Abstract
Tenosynovitis represents a common clinical condition characterized by inflammation of the synovium that encases the tendon sheath. Although tenosynovities may be noted in any tendon in the body, extremities such as hand, and foot remain the sites of high predilection to acquire this condition. The predominant cause of this predilection rests in the intricate tendon arrangements in these extremities that permit fine motor actions. This editorial explores the common causes and the complications associated with this condition to improve the understanding of the readers of this common condition encountered in our everyday clinical practice.
Keywords: Tenosynovitis, Gout, Hand, Complications, Infection
Core tip: Hand tenosynovitis can be due to either infective or non-infective reasons such as idiopathic, overuse, and autoimmune reasons. Although infective tenosynovitis is usually due to traumatic insults, systemic reasons do exist. Similarly, among the non-infective causes, apart from the autoimmune and overuse causes, idiopathic tenosynovitis also contributes to its etiology. The common complications encountered with this condition depend on the cause, where infective tenosynovitis may result in stiffness, adhesion, deformity, and further spread of infection to deeper structures, and non-infective tenosynovitis results in stenosing tenosynovitis that presents with contractures all of which necessitates surgical management.
INTRODUCTION
Tenosynovitis represents a common clinical condition characterized by inflammation of the synovium that encases the tendon causing pain, swelling, and stiffness. Although every tendon in the body is susceptible to the condition, it is more common in the wrist, hand, and foot. Knowledge of the tendon anatomy aids in understanding the causes, treatments, and complications of tenosynovitis. For example, the hand is a good example of how the tendon and the sheath are related. The tendons in the hand are arranged in a complex way that allows the hand to grip, grasp, and perform fine movements. Once the tendon leaves the carpal tunnel at the level of the wrist joint, the flexor digitorium superficialis and profundus tendons cross the palmar aspect to enter the fibrous tunnels in each finger. Inside each tunnel, the tendons are wrapped by a bursa or synovial sheath. The tendon sheath is composed of a synovial layer and a fibrous tunnel segment. This tendon sheath structure creates a low-friction environment, which enables the tendon to glide smoothly and prevents damage from friction. The fibrous sheath holds the tendon in place and stops it from bowstringing upon repetitive flexion movements.
ETIOLOGY
Tenosynovitis can be due to infectious or non-infectious causes as shown in Figure 1. The possible etiology for non-infectious origin includes autoimmune, overuse, and idiopathic causes.
Figure 1.
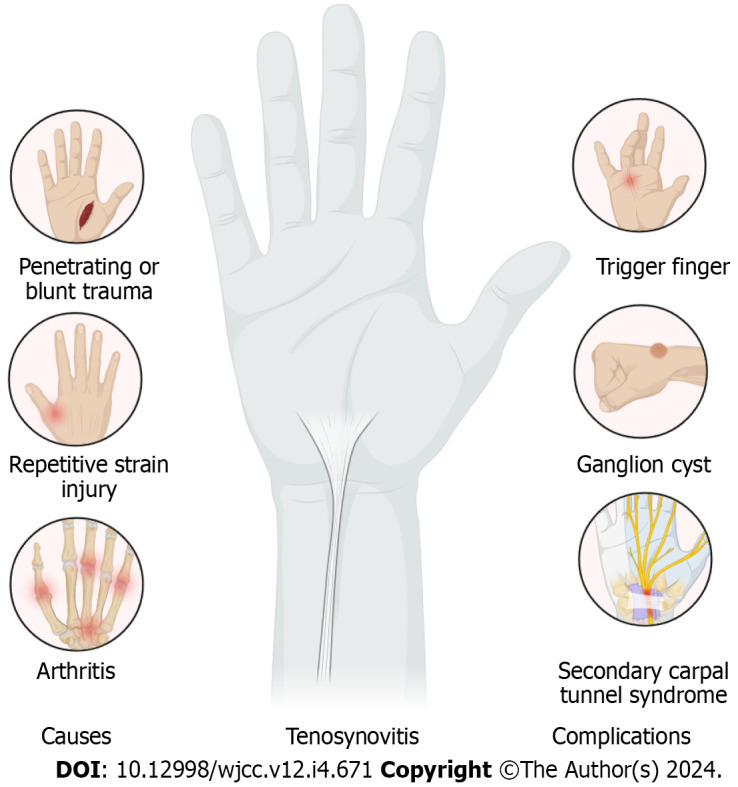
Common causes and complications with the tenosynovitis of the tendons of the hand.
Autoimmune
Tenosynovitis is noted in 87% of the patients with rheumatoid arthritis on magnetic resonance imaging (MRI) showing a very strong connection between them[1]. Synovial tissues are the pathologic structures in rheumatoid arthritis. Owing to the synovial component noted in the tendon sheath, synovial inflammation plays an important role in the disease process and the patient’s symptoms[2]. Psoriatic arthritis is also a frequent autoimmune condition that is commonly associated with tenosynovitis[3].
Overuse
Repeated movements can lead to synovial sheath inflammation that results in strain injury or overuse syndrome to the synovial sheath. Owing to the repetitive irritation to the synovial sheath tenosynovitis occurs.
Idiopathic
The condition can also be idiopathic without any known causes ascertained for its development.
Infectious
Direct injury contamination or spread from the infected soft tissues in the vicinity, infective tenosynovitis could result from the transfer of infectious agents. The most frequent organisms responsible include Staphylococcus aureus (40% to 75%) followed by methicillin-resistant Staphylococcus aureus MRSA (29%). Human bites could result in the injection of common skin bacteria such as Staphylococcus epidermidis, beta-hemolytic Streptococcus, Pseudomonas aeruginosa, and Eikinella into the tendon sheath. Pasturella multocida infection is also noted in animal bites[4].
EPIDEMIOLOGY
The epidemiology of tenosynovitis depends on the cause. The overall incidence of stenosing tenosynovitis in the general population is 1.7% to 2.6%[5]. The reported incidence increases to 10% to 20% in people with diabetes mellitus[6]. Hand is associated with 2.5% to 9.4% of infectious tenosynovitis with concomitant hand infections[7]. On average 55% of the people with rheumatoid arthritis report the symptoms in 3.1 tendons[8].
PATHOPHYSIOLOGY
Tenosynovitis is when the tendon sheath, which is a fluid-filled tissue that covers the tendon, gets inflamed. The cause of tenosynovitis can be different, but the inflammation and thickening of the tendon sheath are noted in all cases[9]. This affects the tendon synovium or the tendon itself and makes it harder for the tendon to glide normally. Some tendons, like the Achilles tendon, do not have a sheath and are not affected by tenosynovitis. Infectious tenosynovitis can get worse over time and damage the sheath, tendon, and nearby structures in sequential stages[10].
PRESENTING COMPLAINTS
A good history can help find the cause of tenosynovitis, which is important for treatment[7,9,11]. An infection may be caused if there is an incident of fever, ulceration, injury, or pus with sudden pain, or stiffness in the fingers or toes. A chronic condition like arthritis or autoimmune disorder may be the cause if there is a history of insidious onset of symptoms. Physical exam findings depend on the cause and severity of tenosynovitis, but they usually show pain, swelling, and redness, along with reduced joint movements. For infectious flexor tenosynovitis, there are four cardinal signs such as pain in the flexor sheath, swelling of the tendon, stiffness of the tendon at rest, and pain when stretching the tendon[12]. These signs are very good at finding pyogenic flexor tenosynovitis, but they are not very specific[13]. Other causes of tenosynovitis have different physical signs such as rheumatoid nodules or hand deformities in rheumatoid arthritis, and tophi or crustal deposits in crystalline arthropathy[14,15]. The physical exam may not be evident in chronic overuse injuries. Tenosynovitis can get worse and cause visible stiffness and tightness of the tendon. Stenosing tenosynovitis is when the flexor tendon becomes too big for the flexor retinaculum pulley (A1 pulley), which causes the joint to “catch” or “lock” resulting in trigger finger which causes bending stiffness at the proximal interphalangeal (PIP) joints[14]. PIP stiffness of the thumb results from the stenosing tenosynovitis of the abductor pollicis longus (APL) and extensor pollicis brevis, noted in clinical examination with a positive Finklestein test (pain during acute bending of hand and wrist altogether) and is called de-Quervain tenosynovitis.
INVESTIGATIONS
The various etiology of tenosynovitis can be elucidated by laboratory tests. However, they are not always needed. For infectious reasons causing tenosynovitis, high white cell count, blood culture, and sensitivity of regional specimens may be employed. Specific markers are available to rule out autoinflammatory diseases. Laboratory examination for crystalline arthropathy conditions could help in differentiating them from infection or inflammation when in question[16].
Imaging tests aid in confirming the diagnosis of tenosynovitis. However, they are not always needed. The radiographic findings noted in the inflammatory tenosynovities include the hardening of synovial membrane or bone reaction; which can also be normal. A computed tomography (CT) scan can aid in identifying bone erosion or deformities, but it is not very good at identifying synovitis and tenosynovitis[17].
Ultrasound can often help with diagnosis, especially in hand tenosynovitis with 15% of tendons showing changes in the form of unclear edges in 62%[18]. Also, thicker tendons could be seen in 44% of fingers, with 6% more demonstrating cysts in the sheath and 4% with other findings in the metacarpophalangeal joints[18]. MRI could be considered in cases where ultrasound could not delineate the details needed. Infective tenosynovitis could use contrast images to visualize abscesses better. MRI signs of tenosynovitis can vary depending on the cause, but they often show swelling around the tendon and thicker extensor brevis longus and APL tendons in de-Quervain tenosynovitis[19]. The bone marrow signals usually go up even before the tenosynovitis features in rheumatoid arthritis[17]. Fluid collections that show enhancement are signs of abscess.
MANAGEMENT
Management of infectious tenosynovitis depends on the organism identified; but when unknown, emperical antibiotics employed include vancomycin 15-20 mg/kg/dose IV every 8 to 12 h, or a 3rd-generation cephalosporin 1-2 g IV every 24 h[7]. The duration of antibiotics depends on clinical signs, the presence of systemic infection, and infection source. Stage 1 infection is managed with sheath washing either by tube-directed therapy or open lavage[7]. Stage 2 or 3 infections usually require an open lavage[19,20].
Non-infectious causes of tenosynovitis are managed with the help of non-steroidal anti-inflammatory drugs (NSAIDs) such as naproxen[21]. Apart from the drugs, the common first-line management options include modification of activities that aggravate the symptoms, rest, and glucocorticoid therapy[21-23]. Disease-modifying antirheumatic drugs (DMARDs) especially glucocorticoids will be more helpful in patients who are not responding to the NSAIDs[24]. Surgery may be needed after 3 to 6 months if the condition worsens despite careful management[21]. Surgery may involve debridement and adhesiolysis[21,25].
The common differential diagnosis of the condition is cellulitis and joint-related diseases. In cellulitis the condition may mimic tenosynovitis, making it hard to move the joint due to swelling and pain. Other conditions that affect the joints such as osteoarthritis, gout, pseudogout, rheumatoid arthritis, and psoriatic arthritis may also mimic the condition. Recent or old injuries of bone or tendon may also present like stenosing tenosynovitis. Dupuytren contractures can also mimic the stenosing variant of tenosynovitis and it is due to the facial hardening resulting in chronic finger locking.
PROGNOSIS
The early management in the form of antibiotics and lavage results in best results in cases of infectious tenosynovitis[7]. Bad prognostic indicators in the management of infective tenosynovitis include infection with organisms such as Streptococcus pyogenes or polymicrobial infection, delayed antibiotic therapy and surgery, pus around the tendon, diabetes mellitus, associated renal disease, and blood vessel disease[12,20]. Stage 3 disease with severe damage has the worst results with a 59% risk of tendon rupture[7]. The results of non-infectious tenosynovitis depend on the cause. In stenosing tenosynovitis, 93% usually respond with good results, with finger signs improving within 6 to 10 weeks of plastic splint usage, and 54% recorded complete healing[22]. About half of the patients who need glucocorticoid therapy after failed conservative therapy have lasting relief for more than a year[23]. Surgery also has a good outcome, with only 4.6% of patients having recurrent symptoms[26]. Patients with diabetes mellitus are resistant to management with corticosteroid or surgical treatment and show poor outcomes[27].
COMPLICATIONS
Infectious/pyogenic tenosynovitis has a high complication rate of 38%. It results in finger stiffness that lasts long with changes in the bone or tendon, and further risk of recurrent infection in the deep spaces of the hand, tenolysis, adhesions, and sometimes necessitating amputation[7]. Non-infectious tenosynovitis can worsen and become stenosing tenosynovitis, which leads to chronic contractures and flexion deformities that need surgery; secondary carpal tunnel syndrome or sometimes present with ganglion cyst as shown in Figure 1. Non-infectious tenosynovitis that requires surgery might also suffer from secondary complications such as infection, nerve damage, flexor tendon problems, and tissue scars due to the procedure[28].
To prevent infectious tenosynovitis, it is important to avoid situations that can infect the hands. The patient should also notice early signs of infection like tenderness, pain, contracture, and swelling of a finger and seek emergent treatment[7]. Patients with non-infectious tenosynovitis are advised to limit activities that aggravate their symptoms and to control the systemic disease that might play a role in the disease process.
CONCLUSION
It is very important to identify infectious tenosynovitis early with history and physical examination to initiate emergent treatment with antibiotics and if needed surgery to avoid serious complications. Ultrasound can help when radiographs are not useful. MRI is better than CT for further evaluation. The first line of management of non-infectious tenosynovitis remains conservative therapy with NSAIDs and splinting. In resistant cases, DMARDs, steroid injections, and surgery may be needed.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: November 4, 2023
First decision: December 21, 2023
Article in press: January 12, 2024
Specialty type: Orthopedics
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Keppeke GD, Chile S-Editor: Gong ZM L-Editor: A P-Editor: Zhao S
Contributor Information
Sathish Muthu, Department of Orthopaedics, Government Medical College, Karur 639004, Tamil Nadu, India; Orthopaedic Research Group, Coimbatore 641045, Tamil Nadu, India; Department of Biotechnology, Faculty of Engineering, Karpagam Academy of Higher Education, Coimbatore 641021, Tamil Nadu, India. drsathishmuthu@gmail.com.
Saravanan Annamalai, Department of Orthopaedics, Government Thiruvallur Medical College, Thiruvallur 631203, Tamil Nadu, India.
Velmurugan Kandasamy, Department of Orthopaedics, Government Kilpauk Medical College, Chennai 600010, Tamil Nadu, India.
References
- 1.Rogier C, Hayer S, van der Helm-van Mil A. Not only synovitis but also tenosynovitis needs to be considered: why it is time to update textbook images of rheumatoid arthritis. Ann Rheum Dis. 2020;79:546–547. doi: 10.1136/annrheumdis-2019-216350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hayer S, Redlich K, Korb A, Hermann S, Smolen J, Schett G. Tenosynovitis and osteoclast formation as the initial preclinical changes in a murine model of inflammatory arthritis. Arthritis Rheum. 2007;56:79–88. doi: 10.1002/art.22313. [DOI] [PubMed] [Google Scholar]
- 3.McQueen F, Lassere M, Østergaard M. Magnetic resonance imaging in psoriatic arthritis: a review of the literature. Arthritis Res Ther. 2006;8:207. doi: 10.1186/ar1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flevas DA, Syngouna S, Fandridis E, Tsiodras S, Mavrogenis AF. Infections of the hand: an overview. EFORT Open Rev. 2019;4:183–193. doi: 10.1302/2058-5241.4.180082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cagliero E, Apruzzese W, Perlmutter GS, Nathan DM. Musculoskeletal disorders of the hand and shoulder in patients with diabetes mellitus. Am J Med. 2002;112:487–490. doi: 10.1016/s0002-9343(02)01045-8. [DOI] [PubMed] [Google Scholar]
- 6.Strom L. Trigger finger in diabetes. J Med Soc N J. 1977;74:951–954. [PubMed] [Google Scholar]
- 7.Giladi AM, Malay S, Chung KC. A systematic review of the management of acute pyogenic flexor tenosynovitis. J Hand Surg Eur Vol. 2015;40:720–728. doi: 10.1177/1753193415570248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gray RG, Gottlieb NL. Hand flexor tenosynovitis in rheumatoid arthritis. Prevalence, distribution, and associated rheumatic features. Arthritis Rheum. 1977;20:1003–1008. doi: 10.1002/art.1780200414. [DOI] [PubMed] [Google Scholar]
- 9.Adams JE, Habbu R. Tendinopathies of the Hand and Wrist. J Am Acad Orthop Surg. 2015;23:741–750. doi: 10.5435/JAAOS-D-14-00216. [DOI] [PubMed] [Google Scholar]
- 10.Michon J. [Phlegmon of the tendon sheaths] Ann Chir. 1974;28:277–280. [PubMed] [Google Scholar]
- 11.Hyatt BT, Bagg MR. Flexor Tenosynovitis. Orthop Clin North Am. 2017;48:217–227. doi: 10.1016/j.ocl.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Pang HN, Teoh LC, Yam AK, Lee JY, Puhaindran ME, Tan AB. Factors affecting the prognosis of pyogenic flexor tenosynovitis. J Bone Joint Surg Am. 2007;89:1742–1748. doi: 10.2106/JBJS.F.01356. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy CD, Lauder AS, Pribaz JR, Kennedy SA. Differentiation Between Pyogenic Flexor Tenosynovitis and Other Finger Infections. Hand (N Y) 2017;12:585–590. doi: 10.1177/1558944717692089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blood TD, Morrell NT, Weiss AC. Tenosynovitis of the Hand and Wrist: A Critical Analysis Review. JBJS Rev. 2016;4 doi: 10.2106/JBJS.RVW.O.00061. [DOI] [PubMed] [Google Scholar]
- 15.Lee DY, Eo S, Lim S, Yoon JS. Gouty tenosynovitis with compartment syndrome in the hand: A case report. World J Clin Cases. 2023;11:7492–7496. doi: 10.12998/wjcc.v11.i30.7492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kostman JR, Rush P, Reginato AJ. Granulomatous tophaceous gout mimicking tuberculous tenosynovitis: report of two cases. Clin Infect Dis. 1995;21:217–219. doi: 10.1093/clinids/21.1.217. [DOI] [PubMed] [Google Scholar]
- 17.Østergaard M, Boesen M. Imaging in rheumatoid arthritis: the role of magnetic resonance imaging and computed tomography. Radiol Med. 2019;124:1128–1141. doi: 10.1007/s11547-019-01014-y. [DOI] [PubMed] [Google Scholar]
- 18.Kim HR, Lee SH. Ultrasonographic assessment of clinically diagnosed trigger fingers. Rheumatol Int. 2010;30:1455–1458. doi: 10.1007/s00296-009-1165-3. [DOI] [PubMed] [Google Scholar]
- 19.Müller CT, Uçkay I, Erba P, Lipsky BA, Hoffmeyer P, Beaulieu JY. Septic Tenosynovitis of the Hand: Factors Predicting Need for Subsequent Débridement. Plast Reconstr Surg. 2015;136:338e–343e. doi: 10.1097/PRS.0000000000001510. [DOI] [PubMed] [Google Scholar]
- 20.Mamane W, Lippmann S, Israel D, Ramdhian-Wihlm R, Temam M, Mas V, Pierrart J, Masmejean EH. Infectious flexor hand tenosynovitis: State of knowledge. A study of 120 cases. J Orthop. 2018;15:701–706. doi: 10.1016/j.jor.2018.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wagner ER, Gottschalk MB. Tendinopathies of the Forearm, Wrist, and Hand. Clin Plast Surg. 2019;46:317–327. doi: 10.1016/j.cps.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Colbourn J, Heath N, Manary S, Pacifico D. Effectiveness of splinting for the treatment of trigger finger. J Hand Ther. 2008;21:336–343. doi: 10.1197/j.jht.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Rozental TD, Zurakowski D, Blazar PE. Trigger finger: prognostic indicators of recurrence following corticosteroid injection. J Bone Joint Surg Am. 2008;90:1665–1672. doi: 10.2106/JBJS.G.00693. [DOI] [PubMed] [Google Scholar]
- 24.Hammer HB, Kvien TK, Terslev L. Tenosynovitis in rheumatoid arthritis patients on biologic treatment: involvement and sensitivity to change compared to joint inflammation. Clin Exp Rheumatol. 2017;35:959–965. [PubMed] [Google Scholar]
- 25.Fiorini HJ, Tamaoki MJ, Lenza M, Gomes Dos Santos JB, Faloppa F, Belloti JC. Surgery for trigger finger. Cochrane Database Syst Rev. 2018;2:CD009860. doi: 10.1002/14651858.CD009860.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mishra SR, Gaur AK, Choudhary MM, Ramesh J. Percutaneous A1 pulley release by the tip of a 20-g hypodermic needle before open surgical procedure in trigger finger management. Tech Hand Up Extrem Surg. 2013;17:112–115. doi: 10.1097/BTH.0b013e31828ef983. [DOI] [PubMed] [Google Scholar]
- 27.Stahl S, Kanter Y, Karnielli E. Outcome of trigger finger treatment in diabetes. J Diabetes Complications. 1997;11:287–290. doi: 10.1016/s1056-8727(96)00076-1. [DOI] [PubMed] [Google Scholar]
- 28.Ryzewicz M, Wolf JM. Trigger digits: principles, management, and complications. J Hand Surg Am. 2006;31:135–146. doi: 10.1016/j.jhsa.2005.10.013. [DOI] [PubMed] [Google Scholar]


