Abstract
Objectives
We examined racial and gender disparities in the under-recognition of mental health disorders in adolescents and young adults (AYA) as defined by a suicide-related diagnosis without a previous mental or behavioral health diagnosis (MBHD).
Methods
We employed a series of adjusted mixed multilevel logistic regression models to determine the odds of specific mental health diagnoses (anxiety, depression, suicide-related) in a large, U.S. pediatric ambulatory care group (ages 8–20) using Electronic Medical Record (EMR) Data.
Results
Using the reference group of White males, White females had 17% increased odds of having a suicide-related diagnosis (OR 1.17, 95% CI 1.03, 1.34) and Black females had 48% increased odds of suicide-related diagnosis (OR 1.48, 95% CI 1.28, 1.71). Conversely, White females had 75% increased odds of recorded anxiety (OR 1.75, 95% CI 1.62, 1.89), Black males had 62% decreased odds of anxiety (OR 0.38, 95% CI 0.33, 0.42), and Black females had 33% decreased odds of anxiety (OR .67, 95% CI .60, .74). White females had 81% increased odds of having recorded depression (OR 1.81, 95% CI 1.62, 2.04) and Black females had 80% increased odds of under-recognized need for MBHD services (OR 1.80, 95% CI 1.53, 2.13) as defined by a suicide-related diagnosis without a previous mental health diagnosis.
Conclusions
Black AYA patients are either not accessing or identified as needing mental health services at the same rates as White peers, and Black females are experiencing the most under-recognition of need for mental health services.
Keywords: suicide, anxiety, depression, adolescent, disparities
Background
There is clearly a mental health crisis among adolescents and young adults (AYA) in the U.S. Alarming rates of anxiety, depression, and suicide have led to nationwide calls for action to address the growing problem. 1 It is also becoming clear that mental health problems are not affecting all AYA uniformly. The national suicide death rate for Black adolescent females increased by 183% from 2001 to 2019.2 According to the 2019 High School Youth Risk Behavior Survey, 41.2% of Black and 46.1% of White adolescent females reported feeling sad or hopeless almost every day for 2 weeks or more in the year prior to the survey, numbers nearly double that of their White or Black male counterparts (who still reported feeling sad and hopeless at rates of 21.4% and 17.3%, respectively).3 Given indicators of need for mental health care among adolescents, it is notable that Black youth are less likely than their White peers to access and receive such services.4 A study using data from the nationally-representative Medical Expenditure Panel Survey found that, among 5 to 17 year old patients in need of mental health treatment, fewer than half engaged with mental health care, and female, minoritized, and uninsured patients were significantly less likely to initiate treatment.5 Even when other factors related to use of mental health services, such as income, insurance and type and severity of diagnoses are taken into account, the differences in utilization by gender and race persist.6,7
It is informative to examine under-recognition of need for mental health services among AYA through a lens of intersectionality of race and gender.8 There are subgroup-specific stressors unique to the lived experience of Black AYA females in the U.S. that are contributing to the mental health crisis in this group, while Black males and White males and females are living with potentially very different sets of stressors and sociocultural constructs.9 Ultimately, it may be most helpful to generate tailored interventions for subgroups of at-risk AYA, as opposed to “one size fits all” programs.9,10 Examining subgroups of White females, Black males and Black females, specifically as they compare to White males can help to tease apart the complicated web of gender and race when it comes to mental health services needs and utilization.
The measurement of mental health needs and service utilization among AYA is challenging. Most U.S. studies report data from large- or small-scale surveys, consisting of either self-reported utilization of services and/or employing validated self-report tools. Some European and Australian studies have reported more broadly about mental health indicators using national health records, but these studies have focused on largely white, homogeneous populations.11 The increasing availability of electronic medical record (EMR) data holds promise for research in this area, as it may provide a vital dimension to understanding patient-level service interaction and utilization and ultimately allow for a more precise approach to patient care. While EMR data does not have the targeted, validated information that may be found in a national survey, it is a readily available means for understanding longitudinal interactions with service providers as they relate to patients’ histories, diagnoses, referrals for outside care and medications.
While a mental and behavioral health disorder (MBHD) related diagnosis code would be reliant on either the recognition of a patient’s mental health needs and/or a patient accessing care, the recording of a suicide attempt or intentional self-harm is not, necessarily, as a suicide attempt is often entered as a diagnosis in the patient’s medical record by either the admitting hospital or primary care physician (PCP) at the time of the attempt or follow up visit. Similarly, suicidal ideation may be entered into a patient’s record as a result of a positive screening using the PHQ-9 screening tool for depression.12 Previous studies have found that treatment of underlying MBHD can reduce rates of suicide attempt and/or ideation, and that there is a strong correlation between self-perceived unmet need for mental health services and suicidality13–17 (See Figure 1 for our guiding conceptual framework for unrecognized need for MHT for AYA in a primary care setting). While some research has shown increased interaction with primary care providers for 30 days in the 6 months prior to a suicide attempt in AYA, little is known about interaction with primary care in the year or years preceding a suicide attempt.18,19 Exploration of patients with recorded suicide attempt or other suicide-related diagnosis code given prior MBHD diagnosis and/or treatment using EMR data may shed new light on the dynamics of under-recognition of mental health disorders, especially in relation to intersectionality of gender and race. Thus, our objective was to examine the association between patient demographics (composite sex and race) and having an MBHD diagnosis recorded prior to a suicide-related diagnosis code, using data from a large pediatric primary care practice.
Figure 1.
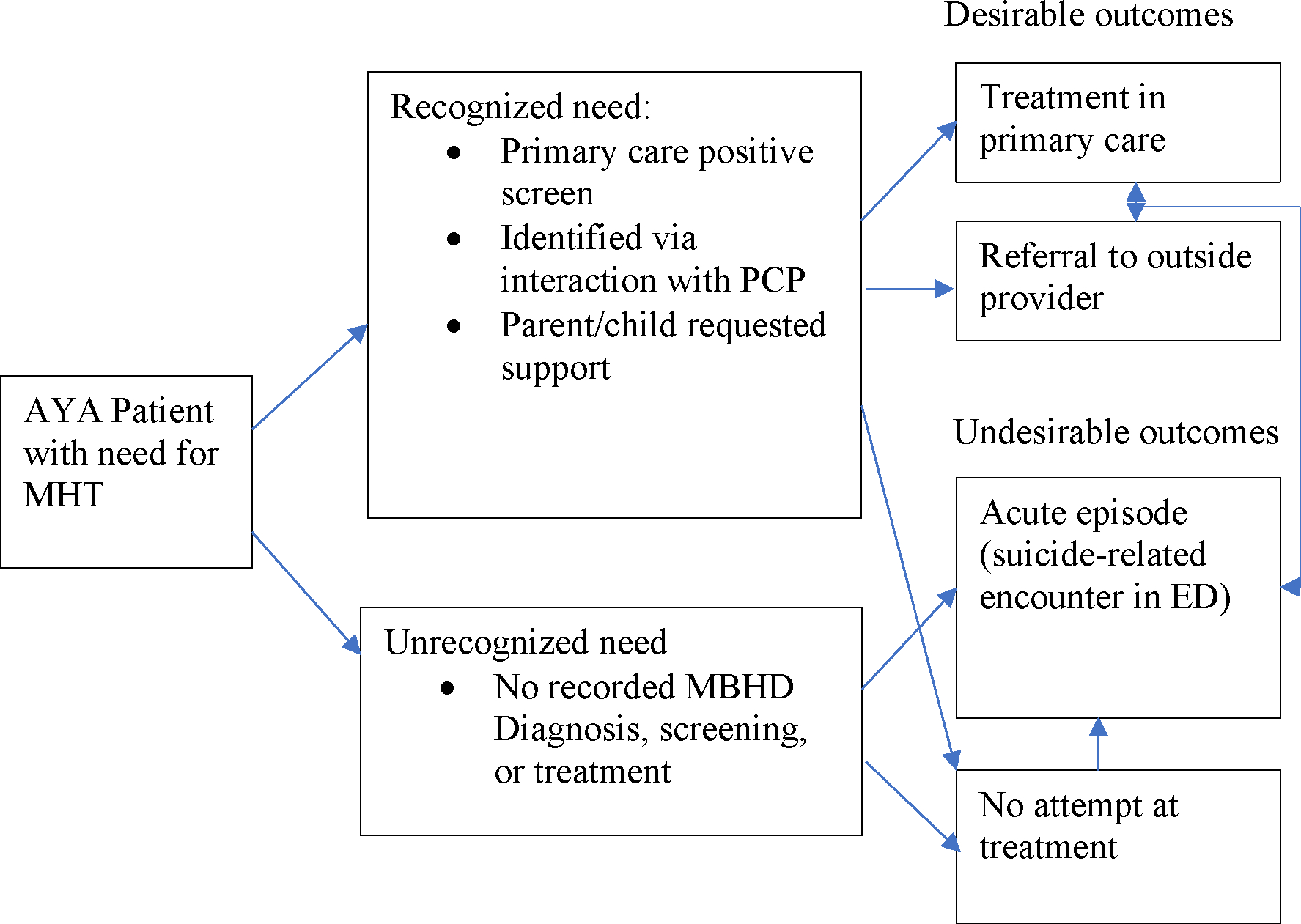
Conceptual Framework for Recognized/Unrecognized Need for Mental Health Treatment (MHT) in Adolescents and Young Adults in Primary Care (AYA)
Methods
We conducted a retrospective cross-sectional study using outpatient encounter records from the Johns Hopkins Community Physicians (JHCP), a system that includes 40 locations providing ambulatory, general, and specialty care throughout Maryland. De-identified patient data was extracted from Epic, the EMR system used by JHCP since 2013. The institutional review boards of Johns Hopkins approved this study as minimal risk and waived the requirement for informed consent.
The study cohort included patients from JHCP pediatric and family practices, ages 8–20 years old, who had at least two years between a first recorded encounter and a last recorded encounter between 1/1/2013 and 12/31/2021. The outcomes of interest were “ever” having a diagnosis of anxiety, depression, suicide-related diagnosis and/or under-recognition of mental health diagnoses. We focus primarily on anxiety and depression, because these are two of the most common MBHD treated in primary care, both can be difficult for pediatricians to recognize and both have also been correlated with suicidality.4,7,20 Under-recognition of mental health diagnoses was defined as positive if a patient had a suicide-related diagnosis recorded, but no diagnosis of any MBHD in the medical record predating the suicide-related diagnosis. In order to capture all suicide-related diagnoses, we used a broad classification of all suicide-related diagnoses, including suicidal ideation, suicide attempt and/or intentional self-harm.21 Any MBHD was defined as a composite of adjustment disorder, anxiety disorder, bipolar disorder, disruptive behavior disorder, mood disorder/depression, impulse control disorder, personality disorder and schizophrenia. Outcomes were defined as having an ICD-10 code listed as encounter diagnosis, problem list entry, or referral for outside care and were classified using the Clinical Classifications Software Refined for ICD-10-CM Diagnoses22 (Supplemental Table 1).
In order to isolate the intersection between race and gender, we generated a four-level composite gender and race variable, coded as 1) White male, 2) White female, 3) Black male, 4) Black female with White males as the reference group. This allows us to look at race and gender concurrently as each subgroup compares to the non-minoritized subgroup (White males). Because we were interested in the impact of minoritized identities (and intersectional minoritized identities – e.g., Black females), White males were used as the reference group as they would be the least likely to experience structural racism and sexism in relation to health care and the stressors of being in a minoritized group that may negatively impact mental health. Gender was defined using the “sex” variable in the Epic demographic module, which represented legal sex of the patient as reported by the parent or caregiver upon registration with the health system. More specific information about gender identity was not collected within the JHCP Epic system until 2019. Race was defined using the first chosen race category for the child by parent or caregiver upon registration with the health system. Elixhauser score was calculated using encounter diagnosis codes, and was used as a measure of underlying comorbidities.23 Insurance was classified based on insurance at first recorded encounter and was categorized as public, private, or other (self-pay, none). Years between first and last encounter in the data was used as a proxy for time at risk of having one of the outcomes of interest and was calculated using the first and last encounter each patient had during the study period. Number of encounters during the study period was included to account for additional differences in utilization.
We employed a series of mixed multilevel logistic regression models to determine the odds of the MBHD outcomes (anxiety, depression, suicide-related diagnosis) and under-recognition of mental health diagnoses. We examined the odds of the various outcomes, focusing on patients identifying as either White or Black and either male or female. The predictor variables of interest were gender, race and the composite gender and race variable. Multivariable models included age, insurance type, total number of encounters during the study period, and Elixhauser comorbidity score as covariates. Given the potential clustering of patient outcomes and demographic characteristics within practices, individual JHCP practices were analyzed as a nested level within the model. All analyses were conducted using Stata software, version 17.0.24
Results
The study consisted of 29,176 patients, with a mean age of 11.5 years. Per the demographic data in the EMR, about half (51.6%) of patients were female, 48.4% were male and less than 1% were nonbinary or reported a different sex (excluded from this analysis). A third (33.2%) of the patients identified as Black and 51.6% of patients identified as White (Table 1). Other races were excluded from this analysis (15.2% of patients). As for the outcomes of interest, based on medical records, 22.3% of the study population had an anxiety diagnosis, 10.5% had a depression diagnosis, 7.3% had a suicide-related diagnosis. Using the proxy of suicide-related diagnosis with no prior diagnosis of any MBHD, 5.3% of patients had under-recognized need for mental health services.
Table 1:
Characteristics of the Study Sample (n=29,176)*
| Characteristic | Mean (SD) or n (%) |
|---|---|
| Age at first encounter, mean (SD) | 11.5 (3.0) |
| Gender | |
| Female | 15044 (51.6%) |
| Male | 14117 (48.4%) |
| Nonbinary | 11 (<1%) |
| Other or Unknown | 4 (<1%) |
| Race | |
| Black or African American | 9695 (33.2%) |
| White | 15060 (51.6%) |
| Asian | 1654 (5.7%) |
| Other or Unknown | 2767 (9.5%) |
| Ethnicity | |
| Hispanic or Latino | 2218 (7.6%) |
| Not Hispanic or Latino | 26206 (89.8%) |
| Unknown/Choose Not to Disclose | 752 (2.6%) |
| Insurance | |
| Public | 6116 (21.1%) |
| Private | 14621 (50.5%) |
| Other | 8217 (28.4%) |
| Elixhauser comorbidity score, mean (SD) | 0.7 (0.9) |
| Number of encounters during the study period, mean (SD) | 10.8 (7.4) |
| Years between first and last encounter, mean (SD) | 4.6 (1.8) |
| Anxiety | 6502 (22.3%) |
| Depression | 3072 (10.5%) |
| Suicide-Related Diagnosis | 2139 (7.3%) |
| Under-recognized need for MBHD services** | 1542 (5.3%) |
| Any MBHD (includes below and Anxiety & Depression) | 11631 (39.9%) |
| ADHD | 3908 (13.4%) |
| Behavioral Disorder | 4652 (16.0%) |
| Impulse Control Disorder | 98 (0.34%) |
| Personality Disorder | 50 (0.17%) |
| Schizophrenia | 63 (0.22%) |
| Combined Gender and Race Variable | N=24547 |
| White male | 7344 (29.7%) |
| White female | 7707 (31.2%) |
| Black male | 4613 (18.6%) |
| Black female | 5079 (20.5%) |
Study population: patients ages 8–20 with >2 years between first and last recorded JHCP encounter (1/1/15–12/31/21)
Under-recognition of mental health diagnoses proxy: this is calculated as positive (1) if a patient has a suicide-related diagnosis in the medical record, but there is no prior diagnosis of an MBHD in the medical record.
The analytical cohort consisted of 24,547 patients (excluding 4,629 patients not in the four gender/race categories of interest, Table 2). In the multilevel multivariable logistic regression analysis focusing on race alone, Black patients had 61% decreased odds of having recorded anxiety as compared to White patients (OR 0.39, 95% CI 0.35, 0.41), 35% decreased odds of recorded depression (OR 0.65, 95% CI 0.59, 0.72), 19% increased odds of suicide-related diagnosis (OR 1.19, 95% CI 1.06, 1.32), and 40% increased odds of under-recognition of mental health disorder (OR 1.23, 95% CI 1.23, 1.58). Focusing on gender alone, female patients had 76% increased odds of having recorded anxiety as compared to males (OR 1.76, 95% CI 1.64, 1.88), 73% increased odds of recorded depression (OR 1.73, 95% CI 1.58, 1.90), 26% increased odds of suicide-related diagnosis (OR 1.2, 95% CI 1.13, 1.38) and 31% increased odds of under-recognition of mental health disorder (OR 1.31, 95% CI 1.16, 1.47).
Table 2:
Adjusted* Odds Ratio of Ever Diagnosis of MBHD by Race and Gender (n=24,547)
| N | Anxiety | Depression | Suicide-Related Diagnosis | Under-recognition of need for services | |
|---|---|---|---|---|---|
| Race | |||||
| White | 15060 | Reference | |||
| Black | 9695 | 0.39 (0.35, 0.41) | 0.65 (0.59, 0.72) | 1.19 (1.06, 1.32) | 1.40 (1.23, 1.58) |
| Gender | |||||
| Male | 14117 | Reference | |||
| Female | 15044 | 1.76 (1.64, 1.88) | 1.73 (1.58, 1.90) | 1.26 (1.13, 1.38) | 1.31 (1.16, 1.47) |
| Males Only | |||||
| White | 7344 | Reference | |||
| Black | 4613 | 0.37 (0.33, 0.42) | 0.68 (0.58, 0.80) | 1.11 (0.94, 1.32) | 1.20 (.99, 1.46) |
| Females Only | |||||
| White | 7707 | Reference | |||
| Black | 5079 | 0.38 (0.34, 0.42) | 0.64 (0.56, 0.73) | 1.26 (1.09, 1.45) | 1.57 (1.34, 1.85) |
| White Patients Only | |||||
| Male | 7344 | Reference | |||
| Female | 7707 | 1.74 (1.61, 1.89) | 1.81 (1.61, 2.04) | 1.18 (1.04, 1.35) | 1.17 (1.00, 1.37) |
| Black Patients Only | |||||
| Male | 4613 | Reference | |||
| Female | 5079 | 1.80 (1.58, 2.05) | 1.62 (1.38, 1.90) | 1.36 (1.17, 1.59) | 1.50 (1.26, 1.78) |
| Composite Race & Gender | |||||
| White Male | 7344 | Reference | |||
| White Female | 7707 | 1.75 (1.62, 1.89) | 1.81 (1.62, 2.04) | 1.17 (1.03, 1.34) | 1.15 (0.98, 1.34) |
| Black Male | 4613 | 0.38 (0.33, 0.42) | 0.72 (0.61, 0.84) | 1.09 (0.93, 1.28) | 1.18 (0.98, 1.42) |
| Black Female | 5079 | 0.67 (0.60, 0.74) | 1.13 (0.98, 1.30) | 1.48 (1.28, 1.71) | 1.80 (1.53, 2.13) |
Multivariable multilevel mixed logistic regression adjusted for age, insurance, number of encounters during the study period, years between first and last encounter in the data and Elixhauser score; practice is nested level
Under-recognition of mental health diagnoses proxy: this is calculated as positive (1) if a patient has a suicide-related diagnosis in the medical record, but there is no prior diagnosis of an MBHD in the medical record
Under-recognition of mental health diagnoses proxy: this is calculated as positive (1) if a patient has a suicide-related diagnosis in the medical record, but there is no prior diagnosis of an MBHD in the medical record
In the multilevel multivariable logistic regression analysis using the race and gender composite variable with White males as the reference group, White females had 75% increased odds of having recorded anxiety (OR 1.75, 95% CI 1.62, 1.89), Black males had 62% decreased odds of having recorded anxiety (OR 0.38, 95% CI 0.33, 0.43), and Black females had 33% decreased odds of having recorded anxiety (OR 0.67, 95% CI 0.60, 0.74). White females had 81% increased odds of having recorded depression (OR 1.81, 95% CI 1.62, 2.04). Black males had 28% decreased odds of having recorded depression (OR 0.72, 95% CI 0.61, 0.84), and Black females did not have a statistically significant increased odds of recorded depression as compared to White males.
Compared to White males, White females had 17% increased odds of having a recorded suicide-related diagnosis (OR 1.17, 95% CI 1.03, 1.34) and Black females had 48% increased odds of having recorded suicide-related diagnosis (OR 1.48, 95% CI 1.28, 1.71, Table 2), Black males did not have a statistically significant increased odds of having recorded suicide-related diagnosis as compared to White males. For the outcome of under-recognition of need for mental health services, White females and Black males did not differ significantly from White males, but Black females had 80% increased odds of under-recognition of need for MBHD services (OR 1.80, 95% CI 1.53, 2.13).
Discussion
The data from this large system of primary care practice support previous findings that Black AYA patients are disproportionately experiencing under-recognition of mental health problems.4. Black AYA patients are less likely to have a recorded diagnosis of anxiety or depression, and Black females are more likely to have unrecognized mental health needs, while having similar odds of suicide-related diagnoses. Females have higher odds of recorded anxiety, depression and suicide-related diagnosis as compared to males. Females, especially Black females, have disproportionately high odds of under-recognized need, which supports previous findings.25,26
There is solid consensus that the mental health crisis is impacting all AYA, regardless of race or gender.27 Combining race and gender was a way to illuminate some of the specific disparities associated with intersectional identities in mental health services access and utilization and under-recognition of need for services.8,28 White males were used as the reference group because of historical advantages resulting from structural racism and sexism, both removing some natural stressors from the mental health of this group and allowing this group better access to mental health services.29
This study has some limitations, there is inherent ascertainment bias when using EMR data to assess prevalence of disease. If a patient does not report mental health problems, this may represent actual lack of need for services, but it may just as well indicate that the patient was unwilling to discuss or disclose needs to their primary care provider. In this case, our results would likely underestimate under-recognition of need for mental health services and related disparities. It is also possible that some providers or practices are better equipped for mental health screening than others, which could add to observed disparities. As this study is using only Epic data from one health system, it is also possible that we are missing data on patients who sought mental health services from outside providers or patients who had an undocumented incidence of suicidal ideation, suicide attempt and/or intentional self-harm. However, integration of data through the Health Information Exchange in Maryland has increased the likelihood of capturing these diagnoses in our study.
Another limitation inherent in clinical EMR data is that we cannot have a complete sense of time a patient is at risk for exposure to any given outcome, though we do use a proxy in this analysis of years between first encounter during the study period until the last encounter in the study period. Finally, insurance type of the first encounter during the study period was our only measure of socioeconomic status (SES) (noting the limitation that insurance type may have changed over the study period) to use as control variables in our model. We would note, however, that we are interested in the interplay between race and SES as they impact mental health services utilization, as opposed to one or the other.
Predicting suicidal behavior using clinical data has proven extremely difficult for researchers, and studies have consistently found low positive predictive values of risk assessment tools, possibly due to the nature of many suicide episodes as impulsive acts resulting from precipitating crises.30 It should be noted that our measure of under-recognition of mental health diagnoses is a proxy for unrecognized need for mental health services in primary care rather than a validated metric of unmet need. We seek to use the proxy measure in this work to highlight racial and gender disparities in one important evidence-based strategy for suicide prevention, recognition of need for mental health care and initiation of mental health treatment.17,18,30 Future studies should seek to use validated measures of unmet mental health care need, or create new validated measures when possible.
This study differs from previous work focused on suicidality and health services utilization in a few important ways. First, as mentioned above, previous work has focused on predicting suicide risk using diagnoses and health services utilization patterns of patients with suicide attempt or death by suicide.18,19 In this study, we are more interested in describing who is not connecting with mental health care prior to a suicide-related encounter, as there may be actionable steps to better identify and engage these patients in preventive treatment. While primary care EMR data may not capture all interactions with mental health services, it important to know whether there may be missed opportunities for intervention at the primary care level, to provide the best possible screening and safety net for AYA patients at risk of suicide.
The accessibility of clinical data for research and quality improvement has increased tremendously in recent years, and it is critical for health systems to make the most of available patient data to identify disparities in access and treatment as well as patients at risk for negative outcomes. This study provides one step in the roadmap to best practices using EMR data for research, but much more work is needed in this area, both to improve the way the EMR collects and tracks patient data and how this data is utilized.
Future work should explore utilization dynamics for patients who identified as Asian, Hispanic ethnicity or as more than one race in the EMR, as there may be important differences and this study was limited to the first selected race in the patient’s record. Finally, we would emphasize that Black and White AYA patients were specified in this work due to the association between race and complex sociocultural constructs that may impact health care utilization and access, as opposed to any presumed biological mechanism for the outcomes we explored.
Despite policies and programs targeted at reducing disparities in mental health care access and utilization, this study supports previous research that gaps in care persist.31 Qualitative studies have found that AYA from minoritized racial groups displaying symptoms of mental health problems are more likely to receive punishment in school or be incarcerated than they are to receive mental health services.6 Youth suicide prevention programs may be most effective if implemented in multiple different settings, most importantly in schools, where universal screening may reduce disparities in identifying patients in need of care.32 Our findings support this idea and point to the need for precision gender- and race- tailored interventions to close gaps in access and utilization. Innovative programs to reduce disparities in mental health services will require continued unpacking of the historical, sociocultural, economic and structural factors that create barriers to accessing needed services for Black females and males.
Supplementary Material
Implications and Contribution.
This research found racial and gender disparities in the under-recognition of mental health disorders among adolescents and young adults (AYA) in a primary care setting. In particular, Black AYA female patients are 80% more likely to have under-recognized need for mental health services than White AYA male patients.
Funding:
This work was supported by the National Institute of Health /BIRCWH Grant mechanism (Dr. Prichett, K12AR084229), the Stanley Medical Research Institute (grant #7R-1690) and the National Institute of Drug Abuse (Dr. Young, K23 DA044288). This work was also supported by Johns Hopkins Biostatistics, Epidemiology and Data Management (BEAD) Core (internal funding); Dr. Young has received research support from NIH, the Brain and Behavior Research Foundation, Supernus Pharmaceuticals and Psychnostics, LLC. She has served as a consultant to NIH, PCORI and the Montana State University’s American Indian/Alaska Native Clinical & Translational Research Program, on the Board of Directors for Helping Give Away Psychological Science and on the editorial boards for the Journal of Clinical Child and Adolescent Psychology and Evidence-Based Practice in Child and Adolescent Mental Health. All other authors certify that they have no affiliations with or involvement in any organization or entity with a financial or non-financial interest in the subject matter or materials discussed in this manuscript. The findings and conclusions in this article are those of the authors and do not necessarily reflect the opinions of the National Institute of Health.
Abbreviations:
- AYA
Adolescents and young adults
- MBHD
Mental or behavioral health diagnosis
- EMR
Electronic Medical Record
- PCP
Primary care physician
- JHCP
Johns Hopkins Community Physicians
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Richmond LM. Surgeon General Calls for Action to Address Youth Mental Health Crisis. Psychiatr News. 2022;57(02):appi.pn.2022.2.11. doi: 10.1176/appi.pn.2022.2.11 [DOI] [Google Scholar]
- 2.AHR. America’s health rankings analysis of CDC Wonder, multiple cause of death files, United Health Foundation, available at: americashealthrankings.org, accessed 2022.
- 3.CDC. Centers for Disease Control and Prevention. 2019 Youth Risk Behavior Survey Questionnaire. Available at: www.cdc.gov/yrbs. Accessed on 5/4/23.
- 4.Wittchen HU, Mühlig S, Beesdo K. Mental disorders in primary care. Dialogues Clin Neurosci. 2003;5(2):115–128. doi: 10.31887/DCNS.2003.5.2/huwittchen [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saloner B, Carson N, Cook BL. Episodes of Mental Health Treatment Among a Nationally Representative Sample of Children and Adolescents. Med Care Res Rev. 2014;71(3):261–279. doi: 10.1177/1077558713518347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marrast L, Himmelstein DU, Woolhandler S. Racial and Ethnic Disparities in Mental Health Care for Children and Young Adults: A National Study. Int J Health Serv. 2016;46(4):810–824. doi: 10.1177/0020731416662736 [DOI] [PubMed] [Google Scholar]
- 7.Merikangas KR, He J ping, Burstein M, et al. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crenshaw K Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color. Stanford Law Rev. 1991;43(6):1241. doi: 10.2307/1229039 [DOI] [Google Scholar]
- 9.English D, Lambert SF, Tynes BM, Bowleg L, Zea MC, Howard LC. Daily multidimensional racial discrimination among Black U.S. American adolescents. J Appl Dev Psychol. 2020;66:101068. doi: 10.1016/j.appdev.2019.101068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shobeiri P, Kalantari A, Teixeira AL, Rezaei N. Shedding light on biological sex differences and microbiota–gut–brain axis: a comprehensive review of its roles in neuropsychiatric disorders. Biol Sex Differ. 2022;13(1):12. doi: 10.1186/s13293-022-00422-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhao Y, Leach LS, Walsh E, et al. COVID-19 and mental health in Australia – a scoping review. BMC Public Health. 2022;22(1):1200. doi: 10.1186/s12889-022-13527-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benton TD, Muhrer E, Jones JD, Lewis J. Dysregulation and Suicide in Children and Adolescents. Child Adolesc Psychiatr Clin N Am. 2021;30(2):389–399. doi: 10.1016/j.chc.2020.10.008 [DOI] [PubMed] [Google Scholar]
- 14.Mokkenstorm J, Franx G, Gilissen R, Kerkhof A, Smit JH. Suicide Prevention Guideline Implementation in Specialist Mental Healthcare Institutions in The Netherlands. Int J Environ Res Public Health. 2018;15(5):910. doi: 10.3390/ijerph15050910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trigylidas TE, Reynolds EM, Teshome G, Dykstra HK, Lichenstein R. Paediatric suicide in the USA: Analysis of the national child death case reporting system. Inj Prev. 2016;22(4):268–273. doi: 10.1136/injuryprev-2015-041796 [DOI] [PubMed] [Google Scholar]
- 16.Ali MM, Lackey S, Mutter R, McKeon R. The Relationship Between Perceived Unmet Mental Health Care Needs and Suicidal Ideation and Attempt. Adm Policy Ment Health Ment Health Serv Res. 2018;45(5):709–715. doi: 10.1007/s10488-018-0856-z [DOI] [PubMed] [Google Scholar]
- 17.Becerra MB, Becerra BJ, Hassija CM, Safdar N. Unmet Mental Healthcare Need and Suicidal Ideation Among U.S. Veterans. Am J Prev Med. 2016;51(1):90–94. doi: 10.1016/j.amepre.2016.01.015 [DOI] [PubMed] [Google Scholar]
- 18.Doupnik SK, Passarella M, Terwiesch C, Marcus SC. Mental Health Service Use Before and After a Suicidal Crisis Among Children and Adolescents in a United States National Medicaid Sample. Acad Pediatr. 2021;21(7):1171–1178. doi: 10.1016/j.acap.2021.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fontanella CA, Warner LA, Steelesmith D, Bridge JA, Sweeney HA, Campo JV. Clinical Profiles and Health Services Patterns of Medicaid-Enrolled Youths Who Died by Suicide. JAMA Pediatr. 2020;174(5):470. doi: 10.1001/jamapediatrics.2020.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spielvogle H, McCarty CA, Richardson LP. Brief Therapy for Anxiety and Depression in the Pediatric Primary Care Setting: Implications and Next Steps. JAMA Pediatr. 2017;171(10):1006. doi: 10.1001/jamapediatrics.2017.2854 [DOI] [PubMed] [Google Scholar]
- 21.Bommersbach TJ, McKean AJ, Olfson M, Rhee TG. National Trends in Mental Health–Related Emergency Department Visits Among Youth, 2011–2020. JAMA. 2023;329(17):1469. doi: 10.1001/jama.2023.4809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HCUP. The Clinical Classifications Software Refined (CCSR) for ICD-10-CM Diagnoses. Published 2023. Accessed January 6, 2023. https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/dxccsr.jsp
- 23.Menendez ME, Neuhaus V, van Dijk NC, Ring D. The Elixhauser Comorbidity Method Outperforms the Charlson Index in Predicting Inpatient Death After Orthopaedic Surgery. Clin Orthop. 2014;472(9):2878–2886. doi: 10.1007/s11999-014-3686-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.StataCorp. Stata Statistical Software: Release 17. Published online 2021. [Google Scholar]
- 25.Price JH, Khubchandani J. The Changing Characteristics of African-American Adolescent Suicides, 2001–2017. J Community Health. 2019;44(4):756–763. doi: 10.1007/s10900-019-00678-x [DOI] [PubMed] [Google Scholar]
- 26.Ketchen Lipson S, Gaddis SM, Heinze J, Beck K, Eisenberg D. Variations in Student Mental Health and Treatment Utilization Across US Colleges and Universities. J Am Coll Health. 2015;63(6):388–396. doi: 10.1080/07448481.2015.1040411 [DOI] [PubMed] [Google Scholar]
- 27.Hoffmann JA, Alegría M, Alvarez K, et al. Disparities in Pediatric Mental and Behavioral Health Conditions. Pediatrics. 2022;150(4):e2022058227. doi: 10.1542/peds.2022-058227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cho S, Crenshaw KW, McCall L. Toward a Field of Intersectionality Studies: Theory, Applications, and Praxis. Signs J Women Cult Soc. 2013;38(4):785–810. doi: 10.1086/669608 [DOI] [Google Scholar]
- 29.Thomeer MB, Moody MD, Yahirun J. Racial and Ethnic Disparities in Mental Health and Mental Health Care During The COVID-19 Pandemic. J Racial Ethn Health Disparities. Published online March 22, 2022. doi: 10.1007/s40615-022-01284-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Large MM. The role of prediction in suicide prevention. Dialogues Clin Neurosci. 2018;20(3):197–205. doi: 10.31887/DCNS.2018.20.3/mlarge [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rodgers CRR, Flores MW, Bassey O, Augenblick JM, Cook BL. Racial/Ethnic Disparity Trends in Children’s Mental Health Care Access and Expenditures From 2010–2017: Disparities Remain Despite Sweeping Policy Reform. J Am Acad Child Adolesc Psychiatry. 2022;61(7):915–925. doi: 10.1016/j.jaac.2021.09.420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ayer L, Colpe LJ. The Key Role of Schools in Youth Suicide Prevention. J Am Acad Child Adolesc Psychiatry. 2023;62(1):19–21. doi: 10.1016/j.jaac.2022.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


