Abstract
Objective:
To investigate the incidence of women with breast implants in 1964–2017
Patients and Methods:
All women with breast implants in Olmsted County, MN between January 1, 1992 and December 31, 2017 were identified, and a comprehensive review of individual medical records was performed, adding to a previously identified cohort of women with breast implants in 1964–1991. Incidence rates were calculated and were age- and sex-adjusted to the US white female 2010 population.
Results:
In 1992–2017, 948 women with breast implants were identified, totaling 1696 Olmsted County, MN women with breast implants in 1964–2017. Overall incidence was 63.3 (60.2, 66.4) per 100,000 women, but incidence varied significantly over time. Women in 1964–1991 were more likely to have implants for cosmetic reasons and more likely to have silicone implants compared to the 1992–2017 cohort. The overall standardized mortality rate was 1.17 (95% CI 0.99–1.38) in 1964–1991 and 0.94 (95% CI 0.66–1.29) in 1992–2017. In 1992–2017, breast reconstruction patients had a significantly elevated risk of implant rupture and implant removal versus breast augmentation patients.
Conclusion:
The incidence of breast implants among women in Olmsted County, MN has varied drastically over the past five decades, with significant changes in the trends for implant type and reason. The findings of this study may provide further insight regarding how risks associated with implants may vary over time.
Introduction
Despite 60 years of breast implant availability in the US, the epidemiology of breast implants has not been well examined and remains poorly understood overall. Only a handful of studies have attempted to estimate the prevalence of women with breast implants, all conducted prior to the 1992 Food and drug Administration (FDA) moratorium restricting silicone implant use [1–3]. In the modern era, most available data regarding breast implants comes from annual statistics reports of the American Society of Plastic Surgeons (ASPS) [4]. While these reports provide insight into the number of breast procedures performed each year, they are insufficient for deriving meaningful epidemiological data. In addition, no published study has attempted to estimate the incidence of breast implants among US women nor have previous reports been able to clearly elucidate how the trends in reason for breast implant or implant type have varied over time. Therefore, the purpose of this population-based cohort study is to address this gap by examining the incidence of breast implants from 1964 to 2017, considering essentially the entire period of breast implant availability in the US. In addition, this study assesses how trends in breast implant type and reason have shifted over time, as well as how this relates to rupture, removal, and mortality outcomes.
Materials and Methods
Data Source
The population of Olmsted County, Minnesota serves as an excellent data source for investigating the epidemiology of breast implants due to the resources of the Rochester Epidemiology Project (REP). REP is a centralized medical record linkage system that provides ready access to records from all health care providers in the local area, uniquely enabling long-term population-based studies [5]. Institutional review board approval from Mayo Clinic and Olmsted Medical Center was obtained for this study.
Study population
All individuals with a breast implant procedure or diagnosis code between January 1, 1991 and September 30, 2018 were identified. Medical records were then individually reviewed, and patients with first-time implants placed between January 1, 1992 and December 31, 2017 were included in the study. Those who were not residents of Olmsted County, MN at the time of implant placement were excluded.
Implant type was classified as silicone, saline, or combined (i.e., dual-lumen implants with silicone and saline). Reason for implant was classified as cosmetic (e.g., breast hypoplasia, congenital breast asymmetry), breast cancer, prophylactic, or other/unknown. For patients who had more than one breast implant procedure, implant type and reason were classified in accordance with the first breast implantation.
This 1992–2017 cohort extended a previously identified cohort of Olmsted County, MN women with breast implants in January 1, 1964 to December 31, 1991 [6]. Combined implants were included in the silicone category for this cohort. Women in both cohorts were followed until death, migration, or last medical record. Throughout the manuscript, “women” refers to individuals assigned female at birth.
Statistical analysis
Descriptive statistics were used to summarize the data. Chi-square and rank sum tests were used to compare characteristics between time periods. Age- and sex-specific incidence rates were calculated using the number of incident breast implantations as the numerator and REP census population counts as the denominator, adjusted to the US white female 2010 population. To calculate 95% confidence intervals (CI), it was assumed incidence followed a Poisson distribution. Poisson regression models with smoothing splines were used to estimate trends in implant incidence over time. Annual incidence rates were illustrated using 3-year centered, moving averages.
Mortality risk was determined using the Kaplan-Meier method. Standardized mortality ratios (SMR) and 95% CI were computed by comparing the observed number of deaths to the expected mortality for women of the same age and calendar year using Minnesota life tables. For the 1992–2017 cohort, cumulative incidence of first implant rupture and first implant removal were calculated (by individual, not by implant), adjusting for the competing risk of death and implant removal (rupture analysis only). Associations between implant ruptures and removals with implant reason, type, age, and calendar year were assessed using Cox proportional hazard models. Analyses were performed using SAS version 9.4 and R version 4.0.3 (R Foundation for Statistical Computing).
Results
A total of 951 individuals with breast implants in 1992–2017 were identified. Of these individuals, three were assigned male at birth and were omitted. Adding to the 748 women in 1964–1991, a total of 1696 Olmsted County, MN women were identified with a confirmed breast implantation in 1964–2017.
Table 1 shows the baseline characteristics of women with breast implants. Women with breast augmentations were notably younger than women with implant-based reconstructions (IBR) for cancer or prophylaxis (cosmetic (mean, SD): 32.5±8.0 years; cancer: 50.6±10.6 years; prophylactic: 41.9±9.5 years). Women in both cohorts were more likely to have silicone implants and implants for cosmetic reasons, but this trend was less pronounced in later decades (1964–1991: 84.5% silicone/combined, 71.0% cosmetic; 1992–2017: 57.5% silicone/combined, 53.6% cosmetic). Among women with breast augmentations in 1992–2017, implants were predominantly saline (65.9%), in comparison to those with IBRs during the same period, where most implants were silicone only (cancer: 77.1%; prophylactic: 68.4%). In addition, 79% of IBR patients underwent two-stage reconstructions utilizing tissue expanders, with increased use of tissue expanders in the latter half of the study period (45% in 1992–2004 vs. 88% in 2005–2017).
Table 1.
Characteristics of Olmsted County, MN women with breast implants in 1964–2017
| 1964–1991 (n=748) | 1992–2017 (n=948) | 1964–2017 (n=1696) | p value | |
|---|---|---|---|---|
| Race/ethnicity, n (%) | <0.001a | |||
| American Indian | 3 (0.4) | 3 (0.3) | 6 (0.4) | |
| Asian/Hawaiian/Pacific Island | 9 (1.2) | 45 (4.8) | 54 (3.2) | |
| Black | 0 (0.0) | 8 (0.9) | 8 (0.5) | |
| Hispanic/Latino | 10 (1.4) | 30 (3.2) | 40 (2.4) | |
| White | 710 (96.9) | 821 (88.1) | 1531 (92.0) | |
| Other/Mixed | 1 (0.1) | 25 (2.7) | 26 (1.6) | |
| Unknown | 15 | 16 | 31 | |
| Age at implant (years), mean (SD) | ||||
| All women | 34.9 (10.5) | 41.4 (12.4) | 38.5 (12.0) | <0.001a |
| Cosmetic | 30.8 (6.9) | 34.3 (8.7) | 32.5 (8.0) | <0.001a |
| Cancer | 49.1 (11.0) | 51.2 (10.3) | 50.6 (10.6) | 0.066a |
| Prophylactic | 39.7 (7.7) | 43.9 (10.5) | 41.9 (9.5) | 0.007a |
| Type of implant, n (%) | <0.001b | |||
| Saline | 116 (15.5) | 398 (42.5) | 514 (30.5) | |
| Silicone/Combinedc | 632 (84.5) | 539 (57.5) | 1171 (69.5) | |
| Missing | 0 | 11 | 11 | |
| Reason for implant, n (%) | <0.001b | |||
| Cosmetic | 531 (71.0) | 508 (53.6) | 1039 (61.3) | |
| Cancer | 125 (16.7) | 339 (35.8) | 464 (27.4) | |
| Prophylactic | 92 (12.3) | 99 (10.4) | 191 (11.3) | |
| Other / Unknown | 0 (0.0) | 2 (0.2) | 2 (0.1) |
Kruskal-Wallis p-value
Chi-Square p-value
Includes silicone only and combined implant types. In 1964–1991, these were collected as a single category. In 1992–2017, these were collected separately (498 silicone only and 41 combined).
Incidence of breast implants
The overall incidence of breast implants in 1964–2017 was 63.3 (95% CI 60.2–66.4) per 100,000 women (age-adjusted to US white female 2010 population). Incidence was highest in women aged 25–34 years (117.2 per 100,000) (Table 2). Incidence of breast implants peaked in the late 1970’s and 1980’s before dropping rapidly in the 1990’s (Figure 1a). Rates remained low until the early 2000’s when incidence steadily increased before plateauing around 2005, staying fairly consistent through the end of the study.
Table 2.
Age-specific incidence rates of Olmsted County, MN women with breast implants in 1964–2017
| Age | N | Incidence per 100,000 (95% CI) |
|---|---|---|
| 14–24 | 167 | 30.4 |
| 25–34 | 615 | 117.2 |
| 35–44 | 444 | 103.5 |
| 45–54 | 289 | 79.3 |
| 55–64 | 130 | 47.0 |
| 65–74 | 43 | 22.2 |
| 75–84 | 8 | 6.1 |
| 85+ | 0 | 0.0 |
| Total | 1696 | 63.3a (60.2, 66.4) |
Age-adjusted to US white female 2010 population
Figure 1.
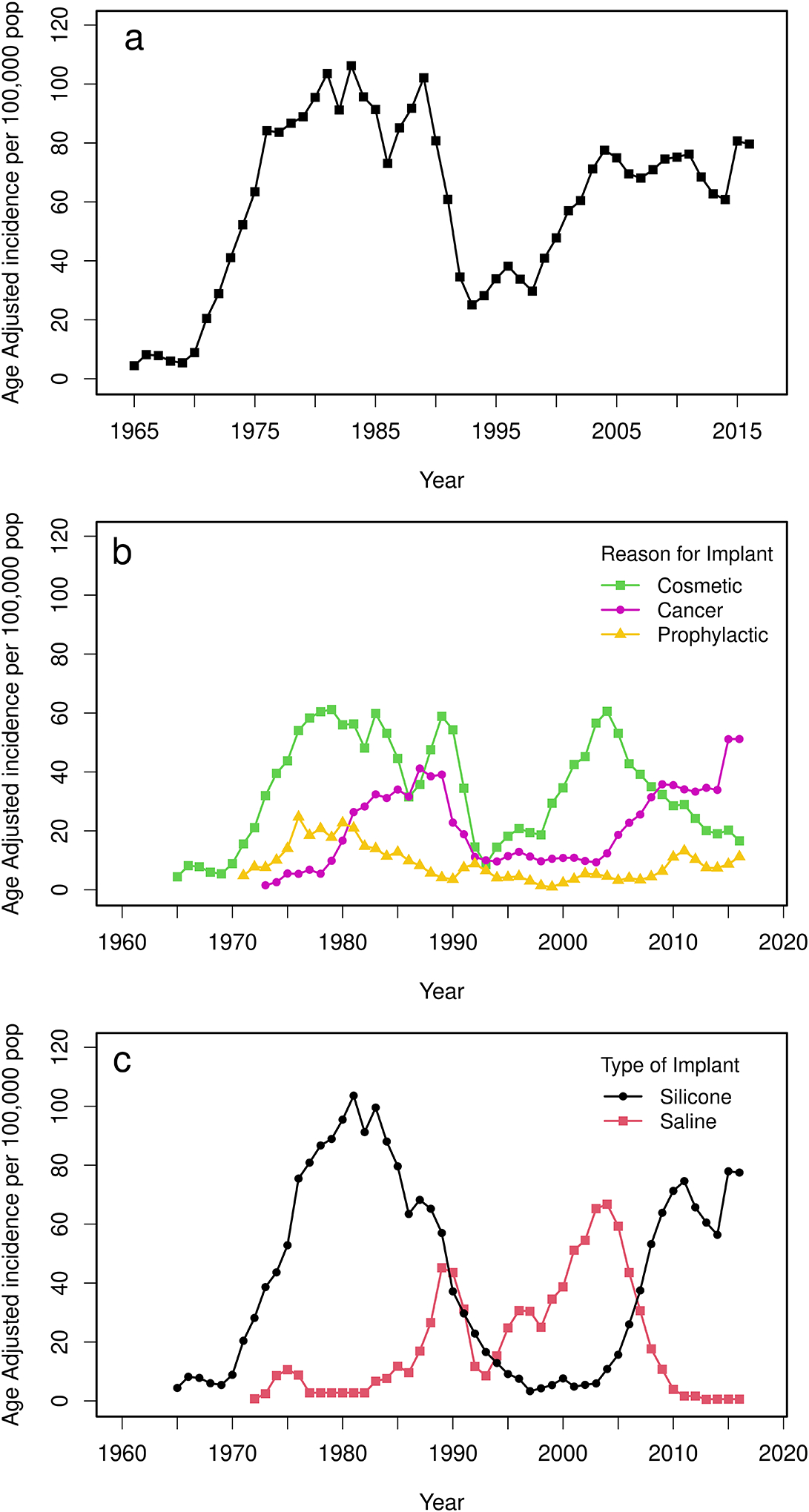
Trends in age-adjusted breast implant incidence over time (a), by reason for implant (b), and type of implant (c). Silicone group includes silicone only and combined implant types.
Incidence of breast implants by implant reason
The earliest cases of breast implantation in our study (1960’s) were for cosmetic reasons, with incidence increasing year after year for nearly a decade after 1970 (Figure 1b). Around 1979, just as cosmetic implants reached an all-time high, the incidence of implants for cancer began climbing for the first time, eventually peaking and briefly overtaking as the top reason for implants around 1987. At the end of the 1964–1991 cohort, both cosmetic and cancer implant rates dropped rapidly, reaching extreme lows by 1993. However, the incidence of cosmetic implants recovered soon after, while implants for cancer remained low for over a decade. Around 2005, trends shifted once again as breast augmentations began decreasing and implants for cancer began increasing, eventually converging in 2008–2009. Since then, cancer remained the top reason for breast implants with increased margins over time, while the incidence of cosmetic implants continued to drop, reaching the lowest rates in over 20 years by the end of the study. Apart from the 1970’s, implants for prophylaxis remained the least common reason for breast implantation.
Incidence of breast implants by implant type
Silicone implants were more popular than saline implants throughout 1964–1991 (Figure 1c); incidence grew rapidly in the 1970’s, peaking around 1980, but fell only a few years later. As the popularity of silicone implants waned, the incidence of saline implants grew, briefly surpassing silicone around 1990. However, rates for both types dropped soon thereafter. Saline use recovered quickly, overtaking as the top implant type for many years, before declining again around 2005. Around this time, silicone incidence, which had been significantly low for over a decade, began increasing and once again became the more popular implant type around 2007. Silicone use remained high through the end of the study, while saline use continued to drop, maintaining near-zero levels since 2010. In 2010–2017, only 4 women received saline implants.
Risk of mortality
The overall SMR for women with breast implants was 1.12 (95% CI 0.96–1.29) (Table 3). Mortality risk was slightly greater in 1964–1991 vs. 1992–2017 (SMR 1.17, 95% CI 0.99–1.38 vs. SMR 0.94, 95% CI 0.66–1.29), with a notably elevated risk among women who had implants for cancer in the earlier cohort vs. the later cohort (SMR 2.01, 95% CI 1.59–2.51 vs. SMR 1.17, 95% CI 0.78–1.68). Cosmetic and prophylactic implant patients exhibited decreased mortality risks in both cohorts, particularly in 1992–2017 (cosmetic: SMR 0.66, 95% CI 0.27–1.36; prophylactic: SMR 0.40, 95% CI 0.05–1.45).
Table 3.
Risk of mortality among Olmsted County, MN women with breast implants
| 1964–1991 (n=748) | 1992–2017 (n=948) | 1964–2017 (n=1696) | |
|---|---|---|---|
| Length of follow up (years), median (IQR) | 30.8 (10.5, 37.0) | 10.8 (5.7, 16.3) | 14.4 (6.3, 30.0) |
| Number of deaths, O/E | 148 / 126 | 38 / 41 | 186 / 167 |
| SMR (95% CI) | 1.17 (0.99, 1.38) | 0.94 (0.66, 1.29) | 1.12 (0.96, 1.29) |
| Cosmetic, O/E | 45 / 57 | 7 / 11 | 52 / 68 |
| SMR (95% CI) | 0.79 (0.57, 1.05) | 0.66 (0.27, 1.36) | 0.77 (0.57, 1.01) |
| Cancer, O/E | 79 / 39 | 29 / 25 | 108 / 64 |
| SMR (95% CI) | 2.01 (1.59, 2.51) | 1.17 (0.78, 1.68) | 1.69 (1.38, 2.03) |
| Prophylactic, O/E | 24 / 30 | 2 / 5 | 26 / 35 |
| SMR (95% CI) | 0.81 (0.52, 1.20) | 0.40 (0.05, 1.45) | 0.75 (0.49, 1.10) |
O/E, observed number of deaths / expected number of deaths; SMR, standardized mortality ratio
Risk of first implant rupture
In 1992–2017, risk of first implant rupture increased from 3.1% (95% CI 2.2–4.6) at 5 years to 15.9% (95% CI 12.1–20.8) at 20 years post-implant. IBR patients had a significantly elevated rupture risk vs. breast augmentation patients (cancer: hazard ratio [HR] 3.25, 95% CI 1.55–6.81; prophylactic: HR 3.99, 95% CI 1.86–8.53). Rupture risk for cancer and prophylactic patients at 15 years was 18.7% (95% CI 12.8–27.4) and 23.5% (95% CI 13.8–40.0), respectively, compared to 6.3% (95% CI 4.3–9.4) for cosmetic implants (Figure 2a). Risk of rupture by implant type did not reach significance (p=0.92); risk at 15 years was 9.6% (95% CI 7.0–13.2) for saline, 14.5% (95% CI 7.5–28.1) for silicone, and 38.6% (95% CI 25.9–57.6) for combined (Figure 2b). There were no associations between rupture risk and calendar year or age at implant.
Figure 2.
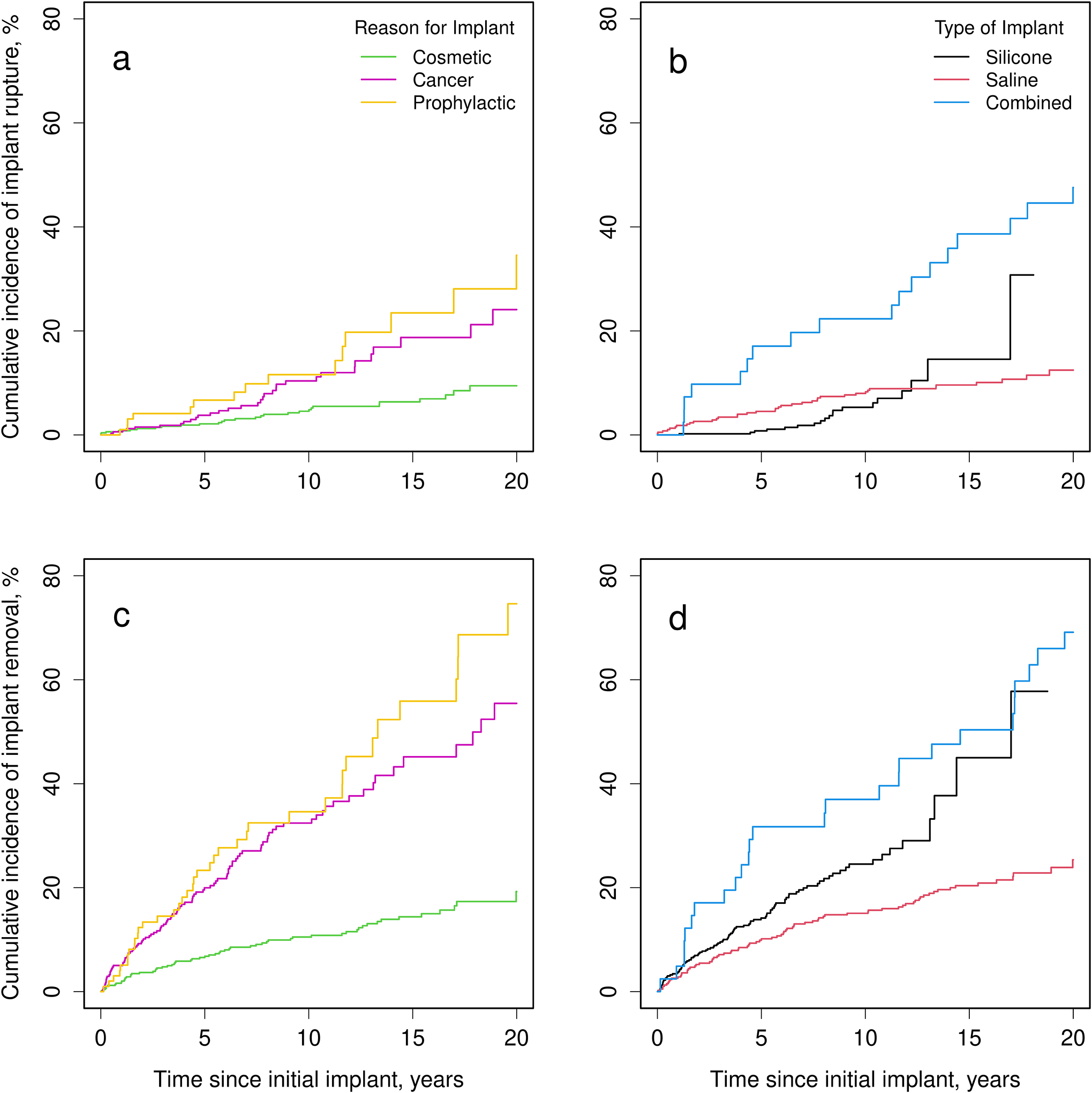
Cumulative incidence of first implant rupture by implant reason (a) and by implant type (b) in 1992–2017. Cumulative incidence of first implant removal by implant reason (c) and by implant type (d) in 1992–2017. Incidence for combined implants is shown separately; silicone incidence includes silicone implants only.
Risk of first implant removal
Of the 948 implant patients in 1992–2017, 209 had their first implant(s) removed during the available follow-up period, with 67% undergoing immediate implant exchange, 11% undergoing delayed implant replacement, and 22% opting for no implant replacement following removal. Risk of first implant removal increased from 13.2% (95% CI 11.1–15.6) at 5 years to 35.3% (95% CI 30.3–41.2) at 20 years post-implant, with a significantly increased risk among IBR patients vs. augmentation patients (cancer: HR 3.38, 95% CI 2.19–5.24, p<.001); prophylactic: HR 4.26, 95% CI 2.68–6.76, p<.001). Removal risk for cancer and prophylactic patients at 15 years was 45.2% (95% CI 37.3–54.7) and 55.9% (95% CI 42.6–73.2), respectively, compared to 14.4% (95% CI 11.2–18.5) for cosmetic patients (Figure 2c). Risk of removal was not significantly different across implant types (p=0.78). Risk of removal at 15 years was 20.4% (95% CI 16.5–25.2) for saline, 45.0% (95% CI 30.6–66.1) for silicone, and 50.4% (95% CI 36.9–68.8) for combined (Figure 2d). There were no associations between removal risk and calendar year or age at implant.
Reasons for implant removal
Reasons contributing to implant removal were either functional or cosmetic, with some removals involving multiple complications in one or both categories. Functional complications included pain/discomfort (29.2%), capsular contracture (29.7%), rupture/deflation (26.3%), infection/wound dehiscence/inflammation (13.9%), and breast cancer/prophylaxis (5.3%). Cosmetic complications, such as asymmetry or malposition, played a role in 50.7% of removals. There were 18 patients who had implants removed for unknown reasons or reasons unrelated to the above complications (e.g., request to remove implants with textured coating or to change implant size with no other complications). Patients with combined or saline implants were more likely to have rupture listed as a reason for removal than patients with silicone implants (combined: HR 1.94, 95% CI 0.55–6.86; saline: HR 1.70, 95% CI 0.64–4.53). Cancer and prophylactic patients were more likely to have infection, wound dehiscence, or inflammation listed as a reason for removal than cosmetic patients (p=0.010; HR: 16.60, 95% CI 1.98–138.92).
Discussion
Incidence of breast implants
To our knowledge, this is the first study to investigate the incidence of breast implants in the US over nearly the entirety of their existence. Overall, the variation in incidence correlates with notable changes in the perceptions and policies of breast implants over the years (Supplementary Figure 1). In the 1980s, anecdotal reports linking silicone breast implants with systemic conditions may account for the fluctuating rates seen during this time. In 1992, the FDA placed a moratorium on the use of silicone implants for breast augmentations [7], reasonably corresponding to a significant drop in incidence. However, implant rates began to increase around 2000 despite no changes to the FDA policy, and when the moratorium was lifted in 2006, incidence for implants of all types and reasons remained largely unchanged, never again reaching the high rates seen in the late 1970’s and 1980’s. Possible explanations for these trend variations are further discussed in the following sections.
Incidence of breast implants by reason
While implants for cosmetic reasons initially dominated, the incidence of IBR for cancer began increasing around 1980, likely related to advancements that increased the utility of implants in reconstructions (e.g., tissue expanders, dual-lumen implants) [8, 9]. In addition, breast cancer incidence increased in the 1980s due to an increase in mammography screenings [10].
Following the drop in incidence in the early 1990’s, seemingly spurred by increased media attention and impending FDA action, cosmetic implant use recovered quickly while IBR for cancer remained low for over a decade. Perhaps, women with a recent cancer history were more wary of the controversies surrounding implants and thus less likely to seek IBR. The sustained low incidence also corresponds with a near 13% drop in invasive breast cancer rates in 1999–2004 [11]. However, incidence of IBR for cancer began increasing around 2004, reaching all-time highs in recent years. The explanation behind this marked growth is likely multifactorial. First, the Women’s Health and Cancer Rights Act, implemented in 1998, required insurance payers to cover breast reconstruction following mastectomy [12]. As a result, IBR grew 11% per year from 1998 to 2008 [13]. Importantly, this growth coincided with an increase in bilateral mastectomies [13], as it was found that women with a bilateral mastectomy were more than twice as likely to seek reconstruction than women with a unilateral mastectomy [14]. The increased preference for bilateral mastectomy may be linked to patient overestimation of future cancer risk and desire to achieve “peace of mind” [15–17]. Another factor fueling the rise in IBR has been the shift away from autologous breast reconstruction, likely attributable to declining reimbursements for these more complicated procedures [18–22].
In contrast to the rise in IBR, breast augmentation rates continually declined in the last 10–15 years of the study. Considering the steadily increasing US population, ASPS data is concordant with this finding [4]. The decline in breast augmentations may be related to the increase in obesity among Americans, as women with a higher body mass index may be less likely to undergo breast augmentation [23–28] and may also be poorer candidates for breast procedures due to an increased risk of complications [29–31]. In addition, reports on the connection between breast implants and anaplastic large cell lymphoma, first noted in 1997 [32], have continued to surface [7, 33–37], likely precipitating the decline in recent years.
Incidence of breast implants by type
Except for the era covered by the FDA moratorium, the incidence of silicone implants was greater than saline for the majority of the study. Despite the controversy of silicone implants, they tend to mimic the consistency and weight of natural breast tissue better than saline [38, 39]. Surgeon preferences have likely also played a role, as one study found the second most important factor in a patient’s decision between silicone and saline was the physician’s explanation of the differences [40].
Risk of mortality
SMR was elevated in 1964–1991 vs. 1992–2017, seemingly due to the increased mortality among cancer patients in the earlier cohort. This aligns with expectations, as US breast cancer mortality improved considerably between the two eras with an estimated 30% decrease from 1980 to 2014 [41]. The mortality benefits seen among cosmetic and prophylactic women may be linked to healthier lifestyles or higher socioeconomic status [42, 43]. Overall, the variation in mortality risk more likely reflects differences in the populations of women with implants over time rather than differences in the safety of implants.
Risk of implant rupture
Consistent with prior reports [44–51], cumulative risk of implant rupture at 5 years was 3.1%, with a higher risk among IBR vs. augmentation patients. A major factor leading to implant rupture is iatrogenic damage during operations [52], and given IBR patients have a known increased risk of reoperation [28, 45, 47, 49–51, 53], this may explain their elevated rupture risk. Although the differences did not reach significance, patients with combined implants appeared to have an increased risk of rupture vs. those with silicone and saline implants. With one exception, all women with combined implants were cancer or prophylactic patients. Therefore, rupture risk for combined implants may be inflated due to their near-exclusive use in IBR or vice versa.
Risk of implant removal
Consistent with prior reports [28, 45, 46, 48, 49, 54], cumulative risk of implant removal at 5 years was 13.2%, with a higher incidence among IBR vs. augmentation patients. Given the elevated rupture risk among IBR patients, the increased risk of removal is not surprising. Although the difference was nonsignificant, removals of saline implants were lower than silicone and combined implants, but again, this may be confounded due to the relationships between implant type and reason.
Reasons for implant removal
Cosmetic complications contributed to over half of implant removals, which was expected given appearance issues can accompany a host of functional implant complications. In prior studies [45, 47, 49, 55–58], request for implant size/style change was a top reason for implant removal. In our study, patients rarely requested reoperation to change implant size/style without also citing an objective functional or cosmetic concern, potentially suggesting it may be easier for women (and/or their surgeons) to justify reoperation on the basis of addressing a complication.
Capsular contracture and rupture are two significant complications of breast implants, as they often necessitate reoperation or implant removal; prior studies reported similar frequencies of these complications leading to explantation [47, 51, 59]. Patients with removal of saline implants were more likely to have rupture as a reason for removal than patients with removal of silicone implants, likely due to saline ruptures being more readily detectable. IBR patients with removals were more likely to have infection, wound dehiscence, or inflammation as a removal reason than cosmetic patients, which is concordant with previous reports [28, 31, 45, 47–49, 53, 60, 61].
A notable strength of this study includes the usage of REP to identify all cases of breast implants in Olmsted County, followed by verification via comprehensive medical record review, eliminating referral bias. However, this study is not without limitations. The population of Olmsted County is predominately white and most procedures took place at Mayo Clinic, an academic medical center, potentially limiting generalizability to more diverse populations and other providers, respectively.
In conclusion, this study documents the changes in breast implant incidence among women from 1964 through 2017, emphasizing the shifting trends in implant reason and type. The results may provide further insight regarding how risks of adverse outcomes associated with implants may vary, as discrepancies more likely indicate differences in the populations of women with implants over time rather than differences in the safety of implants. Lastly, this study provides a foundation for future research, as the identified cohort may be used for subsequent analyses investigating outcomes associated with breast implants.
Supplementary Material
Supplementary Figure 1. Breast implant milestones corresponding with changes in breast implant incidence over time. ALCL, anaplastic large cell lymphoma; BI, breast implants; BIA-ALCL, breast implant-associated anaplastic large cell lymphoma; IOM, Institute of Medicine; SD, systemic disease; WHCRA, Women’s Health and Cancer Rights Act.
Conflict of Interest and Financial Disclosures:
This work was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health (NIH) under Award Number R01 AG034676 and CTSA Grant Number UL1TR002377 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. All authors declare no conflicts of interest relevant to the current study.
Abbreviations
- ASPS
American Society of Plastic Surgeons
- REP
Rochester Epidemiology Project
- CI
confidence interval
- IBR
implant-based reconstruction
- HR
hazard ratio
- SMR
standardized mortality ratio
Footnotes
Compliance with Ethical Standards
The authors declare that they have no conflicts of interest to disclose.
This article does not contain any studies with human participants or animals performed by any of the authors.
For this type of study, formal consent was not required.
References
- 1.Cook RR, Delongchamp RR, Woodbury M, Perkins LL, Harrison MC (1995) The prevalence of women with breast implants in the United States--1989. J Clin Epidemiol. 48(4):519–25. doi: 10.1016/0895-4356(94)00208-8. Epub 1995/04/01. [DOI] [PubMed] [Google Scholar]
- 2.Terry MB, Skovron ML, Garbers S, Sonnenschein E, Toniolo P (1995) The estimated frequency of cosmetic breast augmentation among US women, 1963 through 1988. Am J Public Health. 85(8 Pt 1):1122–4. doi: 10.2105/ajph.85.8_pt_1.1122. Epub 1995/08/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bright RA, Jeng LL, Moore RM (1993) National survey of self-reported breast implants: 1988 estimates. J Long Term Eff Med Implants. 3(1):81–9. Epub 1992/12/09. [PubMed] [Google Scholar]
- 4.American Society of Plastic Surgeons. Plastic Surgery Statistics [cited 2022]. Available from: https://www.plasticsurgery.org/news/plastic-surgery-statistics.
- 5.St Sauver JL, Grossardt BR, Yawn BP, Melton III LJ, Pankratz JJ, Brue SM, et al. (2012) Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 41(6):1614–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabriel SE, O’Fallon WM, Kurland LT, Beard CM, Woods JE, Melton LJ 3rd (1994) Risk of connective-tissue diseases and other disorders after breast implantation. N Engl J Med. 330(24):1697–702. doi: 10.1056/nejm199406163302401. Epub 1994/06/16. [DOI] [PubMed] [Google Scholar]
- 7.Center for Devices and Radiological Health U.S. Food and Drug Administration (2011) FDA Update on the Safety of Silicone Gel-Filled Breast Implants.
- 8.Radovan C (1982) Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg. 69(2):195–208. [DOI] [PubMed] [Google Scholar]
- 9.Becker H (1984) Breast reconstruction using an inflatable breast implant with detachable reservoir. Plast Reconstr Surg. 73(4):678–83. doi: 10.1097/00006534-198404000-00031. Epub 1984/04/01. [DOI] [PubMed] [Google Scholar]
- 10.Breen N, Gentleman JF, Schiller JS (2011) Update on mammography trends: comparisons of rates in 2000, 2005, and 2008. Cancer. 117(10):2209–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Cancer Society (2019) Breast Cancer Facts & Figures 2019–2020. Atlanta. [Google Scholar]
- 12.Women’s Health and Cancer Rights Act of 1998, (1998).
- 13.Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, et al. (2013) A Paradigm Shift in U.S. Breast Reconstruction: Increasing Implant Rates. Plast Reconstr Surg. 131(1):15–23. doi: 10.1097/PRS.0b013e3182729cde. [DOI] [PubMed] [Google Scholar]
- 14.Albornoz CR, Matros E, Lee CN, Hudis CA, Pusic AL, Elkin E, et al. (2015) Bilateral Mastectomy versus Breast-Conserving Surgery for Early-Stage Breast Cancer: The Role of Breast Reconstruction. Plast Reconstr Surg. 135(6):1518–26. doi: 10.1097/prs.0000000000001276. Epub 2015/05/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenberg SM, Tracy MS, Meyer ME, Sepucha K, Gelber S, Hirshfield-Bartek J, et al. (2013) Perceptions, knowledge, and satisfaction with contralateral prophylactic mastectomy among young women with breast cancer: a cross-sectional survey. Ann Intern Med. 159(6):373–81. doi: 10.7326/0003-4819-159-6-201309170-00003. Epub 2013/09/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hawley ST, Jagsi R, Morrow M, Janz NK, Hamilton A, Graff JJ, et al. (2014) Social and Clinical Determinants of Contralateral Prophylactic Mastectomy. JAMA Surg. 149(6):582–9. doi: 10.1001/jamasurg.2013.5689. Epub 2014/05/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yao K, Sisco M, Bedrosian I (2016) Contralateral prophylactic mastectomy: current perspectives. Int J Womens Health. 8:213–23. doi: 10.2147/ijwh.S82816. Epub 2016/07/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farhangkhoee H, Matros E, Disa J (2016) Trends and concepts in post-mastectomy breast reconstruction. J Surg Oncol. 113(8):891–4. doi: 10.1002/jso.24201. Epub 2016/02/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panchal H, Matros E (2017) Current Trends in Postmastectomy Breast Reconstruction. Plast Reconstr Surg. 140(5S):7S–13S. doi: 10.1097/prs.0000000000003941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheckter CC, Panchal HJ, Razdan SN, Rubin D, Yi D, Disa JJ, et al. (2018) The Influence of Physician Payments on the Method of Breast Reconstruction: A National Claims Analysis. Plast Reconstr Surg. 142(4):434e–42e. doi: 10.1097/prs.0000000000004727. Epub 2018/07/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hernandez-Boussard T, Zeidler K, Barzin A, Lee G, Curtin C (2013) Breast reconstruction national trends and healthcare implications. Breast J. 19(5):463–9. doi: 10.1111/tbj.12148. Epub 2013/06/14. [DOI] [PubMed] [Google Scholar]
- 22.Alderman AK, Atisha D, Streu R, Salem B, Gay A, Abrahamse P, et al. (2011) Patterns and correlates of postmastectomy breast reconstruction by U.S. Plastic surgeons: results from a national survey. Plast Reconstr Surg. 127(5):1796–803. doi: 10.1097/PRS.0b013e31820cf183. Epub 2011/05/03. [DOI] [PubMed] [Google Scholar]
- 23.Alderman A, Pusic A, Murphy DK (2016) Prospective Analysis of Primary Breast Augmentation on Body Image Using the BREAST-Q: Results from a Nationwide Study. Plast Reconstr Surg. 137(6):954e–60e. doi: 10.1097/PRS.0000000000002183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cook LS, Daling JR, Voigt LF, deHart MP, Malone KE, Stanford JL, et al. (1997) Characteristics of Women With and Without Breast Augmentation. JAMA. 277(20):1612–7. doi: 10.1001/jama.1997.03540440046031. [DOI] [PubMed] [Google Scholar]
- 25.Maher JL, Bennett DC, Bennett LL, Grothaus P, Mahabir RC (2010) Breast augmentation: A geographical comparison. Can J Plast Surg. 18(4):e44–6. Epub 2010/01/01. [PMC free article] [PubMed] [Google Scholar]
- 26.Fryzek JP, Weiderpass E, Signorello LB, Hakelius L, Lipworth L, Blot WJ, et al. (2000) Characteristics of women with cosmetic breast augmentation surgery compared with breast reduction surgery patients and women in the general population of Sweden. Ann Plast Surg. 45(4):349–56. doi: 10.1097/00000637-200045040-00001. Epub 2000/10/19. [DOI] [PubMed] [Google Scholar]
- 27.Kjøller K, Hölmich LR, Fryzek JP, Jacobsen PH, Friis S, McLaughlin JK, et al. (2003) Characteristics of women with cosmetic breast implants compared with women with other types of cosmetic surgery and population-based controls in Denmark. Ann Plast Surg. 50(1):6–12. doi: 10.1097/00000637-200301000-00002. Epub 2003/01/25. [DOI] [PubMed] [Google Scholar]
- 28.Stevens WG, Calobrace MB, Harrington J, Alizadeh K, Zeidler KR, d’Incelli RC (2016) Nine-Year Core Study Data for Sientra’s FDA-Approved Round and Shaped Implants with High-Strength Cohesive Silicone Gel. Aesthet Surg J. 36(4):404–16. doi: 10.1093/asj/sjw015. [DOI] [PubMed] [Google Scholar]
- 29.Lee K, Kruper L, Dieli-Conwright CM, Mortimer JE (2019) The Impact of Obesity on Breast Cancer Diagnosis and Treatment. Curr Oncol Rep. 21(5):41. doi: 10.1007/s11912-019-0787-1. Epub 2019/03/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen CL, Shore AD, Johns R, Clark JM, Manahan M, Makary MA (2011) The impact of obesity on breast surgery complications. Plast Reconstr Surg. 128(5):395e–402e. [DOI] [PubMed] [Google Scholar]
- 31.Washer LL, Gutowski K (2012) Breast implant infections. Infect Dis Clin North Am. 26(1):111–25. doi: 10.1016/j.idc.2011.09.003. Epub 2012/01/31. [DOI] [PubMed] [Google Scholar]
- 32.Keech JA Jr., Creech BJ (1997) Anaplastic T-cell lymphoma in proximity to a saline-filled breast implant. Plast Reconstr Surg. 100(2):554–5. doi: 10.1097/00006534-199708000-00065. Epub 1997/08/01. [DOI] [PubMed] [Google Scholar]
- 33.Gidengil CA, Predmore Z, Mattke S, van Busum K, Kim B (2015) Breast implant-associated anaplastic large cell lymphoma: a systematic review. Plast Reconstr Surg. 135(3):713–20. doi: 10.1097/prs.0000000000001037. Epub 2014/12/10. [DOI] [PubMed] [Google Scholar]
- 34.de Jong D, Vasmel WL, de Boer JP, Verhave G, Barbé E, Casparie MK, et al. (2008) Anaplastic large-cell lymphoma in women with breast implants. JAMA. 300(17):2030–5. doi: 10.1001/jama.2008.585. Epub 2008/11/06. [DOI] [PubMed] [Google Scholar]
- 35.Kellogg BC, Hiro ME, Payne WG (2014) Implant-associated anaplastic large cell lymphoma: beyond breast prostheses. Ann Plast Surg. 73(4):461–4. doi: 10.1097/SAP.0b013e31827faff2. Epub 2013/06/01. [DOI] [PubMed] [Google Scholar]
- 36.Wong AK, Lopategui J, Clancy S, Kulber D, Bose S (2008) Anaplastic large cell lymphoma associated with a breast implant capsule: a case report and review of the literature. Am J Surg Pathol. 32(8):1265–8. doi: 10.1097/PAS.0b013e318162bcc1. Epub 2008/07/03. [DOI] [PubMed] [Google Scholar]
- 37.Patel BC, Wong CS, Wright T, Schaffner AD. Breast Implants. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 38.Gabriel A, Maxwell GP (2015) The Evolution of Breast Implants. Clin Plast Surg. 42(4):399–404. doi: 10.1016/j.cps.2015.06.015. Epub 2015/09/27. [DOI] [PubMed] [Google Scholar]
- 39.Hidalgo DA, Spector JA (2014) Breast augmentation. Plast Reconstr Surg. 133(4):567e–83e. doi: 10.1097/prs.0000000000000033. Epub 2014/03/29. [DOI] [PubMed] [Google Scholar]
- 40.Walden JL, Panagopoulous G, Shrader SW (2010) Contemporary decision making and perception in patients undergoing cosmetic breast augmentation. Aesthet Surg J. 30(3):395–403. doi: 10.1177/1090820x10374101. Epub 2010/07/06. [DOI] [PubMed] [Google Scholar]
- 41.Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, Stubbs RW, Bertozzi-Villa A, Morozoff C, et al. (2017) Trends and patterns of disparities in cancer mortality among US counties, 1980–2014. JAMA. 317(4):388–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brinton LA, Lubin JH, Burich MC, Colton T, Hoover RN (2001) Mortality among augmentation mammoplasty patients. Epidemiology. 12(3):321–6. doi: 10.1097/00001648-200105000-00012. Epub 2001/05/05. [DOI] [PubMed] [Google Scholar]
- 43.Villeneuve PJ, Holowaty EJ, Brisson J, Xie L, Ugnat AM, Latulippe L, et al. (2006) Mortality among Canadian women with cosmetic breast implants. Am J Epidemiol. 164(4):334–41. doi: 10.1093/aje/kwj214. Epub 2006/06/17. [DOI] [PubMed] [Google Scholar]
- 44.Bae J, Jeon BJ, Mun GH, Bang SI, Pyon JK, Lee KT (2022) Predictors for Implant Rupture in Two-Stage Tissue Expander-Based Breast Reconstruction: A Retrospective Cohort Study. Ann Surg Oncol. 29(2):1100–8. doi: 10.1245/s10434-021-10773-w. Epub 2021/10/01. [DOI] [PubMed] [Google Scholar]
- 45.Coroneos CJ, Selber JC, Offodile AC 2nd, Butler CE, Clemens MW (2019) US FDA Breast Implant Postapproval Studies: Long-term Outcomes in 99,993 Patients. Ann Surg. 269(1):30–6. doi: 10.1097/sla.0000000000002990. Epub 2018/09/18. [DOI] [PubMed] [Google Scholar]
- 46.Spear SL, Murphy DK, Slicton A, Walker PS, Group ftISBIUSS (2007) Inamed Silicone Breast Implant Core Study Results at 6 Years. Plast Reconstr Surg. 120(7):8S–16S. doi: 10.1097/01.prs.0000286580.93214.df. [DOI] [PubMed] [Google Scholar]
- 47.Spear SL, Murphy DK (2014) Natrelle round silicone breast implants: Core Study results at 10 years. Plast Reconstr Surg. 133(6):1354–61. doi: 10.1097/prs.0000000000000021. Epub 2014/05/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cunningham B, McCue J (2009) Safety and effectiveness of Mentor’s MemoryGel implants at 6 years. Aesthetic Plast Surg. 33(3):440–4. [DOI] [PubMed] [Google Scholar]
- 49.Maxwell GP, Van Natta BW, Murphy DK, Slicton A, Bengtson BP (2012) Natrelle style 410 form-stable silicone breast implants: core study results at 6 years. Aesthet Surg J. 32(6):709–17. [DOI] [PubMed] [Google Scholar]
- 50.Hammond DC, Canady JW, Love TR, Wixtrom RN, Caplin DA (2017) Mentor Contour Profile Gel Implants: Clinical Outcomes at 10 Years. Plast Reconstr Surg. 140(6):1142–50. doi: 10.1097/prs.0000000000003846. Epub 2017/11/28. [DOI] [PubMed] [Google Scholar]
- 51.Caplin DA, Calobrace MB, Wixtrom RN, Estes MM, Canady JW (2021) MemoryGel Breast Implants: Final Safety and Efficacy Results after 10 Years of Follow-Up. Plast Reconstr Surg. 147(3):556–66. doi: 10.1097/prs.0000000000007635. Epub 2021/02/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Handel N, Garcia ME, Wixtrom R (2013) Breast implant rupture: causes, incidence, clinical impact, and management. Plast Reconstr Surg. 132(5):1128–37. doi: 10.1097/PRS.0b013e3182a4c243. Epub 2013/10/30. [DOI] [PubMed] [Google Scholar]
- 53.Handel N, Cordray T, Gutierrez J, Jensen JA (2006) A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 117(3):757–67. [DOI] [PubMed] [Google Scholar]
- 54.Hammond DC, Migliori MM, Caplin DA, Garcia ME, Phillips CA (2012) Mentor Contour Profile Gel implants: clinical outcomes at 6 years. Plast Reconstr Surg. 129(6):1381–91. [DOI] [PubMed] [Google Scholar]
- 55.Seigle-Murandi F, Lefebvre F, Bruant-Rodier C, Bodin F (2017) Incidence of breast implant rupture in a 12-year retrospective cohort: evidence of quality discrepancy depending on the range. J Plast Reconstr Aesthet Surg. 70(1):42–6. [DOI] [PubMed] [Google Scholar]
- 56.Montemurro P, Fischer S, Hager S, Hedén P (2019) Secondary Breast Augmentation: Is There a Trend for Bigger Implants? Aesthetic Plast Surg. 43(1):59–69. doi: 10.1007/s00266-018-1244-5. Epub 2018/10/03. [DOI] [PubMed] [Google Scholar]
- 57.Hidalgo DA, Sinno S (2016) Current Trends and Controversies in Breast Augmentation. Plast Reconstr Surg. 137(4):1142–50. doi: 10.1097/01.prs.0000481110.31939.e4. Epub 2016/03/29. [DOI] [PubMed] [Google Scholar]
- 58.Cunningham B (2007) The Mentor Core Study on Silicone MemoryGel Breast Implants. Plast Reconstr Surg. 120(7 Suppl 1):19s–29s. doi: 10.1097/01.prs.0000286574.88752.04. Epub 2007/12/27. [DOI] [PubMed] [Google Scholar]
- 59.Embrey M, Adams EE, Cunningham B, Peters W, Young VL, Carlo GL (1999) Factors associated with breast implant rupture: pilot of a retrospective analysis. Aesthetic Plast Surg. 23(3):207–12. doi: 10.1007/s002669900269. Epub 1999/06/29. [DOI] [PubMed] [Google Scholar]
- 60.Handel N, Jensen JA, Black Q, Waisman JR, Silverstein MJ (1995) The fate of breast implants: a critical analysis of complications and outcomes. Plast Reconstr Surg. 96(7):1521–33. doi: 10.1097/00006534-199512000-00003. Epub 1995/12/01. [DOI] [PubMed] [Google Scholar]
- 61.Ozturk CN, Ozturk C, Soucise A, Platek M, Ahsan N, Lohman R, et al. (2018) Expander/Implant Removal After Breast Reconstruction: Analysis of Risk Factors and Timeline. Aesthetic Plast Surg. 42(1):64–72. doi: 10.1007/s00266-017-1031-8. Epub 2017/12/23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. Breast implant milestones corresponding with changes in breast implant incidence over time. ALCL, anaplastic large cell lymphoma; BI, breast implants; BIA-ALCL, breast implant-associated anaplastic large cell lymphoma; IOM, Institute of Medicine; SD, systemic disease; WHCRA, Women’s Health and Cancer Rights Act.


