Conflict of Interest
We declare no competing interests.
Ethics Committee Approval
Approvals from each country can be found in the supplementary appendix.
Data Sharing
Data are largely unavailable because of the privacy regulations of participating jurisdictions.
REFERENCES:
- 1.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A Incidence and Economic Burden of Osteoporosis-Related Fractures in the United States, 2005–2025. Journal of Bone and Mineral Research. 2007;22(3):465–475. doi: 10.1359/JBMR.061113 [DOI] [PubMed] [Google Scholar]
- 2.Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop. 2011;45(1):15. doi: 10.4103/0019-5413.73656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Royal College of Physicians. National Hip Fracture Database Annual Report 2019.; 2019.
- 4.Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: Trends and geographical variations over the last 40 years. Injury. 2008;39(10):1157–1163. doi: 10.1016/j.injury.2008.03.022 [DOI] [PubMed] [Google Scholar]
- 5.Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ : Canadian Medical Association Journal. 2010;182(15):1609. doi: 10.1503/CMAJ.092220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oseph J, Uckerman DZ. Hip Fracture. https://doi.org/101056/NEJM199606063342307. 1996;334(23):1519–1525. doi: 10.1056/NEJM199606063342307 [DOI] [PubMed] [Google Scholar]
- 7.Loggers SAI, van Lieshout EMM, Joosse P, Verhofstad MHJ, Willems HC. Prognosis of nonoperative treatment in elderly patients with a hip fracture: A systematic review and meta-analysis. Injury. 2020;51(11):2407–2413. doi: 10.1016/J.INJURY.2020.08.027 [DOI] [PubMed] [Google Scholar]
- 8.Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM. Survival and Functional Outcomes After Hip Fracture Among Nursing Home Residents. JAMA Intern Med. 2014;174(8):1273–1280. doi: 10.1001/JAMAINTERNMED.2014.2362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berry SD, Rothbaum RR, Kiel DP, Lee Y, Mitchell SL. Association of Clinical Outcomes With Surgical Repair of Hip Fracture vs Nonsurgical Management in Nursing Home Residents With Advanced Dementia. JAMA Intern Med. 2018;178(6):774–780. doi: 10.1001/JAMAINTERNMED.2018.0743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cram P, Yan L, Bohm E, et al. Trends in Operative and Nonoperative Hip Fracture Management 1990–2014: A Longitudinal Analysis of Manitoba Administrative Data. J Am Geriatr Soc. 2017;65(1):27–34. doi: 10.1111/JGS.14538 [DOI] [PubMed] [Google Scholar]
- 11.Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. New England Journal of Medicine. 2017;377(21):2053–2062. doi: 10.1056/nejmcp1611090 [DOI] [PubMed] [Google Scholar]
- 12.Total Hip Arthroplasty or Hemiarthroplasty for Hip Fracture. New England Journal of Medicine. 2019;381(23):2199–2208. doi: 10.1056/NEJMOA1906190/SUPPL_FILE/NEJMOA1906190_DATA-SHARING.PDF [DOI] [PubMed] [Google Scholar]
- 13.Wang F, Zhang H, Zhang Z, Ma C, Feng X. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis. BMC Musculoskelet Disord. 2015;16(1). doi: 10.1186/S12891-015-0696-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nauth A, Creek AT, Zellar A, et al. Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. The Lancet. 2017;389(10078):1519–1527. doi: 10.1016/S0140-6736(17)30066-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beaupre LA, Wai EK, Hoover DR, et al. A comparison of outcomes between Canada and the United States in patients recovering from hip fracture repair: secondary analysis of the FOCUS trial. International Journal for Quality in Health Care. 2018;30(2):97–103. doi: 10.1093/INTQHC/MZX199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blankart CR, van Gool K, Papanicolas I, et al. International comparison of spending and utilization at the end of life for hip fracture patients. Health Serv Res. 2021;56(Suppl 3):1370. doi: 10.1111/1475-6773.13734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cram P, Lix LM, Bohm E, et al. Hip fracture care in Manitoba, Canada and New York State, United States: an analysis of administrative data. CMAJ Open. 2019;7(1):E55. doi: 10.9778/CMAJO.20180126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh ME, Sorensen J, Blake C, Johnsen SP, Kristensen PK. Geographic variation in hip fracture surgery rate, care quality and outcomes: a comparison between national registries in Ireland and Denmark. Arch Osteoporos. 2022;17(1):1–12. doi: 10.1007/S11657-022-01169-8/FIGURES/3 [DOI] [PubMed] [Google Scholar]
- 19.Kim H, Cheng SH, Yamana H, et al. Variations in hip fracture inpatient care in Japan, Korea, and Taiwan: an analysis of health administrative data. BMC Health Serv Res. 2021;21(1):1–11. doi: 10.1186/S12913-021-06621-Y/TABLES/4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Werner M, Macke C, Gogol M, Krettek C, Liodakis E. Differences in hip fracture care in Europe: a systematic review of recent annual reports of hip fracture registries. European Journal of Trauma and Emergency Surgery. 2022;48(3):1625–1638. doi: 10.1007/S00068-021-01797-8/TABLES/5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papanicolas I, Figueroa JF, Schoenfeld AJ, et al. Differences in health care spending and utilization among older frail adults in high-income countries: ICCONIC hip fracture persona. Health Serv Res. 2021;56(S3):1335–1346. doi: 10.1111/1475-6773.13739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorenzoni L, Marino A, Or Z, et al. Why the US spends more treating high-need high-cost patients: a comparative study of pricing and utilization of care in six high-income countries. Health Policy (New York). 2023;128:55–61. doi: 10.1016/J.HEALTHPOL.2022.12.004 [DOI] [PubMed] [Google Scholar]
- 23.Cram P, Hatfield LA, Bakx P, et al. Variation in revascularisation use and outcomes of patients in hospital with acute myocardial infarction across six high income countries: cross sectional cohort study. BMJ. 2022;377. doi: 10.1136/BMJ-2021-069164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Landon BE, Hatfield LA, Bakx P, et al. Differences in Treatment Patterns and Outcomes of Acute Myocardial Infarction for Low- and High-Income Patients in 6 Countries. JAMA. 2023;329(13):1088–1097. doi: 10.1001/JAMA.2023.1699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhu Y, Xing X, Liu S, Chen W, Zhang X, Zhang Y. Epidemiology of low-energy wrist, hip, and spine fractures in Chinese populations 50 years or older: A national population-based survey. Medicine. 2020;99(5):e18531. doi: 10.1097/MD.0000000000018531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.MLR.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 27.Curtin LR, Klein RJ. Direct standardization (age-adjusted death rates). Healthy People 2000 Stat Notes. 1995;(6):1–10. [PubMed] [Google Scholar]
- 28.Cram P, Girotra S, Matelski J, et al. Utilization of Advanced Cardiovascular Therapies in the United States and Canada: An Observational Study of New York and Ontario Administrative Data. Circ Cardiovasc Qual Outcomes. 2020;13(1). doi: 10.1161/CIRCOUTCOMES.119.006037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cram P, Landon BE, Matelski J, et al. Utilization and Outcomes for Spine Surgery in the United States and Canada. Spine (Phila Pa 1976). 2019;44(19):1371–1380. doi: 10.1097/BRS.0000000000003083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vesterager JD, Madsen M, Hjelholt TJ, Kristensen PK, Pedersen AB. Prediction Ability of Charlson, Elixhauser, and Rx-Risk Comorbidity Indices for Mortality in Patients with Hip Fracture. A Danish Population-Based Cohort Study from 2014 – 2018. Clin Epidemiol. 2022;14:275. doi: 10.2147/CLEP.S346745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aguinis H, Vassar M, Wayant C. On reporting and interpreting statistical significance and p values in medical research. BMJ Evid Based Med. 2021;26(2):39–42. doi: 10.1136/BMJEBM-2019-111264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Papanicolas I, Riley K, Abiona O, et al. Differences in health outcomes for high-need high-cost patients across high-income countries. Health Serv Res. 2021;56 Suppl 3(Suppl 3):1347–1357. doi: 10.1111/1475-6773.13735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–413. doi: 10.1007/PL00004148 [DOI] [PubMed] [Google Scholar]
- 34.Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: A meta-analysis of 14 randomized studies with 2,289 patients. New Pub: Medical Journals Sweden. 2009;77(3):359–367. doi: 10.1080/17453670610046262 [DOI] [PubMed] [Google Scholar]
- 35.Management of Hip Fractures in Older Adults Evidence-Based Clinical Practice Guideline.; 2021. https://www.aaos.org/hipfxcpg [DOI] [PubMed]
- 36.Metcalfe D, Zogg CK, Judge A, et al. Pay for performance and hip fracture outcomes: An interrupted time series and difference-in-differences analysis in England and Scotland. Bone and Joint Journal. 2019;101 B(8):1015–1023. doi: 10.1302/0301-620X.101B8.BJJ-2019-0173.R1/LETTERTOEDITOR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weil YA, Bernstein BP, Maqungo S, Khoury A, Liebergall M, Laubscher M. Hip fracture care and national systems in Israel and South Africa. OTA Int. 2020;3(1):e065. doi: 10.1097/OI9.0000000000000065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Budgets and Tariffs, Ministry of Health. Accessed January 31, 2023. https://www.health.gov.il/English/Topics/finance/Pages/default.aspx
- 39.Quinlan ND, Hogarth DA, Chen DQ, Werner BC, Browne JA. Hospital and Surgeon Reimbursement Trends for Femoral Neck Fractures Treated With Hip Hemiarthroplasty and Total Hip Arthroplasty. J Arthroplasty. 2020;35(11):3067–3075. doi: 10.1016/J.ARTH.2020.05.059 [DOI] [PubMed] [Google Scholar]
- 40.Current health expenditure (% of GDP) | Data. Accessed March 29, 2023. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS
- 41.Finkelstein A, Ji Y, Mahoney N, Skinner J. Mandatory Medicare Bundled Payment Program for Lower Extremity Joint Replacement and Discharge to Institutional Postacute Care: Interim Analysis of the First Year of a 5-Year Randomized Trial. JAMA. 2018;320(9):892–900. doi: 10.1001/JAMA.2018.12346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barnett ML, Wilcock A, McWilliams JM, et al. Two-Year Evaluation of Mandatory Bundled Payments for Joint Replacement. New England Journal of Medicine. 2019;380(3):252–262. doi: 10.1056/NEJMSA1809010/SUPPL_FILE/NEJMSA1809010_DATA-SHARING.PDF [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pincus D, Ravi B, Wasserstein D, et al. Association Between Wait Time and 30-Day Mortality in Adults Undergoing Hip Fracture Surgery. JAMA. 2017;318(20):1994–2003. doi: 10.1001/JAMA.2017.17606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bohm E, Loucks MsL, Wittmeier MsK, Lix LM, Oppenheimer L Reduced time to surgery improves mortality and length of stay following hip fracture: results from an intervention study in a Canadian health authority. Can J Surg. 2015;58(4):257–263. doi: 10.1503/CJS.017714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Colais P, di Martino M, Fusco D, Perucci CA, Davoli M. The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatr. 2015;15(1):1–8. doi: 10.1186/S12877-015-0140-Y/FIGURES/4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: Is delay before surgery important? Journal of Bone and Joint Surgery. 2005;87(3):483–489. doi: 10.2106/JBJS.D.01796 [DOI] [PubMed] [Google Scholar]
- 47.Klestil T, Röder C, Stotter C, et al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Scientific Reports 2018 8:1. 2018;8(1):1–15. doi: 10.1038/s41598-018-32098-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang CB, Lin CFJ, Liang WM, et al. Excess mortality after hip fracture among the elderly in Taiwan: A nationwide population-based cohort study. Bone. 2013;56(1):147–153. doi: 10.1016/J.BONE.2013.05.015 [DOI] [PubMed] [Google Scholar]
- 49.Novack V, Jotkowitz A, Etzion O, Porath A. Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int J Qual Health Care. 2007;19(3):170–176. doi: 10.1093/INTQHC/MZM003 [DOI] [PubMed] [Google Scholar]
- 50.Borges FK, Bhandari M, Guerra-Farfan E, et al. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. The Lancet. 2020;395(10225):698–708. doi: 10.1016/S0140-6736(20)30058-1 [DOI] [PubMed] [Google Scholar]
- 51.Tewari P, Sweeney BF, Lemos JL, et al. Evaluation of Systemwide Improvement Programs to Optimize Time to Surgery for Patients With Hip Fractures: A Systematic Review. JAMA Netw Open. 2022;5(9). doi: 10.1001/JAMANETWORKOPEN.2022.31911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Peleg K, Rozenfeld M, Radomislensky I, Novikov I, Freedman LS, Israeli A. Policy encouraging earlier hip fracture surgery can decrease the long-term mortality of elderly patients. Injury. 2014;45(7):1085–1090. doi: 10.1016/j.injury.2014.03.009 [DOI] [PubMed] [Google Scholar]
- 53.Denis A, Montreuil J, Reindl R, Berry GK, Harvey EJ, Bernstein M. Time-to-Incision for Hip Fractures in a Canadian Level-1 Trauma Centre: Are We Respecting the Guidelines? Canadian Geriatrics Journal. 2022;25(1):57. doi: 10.5770/CGJ.25.529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Neuburger J, Currie C, Wakeman R, et al. The Impact of a National Clinician-led Audit Initiative on Care and Mortality after Hip Fracture in England: An External Evaluation using Time Trends in Non-audit Data. Med Care. 2015;53(8):686. doi: 10.1097/MLR.0000000000000383 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are largely unavailable because of the privacy regulations of participating jurisdictions.


