Abstract
Metabolic disease is increasing in people with HIV (PWH) in South Africa, but little is known about self-perceptions of body size, health, and nutritional behavior in this population. We performed a cross-sectional analysis of individual-level data from the 2016 South Africa Demographic and Health Survey. This survey measured HIV serostatus and body mass index (BMI). We categorized participants into six BMI groups: 18.5 – 22 kg/m2, 22 – 25 kg/m2, 25 – 27.5 kg/m2, 27.5 – 30 kg/m2, 30 – 35 kg/m2, and ≥ 35 kg/m2 and stratified these groups by HIV serostatus. Our outcomes were self-reported 1) body size and 2) health status among all participants, and intake of 3) chips and 4) sugar-sweetened beverages in PWH. We described these metrics and used multivariable regression to evaluate the relationship between the nutritional behaviors and BMI ≥25 kg/m2 in PWH only, adjusting for age, sex, and educational attainment, as well as household wealth quintile. Of 6,138 participants, 1,163 (19.7%) were PWH. Among PWH, <10% with a BMI 25-30 kg/m2, <20% with a BMI 30-35 kg/m2 and <50% with a BMI ≥35 kg/m2 self-reported as overweight or obese. PWH reported being in poor health at higher rates than those without HIV at each BMI category except ≥35 kg/m2. In adjusted models, SSB consumption was associated with BMI ≥25 kg/m2 (1.13 [1.01 – 1.25], p = 0.033) in PWH. Perceptions of body size may challenge efforts to prevent weight gain in PWH in South Africa. SSB intake reduction should be further explored as a modifiable risk factor for obesity.
Keywords: obesity, HIV, self-perceptions, nutrition
South Africa faces a growing epidemic of metabolic disease, as more than two-thirds of adult women and one-third of adult men, including both people with HIV (PWH) and those without HIV, were overweight or had obesity in 2016.1-4 Additionally, in 2018, diabetes was named the second leading cause of death in the country.4,5 For people with HIV (PWH), the risk of metabolic disease is heightened by excess weight gain that may accompany newer antiretroviral treatment regimens including integrase inhibitors.6,7 The confluence of aging, urbanization and changes in diet and activity that have contributed to a high prevalence of overweight and obesity in the general population,8 compounded by ART-associated excess weight gain, are expected to place PWH at particularly high risk of both obesity and downstream type 2 diabetes (hereafter “diabetes”).9-12 This is a pressing concern for the South African national HIV treatment program which has transitioned nearly 6 million people with HIV to dolutegravir-based regimens (DTG), the preferred first-line ART regimen as recommended by the WHO and one that has been associated with weight gain. Without intervention, excess ART-emergent weight gain in PWH may further exacerbate an already pressing public health problem.13
Given these trends, there is a pressing need for effective strategies to prevent weight gain and diabetes in PWH in South Africa and ART programs have shown preliminary promise as a platform through which delivery of such interventions may be pursued.14-16 However, there are few studies about key themes relevant to intervention development, including self-perceptions of body habitus and the health threats of obesity particular to PWH in this context.17,18 Similarly, there is little evidence about potentially modifiable nutritional behaviors as risk factors for overweight and obesity among PWH. Together, this understanding is critically important to identify and design interventions that show promise to prevent metabolic disease in PWH, as the success of any measures relies in part on these perceptions and possibly also modifiable behaviors that increase risk of weight gain and are amendable to intervention.
In this study, we assessed self-perceptions of health and body size among people with and without HIV in South Africa and explored the relationship between nutritional behavior and risk of overweight or obesity among PWH. To do this, we used nationally representative population-based data from the South Africa Demographic and Health Survey (SADHS) conducted in 2016, shortly before the roll-out of integrase inhibitor-based ART. This survey included measures of both HIV serostatus and anthropometry, along with questions relevant to the themes of interest. This analysis offers important data to inform the design of interventions and policies that may prevent weight gain and diabetes in PWH in South Africa, with potential implications for PWH in other settings.
METHODS
Data source
We performed a cross-sectional analysis of individual-level data from the nationally representative, population-based SADHS 2016.1 The survey was conducted by Statistics South Africa in partnership with the Demographic and Health Surveys. SADHS 2016’s objective was to provide recent information on demographic and health indicators for the South African population that can be used to design effective programs and policies to improve national public health.1 The survey provided valuable information on HIV/AIDS knowledge and status, non-communicable disease (NCD) prevalence, dietary practices, body perception, and biological measures such as body mass index (BMI) and HIV antibody status. All participants in the survey were between the ages of 15 and 49.1 Our study sample was restricted to all participants who had data on HIV status and measured body mass index (BMI). Finally, we excluded those who were underweight with a BMI <18.5 kg/m2. The reasoning for this was that those who are underweight may be more likely to have a secondary health problem that would influence their reporting of the outcomes of interest in this study.
HIV testing and anthropometric measures
Individuals who consented to HIV testing had blood specimens collected. These were assessed using an enzyme-linked immunosorbent assay (ELISA, Genscreen HIV ½ Combi Assay Bio-Rad) based on a parallel testing algorithm to ensure accuracy. Height was measured using Seca 213 stadiometers and weight measured using Seca 878 digital scales. Participant BMI values were calculated by dividing the individual’s weight (measured in kg) by height (measured in meters) squared, which we then selected as our primary exposure of interest. To facilitate analysis, we categorized individuals into the following BMI groups: 18.5 – 22 kg/m2, 22 – 25 kg/m2, 25 – 27.5 kg/m2, 27.5 – 30 kg/m2, 30 – 35 kg/m2, and ≥ 35 kg/m2. We chose to use more granular BMI groups as this is frequently done in the obesity-related literature and because the applicability of traditional, clinical BMI thresholds for defining obesity in global populations have been questioned.19-21 Additionally, we defined a binary variable for whether a participant was overweight or had obesity (≥25 kg/m2), as opposed to normal weight, using widely accepted clinical cut-offs. Finally, we classified these BMI groups further based on HIV serostatus.
Participant survey responses of self-perception and nutritional behavior
The primary outcomes of interest were 1) self-reported body size and 2) self-reported overall health status. Participants were asked two questions in this thematic area: 1) “Do you personally think that you are underweight, normal weight, overweight, or obese?”; and 2) “Would you say your health is poor, average, good, or excellent?” We dichotomized responses into the following categories: 1) underweight or normal weight v. overweight or obese and 2) average, good, or excellent health v. poor health.
Secondary outcomes of interest were two self-reported nutritional behaviors, specifically intake of potato chips and sugar-sweetened beverages (SSB), among only PWH due to the interest in identifying potential entry points for behavior modification specific to this subpopulation. Participants were asked a series of questions about specific nutritional behaviors that may relate to risk of obesity. The first question centered on intake of chips and other snack foods that we hypothesized may be associated with obesity in this group, and read as follows: “How often do you eat chips such as a packet of crispy chips or similar salty snacks such as Doritos, cheese curls, salted nuts, salty biscuits, etc.?” with possible responses being “every day,” at least once a week, “occasionally,” and “never.” We considered responses of “every day” or “at least once a week” to be frequent chips consumption, while responses of “occasionally” or “never” to be infrequent chips consumption.
The second question was, “Yesterday, did you drink any sugar-sweetened drinks? Sugar sweetened drinks include fizzy drinks like Coke or drinks like Squash where water is added, but not diet or unsweetened cold drinks” and “Yesterday, did you drink any fruit juice?” We defined a participant as a probable regular consumer of sugar-sweetened beverages if they responded yes to either question or infrequent if they responded no to both.
Statistical analysis
We summarized and compared individual sociodemographic characteristics by HIV serostatus, with chi-squared tests of comparison across groups where appropriate. We performed a descriptive analysis of the percentage of participants in each of the BMI categories reported self-perception as overweight or obese, overall, and then among PWH and people without HIV separately. This analysis was then repeated with self-perception of poor health as the outcome of interest. To assess the relationship between BMI and self-perception of health and body size, we conducted adjusted Poisson regression models with a robust error structure stratified by HIV status with our two self-perception variables as the outcomes and a BMI category in the groups described as the exposure variable of interest.
For our secondary analysis of nutritional behavior among PWH, we restricted our sample to PWH. We performed two separate descriptive analyses of what percentage of participants in each of the previously defined BMI categories reported frequent chips and regular SSB intake, respectively. Finally, we conducted adjusted Poisson regression models with our two nutritional behaviors serving each service as an exposure variable (in separate models) and a binary variable for whether the participant has a BMI ≥25 kg/m2 as the outcome of interest. All analyses were estimated with a robust error structure that made use of sampling weights rescaled to account for missing responses and measures. All Poisson regressions were adjusted for age in years, sex, and educational attainment categorized as no education, primary schooling, secondary schooling, and greater than secondary education. All data analyses were conducted using Stata 16.1 (StataCorp, College Station, TX).
Sensitivity analyses
We tested the robustness of our result through several sensitivity analyses. First, we recategorized the BMI groups as follows, 18.5 – 25 kg/m2, 25 – 30 kg/m2, and ≥ 35 kg/m2 and explored the proportion of each group that reported each of the possible options for self-perception of health and self-perception of body size, without dichotomizing these responses. Second, we re-estimated the adjusted Poisson regression models for the dichotomized self-perception using the categorization of BMI in three groups as the exposure variable of interest. Third, we modelled the adjusted relationships between BMI and self-perception and nutritional behavior and being overweight or obese using multivariable logistic regressions. Fourth, we included wealth quintile as an additional covariate in our models.
Results
Our analytical sample included 1,163 PWH (19.7%) and 4,975 people without HIV (80.3%). Comparisons of individual sociodemographic characteristics by HIV serostatus are presented in Table 1. When compared to those without HIV, PWH were younger (mean age 38.5 years vs 40.1 years, t-statistic = 2.66, p = 0.008) and a greater percentage of them were female (74.4% vs 60.3%, corrected F -statistic = 41.12, p < 0.001), had at least a secondary-level education (corrected F-statistic = 6.81, p < 0.001), and were of lower socio-economic status (corrected F-statistic = 8.30, p < 0.001).
Table 1.
Cohort demographics by HIV serostatus
| Characteristics | HIV + (N = 1,163) |
HIV − (N = 4975) |
Test statistic |
p-value |
|---|---|---|---|---|
| Age, years | 38.5 [37.6 - 39.5] | 40.1 [39.3 – 41.0] | 2.66 | 0.008 |
| Female | 888 (74.4) | 3,038 (60.3) | 41.12 | <0.001 |
| Education | 6.81 | <0.001 | ||
| No education | 91 (6.5) | 514 (8.8) | ||
| Primary | 280 (19.9) | 1,089 (19) | ||
| Secondary | 801 (68.8) | 3,243 (62.3) | ||
| Higher | 49 (4.8) | 436 (9.8) | ||
| Wealth | 8.30 | <0.001 | ||
| Poorest | 322 (25.4) | 1,156 (21.1) | ||
| Poorer | 327 (23.4) | 1,101 (18.9) | ||
| Middle | 310 (24.5) | 1,241 (21.1) | ||
| Richer | 201 (17.1) | 1,084 (19.8) | ||
| Richest | 75 (9.7) | 751 (19.1) |
Results presented as either mean [95% confidence interval] or unweighted n (weighted %). P-values estimated using linear regression models (along with the absolute value of the t-statistic) for continuous variables and Chi squared tests (along with corrected Pearson’s F statistic) for categorical variables. Estimates calculated using survey design weights.
Self-perception of body size and health
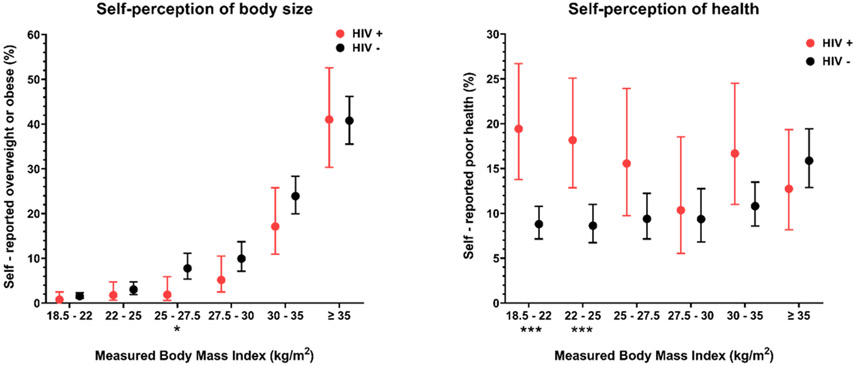
Overall, 12.5% [11.3 – 13.8] of individuals reported being overweight or obese at any BMI category. When stratified by HIV serostatus, PWH self-reported being overweight or having obesity at lower rates when compared to those without HIV at each BMI category except for the ≥ 35 kg/m2 group, though not all these comparisons were statistically significant. (Figure 1). For example, among those with a BMI of 25 – 27.5 kg/m2,1.9% of PWH and 7.8% of people without HIV reported being overweight or obese (corrected F-statistic = 6.45, p=0.011); among those with a BMI of 30 – 35 kg/m2 17.1% (10.9 - 25.8) and 23.9% (19.9 - 28.4) reported being overweight or obese (corrected F-statistic = 2.06, p=0.152), respectively. Conversely, compared to those without HIV, PWH reported being in poor health at higher rates at each BMI category except for the ≥ 35 kg/m2 group. Several but not all of these group comparisons were statistically significant (Figure 1, Appendix eTable 1 and eTable 2). Table 2 and Table 3 show adjusted Poisson regression models, performed separately for PWH and people without HIV, that estimate the relationship between actual BMI and self-perception as overweight or obese and self-perceived poor health, respectively. When comparing risk ratios (RR) associated with each BMI category relative to the 18.5 – 22 kg/m2 group, we observed a statistically significant positive association between actual BMI and self-perception as overweight or obese beginning at the 27.5 kg/m2 group for PWH (RR 8.07 [1.94 – 33.55]), but a similar, positive association beginning at the 22 – 25 kg/m2 group for those without HIV (RR 1.79 [1.02 – 3.15]). There were no differences in the association between actual BMI and self-perceived poor health across the two groups.
Figure 1. Participant self-perception of body size and health by actual BMI, stratified by HIV serostatus.
Figure shows the weighted proportion of participants in each BMI group that reported self-perception as overweight or obese and the weighted proportion of participants in each BMI group that reported self-perceived poor health. Error bars represent 95% confidence intervals. * indicates p-value <0.05, ** indicates p-value < 0.01, *** indicates p-value <0.001. P-values calculated through chi-squared tests by BMI group, accounting for sampling weights.
Table 2.
Multivariable Poisson regression models of the relationship between BMI and self-perception of being overweight or obese, stratified by HIV status
| HIV positive | HIV negative | |||
|---|---|---|---|---|
| RR (95% CI) | t-statistic | RR (95% CI) | t-statistic | |
| BMI | ||||
| 18.5 - 22 | REF | - | REF | - |
| 22 - 25 | 2.55 (0.55 - 11.85) | 1.20 | 1.79 (1.02 - 3.15) | 2.02 |
| 25 - 27.5 | 2.96 (0.55 - 15.96) | 1.26 | 5.58 (3.26 - 9.54) | 6.29 |
| 27.5 - 30 | 8.07 (1.94 - 33.55) | 2.88 | 7.85 (4.60 - 13.40) | 7.57 |
| 30 - 35 | 30.73 (8.68 - 108.78) | 5.32 | 19.94 (12.56 - 31.64) | 12.73 |
| ≥ 35 | 68.54 (20.21 - 232.4) | 6.80 | 35.68 (22.68 - 56.14) | 15.49 |
| Age | 0.97 (0.95 - 0.99) | 2.97 | 0.99 (0.99 – 1.00) | 1.89 |
| Sex | ||||
| Male | REF | - | REF | - |
| Female | 0.81 (0.42 - 1.59) | 0.60 | 0.69 (0.56 - 0.86) | 3.41 |
| Education | ||||
| No education | REF | - | REF | - |
| Primary | 0.77 (0.15 - 4.07) | 0.30 | 1.09 (0.70 - 1.70) | 0.38 |
| Secondary | 1.12 (0.23 - 5.45) | 0.14 | 1.93 (1.24 – 3.01) | 2.92 |
| Higher | 0.58 (0.08 - 4.01) | 0.55 | 3.17 (2.03 - 4.93) | 5.11 |
Multivariable Poisson regressions estimated with sampling weights. Results presented as risk ratios (95% confidence intervals). t-statistics presented as absolute values.
Table 3.
Multivariable Poisson regression models of the relationship between BMI and self-perception of poor health, stratified by HIV status
| HIV positive | HIV negative | |||
|---|---|---|---|---|
| Self-perceived overweight/obese |
Self-perceived poor health |
Self-perceived overweight/obese |
Self-perceived poor health |
|
| BMI | ||||
| 18.5 - 22 | REF | - | REF | - |
| 22 - 25 | 0.89 (0.57 - 1.38) | 0.54 | 0.80 (0.58 - 1.09) | 1.41 |
| 25 - 27.5 | 0.66 (0.40 - 1.09) | 1.62 | 0.73 (0.53 - 1.02) | 1.87 |
| 27.5 - 30 | 0.45 (0.23 - 0.88) | 2.35 | 0.60 (0.42 - 0.85) | 2.89 |
| 30 - 35 | 0.67 (0.41 - 1.08) | 1.64 | 0.67 (0.49 - 0.90) | 2.62 |
| ≥ 35 | 0.46 (0.28 - 0.76) | 3.02 | 1.01 (0.76 - 1.33) | 0.04 |
| Age | 1.03 (1.02 - 1.05) | 5.78 | 1.04 (1.03 - 1.04) | 12.47 |
| Sex | ||||
| Male | REF | - | REF | - |
| Female | 1.52 (1.03 - 2.23) | 2.12 | 1.21 (.96 - 1.52) | 1.61 |
| Education | ||||
| No education | REF | - | REF | - |
| Primary | 0.65 (0.45 - 0.94) | 2.28 | 1.04 (0.82 - 1.31) | 0.34 |
| Secondary | 0.47 (0.31 - 0.71) | 3.54 | 0.78 (0.59 - 1.03) | 1.77 |
| Higher | 0.10 (0.01 - 0.69) | 2.35 | 0.19 (0.10 - 0.39) | 4.68 |
Multivariable Poisson regressions estimated with sampling weights. Results presented as risk ratios (95% confidence intervals). t-statistics presented as absolute values.
In sensitivity analyses where BMI was recategorized into three groups, we identified very similar associations between actual BMI and self-perception as overweight or having obesity between the two groups (Appendix eFigure 1 and eFigure 2). In the models of self-perceived poor health, both the 25 – 30 kg/m2 and ≥ 30 kg/m2 categories were associated with statistically significant RRs (0.61 [0.40 – 0.92] and 0.61 [0.41 – 0.90], respectively) among PWH. When the sample was restricted to those without HIV, only the 25 – 30 kg/m2 category was associated with a statistically significant RR (0.75 [0.59 – 0.95]) (Appendix eTable 3).
Nutritional Behavior
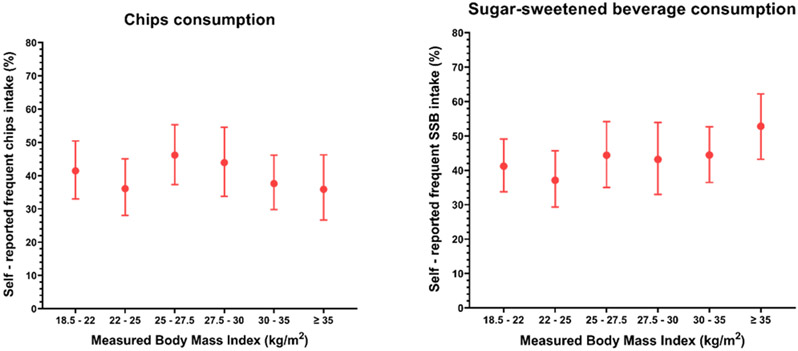
Rates of frequent chips and SSB consumption by BMI category among PWH are shown in Figure 2. The percentages of PWH who reported frequent chips consumption in ascending order of BMI group were as follows: 41.4% [33.0 – 50.4], 36.1% [28.0 – 45.0], 46.2% [37.3 – 55.3], 43.9% [33.8 – 54.6], 37.6% [29.8 – 46.1], and 35.9% [26.7 – 46.2]. The percentages of PWH who reported SSB consumption did not vary across ascending BMI groups, as follows: 41.2% [33.7 – 49.1], 37.1% [29.3 – 45.7], 44.4% [35.0 – 54.2], 43.2% [33.0 – 53.9], 44.4% [36.5 – 52.7], and 52.8% [43.2 – 62.2]. In adjusted Poisson regression models, we found a significant, positive relationship between frequent SSB consumption and risk of overweight or obesity among PWH (1.13 [1.01 – 1.25], t-statistic = 2.14, p = 0.033). (Table 4) There was no statistically significant association with frequent chips consumption (Appendix eTable 8). In sensitivity analyses, the use of logistic regression and addition of wealth to these models did not alter these findings (Appendix eTables 4-7).
Figure 2. Nutritional risk factors by actual BMI among people with HIV.
Figure shows the weighted proportion of participants in each BMI group that reported frequent chips intake and the proportion of participants in each BMI group that reported sugar-sweetened beverages. Error bars represent 95% confidence intervals.
Table 4.
Multivariable Poisson regression models of the relationship between sugar-sweetened beverage intake and being overweight or obese among people living with HIV
| BMI ≥25 kg/m2 | RR (95% CI) | t-statistic | p-value |
|---|---|---|---|
| Nutritional risk factor | |||
| Infrequent intake | REF | ||
| Frequent intake | 1.13 (1.01 - 1.25) | 2.14 | 0.033 |
| Age | 1.02 (1.01 - 1.02) | 5.78 | <0.001 |
| Sex | |||
| Male | REF | ||
| Female | 2.33 (1.87 - 2.91) | 7.48 | <0.001 |
| Education | |||
| No education | REF | ||
| Primary | 1.11 (0.90 - 1.37) | 1.01 | 0.315 |
| Secondary | 1.30 (1.06 - 1.59) | 2.51 | 0.012 |
| Higher | 1.70 (1.33 - 2.18) | 4.26 | <0.001 |
Multivariable Poisson regressions estimated with sampling weights. Results presented as risk ratios (95% confidence intervals). t-statistics presented as absolute values. Abbreviations: BMI = body mass index, CI = confidence interval, RR = risk ratio, and SSB = sugar-sweetened beverages.
DISCUSSION
This study identified important and distinct patterns of self-perception in both overall health status and body size among PWH, with <10% with a BMI 25-30 kg/m2, <20% with a BMI 30-35 kg/m2 and <50% with a BMI ≥35 kg/m2 self-reporting as overweight or obese. Moreover, a substantially greater proportion of PWH perceived themselves as being in poor health at every BMI category in the traditionally defined “normal,” “overweight,” or “obese” categories except >35 kg/m2. Furthermore, PWH with overweight or obesity were more likely to report sugar-sweetened beverage intake. This finding suggests that SSB intake may be a nutritional behavior associated with obesity in this population that could also be modified through public health interventions.
These results are important for several reasons. First, with the transition of all PWH to dolutegravir-based ART regimens in South Africa and beyond, there is a growing concern that the treatment of HIV may itself exacerbate obesity and increase the risk of downstream cardiovascular and metabolic disease.9 This is particularly important given the movement toward initiating ART early in the disease process and the fact that studies increasingly demonstrate risk of weight gain beyond the “return to health” phenomena that is expected with treatment initiation in later-stage disease. A deeper understanding of the perceptions of actual and desired body size for PWH in this setting, as well as possible modifiable behavioral risk factors for obesity specific to this group, are useful to inform the design of policies, programs, and interventions to prevent weight gain and diabetes in this population. Furthermore, an understanding of the health threat of obesity may be an important element in efforts to prevent weight gain in this population. Additionally, these insights may also offer valuable context for providers who wish to counsel patients in clinical settings about the possible health complications of obesity.
The results also revealed that SSB intake may be associated with overweight or obesity in PWH. This is important because decreasing the intake of sugary beverages has been a focal point of intervention studies to prevent weight gain across numerous contexts and an important South African national policy via taxes on these items.22,23 Our findings reinforce the possibility that this specific behavior to serve as an effective focal point for future individual-based interventions to prevent obesity in this population. However, this behavior should first be studied in greater detail using stronger causal inference approaches. Additionally, women and PWH with higher educational attainment were also more likely be to be overweight or obese based on these traditional BMI thresholds. These findings are important given the well-described risk of ART-associated weight gain in women with HIV as compared to men with HIV, as interventions centered on these groups may also be a priority in the effort to limit risk of excess weight gain and diabetes.
These results are consistent with several important prior studies from South Africa that have described the perceived health threat of obesity in the general population. The first was conducted in 2014-2015.17 This study consisted of a series of focus group discussions with a total of 78 participants from a township outside of Cape Town.17 The participants were sampled from among those who took part in the Prospective Urban and Rural Epidemiology (PURE) cohort study of cardiovascular health in adults and included men and women across a wide range of BMIs. This study revealed several important findings. First, most participants expressed that being overweight was more desirable while underweight was associated with stigmatized diseases such as HIV, TB, and cancer.17 These findings were similar to a second study of body perceptions among university-employed South African women and a more recent one of adults living in Soweto.18,24 In addition, women and especially overweight women, tended to underestimate their body size and had low perceptions of the threat of obesity. Additionally, a community-based survey of 1,050 people in three provinces (Gauteng, North West, and Mpumalanga) showed that >90% of those who were overweight according to their calculated BMI did not perceive any risk of developing obesity-related diseases.25 These findings are generally concordant with the low proportion of self-reported overweight or obesity in our analysis and the much larger proportion of PWH who self-reported being in poor health at what is considered by traditional clinical standards to be a normal or overweight BMI, as compared to people without HIV at this same BMI in this context. Though these findings cannot establish a causal link between body weight and either actual or perceived health status, they do reinforce to the hypothesis that thinness may be viewed by some as a sign of illness, and specifically advanced HIV, and that higher body weight signifies one is healthy.
There are several limitations to this study. First, there were no additional HIV-related parameters available to further characterize ART treatment history, viral load, or nadir CD4 count. In addition, while sampling weights have been created to account for non-participation in the HIV biomarker; these weights assume that non-response to the HIV test is missing at random. If this assumption is violated, the survey results may not be fully generalizable. Second, in this sample and minimal information about comorbid medical conditions. This lack of information could confound the findings, as it is possible that people who self-rate their health as poor may in fact be suffering from untreated HIV, an opportunistic infection, or another unmeasured health complication. Third, the survey primarily sampled women ages 15 to 49 and men ages 15-59. Given this, the analysis is unable to address well how these perceptions and behaviors may differ in older adults. Fourth, given the cross-sectional nature of these data, we were unable to establish a definitive causal relationship between the exposures and outcomes of interest. However, there is a strong and well-accepted biological basis for these dietary behaviors to increase risk of obesity. Additionally, the reporting of dietary behavior such as SSB intake may not be perfectly accurate due to recall or social desirability biases in this population. In particular, the questions about SSB intake focus on the 24-hour period prior to the survey and this may not fully capture general dietary trends. However, there are also several important strengths of the study. First, this is a nationally representative survey that should offer a generalizable assessment of this theme in the South African context. In addition, both BMI and HIV serostatus are biologically measured and thus analyses do not rely on self-reported data, which may be less accurate than what is presented here.
In summary, in this study we found that PWH reported important differences in the self-perception of their health at traditionally defined normal or overweight BMI compared to people without HIV in South Africa. Furthermore, SSB intake was associated with being overweight or having obesity in South African PWH. These findings offer important insight to inform future policies and interventions to prevent obesity and diabetes in PWH, currently a pressing public health concern in the context of the growing rates of obesity and diabetes in this region.
Supplementary Material
Acknowledgements:
We would like to thank both the survey teams and participants in the 2016 South Africa Demographic and Health Survey.
Statements and Declarations:
This research was supported by the National Institutes of Health/National Institute on Diabetes, Digestive and Kidney Diseases (NIH/NIDDK) grant K23DK125162 (PI: Manne-Goehler). The authors have no competing interests or other funding sources to disclose. The 2016 South Africa Demographic and Health Survey protocol was reviewed and approved by the SAMRC Ethics Committee and the ICF Institutional Review Board. Informed consent was conducted per the survey’s procedures. This analysis of the secondary deidentified survey data was exempt from additional ethical clearance.
Bibliography
- 1.ICF. The DHS Program: Demographic and Health Surveys. 2021. https://dhsprogram.com/ (accessed March 25, 2021.
- 2.Flood D, Seiglie JA, Dunn M, et al. The state of diabetes treatment coverage in 55 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data in 680 102 adults. Lancet Healthy Longev 2021; 2(6): e340–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manne-Goehler J, Atun R, Stokes A, et al. Diabetes diagnosis and care in sub-Saharan Africa: pooled analysis of individual data from 12 countries. Lancet Diabetes Endocrinol 2016; 4(11): 903–12. [DOI] [PubMed] [Google Scholar]
- 4.Stokes A, Berry KM, McHiza Z, et al. Prevalence and unmet need for diabetes care across the care continuum in a national sample of South African adults: Evidence from the SANHANES-1, 2011-2012. PLoS One 2017; 12(10): e0184264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Statistics South Africa. TB tops leading causes of death in SA in 2018. 2021. https://www.statssa.gov.za/?p=14435 (accessed October 17 2022).
- 6.Venter WDF, Moorhouse M, Sokhela S, et al. Dolutegravir plus Two Different Prodrugs of Tenofovir to Treat HIV. N Engl J Med 2019; 381(9): 803–15. [DOI] [PubMed] [Google Scholar]
- 7.Verburgh ML, Wit F, Boyd A, Verboeket SO, Reiss P, van der Valk M. One in 10 Virally Suppressed Persons With HIV in The Netherlands Experiences >/=10% Weight Gain After Switching to Tenofovir Alafenamide and/or Integrase Strand Transfer Inhibitor. Open Forum Infect Dis 2022; 9(7): ofac291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Popkin BM. Nutrition Transition and the Global Diabetes Epidemic. Curr Diab Rep 2015; 15(9): 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Milic J, Renzetti S, Ferrari D, et al. Relationship between weight gain and insulin resistance in people living with HIV switching to integrase strand transfer inhibitors-based regimens. AIDS 2022; 36(12): 1643–53. [DOI] [PubMed] [Google Scholar]
- 10.Herrin M, Tate JP, Akgun KM, et al. Weight Gain and Incident Diabetes Among HIV-Infected Veterans Initiating Antiretroviral Therapy Compared With Uninfected Individuals. J Acquir Immune Defic Syndr 2016; 73(2): 228–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Esber AL, Chang D, Iroezindu M, et al. Weight gain during the dolutegravir transition in the African Cohort Study. J Int AIDS Soc 2022; 25(4): e25899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bailin SS, Koethe JR. Diabetes in HIV: the Link to Weight Gain. Curr HIV/AIDS Rep 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCann K, Shah S, Hindley L, et al. Implications of weight gain with newer anti-retrovirals: 10-year predictions of cardiovascular disease and diabetes. AIDS 2021; 35(10): 1657–65. [DOI] [PubMed] [Google Scholar]
- 14.Manne-Goehler J, Ogbuoji O, Barnighausen TW. Converting HIV programmes into chronic-care platforms. Lancet HIV 2020; 7(9): e600–e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manne-Goehler J, Siedner MJ, Montana L, et al. Hypertension and diabetes control along the HIV care cascade in rural South Africa. J Int AIDS Soc 2019; 22(3): e25213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Magodoro IM, Okello S, Dungeni M, Castle AC, Mureyani S, Danaei G. Association between HIV and Prevalent Hypertension and Diabetes Mellitus in South Africa: Analysis of a Nationally Representative Cross-Sectional Survey. Int J Infect Dis 2022; 121: 217–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Okop KJ, Mukumbang FC, Mathole T, Levitt N, Puoane T. Perceptions of body size, obesity threat and the willingness to lose weight among black South African adults: a qualitative study. BMC Public Health 2016; 16: 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gradidge PJ, Golele P, Cohen E. Body weight perceptions and obesity amongst university employed South African women. Women Health 2020; 60(8): 851–62. [DOI] [PubMed] [Google Scholar]
- 19.Teufel F, Seiglie JA, Geldsetzer P, et al. Body-mass index and diabetes risk in 57 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data in 685 616 adults. Lancet 2021; 398(10296): 238–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Motala AA, Esterhuizen T, Pirie FJ, Omar MA. The prevalence of metabolic syndrome and determination of the optimal waist circumference cutoff points in a rural South african community. Diabetes Care 2011; 34(4): 1032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Caleyachetty R, Barber TM, Mohammed NI, et al. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol 2021; 9(7): 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Essman M, Taillie LS, Frank T, Ng SW, Popkin BM, Swart EC. Taxed and untaxed beverage intake by South African young adults after a national sugar-sweetened beverage tax: A before-and-after study. PLoS Med 2021; 18(5): e1003574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malik VS, Hu FB. The role of sugar-sweetened beverages in the global epidemics of obesity and chronic diseases. Nat Rev Endocrinol 2022; 18(4): 205–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bosire EN, Cohen E, Erzse A, Goldstein SJ, Hofman KJ, Norris SA. 'I'd say I'm fat, I'm not obese': obesity normalisation in urban-poor South Africa. Public Health Nutr 2020; 23(9): 1515–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manafe M, Chelule PK, Madiba S. Views of Own Body Weight and the Perceived Risks of Developing Obesity and NCDs in South African Adults. Int J Environ Res Public Health 2021; 18(21). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.