Abstract
Objectives:
This study aimed to investigate the impact of air pollution on birth outcomes in the US over several decades.
Study design:
Approximately 70 million birth records were assessed for the years 1980 to 2020. This study focussed on seven measures of birth outcomes, including birth weight, low birth weight, very low birth weight, full-term birth weight, foetal growth, gestational age and very premature birth.
Methods:
An instrumental variable identification strategy was used that exploited within county-month and within month-year of birth variations in exposure to precipitation-induced changes in air pollution.
Results:
Air pollution was found to have negative and large effects on a wide range of birth outcomes. The study findings suggest that a one-standard-deviation increase in ozone was associated with a 6.4% and 12.8% increase (from the mean) in the proportion of low birth weight and very preterm birth infants, respectively. Further analyses suggest that these effects were heterogeneous across trimesters of pregnancy and reveal larger impacts during the second and third trimesters.
Conclusions:
The results suggest that the ordinary least square estimates of previous studies considerably underestimate the true effects of pollution on birth outcomes. Policies that aim to improve the health capital of future generations should allocate more resources and initiatives to improving environmental air quality.
Keywords: Air Pollution, Birth Outcomes, Infant Health, Precipitation
Introduction
It is well documented that the period of prenatal development is a critical period for infants’ health outcomes. (1–4) The primary hypothesis is the influence of external stressors on foetal development and the subsequent changes in epigenetic programming that result in deteriorations in physiological growth. (2,5) A strand of this literature evaluates the detrimental effects of air pollution on infants’ health outcomes. (6–8) Based on the foetal origin hypothesis, pollution operates as an environmental trigger and sends a signal to the reproductive system of the mother. This information changes the epigenetic codes and causes a process called methylation, in which some methyl molecules are attached to specific parts of DNA and silence-off some growth-related genes. The main purpose of this gene regulation is to increase the chances of survival. However, this change in epigenetic programming results in reduced tissue growth and degenerated organ development, and can be detected in poorer initial health measurements at birth, including lower birth weight (6) and lower gestational age. (9–11) Indeed, several studies have shown that prenatal exposure to pollution is associated with negative health outcomes for infants. (12,13) The current study joins this literature by providing evidence of the effects of air pollution on birth outcomes using a large study population observed over the years 1980–2020.
The contribution of the current study to the ongoing research on the negative health effects of air pollution is two-fold. In contrast to many studies that employed ordinary least square (OLS) strategies (14) and worked with cross-sectional estimates, (15) this study used a new method to exploit the exogenous within county-month variations in air pollution. Second, previous research frequently focussed on a specific geographic area or a limited time period; (3,16–18) however, the current study used birth data from many counties across US states and over 41 years (1980–2020). This more comprehensive data allowed a wider variation in air pollution levels and also made the estimates more representative of the US population.
Methods
Data
The primary source of data was county-identified restricted-access vital statistics birth records extracted from the National Center for Health Statistics (NCHS) for the years 1980–2020. The data covered all birth records in the US and provided information on several birth outcomes as well as limited information on parental characteristics. Each birth record included data on gender, birth weight, gestational age, Apgar score and year-month of birth. The data also contained the mother’s race, ethnicity, age, smoking status, education and marital status, and there was limited information about the father, including age and race.
This study restricted the sample to mothers aged 15–45 years old, since births out of this age range are uncommon, and their outcomes may have been strongly driven by age-related factors. Finally, the sample was restricted to the years 1980–2020 since both birth data and air pollution data are more comprehensive for the years post-1980.
Air pollution data were retrieved from daily pollution reports of the Environmental Protection Agency (EPA). The data were monitor-based and reported various pollutant measures on a daily basis. This study focussed on two important and widely reported measures, as follows: (1) ozone; and (2) PM10 (particulate matter <10 μm). Pollution data were restricted to counties that reported these pollutants every month of the year and did so for all months in a given year, which resulted in a subset of 1270 counties (see appendix A in the supplementary material for a list of the counties included in the final sample). Figure 1 shows the geographic distribution of these counties across the US.
Figure 1 -.
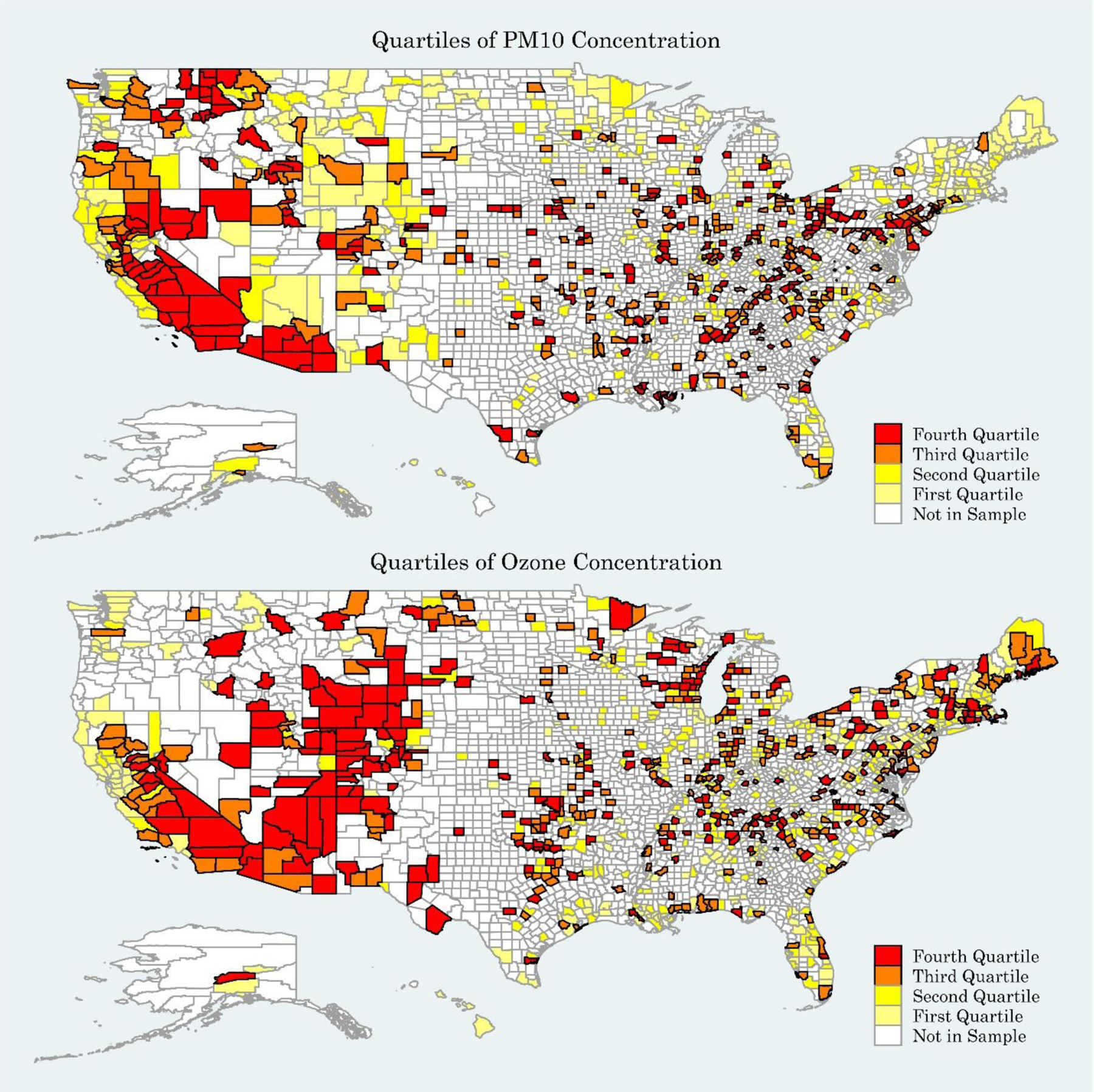
Geographic Distribution of Pollution Measures across US Counties
County-level temperature, humidity and precipitation data were also extracted from the Global Surface Summary of the Day data files provided by the National Oceanic and Atmospheric Administration (NOAA). The NOAA dataset reported the exact location of each station. The longitude and latitude of the county centroid was used in order to map stations across counties. Figure 2 illustrates the statistical distribution of ozone and PM10 concentration through a series of boxplots.
Figure 2 -.
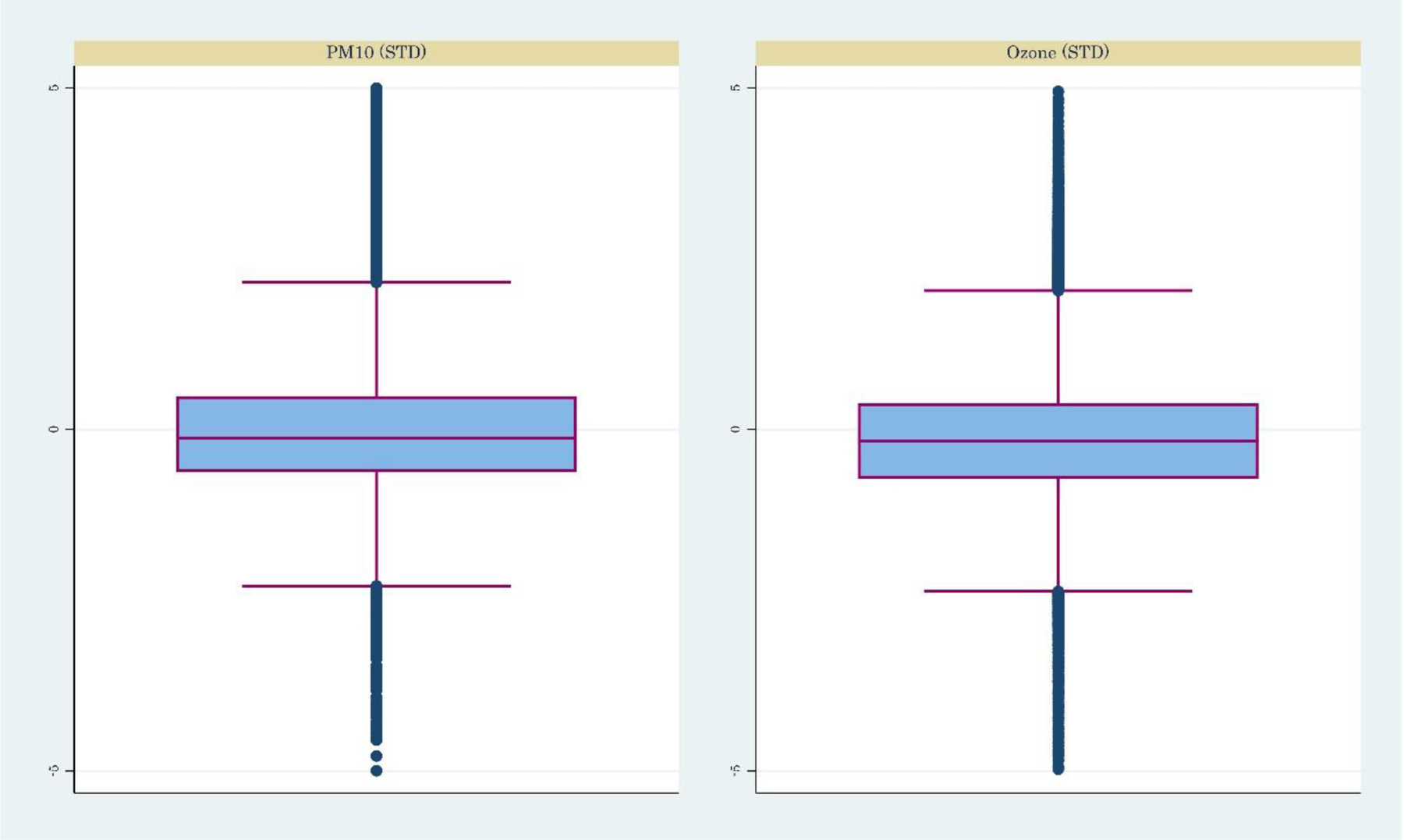
Boxplots of Endogenous Variables
The final study sample was collapsed at the county-month-year-gender-race level. The number of pre-collapse individual observations was 69,936,360. Table 1 reports the summary statistics of the final sample. Approximately 7.2% of births were categorised as low birth weight (i.e., having a birth weight <2500 grams). The average gestational age was 38.8 weeks. The average prenatal exposure to PM10 was 22.9 micrograms per cubic metre (μg/m3). The average ozone exposure was 28.6 μg/m3. To enable easy interpretation of the results, the pollution measures and atmospheric measures were standardised.
Table 1 -.
Summary Statistics
| Variable | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|
| Average Infants’ Characteristics: | ||||
| Birth Weight (in grams) | 3292.851 | 318.895 | 227 | 7777 |
| Low Birth Weight | .07 | .136 | 0 | 1 |
| Very Low Birth Weight | .012 | .058 | 0 | 1 |
| Full-Term Birth Weight (grams) | 3376.137 | 271.733 | 804 | 7777 |
| Foetal Growth (grams/week) | 84.829 | 7.395 | 9.08 | 210.189 |
| Gestational Age (weeks) | 38.792 | 1.381 | 17 | 47 |
| Very Premature Birth | .007 | .043 | 0 | 1 |
| Birth Counts | 45.952 | 152.467 | 1.007 | 8120.813 |
| Average Parental Characteristics: | ||||
| Age of Mother (years) | 26.127 | 3.348 | 11 | 51 |
| Mother Race: Black | .238 | .398 | 0 | 1 |
| Mother Hispanic | .027 | .096 | 0 | 1 |
| Mother Race: Other | .104 | .272 | 0 | 1 |
| Father Race: White | .574 | .402 | 0 | 1 |
| Father Race: Black | .132 | .253 | 0 | 1 |
| Father Hispanic | .023 | .083 | 0 | 1 |
| Mother’s Education Missing | .048 | .199 | 0 | 1 |
| Mother’s Education< High School | .024 | .085 | 0 | 1 |
| Mother’s Education=High School | .502 | .296 | 0 | 1 |
| Mother’s Education Some College | .242 | .232 | 0 | 1 |
| Mother’s Education Bachelor | .116 | .169 | 0 | 1 |
| Mother’s Education Master-PHD | .068 | .129 | 0 | 1 |
| Mother Cigar/Tobacco Smoker | .143 | .204 | 0 | 1 |
| Any Prenatal Visits | .964 | .106 | 0 | 1 |
| Father’s Age <30 years | .207 | .214 | 0 | 1 |
| Exposure Measures: | ||||
| PM10 (μg/m3) | 22.931 | 7.995 | −100.547 | 174.626 |
| Standardized PM10 | 0 | 1 | −15.444 | 18.973 |
| Ozone (μg/m3) | 28.55 | 6.996 | −116.617 | 137.543 |
| Standardised Ozone | 0 | 1 | −20.75 | 15.579 |
| Precipitation (inch) | 6.445 | 6.226 | −148.467 | 468.571 |
| Standardised Precipitation | 0 | 1 | −24.88 | 74.221 |
| Observations | 535,036 | |||
| No. of Pre-Collapse Observations | 69,936,360 | |||
In further analyses, this study also used county-level sociodemographic data from several sources. Data on population composition came from the Surveillance, Epidemiology and End Results (SEER) programme.(19) Income data were extracted from the Bureau of Economic Analysis. Average industry wage and industry-specific employment data came from the Quarterly Census of Employment and Wages.
Statistical Methods
The econometric method used in this study compares birth outcomes of mothers in county-months that were exposed to higher/lower levels of air pollution due to inter-countymonth variations in precipitation. Specifically, the study employed the following two-stage leastsquare estimations (equations 1 and 2):1,2
| (1) |
| (2) |
The data were aggregated into county (c), month (m), year (t), child’s race (White/non-White, r) and child’s gender (male/female, g). In this formulation, P was standardised pollution measure (ozone and PM10). In equation 1, the parameter PRCP represents standardised values of precipitation. It is important to note that the exposure measures (pollution and precipitation) were the average of these variables in the county of residence of the mother during the period of pregnancy. For instance, for a mother with 9 months of pregnancy, these measures are calculated as the 9-month average leading to the month of birth.
The parameter y represents the birth outcome of each child. This study focussed on the following seven outcomes: (1) birth weight - the child’s weight at birth, measured in grams; (2) low birth weight – this is a dummy that indicates whether the child’s birth weight was <2500 grams; (3) very low birth weight - this is a dummy that equals ‘1’ if the child’s birth weight was <1500 grams and ‘0’ otherwise; (4) full-term birth weight – this is the birth weight of infants who reach maturity in their prenatal period (i.e., birth weight of those with gestational age between 37 and 42 weeks); (5) foetal growth - this is the average weekly growth of infants during their gestational period (i.e., birth weight divided by gestational weeks);3 (6) gestational age – this is a clinical estimate of the period between the first day of a woman’s last menstrual period and the day of birth; (7) very premature birth - this is a dummy that equals ‘1’ if the gestational age was <28 weeks and ‘0’ otherwise.
To account for differences in birth outcomes among families of different sociodemographic backgrounds, a series of average cell-level parental controls in X and Z in the first stage and second stage, respectively, were included. These controls included mother’s race (Black, other race)4, mother’s ethnicity (Hispanic/Non-Hispanic), mother’s age, mother’s education (six categories: less than high school, high school, some college, bachelor degree, master-PhD degree, and missing information on education), mother having any prenatal visits, and father’s age (eleven categories: 15–20, 21–25, 26–30, 31–35, 36–40, 41–45, 46–50, 51–55, 56–60, 61–65, ≥66 years).
A relatively large strand of research suggests that temperature and humidity have direct impacts on birth outcomes. (20–22) These variables may coincide with precipitation and reveal seasonality patterns of changes. To account for these variations, average county-level temperature and humidity in W and V in first and second stage regressions, respectively, were included.
The matrix of fixed effects, represented by ζ and ξ in the first and second stage, included the child’s gender, race, county-by-month fixed effects and year-by-month fixed effects. The county-by-month fixed effects controlled for all seasonality in atmospheric variables and pollution that could alter the associations.5 This allowed the variation to come from precipitation-induced changes in pollution within a county-month. The year-by-month fixed effects accounted for all nonlinearities in birth outcomes across months and years.6 The set of county fixed effects (included in county-month fixed effects) absorbed all county-specific characteristics of local areas that do not vary over time. Standard errors were clustered at the county level to control for serial autocorrelation in the error terms.
Results
Precipitation and Air Pollution
To explore the relevance assumption and first-stage effects, this study used the same set of fixed effects as discussed above and regressed air pollution measures on precipitation measures. The results are reported in Table 2. Models that incorporated a stricter set of fixed effects and adjust for more covariates are presented in consecutive columns. The estimated effects suggest a strong and negative association between precipitation and air pollution. The magnitudes of the marginal effects are statistically and economically meaningful. For instance, a one-standard-deviation increase in precipitation was associated with 6.5% and 12.2% of a standard-deviation decrease in ozone and PM10, respectively. Overall, these results point to strong first stage effects and are in line with several studies that suggest an association between pollution and precipitation. (23–27)
Table 2 –
First-Stage Effects of Instruments on Pollution Outcomes
| Variable | Outcomes | |||||
|---|---|---|---|---|---|---|
| Ozone (STD) | PM10 (STD) | |||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Precipitation (STD) | −.06188*** | −.06034*** | −.06505*** | −.12671*** | −.12511*** | −.12176*** |
| (.01668) | (.01657) | (.0167) | (.02969) | (.03062) | (.02726) | |
| Observations | 535,036 | 535,036 | 535,036 | 392,419 | 392,417 | 392,417 |
| R-squared | .66233 | .69027 | .69406 | .78829 | .79629 | .8035 |
| County Fixed Effects | Yes | Yes | Yes | Yes | Yes | Yes |
| Year-Month Fixed Effects | Yes | Yes | Yes | Yes | Yes | Yes |
| County-by-Month Fixed Effects | No | Yes | Yes | No | Yes | Yes |
| County Controls | No | No | Yes | No | No | Yes |
Notes. Standard errors, clustered at the county level, are in parentheses. The regressions are weighted using the total number of births in each county.
p<0.01,
p<0.05,
p<0.1
STD, standard deviation.
Ordinary Least Square Results
The OLS association between air pollution and birth outcomes was investigated. The results for using ozone and PM10 as the explanatory variables are reported in Table 3. Some statistical association between air pollution and birth outcomes was observed; however, the effects were economically small. For instance, a one-standard-deviation increase in ozone and PM10 decreased birth weight by 1.1 and 1.6 grams, respectively. The marginal effects were small, but statistically significant.
Table 3 -.
The results of OLS Regressions of Pollution on Birth Outcomes
| Pollutant | Outcomes | ||||||
|---|---|---|---|---|---|---|---|
| Birth Weight | Low Birth Weight | Very Low Birth Weight | Full-Term Birth Weight | Foetal Growth | Gestational Weeks | Very Premature Birth | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Ozone | |||||||
| Ozone (STD) | −1.07985** | .00019 | .00006 | −.64488* | −.02318** | −.00222 | .00002 |
| (.47762) | (.00012) | (.00004) | (.38525) | (.00941) | (.00257) | (.00003) | |
| Observations | 798022 | 798022 | 798022 | 792308 | 798022 | 798022 | 798022 |
| R-squared | .71949 | .34556 | .14608 | .73643 | .71574 | .43423 | .11265 |
| Mean DV | 3311.207 | 0.064 | 0.012 | 3390.830 | 85.283 | 38.819 | 0.006 |
| %Change | −0.033 | 0.292 | 0.504 | −0.019 | −0.027 | −0.006 | 0.346 |
| PM 10 | |||||||
| PM10 (STD) | −1.60888* | .0008*** | .00013** | −.48865 | −.01324 | −.0134*** | .00013*** |
| (.88414) | (.00021) | (.00006) | (.76308) | (.01771) | (.00502) | (.00005) | |
| Observations | 545989 | 545989 | 545989 | 541805 | 545989 | 545989 | 545989 |
| R-squared | .74984 | .39671 | .1813 | .75999 | .74275 | .48556 | .14522 |
| Mean DV | 3312.907 | 0.064 | 0.012 | 3392.476 | 85.271 | 38.845 | 0.006 |
| %Change | −0.049 | 1.245 | 1.043 | −0.014 | −0.016 | −0.034 | 2.221 |
Notes. Standard errors, clustered at the county level, are in parentheses. The regressions include mother’s race dummy, child gender dummy, county-by-month fixed effects, and year-by-month fixed effects. The regressions also include average county-level parental controls including mother education (five categories), mother age, father race being White, father’s ethnicity, smoker mothers, father age (10 categories) and prenatal visits. All regressions contain controls for county-level temperature and humidity. The regressions are weighted using the total number of births in each cell.
p<0.01,
p<0.05,
p<0.1
Two-Stage Least-Square Instrumental-Variable Results
The results of the two-stage least-square estimations introduced in equations 1 and 2 are reported in Table 4 for ozone and PM10.7 The coefficient, standard error, R-squared, mean of the dependent variable and the implied percentage change (coefficient divided by the mean of the outcome) in subsequent rows are reported. The F-statistics (reported in the last row for each pollutant) are above conventional limits for weak instruments and rule out concerns of weak instrumental-variable estimates.
Table 4 -.
The Results of Two-Stage Least-Square Instrumental-Variable Regressions of Pollution on Birth Outcomes
| Pollutant | Outcomes | ||||||
|---|---|---|---|---|---|---|---|
| Birth Weight | Low Birth Weight | Very Low Birth Weight | Full-Term Birth Weight | Foetal Growth | Gestational Weeks | Very Premature Birth | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Ozone | |||||||
| Ozone (STD) | −20.09637*** | .00409** | .00114** | −14.57308*** | −.39178*** | −.06353* | .00077* |
| (6.31102) | (.00163) | (.00046) | (5.5523) | (.11123) | (.03577) | (.00041) | |
| Observations | 535,036 | 535,036 | 535,036 | 532,693 | 535,036 | 535,036 | 535,036 |
| R-squared | .08273 | .05176 | .0263 | .05317 | .06441 | .04515 | .02205 |
| Mean DV | 3309.772 | 0.064 | 0.012 | 3389.140 | 85.260 | 38.814 | 0.006 |
| %Change | −0.607 | 6.383 | 9.527 | −0.430 | −0.460 | −0.164 | 12.819 |
| F-Stat | 63.970 | 75.439 | 162.420 | 56.815 | 66.054 | 74.664 | 136.850 |
| PM 10 | |||||||
| PM10 (STD) | −19.49962*** | .00378** | .00129*** | −12.59806** | −.2778** | −.10734*** | .00129*** |
| (6.32009) | (.00159) | (.00046) | (5.74615) | (.11034) | (.03613) | (.00045) | |
| Observations | 392,417 | 392,417 | 392,417 | 390,266 | 392,417 | 392,417 | 392,417 |
| R-squared | .10884 | .06797 | .0328 | .07145 | .08856 | .04286 | .02577 |
| Mean DV | 3312.433 | 0.064 | 0.012 | 3391.491 | 85.278 | 38.837 | 0.006 |
| %Change | −0.589 | 5.911 | 10.721 | −0.371 | −0.326 | −0.276 | 21.568 |
| F-Stat | 64.941 | 65.865 | 158.921 | 52.106 | 60.370 | 64.321 | 124.001 |
Notes. Standard errors, clustered at the county level, are in parentheses. The regressions include mother’s race dummy, child gender dummy, county-bymonth fixed effects, and year-by-month fixed effects. The regressions also include average county-level parental controls including mother education (five categories), mother age, father race being White, father’s ethnicity, smoker mothers, father age (10 categories), and prenatal visits. All regressions contain controls for county-level temperature and humidity. The regressions are weighted using the total number of births in each cell.
p<0.01,
p<0.05,
p<0.1
The results show considerable reductions in birth weight and increases in low birth weight and very low birth weight. For instance, a one-standard-deviation rise in ozone and PM10 is associated with 20.1 and 19.5 grams lower birth weight, respectively (Table 4, column 1). The same increase in ozone and PM10 is associated with a 6.4% and 5.9% increase (from the mean) in the proportion of low birth weight infants, and a 9.5% and 10.7% increase in the proportion of infants with very low birth weight (Table 4, columns 2 and 3, respectively). These findings suggests that the adverse effects of air pollution are more pronounced for infants at the lower end of the birth weight distribution.
The effects of ozone and PM10 on full-term birth weight are smaller than the effects on overall birth weight (Table 4, column 4). The effects on foetal growth suggest a significant reduction of 0.27–0.39 grams/week for a one-standard-deviation rise in air pollution measures (Table 4, column 5). The effects on gestational weeks are larger than the OLS estimates presented in Table 3 and are statistically significant (Table 4, column 6). In addition, significant increases in very preterm births are seen (Table 4, column 7); a one-standard-deviation increase in ozone and PM10 is associated with a 12.8% and 21.6% increase in the proportion of very premature births, respectively.
These findings are considerably larger than the OLS estimates in Table 3, which suggests the endogeneity issues underestimate the relationships between air pollution and birth outcomes. Moreover, these findings are in line with several other studies. For instance, Currie et al.(3) employ data from New Jersey and include family fixed effects and find that a one-standard-deviation rise in ozone and PM10 during the last trimester of pregnancy is associated with 4.9 and 1.2 grams lower birth weight (compare with 19–20 grams in the current results). Palma et al.(28) use variation in rainfall shocks as an instrument for exogenous variation in air pollution and find that a one-standard-deviation rise in PM10 is associated with a 22% reduction in the prevalence of low birth weight (compare with 6% in the current study results [Table 4, column 2]).
To gain an understanding of the magnitude of the current findings, the implied effects can be compared with other results using studies that employ similar data over a similar period. For instance, Noghanibehambari and Salari(29) used the NCHS birth record data over the years 1990–2017 and showed that welfare payments under the Unemployment Insurance programme improve birth outcomes. Their estimates suggested that a $1000 increase in benefits is associated with an approximately 13.5 grams higher birth weight among likely affected women. Therefore, a $1000 increase in welfare spending can roughly be offset by a 0.7 standard-deviation rise in ozone or PM10. Hoynes et al.(30) explored the externality of tax rebates under Earned Income Tax Credit (EITC) programmes on infants’ health outcomes. These authors used NCHS birth data over the years 1983–1999 and found that a $1000 treatment-on-treated effect is associated with a roughly 2.2–2.9% reduction in low birth weight. Therefore, a one-standard-deviation reduction in ozone or PM10 is equivalent to about a $2000–2700 rise in the EITC welfare payments.
Robustness Checks
A series of robustness checks were implemented (see appendices in the supplementary material). In Appendix C, the effects of lagged values of air pollution were explored (i.e., the assignment of pollution in pre-prenatal development period). Small and mostly insignificant effects were found, suggesting that the effects are primarily concentrated to the in-utero period. Furthermore, in Appendix D, the robustness of the results is shown to the functional form and the nonlinearities in the effects is explored by replacing the pollution exposures and instruments with the logarithm of their respective values. The magnitudes of the effects are comparable to those of the main results. As an additional robustness check, controls for local and seasonal variations in incidences of wildfire were included into the current study regressions; the results are reported and discussed in Appendix H. The results were found to be comparable to the main findings. In Appendix J, it is shown that the results are not driven by selective fertility of mothers. Specifically, it is shown that the instrument is not correlated with a series of observable characteristics of mothers; hence, the study does not expect to find associations with unobservable features. (31)
Discussion
Quantifying the adverse effects of air pollution on health outcomes is important for policymakers in the areas of both health and the environment. The health impacts of pollution add to the costs associated with pollution and help policymakers in evaluating more refined solutions to reduce pollution. Evaluating the costs associated with pollution is important as the levels of pollution have steadily risen during the past decades and studies reveal no declining pattern. (32) The current study aimed add to the literature by quantifying the associations between air pollution and birth outcomes. These results suggest two important implications for public health policy and practice. First, the magnitude of effects is considerably large, which highlights the importance of implementing pollution abatement policies and enacting public health policies that target pregnant women and infants for both short- and long-term benefits. While the short-term benefits of such policies are observed through improvements in infants’ health at birth, the long-term benefits lie on the link between birth outcomes and outcomes across the life course, such as education, income, height and later-life mortality. (33–37) Second, as discussed further in Appendix B, greater effects were observed for infants of low educated mothers and those in low-income counties. In addition, several studies highlight the disparities in infants’ health based on maternal education and family socio-economic status. (38,39) Therefore, the results of the current study imply that public health and environmental policies that aim to reduce pollution have the potential to reduce health disparities and close the gap in infants’ health across different subpopulations.
The current study findings are in line with previous literature that suggests a negative association between air pollution and health outcomes. (15,40–42)8 However, these studies frequently focus on a limited geography (e.g., city, county, state), (43,44) a limited time period (40) and employ cross-sectional studies, which rely on the direct link between ecological measures and birth outcomes. (8,10,45,46) As discussed above, these direct links pick up on unobserved confounders and tend to underestimate the true effects. The instrumental variable approach used in the current study partly solved this issue and suggested considerably larger negative associations between pollution and birth outcomes.
The identification strategy design used in the current study exploited within county-month variations in air pollution measures that are caused by changes in precipitation. The findings suggest significant adverse impacts on birth outcomes. The effects are more pronounced for infants at the lower end of birth weight and gestational age distributions. Going from the least polluted county in our sample (Hancock, Main) to the most polluted county (Pinal, Arizona), the pollution measure of PM10 increases from 5.2 μg/m3 to 50.5 μg/m3, an increase of 5.9 standard deviations of PM10 over the study period. The results suggest that this increase in pollution is associated with 118 grams lower birth weight and a 37% higher proportion of low birth weight infants. A series of placebo tests show that the effects are specific to exposure during prenatal development. Finally, this study also showed that these effects were heterogeneous across pregnancy trimesters, with the largest effects observed in the second and third trimesters.
This study has several limitations that should be considered when interpreting the results. First, although an attempt was made to solve the endogeneity issues using precipitation-induced changes in pollution, this instrument could still be endogenously determined by pollution levels and other meteorological measures, such as temperature, which have direct effects on infants’ health outcomes. (7,17) Therefore, the observed effects reveal associations and caution should be taken when interpreting these links as a cause-and-effect relationship. Second, data availability limited the scope of this study to roughly 900 counties for which consistent pollution monitoring data were available. Relying on monitor-based measures of pollution is problematic for two reasons: (1) the locations are usually in urban areas, where there is a large enough population to warrant installation of the monitor; and (2) there is evidence that pollution monitoring is itself endogenous and agents avoid pollution hotspots, and this avoidance behaviour is more pronounced in low-income areas and counties with a higher percentage of Black individuals in the population. (47) Therefore, different results may have been observed if the study had access to pollution levels in all counties. Third, infants’ health, as the observed birth outcomes, was based on birth weight and gestational age. However, pollution, as documented in several studies, may result in foetal and neonatal death. (10,48) If more vulnerable infants did not survive due to in-utero exposure to pollution, then the observed associations do not reveal the full costs of pollution and underestimate the true effects. A more comprehensive analysis would use data that also includes foetal death and consider the mortality selection prior to birth in the model.
In conclusion, the results suggest that the ordinary least square estimates of previous studies considerably underestimate the true effects of pollution on birth outcomes. Policies that aim to improve the health capital of future generations should allocate more resources and initiatives to improving environmental air quality.
Supplementary Material
Funding
The authors would like to acknowledge financial support from the Center for Demography of Health and Aging (CDHA) at the University of Wisconsin-Madison under NIA core grant P30 AG17266.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing interests
The authors claim that they have no conflict of interest to report.
While in the paper, we focus on the whole pregnancy period exposure, in Appendix K, we explore the effects for exposures during different trimesters.
To satisfy the exclusion restriction assumption, the instrument requires to operate only through the endogenous variable and do not have a direct impact on the outcome. To validate this, we regress birth outcomes on precipitation while controlling for pollution, humidity, temperature, and a full set of fixed effects. The results, reported and discussed in Appendix I, fail to provide a direct link between precipitation and birth outcomes.
To satisfy the exclusion restriction assumption, the instrument requires to operate only through the endogenous variable and do not have a direct impact on the outcome. To validate this, we regress birth outcomes on precipitation while controlling for pollution, humidity, temperature, and a full set of fixed effects. The results, reported and discussed in Appendix I, fail to provide a direct link between precipitation and birth outcomes (35,63,64).
The reference group will be White.
In the sample analysis of PM10 and ozone, there are 891 and 965 counties, respectively. Interacting county fixed effects by month dummies, therefore, results in about 10,692 and 11,580 control variables in the regressions.
There are 29 years of data and 12 months. Therefore, year-by-month fixed effects adds 348 control variables to our regressions.
In Appendix G, we also examine the impacts of PM2.5 as the endogenous pollutant regressor and find effects that are considerably larger than those of PM10.
Although not directly tested, these studies suggest several mechanisms through which pollution affects birth outcomes. For instance, air pollutants such as PM10 and PM2.5 may induce inflammation and oxidative stress in mother’s body, resulting in placental dysfunction (65,66). Other channels include direct harm to the foetus, modifications in maternal heart or lung function, inflammation throughout the body due to oxidative stress, inflammation in the placenta, changes in gene expression in the placenta, adjustments in blood thickness, immune system disruption and epigenetic changes (67).
Availability of data and materials
The data and replication codes are available upon request.
References
- 1.Zong ZQ, Chen SW, Wu Y, Gui SY, Zhang XJ, Hu CY. Ambient air pollution exposure and telomere length: a systematic review and meta-analysis. Public Health. 2023. Feb 1;215:42–55. [DOI] [PubMed] [Google Scholar]
- 2.Almond D, Currie J. Killing Me Softly: The Fetal Origins Hypothesis. J Econ Perspect. 2011. Jun;25(3):153–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Currie J, Neidell M, Schmieder JF. Air pollution and infant health: Lessons from New Jersey. J Health Econ. 2009. May 1;28(3):688–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Currie J, Schwandt H. The 9/11 dust cloud and pregnancy outcomes: A reconsideration. J Hum Resour [Internet]. 2016. Jun;51(4):805–31. Available from: http://jhr.uwpress.org/content/51/4/805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barker DJP, Eriksson JG, Forsén T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol [Internet]. 2002. Dec;31(6):1235–9. Available from: https://academic.oup.com/ije/article/31/6/1235/939543 [DOI] [PubMed] [Google Scholar]
- 6.Schneider C, Schuele H, Baum CF, Landrigan PJ, Hawkins SS. Associations between prenatal exposure to power plants and birth outcomes across the United States. Public Health. 2023. Mar 1;216:30–2. [DOI] [PubMed] [Google Scholar]
- 7.Arroyo V, Díaz J, Carmona R, Ortiz C, Linares C. Impact of air pollution and temperature on adverse birth outcomes: Madrid, 2001–2009. Environ Pollut. 2016. Nov 1;218:1154–61. [DOI] [PubMed] [Google Scholar]
- 8.Franklin P, Tan M, Hemy N, Hall GL. Maternal Exposure to Indoor Air Pollution and Birth Outcomes. Int J Environ Res Public Heal 2019, Vol 16, Page 1364 [Internet]. 2019. Apr 16 [cited 2022 Apr 26];16(8):1364. Available from: https://www.mdpi.com/16604601/16/8/1364/htm [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altindag DT, Baek D, Mocan N. Chinese Yellow Dust and Korean infant health. Soc Sci Med. 2017. Aug 1;186:78–86. [DOI] [PubMed] [Google Scholar]
- 10.Inoue T, Nunokawa N, Kurisu D, Ogasawara K. Particulate air pollution, birth outcomes, and infant mortality: Evidence from Japan’s automobile emission control law of 1992. SSM - Popul Heal. 2020. Aug 1;11:100590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeCicca P, Malak N. When good fences aren’t enough: The impact of neighboring air pollution on infant health. J Environ Econ Manage. 2020. Jul 1;102:102324. [Google Scholar]
- 12.Luechinger S Air pollution and infant mortality: A natural experiment from power plant desulfurization. J Health Econ. 2014. Sep 1;37(1):219–31. [DOI] [PubMed] [Google Scholar]
- 13.Currie J, Schmieder JF. Fetal Exposures to Toxic Releases and Infant Health. Am Econ Rev [Internet]. 2009. May [cited 2022 May 8];99(2):177–83. Available from: http://www.aeaweb.org/articles.php?doi=10.1257/aer.99.2.177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salam MT, Millstein J, Li YF, Lurmann FW, Margolis HG, Gilliland FD. Birth Outcomes and Prenatal Exposure to Ozone, Carbon Monoxide, and Particulate Matter: Results from the Children’s Health Study. Environ Health Perspect [Internet]. 2005. Nov [cited 2022 Nov 10];113(11):1638–44. Available from: https://ehp.niehs.nih.gov/doi/10.1289/ehp.8111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shah PS, Balkhair T. Air pollution and birth outcomes: A systematic review. Environ Int. 2011. Feb 1;37(2):498–516. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez DJX, Sherris AR, Yang W, Stevenson DK, Padula AM, Baiocchi M, et al. Oil and gas production and spontaneous preterm birth in the San Joaquin Valley, CA: A case–control study. Environ Epidemiol [Internet]. 2020. [cited 2022 Apr 26];4(4). Available from: /pmc/articles/PMC7423522/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andalón M, Azevedo JP, Rodríguez-Castelán C, Sanfelice V, Valderrama-González D. Weather Shocks and Health at Birth in Colombia. World Dev. 2016. Jun 1;82:69–82. [Google Scholar]
- 18.Lee PC, Roberts JM, Catov JM, Talbott EO, Ritz B. First trimester exposure to ambient air pollution, pregnancy complications and adverse birth outcomes in Allegheny County, PA. Matern Child Health J [Internet]. 2013. Apr 28 [cited 2022 Apr 26];17(3):545–55. Available from: https://link.springer.com/article/10.1007/s10995-012-1028-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.SEER. Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) Research Data (1975–2016). Natl Cancer Institute, DCCPS, Surveill Res Progr. 2019; [Google Scholar]
- 20.Basagaña X, Michael Y, Lensky IM, Rubin L, Grotto I, Vadislavsky E, et al. Low and High Ambient Temperatures during Pregnancy and Birth Weight among 624,940 Singleton Term Births in Israel (2010–2014): An Investigation of Potential Windows of Susceptibility. Environ Health Perspect [Internet]. 2021. Oct 13 [cited 2022 Sep 27];129(10). Available from: https://ehp.niehs.nih.gov/doi/10.1289/EHP8117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grace K, Davenport F, Hanson H, Funk C, Shukla S. Linking climate change and health outcomes: Examining the relationship between temperature, precipitation and birth weight in Africa. Glob Environ Chang. 2015. Nov 1;35:125–37. [Google Scholar]
- 22.Hajdu T, Hajdu G. Temperature, climate change, and birth weight: evidence from Hungary. Popul Environ [Internet]. 2021. Dec 1 [cited 2022 Sep 27];43(2):131–48. Available from: https://link.springer.com/article/10.1007/s11111-021-00380-y [Google Scholar]
- 23.Aw J, Kleeman MJ. Evaluating the first-order effect of intraannual temperature variability on urban air pollution. J Geophys Res Atmos [Internet]. 2003. Jun 27 [cited 2022 Apr 29];108(D12):4365. Available from: https://onlinelibrary.wiley.com/doi/full/10.1029/2002JD002688 [Google Scholar]
- 24.Breitner S, Wolf K, Devlin RB, Diaz-Sanchez D, Peters A, Schneider A. Short-term effects of air temperature on mortality and effect modification by air pollution in three cities of Bavaria, Germany: A time-series analysis. Sci Total Environ. 2014. Jul 1;485–486(1):49–61. [DOI] [PubMed] [Google Scholar]
- 25.Buckley JP, Samet JM, Richardson DB. Does air pollution confound studies of temperature? Epidemiology [Internet]. 2014. Mar [cited 2022 Apr 29];25(2):242–5. Available from: https://journals.lww.com/epidem/Fulltext/2014/03000/Commentary__Does_Air_Pollution_Confound_Studies_of.14.aspx [DOI] [PubMed] [Google Scholar]
- 26.Wang J, Liu X, Dong M, Sun X, Xiao J, Zeng W, et al. Associations of maternal ambient temperature exposures during pregnancy with the placental weight, volume and PFR: A birth cohort study in Guangzhou, China. Environ Int. 2020. Jun 1;139:105682. [DOI] [PubMed] [Google Scholar]
- 27.Roberts S Interactions between particulate air pollution and temperature in air pollution mortality time series studies. Environ Res. 2004. Nov 1;96(3):328–37. [DOI] [PubMed] [Google Scholar]
- 28.Palma A, Petrunyk I, Vuri D. Prenatal air pollution exposure and neonatal health. Health Econ [Internet]. 2022. May 1 [cited 2022 Apr 26];31(5):729–59. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/hec.4474 [DOI] [PubMed] [Google Scholar]
- 29.Noghanibehambari H, Salari M. Health benefits of social insurance. Health Econ [Internet]. 2020. Dec;29(12):1813–22. Available from: https://onlinelibrary.wiley.com/doi/10.1002/hec.4170 [DOI] [PubMed] [Google Scholar]
- 30.Hoynes H, Miller D, Simon D. Income, the earned income tax credit, and infant health. Am Econ J Econ Policy. 2015;7(1):172–211. [Google Scholar]
- 31.Altonji JG, Elder TE, Taber CR. Selection on Observed and Unobserved Variables: Assessing the Effectiveness of Catholic Schools. J Polit Econ [Internet]. 2005. Jul 19 [cited 2021 Nov 15];113(1):151–84. Available from: https://www.journals.uchicago.edu/doi/abs/10.1086/426036 [Google Scholar]
- 32.Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N Engl J Med [Internet]. 2019. Aug 22 [cited 2022 Apr 29];381(8):705–15. Available from: https://www.nejm.org/doi/full/10.1056/NEJMoa1817364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Black SE, Devereux PJ, Salvanes KG. From the cradle to the labor market? The effect of birth weight on adult outcomes. Q J Econ [Internet]. 2007. Feb;122(1):409–39. Available from: https://academic.oup.com/qje/article-lookup/doi/10.1162/qjec.122.1.409 [Google Scholar]
- 34.Royer H Separated at girth: US twin estimates of the effects of birth weight. Am Econ J Appl Econ. 2009. Jun;1(1):49–85. [Google Scholar]
- 35.Behrman JR, Rosenzweig MR. Returns to birthweight. Vol. 86, Review of Economics and Statistics. 2004. p. 586–601. [Google Scholar]
- 36.Maruyama S, Heinesen E. Another look at returns to birthweight. J Health Econ. 2020. Mar;70:102269. [DOI] [PubMed] [Google Scholar]
- 37.Fletcher JM. The medium term schooling and health effects of low birth weight: Evidence from siblings. Econ Educ Rev. 2011. Jun;30(3):517–27. [Google Scholar]
- 38.Gage TB, Fang F, O’Neill E, DiRienzo G. Maternal Education, Birth Weight, and Infant Mortality in the United States. Demography [Internet]. 2013;50(2):615–35. Available from: https://pubmed.ncbi.nlm.nih.gov/23073749/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jackson MI, Rauscher E, Burns A. Social Spending and Educational Gaps in Infant Health in the United States, 1998–2017. Demography [Internet]. 2022. Oct 1 [cited 2023 Jun 30];59(5):1873–909. Available from: http://read.dukeupress.edu/demography/article-pdf/59/5/1873/1646360/1873jackson.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maisonet M, Correa A, Misra D, Jaakkola JJK. A review of the literature on the effects of ambient air pollution on fetal growth. Environ Res. 2004. May 1;95(1):106–15. [DOI] [PubMed] [Google Scholar]
- 41.Rappazzo KM, Nichols JL, Rice RB, Luben TJ. Ozone exposure during early pregnancy and preterm birth: A systematic review and meta-analysis. Environ Res. 2021. Jul 1;198:111317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lamichhane DK, Leem J-H, Lee J-Y, Kim H-C. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ Health Toxicol [Internet]. 2015. Nov 3 [cited 2023 Sep 3];30:e2015011. Available from: http://www.eaht.org/journal/view.php?doi=10.5620/eht.e2015011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilhelm M, Ritz B. Local Variations in CO and Particulate Air Pollution and Adverse Birth Outcomes in Los Angeles County, California, USA. Environ Health Perspect [Internet]. 2005. Sep [cited 2023 Sep 3];113(9):1212–21. Available from: https://ehp.niehs.nih.gov/doi/10.1289/ehp.7751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilhelm M, Ritz B. Residential proximity to traffic and adverse birth outcomes in Los Angeles county, California, 1994–1996. Environ Health Perspect [Internet]. 2003. Feb 1 [cited 2023 Sep 3];111(2):207–16. Available from: https://ehp.niehs.nih.gov/doi/10.1289/ehp.5688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xie X, Ding G, Cui C, Chen L, Gao Y, Zhou Y, et al. The effects of low-level prenatal lead exposure on birth outcomes. Environ Pollut. 2013. Apr 1;175:30–4. [DOI] [PubMed] [Google Scholar]
- 46.Stieb DM, Chen L, Eshoul M, Judek S. Ambient air pollution, birth weight and preterm birth: A systematic review and meta-analysis. Environ Res. 2012. Aug 1;117:100–11. [DOI] [PubMed] [Google Scholar]
- 47.Grainger C, Schreiber A. Discrimination in Ambient Air Pollution Monitoring? AEA Pap Proc. 2019. May 1;109:277–82. [Google Scholar]
- 48.Rammah A, Whitworth KW, Han I, Chan W, Symanski E. Time-Varying Exposure to Ozone and Risk of Stillbirth in a Nonattainment Urban Region. Am J Epidemiol [Internet]. 2019. Jul 1 [cited 2022 Nov 10];188(7):1288–95. Available from: https://academic.oup.com/aje/article/188/7/1288/5492683 [DOI] [PubMed] [Google Scholar]
- 49.Liang Z, Yang Y, Qian Z, Ruan Z, Chang J, Vaughn MG, et al. Ambient PM2.5 and birth outcomes: Estimating the association and attributable risk using a birth cohort study in nine Chinese cities. Environ Int. 2019. May 1;126:329–35. [DOI] [PubMed] [Google Scholar]
- 50.Lubczyńska MJ, Sunyer J, Tiemeier H, Porta D, Kasper-Sonnenberg M, Jaddoe VWV, et al. Exposure to elemental composition of outdoor PM2.5 at birth and cognitive and psychomotor function in childhood in four European birth cohorts. Environ Int. 2017. Dec 1;109:170–80. [DOI] [PubMed] [Google Scholar]
- 51.Evans J, Bansal A, Schoenaker DAJM, Cherbuin N, Peek MJ, Davis DL. Birth Outcomes, Health, and Health Care Needs of Childbearing Women following Wildfire Disasters: An Integrative, State-of-the-Science Review. Environ Health Perspect [Internet]. 2022. Aug [cited 2022 Sep 27];130(8). Available from: https://ehp.niehs.nih.gov/doi/10.1289/EHP10544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Heft-Neal S, Driscoll A, Yang W, Shaw G, Burke M. Associations between wildfire smoke exposure during pregnancy and risk of preterm birth in California. Environ Res. 2022. Jan 1;203:111872. [DOI] [PubMed] [Google Scholar]
- 53.Brown AP, Cai L, Laufer BI, Miller LA, LaSalle JM, Ji H. Long-term effects of wildfire smoke exposure during early life on the nasal epigenome in rhesus macaques. Environ Int. 2022. Jan 1;158:106993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Amjad S, Chojecki D, Osornio-Vargas A, Ospina MB. Wildfire exposure during pregnancy and the risk of adverse birth outcomes: A systematic review. Environ Int. 2021. Nov 1;156:106644. [DOI] [PubMed] [Google Scholar]
- 55.Rangel MA, Vogl TS. Agricultural Fires and Health at Birth. Rev Econ Stat [Internet]. 2019. Oct 1 [cited 2022 Apr 26];101(4):616–30. Available from: https://direct.mit.edu/rest/article/101/4/616/58569/Agricultural-Fires-and-Health-at-Birth [Google Scholar]
- 56.Strand LB, Barnett AG, Tong S. The influence of season and ambient temperature on birth outcomes: A review of the epidemiological literature. Vol. 111, Environmental Research. Academic Press; 2011. p. 451–62. [DOI] [PubMed] [Google Scholar]
- 57.Beine M, Jeusette L. A meta-analysis of the literature on climate change and migration. J Demogr Econ [Internet]. 2021. Sep 1 [cited 2022 Apr 29];87(3):293–344. Available from: https://www.cambridge.org/core/journals/journal-of-demographiceconomics/article/abs/metaanalysis-of-the-literature-on-climate-change-and-migration/D2CD417C7B639935326D67E42BDE6812 [Google Scholar]
- 58.Lavigne E, Yasseen AS, Stieb DM, Hystad P, van Donkelaar A, Martin RV., et al. Ambient air pollution and adverse birth outcomes: Differences by maternal comorbidities. Environ Res. 2016. Jul 1;148:457–66. [DOI] [PubMed] [Google Scholar]
- 59.Ross Z, Ito K, Johnson S, Yee M, Pezeshki G, Clougherty JE, et al. Spatial and temporal estimation of air pollutants in New York City: Exposure assignment for use in a birth outcomes study. Environ Heal A Glob Access Sci Source [Internet]. 2013. Jun 27 [cited 2022 Apr 29];12(1):1–13. Available from: https://ehjournal.biomedcentral.com/articles/10.1186/1476-069X-12-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eiríksdóttir VH, Ásgeirsdóttir TL, Bjarnadóttir RI, Kaestner R, Cnattingius S, Valdimarsdóttir UA. Low Birth Weight, Small for Gestational Age and Preterm Births before and after the Economic Collapse in Iceland: A Population Based Cohort Study. PLoS One [Internet]. 2013. Dec 4 [cited 2022 May 21];8(12):e80499. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Strauss RS. Adult functional outcome of those born small for gestational age: twenty-six--year follow-up of the 1970 British birth cohort. Jama. 2000;283(5):625–32. [DOI] [PubMed] [Google Scholar]
- 62.Pojda J, Kelley L. Low birthweight. 2000.
- 63.Malmqvist E, Liew Z, Källén K, Rignell-Hydbom A, Rittner R, Rylander L, et al. Fetal growth and air pollution - A study on ultrasound and birth measures. Environ Res. 2017. Jan 1;152:73–80. [DOI] [PubMed] [Google Scholar]
- 64.Ritz B, Qiu J, Lee PC, Lurmann F, Penfold B, Erin Weiss R, et al. Prenatal air pollution exposure and ultrasound measures of fetal growth in Los Angeles, California. Environ Res. 2014. Apr 1;130:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Welch BM, McNell EE, Edin ML, Ferguson KK. Inflammation and oxidative stress as mediators of the impacts of environmental exposures on human pregnancy: Evidence from oxylipins. Pharmacol Ther. 2022. Nov 1;239:108181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Badehnoosh B, Karamali M, Zarrati M, Jamilian M, Bahmani F, Tajabadi-Ebrahimi M, et al. The effects of probiotic supplementation on biomarkers of inflammation, oxidative stress and pregnancy outcomes in gestational diabetes. J Matern Neonatal Med [Internet]. 2017. May 3 [cited 2023 Sep 3];31(9):1128–36. Available from: https://www.tandfonline.com/doi/abs/10.1080/14767058.2017.1310193 [DOI] [PubMed] [Google Scholar]
- 67.Bekkar B, Pacheco S, Basu R, Basu R, Denicola N. Association of Air Pollution and Heat Exposure With Preterm Birth, Low Birth Weight, and Stillbirth in the US: A Systematic Review. JAMA Netw Open [Internet]. 2020. Jun 1 [cited 2023 Sep 3];3(6):e208243–e208243. Available from: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2767260 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data and replication codes are available upon request.


