Abstract
Objective:
Anterior knee pain (AKP) is associated with patellofemoral osteoarthritis (PFOA), but longitudinal studies are lacking. If AKP precedes PFOA, it may create an opportunity to identify and intervene earlier in the disease process. The purpose of this study was to examine the longitudinal relation of AKP to worsening PF cartilage over two years.
Design:
Participants were recruited from the Multicenter Osteoarthritis Study (MOST), a longitudinal study of individuals with or at-risk for knee OA. Exclusion criteria included bilateral knee replacements, arthritis other than OA, and radiographic PFOA. At baseline, participants completed a knee pain map questionnaire and underwent knee MRI. Imaging was repeated at 2-year follow-up. Exposure was presence of frequent AKP. Outcome was worsening cartilage damage in the PF joint defined as increase in MRI Osteoarthritis Knee Score from baseline to 2 years. Log-binomial models were used to calculate risk ratios (RR).
Results:
One knee from 1,083 participants (age 56.7 ± 6.6 years; BMI 28.0 ± 4.9 kg/m2) was included. Frequent AKP and frequent isolated AKP were present at baseline in 14.5% and 3.6%, respectively. Frequent AKP was associated with an increased risk (RR: 1.78, 95% CI: 1.21, 2.62) of 2-year worsening cartilage damage in the lateral PF compartment. No association was found between frequent AKP and worsening in the medial PF joint.
Conclusion:
Frequent AKP at baseline was associated with worsening cartilage damage in the lateral PF joint over 2 years.
Keywords: Anterior Knee Pain, Patellofemoral OA, Patellofemoral Cartilage
Introduction/Background
Early identification of individuals with or at-risk for developing knee osteoarthritis (OA) may lead to more effective therapeutic intervention and mitigate downstream effects of the disease. Studies of risk factors for knee OA have focused on tibiofemoral (TF) OA despite OA in the patellofemoral (PF) joint potentially representing the first step in the continuum of knee OA. Isolated PFOA is more prevalent than isolated TFOA, and presence of PFOA increases the risk for developing OA in the TF compartment.1,2 PFOA affects individuals at a younger age than TFOA. Thus, PFOA can have detrimental effects on participation in life roles for decades, including occupational tasks, domestic and parenting duties, and physical activity. Understanding risk factors specific to PFOA could help identify individuals early in the knee OA process, develop targeted treatments, and potentially alter the natural history of both PF and TF OA.
Anterior knee pain (AKP) may represent a potential marker for individuals that will go on to develop PFOA. AKP is associated with both radiographic signs of PFOA and biomechanical risk factors for OA. Two-thirds of individuals with persistent AKP have radiographic PFOA.3 Additionally, compared to those without AKP, individuals with AKP have twice the prevalence of MRI-detected cartilage damage in the PF joint.4 Increased or aberrant loading is associated with the initiation and progression of knee OA,5 and individuals with AKP have higher stress in the PF joint during knee flexion.6 Higher PF joint stress represents a potential mechanism for progression to PFOA.
To date, longitudinal studies are lacking in this area and are necessary to establish the temporal relation between AKP and PFOA. If AKP precedes PFOA, there is an opportunity to identify individuals that may benefit from intervention prior to PFOA onset to mitigate the long-term consequences of the disease. Thus, the purpose of this study was to examine the longitudinal relation of AKP to worsening PF cartilage over two years. We hypothesized that AKP would increase the risk of 2-year cartilage worsening the PF joint.
Methods
Participants were from the Multicenter Osteoarthritis Study (MOST), a longitudinal study of individuals with or at-risk for knee OA. The current analysis focuses on participants from the second wave of enrollment that occurred from 2016–2018 consisting of younger individuals earlier in the disease process (ages 45 – 69 years, Kellgren-Lawrence (KL) grade 0–2 and no severe or continuous knee pain), enabling the investigation of early disease risk factors. Participants were not eligible for enrollment if they had bilateral knee replacements, had a diagnosis of arthritis other than OA, were unable to provide informed consent, or were unlikely to attend follow-up visits. Participants were excluded from the current analysis if they had radiographic PFOA at baseline assessed with lateral view radiographs. PFOA was defined as presence of any osteophyte grade 2 or higher, or joint space narrowing of at least grade 2 plus osteophyte, sclerosis, or cyst of any grade in the PF joint.7 Participants filled out questionnaires related to knee pain at baseline and underwent imaging, including MRI and standard radiographs. MRI was repeated at a follow-up visit two years later.
Knee Pain
Presence of frequent AKP at baseline was the primary exposure. Participants were asked about their knee pain, including location and frequency. If participants reported pain in their knee, they were asked to mark where they experienced their pain on a knee pain map, consisting of an illustration of the knee divided into regions (Supplement 1). This knee pain map was developed to identify common locations of knee pain and has be previously used in studies from our group.8 Participants were grouped based on their frequency and location of pain. Those that reported having knee pain “most days in the last month” were considered to have frequent knee pain. Those with frequent knee pain that reported pain in the anterior region and no other region on the knee pain map were categorized as frequent isolated AKP. Those with frequent knee pain that marked pain in the anterior region as well as any other knee region were categorized as frequent AKP. Participants without frequent knee pain and those with frequent knee pain not in the anterior region were combined as a reference group.
Worsening Cartilage Damage
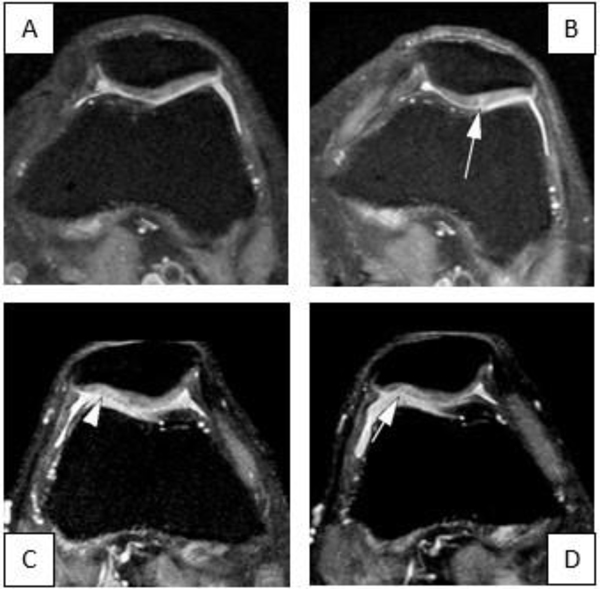
Worsening cartilage damage in the PF joint was the primary outcome measure. One knee was imaged with MRI at baseline and 2-year follow-up visit for all participants. Images were scored semi-quantitatively using the MRI Osteoarthritis Knee Score (MOAKS) system. The knee is divided into 14 total subregions, 4 in the PF and 10 in the TF joint. The medial PF joint was defined as the medial patella and anterior medial femur subregions, the lateral PF joint was the lateral patella and the anterior lateral femur subregions. Each subregion is scored from 0 to 3 for both the size of any cartilage loss as well as % full-thickness loss, with 0 representing no cartilage loss and 3 representing >75% cartilage surface within the subregion affected. Worsening cartilage damage was defined as any increase in MOAKS score, in either size or area, from baseline to 2-year follow-up including incidence, (i.e., subregions that were scored 0 at baseline and developed any cartilage damage in 2 years) (Figure 1). Two-year TF worsening cartilage damage was defined as any increase in MOAKS score in TF subregions.
Figure 1.
Definition of cartilage worsening was defined as either incident damage or worsening from pre-existing damage in any of the four patellofemoral subregions. A. Axial proton density-weighted fat suppressed mage shows a normal articular surface at the medial lateral patella facet in this participant with anterior knee pain. B. Follow up image 2 years later shows incident superficial cartilage fissurre at the lateral patella facet (arrow). C. In another participant with anterior knee pain the baseline MRI shows definite superficial cartilage damage ate lateral patella facet at baseline (arrowhead). D. Two years later there is progression to definite full-thickness damage at the lateral patella (arrow) defining this knee has worsening in cartilage damage from baseline to follow-up.
Statistical Analysis
Log binomial regression was used to calculate risk ratios (RRs) and examine the relationship of AKP to worsening cartilage damage. Four separate models were run to account for both exposures (frequent AKP and frequent isolated AKP) and both outcomes (medial and lateral PF compartments). All models were adjusted for age, sex, body mass index (BMI), race, and presence of radiographic TFOA at baseline. Sensitivity analyses were performed to confirm associations observed were due to frequent AKP specifically and not just knee pain or pain reported elsewhere within the knee. We repeated our analyses using the presence of frequent knee pain regardless of location as the exposure and an analysis comparing those with AKP to those with pain elsewhere in the knee. Additionally, we performed an analysis with worsening cartilage damage in the TF joint as the outcome to investigate whether any association of frequent AKP was specific to the PF joint. To determine the influence of baseline cartilage damage, we performed sensitivity analyses stratifying our primary analyses by presence of baseline cartilage damage. Individuals with MOAKS ≥ 2 at baseline in either subregion of the lateral and medial PF joint were considered to have cartilage damage at baseline.
Results
One knee from 1,083 individuals were included in the analysis. At baseline, the mean (standard deviation) age and BMI were 56.7 ± 6.6 years and 28.0 ± 4.9 kg/m2, respectively; 57%, 77.4%, and 8.6% were female, white, and had radiographic TFOA. Thirty-nine participants (3.6%) met the criteria for frequent isolated AKP and one hundred fifty-seven (14.5%) had frequent AKP. Two-year worsening cartilage damage was present in 11% and 14.1% for the lateral and medial PF joints, respectively. Worsening cartilage damage in the TF joint was present in 19.4% of participants.
Frequent AKP at baseline was associated with an increased risk (RR: 1.78, 95% CI: 1.21, 2.62) of worsening cartilage damage in the lateral PF joint (Table 1). A similar pattern was seen for frequent isolated AKP and lateral worsening cartilage damage, but this association was not statistically significant (RR: 1.55, 95% CI: 0.78, 3.08) (Table 2). No significant associations between AKP and medial PF joint worsening were observed. Sensitivity analysis showed no significant association between the presence of frequent knee pain regardless of location and the risk of 2-year worsening cartilage damage in either the medial or lateral compartment of the PF joint. When comparing to those with frequent knee pain that was not anterior, those with frequent knee pain in the anterior region had a higher risk (RR: 3.72, 95% CI: 1.49, 9.31) of cartilage worsening in the lateral PF joint. There was no significant association between the presence of frequent AKP (RR: 1.18; 95% CI: 0.81, 1.70) or frequent isolated AKP (RR: 1.33, 95% CI: 0.81, 2.19) and 2-year cartilage damage worsening in the TF joint.
Table 1:
Relation of frequent anterior knee pain to worsening cartilage damage by compartment
| Compartment | Outcome Prevalence: Reference Group | Outcome Prevalence: Exposure Group | Risk Ratio (95% CI) |
|---|---|---|---|
| Lateral PF | 90/926 (9.7%) | 29/157 (18.5%) | 1.78 (1.21, 2.62) |
| Medial PF | 128/926 (13.8% | 25/157 (15.9%) | 1.11 (0.75, 1.65) |
| Tibiofemoral* | 133/850 (15.7%) | 27/140 (19.3%) | 1.18 (0.81, 1.70) |
Outcome prevalence describes 2-year worsening cartilage damage. Exposure group represents individuals with frequent knee pain including pain in the anterior region at baseline. Reference group includes individuals without frequent knee pain as well as those with frequent knee pain anywhere except the anterior region. Models were adjusted for age, BMI, sex, race, and presence of TFOA at baseline.
Individuals with radiographic TFOA at baseline were omitted from analysis.
Table 2:
Relation of frequent isolated anterior knee pain to worsening cartilage damage by compartment
| Compartment | Outcome Prevalence: Reference Group | Outcome Prevalence: Exposure Group | Risk Ratio (95% CI) |
|---|---|---|---|
| Lateral PF | 112/1044 (10.7%) | 7/39 (18.0%) | 1.55 (0.78, 3.08) |
| Medial PF | 146/1044 (14.0%) | 7/39 (18.0%) | 1.26 (0.63, 2.50) |
| Tibiofemoral* | 150/952 (15.8%) | 10/38 (26.3%) | 1.33 (0.81, 2.19) |
Outcome prevalence describes 2-year worsening cartilage damage. Exposure group represents individuals with frequent knee pain exclusively in the anterior region. Reference group includes individuals without frequent knee pain as well as those with frequent knee pain not confined to the anterior region. Models were adjusted for age, BMI, sex, race, and presence of TFOA at baseline.
Individuals with radiographic TFOA at baseline were omitted from analysis.
For individuals with cartilage damage (MOAKS ≥ 2) at baseline, there was no significant association between presence of frequent AKP and cartilage damage worsening (RR: 1.16; 95% CI: 0.66, 2.06) in the lateral PF joint. In individuals without cartilage damage at baseline, frequent AKP was associated with increased risk of lateral PF worsening cartilage damage (RR: 1.97; 95% CI: 1.04, 3.73). No significant association was found between frequent AKP and medial PF worsening cartilage damage in individuals with (RR: 1.20; 95% CI: 0.71, 2.04) and without (RR: 0.79; 95% CI: 0.36, 1.74) cartilage damage at baseline.
Discussion
The presence of frequent AKP nearly doubled the risk of cartilage damage worsening in the lateral PF joint over two years. This effect was greater when comparing frequent AKP to those with knee pain in other regions, reinforcing that AKP specifically, not just the presence of pain in the knee, is driving this association. When comparing those that reported frequent knee pain regardless of the location to those without frequent knee pain, no significant associations were seen. This finding further supports the importance of the location of pain as a potential risk factor of PF cartilage damage worsening. Similar trends were seen in those with frequent isolated AKP. However, a low prevalence of those with frequent isolated AKP at baseline limited the precision of this finding. No significant association was found between AKP and 2-year cartilage worsening in the medial PF compartment or the TF joint. These findings support previous studies suggesting a link between AKP and PFOA,3,7 and further our understanding of a temporal relationship demonstrating that AKP increases the risk of cartilage worsening in the lateral PF joint. AKP may be a specific risk factor for lateral PFOA since no association was found between frequent AKP and 2-year cartilage worsening in the TF joint. Thus, our work contributes to fill gaps in literature on the relation between AKP and PFOA.
When stratifying for presence of cartilage damage at baseline, the association between frequent AKP and lateral PF cartilage worsening showed elevated risk in individuals without cartilage damage at baseline. In individuals with cartilage damage at baseline, the risk between frequent AKP and lateral worsening cartilage damage was attenuated and not significant. These findings suggest that frequent AKP may be a risk factor for worsening cartilage damage in individuals without prevalent cartilage damage.
Given our understanding of the complex relationship between loading and cartilage health in knee OA, timely intervention is necessary to optimize the benefits of treatments. Healthy cartilage positively adapts to loading in order to resist increased stresses.9 This relationship is disrupted in individuals with OA, and cartilage can no longer adapt to increased loading.9,10 AKP may be used as a screening tool that could permit earlier intervention in individuals at-risk for PFOA.
AKP was associated with increased risk of cartilage worsening in the lateral, but not medial, PF compartment. This is consistent with our understanding of biomechanical influences on the knee. Utilizing finite element modeling, Farrokhi et al.6 observed greater stresses during knee flexion in the lateral PF joint in individuals with AKP compared to those without knee pain. Although our study did not account for knee joint alignment, frontal plane alignment is associated with development of PF osteophytes and cartilage worsening.11 This association is compartment specific with varus alignment increasing risk for worsening in the medial PF and valgus alignment increasing risk to the lateral PF. Rehabilitation programs aimed at improving neuromuscular control of the hip and limiting dynamic knee valgus moments have been shown to reduce pain in individuals with AKP5 and may also mitigate the development of PFOA. The presence of AKP may be used to identify individuals more likely to respond to rehabilitation strategies aimed at decreasing stress within the lateral PF joint.
Similar to previous studies,12 we reported a higher prevalence of 2-year worsening in the medial PF compartment compared to the lateral PF compartment. From a biomechanical perspective, the lateral PF joint is exposed to more stress.6 Thus, if PFOA is a disease of abnormal mechanics, we would expect to see greater rates of PFOA in the lateral compartment. Most rehabilitation strategies (e.g., taping, bracing) are aimed at reducing the stress experienced by the lateral PF joint. The fact that medial PF cartilage worsening is more prevalent over two years suggests that there are unknown mechanical factors or mechanisms that explain its etiology. One possible reason may be the presence of medial PF plicas. Medial patella plica are highly prevalent in individuals with chronic knee pain and are associated with cartilage damage within the medial PF joint.13 Further research investigating possible explanations for the prevalence of medial PFOA are needed.
Our study does have several limitations. First, we utilized the lateral radiograph view at baseline to exclude those with radiographic PFOA. Lateral views are less sensitive than skyline views in evaluating PFOA,14 so it is possible that our analysis included some individuals with radiographic PFOA. The anterior region of the knee pain map used in MOST broadly includes the patella and peri-patella region. It is possible that individuals had AKP coming from other anatomical structures, such as the fat pad or patellar/quadriceps tendons. Lastly, our population consisted of individuals with a mean age of 56.7 years. While this is a younger cohort than those typically seen in research examining OA risk factors, investigating the same question in a younger cohort may help identify risk factors earlier in the disease process; however, such studies would require a large sample due to the lower prevalence of PFOA in younger individuals.
Conclusion
Individuals with frequent AKP had increased risk of 2-year cartilage worsening in the lateral PF joint. Frequent AKP may be a potential risk factor to screen for those at-risk for developing PFOA. Further research is needed to determine if identifying individuals with frequent AKP for targeted interventions mitigates the downstream effects of PFOA.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stefanik JJ, Guermazi A, Roemer FW, et al. Changes in patellofemoral and tibiofemoral joint cartilage damage and bone marrow lesions over 7 years: the Multicenter Osteoarthritis Study. Osteoarthr Cartil. 2016;24(7):1160–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duncan R, Peat G, Thomas E, Hay EM, Croft P. Incidence, progression and sequence of development of radiographic knee osteoarthritis in a symptomatic population. Ann Rheum Dis. 2011;70(11):1944–1948. doi: 10.1136/ard.2011.151050 [DOI] [PubMed] [Google Scholar]
- 3.Collins NJ, Oei EHG, de Kanter JL, Vicenzino B, Crossley KM. Prevalence of Radiographic and Magnetic Resonance Imaging Features of Patellofemoral Osteoarthritis in Young and Middle-Aged Adults With Persistent Patellofemoral Pain. Arthritis Care Res. 2019;71(8):1068–1073. doi: 10.1002/acr.23726 [DOI] [PubMed] [Google Scholar]
- 4.Macri EM, Neogi T, Jarraya M, et al. Can MRI-defined osteoarthritis features explain anterior knee pain in individuals with, or at risk for, knee osteoarthritis? The MOST Study. Arthritis Care Res (Hoboken). Published online March 2021. doi: 10.1002/acr.24604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farrokhi S, Voycheck CA, Tashman S, Fitzgerald GK. A biomechanical perspective on physical therapy management of knee osteoarthritis. J Orthop Sports Phys Ther. 2013;43(9):600–619. doi: 10.2519/jospt.2013.4121 [DOI] [PubMed] [Google Scholar]
- 6.Farrokhi S, Keyak JH, Powers CM. Individuals with patellofemoral pain exhibit greater patellofemoral joint stress: A finite element analysis study. Osteoarthr Cartil. 2011;19(3):287–294. doi: 10.1016/j.joca.2010.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macri EM, Neogi T, Tolstykh I, et al. Relation of Patellofemoral Joint Alignment, Morphology, and Radiographic Osteoarthritis to Frequent Anterior Knee Pain: Data from the Multicenter Osteoarthritis Study. Arthritis Care Res. 2020;72(8):1066–1073. doi: 10.1002/acr.24004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stefanik JJ, Neogi T, Niu J, et al. The diagnostic performance of anterior knee pain and activity-related pain in identifying knees with structural damage in the patellofemoral joint: The Multicenter Osteoarthritis Study. J Rheumatol. 2014;41(8):1695–1702. doi: 10.3899/jrheum.131555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edd SN, Omoumi P, Andriacchi TP, Jolles BM, Favre J. Modeling knee osteoarthritis pathophysiology using an integrated joint system (IJS): a systematic review of relationships among cartilage thickness, gait mechanics, and subchondral bone mineral density. Osteoarthr Cartil. 2018;26(11):1425–1437. doi: 10.1016/j.joca.2018.06.017 [DOI] [PubMed] [Google Scholar]
- 10.Mahmoudian A, Lohmander LS, Mobasheri A, Englund M, Luyten FP. Early-stage symptomatic osteoarthritis of the knee — time for action. Nat Rev Rheumatol. 2021;17(10):621–632. doi: 10.1038/s41584-021-00673-4 [DOI] [PubMed] [Google Scholar]
- 11.Macri EM, Felson DT, Ziegler ML, et al. The association of frontal plane alignment to MRI-defined worsening of patellofemoral osteoarthritis: the MOST study. Osteoarthr Cartil. 2019;27(3):459–467. doi: 10.1016/j.joca.2018.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gross KD, Niu J, Stefanik JJ, et al. Breaking the law of valgus: The surprising and unexplained prevalence of medial patellofemoral cartilage damage. Ann Rheum Dis. 2012;71(11):1827–1832. doi: 10.1136/annrheumdis-2011-200606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayashi D, Xu L, Guermazi A, et al. Prevalence of MRI-detected mediopatellar plica in subjects with knee pain and the association with MRI-detected patellofemoral cartilage damage and bone marrow lesions: Data from the Joints on Glucosamine study. BMC Musculoskelet Disord. 2013;14. doi: 10.1186/1471-2474-14-292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davies AP, Vince AS, Shepstone L, Donell ST, Glasgow MM. The Radiologic Prevalence of Patellofemoral Osteoarthritis. Clin Orthop Relat Res. 2002;402. https://journals.lww.com/corr/Fulltext/2002/09000/The_Radiologic_Prevalence_of_Patellofemoral.20.aspx [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.