Abstract
Racism drives population health inequities by shaping the unequal distribution of key social determinants of health, such as socioeconomic resources and exposure to stressors. Research on interrelationships among race, socioeconomic resources, stressors, and health has proceeded along two lines that have largely remained separate: one examining differential effects of socioeconomic resources and stressors on health across racialized groups (moderation processes), and the other examining the role of socioeconomic resources and stressors in contributing to racial inequities in health (mediation processes). We conceptually and analytically integrate these areas using race theory and a novel moderated mediation approach to path analysis to formally quantify the extent to which an array of socioeconomic resources and stressors—collectively and individually—mediate racialized health inequities among a sample of older adults from the Health and Retirement Study. Our results yield theoretical contributions by showing how the socioeconomic status–health gradient and stress processes are racialized (24% of associations examined varied by race), substantive contributions by quantifying the extent of moderated mediation of racial inequities (approximately 70%) and the relative importance of various social factors, and methodological contributions by showing how commonly used simple mediation approaches that ignore racialized moderation processes overestimate—by between 5% and 30%—the collective roles of socioeconomic status and stressors in accounting for racial inequities in health.
Keywords: Racism, Health disparities, Socioeconomic resources, Stress, Aging
Introduction
Within racialized societies such as the United States, racial inequities are a prominent feature of the population health landscape (Du Bois 1899; Williams et al. 2019). People racialized as Black and Mexican American, for example, experience more morbidity and unnecessary suffering than their White counterparts, especially in middle and later life (Boen and Hummer 2019; Brown 2018; Garcia et al. 2019). Two projected U.S. population trends—growth in racial diversity and population aging—suggest that the burden of excess human suffering due to racial inequities in health among older adults is likely to increase in the future (Ortman et al. 2014). These patterns underscore the urgency of understanding and addressing barriers to achieving health equity.
This study draws upon racialized social systems theory to conceptualize racism— not inherent or biological difference—as the underlying cause of racial differences in the distributions of resources, risks, and health, as well as the relationships among these factors (Bonilla-Silva 1997; Brown and Homan 2023; Graetz et al. 2022; Sewell 2016; Zuberi and Bonilla-Silva 2008). Decades of research suggest that racism indirectly harms the health of racially marginalized groups through an array of pathways, including unequal access to socioeconomic resources and differential exposure to stressors (Goosby et al. 2018; Hayward et al. 2000; Phelan and Link 2015; Williams et al. 2019). While it is well established that social conditions underlie health inequities, the proportion of the racial health gap that is due to differences in socioeconomic resources and stressors is largely unknown—especially among older adults (Williams 2018).
Our understanding of the processes underlying racial inequities in health has been hindered by several limitations of prior studies. First, previous studies have not examined mediation processes while simultaneously taking into account potential racial differences in the effects of these mediating factors on health (i.e., a “moderated mediation” approach; Preacher et al. 2007). Emerging evidence indicates that the relationships among socioeconomic status (SES), stressors, and health vary by race (Assari 2018; Bratter and Gorman 2011; Cobb et al. 2020; Colen et al. 2018; DeAngelis 2020). This suggests that inattention to conditional indirect effects may lead to over- or underestimating the extent to which these factors mediate racial inequities in health. Second, prior research has not formally tested the extent to which SES and stressors collectively and individually mediate racial inequities in health. Because of the dearth of formal tests of mediation processes, it remains unclear precisely how much socioeconomic inequalities and stress processes contribute to racialized health inequities. Third, previous research has typically lacked comprehensive measurement of stressors, which has hindered our understanding of racial differences in specific types of stressors (e.g., chronic strains, discrimination, traumas, and neighborhood stressors) and their unique contributions to health inequalities (Turner 2013). Fourth, because prior studies on the topic have typically focused on a single health outcome, we know little about the degree to which racialized mediation processes are similar for a range of health outcomes. Thus, there are many ways in which our knowledge regarding the contributions of SES and stressors to racial inequities in health remains incomplete.
This study extends the literature on the social determinants of health by utilizing race theory in tandem with structural equation modeling to formally quantify the contributions of an array of socioeconomic resources and stressors—collectively and individually—to racialized inequities in health among older, U.S.-born non-Hispanic Blacks, Mexican Americans, and non-Hispanic Whites.1 Specifically, we address four interrelated research questions: (1) Are relationships among SES, stressors, and health conditional on (i.e., moderated by) race? (2) To what extent do SES and stressors collectively mediate racial health inequities when using a “moderated mediation” approach—that is, simultaneously testing mediation processes while also accounting for possible racial differences in associations among SES, stressors, and health? (3) What are the relative contributions of each of the socioeconomic and stress factors to racialized health inequities? (4) To what extent does a “simple mediation” approach—that is, assuming equivalent associations among SES, stressors, and health across racial groups—misestimate the degree to which socioeconomic and stress factors account for racialized inequities in health?
Furthermore, to gain a more comprehensive understanding of the etiology of racialized health inequities, this study examines three measures of health that are salient in middle and later life: self-rated health, biological risk, and functional limitations. These commonly used measures of population health and aging processes capture not only subjective and objective facets of health, but also specific and global ones. By investigating a range of health outcomes that differ in terms of strengths, limitations, and etiologies, we are likely to gain a more accurate and comprehensive understanding of the processes leading to health inequities (Aneshensel 2005). This study highlights the importance of analytically integrating moderation and mediation processes for clarifying the extent to which SES and stressors mediate racialized inequities in health and, more generally, for understanding the social pathways underlying health stratification.
Background
Racial Inequities in SES, Exposure to Stressors, and Health
Racialized social systems theory highlights how racism is the driving cause of all racial inequities in society, as well as the cause of the creation, evolution, and meanings of racial categories themselves (Bonilla-Silva 1997). Constructivist perspectives underscore the fact that “race” is a sociopolitical construct that assigns a hierarchy of value to humans (i.e., a racial order) on the basis of false assumptions that groups racialized as non-White are biologically inferior to groups racialized as White (Golash-Boza 2016; Omi and Winant 2015). Moreover, race theories illustrate how racism involves inter-connected systems of racial discrimination across societal domains (e.g., social, economic, political, health care, and criminal-legal spheres) that create and perpetuate the relational subordination of minoritized groups (Bonilla-Silva 1997; Brown and Homan 2023). These conditions reinforce—and are reinforced by—discriminatory beliefs, values, and the inequitable distribution of resources and risks (Bailey et al. 2017; Delgado and Stefancic 2017; Reskin 2012; Williams and Baker 2021).
Drawing on race theories, population health science is increasingly conceptualizing systemic racism as an “upstream” cause of “downstream” determinants of health such as access to resources and exposures to risk (Brown and Homan 2023). Thus, one pathway through which systemic racism affects population health is by shaping the distribution of proximal social determinants of health (e.g., socioeconomic resources and stressors) as well as their racialized effects on health (Graetz et al. 2022; Hardeman et al. 2022; Phelan and Link 2015). Importantly, current cohorts of older Black and Mexican American people came of age during the Jim Crow era and, thus, they have endured both overt forms of racism that were more prevalent in the past as well as subtler (but still pernicious) contemporary forms of racism (Bonilla-Silva 2017; Keith 2014). Consequently, they have experienced an accumulation of racialized social disadvantages throughout their lives. Within this context of racialized barriers to opportunities for achievement and economic advancement, it is not surprising that Blacks and Mexican Americans are disadvantaged relative to Whites in terms of socioeconomic resources, including educational attainment, income, and wealth (Brown 2016; Kao and Thompson 2003; Williams and Baker 2021). Socioeconomic factors, in turn, impact health by providing material resources as well as knowledge, autonomy, power, freedom, and prestige, which provide opportunities for healthy living and are useful for minimizing exposure to risks—including stressors (O’Rand and Lynch 2018; Phelan et al. 2010). The preponderance of evidence indicates that racial inequities in socioeconomic resources account for some but not the entirety of racial stratification in health in middle and later life (Boen 2016; Brown 2018).
In addition to SES, there is growing interest in understanding the extent to which unequal exposure to stressors contributes to racial health inequities. The Stress Process Model is a leading framework that helps elucidate the role that stress plays in social gradients in health (Pearlin et al. 2005). Two central propositions of the model are (1) social conditions—for example, racial and socioeconomic stratification—shape exposure to stressors, and (2) stressors negatively affect health (Keith 2014). Applied to the race–health relationship, the Stress Process Model posits that racial inequities in health derive, in part, from minoritized groups’ greater exposure to economic adversity and stressors, which are interrelated and harmful for health (Turner 2013).
Empirical findings support key tenets of the Stress Process Model. For example, compared with Whites, Black and Mexican American people are more likely to experience economic adversity (Brown 2016), chronic stressors (Thoits 2010; Turner and Avison 2003), financial strains (Brown et al. 2020), neighborhood disorder (Sternthal et al. 2011), neighborhood mistrust (Millar 2020), traumas (Turner et al. 2016), and perceived discrimination (Williams and Mohammed 2013). Moreover, consistent with the Stress Process Model, there is evidence that economic adversity leads to greater exposure to a wide array of stressors (Turner 2013).
The deleterious health consequences of exposure to stressors, particularly chronic exposure, are also well-documented. Indeed, a plethora of studies provide evidence suggesting that social factors, including stressors, become embodied at biological and molecular levels (Eisenberger 2013; Goosby et al. 2018; Green and Darity 2010). One major mechanism through which this is achieved is through the body’s stress response. When a threat (e.g., a stressor) is perceived, the brain’s neural regions facilitate downstream physiological responses in efforts to resolve or eliminate the threat, such as activating the sympathetic nervous system (SNS) and the hypothalamus– pituitary–adrenal (HPA) axis. Once activated, these systems release chemical mediators (e.g., cortisol, catecholamines) to prepare and protect the body from threat (Liu et al. 2017). This results in increased heart rate, respiration, and blood pressure and the suppression of immune function (Vitlic et al. 2014). The body’s immune system may also activate when a threat is detected, leading to the release of inflammatory cells and pro-inflammatory cytokines (Chen et al. 2018; Horowitz et al. 2020). When exposure is acute, the body is generally able to return to homeostasis, or its baseline condition, once the threat is eliminated. Chronic exposure to stressors, however, makes it difficult for the body’s responses to return to baseline (Goosby et al. 2018). Prolonged activation and overactivation of the immune system can lead to chronic inflammation and dysregulation of the body’s various stress responses (Furman et al. 2019; Liu et al. 2017). These processes, in turn, increase risk of wear and tear on the body and, ultimately, accelerated aging and diminished health (Goosby et al. 2018; Juster et al. 2010; Seeman et al. 2001).
Gaps in the Literature
Despite strong evidence that SES and exposure to stressors shape population health, their relative contributions to racial inequities in health remain unclear owing to several gaps in the literature. First, prior studies on social determinants of racial health inequities have often employed simple mediation approaches that assumed the relationships among SES, stress, and health are invariant across racial groups (e.g., Sternthal et al. 2011; Tackett et al. 2017). Such approaches may lead to biased estimates of mediation processes, as they do not take into account drastic racial differences in experiences as a result of living in a racialized society (Graetz et al. 2022). Growing evidence suggests that SES–stress and SES–health relationships vary along racial lines, consistent with marginalization-related diminished returns theory (Assari et al. 2020). For example, several studies have shown that the protective effects of socioeconomic resources for both stress exposure and health are weaker for Blacks and Mexican Americans than for Whites, owing to their greater cumulative exposure to racialized social disadvantages (Assari 2018; Assari et al. 2020; Brown et al. 2016; Colen et al. 2018; Gaydosh et al. 2018; Hudson et al. 2013; Pearson 2008). Indeed, even after adjusting for group differences in SES, Blacks and Mexican Americans are more likely than Whites to live in toxic neighborhoods, experience discrimination, receive lower quality education, and be incarcerated—conditions that are stressful and harmful for health (Gee and Ford 2011; Phelan and Link 2015; Sewell 2016). Furthermore, among racially subordinate groups, greater socioeconomic attainment often involves working or living in predominantly White spaces, which increases exposure to interpersonal discrimination (Assari and Lankarani 2016; DeAngelis 2022; Forman 2003); greater attainment also requires sustained and high-effort coping given the racialized barriers to socioeconomic opportunities (DeAngelis 2020; Hudson et al. 2016; Sellers et al. 2012). Such coping may expend a considerable amount of energy, further leading to the overactivation of the body’s stress response (Brody et al. 2013). Collectively, these experiences are likely to undermine the benefits of socioeconomic resources, leading Blacks and Mexican Americans to reap smaller health gains from higher SES (Boen 2016; Brown et al. 2016; Hudson et al. 2013) and experience little or no health benefit from upward mobility across the life course (Walsemann et al. 2016). Relatively little is known about whether the effects of stressors on health are conditional on race. Consistent with the notion of differential vulnerability, a handful of studies suggest that several types of stressors (e.g., chronic and financial strains, traumas, and perceived discrimination) have a stronger negative association with health among Whites than among Black people (Assari and Lankarani 2016; Bratter and Gorman 2011; Cobb et al. 2020). One explanation for this phenomenon is that older racially subordinate groups—who have often endured elevated exposure to stressors throughout their lives (Thoits 2010)—are a select group and may be especially resilient in the face of adversity because they are more accustomed to managing stressors than their White counterparts (Ayalon and Gum 2011; Barnes et al. 2008; Keith 2014). Relatedly, there is evidence that older Black and Mexican American individuals appraise stressors as less stressful than their White counterparts (Brown et al. 2020) and can become habituated to repeated stress, leading to reduced harm through a process whereby HPA activation from a stressor diminishes with subsequent exposures to the same stressor (McCarty 2016). In sum, existing evidence points to racial differences in the effects of stressors on health.
Notably, the growing lines of research on the differential effects of SES and stress on health across racial groups (i.e., racialized moderation) have developed largely independently of research attempting to understand the social determinants of health contributing to observed racial health inequalities (i.e., mediation of the race–health relationship). As a result, existing studies examining the mediating roles of social factors generally fail to simultaneously account for racial differences in the effects of social factors and are therefore likely to obscure the social pathways leading to racial inequities in health (Pearson 2008; Williams and Mohammed 2013).
A second gap in the literature is that prior studies on the roles of SES and stressors have not formally tested the extent to which these factors mediate racial inequities in health. Rather, previous work has typically inferred mediation processes by assessing changes to the magnitude and statistical significance of coefficients for racialized groups after adjusting for SES and stressors (Sternthal et al. 2011). However, formal tests for mediation would provide greater certainty and specificity about the extent to which various factors account for the relationship between race and health (Bollen 1989; Little et al. 2007). A recent study by Bell and colleagues (2020) conducted a mediation analysis, using the Karlson–Holm–Breen (KHB) method (Karlson et al. 2012), that suggested income and homeownership partially mediated Black–White disparities in self-rated health. This study, however, did not use a moderated mediation approach to account for potential racial differences in the health consequences of income or homeownership, nor did it assess the (moderated) mediating role of stressors.
Third, prior studies on stressors as factors underlying racial health inequalities have tended to examine a single or small set of stressors, overlooking the joint consequences of numerous stressors. As a result, previous research may have underestimated racial differences in stress exposure and the role that differential exposure to stressors plays in health inequalities (Lewis et al. 2015; Turner and Avison 2003). Given that stressors tend to “cluster” or co-occur, inattention to the simultaneous impacts of a range of stressors likely masks their unique effects on health in general, and on racial health inequities in particular (Thoits 2010; Turner 2013).
Fourth, prior studies on the topic have often focused on a single measure of health. Notably, the health consequences of SES and stressors may vary depending on the outcome. Given the multidimensionality of health and distinct disease etiologies, examining only one measure of health is likely to provide an incomplete picture. This underscores the importance of investigating multiple health outcomes to provide a more comprehensive understanding of the social pathways underlying health inequalities (Aneshensel 2005; Turner 2013).
Finally, studies that explore how SES and stressors contribute to racial inequities in health have suffered from limited generalizability because they have often excluded Mexican Americans (e.g., Bell et al. 2020) and relied on convenience or community-based samples (e.g., Sternthal et al. 2011). It is particularly critical to study factors shaping the health of Mexican Americans, given that they are one of the largest and fastest growing minoritized groups in the United States (Ortman et al. 2014).
Current Study
This study advances existing scholarship on racialized health inequities by integrating insights from research on the moderating role of race in SES, stress, and health relationships with literature assessing the explanatory roles of SES and stressors as pathways underlying racial inequities in health. Using a nationally representative sample of Black, Mexican American, and White older adults, we first assess the extent of moderation. Next, we employ a moderated mediation approach to path analysis (Preacher et al. 2007) to formally quantify the role of a wide array of socioeconomic resources and stressors in shaping racial health inequities. Finally, we compare these results to those from a simple mediation approach to determine whether mediation models that ignore moderating effects overstate the extent to which unequal access to socioeconomic resources and exposure to stressors account for racial health inequities.
First, informed by theoretical research and empirical studies on how the relationships among socioeconomic resources, stressors, and health are conditional on race, we hypothesize that:
Hypothesis 1:
The associations among socioeconomic resources, stressors, and health are weaker among Blacks and Mexican Americans than among Whites.
These patterns would likely reflect the less protective effects of SES and greater habituation and resilience to stressors among Blacks and Mexican Americans than Whites owing to racialized access to resources, exposures to risks, and selective survival.
Next, because SES and stressors are key social determinants of health that are unequally distributed along racial lines, we hypothesize that structural equation models of moderated mediation will show:
Hypothesis 2:
Socioeconomic resources and stressors collectively mediate a substantial proportion of racial inequities in health.
Measures of SES and stressors included in this study are likely to only partially mediate racial inequities in health because systemic racism undermines the health of Black and Mexican American individuals through myriad unmeasured pathways besides SES and stress exposure (Phelan and Link 2015; Williams et al. 2019). Given the scant research that has formally tested how SES and stressors jointly mediate racial inequities in health, there is not a sufficient body of knowledge to hypothesize about the precise extent of their mediation.
Regarding the relative contribution of each of the socioeconomic resources to explaining racial health inequities, we hypothesize that:
Hypothesis 3a:
Education and wealth will be particularly strong mediators of racial inequalities in health.
Prior research has shown that education and wealth are key social determinants of health because they provide access to a range of health promoting factors (as noted earlier). Robust education–health and wealth–health relationships in tandem with large racial inequalities in educational and wealth suggest that these socioeconomic factors play a key role in shaping racial inequities in health.
With respect to the relative contributions of stressors, we hypothesize that:
Hypothesis 3b:
Compared to acute or eventful stressors, stressors that are chronic or recurring will be stronger mediators of racial inequities in health.
Chronic strains and recurring stressors are unequally distributed along racial lines and are especially deleterious for health, and thus they are likely to make a substantial contribution to racial inequities in health.
Finally, if Hypothesis 1 is correct and the relationships among socioeconomic resources, stressors, and health are weaker among racially subordinated groups than among Whites, then accounting for these differential effects will likely diminish the extent to which SES and stressors collectively mediate racial inequities in health. Therefore, we hypothesize that:
Hypothesis 4:
Compared to moderated mediation analyses, simple mediation models that ignore differential effects by race overstate the extent to which unequal SES and stress exposure collectively account for racial health inequities.
Confirmation of Hypothesis 4 would suggest that we know far less about the specific social pathways underlying racialized inequities in health than previously assumed.
Data and Methods
This study uses data from the Health and Retirement Study (HRS). The target population for the HRS includes all English- or Spanish-speaking adults in the contiguous United States over the age of 50. Black and Hispanic individuals were oversampled, and respondents were interviewed biennially beginning in 1992. In 2006, the HRS added a Psychosocial Module that includes information on an array of stressors, with follow-up interviews every four years. Half of the core panel participants were randomly assigned to complete this module in 2006; the other half were assigned to complete the module in 2008. The Psychosocial Module was fielded again in 2010 to half of HRS participants (to new respondents and those who were eligible in 2006); in 2012, the other half of the sample (new respondents and those who were eligible in 2008) were assigned to complete the module. Our analyses rely on information from the 2006, 2008, 2010, and 2012 Core Data and Psychosocial Modules. The analytic sample for this study includes U.S.-born respondents (1931–1959 birth cohorts) who self-identify as non-Hispanic Black (n = 7,969), Mexican American (n = 1,620), or non-Hispanic White (n = 25,315) and are aged 51–86 at the time of the interview. Other racial groups were excluded owing to small sample sizes.
Outcome Measures
Self-rated health is assessed by respondents’ answers to the question, “In general, would you say your health is: excellent, very good, good, fair, or poor?”; responses ranged from 1 (poor) to 5 (excellent). Self-rated health is a reliable and valid global measure of health (Idler and Benyamini 1997; Jylhä 2009; Schnittker and Bacak 2014); given that it is among the most commonly used measures of population health, including it as one of the health outcomes in this study has considerable utility for comparability with prior research.2
Cumulative biological risk (Crimmins et al. 2007; Juster et al. 2010; Seeman et al. 2001) is assessed by a latent scale based on eight biological markers of multisystemic physiological dysregulation: systolic and diastolic blood pressure; body mass index (BMI); overall cholesterol; high-density lipoprotein (HDL) cholesterol; glycated hemoglobin; C-reactive protein; and cystatin C. Dichotomous measures indicate whether the respondent is in the highest risk quartile for each of the biomarkers.3 These items were used to estimate a single latent dimension corresponding to cumulative biological risk using confirmatory factor analysis (CFA).4 High cumulative biological risk scores reflect physiological “wear and tear” as a result of repeated activation of the body’s stress response (Crimmins et al. 2007).
Functional limitations are assessed by a summary measure indicating whether the respondent reports having difficulty performing a set of tasks: walking several blocks; walking one block; walking across the room; sitting for two hours; getting up from a chair after having sat for a while; climbing several flights of stairs; climbing a single flight of stairs; stooping, kneeling, or crouching; lifting or carrying 10 pounds; picking up a dime off of a table; raising one’s arms above one’s shoulders; and pushing or pulling large objects such as furniture. To be consistent with prior research (Haas and Rohlfsen 2010), we used a summary measure of the total number of limitations ranging from 0 to 12 (Cronbach’s alpha = .84).
Racialized Categories
Racialized categories are sociopolitical constructs that have real consequences. We use the following dichotomous measures of racialized categories, which reflect respondents’ self-reported identification: non-Hispanic Black, Mexican American, and non-Hispanic White (reference group).
Mediators
We examine the direct and mediating effects of socioeconomic resources and stressors on health. Measures of socioeconomic status include education (in years), household income, and household wealth (total assets minus total liabilities). Household income and wealth measures reflect resources from both spouses (partners) for married (cohabiting) respondents.5
We examine an array of stressors: chronic stressors, financial strain, neighborhood disorder, neighborhood mistrust, everyday discrimination, multiple attributions of discrimination, major discrimination, and traumatic events. The measure of chronic stressors (six-item inventory; Troxel et al. 2003) assesses exposure to current and ongoing problems that have lasted 12 months or longer, such as having a family member who has health problems or abuses drugs or alcohol; difficulties at work; housing problems; and strain in a close relationship. A financial strain index captures difficulty in meeting monthly payments on bills, ranging from 1 (not at all difficult) to 5 (completely difficult; Campbell et al. 1976). A neighborhood disorder variable measures respondents’ perceptions about neighborhood conditions (Millar 2020)—vandalism/ graffiti, rubbish, vacant houses, and crime (four-item index, α = .640). An index of neighborhood mistrust (Millar 2020) assesses neighborhood social climate—feeling a lack of belongingness, and perceptions that neighbors are untrustworthy, unfriendly, and unreliable (four-item inventory, α = .820).
Stressors associated with perceived discrimination are captured by several measures. The validated Everyday Discrimination Scale (six-item mean index, α = .840; Williams et al. 1997) assesses how often respondents experience hassles associated with perceived unfair treatment in their “day-to-day life.” Respondents were also asked about what factors(s) they attribute to their unfair treatment (e.g., race, gender, national origin, age, sexual orientation, or other statuses). Those who reported multiple attributions of discrimination were compared with those who reported a single attribution or none (see Grollman 2014). The Major Discrimination Scale (seven-item inventory; Williams et al. 1997) captures perceptions of significant discriminatory events that occurred at any point in life in various domains, such as work, housing, lending, or criminal justice and health care systems. The lifetime traumas measure captures whether at any point in life the respondent experienced a range of traumatic events: the death of a child; natural disasters; substance abuse or life-threatening illnesses or accidents among family members; or conflict involving fire-arms (seven-item inventory; Krause et al. 2004).
Control Variables
To reduce the risk of biased estimates, analyses control for several factors that are known to be associated with the focal predictors and outcome measures. Specifically, all analyses control for an array of potentially confounding factors: age (in years), sex (1 = female; 0 = male), marital status (1 = married; 0 = not married), private health insurance (1 = yes; 0 = no), and birth cohort (1 = 1931–1941; 2 = 1942–1947; 3 = 1948–1953; 4 = 1954–1959). We also control for medication use for six key metabolic syndrome–related classes of drugs: (1) blood pressure, (2) diabetes (oral administration), (3) insulin (shots or pump), (4) heart problems (e.g., myocardial infarction treatment), (5) stroke, and (6) cholesterol. We provide details of the pharmacotherapy measure specification and sensitivity analyses in online appendix A.
Analytic Strategy
Statistical Methodology
We use a structural equation model (SEM) approach to analyze the role of socioeconomic factors and psychosocial stressors as mediators of the race–health relationship. More specifically, we use SEM path analysis (Wright 2015) to decompose racialized inequities in health into direct, indirect (via SES and stressor mediators), and total effects (Bollen 1989; Loehlin 2004; Sobel 1987). It is important to note that racial inequities are not caused by inherent or biological differences, but rather by relations of subordination that have their roots in racism (Graetz et al. 2022; Roberts 2011; Williams and Baker 2021; Zuberi and Bonilla-Silva 2008). As detailed in the following, we use path analysis to fit a moderated serial mediation model (Preacher et al. 2007), in which there are two theoretically dictated layers of mediator variables, the coefficients of which are allowed to vary across racialized groups. Additionally, for comparison, we also fit simple serial mediation models, which are exactly the same as the moderated serial mediation models except the mediator variable coefficients are constrained to be equal across racialized groups. For the sake of readability, hereafter we drop the term “serial” and these models will be referred to as moderated mediation and simple mediation. All analyses were conducted on pooled data from two waves of data collection; thus, all equations in all models adjust for a (fixed) dichotomous wave indicator. Additional statistical methodology details (e.g., missing data, survey weights, robust standard errors, equations) are provided in online appendix A.
Modeling Strategy: Simple Mediation Versus Moderated Mediation
As noted, moderated mediation models were fit using SEM path analysis. For comparison and continuity with previous research, we also estimated and present a related set of simple mediation models. While the moderated mediation models were empirically superior (as assessed by omnibus likelihood ratio tests and individual coefficient tests), we find the explicit comparison of the preferred moderated mediation model to the simple mediation model instructive. This is because the comparison demonstrates that assuming racial invariance across mediator effects, as the commonly used simple mediation model implicitly does, generally results in overestimation of the magnitude of mediation and distortions of the patterns of mediation among Black and Mexican American groups, by imposing the pattern exhibited in the White group owing to its larger sample size.
Figure 1 provides simplified path diagrams of the two model specifications. We emphasize that the path diagram is simplified as, for the sake of parsimony, it omits control variables (which are included in all estimated equations), represents groups of similar mediator variables as single boxes (i.e., SES and stressors), and omits estimated covariances and variances.
Fig. 1.
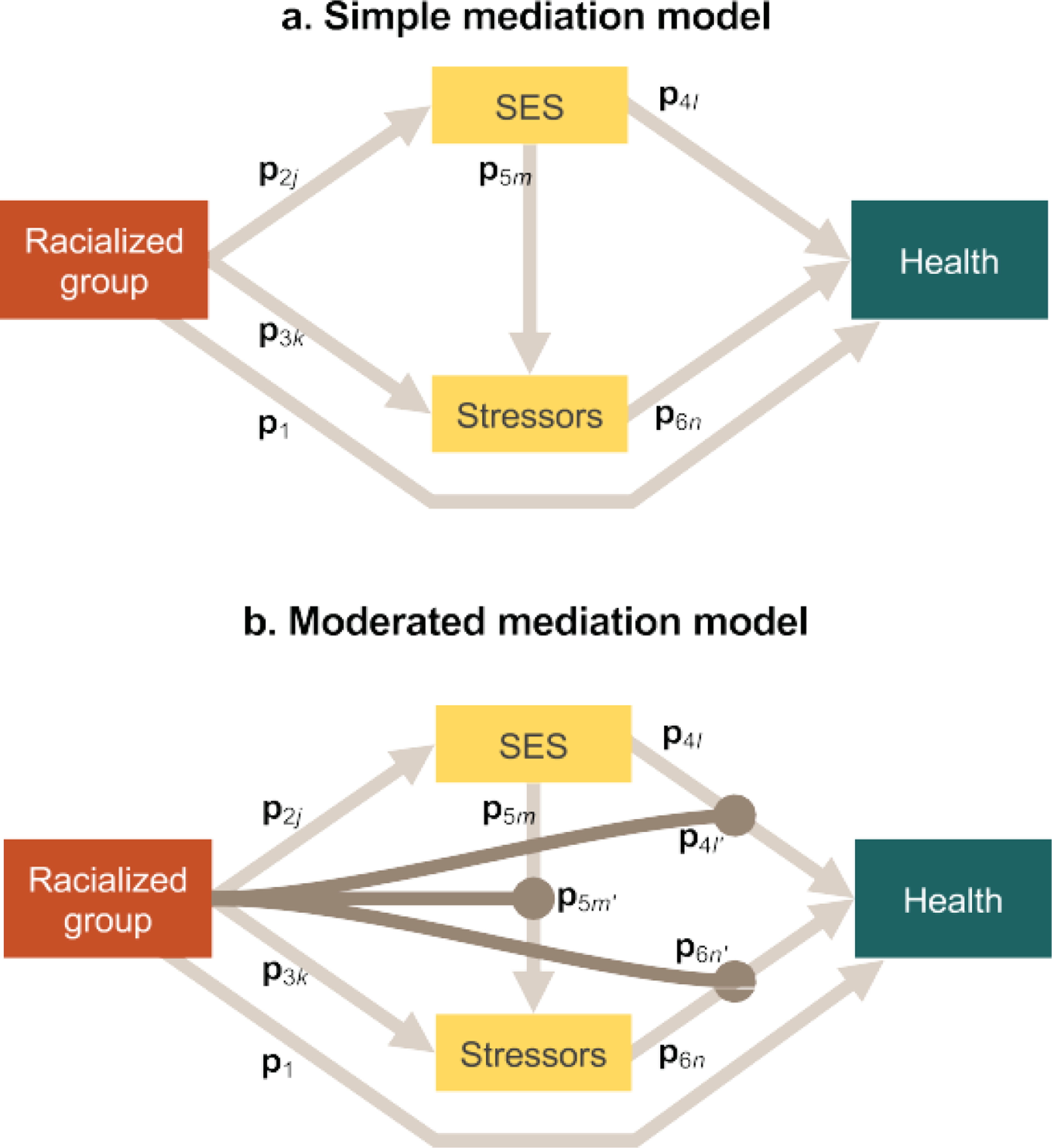
Simplified path diagram depicting simple mediation (panel a) and moderated mediation models (panel b). Racialized inequities are not caused by inherent or biological differences, but rather by relations of subordination that have their roots in racism. SES = socioeconomic status.
In panel a of Figure 1, the simple mediation model is depicted (MacKinnon et al. 2007; MacKinnon et al. 2002). Here, racialized group is specified as a distal independent variable, which has direct effects on the ultimate outcome—health (path vector p1)—as well as on the first layer of (three SES) mediator variables (path vector p2j) and the second layer of (eight stressor) mediator variables (path vector p3k ). Next, the first layer of (three SES) mediator variables has direct effects on both the ultimate outcome—health (path vector p4l)—and the second layer of (eight stressor) mediator variables (path vector p5m). Finally, the second layer of (stressor) mediator variables is specified to have a direct effect on the ultimate outcome, health (path vector p6n). In total, the simple mediation model comprises 12 equations: one for the ultimate outcome (health), three for the SES mediators (education, income, wealth), and eight for the stressor mediators (chronic stressors, financial strain, neighborhood disorder, neighborhood mistrust, three discrimination measures, and traumas).
Panel b of Figure 1 depicts the preferred moderated mediation model. It has all of the paths included in the simple mediation model, with the addition of the racialized moderation effects depicted as path vectors p4l’, p5m’, and p6n’. Formally, these moderation effects are defined as the coefficients of interaction terms calculated as the product of racialized group * mediator variables. Intuitively, this allows the effects of the mediators to vary by race, enabling tests of, for example, whether education has a larger protective effect on health among White compared with Black respondents. All significant moderating effects are noted in Figures 2 and 3. Because the moderated serial mediation models fit decisively better, we focus discussion on those results. The full results of both model sets depicted in Figure 1 are provided in online appendix B. Both the simple mediation model and the moderated mediation model specifications were fit for our set of three health outcomes. Also, for ease of presentation, the HRS data were subset to estimate racial comparison in two sets of models—the first comparing Black and White respondents and the second comparing Mexican American and White respondents. Thus, in total we estimated and present 12 models (2 race comparisons * 3 health outcomes * 2 model specifications). Given that the methodological aspect is a major contribution of this article, we have created an Open Science Framework directory containing all analysis scripts for the current study, which is publicly accessible at https://osf.io/hj6zd/.6
Fig. 2.
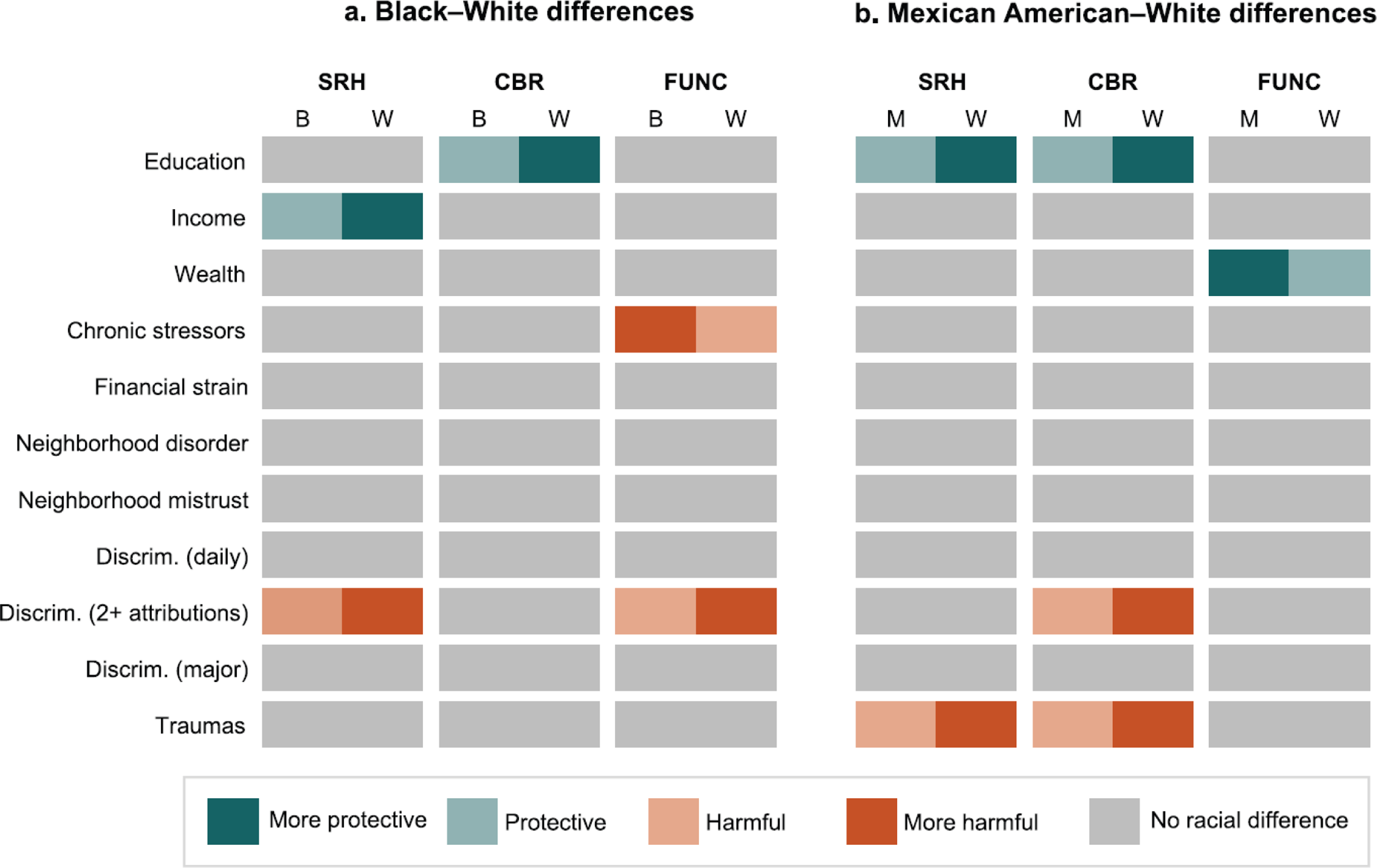
Moderation effects: racialized differences in associations among socioeconomic status, stressors, and health. Estimates of moderation are based on results from online appendix Tables B3 and B4. SRH = self-rated health. CBR = cumulative biological risk. FUNC = functional limitations. B = Black. W = White. M = Mexican American. Discrim. = discrimination.
Fig. 3.
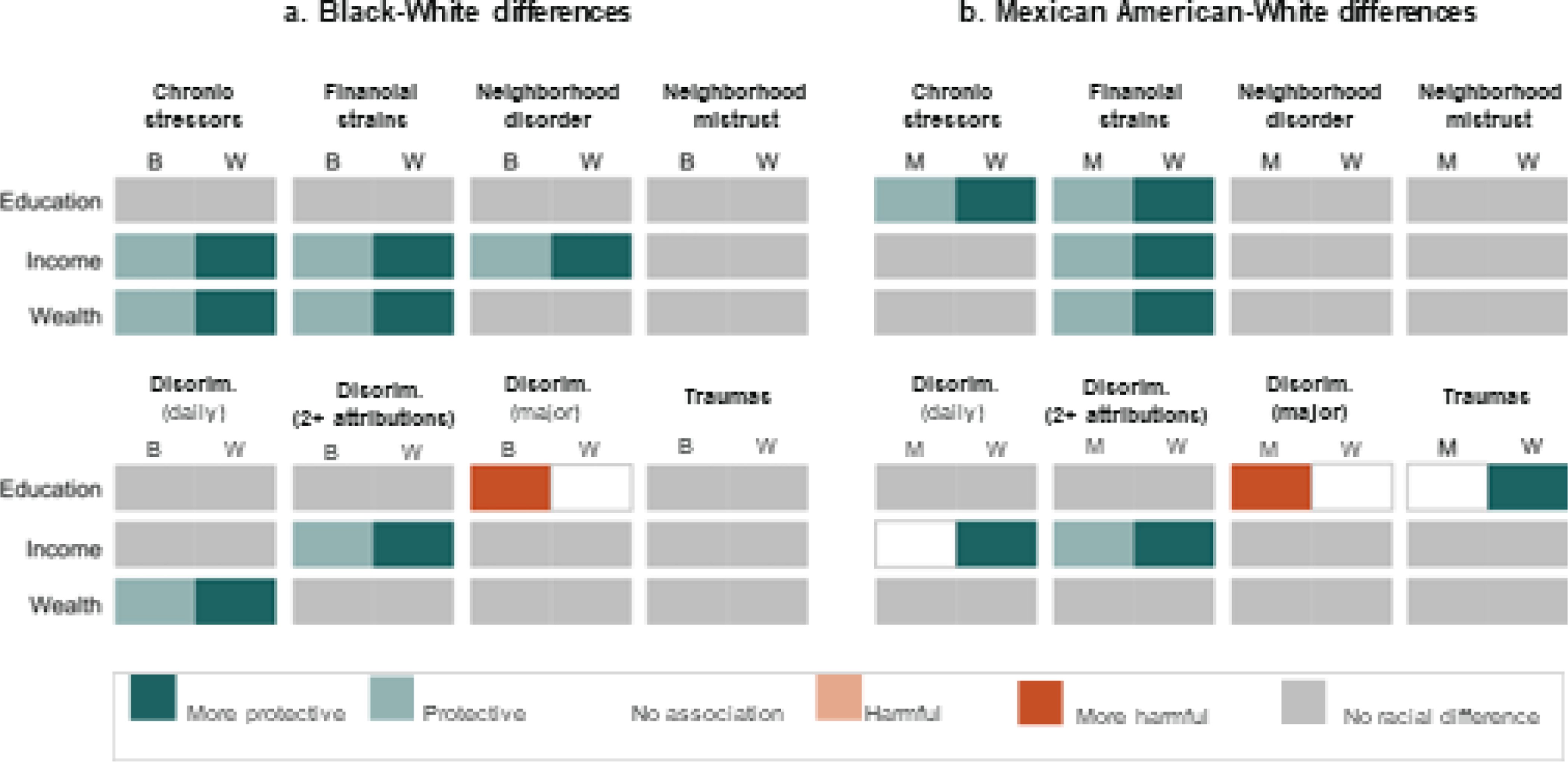
Moderation effects: racialized differences in associations among socioeconomic status and stressors. Estimates of moderation are based on results from online appendix Tables B3 and B4. B = Black. W = White. M = Mexican American. Discrim. = discrimination.
Results
Descriptive statistics are presented in Table 1. This table includes information on the means (and proportions) and variance of the study variables, as well as the extent to which they differ across racialized groups.
Table 1.
Weighted descriptive statistics, by racialized group
| Black | Mexican American | White | |
|---|---|---|---|
| Health Measures | |||
| Self-rated health | 3.10* | 3.26* | 2.67 |
| Cumulative biological risk (latent) | .11* | .10* | –.04 |
| Functional limitations | 3.37* | 3.10* | 2.53 |
| Mediators | |||
| Education (years) | 12.38* | 11.06* | 13.32 |
| Income (logged) | 10.01* | 9.69* | 10.82 |
| Wealth (logged) | 7.26* | 8.50* | 11.26 |
| Chronic stressors | 2.96* | 2.64 | 2.40 |
| Financial strain | 2.47* | 2.43* | 1.95 |
| Neighborhood disorder | 3.25* | 3.10* | 2.36 |
| Neighborhood mistrust | 3.16* | 2.99* | 2.42 |
| Discrim. (everyday) | 1.80* | 1.62 | 1.62 |
| Discrim. (2+ attributions) | .41* | .26 | .21 |
| Discrim. (major) | .86* | .43 | .47 |
| Traumas | 1.18 | 1.16 | 1.18 |
| Controls | |||
| Age | 64.28* | 63.31* | 66.32 |
| Female | .60* | .54 | .54 |
| Marital status (1 = married) | .51* | .76 | .75 |
| Private health insurance | .39* | .29* | .51 |
| Pharmacotherapy | .87* | .81 | .78 |
| n | 7,969 | 1,620 | 25,315 |
Notes: Means for dummy variables can be interpreted as the proportion of the sample coded 1 on that indicator. Values are based on information from respondents’ first interview. Welch–Satterthwaite t tests were computed for difference in means with unequal variances.
p < .05 for comparison of racial group to Whites
Racial Inequalities in SES and Stressors
Estimates from the SEM path analyses for the Black–White and Mexican American– White analyses are presented in online appendix Tables B1–B4. Findings provide evidence of several important patterns. First, results show that Blacks and Mexican Americans are disadvantaged relative to Whites on all of the measures of socioeconomic resources (education, income, and wealth). Second, compared with Whites, Blacks have elevated levels of exposure to seven of the eight measures of stressors (chronic stressors, financial strains, neighborhood disorder, neighborhood mistrust, everyday discrimination, multiple attributions of discrimination, and major discrimination), and Mexican Americans have elevated exposure to five of the stressors (chronic stressors, financial strains, neighborhood disorder, neighborhood mistrust, and multiple attributions of discrimination). Third, socioeconomic resources consistently have statistically significant protective effects on health. Fourth, although the effects vary across health outcomes, the majority of the stressors examined in the study are predictive of worse health. For example, chronic stressors, financial strains, neighborhood disorder, neighborhood mistrust, everyday discrimination, multiple attributions of discrimination, and traumatic events are associated with worse self-rated health.
Moderation Effects: Racial Differences in the Associations Among SES, Stressors, and Health
Figures 2 and 3 summarize the extent of racial moderation of the relationships among key study measures (more detailed information on moderation is included in online appendix Tables B3 and B4). Consistent with Hypothesis 1, the associations among socioeconomic resources, stressors, and health tend to be weaker among Blacks and Mexican Americans associations examined among covariates and the three health outcomes than among Whites. Indeed, 23% (13 of 57) of the are statistically different for Blacks compared with Whites (Figures 2 and 3). For example, the protective effects of income for self-rated health are weaker among Blacks relative to Whites. Similarly, education is less protective for Blacks than for Whites in terms of cumulative biological risk (panel a, Figure 2). In addition, the positive associations between reporting multiple attributions of discrimination and worse self-rated health and functional limitations are weaker among Blacks than among Whites. Interestingly, the deleterious effects of chronic stressors on functional limitations are greater among Blacks than among Whites.
Many of the associations between socioeconomic resources and exposure to stressors also vary by race (see panel a of Figure 3). For instance, education is positively associated with experiences of major discrimination among Blacks but not Whites. Furthermore, income is less protective for Blacks than for Whites in terms of exposure to chronic stressors, financial strains, neighborhood disorder, and multiple attributions of discrimination. There are also several instances where wealth is less protective for stress exposure for Blacks compared with Whites (e.g., chronic stressors, financial strain, and everyday discrimination).
Findings from Figures 2 and 3 also show that 25% (14 of 57) of the associations examined among socioeconomic factors, stressors, and health are statistically different for Mexican Americans compared with Whites. For example, education is less protective for Mexican Americans than for Whites with respect to self-rated health and cumulative biological risk; wealth is more protective of functional limitations among Mexican Americans (panel b, Figure 2). In addition, the positive relationships between traumatic events and worse self-rated health and cumulative biological risk are weaker for Mexican Americans than for Whites; a similar racialized pattern is evident for the deleterious effects of multiple attributions of discrimination on cumulative biological risk. Notably, education is predictive of greater exposure to major discrimination for Mexican Americans but not for Whites (panel b, Figure 3). Moreover, education is less protective for Mexican Americans in terms of exposure to chronic stressors and financial strain, and it is protective of exposure to traumatic events for Whites but not for Mexican Americans. Results also show that income is less protective for Mexican Americans than for Whites with respect to financial strain and multiple attributions of discrimination, and that it is protective of everyday discrimination for Whites but not for Mexican Americans (panel b, Figure 3). Furthermore, wealth is more protective of financial strain for Whites than for Mexican Americans. Collectively, the broad-based racial differences in the associations among SES, stressors, and health point to the importance of accounting for moderation processes when conducting mediation analyses in order to avoid biased estimates of mediation processes.
(Moderated) Mediation of Racial Inequalities in Health
Results from mediation analyses of health inequalities between Blacks and Whites (Table 2) and between Mexican Americans and Whites (Table 3) are presented graphically in Figure 4, for both moderated mediation and simple mediation. Consistent with Hypothesis 2, moderated mediation models show that, collectively, SES and stressors partially mediate racial inequities in health: Black–White inequalities in self-rated health, cumulative biological risk, and functional limitations are mediated by 75%, 37%, and 105%, respectively (72% average across outcomes); Mexican American–White inequalities in these outcomes are mediated by 67%, 53%, and 94%, respectively (71% average across outcomes).
Table 2.
Mediation estimates of Black-white in health, using moderated and simple mediation models (n=33,284)
| Self-Rated Health |
Cumulative Biological Risk |
Functional Limitations |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| A. Moderated Mediation | Beta | t Stat | SE | Beta | t Stat | SE | Beta | t Stat | SE |
| Total Effect | −0.18 *** | −14.13 | 0.01 | 0.18 *** | 13.02 | 0.01 | 0.12 *** | 9.26 | 0.01 |
| Indirect Effect | −0.14 *** | −20.04 | 0.01 | 0.07 *** | 13.37 | 0.01 | 0.13*** | 19.06 | 0.01 |
| Proportion Mediated | 0.75 | 0.37 | 1.05 | ||||||
| Mediators (proportion of total effect) | |||||||||
| Education | 0.19 *** | 11.42 | 0.02 | 0.08 *** | 6.90 | 0.01 | 0.22 *** | 9.93 | 0.02 |
| Income | 0.15 *** | 9.03 | 0.02 | 0.04 ** | 3.03 | 0.01 | 0.17 *** | 7.57 | 0.02 |
| Wealth | 0.17*** | 9.92 | 0.02 | 0.11 *** | 7.05 | 0.02 | 0.28 *** | 9.66 | 0.03 |
| Chronic stressors | 0.05 *** | 5.86 | 0.01 | 0.01 ** | 2.68 | 0.01 | 0.07 *** | 5.57 | 0.01 |
| 1 inancial strain | 0.04*** | 5.01 | 0.01 | 0.02 *** | 3.54 | 0.01 | 0.06 *** | 4.86 | 0.01 |
| Neighborhood disorder | 0.05 *** | 3.14 | 0.01 | 0.01 | 0.36 | 0.02 | 0.07 *** | 3.13 | 0.02 |
| Neighborhood mistrust | 0.05 *** | 4.28 | 0.01 | 0.01 | 1.07 | 0.01 | 0.04 * | 2.02 | 0.02 |
| Discrim. (daily) | 0.01* | 2.50 | 0.00 | 0.00 | 0.01 | 0.00 | 0.02 | 2.55 | 0.01 |
| Discrim. (2+ attributions) | 0.04 *** | 4.53 | 0.01 | 0.07 *** | 6.74 | 0.01 | 0.09 *** | 5.73 | 0.02 |
| Discrim. (major) | −0.01 | −0.93 | 0.01 | 0.01 | 1.35 | 0.01 | 0.03 * | 2.43 | 0.01 |
| Traumas | 0.01 | 0.83 | 0.01 | 0.00 | 0.77 | 0.00 | 0.01 | 0.85 | 0.01 |
| Self-Rated Health |
Cumulative Biological Risk |
Functional Limitations |
|||||||
| B. Simple Mediation | Beta | t Stat | SE | Beta | t Stat | SE | Beta | t Stat | SE |
|
| |||||||||
| Total Effect | −0.15 *** | −13 *** | 0.01 | 0.14 *** | 11.34 | 0.01 | 0.11 *** | 8.01 | 0.01 |
| Indirect Effect | −0.13 *** | −19.94 | 0.01 | 0.07 *** | 13.70 | 0.00 | 0.12 *** | 18.93 | 0.01 |
| Proportion Mediated | 0.S4 | 0.48 | 1.13 | ||||||
| Mediators {proportion of total effect) | |||||||||
| Education | 0.23 *** | 11.54 | 0.02 | 0.13 *** | 7.80 | 0.02 | 0.26 *** | 10.15 | 0.03 |
| Income | 0.18 *** | 9.72 | 0.02 | 0.05 *** | 3.30 | 0.02 | 0.20 *** | 7.98 | 0.02 |
| Wealth | 0.21 *** | 9.99 | 0.02 | 0.15 *** | 7.32 | 0.02 | 0.33 *** | 9.73 | 0.03 |
| Chronic stressors | 0.05 *** | 4.81 | 0.01 | 0.01 * | 2.56 | 0.01 | 0.06 *** | 4.61 | 0.01 |
| Financial strain | 0.02 * | 1.90 | 0.01 | 0.01 | 1.81 | 0.01 | 0.02 | 1.95 | 0.01 |
| Neighborhood disorder | 0.05 ** | 3.02 | 0.02 | 0.01 | 0.54 | 0.02 | 0.07 ** | 3.15 | 0.02 |
| Neighborhood miitmst | 0.06 *** | 4.50 | 0.01 | 0.02 | 1.14 | 0.01 | 0.04 * | 2.27 | 0.02 |
| Discrim. (daily) | 0.01 * | 2.18 | 0.00 | 0.00 | 0.10 | 0.00 | 0.02 * | 2.34 | 0.01 |
| Discrim. (2+ attributions) | 0.05 *** | 4.87 | 0.01 | 0.09 *** | 6.69 | 0.01 | 0.09 *** | 5.93 | 0.02 |
| Discrim. (major) | −0.01 | −0.99 | 0.01 | 0.02 | 1.44 | 0.01 | 0.03 * | 2.46 | 0.01 |
| Traumas | 0.00 | 0.51 | 0.01 | 0.00 | 0.45 | 0.00 | 0.01 | 0.53 | 0.01 |
p<.05;
p<.01;
p<.001
Table 3.
Mediation estimates of Mexican American-White in health, using moderated mediation models (n=26,935)
| Self-Rated Health |
Cumulative Biological Risk |
Functional Limitations |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| A. Moderated Mediation | Beta | t Stat | SE | Beta | t Stat | SE | Beta | t Stat | SE |
| Total Effect | −0.13 *** | 854 | 0.01 | 0.09 *** | 5.54 | 0.02 | 0.08 *** | 5.35 | 0.02 |
| Indirect Effect | −0.09 *** | −11.78 | 0.01 | 0.05 *** | 10.53 | 0.00 | 0.08 *** | 11.02 | 0.01 |
| Proportion Mediated | 0.67 | 0.53 | 0.94 | ||||||
| Mediators (proportion of total effect) | |||||||||
| Education | 0.32 *** | 10.54 | 0.03 | 0.26 *** | 7.80 | 0.03 | 0.39 *** | 9.31 | 0.04 |
| Income | 0.14 *** | 6.01 | 0.02 | 0.06** | 3.25 | 0.02 | 0.18 *** | 5.50 | 0.03 |
| Wealth | 0.08 *** | 5.07 | 0.02 | 0.08 *** | 4.62 | 0.02 | 0.15 *** | 5.10 | 0.03 |
| Chronic stressors | 0.04 * | 2.10 | 0.02 | 0.01 | 1.70 | 0.01 | 0.05 * | 2.03 | 0.02 |
| Financial stram | 0.02 * | 2.24 | 0.01 | 0.02 * | 2.12 | 0.01 | 0.04 * | 2.24 | 0.02 |
| Neighborhood disorder | 0.02 * | 2.29 | 0.01 | 0.01 | 0.96 | 0.01 | 0.03 ** | 2.62 | 0.01 |
| Neighborhood mistrust | 0.01 | 1.45 | 0.01 | 0.00 | 0.85 | 0.00 | 0.01 | 1.29 | 0.01 |
| Discrim. (daily) | 0.00 | 0.07 | 0.00 | 0.00 | 0.07 | 0.00 | 0.00 | 007 | 0.01 |
| Discrim. (2+ attributions) | 0.02 ** | 3.12 | 0.01 | 0.06 *** | 3.40 | 0.02 | 0.06 *** | 3.34 | 0.02 |
| Discrim. (major) | 0.00 | −0.49 | 0.00 | 0.00 | 0.53 | 0.00 | 0.00 | 0.53 | 0.00 |
| Traumas | 0.02 | 1.34 | 0.01 | 0.01 | 1.29 | 0.01 | 0.03 | 1.35 | 0.02 |
| Self-Rated Health |
Cumulative Biological Risk |
Functional Limitations |
|||||||
| B. Simple Mediation (without moderation) | Beta | t Stat | SE | Beta | t Stat | SE | Beta | t Stat | SE |
|
| |||||||||
| Total Effect | −0.10 *** | −8.16 | 0.01 | 0.06 *** | 4.50 | 0.01 | 0.06 *** | 4.48 | 0.01 |
| Indirect Effect | −0.07 *** | −12.20 | 0.01 | 0.04 *** | 10.20 | 0.00 | 0.06 *** | 11.04 | 0.01 |
| Proportion Mediated | 0.74 | 0.66 | 0.99 | ||||||
| Mediators (proportion of total effect) | |||||||||
| Education | 0.41 *** | 10.60 | 0.04 | 0.38 *** | 7.68 | 0.05 | 0.50 *** | 9.35 | 0.05 |
| Income | 0.18 *** | 6.33 | 0.03 | 0.09 *** | 3.29 | 0.03 | 0.23 *** | 5.73 | 0.04 |
| Wealth | 0.11 *** | 5.10 | 0.02 | 0.13 *** | 4.69 | 0.03 | 0.20 *** | 5.05 | 0.04 |
| Chronic stressors | 0.01 | 0.48 | 0.02 | 0.00 | 0.43 | 0.01 | 0.01 | 0.45 | 0.02 |
| Financial strain | −0.01 | −0.66 | 0.01 | −0.01 | −0.67 | 0.01 | −0.01 | −0.65 | 0.02 |
| Neighborhood disorder | 0.02 * | 2.17 | 0.01 | 0.01 | 0.97 | 0.01 | 0.03 * | 2.42 | 0.01 |
| Neighborhood mistrust | 0.00 | 0.40 | 0.01 | 0.00 | 0.38 | 0.00 | 0.00 | 0.41 | 0.01 |
| Diserim. (daily) | 0.00 | −1.06 | 0.00 | 0.00 | −0.22 | 0.00 | −0.01 | −1.11 | 0.01 |
| Diserim. (2+ attributions) | 0.02 * | 2.44 | 0.01 | 0.05 * | 2.49 | 0.02 | 0.04 * | 2.51 | 0.02 |
| Discrim. (major) | 0.00 | 0.50 | 0.00 | 0.00 | −0.53 | 0.00 | 0.00 | −0.52 | 0.00 |
| Traumas | 0.00 | 0.02 | 0.01 | 0.00 | 0.00 | 0.01 | 0.00 | 0.02 | 0.02 |
p<.05;
p<.01;
p<.001
Fig. 4.

Percentage mediation of racial inequities by socioeconomic status and stressors (collectively), using moderated mediation and simple mediation models. Estimates of mediation are based on results from Tables 2 and 3. Estimates are for the extent of collective mediation for education, income, wealth, chronic stressors, financial strains, neighborhood disorder, neighborhood mistrust, everyday discrimination, multiple attributions of discrimination, major discrimination, and traumas. B = Black. W = White. M = Mexican American.
We also find strong support for Hypothesis 4—that simple mediation models that ignore differential effects by race overstate the extent to which unequal SES and stress exposure collectively account for racial health inequities. Specifically, compared with moderated mediation analyses, simple mediation models overestimated the magnitude of mediation of Black–White inequities in self-rated health by 12% [(84% – 75%) / 75%], in cumulative biological risk by 30% [(48% – 37%) / 37%], and in functional limitations by 8% [(113% – 105%) / 105%]. Simple mediation models overestimated the degree of mediation of Mexican American–White inequities in self-rated health by 10% [(74% – 67%) / 67%], in cumulative biological risk by 25% [(66% – 53%) / 53%], and in functional limitations by 5% [(99% – 94%) / 94%]. Averaging across health measures in this study, simple mediation models overestimated the mediation of Black–White inequities in health by 16%, and they overestimated the mediation of Mexican American–White inequities by 13%. Overall, findings that the magnitude of mediation tends to vary depending on whether differential effects are taken into account underscore the utility of moderated mediation analyses.
Figure 5 (as well as Tables 2 and 3) presents detailed estimates of the extent to which individual measures of socioeconomic resources and stressors mediate racial inequalities for each of the health measures. Although the relative contributions of these factors to racial inequalities vary across the health outcomes and groups, taken together, findings provide support for Hypothesis 3a (among socioeconomic factors, education and wealth are particularly strong mediators) and Hypothesis 3b (among stressors, the strongest mediators are those that are recurring). Averaging across health outcomes, the relative contributions of each of these factors to Black–White health inequities are (panel a, Figure 5): wealth (19%), education (16%), income (12%), multiple attributions for discrimination (7%), chronic stressors (4%), financial strain (4%), neighborhood disorder (4%), neighborhood mistrust (3%), major discrimination (1%), everyday discrimination (1%), and traumas (0%). Corresponding estimates of the average contributions of these factors to health inequities between Mexican Americans and Whites are (panel b, Figure 5): education (32%), income (13%), wealth (10%), multiple attributions of discrimination (5%), chronic stressors (3%), financial strain (3%), neighborhood disorder (2%), neighborhood mistrust (0%), everyday discrimination (0%), major discrimination (0%), and traumas (0%). It is also noteworthy that socioeconomic factors mediate a greater proportion of racial inequities than stressors—a pattern that is consistent across each racial comparison and each health outcome. On average, socioeconomic factors account for 47% of Black–White inequities versus 23% for stressors; socioeconomic factors mediate 55% of Mexican American–White inequities versus 13% for stressors.
Fig. 5.
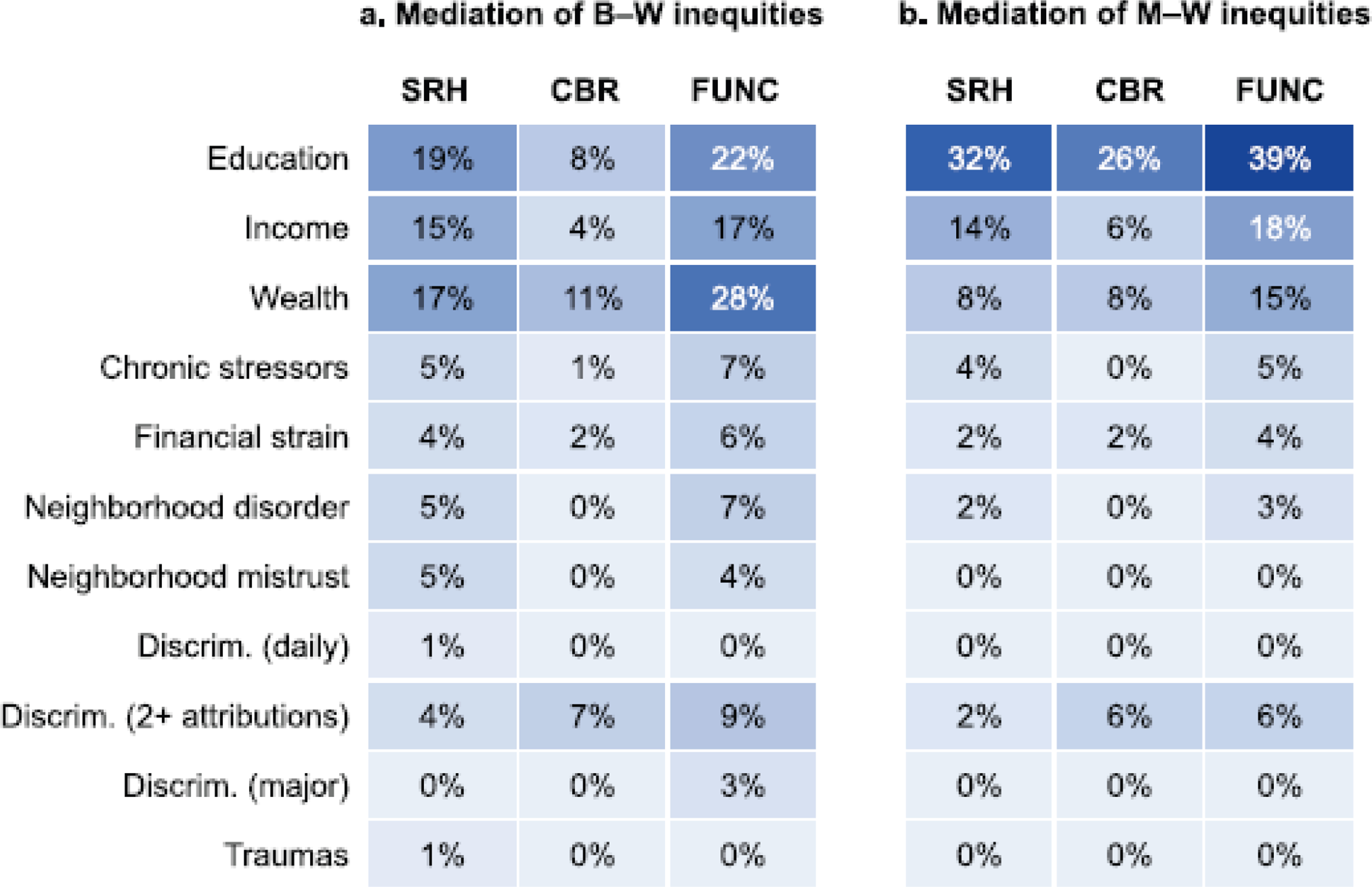
Percentage mediation of racial inequities by socioeconomic status and stressors (individually), using moderated mediation models. Estimates of mediation are based on results from Tables 2 and 3. SRH = self-rated health. CBR = cumulative biological risk. FUNC = functional limitations. B = Black. W = White. M = Mexican American. Discrim. = discrimination.
Discussion
This study extends prior research by formally testing the extent to which racial stratification in socioeconomic resources and stress processes—collectively and individually—mediate racialized inequities in multiple health outcomes among a diverse, nationally representative sample of older adults. In doing so, this study widens our view of the social determinants of health by improving our understanding of social pathways undergirding racial inequities in health. Findings yield theoretical contributions by showing how the SES–health gradient and stress processes are racialized, substantive contributions by quantifying the extent of mediation and the relative importance of various individual factors, and methodological contributions by showing how simple mediation approaches overestimate the collective roles of socioeconomic resources and stressors in accounting for racial health inequities.
Key findings show how relationships among SES, stressors, and health are racialized, and how racial differences in the health effects of these social factors affect mediation processes. Consistent with Hypothesis 1, associations among socioeconomic resources, stressors, and health tended to be weaker among Blacks and Mexican Americans than among Whites. Indeed, substantial proportions of the relationships among covariates and health outcomes were statistically different for Black (23%) and Mexican American people (25%) relative to Whites. Simple mediation analyses that did not adjust for racial differences in the impacts of SES and stressors overestimated the extent to which these factors mediate racialized health inequities by between 5% and 30% (compared with moderated mediation analyses). A key implication is that prior research on the roles of SES and stressors has been able to account for less of the observed racial inequities in health than previously assumed. These findings also highlight the fact that, when estimating the extent to which social factors mediate racial health inequities, it is important to simultaneously examine (1) how racialized inequities in health are contingent on SES and stressors, and (2) how the relationships among SES, stressors, and health are conditional on race.
Results also reveal that socioeconomic inequality along racial lines is a major contributor to inequities in health, providing support for our second hypothesis. For instance, if Black and White older adults had comparable levels of education, income, and wealth, Black–White inequities in self-rated health, cumulative biological risk, and functional limitations would be reduced by 51%, 23%, and 67%, respectively (analogous percentages for Mexican American–White inequities are 54%, 40%, and 72%). Findings that education and wealth are particularly strong mediators of racial inequalities in health are in line with Hypothesis 3a.
The SES–health gradient was weaker among minoritized groups, consistent with marginalization-related diminished returns theory (Assari et al. 2020) and our Hypothesis 1. For example, in several instances, education and income were less protective for the health of Blacks and Mexican Americans than they were for Whites. These findings align with research showing that even among Whites and racialized minorities with comparable levels of SES, minoritized groups receive lower quality educations (Tyson and Lewis 2021), live in less healthy neighborhoods (Massey and Denton 1993), and are exposed to greater levels of discrimination (e.g., harassment by police, predatory lending, and being passed over for jobs and promotions) and other stressors (Forman et al. 1997; Williams 2018). These conditions dilute the protective effects of socioeconomic resources (Assari 2018; Cobb et al. 2020; Colen et al. 2018). Thus, accounting for racial differences in the effects of socioeconomic factors on health is critical for accurately estimating mediation processes. Racialized exposure to stressors is also a key factor underlying racial inequities in health, in line with Hypothesis 2. This study is among the first to quantify the collective and individual contributions of an array of stressors to racial inequities in health among older adults. Findings show that Blacks and Mexican Americans have elevated exposure to a wide range of stressors that have pernicious effects on health. Of the stressors examined, unequal exposure to chronic stressors, financial strains, deleterious neighborhood conditions, and multiple attributions of discrimination account for a considerable portion of racial inequities in health. These findings are consistent with Hypothesis 3b as well as research showing that social stressors that are recurring in major social roles or domains are especially harmful (Thoits 2010).
We also find evidence that the effects of stressors vary by race. In numerous instances, the relationships between stressors (e.g., multiple attributions of everyday discrimination and traumatic events) and health are weaker for Black and Mexican American people than for Whites. These findings are in line with research showing that, compared with older Whites, their Black and Mexican American counterparts appraise exposure to a range of social stressors as less stressful (Brown et al. 2020). When considering possible explanations for racial differences in vulnerability in the face of stressors, it is important to note that current cohorts of older racially subordinated groups came of age during Jim Crow and have endured decades of disproportionate exposure to overt and subtle forms of discrimination and other stressors. As a result, older Black and Mexican American people in this sample are exceptional survivors who may be especially resilient or adept at coping with the harmful effects of stressors (Barnes et al. 2008; Keith 2014). Because Whites occupy a dominant position within the racial hierarchy and experience discrimination far less frequently than other racial groups, on occasions when they perceive that they have been treated unfairly, they may experience inordinate distress (Williams 2018). Experiencing dissonance between perceptions of so-called “reverse discrimination” and feelings of entitlement to racialized privileges customarily afforded to Whites may be stressful and harmful for health (Malat et al. 2018; Metzl 2020).
Our results also reveal that the relationships between socioeconomic factors and stressors are weaker for Blacks and Mexican Americans than for their White counterparts. These weaker protective effects are likely due to greater cumulative exposure to various racialized social disadvantages (Assari 2018; Pearson 2008). For example, acquiring socioeconomic resources often involves learning, working, and living in predominantly White spaces, which increases exposure to discrimination (Assari and Lankarani 2016; DeAngelis 2022).
Collectively, the racialized socioeconomic resources and stress processes examined in this study mediate an average of 72% of Black–White and 71% of Mexican American–White health inequities (with variation across health outcomes). Findings indicate that socioeconomic stratification is a key social pathway leading to racial inequities in health. On average, socioeconomic resources mediate Black–White health inequities twice as much as stressors, and they mediate Mexican American– White inequities four times as much as stressors. It is important to note that the role of stressors in shaping health inequalities along racial lines may be underestimated in this study given the absence of measures of salient racialized stressors—for example, incarceration and police brutality (Lee et al. 2023; Wildeman and Wang 2017), anticipatory discrimination stress (Hicken et al. 2014; Jochman et al. 2019), and vicarious stress exposure through social networks (Lewis et al. 2015). Nonetheless, findings suggests that structural interventions aimed at reducing racial stratification in socioeconomic resources are likely to be particularly efficacious for addressing health inequities.
Within the context of a racialized social system such as the United States, it is not surprising that SES and stress factors do not fully mediate racial inequities in health. Indeed, systemic racism is theorized to generate inequities through a range of other “pathways of embodiment”—for example, pathogenic living conditions, social deprivation, political exclusion, inadequate health care, and lack of freedom and autonomy (Krieger 2012; Phelan and Link 2015; Williams et al. 2019). A growing body of research shows how the health of racially subordinated groups in the United States is harmed by many manifestations of systemic racism, such as racialized policies, residential segregation and place-based racial inequities in political participation, dis-enfranchisement, unequal employment and educational opportunities, and judicial treatment (Brown et al. 2022; Gee and Hicken 2021; Hardeman et al. 2022; Homan and Brown 2022; Sewell 2016). This emergent literature points to the importance of understanding how systemic racism affects health directly as well as indirectly through an array of social pathways (Brown and Homan 2023).
Several limitations of this study warrant discussion. First, given racial inequities in morbidity and mortality in midlife and the fact that the HRS sample is limited to individuals over the age of 50, estimates of racial inequities in health may be conservative (Hayward et al. 2000). Because of mortality selection, respondents in general—and Black respondents in particular—who survive to older ages tend to be relatively advantaged in terms of social determinants of health and overall well-being. Accordingly, results should be interpreted as conditional upon survival to mid-life. Second, owing to data limitations, this study is unable to fully capture life course processes shaping health inequities. Cumulative adversity and stressors across the life course negatively affect subsequent attainment processes, stress exposure, and, ultimately, late-life health (Ferraro et al. 2016; Gee et al. 2012; Turner et al. 2016). Further research is needed to understand the life course processes (e.g., sensitive periods, pathways, cumulative exposures) through which SES and stressors differentially shape health across racialized groups (Walsemann et al. 2016). Third, this study is not able to establish causality among study variables. Future research should utilize longitudinal data and causal inference approaches to examine how racialized systems shape health over time (Graetz et al. 2022). Fourth, it is beyond the scope of this study to determine reasons for heterogeneity in mediation estimates across groups and health measures. It is important to note that the experiences of different racialized groups are distinct, as are the etiologies of racial inequities in various health outcomes (Williams 2018) and the social factors that most strongly influence a given health outcome.
Additionally, intersectional perspectives highlight the importance of investigating whether racialized health patterns and their social underpinnings may be shaped by gender inequities and a host of other social factors (Brown et al. 2016; Hudson et al. 2013). We conducted supplemental analyses to examine this proposition and found mixed evidence of gendered mediation processes (see online appendix C for details). While this is an important topic, an in-depth examination of it is beyond the scope of this study. Future research should take a systematic approach to examining whether, how, and why racialized mediation processes are shaped by a range of social statuses and systems of oppression, such as sexism, colorism, and nativism (Homan et al. 2021; Laster Pirtle and Wright 2021).
Taken together, these results enhance our understanding of ways in which the U.S. racialized social system undermines the health of older Black and Mexican American people. More specifically, findings highlight how socioeconomic stratification and stress processes are key social pathways contributing to racial inequities in health. Results also show that the impacts of SES and stressors on health vary by race, and that mediation analyses that do not simultaneously account for these racialized processes yield biased overestimates of the extent of mediation. More accurate estimates from moderated mediation analyses in this study show that we know less about the social underpinnings of racial health inequities among older adults than previously thought. This underscores the importance of drawing on race theories in tandem with analytically integrated moderation and mediation processes to better understand the racialized social determinants of population health. More broadly, our findings point to the need for researchers to think more seriously about how opportunities for good health are shaped by one’s position in the U.S. racial hierarchy. Quantifying the direct and indirect effects of systemic racism via proximal social determinants of health represents a critical next frontier in research on racialized health inequities.
Supplementary Material
Acknowledgments
This research received support from three National Institute on Aging grants: P30 AG034424 (awarded to the Center for Population Health and Aging at Duke University), P30 AG066615 (awarded to the Carolina Population Center at the University of North Carolina at Chapel Hill), and 2R24AG045061-06 (awarded to the Network on Life Course Health Dynamics and Disparities in 21st Century America). We would also like to thank Dr. Eric Monson for his assistance with visualizing data.
Footnotes
Hereafter, non-Hispanic Black and non-Hispanic White groups will be referred to as Black and White, respectively. Furthermore, although race and ethnicity are conceptually distinct and “Mexican American” is often regarded as an ethnic category, we use racial terminology to describe all groups in this study (including Mexican Americans). We do so because “Mexican American” is a racialized category. Research shows that Mexican Americans in the United States experience processes of racialization (e.g., racial subordination and exclusion) and that many of them consider themselves to be part of a racial group (Flores-Gonzáles et al. 2014).
While there is debate about whether self-rated health captures an equivalent phenomenon across racialized groups, it is commonly used in research on racial inequities in health, and there is considerable evidence of within-group reliability and validity of self-rated health among U.S.-born non-Hispanic Black, Mexican American, and non-Hispanic White populations (Assari and Lankarani 2016, 2017; Brown et al. 2016; Erving and Zajdel 2022; Liang et al. 2010). Moreover, ancillary analyses indicated that self-rated health is predictive of morbidity among each of the racial groups in this study.
Supplemental analyses showed that findings are comparable whether we use this approach or clinical cutoffs.
We estimated the CFA as a single-factor linear SEM measurement model with the eight indicators described above, using full information maximum likelihood (FIML). In accordance with standard psychometric practice (Bollen 1989), the factor variance of this measurement model was fixed at one, all indicator error variances were freely estimated, and two highly theoretically indicated error covariances were specified— one for the systolic and diastolic blood pressure indicators, and a second for the total cholesterol and HDL indicators. All factor loadings were statistically significant (p < .001) and in the expected direction. The omnibus model fit of the measurement model was very good (root mean square error of approximation [RMSEA] = 0.03, p < .001 [H0: RMSEA > 0.05]; comparative fit index = 0.95; Tucker–Lewis index = 0.92).
Income and wealth equivalencies across households were created by dividing income and wealth by the square root of household member size (Brady 2009). Furthermore, income and wealth measures are logged to reduce the skewness and kurtosis of their distributions.
This public OSF directory contains Stata scripts coding the structural equation models of the primary analysis— simple mediation and moderated mediation models— as well as ancillary analyses described in the Discussion section.
References
- Aneshensel CS (2005). Research in mental health: Social etiology versus social consequences. Journal of Health and Social Behavior, 46, 221–228. [DOI] [PubMed] [Google Scholar]
- Assari S. (2018). Health disparities due to diminished return among Black Americans: Public policy solutions. Social Issues and Policy Review, 12, 112–145. [Google Scholar]
- Assari S, Cobb S, Saqib M, & Bazargan M. (2020). Diminished returns of educational attainment on heart disease among Black Americans. Open Cardiovascular Medical Journal, 14, 5–12. 10.2174/1874192402014010005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assari S, & Lankarani MM (2016). Association between stressful life events and depression: Intersection of race and gender. Journal of Racial and Ethnic Health Disparities, 3, 349–356. [DOI] [PubMed] [Google Scholar]
- Assari S, & Lankarani MM (2017). Demographic and socioeconomic determinants of physical and mental self-rated health across 10 ethnic groups in the United States. International Journal of Epidemiological Research, 3(12), 185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayalon L, & Gum AM (2011). The relationships between major lifetime discrimination, everyday discrimination, and mental health in three racial and ethnic groups of older adults. Aging & Mental Health, 15, 587–594. [DOI] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, & Bassett MT (2017). Structural racism and health inequities in the USA: Evidence and interventions. Lancet, 389, 1453–1463. [DOI] [PubMed] [Google Scholar]
- Barnes LL, Medes de Leon CF, Lewis TT, Bienias JL, Wilson RS, & Evans DA (2008). Perceived discrimination and mortality in a population-based study of older adults. American Journal of Public Health, 98, 1241–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CN, Sacks TK, Thomas Tobin CS, & Thorpe RJ Jr. (2020). Racial non-equivalence of socioeconomic status and self-rated health among African Americans and Whites. SSM–Population Health, 10, 100561. 10.1016/j.ssmph.2020.100561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen C. (2016). The role of socioeconomic factors in Black–White health inequities across the life course: Point-in-time measures, long-term exposures, and differential health returns. Social Science & Medicine, 170, 63–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen C, & Hummer RA (2019). Longer—but harder—lives?: The Hispanic health paradox and the social determinants of racial, ethnic, and immigrant–native health disparities from mid-through late-life. Journal of Health and Social Behavior, 60, 434–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA (1989). Structural equations with latent variables. New York, NY: John Wiley and Sons. [Google Scholar]
- Bonilla-Silva E. (1997). Rethinking racism: Toward a structural interpretation. American Sociological Review, 62, 465–480. [Google Scholar]
- Bonilla-Silva E. (2017). Racism without racists: Color-blind racism and the persistence of racial inequality in the United States (5th ed.). Lanham, MD: Rowman & Littlefield. [Google Scholar]
- Brady D. (2009). Rich democracies, poor people: How politics explain poverty. New York, NY: Oxford University Press. [Google Scholar]
- Bratter JL, & Gorman BK (2011). Is discrimination an equal opportunity risk? Racial experiences, socioeconomic status, and health status among Black and White adults. Journal of Health and Social Behavior, 52, 365–382. [DOI] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen E, Miller GE, Kogan SM, & Beach SRH (2013). Is resilience only skin deep? Rural African Americans’ socioeconomic status-related risk and competence in preadolescence and psychological adjustment and allostatic load at age 19. Psychological Science, 24, 1285–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LL, Mitchel UA, & Ailshire JA (2020). Disentangling the stress process: Race and ethnic differences in the experience of chronic stress among older adults. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75, 650–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TH (2016). Diverging fortunes: Racial/ethnic inequality in wealth trajectories in middle and late life. Race and Social Problems, 8, 29–41. [Google Scholar]
- Brown TH (2018). Racial stratification, immigration, and health inequality: A life course–intersectional approach. Social Forces, 96, 1507–1540. [Google Scholar]
- Brown TH, & Homan P. (2023). The future of social determinants of health: Looking upstream to structural drivers. Milbank Quarterly, 101(S1), 36–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TH, Kamis C, & Homan P. (2022). Empirical evidence on structural racism as a driver of racial inequalities in COVID-19 mortality. Frontiers in Public Health, 10, 1007053. 10.3389/fpubh.2022.1007053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TH, Richardson LJ, Hargrove TW, & Thomas CS (2016). Using multiple-hierarchy stratification approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. Journal of Health and Social Behavior, 57, 200–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A, Converse PE, & Rodgers WL (1976). The quality of American life: Perceptions, evaluations, and satisfactions. New York, NY: Russell Sage Foundation. [Google Scholar]
- Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, . . . Zhao L. (2018). Inflammatory responses and inflammation-associated diseases in organs. Oncotarget, 9, 7204–7218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb RJ, Parker LJ, & Thorpe RJ Jr. (2020). Self-reported instances of major discrimination, race/ethnicity, and inflammation among older adults: Evidence from the Health and Retirement Study. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 75, 291–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colen CG, Krueger PM, & Boettner BL (2018). Do rising tides lift all boats? Racial disparities in health across the lifecourse among middle-class African Americans and Whites. SSM–Population Health, 6, 125–135. 10.1016/j.ssmph.2018.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Alley DE, Karlamangla A, & Seeman T. (2007). Hispanic paradox in biological risk profiles. American Journal of Public Health, 97, 1305–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeAngelis RT (2020). Striving while Black: Race and the psychophysiology of goal pursuit. Journal of Health and Social Behavior, 61, 24–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeAngelis RT (2022). Moving on up? Neighborhood status and racism-related distress among Black Americans. Social Forces, 100, 1503–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado R, & Stefancic J. (2017). Critical race theory: An introduction (3rd ed.). New York: New York University Press. [Google Scholar]
- Du Bois WEB (1899). The Philadelphia Negro: A social study. Philadelphia, PA: University of; Pennsylvania. [Google Scholar]
- Eisenberger NI (2013). Social ties and health: A social neuroscience perspective. Current Opinion in Neurobiology, 23, 407–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erving CL, & Zajdel R. (2022). Assessing the validity of self-rated health across ethnic groups: Implications for health disparities research. Journal of Racial and Ethnic Health Disparities, 9, 462–477. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Schafer MH, & Wilkinson LR (2016). Childhood disadvantage and health problems in middle and later life: Early imprints on physical health? American Sociological Review, 81, 107–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores-Gonzáles N, Aranda E, & Vaquera E. (2014). “Doing race”: Latino youth’s identities and the politics of racial exclusion. American Behavioral Scientist, 58, 1834–1851. [Google Scholar]
- Forman TA (2003). The social psychological costs of racial segmentation in the workplace: A study of African Americans’ well-being. Journal of Health and Social Behavior, 44, 332–352. [PubMed] [Google Scholar]
- Forman TA, Williams DR, & Jackson JS (1997). Race, place, and discrimination. In Gardner C. (Ed.), Perspectives on social problems (pp. 231–261). Greenwich, CT: JAI Press. [Google Scholar]
- Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, . . . Slavich GM (2019). Chronic inflammation in the etiology of disease across the life span. Nature Medicine, 25, 1822–1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia MA, Downer B, Chiu C-T, Saenz JL, Rote S, & Wong R. (2019). Racial/ethnic and nativity differences in cognitive life expectancies among older adults in the United States. Gerontologist, 59, 281–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaydosh L, Schorpp KM, Chen E, Miller GE, & Harris KM (2018). College completion predicts lower depression but higher metabolic syndrome among disadvantaged minorities in young adulthood. Proceedings of the National Academy of Sciences, 115, 109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, & Ford CL (2011). Structural racism and health inequities: Old issues, new directions. Du Bois Review, 8, 115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, & Hicken MT (2021). Commentary—Structural racism: The rules and relations of inequity. Ethnicity & Disease, 31(Suppl. 1), 293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Walsemann KM, & Brondolo E. (2012). A life course perspective on how racism may be related to health inequities. American Journal of Public Health, 102, 967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golash-Boza T. (2016). A critical and comprehensive sociological theory of race and racism. Sociology of Race and Ethnicity, 2, 129–141. [Google Scholar]
- Goosby BJ, Cheadle JE, & Mitchell C. (2018). Stress-related biosocial mechanisms of discrimination and African American health inequities. Annual Review of Sociology, 44, 319–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graetz N, Boen CE, & Esposito MH (2022). Structural racism and quantitative causal inference: A life course mediation framework for decomposing racial health disparities. Journal of Health and Social Behavior, 63, 232–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TL, & Darity WA Jr. (2010). Under the skin: Using theories from biology and the social sciences to explore the mechanisms behind the Black–White health gap. American Journal of Public Health, 100(Suppl. 1), S36–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grollman EA (2014). Multiple disadvantaged statuses and health: The role of multiple forms of discrimination. Journal of Health and Social Behavior, 55, 3–19. [DOI] [PubMed] [Google Scholar]
- Haas SA, & Rohlfsen L. (2010). Life course determinants of racial and ethnic disparities in functional health trajectories. Social Science & Medicine, 70, 240–250. [DOI] [PubMed] [Google Scholar]
- Hardeman RR, Homan PA, Chantarat T, Davis BA, & Brown TH (2022). Improving the measurement of structural racism to achieve antiracist health policy. Health Affairs, 41, 179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward MD, Miles TP, Crimmins EM, & Yang Y. (2000). The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review, 65, 910–930. [Google Scholar]
- Hicken MT, Lee H, Morenoff J, House JS, & Williams DR (2014). Racial/ethnic disparities in hypertension prevalence: Reconsidering the role of chronic stress. American Journal of Public Health, 104, 117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan P, Brown TH, & King B. (2021). Structural intersectionality as a new direction for health disparities research. Journal of Health and Social Behavior, 62, 350–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homan PA, & Brown TH (2022). Sick and tired of being excluded: Structural racism in disenfranchisement as a threat to population health equity. Health Affairs, 41, 219–227. [DOI] [PubMed] [Google Scholar]
- Horowitz MA, Cattaneod A, Cattane N, Lopizzo N, Tojo L, Bakunina N, Pariante CM (2020). Glucocorticoids prime the inflammatory response of human hippocampal cells through up-regulation of inflammatory pathways. Brain Behavior & Immunity, 87, 777–794. [DOI] [PubMed] [Google Scholar]
- Hudson DL, Neighbors HW, Geronimus AT, & Jackson JS (2016). Racial discrimination, John Henryism, and depression among African Americans. Journal of Black Psychology, 42, 221–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson DL, Puterman E, Bibbins-Domingo K, Matthews KA, & Adler NE (2013). Race, life course socioeconomic position, racial discrimination, depressive symptoms and self-rated health. Social Science & Medicine, 97, 7–14. [DOI] [PubMed] [Google Scholar]
- Idler EL, & Benyamini Y. (1997). Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior, 38, 21–37. [PubMed] [Google Scholar]
- Jochman JC, Cheadle JE, Goosby BJ, Tomaso C, Kozikowski C, & Nelson T. (2019). Mental health outcomes of discrimination among college students on a predominately White campus: A prospective study. Socius, 5. 10.1177/2378023119842728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juster RP, McEwen BS, & Lupien SJ (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews, 35, 2–16. [DOI] [PubMed] [Google Scholar]
- Jylhä M. (2009). What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science & Medicine, 69, 307–316. [DOI] [PubMed] [Google Scholar]
- Kao G, & Thompson JS (2003). Racial and ethnic stratification in educational achievement and attainment. Annual Review of Sociology, 29, 417–442. [Google Scholar]
- Karlson KB, Holm A, & Breen R. (2012). Comparing regression coefficients between same-sample nested models using logit and probit: A new method. Sociological Methodology, 42, 274–301. [Google Scholar]
- Keith VM (2014). Stress, discrimination, and coping in late life. In Whitfield KE & Baker TA (Eds.), Handbook of minority aging (pp. 65–84). New York, NY: Springer Publishing Company. [Google Scholar]
- Krause N, Shaw BA, & Cairney J. (2004). A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychology and Aging, 19, 637–648. [DOI] [PubMed] [Google Scholar]
- Krieger N. (2012). Methods for the scientific study of discrimination and health: An ecosocial approach. American Journal of Public Health, 102, 936–944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laster Pirtle WN, & Wright T. (2021). Structural gendered racism revealed in pandemic times: Inter-sectional approaches to understanding race and gender health inequities in COVID-19. Gender & Society, 35, 168–179. [Google Scholar]
- Lee H, Larimore S, & Esposito M. (2023). Policing and population health: Past, present, and future. Milbank Quarterly, 101(S1), 119–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, & Williams DR (2015). Self-reported experiences of discrimination and health: Scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology, 11, 407–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J, Quiñones AR, Bennett JM, Ye W, Xu X, Shaw BA, & Ofstedal MB (2010). Evolving self-rated health in middle and old age: How does it differ across Black, Hispanic, and White Americans? Journal of Aging and Health, 22, 3–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little TD, Card NA, Bovaird JA, Preacher KJ, & Crandall CS (2007). Structural equation modeling of mediation and moderation with contextual factors. In Little TD, Bovaird JA, & Card NA (Eds.), Modeling contextual effects in longitudinal studies (pp. 207–230). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Liu Y-Z, Wang Y-X, & Jiang C-L (2017). Inflammation: The common pathway of stress-related diseases. Frontiers in Human Neuroscience, 11, 316. 10.3389/fnhum.2017.00316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loehlin JC (2004). Latent variable models: An introduction to factor, path, and structural equation analysis. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology, 58, 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malat J, Mayorga-Gallo S., & Williams DR. (2018). The effects of Whiteness on the health of Whites in the USA. Social Science & Medicine, 199, 148–156. [DOI] [PubMed] [Google Scholar]
- Massey DS, & Denton NA (1993). American apartheid: Segregation and the making of the underclass. Cambridge, MA: Harvard University Press. [Google Scholar]
- McCarty R. (2016). Learning about stress: Neural, endocrine and behavioral adaptations. Stress, 19, 449–475. [DOI] [PubMed] [Google Scholar]
- Metzl JM (2020). Dying of Whiteness: How the politics of racial resentment is killing America’s heart-land. New York, NY: Basic Books. [Google Scholar]
- Millar RJ (2020). Neighborhood cohesion, disorder, and physical function in older adults: An examination of racial/ethnic differences. Journal of Aging and Health, 32, 1133–1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omi M, & Winant H. (2015). Racial formation in the United States (3rd ed.). New York, NY: Routledge. [Google Scholar]
- O’Rand AM, & Lynch SM (2018). Socioeconomic status, health and mortality in aging populations. In Hayward MD & Majmundar MK (Eds.), Future directions for the demography of aging:Proceedings of a workshop (pp. 67–95). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Ortman JM, Velkoff VA, & Hogan H. (2014). An aging nation: The older population in the United States (Current Population Reports, No. P25-1140). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, & Meersman SC (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46, 205–219. [DOI] [PubMed] [Google Scholar]
- Pearson JA (2008). Can’t buy me Whiteness: New lessons from the Titanic on race, ethnicity, and health. Du Bois Review, 5, 27–48. [Google Scholar]
- Phelan JC, & Link BG (2015). Is racism a fundamental cause of inequalities in health? Annual Review of Sociology, 41, 311–330. [Google Scholar]
- Phelan JC, Link BG, & Tehranifar P. (2010). Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. Journal of Health and Social Behavior, 51(Suppl.), S28–S40. 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, & Hayes AF (2007). Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research, 42, 185–227. [DOI] [PubMed] [Google Scholar]
- Reskin B. (2012). The race discrimination system. Annual Review of Sociology, 38, 17–35. [Google Scholar]
- Roberts D. (2011). Fatal invention: How science, politics, and big business re-create race in the twenty-first century. New York, NY: New Press. [Google Scholar]
- Schnittker J, & Bacak V. (2014). The increasing predictive validity of self-rated health. PLoS One, 9, e84933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, McEwen BS, Rowe JW, & Singer BH (2001). Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences, 98, 4770–4775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers SL, Neighbors HW, Zhang R, & Jackson JS (2012). The impact of goal-striving stress on physical health of White Americans, African Americans, and Caribbean Blacks. Ethnicity & Disease, 22, 21–28. [PubMed] [Google Scholar]
- Sewell AA (2016). The racism-race reification process: A mesolevel political economic framework for understanding racial health disparities. Sociology of Race and Ethnicity, 2, 402–432. [Google Scholar]
- Sobel ME (1987). Direct and indirect effects in linear structural equation models. Sociological Methods & Research, 16, 155–176. [Google Scholar]
- Sternthal MJ, Slopen N, & Williams DR (2011). Racial disparities in health: How much does stress really matter? Du Bois Review, 8, 95–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett JL, Herzhoff K, Smack AJ, Reardon KW, & Adam EK (2017). Does socioeconomic status mediate racial differences in the cortisol response in middle childhood? Health Psychology, 36, 662–672. [DOI] [PubMed] [Google Scholar]
- Thoits PA (2010). Stress and health: Major findings and policy implications. Journal of Health and Social Behavior, 51(Suppl. 1), S41–S53. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, & Sutton-Tyrrell K. (2003). Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology, 22, 300–309. [DOI] [PubMed] [Google Scholar]
- Turner RJ (2013). Understanding health disparities: The relevance of the stress process model. Society and Mental Health, 3, 170–186. [Google Scholar]
- Turner RJ, & Avison WR (2003). Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior, 44, 488–505. [PubMed] [Google Scholar]
- Turner RJ, Thomas CS, & Brown TH (2016). Childhood adversity and adult health: Evaluating intervening mechanisms. Social Science & Medicine, 156, 114–124. [DOI] [PubMed] [Google Scholar]
- Tyson K, & Lewis AE (2021). The “burden” of oppositional culture among Black youth in America. Annual Review of Sociology, 47, 459–477. [Google Scholar]
- Vitlic A, Lord JM, & Phillips AC (2014). Stress, ageing and their influence on functional, cellular and molecular aspects of the immune system. Age, 36, 1169–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsemann KM, Goosby BJ, & Farr D. (2016). Life course SES and cardiovascular risk: Heterogeneity across race/ethnicity and gender. Social Science & Medicine, 152, 147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C, & Wang EA (2017). Mass incarceration, public health, and widening inequality in the USA. Lancet, 389, 1464–1474. [DOI] [PubMed] [Google Scholar]
- Williams DR (2018). Stress and the mental health of populations of color: Advancing our understanding of race-related stressors. Journal of Health and Social Behavior, 59, 466–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Lawrence JA, & Davis BA (2019). Racism and health: Evidence and needed research. Annual Review of Public Health, 40, 105–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2013). Racism and health I: Pathways and scientific evidence. American Behavioral Scientist, 57, 1152–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: Socioeconomic status, stress and discrimination. Journal of Health Psychology, 2, 335–351. [DOI] [PubMed] [Google Scholar]
- Williams DT, & Baker RS (2021). Family structure, risks, and racial stratification in poverty. Social Problems, 68, 964–985. [Google Scholar]
- Wright S. (2015). The method of path coefficients. Annals of Mathematical Statistics, 15, 161–215. [Google Scholar]
- Zuberi T, & Bonilla-Silva E. (Eds.). (2008). White logic, White methods: Racism and methodology. Lanham, MD: Rowman & Littlefield Publishers. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


