Abstract
Objectives:
Pain typically prompts individuals to seek relief. This study aimed to develop and psychometrically validate the Pain Relief Motivation Scales (PRMS), applying revised Reinforcement Sensitivity Theory to measure the neuropsychological systems underlying motivation for pain relief. We hypothesized a 6-factor structure based on previous work, including one behavioral inhibition system (BIS) factor, one Fight-Flight-Freeze System (FFFS) factor, and four behavioral activation system (BAS) factors.
Methods:
Items were generated by adapting the Reinforcement Sensitivity Theory of Personality Questionnaire for relevance to pain relief. Adults with chronic pain were recruited internationally to participate in online survey batteries at baseline and one week later during 2021. We randomly split the sample to conduct exploratory factor analysis (n=253) and confirmatory factor analysis (n=253). Psychometric properties were estimated using the full sample (N=506).
Results:
Parallel analysis revealed that a 5-factor structure best fit the data (21 items): [1] hopelessness about pain relief (BIS), [2] hesitancy for engaging in pain treatments (BIS), [3] persistence in engaging in pain treatments (BAS), [4] relief reactivity (BAS), and [5] risky relief-seeking (BAS). Acceptable internal consistency (Cronbach’s alpha=.68-.80) and test-retest reliability (ICCs=.71-.88) were observed. Construct validity varied from weak to moderate (r’s=.02-.45).
Discussion:
As the first attempt to create an instrument measuring neuropsychological systems underlying motivation for pain relief, the findings show that additional work is needed to refine theory and psychometric rigor in this area. Cautiously, the results suggest that a BIS-BAS model, with minimal FFFS contributions, might be useful for understanding motivation for relief.
Keywords: reinforcement sensitivity theory, reward system, pain relief, motivation, questionnaire
1. Introduction
Pain and relief are aversive and appetitive experiences, respectively, that motivate behavior.1 Motivation to prevent the environmental circumstances that worsen pain and to seek out those producing relief can lead to lifestyle adaptations.2 These cognitive, behavioral, and emotional adaptations (e.g., avoidance of activities for fear of exacerbating pain) do not always lead to ideal outcomes and might exacerbate pain-related disability and/or analgesic misuse.3 Characterizing individual differences in pain relief-related motivation can help guide pain management and research efforts to mitigate these risks.
Reinforcement Sensitivity Theory (RST) is a framework proposing neuropsychological systems underlying motivated behavior. The original RST framework focused on two systems, characterized by negative (e.g., aversive/fear/punishing) and positive (e.g., appetitive/rewarding) valence.4 RST has been revised to describe three systems,5 including the Behavioral Activation System (BAS), the Fight-Flight-Freeze System (FFFS), and the Behavioral Inhibition System (BIS). The BAS is activated by appetitive or reinforcing stimuli, such as pain relief and positive affect. The FFFS is activated by aversive or punishing stimuli, such as the experience of pain. The BIS is activated by conflicting stimuli, meaning situations in which there is approach-avoidance conflict and co-activation of the BAS and FFFS (e.g., an individual wants to engage in an activity that they anticipate will increase their pain). Rumination, worry, and passive avoidance are all BIS-mediated. Neurophysiologically, the mesocorticolimbic system – the system that regulate hedonic motivation and impulses – is associated with these neuropsychological systems.6
Recently, Jensen and colleagues proposed a two-factor BIS-BAS Model of Chronic Pain, which adapts original RST to valued, goal-directed behavior in people with chronic pain.7 Their model does not include the FFFS because (a) this system is not activated on a daily basis, (b) other well-validated approach-avoidance models do not include an FFFS, and (c) BIS and FFFS show a strong association; thus, they potentially comprise one “punishment sensitivity” personality factor.8 The authors further noted that limitations in FFFS measurement hinders the field’s ability to understand RST models in the context of pain.
Several available self-report measures assess motivation using the revised RST framework (a review is here9). For example, the Pain Responses Scale examines cognitive, behavioral, and affective responses to pain using the original RST framework.10 However, none of these measures assess BIS, BAS, and FFFS in the context of motivation for pain relief. Developing a questionnaire addressing motivation for pain relief has important applications to help clinicians individually tailor interventions and identify individuals at-risk for harmful relief-seeking behaviors, as well as to advance research on the mechanisms of relief-related motivation.
This study aimed to develop and assess the psychometrics of a new trait-based measure using the revised RST framework to measure aspects of pain-relief related motivation: The Pain Relief Motivation Scales (PRMS). Using the RST of Personality Questionnaire’s structure,11 we adapted questions to assess cognitive, affective, and perceived behavioral (rather than observed) responses underlying pain relief-related motivation. We chose the RST of Personality Questionnaire as a model, given its use of revised RST, multiple BAS subcomponents, and strong psychometrics.12 Consistent with the RST of Personality Questionnaire, we hypothesized that there would be a six-factor structure spanning (1) Guarded Responses to Poor Relief Outcomes (RST of Personality Questionnaire’s BIS), (2) Fear of Poor Relief Outcomes (RST of Personality Questionnaire’s FFFS), (3) Desire for Relief (RST of Personality Questionnaire’s BAS-Reward Interest), (4) Goal-Driven Persistence for Relief (RST of Personality Questionnaire’s BAS-Goal-Drive Persistence), (5) Relief Reactivity (RST of Personality Questionnaire’s BAS-Reward Reactivity), and (6) Risky Relief-Seeking (RST of Personality Questionnaire’s BAS-Impulsivity). We expected acceptable internal consistency, test-retest reliability, and construct validity of PRMS.
2. Methods
Figure 1 highlights methods used to develop the final PRMS, including measure development procedures, data collection procedures, and data analyses to determine the final factor structure and items selected. Detailed procedures are described below; scale development was the primary aim of this study.
Figure 1.
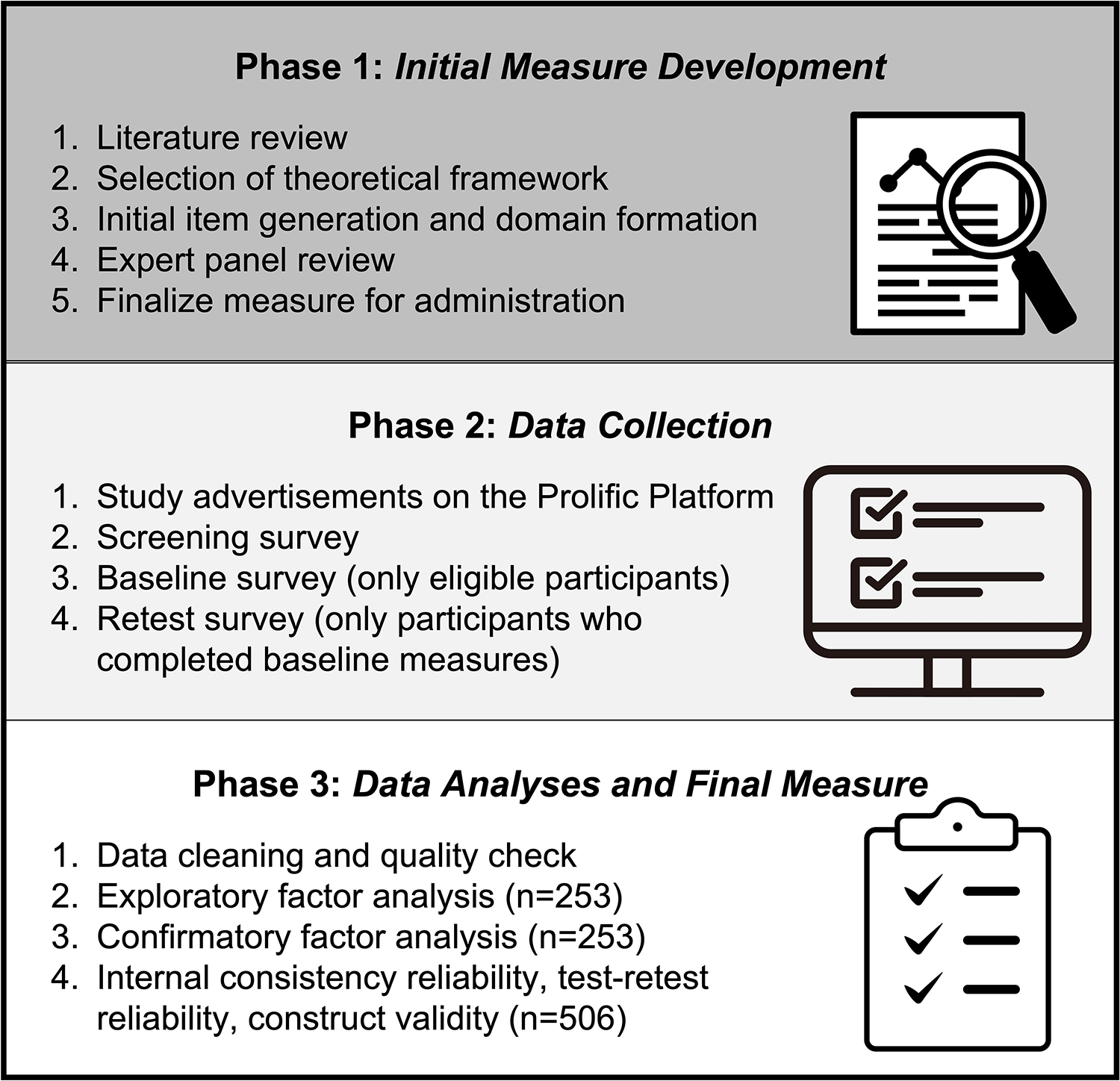
Overview of Steps Involved in Developing the Pain Relief Motivation Scales
2.1. Original Scale Development Procedures
Currently recommended practices were used to develop and report the PRMS.13 A literature review was conducted to determine the theoretical framework (i.e., revised RST), identify existing revised RST-based questionnaires, and generate an initial pool of items. At the time of the literature review (i.e., 2020), no measures applied revised RST in a pain-related context. Since the initial review was conducted, Day and colleagues published the Pain Responses Scale.10 The PRMS is complimentary to, but distinct from, the Pain Responses Scale, given our measure’s focus on motivation for the specific experience of “pain relief” and the Pain Responses Scale’s focus on experiences of pain and associated factors (e.g., escape, approach, despondence, and relaxation).
The initial item pool was generated by adapting the RST of Personality Questionnaire, which addresses limitations of previous measures based on original RST (e.g., Carver and White’s BIS/BAS Scales14) and/or the inclusion of only one BAS factor.11 Psychologists with expertise in affective-motivational systems and pain, several of whom live with chronic pain, developed the items. However, a key limitation of the present measure is that people outside of academia with lived experience of pain across diverse sociocultural and educational backgrounds were not included in the development of this measure, which would have improved its generalizability. A further limitation is that pre-testing of our items was not conducted before running the online survey. The version of the PRMS used in during data collection included 50 questions across six factors (see Section 2.2). Similar to the response scale on the RST of Personality Questionnaire, instructions on the PRMS asked participants to rate the degree to which each statement was true or false using a Likert scale: (1 = very true for me when I’m in pain, 2 = somewhat true for me when I’m in pain, 3 = somewhat false for me when I’m in pain, 4 = very false for me when I’m in pain). Table S1 details the full set of administered items.
2.2. Proposed Factor Structure
Consistent with other measures that use an RST framework, the interpretation of the PRMS is intended for use within subscales and not a total score.
Guarded Responses to Poor Relief Outcomes:
This factor was modified from the RST of Personality Questionnaire’s BIS factor, which was originally operationalized by Corr and Cooper11 as the system responsible for the resolution of conflict within and between the FFFS and BAS. Cognitive functions of the BIS – such as worry, rumination, guarding, and detachment – help resolve FFFS-BAS conflict by encouraging a behavioral resolution of BAS-mediated approach or FFFS-mediated avoidance/escape. In the original PRMS version, Guarded Responses to Poor Relief Outcomes factor items related to worry, rumination, guarding, and detachment in the face of undesirable pain relief outcomes.
Fear of Poor Relief Outcomes:
This factor was modified from the RST of Personality Questionnaire’s FFFS factor, which was originally operationalized as a “punishment sensitivity” system that serves a general purpose to mediate responses to all aversive/punishing stimuli. Corr and Cooper11 described that their FFFS factor was designed to measure stimuli that can be avoided through flight, active avoidance, or freezing; however, they explained that fight-related items were not included in the subscale based on theory and empirical evidence. In the original PRMS version, Fear of Poor Relief Outcomes factor items related to perceived fear, flight, active avoidance, and freezing in the face of undesirable pain relief outcomes.
Desire for Relief:
This factor was modified from the RST of Personality Questionnaire’s Reward Interest factor, which was originally operationalized as a facet related to anticipatory expectation and openness to rewards, such as looking for new opportunities and exploring stimuli that have the potential to be rewarding. In the original PRMS version, Desire for Relief factor items related to openness to look for and try new pain self-management activities and therapeutics.
Goal-Driven Persistence for Relief:
This factor was modified from the RST of Personality Questionnaire’s Goal-Drive Persistence factor, which was originally operationalized as a facet related to maintenance of motivation and persistence when rewards are not immediately available. In the original PRMS version, Goal-Driven Persistence for Relief factor items related to beliefs about self-efficacy and perceived motivation to initiate new, as well as consistently adhere to existing, pain treatments.
Relief Reactivity:
This factor was modified from the RST of Personality Questionnaire’s Reward Reactivity factor, which was originally operationalized as a facet related to the generation and experience of pleasure that provides reinforcement for future BAS behavior. In the original PRMS version, Relief Reactivity factor items related to an individual’s perceived capacity to experience full and lasting pain relief.
Relief-Seeking:
This factor was modified from the RST of Personality Questionnaire’s Impulsivity factor, which was originally operationalized as a facet related to the need for rapid, unplanned action to obtain reward. In the original PRMS version, Relief-Seeking factor items related to craving substances or activities that generate relief, perceptions of unplanned action to obtain pain relief, and willingness to use forms of pain relief without considering potential negative consequences.
2.3. Measures
2.3.1. Sociodemographic and Clinical Pain Characteristics
Participants responded to questions about their sociodemographic and clinical pain characteristics. The full set of questions is provided in the Supplemental Materials (Section 3).
2.3.2. Construct Validity Assessments
The methods, rationale for inclusion, and internal consistency reliabilities for measures used to assess construct validity in the present study are described in the Supplemental Materials, Section 4. Briefly, established questionnaires used in the present study included the RST of Personality Questionnaire,11 Pain Catastrophizing Scale (PCS),15 Chronic Pain Acceptance Questionnaire 8-item (CPAQ-8),16 Snaith-Hamilton Pleasure Scale (SHAPS),17 PROMIS Prescription Pain Medication Misuse v1.0 – Short Form 7a,18 Graded Chronic Pain Scale - Revised (GCPS-R),19 PROMIS Emotional Distress – Anxiety, Depression – Short Forms 4a,20 and the Barratt Impulsiveness Scale – Brief (Impulsiveness).21 We also added attention check items.
2.4. Participants
Participants were enrolled via Prolific Academic (www.prolific.co),22 which is an online survey platform designed for research. Prolific users are asked to complete prescreening questions upon registration. Research survey advertisements are broadcast within a message through the Prolific platform to users whose prescreening responses align with the research survey’s eligibility criteria. In the present study, research survey advertisements were broadcast to Prolific users who endorsed “yes” to lifetime history of pain (i.e., Throughout our lives, we all experience everyday pains like a headache or toothache. Have you had pain other than these everyday kinds of pain? If so, how long?), along with English proficiency, and residence in USA, Canada, or Western Europe were eligible to complete our screener. The latter criterion was chosen because of sociocultural factors impacting questionnaire development and is a limitation of this measure for generalizability cross-culturally. Participants were compensated at a rate of $7 or $7.50 per hour for completing Phase 1 and Phase 2, respectively, in accord with Prolific’s recommendations.
2.5. Survey Procedures
The Johns Hopkins School of Medicine Institutional Review Board approved this study (#00251699). After providing informed consent, prescreened individuals completed our screener. Eligible participants (i.e., individuals who met prescreening criteria and responses on the Graded Chronic Pain Scale – Revised fell in the “mild,” “moderate,” or “high-impact” chronic pain ranges), completed the Baseline survey and, one week later, the Retest survey. De-identified responses were downloaded through Qualtrics.
2.6. Data Analyses
We randomly split the total sample (N=506) to use in exploratory factor analyses ( n=253) and confirmatory factor analysis (n=253). The sample was randomly split using the “sample_n” command within the dplyr R package. This command allows for the random selection of rows in a data set. When investigating reliability and validity, we used the whole sample.
Exploratory factor analysis was conducted using oblique rotation (i.e., goemin) in Mplus Version 823 following best practices.24 Because the revised RST’s factor structure as it applies to motivation for pain relief is not well-established, exploratory factor analysis allowed for one to seven factor models. Parallel analysis, an accurate method for selecting the optimal number of factors,25 was used to make decisions on the number of factors. Model fit indices (i.e., SRMR < 0.08, RMSEA < 0.06, CFI > 0.90),26 factor loadings, presence and magnitude of cross loadings, and conceptual interpretability were reviewed for each exploratory factor analysis model. We followed recommendations by Howard27 and retained items with (1) factor loadings at or above 0.40; (2) cross loadings below 0.30; and (3) difference between primary factor and cross loading is at or above 0.20. Items that do not meet the above-mentioned criteria were sequentially deleted. Following each item’s removal, parallel analysis was re-conducted, and the loadings and fit indices associated with each solution were re-examined. This iterative process was conducted until the optimal model, characterized by good model fit and simple factor structure, was achieved.
After finalizing the exploratory factor analysis, the confirmatory factor analysis model was evaluated using recommended cutoff scores.26 Modification indices were also considered when the model fit was not satisfactory and when consistent with theoretical conceptualizations of PRMS items.28 Note that no additional items were removed during this process. Cronbach’s alpha of .65 was set as the minimum acceptable level for internal consistency reliability.29,30 Intraclass correlation coefficients (ICCs) of .50 was set as the minimum acceptable level for test-retest reliability.31
Construct validity coefficients were computed from baseline data using Pearson’s bi-variate correlations with previously suggested effect size conventions (<.29 = weak, .30-.69 = moderate, >.70 = strong). To assess construct validity, we included the PCS, CPAQ-8, SHAPS, and PROMIS Prescription Pain measures. First, we hypothesized that the PCS would positively associate with the Fear of Poor Relief Outcomes factor, given that both relate to worry, rumination, and magnification about pain and pain relief, respectively. Second, the CPAQ-8 was included to help differentiate whether Guarded Responses to Poor Relief Outcomes was associated with pain acceptance (a hypothesized null association) or hopelessness and other BIS emotions (a hypothesized positive association). Third, we hypothesized that the Relief Reactivity factor on the PRMS would negatively associate with the SHAPS (a higher score indicates greater levels of anhedonia), given that this factor was intended to measure one’s hedonic capacity to experience relief. Fourth, the PROMIS Prescription Pain Medication Misuse measure was included in the present study to test the hypothesis that the Relief Seeking factor on the PRMS was positively associated with scores on this PROMIS measure.
As previously stated, considering the intended interpretation of the PRMS within subscales, we opted to utilize subscale scores instead of total PRMS scores for conducting analyses aimed at examining reliability and validity.
3. Results
3.1. Sample Characteristics
Figure 2 shows recruitment and retention, and Table 1 details participants’ characteristics. Participants’ mean age was 31.8 (11.3) years, and the majority were cisgender women (65.6%), White (87.5%), non-Hispanic (90.5%), and employed full-time (34.4%). Clinically, 53.7% reported chronic pain duration as >5 years, and 54.7% reported experiencing 2–3 co-occurring chronic pain conditions. Participants reported moderate-to-high levels of pain (mean=5.3), depressive (mean=62.9), and anxiety (mean=64.0) symptoms. A total of 187 (37% of the sample) participants reported that they had a pain medication prescription in the past 3 months. Table 2 lists pain treatments at the time of participation.
Figure 2.
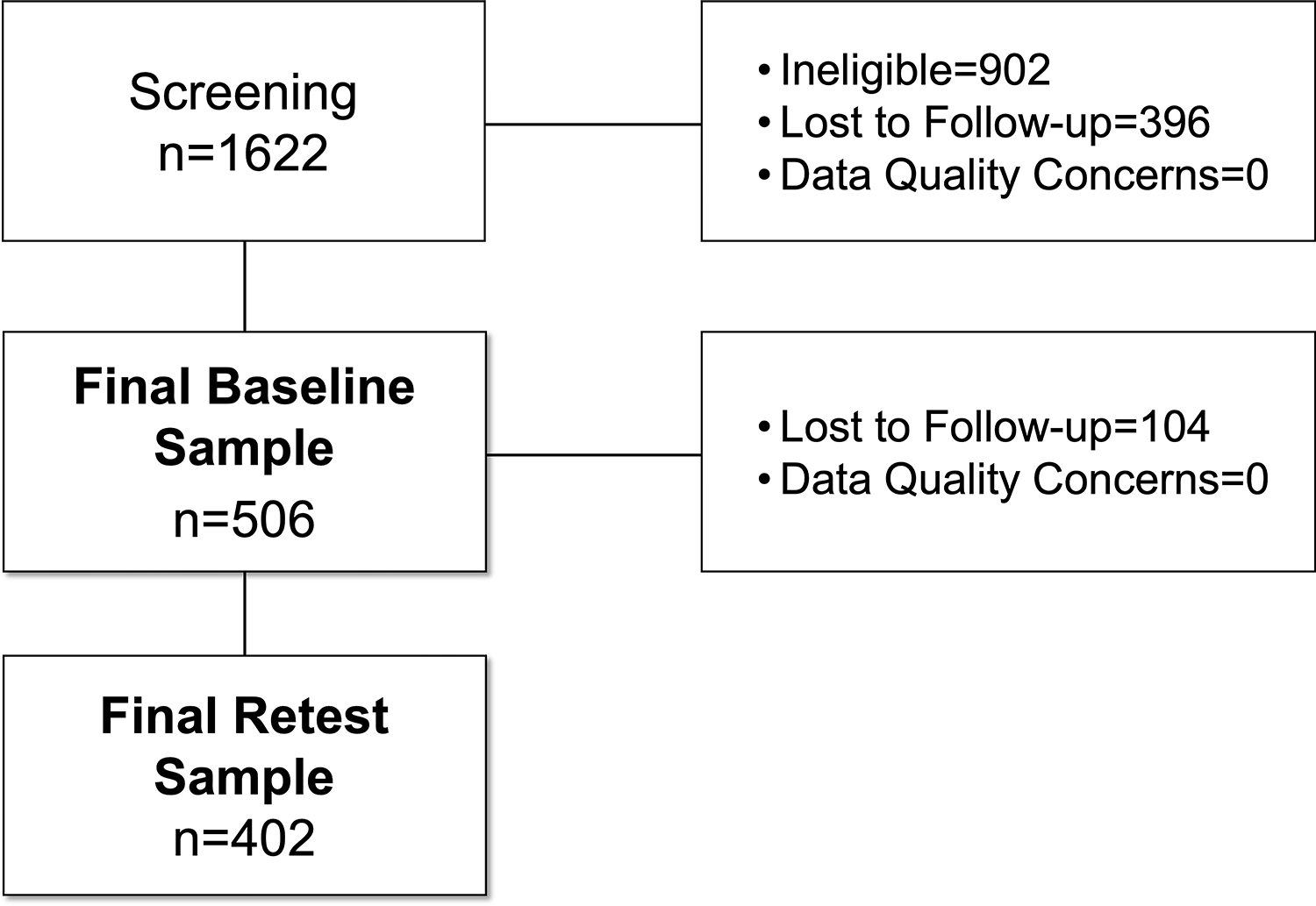
Flowchart of Recruitment and Retention Throughout the Study
3.2. Data Quality
All participants passed the attention check questions that were embedded in the survey. Among the 50 original items across 506 participants (25,150 observations total), only 5 observations had missing data. We used full information maximum likelihood (FIML) in Mplus to handle these missing data during exploratory and confirmatory factor analyses. On average, participants took 1.9 minutes (SD = 1.6) to complete the screening survey, 31.3 minutes (SD = 12.8) to complete the baseline survey, and 7.5 minutes (SD = 6.6) to complete the retest survey.
3.3. Exploratory Factor Analyses
Parallel analysis suggested that a five-factor solution was optimal. With the 50-item pool, the model fit was acceptable except for the CFI (RMSEA = 0.05, CFI = .84, and SRMR = 0.04).
However, we observed low factor loadings and cross loadings for several items. Subsequently, we systematically removed these items and, after each removal, conducted parallel analysis to reassess the model. This process continued until we achieved the optimal model, characterized by good model fit and a simple factor structure.
After this iterative process, 21 items were retained from the original 50. The optimal exploratory factor analysis model was still a five-factor model (RMSEA = .048, CFI = .95, SRMR = .03). Although six factors were originally conceptualized, the final factors were altered to reflect the content domain related to each subgroup of items: (1) BIS Hopelessness About Pain Relief, (2) BIS Hesitancy for Engaging in Pain Treatments, (3) BAS Persistence for Engaging in Pain Treatment, (4) BAS Risky Relief Seeking, and (5) BAS Relief Reactivity. Figure 3 shows the RST of Personality Questionnaire factors that inspired the hypothesized PRMS factors and the empirically-derived final factors. Factor loadings associated with each item are provided in Table S2.
Figure 3.
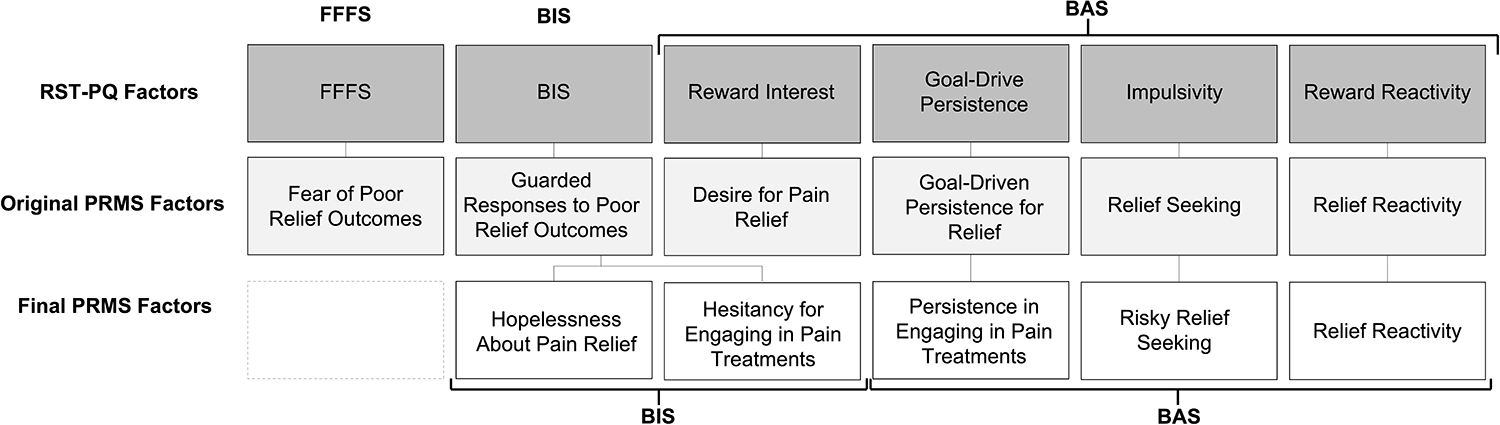
Hypothesized and Empirically-Derived Subscales of the Pain Relief Motivation Scales
Regarding interpretation of the subscale scores, higher scores indicate greater self-report of that factor. Higher subscale scores for BIS-Hopelessness About Pain Relief indicate greater hopelessness about pain relief (subscale range = 4–16). Higher subscale scores for BIS-Hesitancy for Engaging in Pain Treatments indicate greater hesitancy for engaging in pain treatments (subscale range = 3–12). Higher subscale scores for BAS-Persistence in Engaging in Pain Treatments indicate greater persistence in engaging in pain treatments (subscale range = 7–28). Higher subscale scores for BAS-Risky Relief Seeking indicate greater likelihood of engagement in risky behaviors to seek pain relief (subscale range = 4–16). Higher subscale scores for BAS-Relief Reactivity indicate greater reactivity to pain relief (subscale range = 3–12).
3.4. Confirmatory Factor Analyses
Confirmatory factor analysis supported the five-factor exploratory factor analysis model, evidenced by marginal to adequate model fit (RMSEA = .052, CFI = .89, and SRMR = .07). Modification indices were reviewed for estimated impact on model fit and error terms were allowed to covary for the items “I would rather take a medication that I know has side effects than do an activity that takes considerable effort (e.g., meditation, exercise) to relieve my pain” and “I take a long time to decide whether I want to engage in an activity that might relieve my pain.” With the addition of this error covariance, all a priori cutoffs were met in terms of model fit (RMSEA = .049, CFI = .91, and SRMR = .07). Latent factor intercorrelations ranged from −.11 to .43, suggestive of adequate discriminant validity.33 Standardized factor loadings and standard errors are shown in Table 3.
3.5. Internal Consistency Reliability
The PRMS’s internal consistency reliability was acceptable for all subscales. Cronbach’s alphas for baseline, retest administrations were as follows: (1) BIS-Hopelessness About Pain Relief: baseline=.80, retest=.80; (2) BIS-Hesitancy for Engaging in Pain Treatments: baseline=.68, retest=.68; (3) BAS-Persistence in Engaging in Pain Treatments: baseline=.79, retest=.82; (4) BAS-Risky Relief Seeking: baseline=.73, retest=.75; and (5) BAS-Relief Reactivity: baseline=.70, retest=.74.
3.6. Test-Retest Reliability
A total of 402 participants completed the retest (80% retention). The average follow-up timeframe was 7.6 days (SD = .75, range = 7 – 9). Test-retest reliability was adequate: (1) BIS-Hopelessness About Pain Relief = .84; (2) BIS-Hesitancy for Engaging in Pain Treatments = .75; (3) BAS-Persistence in Engaging in Pain Treatments = .85; (4) BAS-Risky Relief Seeking =.71; (5) BAS-Relief Reactivity = .88.
3.7. PRMS Validity
Tables 4 and 5 show Pearson’s r correlations between the two empirically derived BIS-based PRMS factors or three empirically derived BAS-based factors, respectively, with all other PRMS factors, all RST of Personality Questionnaire factors, and all included questionnaires associated with BIS or BAS constructs. An explanation of the findings is detailed in the Supplemental Materials, Section 6. To summarize, the construct validity for BIS-Hopelessness About Pain Relief and BIS-Hesitancy for Engaging in Pain Treatments aligned with our hypotheses by positively associating with factors such as depression, anxiety, anhedonia, and pain and negatively associating with factors such as pain relief capacity and reported motivation for engaging in pain treatments. Further, the construct validity for BAS-Persistence in Engaging in Pain Treatments aligned with hypotheses by negatively associating with factors such as depression, anxiety, and pain and positively associating with pain relief capacity and motivation for pain relief. BAS-Risky Relief Seeking associated with prescription pain medication misuse risk and impulsivity, as hypothesized. However, the construct validity for Relief Reactivity did not align with hypotheses.
4. Discussion
Previous research and theory suggest that pain (an aversive experience) and relief (an appetitive experience) are at opposite ends of a hedonic continuum. Although these phenomena have shared neural and affective mechanisms, much less is comparatively understood about the affective experience of pain relief. For this reason, efforts to develop affective-motivational measures of the pain relief experience provide unique insights into the hedonic continuum compared to measures focused on the experience of pain.
For this reason, this study aimed to develop and validate a measure using revised RST to help researchers and clinicians capture individual differences in trait-based neuropsychological systems underlying motivation for pain relief. Although a six-factor structure was hypothesized – adapting the structure of the RST of Personality Questionnaire for the pain relief context – analyses indicated that a five-factor structure best fit the data. The final factor structure included two BIS factors (Hopelessness About Pain Relief and Hesitancy for Engaging in Pain Treatments) and three BAS factors (Persistence in Engaging in Pain Treatments, Risky Relief Seeking, and Relief Reactivity). Overall, the measure showed adequate internal consistency reliability and test-retest reliability but weak-to-moderate construct validity, suggesting future work is needed to enhance the psychometric properties of the PRMS. Further, this study highlighted several important implications for future mechanistic research in this area.
Regarding subscale performance, BIS-Hopelessness About Pain Relief showed moderate, positive associations with expected constructs, including the RST of Personality Questionnaire’s BIS (but not FFFS) subscale, depression, anxiety, anhedonia, and pain catastrophizing. It most strongly associated with the PCS’s Helplessness subscale. Accordingly, this factor showed a moderate, negative association with self-reported motivation to engage in pain self-management. This factor emerged as a subscale relevant for understanding BIS-related influence in motivation for pain relief.
BIS-Hesitancy for Engaging in Pain Treatments showed moderate, positive correlations with the RST of Personality Questionnaire’s BIS and FFFS subscales, depression, anxiety, anhedonia, and pain catastrophizing. Further, there was a moderate negative association with self-reported motivation to engage in pain self-management. This factor emerged as a subscale related to fear-avoidance BIS components.
BAS-Persistence in Engaging in Pain Treatments showed moderate, positive associations with the RST of Personality Questionnaire’s Goal-Driven Persistence subscale and BAS-relevant constructs of self-reported capacity for pain relief and motivation to engage in pain self-management. It showed moderate, negative associations with impulsiveness, depression, and helplessness. This factor emerged as subscale relevant for understanding BAS-related influence in motivation for pain relief.
BAS-Risky Relief Seeking showed strong construct validity for pain prescription misuse risk and impulsivity, as expected. Although it was not associated with the other BAS-related questionnaires included in the study (e.g., chronic pain acceptance, motivation, and relief capacity), it positively correlated with depression, anhedonia, and pain catastrophizing. Consequently, this factor is a subscale relevant for understanding impulsive and risky pain relief seeking behaviors that associate with BIS-related cognitive-behavioral and affective processes (e.g., anhedonia, depression, pain catastrophizing).
Finally, BAS-Relief Reactivity showed variable construct validity. Although it had a moderate, positive association with the RST of Personality Questionnaire’s Reward Responsiveness subscale – consistent with expectations – it did not significantly associate with responses to capacity for pain relief. Further – contrary to expectations – it had a weak, positive association with all other RST of Personality Questionnaire subscales, negatively associated with pain acceptance and motivation to engage in pain treatments, and showed positive associations with depression, anxiety, anhedonia, and pain catastrophizing. These mixed results challenge the validity of this factor. For this reason, we have published versions of the PRMS with all five factors, as well as without the BAS-Relief Reactivity factor in the supplemental file.
A systematic review of 39 neuroimaging studies examining the neural correlates of RST found associations between prefrontal cortex, ventral striatum, ventral pallidum, and ventral tegmental area structure/function and BAS responses. Further, it identified cingulate and amygdala structure/function as correlates of BIS and FFFS6. The review’s results suggested that dynamic interactions among mesocorticolimbic system regions contribute to BIS, FFFS, and (to a greater extent) BAS processes. Altered mesocorticolimbic system function has been hypothesized as a risk factor for the co-occurrence of chronic pain, depression, and substance use disorder.34 Further, function among mesocorticolimbic regions is associated with the experience of pain relief.35–37 Future work characterizing mesocorticolimbic function using the revised RST framework can help characterize individual difference factors driving motivation for pain relief, such as in the context of hopelessness about pain relief, hesitancy or persistence in engaging in pain treatments, and risky relief-seeking. Given that this is an understudied phenomenon, advances in this area will more completely help explain hedonic mechanisms and sequelae of chronic pain.
Overall, this study suggests that a two-factor BIS-BAS model might better explain motivated behavior underlying pain relief than a three-factor FFFS-BIS-BAS model. This is consistent with the BIS-BAS Model of Chronic Pain,7 which has been more directly applied to study behavioral responses to chronic pain and indirectly to understand pain relief. The BIS-BAS Model of Chronic Pain describes pain and associated cues as aversive stimuli that directly activate the BIS and indirectly suppress the BAS. It further describes that BIS activation in chronic pain results in increased avoidance of activities that exacerbate an individual’s pain, pain-related rumination and worry, and severity of aversive mood states. Reward-activated BAS, on the other hand, is described as potentially having direct links with the appetitive experiences of positive mood states and pain relief through analgesics or self-management. Their framework is partially supported by their previous work showing positive associations among trait-level BIS processes and adverse pain outcomes.38–41 The role of BAS, however, seems to be less important than BIS in explaining pain-related outcomes.42,43
Based on the BIS-BAS Model of Chronic Pain, Day and colleagues developed and psychometrically validated the Pain Responses Scale.10 Their questionnaire measures four overarching responses to pain, including Escape (similar to the PRMS’s BIS-Hesitancy for Engaging in Pain Treatments), Despondence (similar to the PRMS’s BIS-Hopelessness About Pain Relief), Approach (BAS-related, somewhat similar to the PRMS’s BAS-Persistence in Engaging in Pain Treatments), and Relaxation (BAS-related pain acceptance, differs from BAS constructs in the present study). However, their scale measures experiences related to pain, rather than pain relief, which is a novel aspect and strength of the present measure. In examining the subscales’ associations with pain severity and interference, BIS-related subscales were more strongly associated with pain outcomes than BAS-related subscales.
Expanding on this evidence, our findings showed that BIS-related hopelessness about pain relief showed the strongest associations with average pain intensity, depressive symptoms, pain catastrophizing, and capacity for pain relief, so that greater hopelessness associated with worse clinical symptoms. BIS-related hesitancy for engaging in pain treatments, on the other hand, did not associate with pain intensity nor capacity for pain relief and associated with to a weaker degree with pain catastrophizing. This finding suggests that hopelessness might be particularly relevant mechanism of pain and pain relief outcomes. Our findings further expanded on published work by showing that BAS-related persistence and risky relief-seeking might be particularly important in understanding motivation for engaging in pain treatments and pain medication misuse risk, respectively. A future direction for research using the PRMS (particularly, the Persistence in Engaging in Pain Treatments and Risky Relief-Seeking BAS subscales), would be to examine its predictive validity for pain treatment engagement and outcomes to further understand BAS contributions to the BIS-BAS Model of Chronic Pain.
Measure Strengths, Limitations, and Future Applications
A major strength of this study was the focus on pain relief as a novel contribution to an area with limited research, given that most existing scales and research efforts have focused on affective-motivational components of pain rather than pain relief. Additional research in this area will allow for a more comprehensive understanding of the pain-relief hedonic continuum.
Among the study’s limitations, concerns about diversity, equity, accessibility, and inclusion are notable in two ways. First, while the PRMS items were developed by a team of researchers, including some of whom live with chronic pain, we recognize that we missed an invaluable opportunity to gather input from a diverse group of people with lived experiences chronic pain who are not affiliated with academic environments. Their perspectives could have greatly enhanced the refinement of scale items, ensuring their maximum impact and readability for individuals from various educational backgrounds. Second, participants were mostly non-Hispanic White, cisgender women who were employed full-time. This hinders the measure’s generalizability broadly and demonstrates the limitations of using online platforms to collect survey data rather than recruiting through community-based sources. Future work in this area should use community engagement approaches in both scale development and participant recruitment. This future, community-engaged work should also include measures that can help contextualize responses on this measure – such as to the BAS-Risky Relief Seeking or BIS-Hesitancy for Engaging in Pain Treatments – among marginalized groups, such as experiences of discrimination in healthcare settings.
There were several additional limitations. First, many items did not distinguish between pain treatments with and without abuse liability. This aspect of the items made it difficult to discern the relative adaptiveness or risk of harm that some responses reflected. For example, a “very true” response on the Relief Reactivity item, “I have a strong, positive reaction when I experience pain relief” could reflect greater capacity to experience relief (i.e., adaptive response) or the propensity to experience euphorigenic responses associated with substance abuse liability (i.e., risk of harm). Second, retest data were collected one week following the baseline survey, as appropriate for psychometric assessment, but imposes inferential limitations that would be addressed in future studies examining changes in scores over time as a response to manipulations. Third, we were unable to verify self-reported diagnosis of chronic pain with clinician assessment. Future confirmatory studies including people with chronic pain recruited from clinical settings are encouraged. Self-report is the gold standard measure of chronic pain, however, and given that presence of chronic pain was part of the inclusion criteria, the self-report measures were sufficient for the purposes of this study.
Regarding application of the PRMS, it is primarily intended for research use at the present time with future work needed to optimize its psychometric properties as a measure in clinical care. Specifically, research on the affective-motivational aspects of pain relief has been understudied, including behavioral and neuroimaging research. Use of the PRMS can facilitate research in this area and lead to advances in the field’s understanding of the pain-relief hedonic continuum.
Conclusions
Overall, our results support a two-factor BIS-BAS Model of Chronic Pain in the context of pain relief. Future work refining a scale measuring individual differences in hopelessness, persistence, and impulsivity as they relate to the experience of pain relief may inform research and clinical care efforts that bolster adherence to adaptive pain interventions and attenuate risk of analgesic misuse.
Supplementary Material
Acknowledgements
We would like to thank Dr. Jenn-Yun Tein for sharing her valuable expertise in measurement development and consulting on the analytic plan used in the present study. We would also like to thank the participants for their time in completing the survey batteries.
Funding:
F32HL143941 & K23NS124935 (JEL), T32NS070201 (CAH), F32DA049393 & R01NS129887 (CJM)
Footnotes
Conflicts of Interest: JEL is currently employed at the National Institutes of Health but completed work for this project while she was employed at Johns Hopkins University. The opinions expressed in this article are the author’s own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
References
- 1.Leknes S, Tracey I. A common neurobiology for pain and pleasure. Nat Rev Neurosci 2008;9(4):314–320. doi: 10.1038/nrn2333 [DOI] [PubMed] [Google Scholar]
- 2.Becker S, Navratilova E, Nees F, et al. Emotional and motivational pain processing: current state of knowledge and perspectives in translational research. Pain Res Manag 2018; 2018:5457870. doi: 10.1155/2018/5457870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elman I, Borsook D. Common brain mechanisms of chronic pain and addiction. Neuron 2016;89(1):11–36. doi: 10.1016/j.neuron.2015.11.027 [DOI] [PubMed] [Google Scholar]
- 4.Gray JA. The Neuropsychology of Anxiety: An Enquiry into the Functions of the Septo-Hippocampal System. New York, NY, US: Clarendon Press/Oxford University Press; 1982. [Google Scholar]
- 5.Gray JA, McNaughton N. An enquiry into the functions of the septo-hippocampal system. Neuropsychol Anxiety 2000:1–442. [Google Scholar]
- 6.Standen B, Firth J, Sumich A, et al. The neural correlates of reinforcement sensitivity theory: A systematic review of the (f) MRI literature. Psychol Neurosci 2022;15(4):395–422. doi: 10.1037/pne0000284 [DOI] [PubMed] [Google Scholar]
- 7.Jensen MP, Ehde DM, Day MA. The behavioral activation and inhibition systems: implications for understanding and treating chronic pain. J Pain 2016;17(5):529.e1–529.e18. doi: 10.1016/j.jpain.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 8.Serrano-Ibáñez ER, López-Martínez AE, Ramírez-Maestre C, et al. The behavioral inhibition and activation systems and function in patients with chronic pain. Pers Individ Dif 2019;138:56–62. doi: 10.1016/j.paid.2018.09.021 [DOI] [Google Scholar]
- 9.Corr PJ. Reinforcement sensitivity theory of personality questionnaires: structural survey with recommendations. Pers Individ Dif 2016;89:60–64. doi: 10.1016/j.paid.2015.09.045 [DOI] [Google Scholar]
- 10.Day MA, Ward LC, de la Vega R, et al. Development of the pain responses scale: a measure informed by the BIS-BAS model of pain. Eur J Pain 2022;26(2):505–521. [DOI] [PubMed] [Google Scholar]
- 11.Corr PJ, Cooper AJ. The Reinforcement Sensitivity Theory of Personality Questionnaire (RST-PQ): development and validation. Psychol Assess 2016;28(11):1427–1440. doi: 10.1037/pas0000273 [DOI] [PubMed] [Google Scholar]
- 12.Krupić D, Corr PJ, Ručević S, et al. Five reinforcement sensitivity theory (RST) of personality questionnaires: comparison, validity and generalization. Pers Individ Dif 2016;97:19–24. doi: 10.1016/j.paid.2016.03.012 [DOI] [Google Scholar]
- 13.DeVellis RF. Scale development: theory and applications. 4th ed. Los Angeles: SAGE; 2017. [Google Scholar]
- 14.Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. J Pers Soc Psychol 1994;67(2):319. [Google Scholar]
- 15.Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995;7(4):524–532. doi: 10.1037/1040-3590.7.4.524 [DOI] [Google Scholar]
- 16.Fish RA, McGuire B, Hogan M, et al. Validation of the Chronic Pain Acceptance Questionnaire (CPAQ) in an internet sample and development and preliminary validation of the CPAQ-8. Pain 2010;149(3):435–443. doi: 10.1016/j.pain.2009.12.016 [DOI] [PubMed] [Google Scholar]
- 17.Snaith RP, Hamilton M, Morley S, et al. A scale for the assessment of hedonic tone the Snaith–Hamilton Pleasure Scale. Br J Psychiatry 1995;167(1):99–103. doi: 10.1192/bjp.167.1.99 [DOI] [PubMed] [Google Scholar]
- 18.Pilkonis PA, Yu L, Dodds NE, et al. An item bank for abuse of prescription pain medication from the Patient-Reported Outcomes Measurement Information System (PROMIS®). Pain Med 2017;18(8):1516–1527. doi: 10.1093/pm/pnw233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Von Korff M, DeBar LL, Krebs EE, et al. Graded chronic pain scale revised: mild, bothersome, and high impact chronic pain. Pain 2020;161(3):651–661. doi: 10.1097/j.pain.0000000000001758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): depression, anxiety, and anger. Assessment 2011;18(3):263–283. doi: 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steinberg L, Sharp C, Stanford MS, et al. New tricks for an old measure: the development of the Barratt Impulsiveness Scale–Brief (BIS-Brief). Psychol Assess 2013;25(1):216–226. doi: 10.1037/a0030550 [DOI] [PubMed] [Google Scholar]
- 22.Palan S, Schitter C. Prolific.ac—a subject pool for online experiments. J Behav Exp Financ 2018;17:22–27. doi: 10.1016/j.jbef.2017.12.004 [DOI] [Google Scholar]
- 23.Muthén L, Muthén B. Mplus (Version 8)[computer software].(1998–2017). 2017. [Google Scholar]
- 24.Worthington RL, Whittaker TA. Scale development research: a content analysis and recommendations for best practices. Couns Psychol 2006;34(6):806–838. doi: 10.1177/0011000006288127 [DOI] [Google Scholar]
- 25.Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: a tutorial on parallel analysis. Organ Res Methods 2004;7(2):191–205. doi: 10.1177/1094428104263675 [DOI] [Google Scholar]
- 26.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model a Multidiscip J 1999;6(1):1–55. doi: 10.1080/10705519909540118 [DOI] [Google Scholar]
- 27.Howard MC. A review of exploratory factor analysis decisions and overview of current practices: what we are doing and how can we improve? Int J Hum Comput Interact 2016;32(1):51–62. doi: 10.1080/10447318.2015.1087664 [DOI] [Google Scholar]
- 28.Schreiber JB, Nora A, Stage FK, et al. Reporting structural equation modeling and confirmatory factor analysis results: a review. J Educ Res 2006;99(6):323–338. doi: 10.3200/JOER.99.6.323-338 [DOI] [Google Scholar]
- 29.Green SB, Lissitz RW, Mulaik SA. Limitations of coefficient alpha as an index of test unidimensionality. Educ Psychol Meas 1977;37(4):827–838. [Google Scholar]
- 30.Vaske JJ, Beaman J, Sponarski CC. Rethinking internal consistency in Cronbach’s alpha. Leis Sci 2017;39(2):163–173. doi: 10.1080/01490400.2015.1127189 [DOI] [Google Scholar]
- 31.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen J A power primer. Psychol Bull 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- 33.Brown TA. Confirmatory Factor Analysis for Applied Research. 2nd ed. New York: The Guildford Press; 2015. [Google Scholar]
- 34.Serafini RA, Pryce KD, Zachariou V. The Mesolimbic Dopamine System in chronic pain and associated affective comorbidities. Biol Psychiatry 2020;87(1):64–73. doi: 10.1016/j.biopsych.2019.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Becerra L, Navratilova E, Porreca F, et al. Analogous responses in the nucleus accumbens and cingulate cortex to pain onset (aversion) and offset (relief) in rats and humans. J Neurophysiol 2013;110(5):1221–1226. doi: 10.1152/jn.00284.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Becerra L, Borsook D. Signal valence in the nucleus accumbens to pain onset and offset. Eur J pain 2008;12(7):866–869. doi: 10.1016/j.ejpain.2007.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baliki MN, Geha PY, Fields HL, et al. Predicting value of pain and analgesia: nucleus accumbens response to noxious stimuli changes in the presence of chronic pain. Neuron 2010;66(1):149–160. doi: 10.1016/j.neuron.2010.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jensen MP, Tan G, Chua SM. Pain intensity, headache frequency, and the behavioral activation and inhibition systems. Clin J Pain 2015;31(12):1068–1074. doi: 10.1097/AJP.0000000000000215 [DOI] [PubMed] [Google Scholar]
- 39.Day MA, Matthews N, Newman A, et al. An evaluation of the behavioral inhibition and behavioral activation system (BIS-BAS) model of pain. Rehabil Psychol 2019;64(3):279–287. doi: 10.1037/rep0000274 [DOI] [PubMed] [Google Scholar]
- 40.Jensen MP, Sole E, Castarlenas E, et al. Behavioral inhibition, maladaptive pain cognitions, and function in patients with chronic pain. Scand J pain 2017;17:41–48. doi: 10.1016/j.sjpain.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 41.Serrano-Ibáñez ER, Ramírez-Maestre C, López-Martínez AE, et al. Behavioral inhibition and activation systems, and emotional regulation in individuals with chronic musculoskeletal pain. Front Psychiatry 2018;9:394. doi: 10.3389/fpsyt.2018.00394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sánchez-Rodríguez E, Racine M, Castarlenas E, et al. Behavioral activation and inhibition systems: further evaluation of a BIS-BAS model of chronic pain. Pain Med 2021;22(4):848–860. doi: 10.1093/pm/pnaa330 [DOI] [PubMed] [Google Scholar]
- 43.Turner AP, Jensen MP, Day MA, et al. Behavioral activation and behavioral inhibition: an examination of function in chronic pain. Rehabil Psychol 2021;66(1):57–64. doi: 10.1037/rep0000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


