ABSTRACT
From July to September 2023, China reported over 1, 400 confirmed cases of mpox transmitted mainly through sexual contact between males. Meanwhile, the percentage of men who have sex with men at universities in southwestern China is increasing every year, which is likely to lead to a potential spread of mpox on campuses. Vaccination is an effective preventive measure against infectious diseases, this study examined the willingness of university students in Southwest China to receive the mpox vaccine and analyzed the factors influencing their decision. A cross-sectional survey was conducted among 7311 university students from 10 universities in Southwest China between August 13 and September 1, 2023. The survey revealed a hesitancy rate of 56.13% toward the mpox vaccine, with the most common reason being concerns about vaccine safety (1407/4104, 34.29%). Univariate analysis identified 13 variables that significantly differed between the vaccine acceptance and vaccine hesitancy groups. Multivariate logistic regression analyses indicated protective factors for vaccine hesitancy, such as sexually transmitted diseases, previous knowledge about mpox, frequent information about mpox, people can get reinfection of mpox, and worries about mpox endemic in China. Additionally, the confidence and convenience dimensions in the 3Cs model were identified as risk factors for mpox vaccine hesitancy. This study found a high rate of vaccine hesitancy among university students in Southwest China regarding the mpox vaccine. Collaboration between university and healthcare departments is recommended to address mpox vaccine hesitancy among college students, thereby promoting their willingness to receive the mpox vaccine.
KEYWORDS: Mpox, mpox vaccine, university students, vaccine acceptance, vaccine hesitancy
Introduction
Mpox is a zoonotic disease caused by mpox virus (MPXV) which is a large double‐stranded DNA virus and belongs to the Orthopoxvirus genus within the Poxviridae family.1,2 The clinical manifestations of mpox are similar to those of smallpox, including pyrexia, back pain, headache, rash, malaise, and fatigue.3 The complications of mpox may be even life-threatening, such as encephalitis, sepsis.4 MPXV can be transmitted through direct contact with infectious skin, mucosal lesions, and respiratory droplets, or indirect contact with contaminated objects and materials.4 Furthermore, many cases in the current outbreak have been attributed to sexual transmission, particularly among men who have sex with men (MSM).5,6
Before 2022, the spread of MPXV via secondary transmission outside Africa was less reported.7 After a mpox case in England was reported in May 2022, a total of 91,123 confirmed cases and 663 probable cases, including 157 deaths, from 115 countries have been reported to World Health Organization (WHO) as of 30 September 2023.8 What is different from previous waves is this epidemic of mpox involves intensive human-to-human transmission and once raised a global concern.9 Previous studies suggested that antigens derived from members of Orthopoxvirus genus exhibited cross-protective immunity, and the smallpox vaccine could offer 85% effectiveness against MPXV.10 Due to the eradication of smallpox virus and termination of smallpox vaccine vaccination in the 1980s, almost all population born after the 1980s have limited protection against MPXV.
Currently, two smallpox vaccines (ACAM2000 and JYNNEOS) have been approved by the U.S. Food and Drug Administration (FDA) for the emergent immunization of individuals at high risk of exposure and postexposure.11–14 Vaccination has been considered to be the most effective way to prevent and control infectious diseases. However, vaccine hesitancy is listed as one of the top 10 threats to global public health by the WHO and has become an obstacle in achieving herd immunity.15,16 The Strategic Advisory Group of Experts on Immunization (SAGE) Working Group defined vaccine hesitancy as the practice of refusing or delaying vaccination despite the availability of vaccination services.15
The southwestern region of China is among the areas with a higher number of confirmed cases of mpox,17 as well as being a high-risk area for MSM behaviors.18,19 Studies indicated that the prevalence of MSM behaviors in universities is increasing annually,20–22 which may raise concerns about the potential spread of the mpox in campuses. Given the potential risk associated with the spread of mpox, there is a need to conduct investigations about the impact factors of mpox health education and mpox vaccine hesitancy among university students. Conducting such investigations offers several benefits. Firstly, it educates university students on the risks and prevention of mpox, empowering them to take necessary precautions to safeguard themselves and minimize the transmission of mpox.23,24 Secondly, university students can share mpox-related information with their peers and families.25 Lastly, gaining insights into the factors contributing to vaccine hesitancy regarding mpox in advance can aid in the development of a precise and efficient vaccination program to curb the spread of the disease.26 Therefore, this study aims to investigate the willingness of university students in Southwest China to receive the mpox vaccine and its influencing factors, with the intention to provide a scientific basis for mpox prevention.
Material and methods
Study design and participants
An online cross-sectional survey was conducted from August 13, 2023 to September 1, 2023. The “Wenjuanxing” online website was used to administer anonymous self-report questionnaires from university students in Southwest China. The eligibility criteria for participants were as follows: (1) University students in Southwest China include junior college, undergraduate, and postgraduate degrees, (2) Being able to fill in the questionnaire, volunteering to participate in this study and giving informed consent. Simultaneously, participants who (1) completed the questionnaire within 2 min, (2) provided wrong answers to the quality control question, (3) gave logically contradictory answers, and (4) possessed cognitive impairment were excluded upon final screening.
Sample size estimation
The sample size was determined by referring to a previous cross-sectional study conducted in Chinese MSM population regarding mpox vaccine hesitancy.27 The employed sample calculation formula was based on the equation n = Z21−α/2 p (1 − p)/e2, where n represents the minimum required number of participants, p represents the vaccine hesitancy rate, and e represents the required accuracy. This study accounted for an estimated non-response rate of 10%. As a result, the study necessitated a minimum sample size of 315 participants (Z2 = (1.96)2 relative to the 95% confidence interval (CI); p = 13.85%; e = 4%).
Measure
The SAGE Working Group on Vaccine Hesitancy proposed 3Cs model of vaccine hesitancy, in which the influence factors of vaccine hesitancy were classified into three categories: confidence, complacency and convenience.15 After a comprehensive literature review, a questionnaire was compiled based on the 3Cs model of vaccine hesitancy and Mei Li’s findings on students’ COVID-19 vaccine hesitation during the COVID-19 pandemic, getting the authorization from the original authors.28 The questionnaire was divided into three parts. (1) Demographic characteristics of the participants, including age, gender, residence, educational level, medicine specialty or not, sexual orientation, and history of sexually transmitted diseases (STDs). (2) Participants’ level of awareness of mpox and mpox vaccine. (3) Vaccine hesitancy scale with three dimensions: confidence, complacency, and convenience. These three sections are measured on a 5-point Likert scale, with “Agree to Strongly Agree” scoring 1 point and “Strongly Disagree to Unsure” scoring 0 point. Sixty percentage of the total number of entries scored to set a passing grade for the evaluation.
A pre-survey among 217 medical students was conducted, and 217 valid questionnaires were collected. The students were at the age of 23.05 ± 2.27 and 70% were females. The online platform shows that the completion time of a questionnaire is 3 to 5 minutes, within the acceptable time range of the research subjects. Study subjects reported that the questionnaire items were easy to understand and the online self-administered method was acceptable. Based on the pre-survey data, the reliability and validity of the questionnaire were analyzed. Its internal consistency was assessed by calculating the Cronbach’s alpha as 0.970. The definition of vaccine hesitancy and related research was as follow, participants who are undecided and unwilling to be vaccinated were defined as “Vaccine Hesitancy.” Participants who have been vaccinated and would like to get vaccinated were classified as “Vaccine acceptance.”
Ethics statement
Based on the principle of anonymity and informed consent of the participants, data was collected. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The participants would see the purpose of the study and their personal rights clearly in the first page of the questionnaire. The formal questionnaire would only be administered after reading and signing the electronic consent. Electronic informed consent was obtained from each respondent. This study was approved by the Southwest Medical University (Ethics Approval ID: No. SWMUIRBKS-202312–0011).
Statistical analysis
Data were analyzed using IBM SPSS software version 26.0. The relationship between the independent variables (participants’ demographic characteristics, knowledge of mpox information, and results of the 3Cs model dimensions) and the dependent variable (participants’ willingness to receive the vaccines) were analyzed using univariate analysis. The independent variables with p < .05 were searched for multivariate logistic regression analysis to determine the factors affecting the vaccination willingness of participants. The test level was α = 0.05.
Results
Demographic characteristics of participants and their willingness to receive vaccines
This study included 7530 participants from university students in the southwest of China, among which 219 participants did not fill in or return incomplete questionnaires. Thus, 7311 participants completed the survey, with an overall response rate of 97.09%. According to the definition of vaccine hesitancy and the results of the investigation, the acceptance group represented 43.87% of students (3207 out of 7311), and the hesitant group was 56.13% (4104 out of 7311).
χ2 test was applied to assess the difference in the distribution of vaccination hesitancy among characteristics including age, gender, residence, educational level, medicine specialty, sexual orientation, and history of sexually transmitted diseases (STDs). Results showed that medicine specialty (χ2 = 8.67, p = .003), sexual orientation (χ2 = 20.06, p < .001), and history of sexually transmitted diseases (STDs) (χ2 = 64.89, p < .001) were statistically significant between the vaccine hesitancy and vaccine acceptance groups. Rates of vaccine hesitancy (43.97% vs. 43.76%) and vaccine acceptance (56.03% vs. 56.24%) are almost the same in male and female. Even for medical students, the number of vaccine hesitancy and vaccine acceptance are almost same (255/256, 50% vs. 50%) (Table 1).
Table 1.
Demographic characteristics of participants.
| Intention to receive mpox vaccine |
||||
|---|---|---|---|---|
| Item | All participants (N = 7311) | Mpox vaccine acceptance NO. (%) |
Mpox vaccine hesitancy NO. (%) |
P Value |
| Gender | .861 | |||
| Male | 3712 | 1632 (44%) | 2080 (56%) | |
| Female | 3599 | 1575 (43.8%) | 2024 (56.2%) | |
| Age (year) | .537 | |||
| 16–22 | 3266 | 1435 (43.9%) | 1831 (56.1%) | |
| 23–26 | 3421 | 1486 (43.4%) | 1935 (56.6%) | |
| >26 | 624 | 286 (45.8%) | 338 (55.2%) | |
| Residence | .353 | |||
| Rural | 2365 | 1019 (43.1%) | 1346 (56.9%) | |
| Urban | 4946 | 2188 (44.2%) | 2758 (55.8%) | |
| Education level | .275 | |||
| College degree | 2931 | 1253 (42.7%) | 1678 (57.3%) | |
| Bachelor’s degree | 2912 | 1294 (44.4%) | 1618 (55.6%) | |
| ≥ Master’s degree | 1468 | 660 (45%) | 808 (55%) | |
| Medicine specialty | .003 | |||
| Yes | 511 | 256 (50%) | 255 (50%) | |
| No | 6800 | 2951 (43.4%) | 3849 (56.6%) | |
| Sexual orientation | <.001 | |||
| Heterosexual | 7216 | 3153 (43.7%) | 4063 (56.3%) | |
| Double sexuality | 3 | 3 (100%) | 0 (0%) | |
| Homosexual | 80 | 39 (48.8%) | 41 (51.2%) | |
| unclear | 12 | 12 (100%) | 0 (0%) | |
| History of STDs | <.001 | |||
| Yes | 837 | 423 (50.5%) | 414 (49.5%) | |
| No | 4905 | 1991 (40.6%) | 2914 (59.4%) | |
| Undetected and unclear | 1569 | 793 (50.5%) | 776 (49.5%) | |
Abbreviations: STD, sexually transmitted disease.
Sources of mpox vaccine‐related information
As shown in Figure 1, 61.82% of participants acquired information about the mpox vaccine from traditional sources such as TV programs, newspapers, and radio broadcasts, 54.94% of participants obtained information from friends and family members, 45.18% of participants obtained information from internet, 38.65% of participants obtained information from social organizations such as universities and communities, and 8%(628/7311)of participants did not receive any vaccine‐related information.
Figure 1.
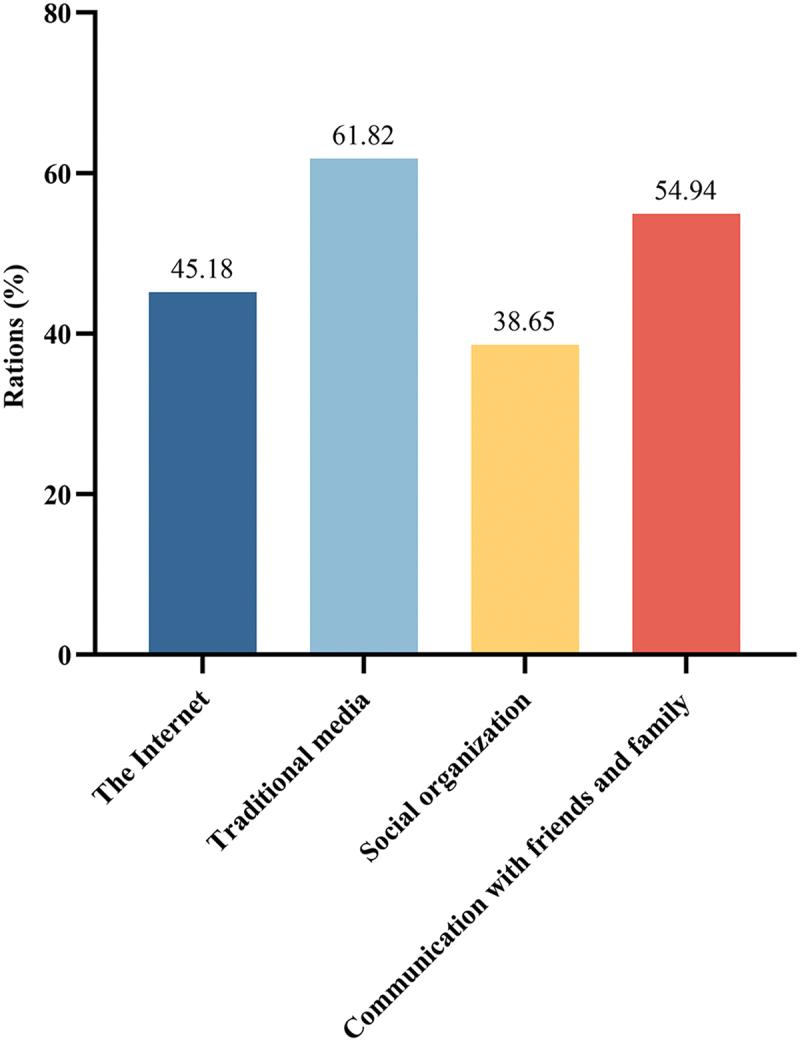
Percentage of information sources related to mpox by different routes. The X axis presents the different information sources that participants have regarding mpox. The Y axis presents the percentage of participants who have knowledge of mpox from different information sources. Everyone participants could choose one to four information sources.
Participants’ perceptions for the mpox vaccine and the results of the 3Cs model dimensions
Among the 7311 participants, more than 90%(6683/7311)participants have known about mpox previously, and only 628 did not hear about mpox. In terms of frequency of information following about mpox, the “Sometimes” and “Seldom or never” groups had a similar number of responses (2819 and 2780, respectively), while the “Often” group had a much lower rate of vaccine hesitation than the vaccine acceptance rate (18.93% VS 81.07%). A total of 3263 students believed that people could get reinfected with MPXV, and the vaccine hesitancy rate was 18.05%. With regard to comprehending mpox and HIV, 4861 (66.49%) participants perceived that HIV-infected individuals accounted for a larger portion of mpox cases. Additionally, 4056 (55.48%) participants believed that HIV‐infected and HIV‐uninfected mpox cases show similar symptoms. The survey findings revealed that a majority of participants (4038/7311, 55.23%) expressed concerns about the increasing prevalence of mpox in China. These participants exhibited a significantly higher rate of vaccine acceptance compared to those who did not express any concerns (82.76% vs. 23.28%). In addition, only the issues of “the HIV‐infected individuals account for a larger proportion of Mpox cases” and “the smallpox vaccine can provide cross‐protection against Mpox” were not correlated with the participants’ willingness to receive mpox vaccination. Other questions were significantly different between the vaccine hesitation group and the vaccine acceptance group (p < .05).
The analysis of the three dimensions of the 3Cs model showed that 5171 (70.73%) participants had confidence in vaccines, 409 (5.6%) participants showed complacency, and 6736 (92.14%) participants considered vaccination to be convenient. Simultaneously, all three dimensions were significantly different (p < .001) between the vaccine hesitant and vaccine acceptance groups (Table 2).
Table 2.
Participants’ perceptions of mpox and results from the 3Cs model.
| Intention to receive mpox vaccine |
||||
|---|---|---|---|---|
| Item | All participants (N = 7311) |
Mpox vaccine acceptance NO. (%) |
Mpox vaccine hesitancy NO. (%) |
P Value |
| Knew about mpox before | <.001 | |||
| Yes | 6683 | 2862 (42.8%) | 3821 (57.2%) | |
| No | 628 | 345 (54.9%) | 283 (45.1%) | |
| Frequency of information following about mpox | <.001 | |||
| Often | 1712 | 324 (18.9%) | 1388 (81.1%) | |
| Sometime | 2819 | 1440 (51.1%) | 1379 (48.9%) | |
| Seldom or never | 2780 | 1443 (51.9%) | 1337 (48.1%) | |
| People can get reinfected | <.001 | |||
| Yes | 3263 | 589 (18.1%) | 2674 (81.9%) | |
| No | 1984 | 1371 (69.1%) | 613 (30.9%) | |
| unclear | 2064 | 1247 (60.4%) | 817 (39.6%) | |
| HIV‐infected individuals account for a larger proportion of mpox cases | .963 | |||
| Yes | 4861 | 2137 (44%) | 2724 (56%) | |
| No | 1086 | 476 (43.9%) | 610 (56.1%) | |
| unclear | 1364 | 594 (43.5%) | 770 (56.5%) | |
| HIV‐infected and HIV‐uninfected mpox cases show similar symptoms | <.001 | |||
| Yes | 4056 | 1298 (32%) | 2758 (68%) | |
| No | 938 | 442 (47.1%) | 496 (52.9%) | |
| unclear | 2317 | 1467 (63.3%) | 850 (36.7%) | |
| Mpox can be detected in semen | .006 | |||
| Yes | 5192 | 2218 (42.7%) | 2974 (57.3%) | |
| No | 1078 | 512 (47.5%) | 566 (52.5%) | |
| unclear | 1041 | 477 (45.8%) | 564 (54.2%) | |
| Have worries about mpox endemic in China | <.001 | |||
| Yes | 4038 | 696 (17.2%) | 3342 (82.8%) | |
| No | 3273 | 2511 (76.7%) | 762 (23.3%) | |
| Smallpox vaccine can provide cross‐protection against mpox | .496 | |||
| Yes | 5070 | 2201 (43.4%) | 2869 (56.6%) | |
| No | 828 | 370 (44.7%) | 458 (55.3%) | |
| unclear | 1413 | 636 (45%) | 777 (55%) | |
| Smallpox vaccine with high protection | <.001 | |||
| Yes | 3410 | 915 (26.8%) | 2495 (73.2%) | |
| No | 783 | 368 (47%) | 415 (53%) | |
| unclear | 3118 | 1924 (61.7%) | 1194 (38.3%) | |
| 3Cs model | ||||
| Confidence | <.001 | |||
| Yes | 5171 | 2108 (40.8%) | 3063 (59.2%) | |
| No | 2140 | 1099 (51.4%) | 1041 (48.6%) | |
| Complacency | <.001 | |||
| Yes | 409 | 324 (79.2%) | 85 (20.8%) | |
| No | 6902 | 2883 (41.8%) | 4019 (58.2%) | |
| Convenience | <.001 | |||
| Yes | 6736 | 2743 (40.7%) | 3993 (59.3%) | |
| No | 575 | 464 (80.7%) | 111 (19.3%) | |
Reasons for vaccine acceptance and vaccine hesitancy
The study also assessed the reasons behind the willingness or unwillingness of the 7,311 participants to be vaccinated. According to the data, the primary reason for participants’ willingness to be vaccinated against mpox was the perceived outweighing of vaccination’s advantages over disadvantages (1181/3207,36.83%). The second and third reasons, namely the belief in the safety of the vaccine (694/3207, 21.63%) and considering the vaccine as the most effective means to combat MPXV (682/3207, 21.28%), had similar percentages. The least common response among participants was the perception that vaccination is a social responsibility (211/3207, 6.57%). In addition, participants expressed various reasons for their reluctance to be vaccinated, including doubts about the safety of the vaccine (34.29%), insufficient information about the vaccine (28.68%), the vaccine not being free (25.8%), doubts about the efficacy of the vaccine (23.6%), a bad vaccination experiences (21.93%), and fear of unknown risks (21.85%) (Figure 2).
Figure 2.
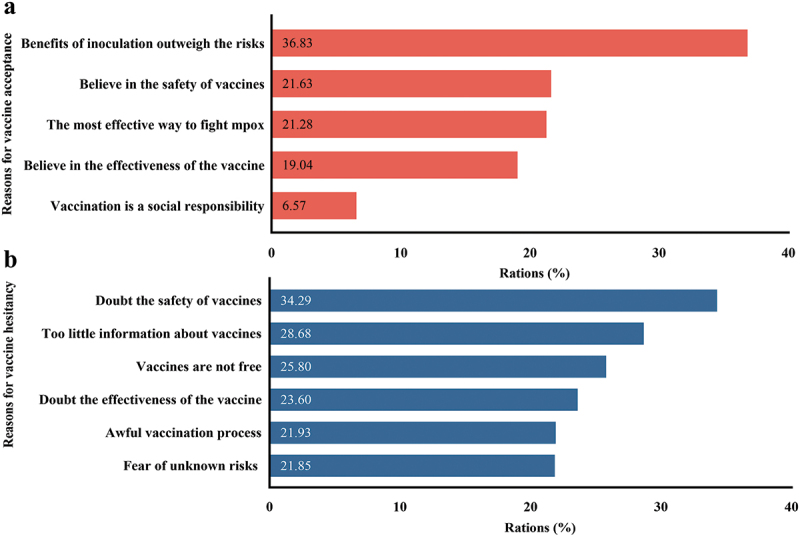
Reasons for vaccine acceptance (a) and vaccine hesitancy (b).
Logistic regression analysis of factors affecting vaccine hesitancy
To identify independent influences on vaccination hesitancy, 13 univariate variables with p < .05 were included in logistic regression model, along with willingness to vaccinate as the dependent variable (0 = vaccine acceptance, 1 = vaccine hesitancy). The results showed that all three dimensions of the 3Cs model (confidence, complacency, and convenience) were independent influences, and lack of confidence in vaccines and inconvenience of vaccination were risk factors for vaccine hesitancy. This indicated that participants with no confidence in vaccines were 1.924 times more likely to experience vaccine hesitancy than participants with vaccine confidence (OR = 1.924, 95%CI = 1.42–2.907, p < .001), and participants with inconvenient access to vaccines were 1.174 times more likely to experience vaccine hesitancy than those with convenient access to vaccines (OR = 1.174, 95%CI = 1.021–1.35, p < .001). In terms of mpox awareness, the results of the regression model revealed that all seven variables exhibited a significant association with vaccine hesitancy. Compared with participants who did not worry about mpox epidemic in China, participants who worried about epidemic of mpox in China were more likely to accept vaccination (OR = 0.133, 95% CI = 0.117–0.151, p < .001,). Moreover, knowledge about Mpox previously was a protective factor for mpox vaccination intentions (OR = 0.781, 95%CI = 0.62–0.983, p = .035, vs. didn’t know about Mpox before). As for the frequency of mpox information, the probability of vaccine hesitancy in the “often” and “sometimes” informed groups (OR = 0.483, 95%CI = 0.408–0.572, p < .001) would be lower than that in the “seldom or never” informed group (OR = 0.843, 95%CI = 0.733–0.969, p < .017) (Table 3).
Table 3.
Predictive factors related with mpox vaccine hesitancy in binary logistic analysis (N = 7311).
| Variables | Mpox vaccine acceptance NO. (%) |
Mpox vaccine hesitancy NO. (%) |
OR (95%CI) | P Value |
|---|---|---|---|---|
| History of STDs | ||||
| Yes | 423 (50.5%) | 414 (49.5%) | 1.035 (0.824–1.301) | .765 |
| No | 1991 (40.6%) | 2914 (59.4%) | 0.828 (0.711–0.966) | .016 |
| Undetected and unclear | 793 (50.5%) | 776 (49.5%) | Ref | |
| Knew about mpox previously | ||||
| Yes | 2862 (42.8%) | 3821 (57.2%) | 0.781 (0.62–0.983) | .035 |
| No | 345 (54.9%) | 283 (45.1%) | Ref | |
| Frequency of information following about mpox | ||||
| Often | 324 (18.9%) | 1388 (81.1%) | 0.483 (0.408–0.572) | <.001 |
| Sometime | 1440 (43.4%) | 1379 (43.4%) | 0.843 (0.733–0.969) | .017 |
| Seldom or never | 1443 (51.1%) | 1337 (48.1%) | Ref | |
| People can get reinfected | ||||
| Yes | 589 (18.1%) | 2674 (81.9%) | 0.319 (0.275–0.37) | <.001 |
| No | 1371 (69.1%) | 613 (30.9%) | 0.993 (0.841–1.171) | .93 |
| unclear | 1247 (60.4%) | 817 (39.6%) | Ref | |
| HIV‐infected and HIV‐uninfected mpox cases show similar symptoms | ||||
| Yes | 1298 (32%) | 2758 (68%) | 0.538 (0.465–0.622) | <.001 |
| No | 442 (47.1%) | 496 (52.9%) | 0.793 (0.646–0.975) | .028 |
| unclear | 1467 (63.6%) | 850 (36.7%) | Ref | |
| Have worries about mpox endemic in China | ||||
| Yes | 696 (17.2%) | 3342 (82.8%) | 0.133 (0.117–0.151) | <.001 |
| No | 2511 (76.7%) | 762 (23.3%) | Ref | |
| Smallpox vaccine with high protection | ||||
| Yes | 915 (26.8%) | 2495 (73.2%) | 0.498 (0.435–0.57) | <.001 |
| No | 368 (47%) | 415 (53%) | 0.769 (0.625–0.947) | .013 |
| unclear | 1924 (61.7%) | 1194 (38.3%) | Ref | |
| Confidence | ||||
| No | 1099 (51.4%) | 1041 (48.6%) | 1.174 (1.021–1.35) | .024 |
| Yes | 2108 (40.8%) | 3063 (59.2%) | Ref | |
| Complacency | ||||
| No | 2883 (41.8%) | 4019 (58.2%) | 0.536 (0.373–0.77) | .001 |
| Yes | 324 (79.2%) | 85 (20.8%) | Ref | |
| Convenience | ||||
| No | 464 (80.7%) | 111 (19.3%) | 1.924 (1.42–2.607) | <.001 |
| Yes | 2743 (40.7%) | 3993 (59.3%) | Ref | |
Abbreviations: STD, sexually transmitted disease; Ref, reference; OR, odds ratio.
Discussion
From June to September 2023, China reported 1,403 newly diagnosed cases of mpox, over 90% of which were identified as MSM population.29 This rapid increase in infections has drawn significant attention. Although observational studies have indicated that smallpox vaccination is highly effective in preventing mpox, with an efficacy rate as high as 85%, the global discontinuation of smallpox vaccination after 1981 has resulted in insufficient immunity against MPXV among individuals under the age of 40.30 Given the ongoing spread of the mpox epidemic in China, mpox vaccination represents the most effective measure to prevent a wider spread of mpox.31 However, the MSM population in Chinese universities exhibits the following characteristics: (1) covert transmission; (2) high sensitivity and privacy; (3) simultaneous inclusion in the high-risk population for HIV; (4) limited awareness regarding mpox and mpox vaccines.32–34 Despite these characteristics, no studies have been conducted in China to investigate the potential barriers to mpox vaccination among college populations. Therefore, this study serves as the first cross-sectional assessment of university students’ willingness and perceptions regarding mpox vaccination in southwestern China, employing the 3Cs model.
Participants in this study were from a variety of subject specialties, which were divided into medical and non-medical majors. Non-medical students exhibit higher levels of vaccine hesitancy, while medical students demonstrate greater ability to evaluate the significance of vaccinations for themselves and others, leveraging their health expertise to make informed vaccination choices.35 During the COVID-19 epidemic, the risk of vaccine hesitancy in females was significantly higher than that in males.36 However, cross-sectional surveys of vaccine hesitancy about mpox vaccine demonstrated that gender had no effects on vaccine hesitancy of Pakistan university students and Chinese healthcare workers,24,37 which is consistent with the findings of the present study. The disparity in gender influence on vaccine hesitancy between COVID-19 and mpox may be due to their differences in transmission mode. Transmission risk is an important potential factor that may influence public attitude toward a vaccine, and the transmission risk of mpox may be underestimated according to a recent study which compared the anti-orthopoxvirus neutralizing antibody levels in MSM population and general adult population.38 Although mpox can spread through multiple routes, sexual transmission still dominates according to reports of WHO and Chinese Center for Disease Control and Prevention.8,29 Furthermore, the participants of this study included all sexual orientation university students, and the data analysis was based on all included participants, which would not lead to a biased evaluation. China reported 501 new confirmed cases of mpox in August 2023. 92.5% of these cases were among MSM population.17 Our results also suggested that sexual orientation and STDs have significant effects on the willingness to accept mpox vaccine. Among the 7311 participants, 837 had AIDS and other diseases, and logistic regression analyses showed that students with sexually transmitted diseases were less likely to exhibit vaccine hesitancy, with only 0.828 times as likely as other students. For example, a multi-regional study conducted in Europe reported that only 8.8% of homosexuals exhibited vaccine hesitancy toward mpox.39 A recent study conducted in China specifically observed that MSM individuals infected with HIV displayed lower levels of vaccine hesitancy compared to their HIV-uninfected counterparts.27
Overall, 56% of the students in this study were reluctant to accept mpox vaccine, presenting high vaccine hesitancy rates compared with that of COVID-19 (41.2%) and influenza (44.7%).40,41 Previous studies indicated that the primary factor contributing to vaccine hesitancy among university students in relation to COVID-19, influenza, and Human Papillomavirus (HPV) is concerns about vaccine safety.42–44 This study got a similar result. Among Chinese university students, the leading cause of hesitancy toward receiving the mpox vaccine was concern regarding its safety, accounting for 34.29% of participants. Regression analysis conducted under the 3Cs model also supports this conclusion, showing that individuals who lack trust in the vaccine are 1.174 times more likely to experience vaccine hesitation compared to those who trust the vaccine. These findings underscore the significance of vaccine confidence. Interestingly, this study revealed that the awareness about vaccine efficacy was not associated with mpox vaccine hesitancy, which was consisted with previous studies on vaccine hesitancy among university students toward to COVID-19, influenza, and HPV vaccines.42–44 Furthermore, surveys which were conducted among MSM population and healthcare workers also demonstrated the lack of association between awareness of vaccine efficacy and mpox vaccine hesitancy.27,37 It was believed that the outstanding performance in COVID-19 vaccine development increased the confidence in vaccines of the people, which further extended to mpox vaccination.37 On the other hand, the low-level knowledge of mpox and low risk perception of mpox among the Chinese population may also weaken the relationship between awareness of vaccine efficacy and vaccine hesitancy.45,46 Therefore, universities and healthcare departments could provide essential information on mpox vaccines and safety knowledge to university students to instill confidence in the vaccines. Importantly, the dissemination process of mpox information gradually enhances the cognitive understanding among university students.
This study has confirmed that cognitive problems such as “People can get reinfected” and “Mpox can be detected in semen” are all influential factors in vaccine hesitancy. Logistic regression analysis further suggests that university students with higher levels of cognitive understanding have a lower probability of vaccine hesitancy. Classroom lectures and promotional activities could enhance the acceptance rate for vaccine among college students.47 A similar study reported the feasibility of a Brazilian awareness campaign aimed at encouraging healthcare workers to receive vaccine against influenza, which successfully increased the vaccination rate to 34.4%. However, due to the lack of continuous education and intervention, this rate dropped to 20.2% at the following year and to 12.75% two years later.48 Thus, comprehensive health education can raise awareness of mpox and improve mpox vaccination rates. Given that over 50% of the information sources regarding mpox are derived from friends and family, it should be results of university students’ lives revolving around their campus and family. Thus, their awareness of diseases and preventive immunization behaviors are strongly influenced by those close to them. Therefore, it is recommended to administer vaccinations to university students as a group in classrooms or community settings, as it can be more effective than individual vaccinations.49
Another important aspect in the model is the convenience of vaccination. Group vaccination offers advantages such as scheduled appointments and designated vaccination locations, which can reduce time constraints and enhance social acceptance, thereby decreasing vaccine hesitancy.50 University students who engage same-sex sexual behaviors are at high risk of MPXV infection. Therefore, healthcare sectors can optimize the vaccination process by ensuring privacy for the vaccinators, eliminating the negative impacts of vaccination, and making the vaccination more convenient.
This study has several limitations. Firstly, the cross-sectional design of the study does not allow for the identification of causal relationships between vaccination intentions and the collected variables. Secondly, the sample was drawn using convenience sampling, which inevitably introduces sampling errors. Thirdly, the findings are specific to university students in Southwest China and cannot be generalized to the entire country or other populations. Lastly, the questionnaire includes sensitive questions that may be susceptible to selection bias. Despite these limitations, this study is the first to assess the willingness and influencing factors of university students in Southwest China toward mpox vaccination. The study specifically selected a region with the highest number of MSM behaviors and the most extensive spread of mpox in China.17,51,52 The study also had a sufficient sample size and good representativeness, providing a scientific vaccination strategy for preventing the transmission of mpox.
Conclusion
The findings of this study indicate that university students in Southwest China exhibit low willingness to receive the mpox vaccine (43.87%). Employing the 3Cs model proposed by the World Health Organization, the study identified several factors significantly associated with vaccination intentions, including sexual orientation, history of sexually transmitted diseases (STDs), level of mpox awareness, vaccine confidence, complacency, and convenience. To address these findings, it is recommended to enhance college students’ understanding of mpox and preventive measures, as well as to promote scientific knowledge about the mpox vaccine on campus. By raising awareness among college students, particularly those who are identified as MSM individuals, hesitation toward the mpox vaccine can be reduced, thus contributing to the prevention of mpox transmission.
Funding Statement
This work was funded by the Bureau of Science Technology & Intellectual Property of Luzhou [No. 2023NYF094], the Postdoctoral Science Foundation of China [No. 2020T130044ZX], the Basic Scientific Research Fund of Southwest Medical University [No. 2018-ZRQN-095, 2019ZZD007, 0903-00040077].
Authors’ contributions
Xiu Yang: Methodology, data curation, formal analysis, investigation, writing-original draft, and writing-review & editing. Xuetao Yang: Conceptualization, methodology, formal analysis, investigation, writing-original draft, and writing-review & editing. Wenyi Jiang: Methodology, data curation, formal analysis, investigation, and writing-review & editing. Na Luo: Investigation and data curation. Yibo Hu: Investigation and formal analysis. Ya Yang: Conceptualization and writing-review & editing. Xidan Yang: Conceptualization and writing-original draft. Lingli Hou: Conceptualization and writing-original draft. Jingjing Zhang: Conceptualization and data curation. Congxia Hu: Conceptualization, methodology, validation, and writing-review & editing. Jihui Lin: Conceptualization, methodology, validation, supervision, project administration, and writing-review & editing. All authors reviewed the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Kugelman JR, Johnston SC, Mulembakani PM, Kisalu N, Lee MS, Koroleva G, McCarthy SE, Gestole MC, Wolfe ND, Fair JN, et al. Genomic variability of monkeypox virus among humans, Democratic Republic of the Congo. Emerg Infect Dis. 2014;20(2):232–9. doi: 10.3201/eid2002.130118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang X, Hu C, Yang X, Yang X, Hu X, Wang X, Liu C, Yuan Y, Du S, Wang PG, et al. Evaluation and comparison of immune responses induced by two mpox mRNA vaccine candidates in mice. J Med Virol. 2023;95(10):e29140. doi: 10.1002/jmv.29140. [DOI] [PubMed] [Google Scholar]
- 3.Kaler J, Hussain A, Flores G, Kheiri S, Desrosiers D.. Monkeypox: a comprehensive review of transmission, pathogenesis, and manifestation. Cureus. 2022;14:e26531. doi: 10.7759/cureus.26531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lum FM, Torres-Ruesta A, Tay MZ, Lin RTP, Lye DC, Rénia L, Ng LFP. Monkeypox: disease epidemiology, host immunity and clinical interventions. Nat Rev Immunol. 2022;22(10):597–613. doi: 10.1038/s41577-022-00775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rizk JG, Lippi G, Henry BM, Forthal DN, Rizk Y. Prevention and treatment of monkeypox. Drugs. 2022;82(9):957–63. doi: 10.1007/s40265-022-01742-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez-Morales AJ, Lopardo G. Monkeypox: another sexually transmitted infection? Pathogens (Basel, Switzerland). 2022;11(7):713. doi: 10.3390/pathogens11070713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thornhill JP, Barkati S, Walmsley S, Rockstroh J, Antinori A, Harrison LB, Palich R, Nori A, Reeves I, Habibi MS, et al. Monkeypox virus infection in humans across 16 Countries — April–June 2022. N Engl J Med. 2022;387(8):679–91. doi: 10.1056/NEJMoa2207323. [DOI] [PubMed] [Google Scholar]
- 8.WHO . 2022-23 Mpox (Monkeypox) outbreak: global trends; [Accessed 2023 Aug 29]. https://worldhealthorg.shinyapps.io/mpx_global/.
- 9.Kozlov M. Monkeypox outbreaks: 4 key questions researchers have. Nature. 2022;606(7913):238–9. doi: 10.1038/d41586-022-01493-6. [DOI] [PubMed] [Google Scholar]
- 10.Di Giulio DB, Eckburg PB. Human monkeypox: an emerging zoonosis. Lancet Infect Dis. 2004;4(1):15–25. doi: 10.1016/s1473-3099(03)00856-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petersen BW, Harms TJ, Reynolds MG, Harrison LH. Use of vaccinia virus smallpox vaccine in laboratory and health care personnel at risk for occupational exposure to orthopoxviruses — recommendations of the advisory committee on immunization practices (ACIP), 2015. Morb Mortal Wkly Rep. 2016;65(10):257–62. doi: 10.15585/mmwr.mm6510a2. [DOI] [PubMed] [Google Scholar]
- 12.Rao AK, Petersen BW, Whitehill F, Razeq JH, Isaacs SN, Merchlinsky MJ, Campos-Outcalt D, Morgan RL, Damon I, Sánchez PJ, et al. Use of JYNNEOS (smallpox and monkeypox vaccine, live, nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses: recommendations of the advisory committee on immunization practices — United States, 2022. Morb Mortal Wkly Rep. 2022;71(22):734–42. doi: 10.15585/mmwr.mm7122e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vivancos R, Anderson C, Blomquist P, Balasegaram S, Bell A, Bishop L, Brown CS, Chow Y, Edeghere O, Florence I, et al. Community transmission of monkeypox in the United Kingdom, April to May 2022. Eurosurveillance. 2022;27(22). doi: 10.2807/1560-7917.Es.2022.27.22.2200422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang X, Yang X, Du S, Hu C, Yang X, Wang X, Hu X, Rcheulishvili N, Wang PG, Lin J. A subunit vaccine candidate composed of mpox virus A29, LM1R, A35R, and B6R elicits robust immune response in mice. Vaccines. 2023;11(9):11. doi: 10.3390/vaccines11091420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 16.Organization WH . Ten threats to global health in 2019; 2019. https://www.who.int/vietnam/news/feature-stories/detail/ten-threats-to-global-health-in-2019.
- 17.Prevention CCfDCa . Monkeypox outbreak surveillance for August 2023; 2023. https://www.chinacdc.cn/jkzt/crb/zl/szkb_13037/gwjszl_13092/202309/t20230908_269405.html.
- 18.M L, X H, Chang W. A study on the spatial and temporal evolution of AIDS distribution in China and its influencing factors. Chinese J Health Stat. 2020;37:116–20. [Google Scholar]
- 19.Qian S, Guo W, Wang L. Spatial analysis of the aggregated AIDS epidemic in China based on geographic information systems. Chinese J Health Stat. 2014;31:1064–7. [Google Scholar]
- 20.Cong L, Ono-Kihara M, Xu G, Ma Q, Pan X, Zhang D, Homma T, Kihara M. The characterisation of sexual behaviour in Chinese male university students who have sex with other men: a cross-sectional study. BMC Public Health. 2008;8(1):250. doi: 10.1186/1471-2458-8-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang Z, Chen W, Jin M, Chen W, Zhou X, Wang H, Chen L, Jiang T. Analysis of homosexual behavior characteristics and influencing factors of male college students in Zhejiang Province. Medicine. 2021;100(30):e26746. doi: 10.1097/md.0000000000026746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fan S, Li P, Hu Y, Gong H, Yu M, Ding Y, Luo Z, Wu G, Ouyang L, Zou H, et al. Geosocial networking smartphone app use and high-risk sexual behaviors among men who have sex with men attending university in China: cross-sectional study. MIR Public Health Surveill. 2022;8(3):e31033. doi: 10.2196/31033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lulli LG, Baldassarre A, Mucci N, Arcangeli G. Prevention, risk exposure, and knowledge of monkeypox in occupational settings: a scoping review. Trop Med Infect Dis. 2022;7(10):276. doi: 10.3390/tropicalmed7100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumar N, Ahmed F, Raza MS, Rajpoot PL, Rehman W, Khatri SA, Mohammed M, Muhammad S, Ahmad R. Monkeypox cross-sectional survey of knowledge, attitudes, practices, and willingness to vaccinate among university students in Pakistan. Vaccines. 2022;11(1):11. doi: 10.3390/vaccines11010097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Betancort-Plata C, Lopez-Delgado L, Jaén-Sanchez N, Tosco-Nuñez T, Suarez-Hormiga L, Lavilla-Salgado C, Pisos-Álamo E, Hernández-Betancor A, Hernández-Cabrera M, Carranza-Rodríguez C, et al. Monkeypox and HIV in the Canary Islands: a different pattern in a mobile population. Trop Med Infect Dis. 2022;7(10):318. doi: 10.3390/tropicalmed7100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ibrahim AM, Zaghamir DEF. Knowledge and attitudes towards mpox and effect of intervention among college of applied medical sciences students. Libyan J Med. 2023;18(1):2222448. doi: 10.1080/19932820.2023.2222448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Y, Peng X, Fu L, Wang B, Sun Y, Chen Y, Lin Y-F, Wu X, Liu Q, Gao Y, et al. Monkeypox awareness and low vaccination hesitancy among men who have sex with men in China. J Med Virol. 2023;95(2):e28567. doi: 10.1002/jmv.28567. [DOI] [PubMed] [Google Scholar]
- 28.Li M, Zheng Y, Luo Y, Ren J, Jiang L, Tang J, Yu X, Luo D, Fan D, Chen Y, et al. Hesitancy toward COVID-19 vaccines among medical students in Southwest China: a cross-sectional study. Hum Vaccin Immunother. 2021;17(11):4021–7. doi: 10.1080/21645515.2021.1957648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prevention CCfDCa . Surveillance of monkeypox outbreaks in 2023; 2023. https://www.chinacdc.cn/jkzt/crb/zl/szkb_13037/gnyq/202310/t20231016_270134.html.
- 30.Isidro J, Borges V, Pinto M, Sobral D, Santos JD, Nunes A, Mixão V, Ferreira R, Santos D, Duarte S, et al. Phylogenomic characterization and signs of microevolution in the 2022 multi-country outbreak of monkeypox virus. Nat Med. 2022;28(8):1569–72. doi: 10.1038/s41591-022-01907-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lv S, Lu J, Li X. Progress in research on monkeypox virus and its vaccine. Chinese J Biol. 2022;35:1409–13. doi: 10.13200/j.cnki.cjb.003776. [DOI] [Google Scholar]
- 32.Wang Y, Li L, Zhou W. The status quo of the coming out of young men who have sex with men and their self-identity and the analysis of the related factors in Mianyang city. Chinese J Hum Sex. 2019;28:149–53. [Google Scholar]
- 33.Liang Y, Li J, Li T. Analysis of behavioral characteristics of AIDS high-risk populations and HIV infection risk. Chinese J Dermatovenereol. 2013;27:1026–8. [Google Scholar]
- 34.Lin HR, Zhang YL, Zeng Y, Li JY, Peng CM, Xu JQ. Analysis and discussion on the epidemiological investigation of 16 cases of monkeypox. China Trop Med . 2023. Nov 15;24(1):107–110. doi: 10.13604/j.cnki.46-1064/r.2024.01.20. [DOI] [Google Scholar]
- 35.Schäfer M, Stark B, Werner AM, Mülder LM, Heller S, Reichel JL, Schwab L, Rigotti T, Beutel ME, Simon P, et al. Determinants of university students’ COVID-19 vaccination intentions and behavior. Sci Rep. 2022;12(1):18067. doi: 10.1038/s41598-022-23044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tavolacci MP, Dechelotte P, Ladner J. COVID-19 vaccine acceptance, hesitancy, and resistancy among university students in France. Vaccines. 2021;9(6). doi: 10.3390/vaccines9060654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hong J, Pan B, Jiang HJ, Zhang QM, Xu XW, Jiang H, Ye J-E, Cui Y, Yan X-J, Zhai X-F, et al. The willingness of Chinese healthcare workers to receive monkeypox vaccine and its independent predictors: a cross-sectional survey. J Med Virol. 2023;95(1):e28294. doi: 10.1002/jmv.28294. [DOI] [PubMed] [Google Scholar]
- 38.Feng Y, Zhang Y, Liu S, Guo M, Huang H, Guo C, Wang W, Zhang W, Tang H, Wan Y, et al. Unexpectedly higher levels of anti-orthopoxvirus neutralizing antibodies are observed among gay men than general adult population. BMC Med. 2023;21(1):183. doi: 10.1186/s12916-023-02872-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reyes-Urueña J, D’Ambrosio A, Croci R, Bluemel B, Cenciarelli O, Pharris A, Dukers-Muijrers N, Nutland W, Niaupari S, Badran J, et al. High monkeypox vaccine acceptance among male users of smartphone-based online gay-dating apps in Europe, 30 July to 12 August 2022. Eurosurveillance. 2022;27(42). doi: 10.2807/1560-7917.Es.2022.27.42.2200757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mose A, Haile K, Timerga A, Delcea C. COVID-19 vaccine hesitancy among medical and health science students attending Wolkite University in Ethiopia. PLoS One. 2022;17(1):e0263081. doi: 10.1371/journal.pone.0263081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zou H, Huang Y, Chen T, Zhang L. Influenza vaccine hesitancy and influencing factors among university students in China: a multicenter cross-sectional survey. Ann Med. 2023;55(1):2195206. doi: 10.1080/07853890.2023.2195206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang Y, Chen C, Wang L, Wu H, Chen T, Zhang L. HPV vaccine hesitancy and influencing factors among university students in China: a cross-sectional survey based on the 3Cs model. Int J Envir Res Pub Health. 2022;19(21):14025. doi: 10.3390/ijerph192114025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen Y, Zhang MX, Lin XQ, Wu H, Tung TH, Zhu JS. COVID-19 vaccine hesitancy between teachers and students in a college, a cross-sectional study in China. Hum Vaccin Immunother. 2022;18(5):2082171. doi: 10.1080/21645515.2022.2082171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Silva J, Bratberg J, Lemay V. COVID-19 and influenza vaccine hesitancy among college students. J Am Pharm Assoc. 2021;61(6):709–14.e1. doi: 10.1016/j.japh.2021.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiao K, Xu Y, Huang S, Zhang Y, Zhou J, Li Y, Xiao Y, Ma W, He L, Ren X, et al. Mpox risk perception and associated factors among Chinese young men who have sex with men: results from a large cross-sectional survey. J Med Virol. 2023;95(8):e29057. doi: 10.1002/jmv.29057. [DOI] [PubMed] [Google Scholar]
- 46.Dong C, Yu Z, Zhao Y, Ma X. Knowledge and vaccination intention of monkeypox in China’s general population: a cross-sectional online survey. Travel Med Infect Dis. 2023;52:102533. doi: 10.1016/j.tmaid.2022.102533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sallam M, Al-Mahzoum K, Dardas LA, Al-Tammemi AB, Al-Majali L, Al-Naimat H, Jardaneh L, AlHadidi F, Al-Salahat K, Al-Ajlouni E, et al. Knowledge of human monkeypox and its relation to conspiracy beliefs among students in Jordanian health schools: filling the knowledge gap on emerging zoonotic viruses. Med (Kaunas, Lithuania). 2022;58(7):924. doi: 10.3390/medicina58070924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Takayanagi IJ, Cardoso MR, Costa SF, Araya ME, Machado CM. Attitudes of health care workers to influenza vaccination: why are they not vaccinated? Am J Infect Control. 2007;35(1):56–61. doi: 10.1016/j.ajic.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 49.Sanchez AM, Busse K, MacKinnon K, Henk L, MacKinnon GE, Brown J, Mauermann, S, Dobrowski, T, Jungmann, J, Bultman, JSingh, S.. Collective action: the medical college of Wisconsin COVID-19 vaccination program. WMJ. 2021;120:305–8. [PubMed] [Google Scholar]
- 50.Dratva J, Wagner A, Zysset A, Volken T. To vaccinate or not to vaccinate—this is the question among Swiss university students. Int J Envir Res Pub Health. 2021;18(17):18. doi: 10.3390/ijerph18179210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ye M, Giri M. Prevalence and correlates of HIV infection among men who have sex with men: a multi-provincial cross-sectional study in the southwest of China. HIV/AIDS (Auckland, NZ). 2018;10:167–75. doi: 10.2147/hiv.S176826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.He J, Yuan L, Wu C. Temporal⁃spatial distribution of AIDS epidemic in China. Chin J Dis Control Prev. 2022;26:541–6. doi: 10.16462/j.cnki.zhjbkz.2022.05.009. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


