Abstract
A child’s death from cancer may increase risk for poor self-worth in bereaved siblings. Furthermore, bereaved parents may experience depressive symptoms and communicate differently with their surviving children. However, limited research has examined family factors associated with self-worth in bereaved siblings. Thus, we examined: (a) differences in parental depressive symptoms, parent–child communication, and sibling self-worth between bereaved and non-bereaved families, and (b) indirect effects of parental depressive symptoms and communication quality on the association between bereavement and sibling self-worth. Bereaved parents and siblings were recruited 3-12 months after a child’s death from cancer. Bereaved (n=72) and non-bereaved families of classmates (n=58) completed home-based questionnaires upon enrollment (T1), and 48 bereaved and 45 non-bereaved families completed one-year follow-up (T2). Relative to controls at T1 and T2, bereaved mothers, but not fathers, reported more depressive symptoms. Bereaved siblings reported poorer maternal and similar paternal communication, and similar levels of self-worth compared to controls. Both cross-sectional and longitudinal serial mediation models for mothers were significant. Bereaved mothers were at greater risk for depressive symptoms, which adversely affected sibling self-worth over time through disrupted mother–child communication. The father sample was limited, but the cross-sectional model was nonsignificant. Mothers and fathers may grieve differently and may require different therapeutic approaches. Family-centered interventions should target bereaved mothers’ emotional adjustment and communication to enhance sibling self-worth. Additionally, clinicians should bolster other sources of support for bereaved siblings to promote adaptive outcomes.
Keywords: bereavement, pediatric cancer, siblings, family processes, communication
Despite improved survival rates, pediatric cancer remains the second leading cause of death in U.S. children (The American Cancer Society, 2022), and the leading cause of death by disease past infancy (National Cancer Institute, 2022). About 16% of children, on average, die within five years of a cancer diagnosis. Of those who survive past five years, 18% will die in the next 25 years (Mertens et al., 2008). The death of a child is a devastating experience, one that affects the entire family, including siblings. The effects of such a loss on bereaved siblings can be profound and extensive given the unique nature of sibling relationships, which are instrumental to many aspects of child development (Howe, Paine, Ross, & Recchia, 2022; Kramer, 2014; Packman, Horsley, Davies, & Kramer, 2006). However, limited research has focused on siblings bereaved by pediatric cancer, and there is a paucity of prospective, controlled studies examining how bereavement affects sibling self-concept [i.e., one’s perception of themselves (M. Rosenberg, 1979)].
Within the first few years of bereavement, siblings generally experience various adverse outcomes. Research suggests bereaved siblings have higher rates of mental disorders than their peers, especially when under age 13 (Bolton et al., 2016), and they are more likely to experience complicated grief and depression compared to either young adults who lost a close friend or non-bereaved young adults (Herberman Mash, Fullerton, & Ursano, 2013). Siblings bereaved by cancer may be uniquely affected because they often experience family disruption, personal sacrifices of their daily routines, worry and sadness, feelings of neglect and isolation, and loss of the companionship of their ill sibling before the death (Yang, Mu, Sheng, Chen, & Hung, 2016). Within one year after the death, cancer-bereaved siblings report higher substance use, anxiety, and depression (A. Rosenberg et al., 2015), and feeling unsupported, unprepared, and unable to control the mourning process (Lövgren, Jalmsell, Eilegård Wallin, Steineck, & Kreicbergs, 2016; Nolbris & Hellström, 2005). These siblings may even experience permanent feelings of sorrow due to special relationships with the deceased child (Nolbris & Hellström, 2005).
However, cancer-bereaved siblings’ adverse experiences seem to improve over time (Eilegård, Steineck, Nyberg, & Kreicbergs, 2013; A. Rosenberg et al., 2015), and some siblings report positive outcomes such as growth and resilience. Bereaved siblings have reported positive changes in their family roles, family and peer relationships, and personality, including increased maturity, compassion, and motivation (Foster et al., 2012). Some retain fond memories of their brother or sister and experience family cohesion and personal growth throughout the course of the child’s illness and death (Eilertsen, Lövgren, Wallin, & Kreicbergs, 2018). Additionally, a recent review suggests that cancer-bereaved children and adolescents (not specific to siblings) experience a relatively high level of psychosocial well-being (Hoffmann, Kaiser, & Kersting, 2018). Although a child’s death can result in both adaptive and maladaptive adjustment in bereaved siblings, limited research has examined how self-concept is affected, despite its associations with a variety of psychosocial outcomes (Hanley & Garland, 2017; Markus & Wurf, 1987; Park, 2006).
Self-concept has been described as an organization of one’s thoughts and feelings about oneself (M. Rosenberg, 1979), of which one aspect is self-worth, the overall value that one places on oneself. This is also referred to as self-esteem, (Harter, 1987), and can be considered a dimension of the self-concept (Gecas, 1982). The present study measured global self-worth to operationalize self-concept, but existing research on bereaved siblings often operationalizes and measures self-concept differently, making it difficult to directly compare findings (Eilegård et al., 2013; Herberman Mash et al., 2013; Hogan & Greenfield, 1991; Michael & Lansdown, 1986). Few studies have examined different dimensions of self-concept among cancer-bereaved siblings, with evidence of low self-esteem in a small sample (Michael & Lansdown, 1986) and in comparison to non-bereaved peers (Eilegård et al., 2013). General research with bereaved siblings notes the risk for low self-esteem and self-worth, especially when their brother or sister was ill for a short period before death (Herberman Mash et al., 2013; Michael & Lansdown, 1986). Variability in sibling self-concept over time has been found following general bereavement (Hogan & Greenfield, 1991), and there is evidence that self-concept may influence future psychological health (Hanley & Garland, 2017; Park, 2006). For instance, studies suggest low self-esteem and self-concept clarity prospectively predict depression (Sowislo & Orth, 2013; Van Dijk et al., 2014). Thus, global self-worth has the potential to act as a risk and protective factor following bereavement (Kapke, Grace, Gerdes, & Lawton, 2017; Thoits, 2013), and understanding factors that contribute to self-worth among bereaved siblings may be important for their adjustment over time.
In addition to siblings, grieving the loss of a child is incredibly difficult and can have lasting effects for parents. Research has shown that in general, bereaved parents are at greater risk of mortality and negative health outcomes (i.e., greater healthcare utilization, acute illness, sleep problems)(October, Dryden-Palmer, Copnell, & Meert, 2018; Youngblut, Brooten, Cantwell, del Moral, & Totapally, 2013). A systematic review reported that cancer-bereaved parents have increased risk of anxiety, depression, prolonged grief, and poor quality of life (A. Rosenberg, Baker, Syrjala, & Wolfe, 2012), and parents may be at risk for psychological distress for several years after the death of their child (Dumont et al., 2022; Pohlkamp, Kreicbergs, & Sveen, 2019; Rasouli, Bø, Reinfjell, Moksnes, & Eilertsen, 2021). Bereaved fathers are less prominent in the literature with research focusing mostly on mother perspectives. Studies suggest fathers may be less overt in their grief (Alam, Barrera, D’Agostino, Nicholas, & Schneiderman, 2012) and less open in their communication than mothers, as they tend to avoid talking about their feelings (Alam et al., 2012; McNeil, Baker, Snyder, Rosenberg, & Kaye, 2021). Fathers may be socialized to be more stoic, and one study found fathers acknowledged they immerse themselves in their work to deal with their grief (Alam et al., 2012).
Despite resilience among some bereaved families (O’Connor & Barrera, 2014), parents’ prolonged grief can result in limited support for and communication with their surviving children (Decinque et al., 2006; Pariseau, Chevalier, Muriel, & Long, 2020), which may affect sibling adjustment. For example, one study found direct associations between maternal symptoms of post-traumatic stress disorder and prolonged grief on sibling mental health, as well as indirect associations between paternal symptoms and sibling outcomes through decreased positive parenting (Morris, Gabert-Quillen, Friebert, Carst, & Delahanty, 2016). Externalizing problems in cancer-bereaved siblings may be partially explained by the impact of mothers’, but not fathers’, distress on their parenting and communication (Howard Sharp et al., 2020). Insufficient and unsatisfactory communication after the death has been linked to distress and long-term anxiety in cancer-bereaved siblings (A. Rosenberg et al., 2015; Wallin, Steineck, Nyberg, & Kreicbergs, 2016), whereas talking about the deceased child with parents can help siblings cope (Barrera, Alam, D’Agostino, Nicholas, & Schneiderman, 2013). Thus, parental grief responses to losing a child to cancer may disrupt parent–child communication with bereaved siblings, and subsequently influence their psychosocial adjustment.
Family systems theory (Cox & Paley, 1997) describes the family as a dynamic system, comprised of individuals and subsystem relationships that have a multidirectional impact on each other. As family systems experience changes and a reorganization of old patterns, it may create risk for family dysfunction. Thus, it is important to consider the multidirectional influences of the family system as they experience and adapt to the death of a child. Bereaved siblings may experience the death as individuals, but they will also be affected by their family members’ grief and the subsequent changes to their relationships. These changes, especially in parent–child communication (Van Dijk et al., 2014), may affect bereaved siblings’ self-concept.
Generally, parent–child communication in adolescence can already be challenging due to changing parent–child relationships and increasing child autonomy, which can lead to altered patterns of self-disclosure and perceptions of privacy (Branje, Laursen, & Collins, 2012). Experiencing the illness trajectory and loss of a child with cancer may result in additional difficulties navigating changing parent–child communication patterns, such as periods of parent–child separation during treatment, siblings feeling forgotten or in the way, and parent mental health concerns (Eilertsen et al., 2018). Relatedly, perceived parental support, parent attachment, and positive parent–child relationships have been linked to higher levels of global self-worth in adolescents (Birkeland, Melkevik, Holsen, & Wold, 2012; Chii, Seok, & Sombuling, 2016; Wouters, Doumen, Germeijs, Colpin, & Verschueren, 2013). A weak but positive association between family communication and self-worth has been reported (Jackson, Bijstra, Oostra, & Bosma, 1998), with evidence of a longitudinal impact of family communication on self-esteem (Birndorf, Ryan, Auinger, & Aten, 2005; Heaven, 1997). Understanding how factors like parental depression and family communication explain changes in the self-worth of cancer-bereaved siblings could inform potential points of intervention during this devastating experience to mitigate maladaptive outcomes (Hanley & Garland, 2017; Park, 2006; Sowislo & Orth, 2013). To our knowledge, no work has examined longitudinal associations between the quality of parent–child communication and self-worth among siblings bereaved by pediatric cancer, and few studies have investigated group differences compared to normative samples.
The present study aimed to fill these gaps by: (a) examining group differences in child global self-worth, parent–child communication, and parental depressive symptoms among a sample of bereaved and non-bereaved, matched comparison families and (b) examining the impact of bereavement on child self-worth via the indirect effects of parental depressive symptoms and parent–child communication. Bereaved siblings were expected to report lower levels of self-worth one and two-years post-death relative to comparison peers. At one-year post-death, bereaved parents were expected to report more depressive symptoms than non-bereaved parents and bereaved siblings were expected to report poorer parent–child communication. Additionally, we expected that bereaved parents’ elevated depressive symptoms and subsequent disrupted parent–child communication quality at one-year post-death would explain lower levels of self-worth in bereaved siblings two-years post-death.
Method
This research was part of a larger longitudinal study, conducted between 2006-2012, examining family adjustment following the death of a child from cancer (Gerhardt et al., 2012). Bereaved families were identified from cancer registries at three children’s hospitals in the United States and Canada. Eligible siblings were: (a) 8-17 years old, (b) English-speaking, (c) living within 100-miles of the hospital, and (d) not receiving full-time special education. To accommodate various family structures, adopted, half-, and step-siblings were eligible if the sibling had regular contact with the deceased child. In families with multiple eligible siblings, one was randomly selected to participate. Initial data were collected in the schools and homes of bereaved and non-bereaved comparison families within the first-year post-death (T1), followed by another home visit in the second-year post-death (T2). Identical measures were completed at both home visits. The current paper includes longitudinal data collected from a subset of mothers, fathers, and one child from each family at both home visits. In this paper, “family” refers to the participating members of each recruited family (i.e., mother, father, and child; mother and child; father and child). Participants missing variables of interest and with children who were too young to complete self-report measures were excluded from analyses.
Procedures
Ethics or Institutional Review Board (ERB/IRB) approval was obtained at each institution prior to recruitment. Three to 12 months after the child’s death, bereaved families received a study introduction letter from the child’s attending oncologist and were recruited via phone 2-3 weeks later. Participants provided informed consent/assent prior to completing questionnaires at each home visit. Families were compensated for their time.
Comparison families were selected from the school visit based on the identification of one classmate who was closest in age, sex, and race to the bereaved sibling. After the school visit, the family of the first potential comparison peer was invited to participate in the home assessment. If they declined, the next potential classmate was recruited. Comparison families were screened to ensure none experienced the death of a child following a live birth.
Participants
Bereaved Families
Of 169 eligible bereaved families, 88 (52.1%) participated in the first home visit. For the current paper, 6 (n = 82) participants in the mother sample and 37 in the father sample (n = 51) did not participate or were missing variables of interest at the first home visit, and 13 in the mother sample and 7 in the father sample were excluded because the child was too young to provide self-report. This resulted in a T1 sample of 69 mothers, 44 fathers, and 72 total families (41 mother-father-child triads, 28 mother-child dyads, 3 father-child dyads). Chi-square tests and independent sample t-tests revealed that excluded participants in the father and mother samples did not differ from participants with T1 variables of interest on background characteristics. Twenty-four (35%) children in the mother sample and 13 (31%) in the father sample were missing the variable of interest at the second home visit, resulting in a final T2 sample of 45 mothers (65.2%), 31 fathers (70.5%), and 48 families (28 mother-father-child triads, 17 mother-child dyads, 3 father-child dyads). In the larger study, there was a 76.1% retention rate between the first and second visit.
The T1 sample of bereaved siblings (n = 72) was primarily female, White, non-Hispanic, and on average 13.19 (SD = 2.23) years of age (range: 10-18). Bereaved mothers and fathers, respectively, were primarily married (71%, n = 49; 88.6%, n = 39) and the biological parent of the participating child (91.3%, n = 63; 86.4%, n = 38). On average, mothers were 40.13 years old (SD = 6.68), with 13.88 years of education (SD = 2.22); fathers were 42.82 (SD = 7.12) years old, with 14.48 (SD = 2.26) years of education. First home visit data collection occurred an average of 11.71 months (SD = 3.73) after the child’s death. The deceased child averaged 12.27 (SD = 5.16) years of age at the time of death, and the average length of time from diagnosis until death was approximately 2.65 years (SD = 2.49). Additional demographic data is in Table 1.
Table 1.
Demographic Characteristics
| Bereaved (n = 72) n (%) |
Control (n = 58) n (%) |
|
|---|---|---|
| Sibling/Child Gender (% Female) | 42 (58.3) | 31 (53.4) |
| Sibling/Child Race | ||
| American Indian/Native Alaskan | 1 (1.4) | 0 |
| Asian | 5 (6.9) | 2 (3.4) |
| Black or African American | 4 (5.6) | 4 (6.9) |
| Native Hawaiian/Pacific Islander | 2 (2.8) | 0 |
| White | 54 (75.0) | 50 (86.2) |
| Other | 6 (8.3) | 2 (3.4) |
| Sibling/Child Ethnicity | ||
| Non-White Hispanic or Latine | 2 (2.8) | 1 (1.7) |
| White Hispanic or Latine | 3 (4.2) | 2 (3.4) |
| Non-Hispanic or Non-Latine | 67 (93.0) | 55 (94.8) |
| Annual Family Income | ||
| $25,000 or below | 12 (16.7) | 8 (13.8) |
| $25,001 - $50,000 | 19 (26.4) | 13 (22.4) |
| $50,001 - $75,000 | 21 (29.2) | 11 (19.0) |
| $75,001 - $100,000 | 8 (11.1) | 12 (20.7) |
| $100,001 or above | 12 (16.7) | 14 (24.1) |
| Birth Ordera | ||
| Younger than deceased child | 34 (47.2) | - |
| Older than deceased child | 33 (45.8) | - |
Note. Mother data was used for child demographics to retain the largest sample, and father data was used when mother data was unavailable (n = 3).
Data were missing for five families.
Comparison Families
Seventy-three of the eligible comparison families participated. For the current paper, 8 (n = 65) participants in the mother sample and 33 in the father sample (n = 40) did not participate or were missing variables of interest at the first home visit, and 10 in the mother sample (n = 55) and 5 in the father sample (n = 35) were excluded because the child was too young to provide self-report. This resulted in a T1 sample of 55 mothers, 35 fathers, and 58 total families (32 mother-father-child triads, 23 mother-child dyads, 3 father-child dyads). Independent sample t-tests revealed that excluded participants had, on average, a lower family income (M = $51,136, SD = $23,355, n = 11) than participants with variables of interest (M = $75,781, SD = $36,469, n = 32), t(27.55) = 2.58, p = .02. Eleven (20%) children in the mother sample and 8 (22.9%) in the father sample were missing the variable of interest at the second home visit, resulting in a final T2 sample of 44 mothers (80%), 27 fathers (77.1%), and 45 families (26 mother-father-child triads, 18 mother-child dyads, 1 father-child dyad). The T1 sample of comparison siblings (n = 58) was primarily female, White, non-Hispanic, and on average 13.17 (SD = 2.23) years of age (range: 10-18). Comparison mothers and fathers, respectively, were primarily married (83.6%, n = 46; 91.4%, n = 32) and the biological parent of the participating child (96.4%, n = 53; 77.1%, n = 27). On average, mothers were 42.27 years old (SD = 6.79) and had 14.49 years of education (SD = 2.36); fathers were 42.11 (SD = 6.63) years old and had 15 (SD = 2.60) years of education. Bereaved and comparison families did not differ significantly on any demographic characteristics (Table 1).
Measures
Demographic Information and Medical Data
A questionnaire assessed parent-report of family background characteristics, including age, race, ethnicity, education, income, and marital status. Permitted by bereaved parents, the deceased child’s medical records were reviewed for dates of birth, diagnosis, and death.
Parental Depressive Symptoms
The Adult Self-Report (ASR)(Achenbach & Rescorla, 2003) is a 126-item inventory assessing adaptive functioning, problem behaviors, and substance use in ages 18-59. The ASR consists of 8 syndrome scales (e.g., Withdrawn, Aggressive Behavior) and 6 DSM-oriented scales (e.g., Depressive Problems, Anxiety Problems) consistent with DSM-V categories (ASEBA, 2022). The ASR was scored electronically and thus, reliability from our sample is not reported. However, the ASR has established reliability and validity (Achenbach & Rescorla, 2003). This study used the 14-item Depressive Problems subscale. Analyses were conducted using raw scores as recommended by the ASR manual (Achenbach & Rescorla, 2003), but T-scores are reported to aid with interpretation (Table 2).
Table 2.
Total and Group Means for Variables of Interest
| Total Sample (nmothers = 124; nfathers = 79) |
Bereaved (nm = 69; nf = 44) |
Comparison (nm = 55; nf = 35) |
Effect Size | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | SD | M | SD | d | |
|
|
|||||||
| T1 Mother Depression | 58.52 | 8.43 | 61.20 | 9.14 | 55.15 | 5.98 | 0 78*** |
| T2 Mother Depression | 56.87 | 7.84 | 58.50 | 9.08 | 55.00 | 5.68 | 0.46* |
| T1 Father Depression | 54.82 | 6.68 | 54.93 | 5.71 | 54.69 | 7.81 | 0.04 |
| T2 Father Depression | 54.32 | 7.82 | 52.60 | 4.20 | 56.57 | 10.58 | 0.49 |
| T1 Mother–Child Communication | 3.60 | 0.64 | 3.48 | 0.65 | 3.76 | 0.61 | 0.45* |
| T2 Mother–Child Communication | 3.67 | 0.72 | 3.53 | 0.75 | 3.83 | 0.65 | 0.42* |
| T1 Father–Child Communication | 3.65 | 0.66 | 3.56 | 0.67 | 3.76 | 0.65 | 0.30 |
| T2 Father–Child Communication | 3.67 | 0.67 | 3.58 | 0.59 | 3.77 | 0.77 | 0.27 |
| T1 Sibling Self-Worth | 3.32 | 0.58 | 3.28 | 0.51 | 3.37 | 0.66 | 0.15 |
| T2 Sibling Self-Worth | 3.44 | 0.60 | 3.38 | 0.61 | 3.52 | 0.57 | 0.22 |
Note. For T2 variables, the total mother sample is 89 (45 bereaved, 44 controls) and the total father sample is 58 (31 bereaved, 27 controls). T-scores are reported for depression variables. Self-worth scores are reported using the mother sample.
p < .05,
p < .001.
Parent–Child Communication
The Parent–Adolescent Communication Scale (PACS) (Barnes & Olson, 1985) consists of 20 items rated on a 5-point scale from “strongly disagree” to “strongly agree” to obtain parent and adolescent-report (10+ years) of their quality of communication. The PACS has two 10-item subscales (Open Family Communication and Problems in Family Communication), as well as a total communication score. This study utilized the total score from the sibling report of parent–adolescent communication. Higher scores reflect better communication quality. The PACS has established validity and reliability (Barnes & Olson, 1985). Internal consistency in this sample was excellent for the Open subscale (αmother = .90, αfather = .91), acceptable for the Problem subscale (αmother = .77, αfather = .77), and good for the total scale (αmother = .87, αfather = .88).
Sibling’s Self-Worth
The Self-Perception Profile for Children (SPPC) (Harter, 1985) is a widely used measure consisting of 5 subscales that assess perceived competence in scholastics, social acceptance, athletic ability, physical appearance, and behavioral conduct, and one scale that assesses global self-worth. The 36 items are phrased as two related statements placed side by side (e.g., “Some kids would rather play outdoors in their spare time. BUT Other kids would rather watch T.V.”). Children respond by deciding which statement is most like them, and then selecting whether the statement is “Sort of true” or “Really true” for them. Validity and reliability have been established, including among children with chronic illnesses (Ferro & Tang, 2017; Harter, 1985). The current study utilized the global self-worth scale, with good internal consistency (α = .84).
Analysis
Attrition analyses were conducted using independent sample t-tests and Chi square tests. Descriptive statistics were computed for variables of interest at both time points. Pearson and point-biserial correlations (α = .05, two-way) examined initial associations between variables of interest at both time points. Independent sample t-tests (α = .05, two-way) and effect sizes were used to examine group differences in outcomes between bereaved and non-bereaved mothers, fathers, and children. Serial mediation models were tested using Ordinary Least Squares (OLS) regression and post-hoc bootstrapping (N = 5000) with PROCESS, an SPSS macro (Hayes, 2012). A p-value <.05 and a 95% confidence interval that did not include zero were considered significant. The first serial mediation model was cross-sectional and examined the serial indirect effect of parental depressive symptoms and parental–child communication on the association between group status and child self-worth at T1. The second serial mediation model examined the serial indirect effect of T1 maternal depressive symptoms and T1 mother–child communication on the association between group status and child self-worth at T2. This longitudinal model included T1 self-worth as a covariate to examine changes in self-worth. T2 depression and communication were not tested in these models, because we were interested in examining cascading effects of maternal depression and communication on self-worth over time. Utilizing Kline’s (2015) rule of thumb, the sample was too small to test an additional covariate Thus, we conducted a sensitivity analysis including the covariate child age. The father sample at T2 (n = 60) was deemed too small to sufficiently test a longitudinal serial mediation model.
Transparency and Openness
We report how we determined our sample size, all data exclusions, all manipulations, and all measures in the study, and we follow TOP (Nosek et al., 2015) and JARS (Appelbaum et al., 2018). Materials and analysis code for this study are available upon request to the senior author. This study was not pre-registered.
Results
Preliminary and Attrition Analyses
Preliminary analyses were conducted, separately for mother and father samples, to examine whether participants with complete data at both time points (nmother = 89, nfather = 58) differed from participants with data only at T1 (nmother = 35, nfather = 21). Independent sample t-tests compared participants on T1 variables of interest, parent and child age, socioeconomic status, number of children in the home, parental education, months since the death, and age at diagnosis and death of the deceased child; Chi-square tests were conducted to examine differences in child gender, marital status, race, and whether the sibling or parent was present during the death. Results indicated that there were no significant differences between participants who did or did not complete T2.
Descriptive statistics are in Table 2. Bereaved mothers reported significantly more T1 depressive symptoms than non-bereaved mothers, t(117.89) = 4.44, p < .001, and significantly more bereaved mothers (35%, n = 24) reported depressive symptoms in the borderline or clinical range compared to non-bereaved mothers (11%, n = 6), X2 (1, N = 124) = 9.51, p = .002. At T2, bereaved mothers still reported more depressive symptoms than non-bereaved mothers, t(80.07) = 2.22, p = .03, and significantly more bereaved mothers (27%, n = 12) reported depressive symptoms in the borderline or clinical range compared to non-bereaved mothers (10%, n = 4), X2 (1, N = 87) = 4.25, p = .04. Bereaved siblings reported significantly poorer mother–child communication at T1, t(122) = −2.46, p = .02, and T2, t(88) = −2.01, p = .048, than controls. Bereaved fathers reported comparable depressive symptoms to controls at both time points (Table 2). However, the medium effect size for T2 depressive symptoms suggests the sample size may have been too small to detect any significant differences (d = .49). Six (14%) bereaved and 7 (20%) control fathers reported symptoms in the borderline or clinical range at T1, and only 2 (6%) bereaved and 3 (11%) controls reported these at T2, with no significant differences. Bereaved siblings and controls reported similar quality of father–child communication. Unexpectedly, bereaved siblings reported similar levels of global self-worth at T1, t(122) = −0.85, p = .40, d = .15, and T2, t(87) = −1.02, p = .31, d = .22, compared to controls.
Correlations can be found in Table 3 and were in the expected directions. Older child age was associated with poorer T1 parent–child communication and T2 self-worth. Bereavement was related to greater T1 and T2 maternal depressive symptoms, and poorer T1 and T2 mother–child communication. Bereavement was not associated with paternal depressive symptoms, father–child communication, or global self-worth at either time point. Greater maternal depressive symptoms at T1 were associated with poorer T1 mother–child communication. Better T1 parent–child communication was associated with higher self-worth at both T1 and T2.
Table 3.
Correlation Table for Total Sample (N = 130; Nmothers = 124, Nfathers = 79)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | T1 Mother Depression | |||||||||||||
| 2. | T2 Mother Depression | .75*** | ||||||||||||
| 3. | T1 Father Depression | .33** | .23 | |||||||||||
| 4. | T2 Father Depression | .22 | .10 | .80*** | ||||||||||
| 5. | T1 Mother-Child Communication | −.30*** | −.27* | −.06 | .02 | |||||||||
| 6. | T2 Mother-Child Communication | −.32** | −.19 | −.07 | −.03 | .70*** | ||||||||
| 7. | T1 Father-Child Communication | −.22* | −.25* | −.12 | −.31* | .56*** | .30** | |||||||
| 8. | T2 Father-Child Communication | −.06 | −.15 | −.06 | −.13 | .40*** | .43*** | .61*** | ||||||
| 9. | T1 Self-Worth | −.10 | −.18 | −.08 | .02 | .45*** | .45*** | .31*** | .34** | |||||
| 10. | T2 Self-Worth | −.01 | .04 | .13 | .03 | .42*** | .59*** | .40*** | .47*** | .58*** | ||||
| 11. | Group Status | .36*** | .23* | .02 | −.25 | −.23** | −.22* | −.16 | −.03 | −.09 | −.11 | |||
| 12. | Child Age | .02 | −.07 | −.10 | .02 | −.25** | −.21* | −.23* | −.14 | −.03 | −.23* | .01 | ||
| 13. | Months since Death | −.14 | −.16 | .04 | .32* | .07 | .12 | −.02 | .19 | .07 | −.03 | — | .24** | |
| 14. | Years Ill | .17 | .21 | .16 | .19 | −.04 | −.14 | .08 | −.02 | .02 | .23 | — | .01 | −.05 |
Note. No other demographic characteristics were correlated with self-worth. For T2 variables, the total mother sample is 89 (45 bereaved, 44 controls) and the total father sample is 58 (31 bereaved, 27 controls).
p < .05,
p < .01,
p < .001.
Cross-Sectional Mediation Analysis
Cross-sectional serial mediation models were used to examine parental depressive symptoms and parent–child communication as potential mediators of the association between bereavement and child global self-worth (Figure 1A). No background characteristics were associated with T1 global self-worth; thus, no covariates were included.
Figure 1.
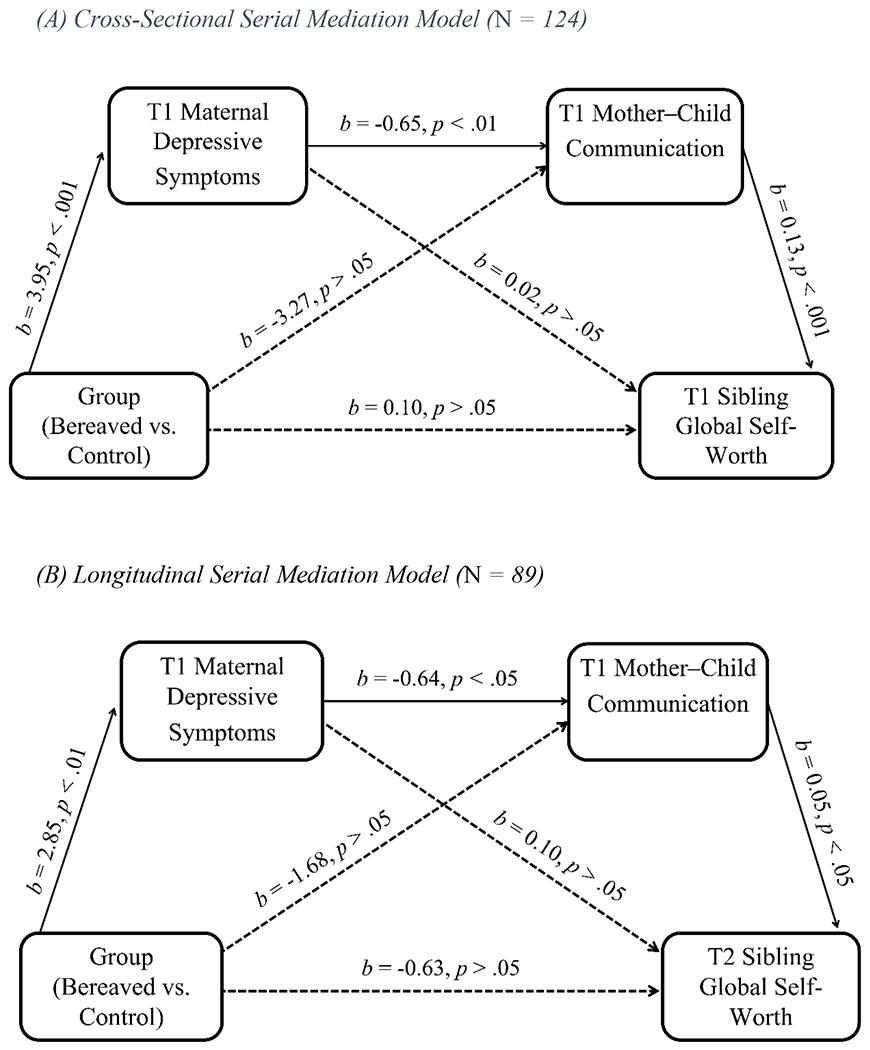
Note. For the model depicted in Figure 1B, T1 self-worth was included as a covariate. T1 self-worth was significantly associated with T2 self-worth (b = 0.47, p < .001).
The final mother model accounted for 20.6% of the variance in self-worth, F(3,120) = 10.38, p < .001, but there was no direct effect of group status on global self-worth. However, the indirect pathway of the effect of group status on global self-worth via maternal depressive symptoms and mother–child communication was significant (95% CI [−0.68, −0.08]). All individual paths were also significant (Figure 1A). Other possible indirect effects of group status on self-worth via one mediator were not significant. The father model accounted for 12.7% of the variance in self-worth, F(3,75) = 3.64, p = .02, but there were no direct or indirect effects of group status on global self-worth (CI: −0.11, 0.06). The only significant individual path was between father–child communication and self-worth (b = .09, p = .003).
Longitudinal Mediation Analysis
The significant cross-sectional model for the mother sample warranted investigation into whether maternal depressive symptoms and mother–child communication would continue to partially account for the variance in self-worth over time. Child age and T1 self-worth were associated with T2 global self-worth, but due to sample size, only T1 self-worth was included as a covariate to determine if this model could predict changes in self-worth over time. An additional sensitivity analysis including child age is reported below.
The final model explained 38.4% of the variance in T2 self-worth, F(4,84) = 13.07, p < .001, but there was no direct effect of group status on global self-worth. The indirect pathway of the effect of group status on T2 global self-worth via T1 maternal depressive symptoms and T1 mother–child communication was significant (95% CI [−0.35, −0.008]). All individual paths in the indirect pathway were significant (Figure 1B). Other possible indirect effects of group status on self-worth via one mediator were not significant.
Although our sample was too small to include additional covariates (Kline, 2015), we conducted a sensitivity analysis which included child age as a covariate due to a significant association with T2 self-worth. All significant individual paths remained significant, except for the path from mother–child communication to T2 self-worth. The indirect effect was no longer significant (95% CI [−0.33, 0.002]).
Discussion
The unique relationship with a sibling, as well as its loss, may significantly affect a child’s self-worth. In the context of pediatric cancer, the impact of this loss may be compounded by the changes and stressors experienced leading up to the death. Research with siblings bereaved by cancer has been limited, lacking prospective, controlled studies and exploration into self-concept as an outcome. Thus, we assessed the global self-worth of bereaved siblings and matched comparison classmates in the first two years after the death, while examining the indirect contributions of parental depressive symptoms and parent–child communication. We found that bereaved siblings reported similar levels of self-worth to comparison classmates. However, we identified family level risk factors (i.e., maternal depressive symptoms, poor quality mother–child communication) that predicted lower self-worth. This study adds to a small body of literature examining bereavement from a family systems perspective and highlights the importance of considering multiple family subsystems when seeking to understand bereavement experiences (Jiao, Chow, & Chen, 2021; Morris et al., 2016).
Literature suggests that bereaved parents are at increased risk for physical and mental health difficulties (October et al., 2018; A. Rosenberg et al., 2012). As expected, bereaved mothers reported significantly more depressive symptoms one year after the death than non-bereaved mothers, with over one-third reporting levels in the borderline or clinical range. Two years after the death, bereaved mothers still reported significantly more depressive symptoms than controls. Depression is of particular concern due to known negative impact on overall physical health, for which bereavement is already a known risk factor (Stroebe, Schut, & Stroebe, 2007). These findings are consistent with studies reporting increased risk of psychological distress in cancer-bereaved parents compared to non-bereaved parents (Kreicbergs, Valdimarsdóttir, Onelöv, Henter, & Steineck, 2004; Rasouli et al., 2021). However, consistent with previous studies within pediatric cancer (Kreicbergs et al., 2004) and perinatal populations (Vance et al., 1995), bereaved fathers reported comparable depressive symptoms to controls and overall lower levels than bereaved mothers. There could be several explanations for these findings, including that fathers may compartmentalize their grief more than mothers in effort to focus on readjusting to life after loss, or that fathers’ are socialized to minimize or deflect their own emotional grief response (Alam et al., 2012; McNeil et al., 2021).
Parent–child relationships and communication have been linked to self-worth (Jackson et al., 1998; Wouters et al., 2013). Our study aligned with these findings, as better communication with mothers and fathers was associated with greater self-worth, and although the T1 father model was nonsignificant, there was a significant effect of father–child communication on self-worth regardless of bereavement. Additionally, bereaved siblings reported significantly poorer quality of mother–child, but not father–child, communication than non-bereaved controls one and two years after the death. Poorer mother–child communication among cancer-bereaved families can partially be explained by increased depressive symptoms at both time points, as research suggests maternal depression can negatively impact mother–child communication in pediatric cancer populations (Rodriguez et al., 2013). Additionally, mothers may be more likely to take on the role of primary caregiver of the ill child, thus spending less time with the sibling and resulting in more prominent mother–child relationship changes after bereavement (Alam et al., 2012). Fathers, on the other hand, may take on the role of primary provider for the family, and also primary caretaker of siblings (Alam et al., 2012; Jones, Pelletier, Decker, Barczyk, & Dungan, 2010). After bereavement, it is possible that father–child communication patterns have changed less than that of mother and child, and thus may look less dissimilar from non-bereaved controls. Limited research has compared communication quality between bereaved siblings and controls, but there is evidence that despite being generally content with the frequency of communication, bereaved siblings still report avoiding discussions and restricting emotion-sharing about the deceased child out of respect for their parents (Wallin et al., 2016). This restriction of emotion-sharing may even commence during the deceased child’s illness trajectory (Pariseau et al., 2020). Thus, the quality of family communication may suffer if siblings are unable to be forthcoming with their feelings and negative emotions, resulting in mismatched perceptions of siblings’ well-being and the level of emotional support provided by parents (Pariseau et al., 2020). Our findings align with other studies that highlight the importance of a family systems perspective in understanding children’s bereavement processes. A recent review of families who lost a parent found that the surviving parent’s and child’s adjustment to the loss are interdependent and the parent can influence their child’s adjustment through parenting, communication, and coping strategies (Jiao et al., 2021).
Unexpectedly, bereaved siblings reported similar levels of global self-worth to controls. This finding contrasts with both cancer-focused and broader research, indicating lower self-worth or self-esteem in bereaved siblings relative to either non-bereaved controls or young adults grieving a close friend (Eilegård et al., 2013; Herberman Mash et al., 2013). However, it is difficult to compare to these findings due to the use of different constructs and measures, calling for more research to determine the most sensitive form of assessing self-concept in this population. Differences in the literature may also be explained by multiple trajectories of self-concept following bereavement (Hogan & Greenfield, 1991) and recently reported high levels of psychosocial adjustment in cancer-bereaved children (Hoffmann et al., 2018), implying resilience among cancer-bereaved siblings. Bereaved families with better adjusted siblings may also have been more willing to participate in this research, necessitating recruitment strategies to include families of varying levels of adjustment and tracking reasons for declining participation.
Although bereaved siblings reported similar levels of self-worth, serial mediation models provided some evidence of risk for lower self-worth. We found that bereaved mothers’ depressive symptoms may disrupt mother–child communication quality one year after the death, and negatively impact surviving siblings’ self-worth both one-year and two-years after the death (even when controlling for T1 self-worth in the longitudinal model). However, this was not true for the father model. These findings suggest that bereaved siblings whose mothers are experiencing high levels of depressive symptoms within the first year of the death may be more vulnerable to later decreases in global self-worth, partially due to disrupted communication quality. This aligns with a qualitative study of cancer-bereaved Japanese adolescents and young adults, which found that the surviving siblings’ perception of their mother’s response to the death was more impactful than the loss itself (Kamibeppu, Sato, & Hoshi, 2015). Similarly, a qualitative study in Hong Kong of young, bereaved siblings (5-11) found that the impact of bereavement on the sibling could result either from the parent’s grief, subsequent family interactions, the loss itself, or a combination. Consistent with family systems theory (Cox & Paley, 1997), the maternal grief response, and subsequent changes to the mother–child relationship (e.g., communication), may have a greater impact on siblings’ global self-worth than the child’s death. Evidence of this can also be found in studies showing that parental grief responses, mental health problems, and communication style are linked to bereaved siblings’ and children’s psychosocial adjustment (Barrera et al., 2013; Jiao et al., 2021; Morris et al., 2016; A. Rosenberg et al., 2015; Wallin et al., 2016). Notably, this study offers a comparison group, emphasizing the role of child/sibling loss over and above non-bereaved levels of maternal depression on child self-worth.
The findings of this study should be considered in the context of several limitations. Despite a larger sample size in the original study, the current paper included a smaller subset and therefore we could not run longitudinal models with father data or properly control for all potentially confounding variables (i.e., child age) in the mother sample. It is possible that with a larger sample and controlling for child age, the mother longitudinal model would no longer be significant, as shown in the sensitivity analysis. Our study recruited families within the first year of bereavement to prospectively explore the immediate impact on families, but this may have influenced recruitment and retention rates due to families being in an earlier stage of grief. Future research on paternal influences in the context of bereavement in pediatric cancer would benefit from longitudinal follow-up further from the child’s death, to examine whether paternal grief reactions persist over time. Although these families are a vulnerable population and are difficult to recruit, low retention rates in the current study may influence the validity of our findings. We did not find significant differences among participants who did not complete a second home visit, but future research is needed to replicate our findings. Additionally, data for this study was collected before the Covid-19 pandemic, thus results may not be generalizable to families more recently bereaved. However, this study is important given the paucity of literature on the topic. Results may not be generalizable to siblings bereaved by other causes, who lost other loved ones, or who are from racially/ethnically diverse groups. It is important to note that although our sample is generally representative of the families of children with cancer at the participating institutions, more research is needed to understand cultural differences in the grieving process. Factors such as parental depression, the parent–child relationship, and parent–child communication may operate differently to impact self-worth in other cultures, requiring culturally responsive interventions.
Despite these limitations, this is, to our knowledge, the first longitudinal, multi-informant, controlled study of siblings bereaved by cancer examining the indirect impact of parental depressive symptoms and parent–child communication on sibling global self-worth through a family systems perspective. Our findings suggest that although bereaved siblings appear resilient and comparable to peers in terms of self-worth, maternal grief responses and subsequent changes to the mother–child relationship may impact cancer-bereaved siblings’ adjustment over time, whereas further examination into paternal factors is warranted. Improving social supports for parents, especially mothers, is recommended as they are likely to experience high levels of depressive symptoms. Screening for depression as part of family bereavement services either before death or soon after may facilitate linkage with psychological support services and earlier mitigation of symptoms. It should be noted that fathers’ grief is not yet fully understood and while they may also benefit from this type of support, mothers and fathers may need different approaches given differences in grief expression. Additionally, bereaved siblings may benefit from multiple sources of support since grieving parents may be unable to meet their needs. Clinicians might consider evidence-based interventions (Dias et al., 2019; Ridley & Frache, 2020), specifically family interventions targeting strategies to improve and maintain parent–child communication quality throughout bereavement to help support siblings and enhance their self-worth and adjustment over time.
Acknowledgments
We have no known conflict of interest to disclose. We report how we determined our sample size, all data exclusions, all manipulations, and all measures in the study, and we follow TOP (Nosek et al., 2015) and JARS (Appelbaum et al., 2018). Materials and analysis code for this study are available upon request to the senior author, Dr. Cynthia Gerhardt. This study was not pre-registered. This data was presented at the 2021 Nationwide Children’s Hospital Annual Research Retreat and the 2022 Society of Pediatric Psychology Annual Conference. This study was funded by the National Cancer Institute (R01 CA09821), as well as by intramural support from Nationwide Children’s Hospital and Cincinnati Children’s Hospital Medical Center. The corresponding author was funded by a National Cancer Institute Diversity Supplement (R01 CA248103-01A1W2). We would like to thank the families who participated in our work.
References
- Achenbach TM, & Rescorla L (2003). Manual for the ASEBA adult forms & profiles. In: Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Alam R, Barrera M, D’Agostino N, Nicholas DB, & Schneiderman G (2012). Bereavement experiences of mothers and fathers over time after the death of a child due to cancer. Death studies, 36(1), 1–22. [DOI] [PubMed] [Google Scholar]
- Appelbaum M, Cooper H, Kline R, Mayo-Wilson E, Nezu A, & Rao S (2018). Journal article reporting standards for quantitative research in psychology: The APA Publications and Communications Board task force report. American Psychologist, 73(1), 3. [DOI] [PubMed] [Google Scholar]
- ASEBA. (2022). Adults (ABCL, ASR). Retrieved from https://aseba.org/adults/
- Barnes HL, & Olson DH (1985). Parent-adolescent communication and the circumplex model. Child development, 438–447. [Google Scholar]
- Barrera M, Alam R, D’Agostino NM, Nicholas DB, & Schneiderman G (2013). Parental perceptions of siblings’ grieving after a childhood cancer death: A longitudinal study. Death studies, 37(1), 25–46. [DOI] [PubMed] [Google Scholar]
- Birkeland MS, Melkevik O, Holsen I, & Wold B (2012). Trajectories of global self-esteem development during adolescence. Journal of Adolescence, 35(1), 43–54. [DOI] [PubMed] [Google Scholar]
- Birndorf S, Ryan S, Auinger P, & Aten M (2005). High self-esteem among adolescents: Longitudinal trends, sex differences, and protective factors. Journal of Adolescent Health, 37(3), 194–201. [DOI] [PubMed] [Google Scholar]
- Bolton JM, Au W, Chateau D, Walld R, Leslie WD, Enns J, … Sareen J. (2016). Bereavement after sibling death: a population-based longitudinal case-control study. World Psychiatry, 15(1), 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branje S, Laursen B, & Collins WA (2012). Parent–child communication during adolescence. In The Routledge handbook of family communication (pp. 283–298): Routledge. [Google Scholar]
- Chii CY, Seok CB, & Sombuling A (2016). Perception of parent and peer attachment and global self-worth: Preliminary data in adolescents.
- Cox M, & Paley B (1997). Families as systems. Annual review of psychology, 48(1), 243–267. [DOI] [PubMed] [Google Scholar]
- Decinque N, Monterosso L, Dadd G, Sidhu R, Macpherson R, & Aoun S (2006). Bereavement support for families following the death of a child from cancer: experience of bereaved parents. Journal of psychosocial oncology, 24(2), 65–83. [DOI] [PubMed] [Google Scholar]
- Dias N, Hendricks-Ferguson V, Wei H, Boring E, Sewell K, & Haase J (2019). A systematic literature review of the current state of knowledge related to interventions for bereaved parents. American Journal of Hospice and Palliative Medicine®, 36(12), 1124–1133. [DOI] [PubMed] [Google Scholar]
- Dumont É, Bourque CJ, Duval M, Payot A, Sultan S, & Team BPR (2022). A portrait of self-reported health and distress in parents whose child died of cancer. OMEGA-Journal of Death and Dying, 85(4), 958–973. [DOI] [PubMed] [Google Scholar]
- Eilegård A, Steineck G, Nyberg T, & Kreicbergs U (2013). Psychological health in siblings who lost a brother or sister to cancer 2 to 9 years earlier. Psycho-Oncology, 22(3), 683–691. [DOI] [PubMed] [Google Scholar]
- Eilertsen M-EB, Lövgren M, Wallin AE, & Kreicbergs U (2018). Cancer-bereaved siblings’ positive and negative memories and experiences of illness and death: A nationwide follow-up. Palliative & supportive care, 16(4), 406–413. [DOI] [PubMed] [Google Scholar]
- Ferro MA, & Tang J (2017). Psychometric properties of the self-perception profile for children in children with chronic illness. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 26(2), 119. [PMC free article] [PubMed] [Google Scholar]
- Foster TL, Gilmer MJ, Vannatta K, Barrera M, Davies B, Dietrich MS, … Gerhardt CA (2012). Changes in siblings after the death of a child from cancer. Cancer nursing, 35(5), 347–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gecas V. (1982). The self-concept. Annual review of sociology, 1–33. [Google Scholar]
- Gerhardt CA, Fairclough DL, Grossenbacher J, Barrera M, Jo Gilmer M, Foster TL, … Vannatta K (2012). Peer relationships of bereaved siblings and comparison classmates after a child’s death from cancer. Journal of Pediatric Psychology, 37(2), 209–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley AW, & Garland EL (2017). Clarity of mind: Structural equation modeling of associations between dispositional mindfulness, self-concept clarity and psychological well-being. Personality and Individual differences, 106, 334–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harter S. (1985). Self-perception profile for children. Hispanic Journal of Behavioral Sciences. [Google Scholar]
- Harter S. (1987). The determinants and mediational role of global self-worth in children. Contemporary topics in developmental psychology. [Google Scholar]
- Hayes AF (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. In: University of Kansas, KS. [Google Scholar]
- Heaven PC (1997). Perceptions of family influences, self-esteem and psychoticism: a two-year longitudinal analysis. Personality and Individual differences, 23(4), 569–574. [Google Scholar]
- Herberman Mash HB, Fullerton CS, & Ursano RJ (2013). Complicated grief and bereavement in young adults following close friend and sibling loss. Depression and anxiety, 30(12), 1202–1210. [DOI] [PubMed] [Google Scholar]
- Hoffmann R, Kaiser J, & Kersting A (2018). Psychosocial outcomes in cancer-bereaved children and adolescents: a systematic review. Psycho-Oncology, 27(10), 2327–2338. [DOI] [PubMed] [Google Scholar]
- Hogan NS, & Greenfield DB (1991). Adolescent sibling bereavement symptomatology in a large community sample. Journal of Adolescent Research, 6( 1), 97–112. [Google Scholar]
- Howard Sharp KM, Meadows EA, Keim MC, Winning AM, Barrera M, Gilmer MJ, … Davies B (2020). The influence of parent distress and parenting on bereaved siblings’ externalizing problems. Journal of Child and Family Studies, 29(4), 1081–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe N, Paine AL, Ross HS, & Recchia H (2022). Sibling relations in early and middle childhood. The Wiley-Blackwell handbook of childhood social development, 443–458. [Google Scholar]
- Jackson S, Bijstra J, Oostra L, & Bosma H (1998). Adolescents’ perceptions of communication with parents relative to specific aspects of relationships with parents and personal development. Journal of Adolescence, 21(3), 305–322. [DOI] [PubMed] [Google Scholar]
- Jiao K, Chow A, & Chen C (2021). Dyadic relationships between a surviving parent and children in widowed families: A systematic scoping review. Family process, 60(3), 888–903. [DOI] [PubMed] [Google Scholar]
- Jones BL, Pelletier W, Decker C, Barczyk A, & Dungan SS (2010). Fathers of children with cancer: A descriptive synthesis of the literature. Social Work in Health Care, 49(5), 458–493. [DOI] [PubMed] [Google Scholar]
- Kamibeppu K, Sato I, & Hoshi Y (2015). The experience of Japanese adolescents and young adults after losing siblings to childhood cancer: Three types of narratives. Journal of Pediatric Oncology Nursing, 32(3), 165–177. [DOI] [PubMed] [Google Scholar]
- Kapke TL, Grace MA, Gerdes AC, & Lawton KE (2017). Latino early adolescent mental health: Examining the impact of family functioning, familism, and global self-worth. Journal of Latina/o Psychology, 5(1), 27. [Google Scholar]
- Kline RB (2015). Principles and practice of structural equation modeling: Guilford publications. [Google Scholar]
- Kramer L (2014). Learning emotional understanding and emotion regulation through sibling interaction. Early Education and Development, 25(2), 160–184. [Google Scholar]
- Kreicbergs U, Valdimarsdóttir U, Onelöv E, Henter J-I, & Steineck G (2004). Anxiety and depression in parents 4–9 years after the loss of a child owing to a malignancy: a population-based follow-up. Psychological medicine, 34(8), 1431–1441. [DOI] [PubMed] [Google Scholar]
- Lövgren M, Jalmsell L, Eilegård Wallin A, Steineck G, & Kreicbergs U (2016). Siblings’ experiences of their brother’s or sister’s cancer death: a nationwide follow-up 2–9 years later. Psycho-Oncology, 25(4), 435–440. [DOI] [PubMed] [Google Scholar]
- Markus H, & Wurf E (1987). The dynamic self-concept: A social psychological perspective. Annual review of psychology, 38(1), 299–337. [Google Scholar]
- McNeil MJ, Baker JN, Snyder I, Rosenberg AR, & Kaye EC (2021). Grief and bereavement in fathers after the death of a child: a systematic review. Pediatrics, 147(4). [DOI] [PubMed] [Google Scholar]
- Mertens AC, Liu Q, Neglia JP, Wasilewski K, Leisenring W, Armstrong GT, … Yasui Y (2008). Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. Journal of the National Cancer Institute, 100(19), 1368–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael SP, & Lansdown R (1986). Adjustment to the death of a sibling. Archives of disease in childhood, 61(3), 278–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris A, Gabert-Quillen C, Friebert S, Carst N, & Delahanty D (2016). The indirect effect of positive parenting on the relationship between parent and sibling bereavement outcomes after the death of a child. Journal of pain and symptom management, 51(1), 60–70. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute, N. I. o. H. (2022, August 19, 2022). Childhood Cancers. Retrieved from https://www.cancer.gov/types/childhood-cancers
- Nolbris M, & Hellström A-L (2005). Siblings’ needs and issues when a brother or sister dies of cancer. Journal of Pediatric Oncology Nursing, 22(4), 227–233. [DOI] [PubMed] [Google Scholar]
- Nosek B, Alter G, Banks G, Borsboom D, Bowman S, Breckler S, … Christensen G (2015). Promoting an open research culture. Science, 348(6242), 1422–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor K, & Barrera M (2014). Changes in parental self-identity following the death of a child to cancer. Death studies, 38(6), 404–411. [DOI] [PubMed] [Google Scholar]
- October T, Dryden-Palmer K, Copnell B, & Meert KL (2018). Caring for parents after the death of a child. Pediatric critical care medicine: a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies, 18(8), S61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packman W, Horsley H, Davies B, & Kramer R (2006). Sibling bereavement and continuing bonds. Death studies, 30(9), 817–841. [DOI] [PubMed] [Google Scholar]
- Pariseau EM, Chevalier L, Muriel AC, & Long KA (2020). Parental awareness of sibling adjustment: Perspectives of parents and siblings of children with cancer. Journal of Family Psychology, 34(6), 698. [DOI] [PubMed] [Google Scholar]
- Park J. (2006). The Impact of adolescent self-concept on psychological health, self-perceived. The concept of self in medicine and health care, 97. [Google Scholar]
- Pohlkamp L, Kreicbergs U, & Sveen J (2019). Bereaved mothers’ and fathers’ prolonged grief and psychological health 1 to 5 years after loss—A nationwide study. Psycho-Oncology, 28(7), 1530–1536. [DOI] [PubMed] [Google Scholar]
- Rasouli O, Bø MA, Reinfjell T, Moksnes UK, & Eilertsen M-EB (2021). Protective and risk factors associated with psychological distress in cancer-bereaved parents: A cross-sectional study. European Journal of Oncology Nursing, 51, 101929. [DOI] [PubMed] [Google Scholar]
- Ridley A, & Frache S (2020). Bereavement care interventions for children under the age of 18 following the death of a sibling: a systematic review. Palliative Medicine, 34(10), 1340–1350. [DOI] [PubMed] [Google Scholar]
- Rodriguez EM, Dunn MJ, Zuckerman T, Hughart L, Vannatta K, Gerhardt CA, … Compas BE (2013). Mother–child communication and maternal depressive symptoms in families of children with cancer: Integrating macro and micro levels of analysis. Journal of Pediatric Psychology, 38(7), 732–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg A, Baker KS, Syrjala K, & Wolfe J (2012). Systematic review of psychosocial morbidities among bereaved parents of children with cancer. Pediatric blood & cancer, 58(4), 503–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg A, Postier A, Osenga K, Kreicbergs U, Neville B, Dussel V, & Wolfe J (2015). Long-term psychosocial outcomes among bereaved siblings of children with cancer. Journal of pain and symptom management, 49(1), 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M. (1979). Conceiving the self. In Conceiving the self(pp. 318–318). [Google Scholar]
- Sowislo JF, & Orth U (2013). Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological bulletin, 139(1), 213. [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H, & Stroebe W (2007). Health outcomes of bereavement. The Lancet, 370(9603), 1960–1973. [DOI] [PubMed] [Google Scholar]
- The American Cancer Society, M. a. E. C. T. (2022, January 12, 2022). Key Statistics for Childhood Cancers. Retrieved from https://www.cancer.org/cancer/cancer-in-children/key-statistics.html [Google Scholar]
- Thoits PA (2013). Self, identity, stress, and mental health. Handbook of the sociology of mental health, 357–377. [Google Scholar]
- Van Dijk M, Branje S, Keijsers L, Hawk S, Hale W, & Meeus W (2014). Self-concept clarity across adolescence: Longitudinal associations with open communication with parents and internalizing symptoms. Journal of youth and adolescence, 43, 1861–1876. [DOI] [PubMed] [Google Scholar]
- Vance JC, Najman JM, Thearle MJ, Embelton G, Foster W, & Boyle FM (1995). Psychological changes in parents eight months after the loss of an infant from stillbirth, neonatal death, or sudden infant death syndrome—a longitudinal study. Pediatrics, 96(5), 933–938. [PubMed] [Google Scholar]
- Wallin AE, Steineck G, Nyberg T, & Kreicbergs U (2016). Insufficient communication and anxiety in cancer-bereaved siblings: A nationwide long-term follow-up. Palliative & Supportive Care, 14(5), 488–494. doi: 10.1017/S1478951515001273 [DOI] [PubMed] [Google Scholar]
- Wouters S, Doumen S, Germeijs V, Colpin H, & Verschueren K (2013). Contingencies of self-worth in early adolescence: The antecedent role of perceived parenting. Social Development, 22(2), 242–258. [Google Scholar]
- Yang H-C, Mu P-F, Sheng C-C, Chen Y-W, & Hung G-Y (2016). A systematic review of the experiences of siblings of children with cancer. Cancer nursing, 39(3), E12–E21. [DOI] [PubMed] [Google Scholar]
- Youngblut JM, Brooten D, Cantwell GP, del Moral T, & Totapally B (2013). Parent health and functioning 13 months after infant or child NICU/PICU death. Pediatrics, 132(5), e1295–e1301. [DOI] [PMC free article] [PubMed] [Google Scholar]


