Abstract
Background:
First-generation algorithms resulted in high-cost features as a representation of need but unintentionally introduced systemic bias based on prior ability to access care. Improved precision health approaches are needed to reduce bias and improve health equity.
Purpose:
To integrate nursing expertise into a clinical definition of high-need cases and develop a clinical classification algorithm for implementing nursing interventions.
Methods:
Two-phase retrospective, descriptive cohort study using 2019 data to build the algorithm (n = 19,20,848) and 2021 data to test it in adults ≥18 years old (n = 15,99,176).
Discussion:
The COMPLEXedex-SDH algorithm identified the following populations: cross-cohort needs (10.9%); high-need persons (cross-cohort needs and other social determinants) (17.7%); suboptimal health care utilization for persons with medical complexity (13.8%); high need persons with suboptimal health care utilization (6.2%).
Conclusion:
The COMPLEXedex-SDH enables the identification of high-need cases and value-based utilization into actionable cohorts to prioritize outreach calls to improve health equity and outcomes.
Keywords: Social determinants of health, Provider–provider communication, Care coordination, Social need
Introduction
Individuals who have significant medical, behavioral health, and/or social service needs, such as multiple or complex chronic health conditions, mental health or substance use disorder (SUD), and/or functional disabilities (Long et al., 2017), account for nearly 5% of the adult population over the age of 18, or roughly 12 million people, in the United States (Hayes et al., 2016). The health care system is often blind to social barriers influencing access to high-quality health care. These individuals, who have high social needs, require innovative and collaborative nursing interventions that connect service providers across the health care sectors, especially during care transitions. For example, persons with housing insecurity may simultaneously require care from the health, behavioral health, and social service sectors at the time of hospital discharge. Yet the fragmented continuum of care adds to their treatment burden (Eton et al., 2017) and jeopardizes the safety of people who already have compromised health. New approaches are needed for identifying individuals with high social and health needs for the deployment of targeted nursing interventions that positively influence health outcomes (Alderwick & Gottlieb, 2019; Samuels-Kalow et al., 2020).
A recent scoping review and gap analysis identified cross-sector collaboration (i.e., care received from two or more community-based service providers) as an impactful intervention to improve outcomes for individuals with high needs (Hewner et al., 2021). However, challenges remain in identifying those persons who have the greatest social need and developing technology that transmits critical information across health care sectors (Hewner et al., 2021). Our pilot work demonstrates that delivering care alerts through a Health Information Exchange (HIE) that triggered an outreach phone call and social need assessment by a Registered Nurse (RN) resulted in improved transitional care continuity and utilization value (with more outpatient [OP] visits and fewer hospitalizations). However, prioritizing the population receiving the interventions to those with the greatest social need and partnering with social service providers to optimize the HIE for shared care planning (Sullivan et al., 2017) requires further research focus and investigation to determine the most accurate need-based stratification techniques.
One approach to mitigating this issue is to use precision health techniques to predict patient needs and/or outcomes. Precision health enables the development of personalized nursing interventions for coordinating care across sectors (community-based service providers) for persons with medical complexity, chronic conditions, and social needs. Precision health, defined by the Council for the Advancement of Nursing Science, is “an emerging approach to individualizing health care [and] includes genomics and other physiological, psychological, environmental, and ethical factors that are central to the development and testing of individualized treatments and preventions strategies for persons, families, and communities” (Hacker et al., 2019, p. 287).
Although precision health has been used to understand patient complexity and utilization, more information is needed to define the characteristics of individuals with high needs to better identify those who would most benefit from cross-sector collaboration and shared care planning. First-generation precision health algorithms were developed from administrative claims data, resulting in the classification of high-cost features as a representation of need (Bates et al., 2014; Joynt et al., 2017). Time and experience have shown that these early approaches have unintentionally introduced systemic bias into clinical algorithms, such as predicting the need for care based on the prior ability to access care (Gervasi et al., 2022; Obermeyer et al., 2019). Thus, next-generation algorithms are urgently needed to improve precision health approaches, reduce bias, and improve health equity (Long et al., 2017; McCradden et al., 2020; Obermeyer et al., 2019; Rajkomar et al., 2018).
Next-generation precision health classification models should consider social determinants of health (SDH) along with current patterns of health care service use, such as the frequency and timing of accessing inpatient (IP), emergency department (ED), and OP services. Innovative and inclusive approaches can lead to targeted nursing interventions that are tailored to individuals with the most need, so they may optimize health care service access and achieve optimal health outcomes. Since social data collection using standardized screening tools is being mandated by the Centers for Medicare and Medicaid Services (CMS) for hospital quality metrics (CMS, n.d.), there are important implications for nursing. The purpose of this exploratory study was to (a) define the features of high-need cases that include the combination of health and social complexity (chronic conditions, SDH, and health care utilization patterns) and (b) develop an actionable clinical classification algorithm for implementing nursing interventions that are tailored to individuals with high needs.
Methods
This retrospective, descriptive cohort study, which included a data use agreement and protocol for deidentification, was approved by the Institutional Review Board at the State University of New York.
Theoretical Framework
The Cumulative Complexity Model (CCM) and the World Health Organization (WHO) definition of SDH underpin this study. The CCM operationalizes patient complexity to guide improvements and interventions for patients with multimorbidity and/or complex needs. Within the CCM, the balance between patient workload (e.g., job, family, and attending appointments) and capacity (e.g., symptoms, finances, and social support) exerts influence on an individual’s ability to attend to self-care activities and access the health care system, which ultimately influences their health outcomes (Shippee et al., 2012). According to the WHO, SDH are the systems and forces shaping the conditions in which people are born, live, work, and age that influence health outcomes (WHO, 2022). The SDH has an important effect on the risk of a person having unmet social needs and includes the complex interactions between individuals, relationships, communities, and societal factors (Centers for Disease Control and Prevention, 2021).
Population Dataset
A limited dataset comprised of demographic, utilization (with dates of service), and international classification of diseases (ICD) codes was extracted from the clinical data repository of the regional HIE for the eight-county region of Western New York for each year 2019 to 2021. The repository collects data from admission, discharge, and transfer notification and continuity of care documents extracted from health care provider electronic health records. The dataset includes information from clinical facilities (hospitals, OP offices), claims data, and data on deaths provided by the CMS. The .CSV files were downloaded and stored in a secure folder.
The source data are combined into a fully deidentified cohort table that includes features of demographics (age, sex (male/female), provider, and insurance type), health conditions (ICD-10 codes) using Clinical Classification Software Refined (CCSR) (Agency for Healthcare Research and Quality [AHRQ], 2021), and counts of annual encounters (IP, ED, and OP visits).
COMPLEXedex Algorithm
Published previously, the COMPLEXedex (Hewner, 2014; Hewner et al., 2014) clinical algorithm is a population-based system for risk-stratified care management of chronic disease and complexity and health service utilization. The algorithm assigns individual cases to 1 of 17 hierarchical categories based on chronic and behavioral health conditions in rank order based on hospitalization rate (Table 1). The COMPLEXedex aggregates the disease categories into four hierarchical segments ranging from the least to the most complex: No chronic (healthy), at-risk (hypertension, lipid disorder, obesity, and smoking history), Major Chronic (which includes mental health and SUD), and System failure (heart failure or chronic kidney disease), so that targeted interventions can be deployed to improve health outcomes (Hewner et al., 2017, 2018). Data on demographics and encounters (IP, ED, and OP) are also collected. While useful in understanding the impact of comorbidity and complexity on risk for health care utilization, additional features are necessary to fully capture the complex SDH of individuals with high needs.
Table 1.
COMPLEXedex-SDH Classification Table and Definitions
| Segment | Disease Rank | Conditions | |||
|---|---|---|---|---|---|
| No-chronic and at-risk | 1–5 | At-risk and no-chronic segments are combined | |||
| Chronic condition cohort (CHRONIC) | |||||
| Major chronic* | 6–7, 10–12 | Asthma, chronic obstructive pulmonary disease, diabetes (DM), coronary artery disease (CAD), and comorbid DM and CAD | |||
| System failure | 13–17 | Heart failure (HF), HF with comorbid DM and/or CAD, and chronic kidney disease | |||
| Behavioral health cohort (BEHAVIORAL) | |||||
| Substance use disorders* | 8 | Alcohol abuse, opioid addiction, and all other substance use disorders | |||
| Mental health disorders* | 9 | Anxiety, depression, bipolar, and/or all other mental health disorders | |||
| Social determinants of health cohort | |||||
| Basic needs | NA | Food, housing, or transportation insecurity | |||
| Hardship | NA | Financial insecurity, material hardship, stress, health care access issues, literacy challenges, employment issues, occupational exposures, or veteran status | |||
| Personal safety and relationships | NA | Social connection, intimate partner violence, elder abuse, trauma, upbringing, psychosocial issues, or sociocultural issues | |||
| Other social determinants | |||||
| Economic disadvantage | NA | Medicaid or Medicare/Medicaid dual eligibility | |||
| Cross-cohort needs definition | |||||
| Conditions found in ≥2 of the 3 cohorts (chronic condition and/or behavioral health (disease rank ≥6) and/or social determinants of health) | |||||
| High need definition | |||||
| Cross-cohort needs and other social determinants (economic disadvantage) | |||||
| Suboptimal utilization definition | |||||
| High IP/ED | NA | > 2 ED visits/year and/or IP hospitalizations and disease rank ≥6 | |||
| OP underutilization | NA | < 2 OP visits/year and disease rank ≥6 | |||
| Low value | NA | Both high IP/ED and OP underutilization and disease rank ≥6 | |||
| High need with suboptimal utilization definition | |||||
| High need and (high IP/ED or OP underutilization) | |||||
Note. ED, emergency department; IP, inpatient; OP, outpatient.
Indicates that these conditions were part of the major chronic segment in the original COMPLEXedex.
Approach
Content experts on the research team included PhD-prepared RNs and nationally-board certified advanced practice RNs (APRN) who are PhD students. One of the doctorally prepared nurses holds a PhD in anthropology, and the other holds a master’s degree in business (health care) administration (MBA). The content experts have over 30 years of combined experience working with large datasets at insurance companies, the New York State Medicaid Data Warehouse, CMS data (Home Health Outcomes and Assessment Information Set and the Master Beneficiary Summary File), regional HIE, and population-level survey data (e.g., the National Health and Aging Trends Study). Additional research team members included PhD-prepared computer scientists and PhD computer science students, and all student work was validated by senior researchers.
A two-phased approach was undertaken to update the COMPLEXedex chronic disease classification algorithm to include SDH. In phase one, two RNs used their content expertise to separate behavioral health (as a separate cohort) from the chronic condition cohort, remove no-chronic and at-risk from the chronic condition cohort, and update the COMPLEXedex clinical algorithm with new ICD-based SDH data features. In the second phase, a consensus-based clinical definition of high-need cases was developed by independent coding of utilization patterns and discussion among four nursing experts of the 2019 data features. Next, a clinical classification algorithm was developed using features from the ICD-based chronic condition, behavioral health, and SDH cohorts; other non-ICD-based social need indicators (such as Medicaid eligibility for economic disadvantage); and utilization patterns. The modified algorithm (COMPLEXedex-SDH) was then tested in the 2021 dataset.
Phase One: Laying the Foundation
Figure 1 outlines the study process.
Figure 1.
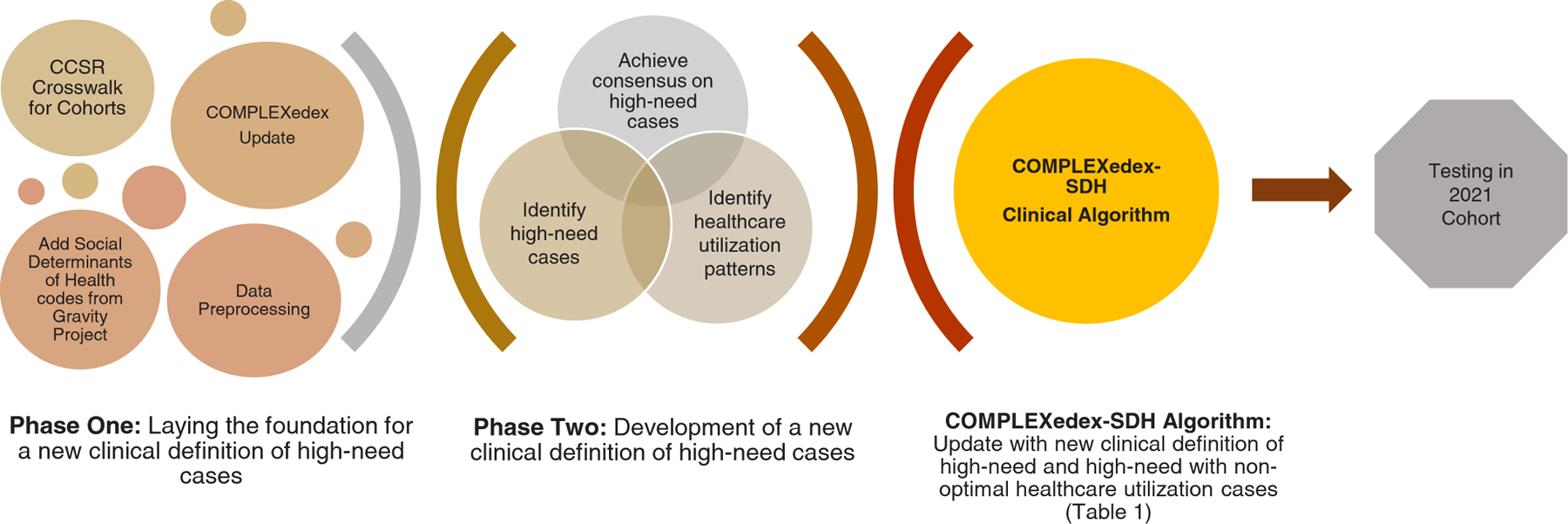
Process flow chart of the research approach. CCSR, Clinical Classification Software Refined.
CCSR Crosswalk for Chronic Condition and Behavioral Health Cohorts.
To update the COMPLEXedex, two doctorally-prepared RNs (first and last author) used the Healthcare Cost and Utilization Project (H-CUP CCSR) (AHRQ, 2021) system to group ICD-10 codes into their corresponding CCSR conditions. The CCSR codes were then assigned to COMPLEXedex conditions and aggregated into segments and cohorts in accordance with the data definitions in Table 1 (Hewner, 2014; Hewner et al., 2014).
Social Determinants of Health Cohort.
The CCSR does not include ICD codes for identifying social needs, so we used the newly created Gravity Project segments of basic needs, hardship, and personal safety/relationships (The Gravity Project, n.d.). The Gravity project aims to develop consensus-based data standards for sharing SDH information across organizations, providers, and caregivers using HIE. Each segment includes specific social needs that were operationally defined using ICD-10 codes following the Gravity project’s framework for classifying SDH. Basic needs included food, housing, or transportation insecurity (Z58, Z59); hardship included financial insecurity, material hardship, stress, health care access issues, literacy challenges, employment issues, occupational exposures, and veteran status (Z55–Z57, Z75); and personal safety/relationships included social connection, intimate partner violence, elder abuse, trauma, upbringing, psychosocial issues, or sociocultural issues (Z60, Z62, Z63, Z65, Z91) (The Gravity Project, n.d.). A total of 121 Z-codes were utilized for related SDH data definitions.
COMPLEXedex Update.
The following data elements were added to the COMPLEXedex: count of chronic conditions with disease rank ≥6, behavioral condition count, SDH condition count, and cross-cohort flag (indicating conditions ≥2 cohorts). Additionally, the COMPLEXedex-SDH also calculates the relative risk of IP admission for the hierarchical disease classification.
Data Preprocessing.
Diagnoses and health care utilization data features from ICD-10 codes and health encounters (IP, ED, OP visits) were identified in the 2019 subset of data (N = 19,20,848). We found that fewer than 3.5% of the cases had any ICD codes identifying social needs, so we added Medicaid or Medicare/Medicaid dual eligibility as a separate social need segment, which we called economic disadvantage (Table 1).
The data were checked for accuracy and missing values by three members of the research team on multiple, randomly selected 1,000 case samples of both positive and negative hits until the updated COMPLEXedex algorithm correctly identified and categorized cases for each year (2019–2021). Variables with missing data were retained in the dataset.
Phase Two: Development of a New Clinical Definition of High-Need Cases
Identifying High-Need Cases.
Multiple meetings discussing how to conceptually identify high-need cases using features available in the dataset were held with the team. We decided to start with a subset of cases with a diabetes diagnosis (n = 1,12,033) based on the assumption that this population would have a higher incidence of multiple chronic conditions, cross-cohort care needs, and possible behavioral health needs compared to the healthy population. Moreover, we chose a population with diabetes, which enabled us to use clinical practice guidelines to benchmark optimal health care system access patterns.
Next, two APRNs from the team, led by the second author, applied clinical practice guidelines and their expertise to identify the key features indicative of cases with the highest needs among an adult sample (≥18 years) in the 2019 dataset. Using a decision tree approach, cases were identified based on a combination of incidence of chronic conditions (diabetes), the presence of the cross-cohort flag, and ≥4 ED visits (Figure 2). We determined that ≥4 ED visits reduced the dataset to approximately 1,000 cases (n = 953), that is, those with the highest level of hospital utilization (highest need) for further analysis of utilization patterns and time between visits.
Figure 2.
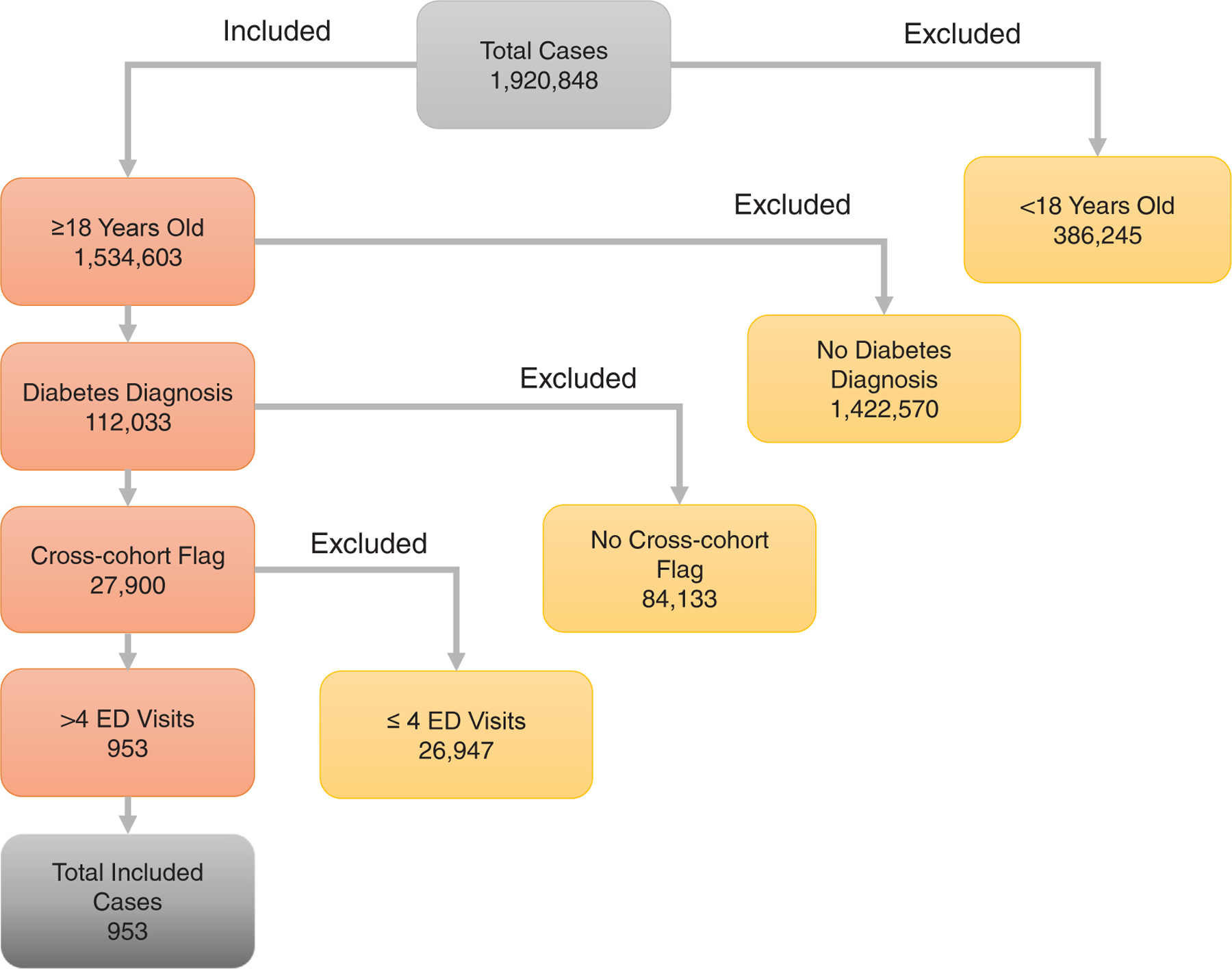
High need case clinical decision tree. ED, emergency department.
Achieving Consensus on High-Need Cases.
Next, we added information about the first 10 IP, ED, and OP encounters from the source data tables that included dates of service. We deidentified dates of service by making the discharge date of the first encounter in the year day 1. All subsequent encounters were identified by the type of encounter and the interval from the prior encounter. Then, we randomly selected a subsample of 400 high-need cases. Four RNs on the team (3 authors) each independently analyzed 100 cases and documented their determination of need in an Excel 2019 spreadsheet (Microsoft Corporation, Redmond, W.A.). The cases were discussed until consensus was achieved on the characteristics of high-need cases.
Identifying Health care Utilization Patterns.
To further refine the algorithm, the expert panel classified health care utilization patterns for the first 10 encounters of any type among the 400 cases, once again independently analyzing 100 cases each. We looked for regular OP visits with rapid OP visits after IP or ED encounters, without 30-day repeat encounters in the hospital setting, or IP or ED encounters without prior OP visits. This process was conducted iteratively, and disagreements were discussed among the group until a consensus definition for both high-need and suboptimal utilization patterns was determined.
COMPLEXedex-SDH Update With New Clinical Definition of High-Need
The consensus findings of a new clinical definition of high need and high need with nonoptimal health care access cases, including SDH items and health care utilization patterns, were used to further update the COMPLEXedex algorithm and create a new high need flag in the dataset (Table 1 and Figure 3) and a subset of high need and suboptimal utilization.
Figure 3.
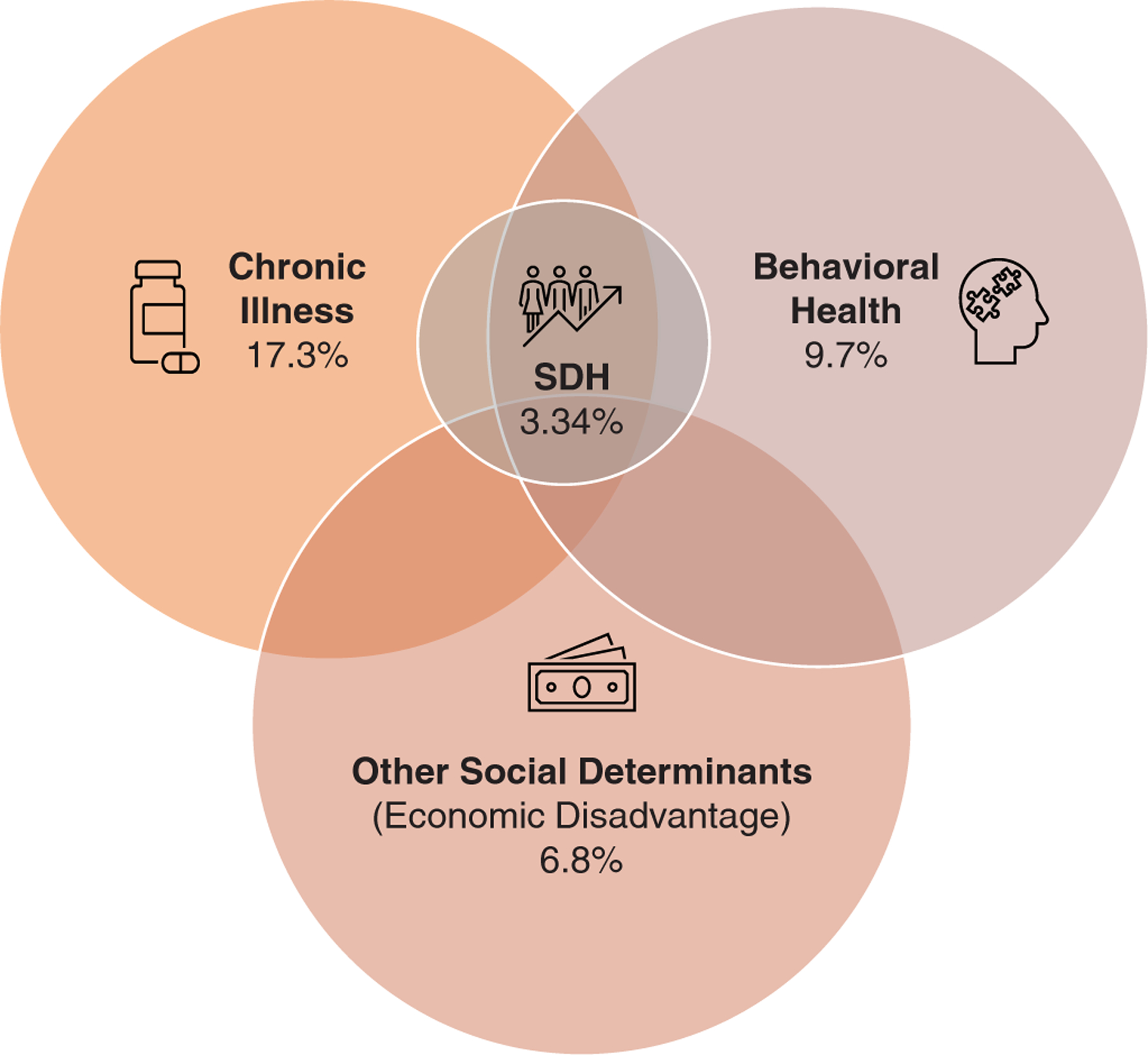
Conceptual model of the COMPLEXedex-SDH algorithm. SDH, social determinants of health.
Testing in 2021 Cohort.
In the final step, the new high-need definition was applied to the total adult sample from the same eight-county region of Western New York for 2021 (N = 15,99,176). The goal was to identify the 5% of the population who should be targeted for interventions created by access to care. Descriptive features were analyzed using IBM SPSS v28 (IBM Corporation, Armonk, N.Y.). The 2020 cohort was intentionally excluded, given the potential for anomalous health utilization patterns during the height of the COVID-19 pandemic.
Findings
A new consensus definition of high-need cases was developed to include a combination of complex chronic conditions, behavioral health, SDH, and health care utilization features. The COMPLEXedex algorithm was updated in accordance with the consensus definition, and the new algorithm was tested through consensus agreement of the research team and descriptive, quantitative analysis.
The COMPLEXedex-SDH
The updated COMPLEXedex-SDH algorithm defines high needs as cross-cohort needs and other social determinants. Cross-cohort needs were defined by conditions found in ≥2 of the 3 chronic condition cohorts (major chronic or system failure [disease rank ≥6], behavioral health, and/or SDH). Suboptimal utilization patterns were classified as High IP/ED (> 2 ED or IP encounters per year and disease rank ≥6), OP underutilization (< 2 annual OP visits with a disease rank ≥6), or Low value (both high IP and ED visits and OP underutilization with disease rank ≥6). High need with suboptimal utilization is where cases are high need, and either OP underutilization or High IP/ED are true (Table 1). The target population for future intervention, therefore, is those individuals who have a need and are currently using low-value approaches to access health care because there is an opportunity to improve their health outcomes by improving access to primary care.
Testing in 2021 Cohort
The total 2021 adult population (N = 15,99,176) had a mean age of 49.24 (median 49 years), 7,60,276 (47.5%) female, and 1,05,955 (6.6%) with unknown sex. There were 1,06,114 (6.6%) Medicaid recipients, 1,94,766 (12.2%) Medicare recipients, and 2,387 (0.1%) dual Medicaid/Medicare recipients. Exactly 3,69,746 (23.1%) of the population was commercially insured, 1,45,472 (9.1%) identified as having other insurance, and 7,80,691(48.8%) with none or undisclosed insurance.
The COMPLEXedex-SDH classified 6,01,221 individuals (17.3%) under chronic conditions (4.2% System Failure and 13.1% Major Chronic). The behavioral health classification included 9.7% of the population (n = 1,53,813), with 8.8% having mental health and 0.9% having SUD (Table 2). However, only 53,776 individuals (3.34%) were flagged for having social needs from the ICD-10 codes (2.58% personal safety and relationships, 0.53% hardships, and 0.23% basic needs). Using Medicaid as a proxy for economic disadvantage, Medicaid and dual eligibility were added as a social risk indicator under a new category of “other social determinants,” flagging an additional 6.8% (n = 1,08,501) of individuals with potential needs (Table 2).
Table 2.
COMPLEXedex-SDH Classification Results in the 2021 Adult Population (n = 15,99,176)
| Segment | Disease Rank | n | % |
|---|---|---|---|
| Chronic condition (CHRONIC) | |||
| No-chronic | 1–5 | 1,169,021 | 73.1 |
| Major chronic | 6–7, 10–12 | 209,595 | 13.1 |
| System failure | 13–17 | 66,747 | 4.2 |
| Behavioral health (BEHAVIORAL) | |||
| Substance use disorders | 8 | 13,648 | 0.9 |
| Mental health disorders | 9 | 140,165 | 8.8 |
| Social determinants of health | |||
| Basic Needs | N/A | 3,828 | 0.23 |
| Hardship | N/A | 8,635 | 0.53 |
| Personal safety and relationships | N/A | 41,313 | 2.58 |
| Other social determinants | |||
| Economic Disadvantage | N/A | 108,501 | 6.8 |
| Cross-cohort needs | |||
| Cross-cohort | N/A | 174,240 | 10.9 |
| High need | |||
| High need | N/A | 282,843 | 17.7 |
| Suboptimal utilization | |||
| High IP/ED | N/A | 113,502 | 7.1 |
| OP underutilization | N/A | 79,721 | 5.0 |
| Low value | N/A | 27,201 | 1.7 |
| High need w/ suboptimal utilization | |||
| High need w/ suboptimal utilization | 98,952 | 6.2 |
Note. ED, emergency department; IP, inpatient; OP, outpatient.
Some columns will not add up to 100% since it is possible to be classified into one or more simultaneously or due to rounding.
The suboptimal utilization category represents 13.8% of the population, with 7.1% (n = 1,13,502) classified as having high IP/ED, 5.0% (n = 79,721) OP underutilization, and 1.7% (n = 27,201) Low-value utilization. Nearly 11% (n = 174,240, 10.9%) of the population had cross-cohort needs, and 2,82,843 (17.7%) were flagged as being high-need overall. Finally, the combined high need with suboptimal utilization is 98,952 for 6.2% of the population. Within the 98,952 cases with high need and suboptimal utilization, the majority (64.3%) have cross-cohort needs, and nearly a quarter (24.7%) are economically disadvantaged based on Medicaid/dual eligibility.
Discussion and Recommendations
This study, as part of an ongoing program of research, introduces a novel approach for defining high-need cases and suboptimal health care utilization based on expert clinical consensus drawing on nursing expertise and clinical practice guidelines, shifting the paradigm from using cost and utilization as the predicted outcome and way to classify persons as high-need/high-cost. The new paradigm uses both medical complexity and social need and adds suboptimal utilization as a feature, indicating poor access to care. Using the COMPLEXedex-SDH clinical algorithm, cases can be classified into actionable cohorts based on transparent metrics that the nurses can use to identify patients and prioritize interventions, such as outreach calls and cross-sector care alerts, to improve health equity and outcomes. While precision health techniques have been used in recent research to assist in the identification and classification of patients and utilization groups (Hewner et al., 2023), the integration of value-based definitions attempts to capture individuals missed by traditional algorithms, improving reach to individuals disproportionally impacted by SDH.
The use of clinical practice guidelines and clinical expertise to define health care utilization patterns is a novel approach not extensively used in previous research. For example, a recent nationally representative study utilizing a sample of 5,040 adults ages 18 to 64 years measured the concepts of complexity and high utilization from indicators including socio-demographics, mental health, substance use disorders, and health behaviors (Pourat et al., 2022).
Pourat et al. (2022) were able to identify individuals with high-need and social risk in the super-utilizing classification; however, those labeled as low utilizers still may have significant needs and risks missed by this traditional high versus low utilization comparison. Parsing out expected OP clinical follow-up and evaluating that with ED and IP use, such as in our study, gives a more holistic picture of how high-need individuals interact with the health care system and the compounding influence of SDH on utilization patterns.
In another study, 9 different clusters of utilization patterns were identified in a sample of 32,017 adults from the U.S. National Health Interview Survey (Recchia et al., 2022), including 6 underutilization clusters and 1 cluster of overutilization of OP and ED services. Importantly, this study identified a class of underutilizers who also had a social risk-related concern (no insurance), which was partially responsible for their patterns of health care utilization. The work of Recchia and colleagues gives insight into the complexities associated with the underutilization of health care services and the nuances related to those clusters, such as having no insurance (Recchia et al., 2022).
Recommendations
Assessing the type and quantity of health care utilization, while important, is much more nuanced in individuals with SDH. For example, an individual may not interact with the health care system until they require a higher level of care, such as emergency medicine, or because they do not have established or easy-to-access OP services. This can occur due to a multitude of reasons, including distrust of the health care system, lack of financial resources, compounding complexity of chronic disease management, and/or mental health barriers. It is imperative to adapt current precision health techniques, taking into consideration differing patterns of utilization and associated SDH risk factors, to properly identify individuals and create equitable interventions. The COMPLEXedex-SDH clinical algorithm is expanding on prior research, incorporating social needs into precision health approaches, as well as further defining optimum utilization to guide clinical interventions, such as comprehensive shared care plans (Sullivan et al., 2017).
Future research will include a modified Delphi study of national experts for a consensus definition of persons with high needs using these preliminary findings as a starting point. We additionally plan to use the newly identified categories found in this study as a starting point for developing predictive algorithms for high need and health outcomes using supervised machine learning approaches and across different health conditions (e.g., heart failure). In addition, we will conduct longitudinal analysis using advanced statistical methods to further refine the COMPLEXedex-SDH algorithm and develop scalable measures for clinical practice use in learning health systems.
Limitations
There are important limitations to this study, including using diabetes as a model. While we acknowledge this limitation, the purpose of this exploratory work was to find a reasonable starting place to better understand SDH and optimal health care utilization patterns within a chronic condition population. Further research is necessary to further develop this preliminary framework for use in other populations. Only 3.34% of our population was flagged as having a social need. This is likely indicative of the fact that clinical sites are not adequately documenting SDH in the electronic health record using Z-codes. For this reason, we used Medicaid eligibility as a marker for economic disadvantage, increasing the proportion of individuals with risk for problematic social needs to 10.14%. While we only had insurance information on half of the population, the algorithm identified 17.7% of the population as high-need and 6.2% with high need and suboptimal utilization. However, it is possible that some individuals were excluded from the high-need classification because their insurance status information was missing. This large cohort of geographically spread cases provides important insights and implications for future research directions.
Conclusions
Precision health techniques have the capability to guide future nursing interventions, allowing for improved continuity and collaboration across health care and social service sectors. To mitigate algorithmic bias, a new definition and approach to finding high-need patients was needed to better identify and stratify people at the highest risk for poor outcomes. These newly stratified individuals can then be targeted for improved transitional care using comprehensive shared care plans across multiple service providers with the intention of improving continuity, removing redundancy, and attenuating complexity and social need-related barriers. This reconceptualized algorithm is a novel approach recognizing the importance of social needs with a goal of improving interventions and outcomes for individuals disproportionately impacted by SDH.
Funding
The research reported in this publication was supported by the Agency for Healthcare Research and Quality under Award number R01 HS028000-01.
Footnotes
CRediT Statement
Suzanne S. Sullivan: Conceptualization, Methodology, Data curation, Investigation, Writing, Visualization, Funding acquisition. Kathryn M. Ledwin: Conceptualization, Methodology, Data curation, Investigation, Formal analysis, Investigation, Validation. Sharon Hewner: Conceptualization, Methodology, Software, Data curation, Investigation, Writing, Visualization, Supervision, Project administration, Funding acquisition.
Declaration of Competing Interest
The authors have no conflicts of interest to report.
References
- Agency for Healthcare Research and Quality (AHRQ). (2021). H-CUP Clinical Classifications Software Refined (CCSR) https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp.
- Alderwick H, & Gottlieb LM (2019). Meanings and misunderstandings: A social determinants of health lexicon for health care systems. Milbank Quarterly, 97(2), 407–419. 10.1111/1468-0009.12390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates DW, Saria S, Ohno-Machado L, Shah A, & Escobar G (2014). Big data in health care: Using analytics to identify and manage high-risk and high-cost patients. Health Affairs ((Millwood)), 33(7), 1123–1131. 10.1377/hlthaff.2014.0041 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2021). The social-ecological model: A framework for prevention https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html.
- Centers for Medicare and Medicaid Services (CMS). (n.d.). Health related social needs https://www.medicaid.gov/health-related-social-needs/index.html.
- Eton DT, Yost KJ, Lai JS, Ridgeway JL, Egginton JS, Rosedahl JK, Linzer M, Boehm DH, Thakur A, Poplau S, Odell L, Montori VM, May CR, & Anderson RT (2017). Development and validation of the Patient Experience with Treatment and Self-management (PETS): A patient-reported measure of treatment burden. Quality of Life Research, 26(2), 489–503. 10.1007/s11136-016-1397-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gervasi SS, Chen IY, Smith-McLallen A, Sontag D, Obermeyer Z, Vennera M, & Chawla R (2022). The potential for bias in machine learning and opportunities for health insurers to address it. Health Affairs, 41(2), 212–218. 10.1377/hlthaff.2021.01287 [DOI] [PubMed] [Google Scholar]
- Hacker ED, McCarthy AM, & DeVon H (2019). Precision health: Emerging science for nursing research. Nursing Outlook, 67(4), 287–289. 10.1016/j.outlook.2019.06.008 [DOI] [PubMed] [Google Scholar]
- Hayes SL, Salzberg CA, McCarthy D, Radley DC, Abrams MK, Shah T, & Anderson GF (2016). High-need, high-cost patients: Who are they and how do they use health care? A population-based comparison of demographics, health care use, and expenditures. Issue Brief (Commonwealth Fund), 26, 1–14. [PubMed] [Google Scholar]
- Hewner S (2014). A population-based care transition model for chronically ill elders. Nursing Economics, 32(3), 109–117. [PubMed] [Google Scholar]
- Hewner S, Casucci S, Sullivan S, Mistretta F, Xue Y, Johnson B, Pratt R, Lin L, & Fox C (2017). Integrating Social Determinants of Health into Primary Care Clinical and Informational Workflow during Care Transitions. EGEMS (Wash. DC), 5(2), 2. 10.13063/2327-9214.1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewner S, Chen C, Anderson L, Pasek L, Anderson A, & Popejoy L (2021). Transitional care models for high-need, high-cost adults in the United States: A scoping review and gap analysis. Professional Case Management, 26(2), 82–98. 10.1097/ncm.0000000000000442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewner S, Seo JY, Gothard SE, & Johnson BJ (2014). Aligning population-based care management with chronic disease complexity. Nursing Outlook, 62(4), 250–258. 10.1016/j.outlook.2014.03.003 [DOI] [PubMed] [Google Scholar]
- Hewner S, Smith E, & Sullivan SS (2023). CIC 2022: Identifying high need primary care patients using nursing knowledge and machine learning methods. Applied Clinical Informatics, 14(03), 408–417. 10.1055/a-2048-7343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewner S, Sullivan SS, & Yu G (2018). Reducing emergency room visits and in-hospitalizations by implementing best practice for transitional care using innovative technology and big data. Worldviews Evidence Based Nursing, 15(3), 170–177. 10.1111/wvn.12286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joynt KE, Figueroa JF, Beaulieu N, Wild RC, Orav EJ, & Jha AK (2017). Segmenting high-cost Medicare patients into potentially actionable cohorts. Healthcare, 5(1–2), 62–67. 10.1016/j.hjdsi.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Long P, A, M., Milstein A, Anderson G, Apton KL, & Dahlberg M (2017). Effective care for high-need patients National Academy of Medicine. https://nam.edu/HighNeeds/highNeedPatients.html. [PubMed]
- McCradden MD, Joshi S, Mazwi M, & Anderson JA (2020). Ethical limitations of algorithmic fairness solutions in health care machine learning. The Lancet Digital Health, 2(5), e221–e223. [DOI] [PubMed] [Google Scholar]
- Obermeyer Z, Powers B, Vogeli C, & Mullainathan S (2019). Dissecting racial bias in an algorithm used to manage the health of populations. Science, 366(6464), 447–453. 10.1126/science.aax2342 [DOI] [PubMed] [Google Scholar]
- Pourat N, Chen X, Tsugawa Y, Lu C, Zhou W, Hoang H, Hair B, Bolton J, & Sripipatana A (2022). Intersection of complexity and high utilization among health center patients aged 18 to 64 years. American Journal of Managed Care, 28(2), 66–72. 10.37765/ajmc.2022.88751 [DOI] [PubMed] [Google Scholar]
- Rajkomar A, Hardt M, Howell MD, Corrado G, & Chin MH (2018). Ensuring fairness in machine learning to advance health equity. Annals of Internal Medicine, 169(12), 866–872. 10.7326/m18-1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Recchia DR, Cramer H, Wardle J, Lee DJ, Ostermann T, & Lauche R (2022). Profiles and predictors of healthcare utilization: Using a cluster-analytic approach to identify typical users across conventional, allied and complementary medicine, and self-care. BMC Health Services Research, 22(1), 29. 10.1186/s12913-021-07426-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuels-Kalow ME, Ciccolo GE, Lin MP, Schoenfeld EM, & Camargo CA Jr. (2020). The terminology of social emergency medicine: Measuring social determinants of health, social risk, and social need. Journal of the American College of Emergency Physicians Open, 1(5), 852–856. 10.1002/emp2.12191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shippee ND, Shah ND, May CR, Mair FS, & Montori VM (2012). Cumulative complexity: A functional, patient-centered model of patient complexity can improve research and practice. Journal of Clinical Epidemiology, 65(10), 1041–1051. 10.1016/j.jclinepi.2012.05.005 [DOI] [PubMed] [Google Scholar]
- Sullivan SS, Mistretta F, Casucci S, & Hewner S (2017). Integrating social context into comprehensive shared care plans: A scoping review. Nursing Outlook, 65(5), 597–606. 10.1016/j.outlook.2017.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Gravity Project (n.d.). https://thegravityproject.net/.
- World Health Organization (WHO). (2022). Social determinants of health Retrieved February 24, 2022 from https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1.


