ABSTRACT
Background:
Infertility is a crucial global public health issue that affects millions of people of reproductive age. Fertility-related stress can negatively impact infertile couples’ quality of life (QoL).
Aims:
This study aimed to assess and compare the psychometric properties of fertility QoL between primary infertile couples’ male and female partners.
Settings and Design:
This cross-sectional study included 114 primary infertile couples visiting the Andrology Laboratory referred from the Gynaecology and Obstetrics Department, AIIMS, Patna.
Materials and Methods:
Data were collected using the Fertility QoL (FertiQoL) tool, an internationally validated questionnaire to measure the reproductive QoL, demographic information and medical history. The FertiQoL questionnaire responses were recorded and analysed.
Statistical Analyses Used:
Statistical analyses used were performed using the SPSS 20.0 version. Descriptive statistics, Kolmogorov–Smirnov test, Cronbach’s alpha and Student’s independent t-tests were used. Statistical significance was set at P < 0.05.
Results:
In our study, the overall estimated Cronbach’s α was 0.83, and males had a significantly better fertility-related QoL in all domains of the FertiQoL, such as emotional (P < 0.000), mind–body (P < 0.000), social (P < 0.004) and tolerability (P < 0.000), except relational and environmental domains, which were lower in them. However, between the groups, the relational domain was significant (0.000) and the environmental domain was non-significant (0.592). Overall, males had a significantly better total core score, total treatment score and overall total FertiQoL score, while females had lower scores.
Conclusion:
Amongst infertile couples, the reproductive QoL was poorer in females than in males. Our study suggests psychological counselling and mental support for females during infertility management.
KEYWORDS: Couples, fertility quality of life, primary infertility, psychometric, quality of life
INTRODUCTION
Infertility is a growingly significant global public health issue that affects roughly 10% to 15% of couples of reproductive age.[1] Infertility affects 186 million people worldwide, including 48 million couples.[2,3] Infertility is classified by the World Health Organization (WHO) as a condition of the reproductive system when a clinical pregnancy cannot be achieved after 1 year of regular, unprotected sexual activity.[4] Infertility is of two types infertility: primary and secondary.
Primary infertility is described as the inability to conceive, whereas secondary infertility is described as the inability to conceive after a previous successful attempt. Globally, most infertile couples experience primary infertility.[5]
According to the WHO, infertility is a significant reproductive health issue that, unlike other illnesses, has catastrophic repercussions on people, families and societies despite not endangering life.[6,7] Unfortunately, little attention is paid to this illness.[8] As a result, both male and female infertile patients may endure psychological anguish and poor reproductive quality of life (QoL).
Furthermore, in today’s assisted reproductive technology practice, psychometric assessment is crucial for evaluating the patient’s QoL and planning subsequent management. Previous research has shown that patients’ attitudes toward infertility and its treatment are often negative. These studies also reported that these changes could affect QoL and overall well-being.[9]
The Fertility QoL (FertiQoL) questionnaire is a gold standard, a multi-dimensional and condition-specific tool to measure QoL in infertile patients, even though there are numerous other questionnaires available to measure QoL.[10] The FertiQoL questionnaire is internationally validated and accepted globally as a standard tool for the assessment of reproductive QoL.[11,12] Patients who scored poorly on the FertiQoL questionnaire might have affected their decision to discontinue treatment, leading to poor pregnancy chances. This could, in turn, affect their QoL.[13]
This study aimed to assess and compare the psychometric properties of FertiQoL between male and female partners of primary infertile couples using the validated FertiQoL questionnaire.
SUBJECTS AND METHODS
The study was conducted at the Andrology Laboratory, Department of Physiology, AIIMS Patna, from April 2019 to March 2020. Subject recruitment was performed after obtaining Ethical Clearance from the Institutional Ethical Committee of the AIIMS, Patna, vide letter no.AIIMS/Pat/IEC/2020/484. Written informed consent was taken from each participant before including them in the study as per ‘National Ethical Guidelines for Biomedical and Health Research Involving Human Participants 2018’ of the Indian Medical Research Council and in accordance with Helsinki Declaration (2013). The minimum required sample size (n) for this observational cross-sectional study was estimated using the equation n = (Z/2)2 S2/d2, considering a power of 90% and an error rate of 5% and considering the standard deviation (SD) resulting from the pilot study undertaken on five adult male participants who were not part of the final study population, the minimum required sample size was 88.
Allowing for 10% of the non-respondents, the corrected minimum sample size required for each group was 97. A total of 114 males and females were recruited for this study, resulting in 228 subjects. After obtaining informed consent, all the participants were asked to respond to the questionnaires in their preferred language (Hindi/English). Male authors for male participants and female co-authors for female participants who underwent special Andrology Laboratory training from NIHFW, New Delhi, recorded the responses to the FertiQoL. The questionnaires were recorded in private to prevent each partner’s influence and to allow them to speak frankly. The FertiQoL questionnaire consists of 36 items to measure QoL in individuals with fertility issues. It includes two modules: core FertiQoL and treatment FertiQoL (optional).
Core FertiQoL module: This module has four domains: emotional, mind–body, relational and social, with each domain having six subscales. Accordingly, there were 24 components in the core FertiQoL module. The effects of infertility on emotions, such as sadness, resentment, jealousy, melancholy and loss, were assessed in the emotional domain. The mind–body domain measures the extent of negative physical symptoms, such as exhaustion and pain, as well as cognitive or behavioural disturbances, such as lack of concentration, disrupted daily activities and delayed life plans, experienced by the individual because of infertility. The relational and social domains are used to quantify the impact of infertility on partnership and social aspects (e.g., social inclusion, expectation and support).
The treatment FertiQoL module consists of the environment and tolerability domains, which collectively consist of ten items. The environmental domain has six subscales that assess accessibility, quality of treatment and interaction with the medical staff. The tolerability domain has four subscales that assess the experience of mental and physical symptoms and disruption of daily life due to treatment. In addition, two single items assessed the overall personal evaluation of physical health and satisfaction with QoL. Items from these domains were randomly presented in the questionnaire and rated on a scale of 0 to 4. Subscale and total FertiQoL scores were computed and transformed to achieve a range of 0 to 100, with higher scores indicating better QoL.
Statistical analysis
Data were analysed using software SPSS statistics for Windows Version 20.0 (IBM Corp., Armonk, NY, USA). Descriptive analysis was performed, and the results of the continuous parameters are expressed as mean ± SD The normality of the data was assessed using the Kolmogorov–Smirnov test. Cronbach’s alpha was used to measure the internal consistency of the FertiQoL, with values above 0.80 indicating excellent, 0.70–0.80 as satisfactory and 0.60–0.70 as acceptable. An independent t-test was used to assess significant differences between the various parameters. Statistical significance was set at P < 0.05.
RESULTS
In the present study, the emotional, mind–body, relational, social, environmental and tolerability components of the FertiQoL questionnaire were assessed and compared between the male and female partners of primary infertile couples. The outcome of the reliability statistics for all the components in both groups is shown in Table 1, and the overall estimated Cronbach’s α was 0.83. Males had a significantly better fertility-related QoL in all domains of FertiQoL, such as emotional (P < 0.000), mind–body (P < 0.000), social (P < 0.004) and tolerability (P < 0.000), except the relational and environmental domains, which were comparatively lower. The relational domain also showed a significant difference (P = 0.000), whereas the environmental domain showed a statistically insignificant (0.592) difference between the groups, as depicted in Table 2 and Figure 1.
Table 1.
Fertility quality of life scores
| Scale | Mean±SD | Cronbach’s alpha | ||
|---|---|---|---|---|
|
| ||||
| Male (114) | Female (114) | Male | Female | |
| Emotional | 54.169±16.876 | 40.863±20.690 | 0.813 | 0.807 |
| Mind–body | 51.718±19.962 | 32.202±21.731 | 0.815 | 0.806 |
| Relational | 55.117±14.678 | 63.452±14.865 | 0.837 | 0.824 |
| Social | 50.993±20.228 | 42.214±25.352 | 0.822 | 0.808 |
| Environmental | 57.784±11.857 | 58.549±9.552 | 0.838 | 0.839 |
| Tolerability | 61.264±13.435 | 52.712±19.236 | 0.824 | 0.821 |
SD=Standard deviation
Table 2.
Comparison of fertility-related quality of life between male and female genders with primary infertility
| Scale | Mean±SD | Independent t-test | ||
|---|---|---|---|---|
|
|
|
|||
| Male (114) | Female (114) | t | P | |
| Emotional | 54.169±16.876 | 40.863±20.690 | 5.321* | 0.000 |
| Mind–body | 51.718±19.962 | 32.202±21.731 | 7.061* | 0.000 |
| Relational | 55.117±14.678 | 63.452±14.865 | −4.260* | 0.000 |
| Social | 50.993±20.228 | 42.214±25.352 | 2.890* | 0.004 |
| Environmental | 57.784±11.857 | 58.549±9.552 | −0.536 | 0.592 |
| Tolerability | 61.264±13.435 | 52.712±19.236 | 3.892* | 0.000 |
| Core FertiQoL - total | 50.877±14.455 | 42.761±17.436 | 3.819* | 0.000 |
| Treatment FertiQoL - total | 23.666±3.659 | 22.495±4.278 | 2.217* | 0.028 |
| Total FertiQoL | 74.543±16.906 | 65.256±20.250 | 3.752* | 0.000 |
*t-value is significant (P≤0.05). FertiQoL=Fertility quality of life, SD=Standard deviation
Figure 1.
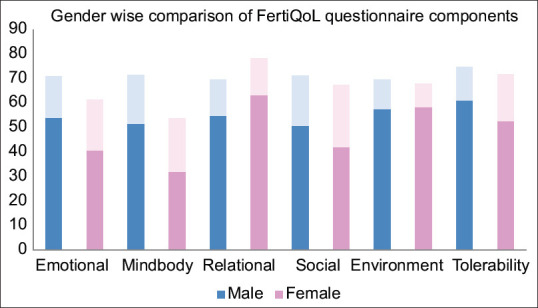
Comparison of fertility quality of life questionnaire scales between males and females of primary infertility couples. FertiQol = Fertility quality of life
DISCUSSION
Infertility is a rising public health issue, with serious social consequences. The incidence of complications associated with infertility is increasing. In terms of emotional, mind–body, social, relational and tolerability, our study revealed that the males had substantially better fertility-related QoL. This was evident with the male partners demonstrating a significantly better total score, that is, total treatment and total FertiQoL, as depicted in Figure 2. This finding was consistent with that of Royani Z et al.,[14] who reported that male partners had a better QoL than infertile female partners.. Previous studies have reported that fertility-related QoL is worse in women than in men.[15,16] Our study also found similar trends: females had a poor fertility-related QoL compared to their male counterparts. Emotional QoL domains were lower in females, indicating their impact and susceptibility to emotional turmoil. Smeenk et al.[17] considered emotional distress to be an important factor contributing to infertility and considered it one of the important reasons that make couples drop out prematurely from the management of infertility. Although in terms of mind–body, relational, social and tolerable QoL, females perceived poorer QoL, they were slightly better in terms of the environmental subscale.
Figure 2.
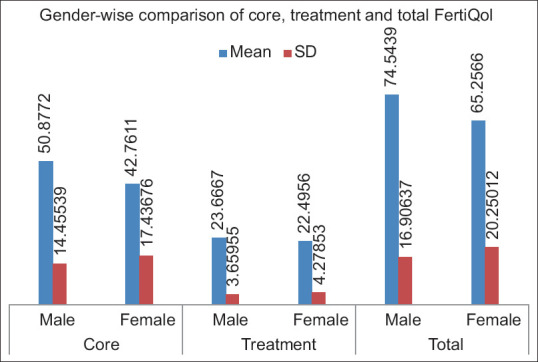
Comparison of total core, total treatment and total fertility quality of life between males and females of primary infertility couples. FertiQol = Fertility quality of life
In Asian countries, infertility is conventionally viewed as a female issue, and women are commonly prejudiced and stigmatised in the family and society as being ‘infertile’, although infertility may be due solely to male partners or combined factors. A study done by Kahyaoglu Sut and Balkanli Kaplan[18] concluded that infertility significantly reduces QoL in women by increasing their anxiety and depression levels, which is consistent with our findings. Amongst couples, the inability to conceive may impose considerable psychological distress on the female partner, leading to feelings of shame and guilt.[19] Women are more susceptible to anxiety and depression than men, and grappling with infertility significantly reduces QoL in women. Some women expressed intense emotions while taking clinical history about their infertility and cried during the FertiQoL questionnaire recording.[20] Both men and women expressed feelings of deep sadness, guilt, loneliness and fear of an insecure future. ‘Why do not you have children yet?’ Confronting questions increases mental stress and feelings of guilt in females. Most females admitted that they avoided social and family gatherings, although both explained their emotions that ‘the house feels empty without the sound of a child’ and they want to become a parent at any cost.
In our study, the environmental subscale score was comparatively better in females, although the difference was not statistically significant. To facilitate this comparison, our study included partners of couples with primary infertility, instead of individual subjects. This ensured that both partners were involved in the search for a solution to their fertility problem when they visited the hospital together; hence, an appropriate comparative assessment can be drawn in the domain. Although both men and women can experience infertility, most often, women in a relationship are perceived to suffer from infertility, regardless of whether they are fertile or their male partners are infertile. Our research supports the findings of previous studies of this relationship.[21,22,23]
Previous research has shown that infertile women believed that their marriages were in trouble and feared being abandoned by their partners, which is in line with our study findings in infertile women.[24] However, very few women with male-related infertility reported feeling more confident about their marriages. Not all female participants in our study were responsible for infertility; nevertheless, they saw it as a tragedy. In contrast, some infertile men responsible for their childless marriages refuse to accept the same. All these factors often lead to a silent struggle in females who struggle to conceive, leading to depression, anxiety, isolation and loss of control.
The psychological vulnerability of most infertile women worsens because they rarely share their experiences with family members or with trusted friends. Feelings of guilt, humiliation and low self-esteem may often result from the inability to reproduce naturally. These adverse emotions can result in various levels of depression, anxiety, distress and poor QoL.[25] Every person is entitled to an optimum standard of physical and mental health that is attainable. However, in the present study, gender inequality was observed. Recognising, acknowledging and supporting infertile women in coping with their diagnoses and treatments are crucial. In addition, infertility providers and counsellors should offer assistance through psychological interventions and emotional support to these patients at the right time, which can improve psychological outcomes and marital relationships and increase patient retention and pregnancy rates.[26,27]
Limitations of the study
The major limitation of our study is that it was conducted as a single-centre study of AIIMS, Patna. Further studies should be conducted in collaboration with many other health institutes. This research study did not evaluate the effect of socioeconomic and educational background on fertility-related QoL.
CONCLUSION
Within the limits of our study, we can conclude that fertility-related QoL in females is poorer than that in males amongst couples with primary infertility. Until recently, little attention has been given to this issue, and very few studies have been conducted on fertility-related QoL across genders in primary infertile couples. Since infertility-related distress is an emergent issue worldwide, health care professionals must consider assessing fertility-related QoL at regular intervals using a holistic approach while examining and treating couples with infertility. Furthermore, in infertility management programmes, there is a need for counselling and psychological interventions along with support from family, friends and society. This could improve overall mental health and QoL, which may increase positive attitudes and hopes amongst infertility-affected couples and ultimately improve their chances of achieving pregnancy.
Authors’ contributions
We confirm that all authors had access to the data, participated in the manuscript’s writing and have seen and approved the submitted version. S. P. D contributed to the study design, writing-original draft preparation, data collection, interpretation of data, manuscript drafting and critical discussion. A. K contributed in data collection, manuscript drafting and critical discussion. A. H. I contributed to statistical analysis. K.V.B.R: Involved in writing reviews and editing. V. S. was involved in manuscript drafting and critical discussion. All authors read and agreed to the published version of the manuscript.
Financial support and sponsorship
AIIMS, Patna.
Conflicts of interest
There are no conflicts of interest.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplemental information. All relevant data are available on reasonable request by e-mailing the corresponding author.
Acknowledgements
We are very thankful to all our study participants who contributed to the study, Institutional Research Cell, Institutional Research Committee, and Director, AIIMS, Patna.
REFERENCES
- 1.Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–12. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- 2.Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: A systematic analysis of 277 health surveys. PLoS Med. 2012;9:e1001356. doi: 10.1371/journal.pmed.1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rutstein, Shea O, Shah IH. DHS Comparative Reports. Calverton, Maryland, USA: ORC Macro and the World Health Organization; 2024. Infecundity, infertility, and childlessness in developing countries. 9. [Google Scholar]
- 4.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, Fertil Steril. 2009;2009;92:1520–4. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 5.Inhorn MC. Global infertility and the globalization of new reproductive technologies: Illustrations from Egypt. Soc Sci Med. 2003;56:1837–51. doi: 10.1016/s0277-9536(02)00208-3. [DOI] [PubMed] [Google Scholar]
- 6.Ombelet W. Global access to infertility care in developing countries: A case of human rights, equity and social justice. Facts Views Vis Obgyn. 2011;3:257–66. [PMC free article] [PubMed] [Google Scholar]
- 7.Cong J, Li P, Zheng L, Tan J. Prevalence and risk factors of infertility at a rural site of Northern China. PLoS One. 2016;11:e0155563. doi: 10.1371/journal.pone.0155563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogawa M, Takamatsu K, Horiguchi F. Evaluation of factors associated with the anxiety and depression of female infertility patients. Biopsychosoc Med. 2011;5:15. doi: 10.1186/1751-0759-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verhaak CM, Smeenk JM, Evers AW, Kremer JA, Kraaimaat FW, Braat DD. Women's emotional adjustment to IVF: A systematic review of 25 years of research. Hum Reprod Update. 2007;13:27–36. doi: 10.1093/humupd/dml040. [DOI] [PubMed] [Google Scholar]
- 10.Boivin J, Takefman J, Braverman A. The fertility quality of life (FertiQoL) tool: Development and general psychometric properties. Fertil Steril. 2011;96:409–15.e3. doi: 10.1016/j.fertnstert.2011.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aarts JW, van Empel IW, Boivin J, Nelen WL, Kremer JA, Verhaak CM. Relationship between quality of life and distress in infertility: A validation study of the Dutch FertiQoL. Hum Reprod. 2011;26:1112–8. doi: 10.1093/humrep/der051. [DOI] [PubMed] [Google Scholar]
- 12.Priangga M, Pratama G, Maidarti M, Harzif A, Wiweko B. Validity of the fertility quality of life (FertiQol) questionnaire in Indonesian infertile women. KnE Med. 2017;1:202. [Google Scholar]
- 13.Gameiro S, Boivin J, Peronace L, Verhaak CM. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum Reprod Update. 2012;18:652–69. doi: 10.1093/humupd/dms031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Royani Z, Heidari M, Vatanparast M, Yaghmaei F, Sarcheshme AK, Majomerd JK. Predictors of quality of life in infertile couples. J Menopausal Med. 2019;25:35–40. doi: 10.6118/jmm.2019.25.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fekkes M, Buitendijk SE, Verrips GH, Braat DD, Brewaeys AM, Dolfing JG, et al. Health-related quality of life in relation to gender and age in couples planning IVF treatment. Hum Reprod. 2003;18:1536–43. doi: 10.1093/humrep/deg276. [DOI] [PubMed] [Google Scholar]
- 16.El-Messidi A, Al-Fozan H, Lin Tan S, Farag R, Tulandi T. Effects of repeated treatment failure on the quality of life of couples with infertility. J Obstet Gynaecol Can. 2004;26:333–6. doi: 10.1016/s1701-2163(16)30361-9. [DOI] [PubMed] [Google Scholar]
- 17.Smeenk JM, Verhaak CM, Stolwijk AM, Kremer JA, Braat DD. Reasons for dropout in an in vitro fertilization/intracytoplasmic sperm injection program. Fertil Steril. 2004;81:262–8. doi: 10.1016/j.fertnstert.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 18.Kahyaoglu Sut H, Balkanli Kaplan P. Quality of life in women with infertility via the FertiQoL and the hospital anxiety and depression scales. Nurs Health Sci. 2015;17:84–9. doi: 10.1111/nhs.12167. [DOI] [PubMed] [Google Scholar]
- 19.Inhorn MC, Patrizio P. Infertility around the globe: New thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update. 2015;21:411–26. doi: 10.1093/humupd/dmv016. [DOI] [PubMed] [Google Scholar]
- 20.Taebi M, Kariman N, Montazeri A, Alavi Majd H. Infertility stigma: A qualitative study on feelings and experiences of infertile women. Int J Fertil Steril. 2021;15:189–96. doi: 10.22074/IJFS.2021.139093.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goker A, Yanikkerem E, Birge O, Kuscu NK. Quality of life in Turkish infertile couples and related factors. Hum Fertil (Camb) 2018;21:195–203. doi: 10.1080/14647273.2017.1322223. [DOI] [PubMed] [Google Scholar]
- 22.Rashidi B, Montazeri A, Ramezanzadeh F, Shariat M, Abedinia N, Ashrafi M. Health-related quality of life in infertile couples receiving IVF or ICSI treatment. BMC Health Serv Res. 2008;8:186. doi: 10.1186/1472-6963-8-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martins MV, Peterson BD, Almeida VM, Costa ME. Direct and indirect effects of perceived social support on women's infertility-related stress. Hum Reprod. 2011;26:2113–21. doi: 10.1093/humrep/der157. [DOI] [PubMed] [Google Scholar]
- 24.Dyer SJ, Abrahams N, Hoffman M, van der Spuy ZM. ‘Men leave me as I cannot have children': Women's experiences with involuntary childlessness. Hum Reprod. 2002;17:1663–8. doi: 10.1093/humrep/17.6.1663. [DOI] [PubMed] [Google Scholar]
- 25.Simionescu G, Doroftei B, Maftei R, Obreja BE, Anton E, Grab D, et al. The complex relationship between infertility and psychological distress (Review) Exp Ther Med. 2021;21:306. doi: 10.3892/etm.2021.9737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chow KM, Cheung MC, Cheung IK. Psychosocial interventions for infertile couples: A critical review. J Clin Nurs. 2016;25:2101–13. doi: 10.1111/jocn.13361. [DOI] [PubMed] [Google Scholar]
- 27.Rooney KL, Domar AD. The impact of stress on fertility treatment. Curr Opin Obstet Gynecol. 2016;28:198–201. doi: 10.1097/GCO.0000000000000261. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplemental information. All relevant data are available on reasonable request by e-mailing the corresponding author.


