Abstract
Background
This is an updated version of the original review, published in Issue 1, 2011, of The Cochrane Library. Acute lower abdominal pain is common, and making a diagnosis is particularly challenging in premenopausal women, as ovulation and menstruation symptoms overlap with symptoms of appendicitis, early pregnancy complications and pelvic infection. A management strategy involving early laparoscopy could potentially provide a more accurate diagnosis, earlier treatment and reduced risk of complications.
Objectives
To evaluate the effectiveness and harms of laparoscopy for the management of acute lower abdominal pain in women of childbearing age.
Search methods
The Menstrual Disorders and Subfertility Group (MDSG) Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library), MEDLINE, EMBASE, PsycINFO, LILACS and CINAHL were searched (October 2013). The International Clinical Trials Registry Platform (ICTRP) was also searched. No new studies were included in this updated version.
Selection criteria
Randomised controlled trials (RCTs) that included women of childbearing age who presented with acute lower abdominal pain, non‐specific lower abdominal pain or suspected appendicitis were included. Trials were included if they evaluated laparoscopy with open appendicectomy, or laparoscopy with a wait and see strategy. Study selection was carried out by two review authors independently.
Data collection and analysis
Data from studies that met the inclusion criteria were independently extracted by two review authors and the risk of bias assessed. We used standard methodological procedures as expected by The Cochrane Collaboration. A summary of findings table was prepared using GRADE criteria.
Main results
A total of 12 studies including 1020 participants were incorporated into the review. These studies had low to moderate risk of bias, mainly because allocation concealment or methods of sequence generation were not adequately reported. In addition, it was not clear whether follow‐up was similar for the treatment groups. The index test was incorporated as a reference standard in the laparoscopy group, and differential verification or partial verification bias may have occurred in most RCTs. Overall the quality of the evidence was low to moderate for most outcomes, as per the GRADE approach.
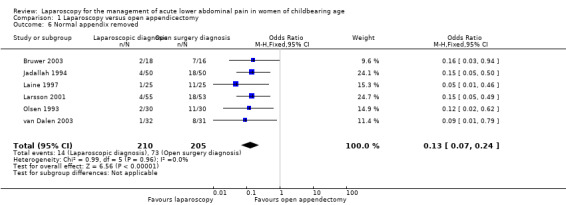
Laparoscopy was compared with open appendicectomy in eight RCTs. Laparoscopy was associated with an increased rate of specific diagnoses (seven RCTs, 561 participants; odds ratio (OR) 4.10, 95% confidence interval (CI) 2.50 to 6.71; I2 = 18%), but no evidence was found of reduced rates for any adverse events (eight RCTs, 623 participants; OR 0.46, 95% CI 0.19 to 1.10; I2 = 0%). A meta‐analysis of seven studies found a significant difference favouring the laparoscopic procedure in the rate of removal of normal appendix (seven RCTs, 475 participants; OR 0.13, 95% CI 0.07 to 0.24; I2 = 0%).
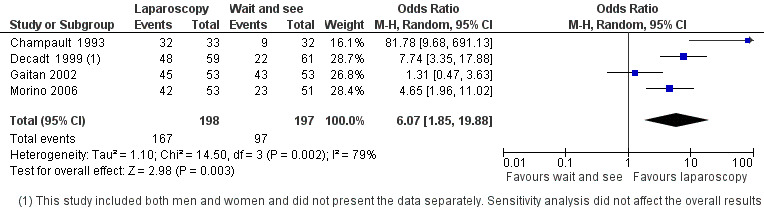
Laparoscopic diagnosis versus a 'wait and see' strategy was investigated in four RCTs. A significant difference favoured laparoscopy in terms of rate of specific diagnoses (four RCTs, 395 participants; OR 6.07, 95% CI 1.85 to 29.88; I2 = 79%), but no evidence suggested a difference in rates of adverse events (OR 0.87, 95% CI 0.45 to 1.67; I2 = 0%).
Authors' conclusions
We found that laparoscopy in women with acute lower abdominal pain, non‐specific lower abdominal pain or suspected appendicitis led to a higher rate of specific diagnoses being made and a lower rate of removal of normal appendices compared with open appendicectomy only. Hospital stays were shorter. No evidence showed an increase in adverse events when any of these strategies were used.
Keywords: Adult, Female, Humans, Young Adult, Appendectomy, Appendectomy/methods, Appendectomy/statistics & numerical data, Laparoscopy, Abdominal Pain, Abdominal Pain/etiology, Acute Pain, Acute Pain/etiology, Appendicitis, Appendicitis/complications, Appendicitis/diagnosis, Appendicitis/surgery, Pelvic Pain, Pelvic Pain/etiology, Premenopause, Randomized Controlled Trials as Topic, Watchful Waiting
Plain language summary
Managing acute lower abdominal pain in women of childbearing age
Review question: Cochrane authors reviewed available evidence on the use of laparoscopy to manage acute lower abdominal pain, non‐specific lower abdominal pain or suspected appendicitis in women of childbearing age. We found 12 studies.
Background: Acute lower abdominal pain is a common occurrence among women of childbearing age and frequently results in referral to hospital because clarifying the cause of the pain is often difficult. Probable diagnoses include ovulation pain, ovarian cysts, pelvic infection, ectopic pregnancy and appendicitis. Many women end up having their appendices removed unnecessarily. It has been suggested that visualisation of the pelvic cavity through laparoscopy could be useful in the management of women such as these.
Study characteristics: Twelve studies were identified with 1020 women from 11 countries. Eight studies compared laparoscopy versus open appendicectomy, and four compared laparoscopy using a wait and see approach. The evidence is current to October 2013.
Key result: In this review of randomised controlled trials, laparoscopy was found to be superior to both open appendicectomy alone and a wait and see strategy, as more specific diagnoses were made before discharge, and shorter hospital stays and earlier return to work (when compared with open appendicectomy only) were reported. No evidence was found of an increase in adverse events when any of these strategies was applied. The rate of removal of normal appendices was reduced with the laparoscopic approach compared with open appendicectomy but was greater when a laparoscopic approach was compared with a wait and see strategy.
Quality of the evidence: The quality of the evidence was ranked as low to moderate for most outcomes, mainly because many of the studies had methodological limitations and imprecision was noted for some outcomes.
Summary of findings
Summary of findings for the main comparison. Laparoscopy compared with open appendicectomy.
| Laparoscopy compared with open appendicectomy for acute lower abdominal pain in women of childbearing age | ||||||
|
Patient or population: women of childbearing age with acute lower abdominal pain Settings: hospital Intervention: laparoscopy Comparison: open appendicectomy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Open appendicectomy | Laparoscopy | |||||
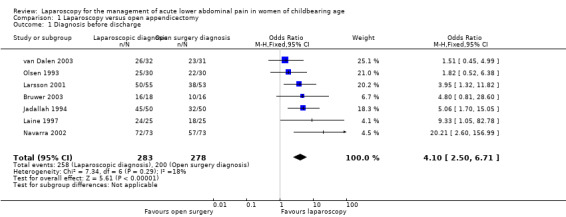
| Diagnosis before discharge | Risk population | OR 4.10 (2.50 to 6.71) | 561 (7) | ⊕⊕⊕⊝ moderate | Most studies had methodological limitations1 | |
| 719 per 1000 | 913 per 1000 (865 to 945) |
|||||
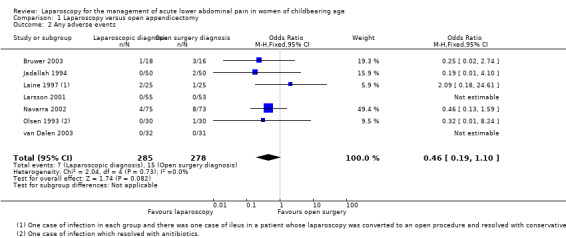
| Any adverse events | Risk population | OR 0.46 (0.19 to 1.10) | 563 (7) | ⊕⊕⊝⊝ low | Most studies had methodological limitations2 | |
| 54 per 1000 | 26 per 1000 (11 to 59) |
|||||
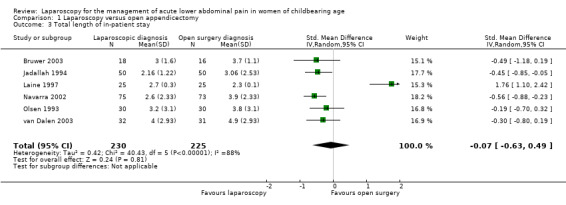
| Total length of in‐patient stay (days) | Mean ranged across control groups from 2.30 to 4.9 | Mean ranged across intervention groups from 2.16 to 4.0 | Mean difference ‐0.07 (‐0.63 to 0.49) | 455 (6) | ⊕⊕⊝⊝ low | Most studies had methodological limitations3 |
| Normal appendix removed | 356 per 1000 | 67 per 1000 (37 to 117) | OR 0.13 (0.07 to 0.24) | 475 (7) | ⊕⊕⊕⊝ moderate | Most studies had methodological limitations4 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Diagnosis before discharge: Six of seven studies had unclear risk of selection and attrition bias and high risk of detection and performance bias.
2Any adverse events: Six of seven studies had unclear risk of selection and attrition bias and high risk of detection and performance bias. Imprecision was noted.
3Five studies had unclear risk of selection and attrition bias and high risk of detection and performance bias. Inconsistency and imprecision were noted.
4Six of seven studies had unclear risk of selection and attrition bias and high risk of detection and performance bias.
Summary of findings 2. Laparoscopy compared with 'wait and see' strategy.
| Laparoscopy compared with 'wait and see' strategy for the management of acute lower abdominal pain in women of childbearing age | ||||||
|
Patient or population: women of childbearing age with acute lower abdominal pain Settings: hospital Intervention: laparoscopy Comparison: 'wait and see' strategy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| 'Wait and see' strategy | Laparoscopy | |||||
| Diagnosis before discharge | Risk population | OR 6.07 (1.85 to 19.88) |
395 (4) | ⊕⊕⊕⊝ moderate | Most studies had methodological limitations1 | |
| 492 per 1000 | 855 per 1000 (642 to 951) | |||||
| Any adverse events | Risk population | OR 0.87 (0.45 to 1.67) |
399 (4) | ⊕⊕⊕⊝ moderate | Most studies had methodological limitations2 | |
| 111 per 1000 | 126 per 1000 (61 to 194) |
|||||
|
Total length of in‐patient stay (days) |
Mean ranged across control groups from 4.65 days | Mean total length of in‐patient stay in the intervention groups was 0.38 standard deviations lower (0.69 to 0.08 lower) | 169 (2) | ⊕⊕⊝⊝ low | Most studies had methodological limitations3 | |
| Normal appendix removed | 275 per 1000 | 666 per 1000 (457 to 818) |
OR 5.14 (2.22 to 11.87) |
104 (1) | ⊕⊕⊝⊝ low | Only one study had methodological limitations4 |
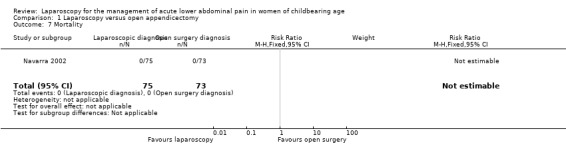
| Mortality | Risk population | OR 1.03 (0.06 to 16.93) |
334 (3) | ⊕⊕⊝⊝ low | Only one study had events of mortality, two studies had no mortality in either arms. Most studies had methodological limitations5 | |
| 6 per 1000 | 6 per 1000 (0 to 93) |
|||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Diagnosis before discharge: One of four studies had low risk of selection bias because investigators used a truly random allocation method. Three of four studies did not inform the concealment method. All had unclear risk of attrition bias and high risk of detection and performance bias.
2Any adverse events: One of four studies had low risk of selection bias because investigators used a truly random allocation method and three of four studies did not inform the method of concealment. All had unclear risk of attrition bias and high risk of detection and performance bias. Imprecision was noted.
3Total length of in‐patient stay: Both studies had low risk of selection bias because investigators used a truly random allocation method, although they did not inform the method of concealment. Both had unclear risk of attrition bias and high risk of detection and performance bias. Inconsistency and imprecision were noted.
4Normal appendix removed: Inconsistency and imprecision were noted. High and unclear risk of bias for most risk of bias domains.
5Mortality: Two of three studies had low risk of selection bias because investigators used a truly random allocation method, although they did not inform the method of concealment. All had unclear risk of attrition bias and high risk of detection and performance bias; thus the estimate had high imprecision.
Background
Description of the condition
Acute lower abdominal pain is commonly seen among patients attending hospital emergency departments (CDC 2003). Acute lower abdominal pain frequently presents as non‐specific abdominal pain (NSAP), defined as pain of less than seven days' duration for which no immediate cause can be found after initial testing has been performed, or pain located on the right iliac fossa. For NSAP, there is no clear indication for surgery (Poulin 2000; Sanders 2006). It has been reported that of all patients with acute abdominal pain, 35% to 43% have NSAP (Irvin 1989; Strömberg 2007). The prevalence is higher in premenopausal women (Decadt 1999). Reaching a diagnosis is particularly challenging in premenopausal women, as the physiological changes associated with ovulation and menstruation can overlap with the symptoms of more serious conditions such as torsion of the ovary, pelvic inflammatory disease, ectopic pregnancy and appendicitis (Whitworth 1988). Such conditions are less likely in postmenopausal women; therefore misdiagnosis is not as common for these women. The incidence of a misdiagnosis could be as high as 26% to 45% in premenopausal women (Beyan 2003; Borgstein 1997; Laine 1997; Sanders 2006; Tzovaras 2007).
The traditional approach to the treatment of suspected appendicitis has been open appendicectomy. With this approach, the incidence of removal of a normal appendix is between 10% and 30% (Althoubaity 2006; Bijnen 2003; Flum 2002). The removal of a normal appendix is associated with substantial complications and costs. Bijnen et al. found that among study participants who underwent a negative appendicectomy for suspected appendicitis, complications occurred in 6%, reoperation was performed in 2% and mean extra hospital costs were EUR 2712 (Bijnen 2003). Another study, performed in the United States, estimated that 261,134 study participants underwent non‐incidental appendicectomy in 1997, of which 15.3% were negative for appendicitis. The trial authors reported that women had a higher rate of removal of a normal appendix. In addition, participants with a normal appendix removed had a significantly longer length of stay and a higher total charge for the admission, as well as higher rates of case fatality and infectious complications (Flum 2002). In the past, women with NSAP have been managed by taking a 'wait and see' approach or, alternatively, by performing open appendicectomy, especially when pain was located on the right iliac fossa. However, with the advent of laparoscopy has come the change to a less invasive diagnostic strategy in patients with acute abdominal pain.
Description of the intervention
This review considered three strategies for the management of acute lower abdominal pain: the wait and see approach, open appendicectomy and laparoscopy.
The so‐called wait and see approach for establishing the cause of NSAP involves close clinical observation and repeated laboratory and diagnostic imaging tests and sometimes laparotomy.
Open appendicectomy involves a surgical incision performed under general anaesthesia, using a right iliac fossa approach, and removal of the appendix, regardless of the presence or absence of pathology.
Laparoscopy is the direct visual examination of the abdominal and pelvic cavities. A minimal incision (1 cm) is made in the abdominal wall to allow a special port with a laparoscope to pass through. The lens is fitted with a video camera and zoom, a light source and a high‐flow insufflator (for introduction of carbon dioxide gas), which allows the performance of surgical procedures when necessary.
How the intervention might work
Diagnostic laparoscopy could provide both a more accurate diagnosis and reduced risks of complications related to delayed diagnosis (Golash 2005; Ou 2000; Salky 1998). Other possible benefits include improved quality of life, less associated pain and reduced length of hospital stay (Golash 2005). Management of conditions that cause acute lower abdominal pain could be enhanced.
It has been estimated that an open appendicectomy strategy can establish the cause of acute lower abdominal pain in 45% of patients (Borgstein 1997), and a wait and see strategy with imaging in 84% (Sala 2007). Laparoscopy is associated with accurate diagnosis in 50% to 95% of patients (Moberg 1998; Sellors 1991; Spirtos 1987). This wide variation could be explained by gender, the accepted period of observation and the location of the pain.
However, laparoscopy is a costly technique that is associated with risks of complications such as bladder and bowel injury and wound infection; the need for anaesthesia (Golash 2005; Navez 1995); and the possibility that a final diagnosis still may not be made (Moberg 1998). One study using laparoscopic examination reported that histopathological examination of the appendix revealed no acute inflammation of the appendix in 24.9% of operated cases (Koch 2002).
The harms of taking the wait and see approach or using the open appendicectomy strategy include increased likelihood of complications such as peritonitis, haemorrhage or infertility associated with a late diagnosis, as well as increased length of in‐patient hospital stay and increased costs. In some cases, a laparotomy (a major surgical procedure involving a large incision (> 10 cm) through the abdominal wall to gain access to the abdominal cavity) might be performed unnecessarily.
Why it is important to do this review
Computed tomographic scanning, ultrasonography and laparoscopy have been advocated to improve accuracy in the diagnosis of appendicitis. It has been suggested that laparoscopy compared with the conventional strategy could lower the rate of diagnostic error in the management of acute abdominal pain. No definitive evidence has shown the comparative benefits and risks of these different strategies. The benefit of using laparoscopy over open surgery in the management of acute appendicitis in pregnant women remains a subject of controversy despite the publication of a number of randomised controlled trials (RCTs).
The intent of this review is to provide a unique evaluation of diagnostic strategies with regard to the management of acute lower abdominal pain in premenopausal women. The scope of the review does not include an evaluation of the diagnostic accuracy of either method in terms of their comparative effectiveness.
The scope of this intervention review reflects the description by Roper 1988, whereby we seek to technically assess and evaluate the appropriate use of an intervention in a given situation. The review sets out to compare both diagnostic strategies in terms of effectiveness, safety, costs and patient preferences.
Another Cochrane review compared the diagnostic and therapeutic effects of laparoscopic and conventional open surgery in all patients with symptoms and signs of acute appendicitis (Sauerland 2010). The review authors concluded that laparoscopy can serve as a diagnostic and therapeutic tool in patients with suspected appendicitis. The diagnostic effects were analysed separately for young women, and a large reduction in unnecessary appendicectomies and improved diagnostic efficacy were reported (Sauerland 2010). Although some of those findings overlap with the findings of our review, we decided to present a detailed description of the diagnostic effectiveness of laparoscopy in women of childbearing age compared with a wait and see strategy.
Objectives
To evaluate the effectiveness and harms of laparoscopy for the management of acute lower abdominal pain in women of childbearing age.
Methods
Criteria for considering studies for this review
Types of studies
Inclusion criteria
All published and unpublished RCTs comparing diagnostic laparoscopy with open appendicectomy or a wait and see strategy.
No limitation on language or publication status was applied. Open randomised clinical trials were included. RCTs that included women as part of the sample were included. Quasi‐RCTs were not included.
Types of participants
Inclusion criteria
RCTs that included premenopausal women who presented with acute lower abdominal pain, non‐specific abdominal pain, right‐sided pain or suspected appendicitis were included. Studies in which participants had a clear diagnosis of appendicitis were excluded.
Non‐specific abdominal pain is defined as pain of less than seven days’ duration for which no immediate cause can be found after initial tests have been performed. Non‐specific abdominal pain does not clearly require surgical intervention (Poulin 2000; Sanders 2006).
Changes were made to the published protocol to include women with suspected appendicitis, and studies where at least 75% of the participants were women of premenopausal age.
Types of interventions
Trials were included if they evaluated the management of premenopausal women with non‐specific acute pain or suspected appendicitis using:
laparoscopy compared with open appendicectomy; or
laparoscopy compared with a wait and see strategy.
Laparoscopy is defined as a surgical procedure in which a laparoscope is used through the abdominal wall with the aim of visualising the pelvic and abdominal cavities to diagnose an underlying cause of pain. Typically, this procedure is performed within the first 72 hours of an in‐patient stay.
Open appendicectomy is performed when a right iliac fossa incision is made and the appendix is excised after the muscular and peritoneal layers are opened.
A wait and see strategy is defined as close clinical observation combined with the use of laboratory tests or diagnostic imaging. It does not include laparoscopy, but it could include laparotomy.
Changes made to the published protocol included that the conventional strategy was replaced by 'wait and see' or by open appendicectomy.
Types of outcome measures
Outcomes measured were related to the effectiveness and safety of each strategy used in the management of non‐specific acute abdominal pain or suspected appendicitis in premenopausal women.
Primary outcomes
Number of specific diagnoses before discharge: number of cases in which a specific diagnosis was reached before discharge, for each strategy studied.
Adverse events (AEs): any events that, in the opinion of the investigator, may adversely affect the rights, welfare or safety of participants in the study as a result of the application of a management method. Complications could be reported in the short term or over the long term. Although removal of a normal appendix is an AE, it was reported separately in the results section, as each participant could be counted only once within each study.
Secondary outcomes
Total length of in‐patient stay.
Mean operating time.
Return to normal activities.
Quality of life.
Mortality.
Cost‐effectiveness, taking into account direct medical costs from the point of view of third‐party payers or institutions.
Search methods for identification of studies
We followed the Menstrual Disorders and Subfertility Group methodology.
Electronic searches
All reports that described RCTs of laparoscopy and acute abdominal pain were sought using the following strategy.
The Menstrual Disorders and Subfertility Group (MDSG) Specialised Register was searched by the Group’s trials search co‐ordinator using the following terms: "laparoscopic" or "laparoscopic excision" or "laparoscopic imaging" or "laparoscopic dye" or "laparoscopic imaging" or "laparoscopic procedure" or "laparoscopic surgery" or "laparoscopic techniques" or "laparoscopy" or Title CONTAINS "laparoscopic" or "laparoscopic excision" or "laparoscopic imaging" or "laparoscopic dye" or "laparoscopic imaging" or "laparoscopic procedure" or "laparoscopic surgery" or "laparoscopic techniques" or "laparoscopy" AND the terms "acute" or "abdominal pain" or "pelvic pain" or "Pain‐abdominal" or "pain‐pelvic" or "ectopic pregnancy" or "pelvic inflammatory disease" or "Ovarian Cysts" or "ovarian cyst" or "acute" or Title CONTAINS "acute" or "abdominal pain" or "pelvic pain" or "Pain‐abdominal" or "pain‐pelvic" or "ectopic pregnancy" or "pelvic inflammatory disease" or "Ovarian Cysts" or "ovarian cyst" or "acute", in the titles, abstracts and keywords.
This register also contains unpublished trial abstracts, which were found by handsearching of 20 relevant journals and conference proceedings.
The search was updated from January 2010 to October 2013 in the Cochrane MDSG Specialised Register, MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials (CENTRAL) and PsycoINFO using the Ovid platform.
A previous search was carried out in the following databases using the Ovid platform.
MEDLINE (1980 to April 2010) (Appendix 1).
EMBASE (1980 to April 2010) (Appendix 2).
CINAHL (1980 to April 2010) (Appendix 3).
CENTRAL (1998 to October 2013) (Appendix 4); PsycINFO (1980 to October 2013) (Appendix 5); and the Cochrane MDSG Specialised Register (Appendix 6).
LILACS (Appendix 7) and SciELO for studies reported in Portuguese and Spanish (February 2013).
Both indexed and free text terms were used. The RCT filter from the MDSG was used.
We also searched the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/en/) search portal (last search May 2013) using the following search strategy: (Laparoscopic OR laparoscopy) AND women AND (abdominal OR pelvic OR appendicitis OR abdomen) AND pain.
Searching other resources
Citation lists from reviewed articles and other relevant publications were searched.
No restrictions, such as language, were applied.
Other strategies for locating studies included personal communication with manufacturers, experts and specialists working in the field and screening of conference proceedings.
Data collection and analysis
Data were analysed using Review Manager software (RevMan 5).
Selection of studies
Two review authors (from Gaitán H, Reveiz L, Elias VM) independently screened the titles and abstracts of trials identified by the search for inclusion based on the selection criteria outlined above. One review author is a content and methodology expert, and the other is a methodology expert.
The full text of an article was retrieved if there was any doubt as to whether the article should be excluded. Gaitán H obtained copies of the studies selected for inclusion and sent them to Reveiz L. Both review authors then independently assessed whether the studies met the inclusion criteria. If disagreement between the two review authors arose, a third review author (Farquhar C) reviewed the information to decide on inclusion or exclusion of a trial.
Further information was sought from the study authors when papers contained insufficient information to allow a decision regarding eligibility for inclusion in the review.
Data extraction and management
Data from studies that met the inclusion criteria were independently extracted by two review authors (Gaitán H, Reveiz L) using a data extraction form. Discrepancies were resolved by discussion.
Data that were extracted included the following.
Inclusion and exclusion criteria, clearly defined.
Baseline information on participants for comparable intervention and control groups at entry (eligibility criteria, age of women, duration of pain, temperature, white blood cell count, abdominal surgery history).
Location of the study.
Trial design.
Power calculation performed.
Method used to generate random allocation.
Methods used to maintain allocation concealment.
Types of interventions provided: type of diagnostic laparoscopic method (video laparoscopy) and type of conventional diagnostic strategy, such as use of laboratory tests, and accepted time of observation.
Other interventions in the groups under evaluation.
Numbers of women enrolled, randomly assigned, excluded after randomisation and analysed.
Outcomes stated in methods versus outcomes reported in results.
Use of any method of blinding of researchers to the intervention for evaluation of outcomes.
How outcomes such as time of hospitalisation before diagnosis, definitive diagnosis, adverse events, recurrent episodes of pain, length of in‐patient stay and cost‐effectiveness were defined.
Differences between groups for outcome assessment in terms of methods used to obtain the definitive diagnosis.
Time of follow‐up of participants to measure outcomes: evolution in terms of recurrent or chronic abdominal pain.
How adverse event reports were validated.
Numbers of participants lost to follow‐up in the two groups.
Use of intention‐to‐treat analysis.
Funding sources reported.
Ethical issues: use of signed informed consent; ethics approval.
This information was collated and presented in the tables Characteristics of included studies and Characteristics of excluded studies.
Assessment of risk of bias in included studies
Two review authors (Reveiz L, Gaitán H) independently assessed the risk of bias of each trial using a simple form and followed the domain‐based evaluation as described in the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011). Review authors discussed discrepancies and achieved consensus on the final assessment.
We assessed the following domains as low, unclear or high risk of bias.
Generation of allocation sequence.
Allocation concealment.
Blinding (of participants, personnel and outcome assessors).
Incomplete outcome data.
Selective reporting.
Other sources.
Generation of allocation sequence (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk (any truly random process, e.g. random number table; computer random number generator); or
unclear risk (the trial was described as randomised, but the method used for allocation sequence generation was not described).
Allocation concealment (checking for possible selection bias)
We described for each included study the methods used to conceal the allocation sequence in sufficient detail and to determine whether the intervention allocation could have been foreseen in advance of, or during, recruitment, or changed after assignment.
We assessed the methods as:
low risk (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or
unclear risk (trial was described as randomised, but the method used to conceal the allocation not described).
Blinding or masking (checking for possible performance and detection bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We judged studies at low risk of bias if they were blinded, or if we judged that lack of blinding could not have affected the results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed blinding methods as:
low risk, high risk or unclear risk for participants;
low risk, high risk or unclear risk for personnel; or
low risk, high risk or unclear risk for outcome assessors.
Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We assessed methods on outcome data as:
low risk (any one of the following): no missing outcome data; reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups; for dichotomous outcome data, the proportions of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size; missing data imputed using appropriate methods;
high risk (any one of the following): reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size; ‘as‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation; potentially inappropriate application of simple imputation; or
unclear risk (any one of the following): insufficient reporting of attrition/exclusions to permit judgement of ‘low risk’ or ‘high risk’ (e.g. number randomly assigned not stated, no reasons provided for missing data); the study did not address this outcome.
Selective reporting bias (reporting bias due to selective outcome reporting)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed reporting methods as:
low risk (any one of the following): The study protocol is available and all of the study’s prespecified (primary and secondary) outcomes of interest in the review have been reported in the prespecified way, or the study protocol is not available, but it is clear that published reports include all expected outcomes, including those that were prespecified (convincing text of this nature may be uncommon);
high risk (any one of the following): Not all of the study’s prespecified primary outcomes have been reported; one or more primary outcomes are reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified; one or more reported primary outcomes were not prespecified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered into a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study; or
unclear risk: Information is insufficient to permit judgement of ‘low risk’ or ‘high risk’.
Free of other bias (bias due to problems not covered elsewhere in the table)
We described for each included study any important concerns that we have about other possible sources of bias (baseline imbalance, sponsorship bias, differential verification bias, partial verification bias and incorporation bias, bias of the presentation data, etc.).
Low risk of bias: The trial appears to be free of other components that could put it at risk of bias.
Unclear risk of bias: The trial may or may not be free of other components that could put it at risk of bias.
High risk of bias: Other factors in the trial could put it at risk of bias (e.g. no sample size calculation made, academic fraud, industry involvement, extreme baseline imbalance).
Measures of treatment effect
Dichotomous data were expressed as odds ratios (ORs) with 95% confidence intervals (CIs) and, when possible, were combined in a meta‐analysis using RevMan 5 software. The OR has mathematically sound properties that are consistent with benefits or harms and work well in small samples with rare events.
For continuous outcome data, such as time of hospitalisation before diagnosis and total length of in‐patient stay, results for each study were expressed as differences in means with 95% CIs and were combined for meta‐analysis, when appropriate, using the mean difference (MD). If the standard deviation was not available, this was imputed using the technique described in the Cochrane Handbook for Systematic Reviews of Interventions (Section 7.7.3.3).
Primary analysis used the fixed‐effect model, and sensitivity analysis (if required) used the random‐effects model. We used the random‐effects model if the I2 statistic was greater than 50% (Higgins 2011).
Cost‐effectiveness and quality of life analyses were summarised in narrative form.
If no data were available for some outcomes, these were described within the review. This potentially indicated the need for further clinical trials in this area.
Unit of analysis issues
When different scales were used to report the same outcomes, and we were not able to convert them, we planned to use standardised mean difference (SMD). This was not necessary, as no outcome data were extracted that required this.
Dealing with missing data
The review authors contacted the lead authors of the trials for which data clarification was required. This contact was made by email.
Assessment of heterogeneity
Statistical analysis was performed in accordance with the guidelines developed by The Cochrane Collaboration (Higgins 2011). Assessment of heterogeneity was possible when two or more primary studies were identified for inclusion in a meta‐analysis. Heterogeneity (variation) between results of different studies was evaluated by:
performing empirical evaluation through visual inspection of the overlap of CIs on the forest plot; poor overlap indicates heterogeneity;
using the Chi2 statistical test for heterogeneity (Higgins 2011);
using an I2 statistic, which evaluates variation between studies (Higgins 2011); if a value greater than 50% was found, substantial heterogeneity was assumed; or
using a random‐effects model or a fixed‐effect model.
Assessment of reporting biases
Publication bias was to be assessed using a funnel plot if 10 or more studies were identified for either of the two comparisons. A gap on either side of the graph would have indicated that some trials had not been found, often as the result of difficulties in locating unpublished trials. No within‐study reporting bias was assessed.
Data synthesis
The presence or absence of heterogeneity was considered before data from trials were pooled. When it was not appropriate to combine the data, primary studies were summarised in narrative form. Women with suspected appendicitis and women with NSAP were analysed separately.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis was planned, if appropriate and possible, with consideration of the following.
Age: Data were not presented that allowed this.
If substantive heterogeneity was seen, the review authors first confirmed the data, then considered:
whether meta‐analysis was warranted; and
whether a subgroup analysis should be completed.
The prespecified potential sources of heterogeneity were considered to explore possible explanations for variations in effects between trials and to guide interpretation of study findings, that is, location, method used to validate time to definitive diagnosis outcomes, location of pain and time of observation before intervention. We were aware of the limited value that interpretation of the causes of heterogeneity has after heterogeneity has been identified.
Protocol change: One of the planned subgroup analyses was changed to become one of the two comparisons.
Sensitivity analysis
A sensitivity analysis was planned to explore whether the results of any meta‐analysis were sensitive to the inclusion or exclusion of RCTs with the following characteristics.
Unpublished studies, as these studies may not have been peer‐reviewed and thus could be of lower quality (all studies were published manuscripts, and therefore this was not undertaken).
Studies with high risk of bias versus studies with low risk of bias.
Studies with no allocation concealment versus those with allocation concealment (this was not done, as most studies did not report on allocation concealment).
Studies in which men were included or women of postmenopausal age were included.
Studies that included participants who did not strictly meet the inclusion criteria (e.g. right‐sided pain) (added as a protocol change).
Results
Description of studies
Results of the search
This is an updated version of the original review, published in Issue 1, 2011, of The Cochrane Library (Gaitan 2011). A total of 2413 titles were reviewed (1010 new titles for this update). Of these, 74 were initially screened as RCTs (11 new titles for this update). Sixty‐four studies were excluded for various reasons. Finally, we identified 12 studies that met the inclusion criteria. See Figure 1 for details of the screening and selection process.
1.
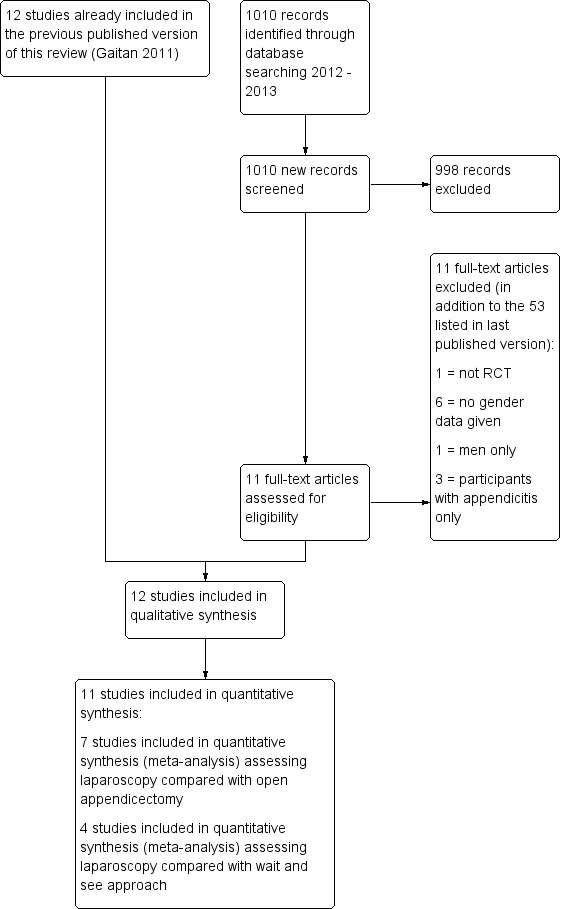
Study flow diagram.
Included studies
At the time of last publication in 2011, 12 studies met the inclusion criteria and were included in the review. No new studies were identified for inclusion in this updated review.
The main characteristics of the included studies are detailed in the table Characteristics of included studies. All studies were published manuscripts. A total of 12 trials from 11 countries were identified: Denmark (Olsen 1993), Kuwait (Jadallah 1994), Finland (Laine 1997), France (Champault 1993), United Kingdom (Decadt 1999), Sweden (Larsson 2001), Colombia (Gaitan 2002), Italy (Morino 2006; Navarra 2002), Saudi Arabia (Al‐Mulhim 2002), New Zealand (van Dalen 2003) and South Africa (Bruwer 2003).
Design: All included studies were randomised controlled trials
Settings: Ten studies were done in the Department of Surgery of a single hospital (Bruwer 2003; Champault 1993; Decadt 1999; Jadallah 1994; Laine 1997; Larsson 2001; Morino 2006; Navarra 2002; Olsen 1993; van Dalen 2003), one in the Department of Gynecology of a single hospital (Gaitan 2002) and one in a single hospital (Al‐Mulhim 2002).
Participants: We included 1020 participants, of whom only 29 (2.8%) were men. The male participants were from just one study (Decadt 1999). Six studies included women with suspected diagnosis of appendicitis (Al‐Mulhim 2002; Jadallah 1994; Larsson 2001; Navarra 2002; Olsen 1993; van Dalen 2003). One study (Laine 1997) included only participants with right‐sided pain, and five studies included women having non‐specific lower abdominal pain (Bruwer 2003; Champault 1993; Decadt 1999; Gaitan 2002; Morino 2006).
Interventions: Of the 12 included RCTs, eight compared laparoscopy with open appendicectomy (Al‐Mulhim 2002; Bruwer 2003; Jadallah 1994; Laine 1997; Larsson 2001; Navarra 2002; Olsen 1993; van Dalen 2003), and four compared laparoscopy versus a wait and see approach (Champault 1993; Decadt 1999; Gaitan 2002; Morino 2006).
Outcomes: Although most studies reported at least one prespecified primary outcome of this review, differences in the reporting and definition of outcomes were noted. Specific diagnosis and adverse events were not reported in four RCTs (Al‐Mulhim 2002; Bruwer 2003; Decadt 1999; Jadallah 1994). Total length of in‐patient stay was not reported in six RCTs (Al‐Mulhim 2002; Bruwer 2003; Decadt 1999; Gaitan 2002; Jadallah 1994; Larsson 2001).
Length of follow‐up: Participants were followed up until discharge from the institutions. Readmission was reported in one RCT (Bruwer 2003). Return to work (Bruwer 2003) and return to normal activities (Bruwer 2003; Laine 1997) were assessed in a few RCTs.
Ten trials were published in English, one in French (Champault 1993) and another in Italian (Navarra 2002).
Funding sources: One study described the source of funds (Gaitan 2002).
Excluded studies
A total of 63 studies were excluded (Excluded studies) for the following reasons: 32 included less than 75% women, and the authors did not provide additional data solely for women (including after written requests were made); five studies included only men, five included only children, 12 did not provide data about gender, five were excluded as they were considered to be non‐randomised or non‐controlled clinical trials and four studies were not included because only participants with a clear diagnosis of appendicitis were included (Excluded studies). The search of the ICTRP retrieved 1332 records, two of which were evaluated (ISRCTN42332281). One of them (NCT00908804) was completed and published but was finally excluded (Kouhia 2010) because only participants with confirmed appendicitis were inlcuded. None of the identified trials were eligible for the review.
Risk of bias in included studies
Overall the studies had a moderate risk of bias, mainly because allocation concealment or methods of sequence generation were not adequately reported. In addition, it was not clear whether follow‐up was similar for the treatment groups. The index test was incorporated as a reference standard in the laparoscopy group, and the differential verification or partial verification bias may have occurred in most RCTs (Figure 2; Figure 3).
2.
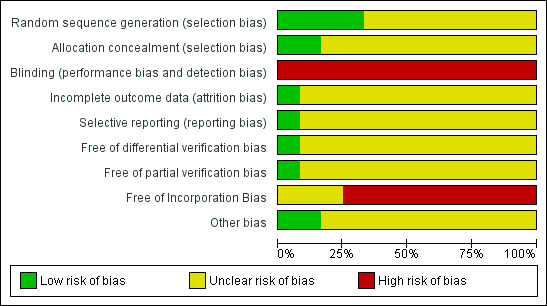
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.
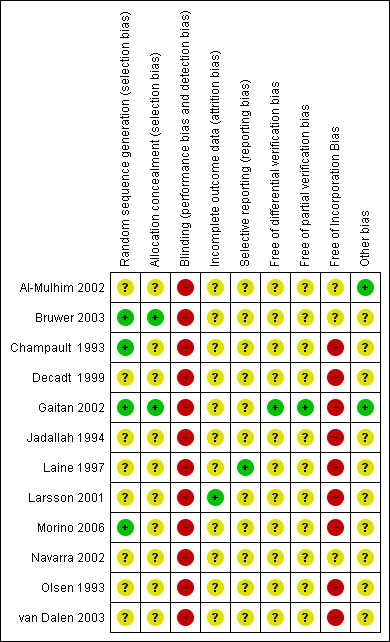
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
See the Characteristics of included studies for more information.
Allocation
Method of sequence generation: Four RCTs adequately reported the methods of generation of randomisation, attained by using a computer‐generated randomisation list (Bruwer 2003; Gaitan 2002; Morino 2006) or a random table with random numbers (Champault 1993). The other RCTs did not report how randomisation was performed.
Allocation concealment: Two RCTs adequately reported how allocation concealment was maintained (Bruwer 2003; Gaitan 2002). In both RCTs, allocation concealment was ensured using sealed, opaque, sequentially numbered envelopes. The other RCTs did not report how allocation concealment was performed and were rated as having unclear risk of bias .
Blinding
Blinding: All studies were open RCTs, and no blinding of participants, clinicians or researchers was reported.
Incomplete outcome data
Incomplete outcome data: All of the included studies were judged as having unclear risk, mainly because It was not clear whether follow‐up was similar in the two groups. Losses to follow‐up were reported in only three RCTS (less than 5%) (Champault 1993; Larsson 2001; van Dalen 2003). We had to impute standard deviations for the total length of in‐patient stay (Navarra 2002; Olsen 1993; van Dalen 2003) and mean operating time in three RCTs (Al‐Mulhim 2002; Navarra 2002; van Dalen 2003). Adverse outcomes and complications frequently were not defined and were not reported in different ways.
Selective reporting
In addition, only two RCTs were considered to be free of selective reporting bias (Champault 1993; Jadallah 1994).
When differential verification of bias and partial verification bias were reported, most studies were judged as having unclear risk of bias; only one study (Gaitan 2002) had low risk of bias. Most studies had high risk of bias when rating Incorporation bias; however, three studies (Al‐Mulhim 2002; Bruwer 2003; Navarra 2002) were judged as having unclear risk of bias.
Other potential sources of bias
In one study (Gaitan 2002), a definitive diagnosis was made by using the same reference standard for the comparison groups; all participants underwent the reference standard method.
Differential verification bias
When differential verification bias was assessed, most studies were judged as having unclear risk of bias; only one study (Gaitan 2002) had low risk of bias.
Partial verification bias
When partial verification bias was assessed, most studies were judged as having unclear risk of bias; only one study (Gaitan 2002) had low risk of bias.
Incorporation bias
When incorporation bias was assessed, almost all studies were judged as having unclear risk of bias; only one study (Gaitan 2002) had low risk of bias.
Effects of interventions
Comparison 1: laparoscopy compared with open appendicectomy
Specfic diagnosis before discharge: Meta‐analysis of seven studies (Bruwer 2003; Jadallah 1994; Laine 1997; Larsson 2001; Navarra 2002; Olsen 1993; van Dalen 2003) found that laparoscopy was associated with a higher rate of diagnosis before discharge (seven RCTs, 561 participants; OR 4.10, 95% CI 2.50 to 6.71; I2 = 18%) (Figure 4).
4.
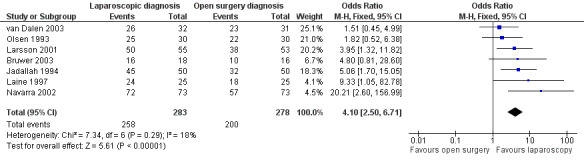
Forest plot of comparison: 1 Laparoscopy versus open appendicectomy, outcome: 1.1 Final diagnosis.
Any adverse events: No evidence was found of a difference in the rate of any adverse event favouring laparoscopy (eight RCTs, 623 participants; OR 0.46, 95% CI 0.19 to 1.10; I2 = 0%) (Figure 5).
5.
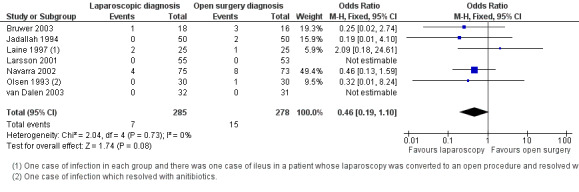
Forest plot of comparison: 1 Laparoscopy versus open appendicectomy, outcome: 1.2 Adverse events.
Total length of in‐patient stay (days): No evidence was found of a significant mean difference in total length of in‐patient stay (six RCTs, 455 participants; MD ‐0.07, 95% CI ‐0.63 to 0.49; I2 88%) (Figure 6) between groups; however, heterogeneity was high, and this result should be interpreted with caution. As standard deviations of total length of in‐patient stay were available in only three studies (Bruwer 2003; Jadallah 1994; Laine 1997), we imputed data for the three other studies (Navarra 2002; Olsen 1993; van Dalen 2003). The study by Laine et al (Laine 1997) was the only RCT in which the total length of in‐patient stay favoured open surgery.
6.
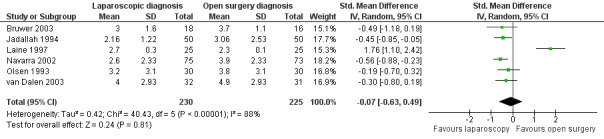
Forest plot of comparison: 1 Laparoscopy versus open appendicectomy, outcome: 1.3 Total length of in‐patient stay.
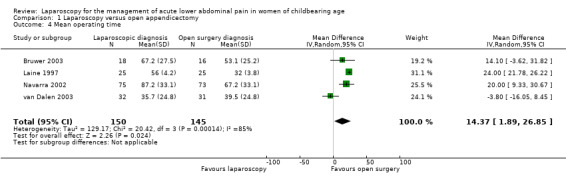
Mean operating time (minutes): Mean operating time was significantly lower in the open appendicectomy group (five RCTs, 355 participants; MD 14.55, 95% CI 3.62 to 25.48; I2 = 85%) (Figure 7); however, heterogeneity was high and this result should be interpreted with caution. Data were available in two studies (Bruwer 2003; Laine 1997), and we imputed data into three of the studies (Al‐Mulhim 2002; Navarra 2002; van Dalen 2003).
7.
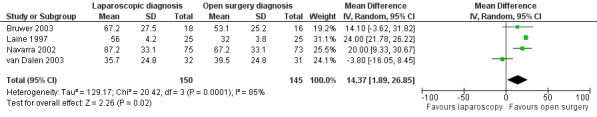
Forest plot of comparison: 1 Laparoscopy versus open appendicectomy, outcome: 1.4 Mean operating time.
Return to normal activities: Mean number of days to return to normal activities was significantly lower in the laparoscopic group (three RCTs, 144 participants; MD ‐5.09, 95% CI ‐5.56 to ‐4.61; I2 = 0%) (Analysis 1.5) (Al‐Mulhim 2002; Bruwer 2003; Laine 1997).
1.5. Analysis.
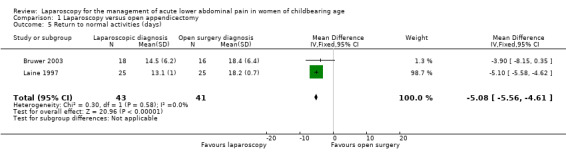
Comparison 1 Laparoscopy versus open appendicectomy, Outcome 5 Return to normal activities (days).
Rate of normal appendix removed: Meta‐analysis of seven studies revealed a significant difference favouring the laparoscopic procedure in the rate of normal appendix removed (seven RCTs, 475 participants; OR 0.13, 95% CI 0.07 to 0.24; I2 = 0%) (Figure 8; Analysis 1.6) (Al‐Mulhim 2002; Bruwer 2003; Jadallah 1994; Laine 1997; Larsson 2001; Olsen 1993; van Dalen 2003).
8.
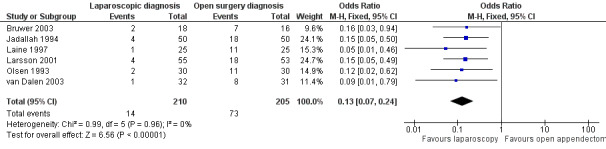
Forest plot of comparison: 1 Laparoscopy versus open appendicectomy, outcome: 1.7 Normal appendix removed.
1.6. Analysis.
Comparison 1 Laparoscopy versus open appendicectomy, Outcome 6 Normal appendix removed.
Mortality: Only one RCT (Bruwer 2003) explicitly reported no deaths in either group (Analysis 1.7).
1.7. Analysis.
Comparison 1 Laparoscopy versus open appendicectomy, Outcome 7 Mortality.
Sensitivity analysis
Navarra 2002 included women older than childbearing age. A sensitivity analysis removing this study did not affect the significance of results for the above analyses.
Laine 1997 included women with right‐sided pain only and therefore did not strictly meet the inclusion criteria for non‐specific pain. A sensitivity analysis removing this study did not affect the significance of results for the above analyses, with the exception of adverse events, which were then found to be reduced by laparoscopic surgery (OR 0.36, 95% CI 0.13 to 0.95).
See also Table 1.
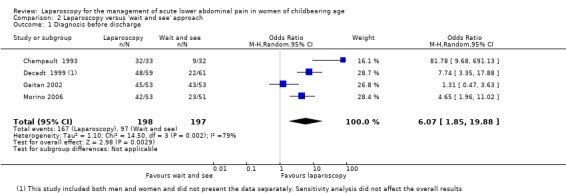
Comparison 2: laparoscopy compared with 'wait and see' strategy
Specific diagnosis before discharge: Meta‐analysis of four RCTs (Champault 1993; Decadt 1999; Gaitan 2002; Morino 2006) found a significant difference favouring laparoscopic diagnosis in the rate of diagnosis before discharge (four RCTs, 395 participants; OR 6.07, 95% CI 1.85 to 19.88; I2 = 79%) (Figure 9); however, heterogeneity was high, and findings should be interpreted with caution.
9.
Forest plot of comparison: 2 Laparoscopy versus 'wait and see' approach, outcome: 2.1 Final diagnosis.
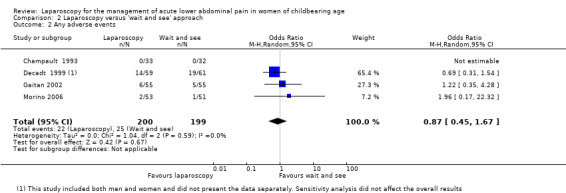
Any adverse events: No significant differences were found in the rates of adverse events (four RCTs, 399 participants; risk ratio (RR) 0.87, 95% CI 0.52 to 1.45; I2 = 0%) (Figure 10).
10.
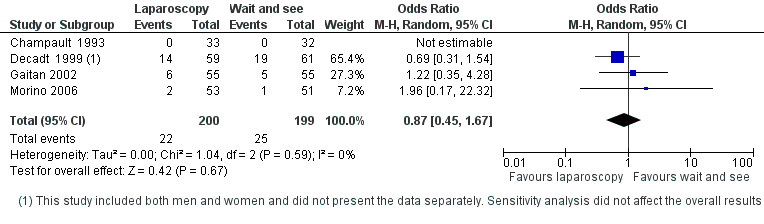
Forest plot of comparison: 2 Laparoscopy versus 'wait and see' approach, outcome: 2.2 Adverse events.
Total length of in‐patient stay (days): A significant difference favouring the laparoscopic group was found in the mean difference of the total length of in‐patient stay (two RCTs, 169 participants; MD ‐0.38, 95% CI ‐0.69 to ‐0.08; I2 = 49%) (Analysis 2.3) (Champault 1993; Morino 2006).
2.3. Analysis.
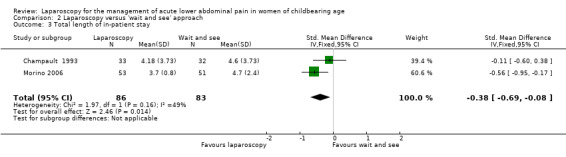
Comparison 2 Laparoscopy versus 'wait and see' approach, Outcome 3 Total length of in‐patient stay.
Mean operating time: No significant difference was reported in the mean operating time (Analysis 2.4) in one RCT (Morino 2006).
2.4. Analysis.
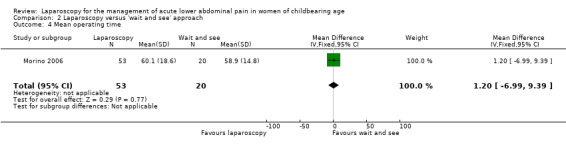
Comparison 2 Laparoscopy versus 'wait and see' approach, Outcome 4 Mean operating time.
Rate of normal appendix removed: A significant difference in the rate of normal appendix removed favouring the 'wait and see' strategy group was found in one study only (Morino 2006) (OR 5.14, 95% CI 2.22 to 11.87) (Analysis 2.5).
2.5. Analysis.
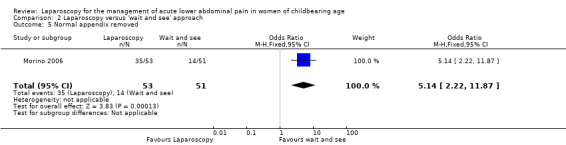
Comparison 2 Laparoscopy versus 'wait and see' approach, Outcome 5 Normal appendix removed.
Mortality: No significant difference between groups (Analysis 2.6) was reported in three RCTs (OR 1.03, 95% CI 0.06 to 16.93) (Decadt 1999;Gaitan 2002; Morino 2006).
2.6. Analysis.
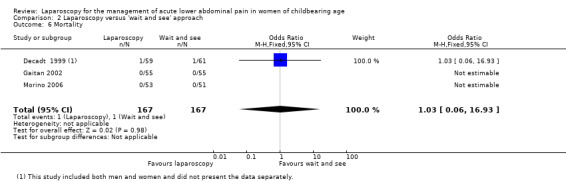
Comparison 2 Laparoscopy versus 'wait and see' approach, Outcome 6 Mortality.
Cost‐effectiveness: Only one study (Gaitan 2002) provided data about the cost‐effectiveness incremental ratio. Diagnostic laparoscopy was more cost‐effective in four of the five possible scenarios.
Quality of life: One study (Decadt 1999) evaluated a well‐being score at admission and six weeks later. This study showed greater improvement in the well‐being score in the laparoscopy group.
Sensitivity analysis:
In the study by Decadt 1999, 24% of the sample were men. A sensitivity analysis removing this study did not affect the significance of the results for the above analyses.
Assessments of the quality of the body of evidence: See also Table 2.
Discussion
Summary of main results
Laparoscopy is superior to both open appendicectomy (OA) and a wait and see strategy in the management of women of childbearing age with acute lower abdominal pain, as an increased rate of specific diagnosis before discharge is accompanied by shorter hospital stays. No significant differences were found in the rates of adverse events favouring laparoscopic appendicectomy (LA) when compared with open appendicectomy or the wait and see strategy. The rate of removal of normal appendices was reduced with laparoscopy compared with open appendicectomy, but the rate was increased when laparoscopy was compared with a wait and see strategy.
Overall completeness and applicability of evidence
Although reasonable numbers of RCTs and participants were included in the two comparisons included in this review, the data are incomplete for a number of clinically important outcomes. For example, data on return to normal activities are available for only two trials in the comparison of laparoscopy versus open appendicectomy; in the comparison of laparoscopy versus a wait and see approach, no data at all are available on this outcome.
The applicability of evidence outside the research setting is reasonable, as all of these studies were conducted in clinical settings that are quite similar. The comparisons described in the review are commonly undertaken and are not difficult to apply. Less than 3% of participants were men. The 12 trials came from Colombia, Italy, Finland, Sweden, Denmark, France, UK, Saudi Arabia, Kuwait, United Kingdom, New Zealand and South Africa.
However, reporting bias is a matter of some concern. See the section below on potential biases.
Quality of the evidence
Overall the studies were of moderate quality (see Table 1; Table 2), mainly because allocation concealment or methods of sequence generation were not adequately reported and no blinding was reported. In addition, it was not clear whether follow‐up was similar in the two treatment groups. The index test was incorporated as the reference standard in the laparoscopy group, and differential verification bias or partial verification bias may have occurred in most RCTs. Losses to follow‐up were less than 5%. Studies that compare OA versus LA are reported to have problems, including the variable expertise of operating surgeons, unclear definitions of complications, reluctance to remove macroscopically normal appendices, difficulty with blinding for postoperative outcomes and, finally, statistical problems with the sample size related to the exploratory nature of the studies (Kapischke 2006).
Most studies had poor reporting of baseline conditions of participants and other measurement bias in both groups of included studies. This limited assessment of the risk of bias. Another limitation for continuous outcomes was the need to provide standard deviations in a number of RCTs.
Potential biases in the review process
Reporting bias is a possibility in this review, as 33 studies of OA versus LA were not included because less than 75% of included participants were women and the trial authors were unable to provide data for women only. This means that the data presented in this review represent only a subset of the women included in clinical trials. It is unfortunate that we were not able to collect data on more women from the studies identified, but as most of these studies were older than 15 years, this was not possible in spite of our efforts. However, in a Cochrane review of laparoscopy versus open surgery for suspected appendicitis, four studies of unselected adults reported that laparoscopy was associated with a similar reduction in the rate of 'no diagnosis' (Sauerland 2010). This Cochrane review also reported a similar reduction in the number of normal appendices removed (Sauerland 2010).
Agreements and disagreements with other studies or reviews
A systematic review of early laparoscopy (within 24 hours of admission) versus conventional approaches for patients with acute abdominal pain (Maggio 2008) reported findings similar to those of our review, with a reduced rate of negative diagnoses before discharge (OR 0.13, 95% CI 0.03 to 0.51). In both this systematic review and our own, significant heterogeneity for this outcome was evident. Our review did not report evidence of a difference in complications between groups (OR 0.31, 95% CI 0.02 to 4.15).
Maggio 2008 included men and women, and one study included all causes of abdominal pain (Schietroma 2007). Another failed to include one RCT (Gaitan 2002). All of the included studies had high risk of selection and measurement bias—a fact that might overvalue the effect.
Open appendicectomy versus laparoscopic appendicectomy has been summarised in a Cochrane review (Sauerland 2010) and in another systematic review (Bennett 2007). Sauerland 2010 evaluated diagnostic performance in a subgroup of fertile women and reported that diagnostic laparoscopy reduced the number of unnecessary appendicectomies (RR 0.20, 95% CI 0.11 to 0.34) and the number of participants without a final diagnosis (RR 0.27, 95% CI 0.17 to 0.44). However, the systematic review by Bennett 2007 included 17 studies and did not find evidence of a statistical difference in the final diagnosis between LA and OA (OR 0.82, 95% CI 0.58 to 1.15), although the review concludes that hospital stay was shorter and risk of adverse events was reduced.
Finally, the systematic review by Li 2010 (Li 2010) did not evaluate the diagnostic performance of the two strategies and did not report a subgroup analysis of women (Li 2010).
Authors' conclusions
Implications for practice.
Laparoscopy should be the first strategy used in the management of women with acute lower abdominal pain as a specific diagnosis before discharge can be made with less time in hospital and earlier return to work.
Implications for research.
More high‐quality research is needed to determine the effectiveness of laparoscopy in specific cases (e.g. women with high body mass indices; when resources are scarce and access to the theatre is limited). Adverse events should also be investigated; several studies did not report AEs, and wide confidence intervals were presented in those that reported them (often regarded as a form of reporting bias).
What's new
| Date | Event | Description |
|---|---|---|
| 11 June 2014 | Review declared as stable | It is unlikely that there will be any new studies for inclusion in this review, and accordingly this is now a stable review. |
History
Protocol first published: Issue 2, 2009 Review first published: Issue 1, 2011
| Date | Event | Description |
|---|---|---|
| 22 October 2013 | New search has been performed | The search was updated and summary of findings tables were included in this version. No new studies were identified |
| 9 October 2013 | New citation required but conclusions have not changed | No new studies were identified for inclusion in this updated review |
| 26 February 2010 | Amended | Title change was made with approval of the editorial office from "Early laparoscopy versus clinical observation for the management of nonspecific acute abdominal pain in women of childbearing age" to " Laparoscopy for management of lower acute abdominal pain in women of childbearing age" as this reflected the clinical intervention better. Other protocol changes were made and are mentioned in the methods section. Some editing of the background also occurred. |
Acknowledgements
Cochrane Menstrual Disorders and Subfertility Group (MDSG) and Professor John Windsor, Department of Surgery, University of Auckland.
Appendices
Appendix 1. MEDLINE search
1 exp Abdomen, Acute/ (7951) 2 (acute abdominal adj5 pain).tw. (2285) 3 (pain adj5 abdomen).tw. (1099) 4 (pelvic adj5 pain).tw. (5988) 5 exp Pelvic Pain/ (5837) 6 (abdomin$ adj5 pain).tw. (35301) 7 exp Abdominal Pain/ (23423) 8 exp Appendicitis/ (14349) 9 exp pelvic infection/ or exp pelvic inflammatory disease/ (9210) 10 pelvic inflammat$ disease.tw. (3409) 11 PID.tw. (2604) 12 exp pregnancy, ectopic/ or exp pregnancy, abdominal/ or exp pregnancy, tubal/ (12306) 13 append$.tw. (40271) 14 exp Ovarian Cysts/ (14351) 15 (Ovar$ adj5 Cyst$).tw. (8132) 16 or/1‐15 (138947) 17 exp Laparoscopy/ (60772) 18 Laparoscop$.tw. (71334) 19 17 or 18 (80751) 20 exp diagnosis/ or exp "diagnostic techniques and procedures"/ or exp early diagnosis/ (5999808) 21 diagnos$.tw. (1467040) 22 (conventional or standard).tw. (738922) 23 (wait adj5 see).tw. (902) 24 (conservat$ or expectant).tw. (127271) 25 (clinical or observ$).tw. (3908721) 26 manage$.tw. (695438) 27 ultraso$.tw. (220084) 28 tomograph$.tw. (215687) 29 or/20‐28 (9458331) 30 16 and 19 and 29 (10318) 31 randomized controlled trial.pt. (333009) 32 controlled clinical trial.pt. (84725) 33 randomized.ab. (248446) 34 placebo.ab. (138145) 35 cross‐over studies/ (30040) 36 (crossover or cross‐over or cross over).tw. (54199) 37 clinical trials as topic.sh. (161434) 38 randomly.ab. (182056) 39 trial.ti. (106887) 40 or/31‐39 (816444) 41 humans.sh. (12444612) 42 40 and 41 (703668) 43 30 and 42 (790) 44 (2008$ or 2009$ or 2010$ or 2011$ or 2012$).ed. (4108570) 45 43 and 44 (224)
This search was updated in February and October 2013
Appendix 2. EMBASE search strategy
1 exp Abdomen, Acute/ (9462) 2 (acute abdominal adj5 pain).tw. (2858) 3 (pain adj5 abdomen).tw. (1521) 4 (pelvic adj5 pain).tw. (7983) 5 (abdomin$ adj5 pain).tw. (47290) 6 exp Abdominal Pain/ (72492) 7 exp Pelvis Pain Syndrome/ (8405) 8 or/1‐7 (109636) 9 Laparoscopy/ (44967) 10 Laparoscop$.tw. (93316) 11 (earl$ adj5 laparoscop$).tw. (2074) 12 or/9‐11 (104285) 13 8 and 12 (7697) 14 Controlled study/ or randomized controlled trial/ (3884819) 15 double blind procedure/ (109817) 16 single blind procedure/ (16128) 17 crossover procedure/ (34455) 18 drug comparison/ (81284) 19 placebo/ (201698) 20 random$.ti,ab,hw,tn,mf. (853728) 21 latin square.ti,ab,hw,tn,mf. (3282) 22 crossover.ti,ab,hw,tn,mf. (57206) 23 cross‐over.ti,ab,hw,tn,mf. (19099) 24 placebo$.ti,ab,hw,tn,mf. (280621) 25 ((doubl$ or singl$ or tripl$ or trebl$) adj5 (blind$ or mask$)).ti,ab,hw,tn,mf. (186278) 26 (comparative adj5 trial$).ti,ab,hw,tn,mf. (65629) 27 (clinical adj5 trial$).ti,ab,hw,tn,mf. (1030107) 28 or/14‐27 (4877370) 29 nonhuman/ (3877817) 30 animal/ not (human/ and animal/) (1332762) 31 or/29‐30 (5196477) 32 28 not 31 (3030627) 33 13 and 32 (1289) 34 (2010$ or 2011$ or 2012$).em. (2701351) 35 33 and 34 (280)
This search was updated in February and October 2013
Appendix 3. CINAHL search strategy
1 exp Abdomen, Acute/ 2 (acute abdominal adj5 pain).tw. 3 (pain adj5 abdomen).tw. 4 (pelvic adj5 pain).tw. 5 exp Pelvic Pain/ 6 (abdomin$ adj5 pain).tw. 7 exp Abdominal Pain/ 8 exp Appendicitis/ 9 exp pelvic infection/ or exp pelvic inflammatory disease/ 10 pelvic inflammat$ disease.tw. 11 PID.tw. 12 exp pregnancy, ectopic/ or exp pregnancy, abdominal/ or exp pregnancy, tubal/ 13 append$.tw. 14 exp Ovarian Cysts/ 15 (Ovar$ adj5 Cyst$).tw. 16 or/1‐15 17 exp Laparoscopy/ 18 Laparoscop$.tw. 19 17 or 18 20 exp diagnosis/ or exp "diagnostic techniques and procedures"/ or exp early diagnosis/ 21 diagnos$.tw. 22 (conventional or standard).tw. 23 (wait adj5 see).tw. 24 (conservat$ or expectant).tw. 25 (clinical or observ$).tw. 26 manage$.tw. 27 ultraso$.tw. 28 tomograph$.tw. 29 or/20‐28 30 16 and 19 and 29 31 exp clinical trials/ 32 Clinical trial.pt. 33 (clinic$ adj trial$1).tw. 34 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$3 or mask$3)).tw. 35 Randomi?ed control$ trial$.tw. 36 Random assignment/ 37 Random$ allocat$.tw. 38 Placebo$.tw. 39 Placebos/ 40 Quantitative studies/ 41 Allocat$ random$.tw. 42 or/31‐41 43 30 and 42 44 from 43 keep 1‐45
Appendix 4. CENTRAL search strategy
1 exp Abdomen, Acute/ (37) 2 (acute abdominal adj5 pain).tw. (50) 3 (pain adj5 abdomen).tw. (42) 4 (pelvic adj5 pain).tw. (451) 5 exp Pelvic Pain/ (510) 6 (abdomin$ adj5 pain).tw. (2203) 7 exp Abdominal Pain/ (781) 8 exp Appendicitis/ (299) 9 exp pelvic infection/ or exp pelvic inflammatory disease/ (399) 10 pelvic inflammat$ disease.tw. (218) 11 PID.tw. (209) 12 exp pregnancy, ectopic/ or exp pregnancy, abdominal/ or exp pregnancy, tubal/ (123) 13 append$.tw. (1030) 14 exp Ovarian Cysts/ (732) 15 (Ovar$ adj5 Cyst$).tw. (158) 16 or/1‐15 (5931) 17 exp Laparoscopy/ (3056) 18 Laparoscop$.tw. (4742) 19 17 or 18 (4912) 20 exp diagnosis/ or exp "diagnostic techniques and procedures"/ or exp early diagnosis/ (200845) 21 diagnos$.tw. (30344) 22 (conventional or standard).tw. (53697) 23 (wait adj5 see).tw. (62) 24 (conservat$ or expectant).tw. (3404) 25 (clinical or observ$).tw. (210273) 26 manage$.tw. (28619) 27 ultraso$.tw. (9253) 28 tomograph$.tw. (5013) 29 or/20‐28 (366147) 30 16 and 19 and 29 (552) 31 limit 30 to yr="2008 ‐Current" (124)
This search was updated in February and October 2013
Appendix 5. PsycINFO search strategy
1 exp Abdomen/ (441) 2 (acute abdominal adj5 pain).tw. (19) 3 (pain adj5 abdomen).tw. (46) 4 (pelvic adj5 pain).tw. (395) 5 append$.tw. (21917) 6 pelvic inflammat$ disease.tw. (59) 7 (Ovar$ adj5 Cyst$).tw. (24) 8 or/1‐7 (22857) 9 Laparoscop$.tw. (229) 10 8 and 9 (27) 11 random.tw. (35688) 12 control.tw. (277569) 13 double‐blind.tw. (16130) 14 clinical trials/ (6181) 15 placebo/ (3239) 16 exp Treatment/ (521145) 17 or/11‐16 (790334) 18 10 and 17 (15)
This search was updated in February and October 2013
Appendix 6. MDSG Specialised Register search strategy
Keywords CONTAINS "laparoscopic" or "laparoscopic excision" or "laparoscopic imaging" or "laparoscopic dye" or "laparoscopic imaging" or "laparoscopic procedure" or "laparoscopic surgery" or "laparoscopic techniques" or "laparoscopy" or Title CONTAINS "laparoscopic" or "laparoscopic excision" or "laparoscopic imaging" or "laparoscopic dye" or "laparoscopic imaging" or "laparoscopic procedure" or "laparoscopic surgery" or "laparoscopic techniques" or "laparoscopy"
AND
Keywords CONTAINS "acute" or "abdominal pain" or "pelvic pain" or "Pain‐abdominal" or "pain‐pelvic" or "ectopic pregnancy" or "pelvic inflammatory disease" or "Ovarian Cysts" or "ovarian cyst" or "acute" Title CONTAINS "acute" or "abdominal pain" or "pelvic pain" or "Pain‐abdominal" or "pain‐pelvic" or "ectopic pregnancy" or "pelvic inflammatory disease" or "Ovarian Cysts" or "ovarian cyst" or "acute"
Appendix 7. LILACS search strategy
Keywords conmtains ( abdominal pain) OR (acute abdominal pain) OR (pelvic pain) OR (acute pelvic pain) OR (pelvic inflammatory disease ) OR (ovarian cyst ) OR (appendicitis ) OR (appendicitis ) OR (non‐specific abdominal pain ) OR (lower abdominal pain ) AND (laparoscopy ) OR (diagnostic laparoscopy ) OR (videolaparoscopy ) OR laparotomy OR (clinical diagnosis ) OR (appendectomy ) OR (open appendectomy ) OR (laparoscopic appendectomy ) AND ( clinical trial) OR (randomized clinical trial) OR (controlled clinical trial)
Terms In spanish: dolor abdominal OR dolor abdominal agudo OR dolor pélvico OR dolor pélvico agudo OR apendicitis OR quiste de ovario OR enfermedad pélvica inflamatoria OR dolor abdominal no especifico AND laparoscopia OR laparoscopia diagnostica OR, laparotomía OR apendicectomia OR apendicetomia abierta, apendicectomia laparoscopica OR diagnostico clinico OR diagnostico convencional AND expermiento clinico OR experimento clinico aleatorizado OR experimento clinico controlado o experimental
Data and analyses
Comparison 1. Laparoscopy versus open appendicectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Diagnosis before discharge | 7 | 561 | Odds Ratio (M‐H, Fixed, 95% CI) | 4.10 [2.50, 6.71] |
| 2 Any adverse events | 7 | 563 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.19, 1.10] |
| 3 Total length of in‐patient stay | 6 | 455 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.63, 0.49] |
| 4 Mean operating time | 4 | 295 | Mean Difference (IV, Random, 95% CI) | 14.37 [1.89, 26.85] |
| 5 Return to normal activities (days) | 2 | 84 | Mean Difference (IV, Fixed, 95% CI) | ‐5.08 [‐5.56, ‐4.61] |
| 6 Normal appendix removed | 6 | 415 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.07, 0.24] |
| 7 Mortality | 1 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
Comparison 1 Laparoscopy versus open appendicectomy, Outcome 1 Diagnosis before discharge.
1.2. Analysis.
Comparison 1 Laparoscopy versus open appendicectomy, Outcome 2 Any adverse events.
1.3. Analysis.
Comparison 1 Laparoscopy versus open appendicectomy, Outcome 3 Total length of in‐patient stay.
1.4. Analysis.
Comparison 1 Laparoscopy versus open appendicectomy, Outcome 4 Mean operating time.
Comparison 2. Laparoscopy versus 'wait and see' approach.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Diagnosis before discharge | 4 | 395 | Odds Ratio (M‐H, Random, 95% CI) | 6.07 [1.85, 19.88] |
| 2 Any adverse events | 4 | 399 | Odds Ratio (M‐H, Random, 95% CI) | 0.87 [0.45, 1.67] |
| 3 Total length of in‐patient stay | 2 | 169 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.38 [‐0.69, ‐0.08] |
| 4 Mean operating time | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐6.99, 9.39] |
| 5 Normal appendix removed | 1 | 104 | Odds Ratio (M‐H, Fixed, 95% CI) | 5.14 [2.22, 11.87] |
| 6 Mortality | 3 | 334 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.06, 16.93] |
2.1. Analysis.
Comparison 2 Laparoscopy versus 'wait and see' approach, Outcome 1 Diagnosis before discharge.
2.2. Analysis.
Comparison 2 Laparoscopy versus 'wait and see' approach, Outcome 2 Any adverse events.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Al‐Mulhim 2002.
| Methods | Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Follow‐up at four weeks 60 participants recruited, 60 randomly assigned No data about participants excluded before random assignment Lost to follow‐up: no data on number of participants seen at four weeks' follow‐up 60 women analysed Single centre: King Fahad Hospital, Hofuf, Al‐Hassa, Kingdom of Saudi Arabia Enrolment between January 1999 and April 2000 Source of funding: not provided Ethical issues: consent form obtained for each participant Method to establish definitive diagnosis: visual examination of appendix and abdominal cavity and histopathological examination of appendix in laparoscopic group. Not clearly stated but in all participants appendix removed and sent for histopathological study in conventional group |
|
| Participants | Women with clinical diagnosis of acute appendicitis Included: patients with clinical diagnosis of acute appendicitis, patients suitable for a right iliac fossa muscle‐splitting approach to the appendix, patients suitable for laparoscopy with no evidence of pregnancy No exclusion criteria stated Mean age (SD): 23 years (14 to 35) in laparoscopy group, 26 years (14 to 42) in conventional group Weight: 54 kg (30 to 82) in laparoscopy group, 58 kg (35 to 90) in conventional group Mean serum white cell count: 12.8 (6.2 to 18.3) in laparoscopy group, 14.5 (8.2 to 19.6) in conventional group "Time of evolution of symptoms, median (range): 20 (6‐72) in laparoscopy group, 4 days (1‐80) in conventional group . of the pain (SD): 22.1 (± 5) in laparoscopy group, 21.5 (± 3) in the conventional group" |
|
| Interventions | Laparoscopic appendicectomy versus open appendicectomy Laparoscopic appendicectomy (group 1): three stab incisions required (a small midline incision was made at the umbilicus and a 10‐mm trocar was inserted, camera was inserted at this site); 5‐mm trocar below right costal margin and another five mm in the left iliac fossa of the abdomen placed under direct vision Open appendicectomy (group 2): carried out through a muscle‐splitting incisor in the right iliac fossa Surgeons participating in this study experienced in laparoscopic surgery; a Registrar with long general surgery experience usually performed open appendicectomy Non‐inflamed appendix removed at both laparoscopic and open surgery, even when a definitive cause of the participant's symptoms was found. Postoperative pain control for both groups: pethidine 1 g/kg every six hours if needed for the first 24 hours, then shifted to intramuscular Voltaren 75 mg per request. Discharge pain medicine: paracetamol tablets |
|
| Outcomes | Pathology findings: reported "Operating time (minutes)": stated in methods and reported Control of pain: number of doses of pethidine and Voltaren stated in methods and reported Mobilisation from bed: stated in methods and reported Reintroduction of liquid and solid diet: stated in methods and reported Return to normal activity: stated in methods and reported Complications: stated in methods and reported |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Text: states that participants were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | Text: states that a sealed envelope system was used |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. No loss to follow‐up reported |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | Unclear risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Low risk | Baseline characteristics reported |
Bruwer 2003.
| Methods | Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Time of follow‐up: four weeks, by phone or personal interview 34 women of 81 participants with appendicitis diagnosis; 47 not included because of exclusion criteria (41) or because a surgeon with laparoscopic skills was not available (4). No consent form given (2) No participants excluded after random assignment Participants lost to follow‐up: not clearly stated 34 women analysed Single centre: Department of Surgery, Tygeberg Hospital and University of Stellenbosch, South Africa Enrolment from April 1997 to March 2001 Source of funding: not stated Ethical issues: protocol approved by the Research Committee of the University of Stellenbosch. Signed consent form used Method to establish definitive diagnosis: visual examination of appendix in abdominal cavity (except in cases with McBurney or Lanz incision) and pathology when appendicectomy was performed |
|
| Participants | Women 15 to 45 years of age in whom appendicitis diagnosis was not associated with clinical signs of acute appendicitis and could not be excluded on clinical and ancillary grounds. Independent decision made that surgical exploration was necessary; informed consent given Exclusion criteria: compromised immune status, positive pregnancy test, major anaesthetic risk as a result of a systemic disease. Evidence of systemic sepsis or complicated appendicitis (peritonitis, or right iliac fossa mass) Mean age: not informed Mean temperature: not reported Mean serum white cell count: not reported Mean days of abdominal pain: not reported |
|
| Interventions | Open versus laparoscopic exploration Laparoscopic appendicectomy employed a three‐port technique. Initial subumbilical port (camera) placed following open access to the peritoneal cavity. Additional ports 5 mm suprapubically and 10 mm in the left iliac fossa Open surgical exploration via right iliac fossa or via abdominal midline incision at the discretion of the operating surgeon. Appendicectomy, if required, performed using conventional techniques. Appendix left intact if alternative pathology was found, except in participants undergoing exploration via McBurney or Lanz incision At least one of the study authors was present as surgeon or assistant during all procedures Appendicectomy performed when acute appendicitis was confirmed and when another pathology was not found to account for clinical presentation . |
|
| Outcomes | Operating time: defined as time from complete anaesthetic induction to skin closure; stated in methods and reported Postoperative stay: calculated as one night for each midnight spent in the hospital; stated in methods and reported Number of analgesic doses in each participant and analgesic days: stated in methods and reported Return to normal activities reported in days: stated in methods and reported Return to work: stated in methods and reported Adverse events: not clearly validated |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Envelope sequence prepared by uninvolved person from a computer‐generated randomisation list |
| Allocation concealment (selection bias) | Low risk | Treatment assigned by opening the next in a series of sequentially numbered envelopes containing instructions for open or laparoscopic appendicectomy |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. All randomly assigned participants analysed |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | Unclear risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | Baseline characteristics not reported |
Champault 1993.
| Methods | Randomisation based on a random table with random numbers Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Time of follow‐up: not stated 66 women among 187 patients with right iliac fossa non‐specific pain accomplished inclusion/exclusion criteria; 65 were randomly assigned No participants excluded after random assignment Participants lost to follow‐up: not clearly stated 65 women analysed Single centre: Surgery and Digestive Department, Jean Verdier Hospital, France Enrolment from September 1991 to August 1992 Source of funding: not stated Ethical issues: not stated Method used to establish definitive diagnosis: visual examination of appendix and abdominal cavity in laparoscopic group; not clearly stated in conventional group; appendices removed and evaluated histologically |
|
| Participants | 65 women with abdominal pain included Exclusion criteria: age younger than 16 years, menopause, pregnancy, previous appendicectomy, clear diagnosis of appendicitis, salpingitis and urinary infection |
|
| Interventions | Inmediate laparoscopy versus conventional method Group 1: laparoscopy in the first 24 hours after admission Group 2: laboratory and imaging tests in the first 24 hours of admission to explore genital, urinary and digestive systems. Those for whom no diagnosis was established after this time could undergo laparoscopy of second intention |
|
| Outcomes | Diagnostic approach: efficacy not defined; stated in methods and reported Complications: not defined; stated in methods and not reported Procedure time: stated in methods and not reported Surgical treatment in the same procedure: stated in methods Hospitalisation time: not stated in methods but reported |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Based on random table with random numbers |
| Allocation concealment (selection bias) | Unclear risk | Nothing stated in text about how concealment was preserved |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in both groups. All randomly assigned participants analysed |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available. Some primary outcomes not reported |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in both groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | All baseline characteristics not reported |
Decadt 1999.
| Methods | Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Follow‐up at six weeks 120 participants recruited, 120 randomly assigned 26 participants refused to enter the trial Lost from follow‐up: 12 participants in group 1 and 16 participants in group two did not answer the survey about well‐being scores at six weeks of discharge 120 participants analysed Single centre: Department of General Surgery, Norfolk and Norwich NHS Trust Hospital, Norwich, UK Enrolment between November 1995 and October 1998 Source of funding: not stated Ethical issues: text states only that informed consent was given Method to establish definitive diagnosis: visual examination of appendix and abdominal cavity and histological examination of the appendix in laparoscopic group. Not clearly stated in conventional group |
|
| Participants | Acute abdominal pain of less than seven days' duration; after examination and baseline investigations, diagnosis remained uncertain Tests: full blood count, measurement of urea, electrolytes, serum amylase, urine culture and pregnancy test in women of reproductive age. Chest and abdominal radiograph if indicated clinically Exclusion criteria: participants in whom surgery was required even if the exact diagnosis was uncertain 91 women and 29 men included: 43 women and 16 men in laparoscopy group and 48 women and 13 men in second group Median age in laparoscopy group: 28 years (16 to 84). Median age in conventional group: 29 years (16 to 62) Median weight: 64 kg (43 to 111) in laparoscopy group; 68 (46 to 134) in conventional group Median serum white cell count: 11,000 (5300 to 23,100) in laparoscopy group; 10,700 (3300 to 25,600) in conventional group |
|
| Interventions | Early laparoscopy performed in first 18 hours versus active observation Laparoscopy performed using an open Hasson technique for the first port placement in the umbilical area with one 5‐mm port in the midline suprapubic area and a third port if necessary When no abnormality identified at laparoscopy, appendicectomy performed Conventional method: information about this method not provided |
|
| Outcomes | Gastrointestinal and general well‐being: assessed on admission and after six weeks of follow‐up by means of combined Gastrointestinal Symptom Rating Scale (GSRS) and Psychological General Well Being Index (PGWB); stated in methods and reported Final diagnosis: reported. Duration of hospital stay: reported Radiological examinations: reported Complications: not validated, reported Readmission: reported Complications: reported Readmission rate: reported |
|
| User defined 1 | 76% of sample: women | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned by sealed envelopes: no further description about how randomisation was generated |
| Allocation concealment (selection bias) | Unclear risk | Paper: states only 'sealed opaque envelopes', nothing about whether they were sequentially numbered or when they were opened |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. All randomly assigned participants analysed. 28/120 did not answer the survey about well‐being scores at six weeks of discharge |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | All baseline characteristics not reported |
Gaitan 2002.
| Methods | Design of RCT: parallel clinical trial Power calculation: stated No blinding used Follow‐up at one week 110 participants recruited, 110 randomly assigned 20 participants excluded before random assignment Lost to follow‐up: eight participants. No information about how they were distributed between groups 110 women analysed Single centre: Instituto Materno Infantil en Bogota, Colombia. A tertiary care maternity and gynaecological hospital Enrolment between November 1997 and June 2000 Source of funding: Colombian Institute for the Development of Science and Technology, COLCIENCIAS Ethical issues: protocol and written consent approved by the Universidad Nacional de Colombia Ethics Committee Method used to establish definitive diagnosis: based on bacteriological cultures of endometrium and endocervix plus histopathological findings of endometrium plus visual examination in laparoscopic group and bacteriological cultures of endometrium and endocervix plus histopathological findings of endometrium plus visual examination or evolution of pain depending on whether participant had undergone laparotomy. Surgical samples sent for pathological study |
|
| Participants | Women between 18 and 45 years old who consulted because of non‐specific lower abdominal pain (NSLAP). NSLAP defined as one of the following: pain not proceeding in a classical course, or, after clinical history had been taken and physical examination, haemogram, urinalysis, pregnancy test and pelvic and transvaginal ultrasonography performed, two examiners did not agree on a diagnosis by the end of six hours of observation Excluded: participants in whom pathology in upper hemi‐abdomen is suspected, with background of peritonitis or intestinal surgery, with two or more intra‐abdominal surgeries, with evidence of urinary infection, kidney lithiasis, cholelithiasis, infectious colitis or irritable colon, with multiple organic dysfunction syndrome, septic shock or hypovolaemic shock, with chronic pelvic pain or pain of more than three months’ evolution, with possible intrauterine pregnancy and unharmed sac, participants weighing more than 100 kg and those with psychiatric disorders Mean age (SD): 27.6 years (± 6.7) in laparoscopy group, 30.2 years (± 6.7) in conventional group Mean temperature (SD): 36.7 °C (± 0.5) in laparoscopy group, 36.5 °C (± 0.9) in conventional group Mean serum white cell count (DS): 8771 (± 3418) in laparoscopy group, 10,253 (± 4029) in conventional group "Time of evolution of pain median (range): 3 days (1 ‐ 60) in laparoscopy group, 4 days (1 ‐ 80) in conventional group . of the pain (SD): 22.1 (± 5) in laparoscopy group, 21.5 (± 3) in the conventional group" Abdominal surgery background number of participants exposed (percentage): 27 (50.9%) in laparoscopy group and 20 (38.5%) in conventional group |
|
| Interventions | Laparoscopic diagnosis versus conventional diagnosis Laparoscopic diagnostic method defined as direct observation of the pelvic cavity with a Wolf laparoscope fitted with a video camera and zoom, a light source and the high‐flow insufflator that allows surgical procedures to be performed. IMI laparoscopy team is experienced in lower abdominal pain diagnosis. Laparoscopic diagnosis of inflammatory pelvic illness reached following Hager’s criteria. Diagnosis of ruptured ectopic pregnancy reached when a bluish mass was seen in the tube, whether associated with hemorrhagic material in the cul‐de‐sac or not Appendicitis and ovarian cyst diagnoses based on observing the changes described above visually. A healthy pelvis diagnosed when no alterations were found Conventional diagnosis method based on clinical assessment and laboratory tests. It could have included surgical interventions, such as precision laparotomy, performed by the IMI emergency team. Diagnosis of inflammatory pelvic illness reached when at least two of Hager's main criteria were present. Diagnosis of appendicitis reached when signs of swelling or necrosis noted. Diagnosis of ectopic pregnancy reached by means of ultrasonography and serial human chorionic gonadotropin determinations, or laparotomy. Ovarian cyst suspected when a mobile mass was detected during pelvic examination, or when an ovarian mass larger than 5 cm was found with laparotomy. Cyst showing active haemorrhage or haemorrhagic content interpreted as ruptured. If adnexae were twisted, torsion diagnosis was made. Diagnosis of a healthy pelvis reached only when no alterations were found in the pelvic organs during laparotomy Both methods compared with a complex standard determined by both histopathological and microbiological criteria and evolution of the underling pathology. Surgical pathology also taken into account. Endocervical samples taken in 109 of 110 women assigned to one of the two groups. Gram stain and N. gonorrhoeae, C. trachomatis, and Mycoplasma cultures were done. Endometrial sample taken for culture of these and other aerobic and anaerobic bacteria with a Pipelle curette after washing of the exocervix with a saline solution. Another sample taken for histopathological examination. Positive endocervical culture or positive endometrial culture of STD bacteria interpreted as PID. PID diagnoses with endometrial biopsies reached using Kiviat’s criteria for endometritis. Decidua, an arias stella reaction or hypersecretory changes used to diagnose ectopic pregnancy or complicated ovarian cysts. Surgical pathology and endometrium biopsies read by one of the study authors |
|
| Outcomes | Conclusive diagnoses: number of cases in which a final diagnosis was reached in each method. Clinical observation, ultrasonography, para‐clinical exams, and visual findings at laparoscopy or laparotomy taken into account; stated in methods and reported Accurate diagnoses: accuracy calculated by comparing each method with a standard; stated in methods and reported Length of in‐patient stay before diagnosis: included only the time elapsed between hospital admission and the beginning of surgical or medical treatment, or spontaneous relief of pain. Not clearly validated; stated in methods and reported . Procedural complications: caused by diagnostic intervention, delayed diagnosis or pain control before admission; stated in methods and reported |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation table |
| Allocation concealment (selection bias) | Low risk | Concealed in sealed, opaque, sequentially numbered envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. Eight of 110 lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Low risk | Definitive diagnosis done with the same reference standard in the two groups |
| Free of partial verification bias | Low risk | All participants undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Low risk | Baseline characteristics reported |
Jadallah 1994.
| Methods | Randomisation performed by using sealed envelopes containing management as specified Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Time of follow‐up: two weeks 100 participants randomly assigned No participants excluded after random assignment Participants lost to follow‐up: not clearly stated 100 women analysed Single centre: Department of Surgery, Mubarack Al‐Khabeer, a teaching hospital, Kuwait Enrolment: July 1988 to March 1990 Source of funding: not stated Ethical issues: study approved by the ethics committee of the faculty of medicine at Kuwait University Method used to establish definitive diagnosis: visual examination of appendix and abdominal cavity in laparoscopic group. Not clearly stated in conventional group. All removed appendices evaluated histologically |
|
| Participants | "Women of childbearing age with acute abdominal pain suggestive of acute appendicitis and laparotomy was thought to be indicated” Exclusion criteria: participants with cardiac and respiratory insufficiency, hemorrhagic diathesis, previous abdominal surgery, morbid obesity, intestinal obstruction and diffuse peritonitis or pregnancy beyond twelfth week excluded Mean age: not informed Mean temperature: not reported Mean serum white cell count: not reported Mean days of abdominal pain: not reported |
|
| Interventions | Laparoscopic appendicectomy versus conventional laparotomy and appendicectomy Study group: diagnostic laparoscopy. If laparoscopy showed overt signs of appendicitis, or if appendix could not be satisfactorily inspected, no cause of the condition identified and participant treated with laparotomy and appendicectomy Participants in whom the appendix showed no abnormality and in whom gynaecological condition could not explain the symptoms: no further operation performed Appendix considered inflamed if congested or turgid, if mesoappendix was tense or if flakes of pus were found on or around the appendix or in the paracaecal area All participants given one dose of gentamicin (80 mg) and metronidazole (500 mg) intravenously Laparoscopy done under general anaesthesia after the bladder had been emptied. Verrey's needle introduced through subumbilical stab incision, later used for the laparoscopy Manipulating probe inserted through another small incision in the right iliac fossa under direct vision All removed appendices examined histologically |
|
| Outcomes | Macroscopic diagnosis of the surgeon: stated in methods and reported Operating time (minutes): stated in methods and reported Hospitalisation time: stated in methods and reported Complications: stated and reported in methods Final diagnosis: reported only in a subset of participants |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Text: states only that participants were randomly allocated to two groups |
| Allocation concealment (selection bias) | Unclear risk | Text: states that a sealed envelope was opened in which management was specified |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. All randomly assigned participants analysed |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available. No definitive diagnosis reported in the conventional group |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | Baseline characteristics not reported |
Laine 1997.
| Methods | Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Time of follow‐up: not clearly stated 50 participants randomly assigned No data about how many participants excluded before random assignment Lost to follow‐up: no data 50 women analysed Single centre: Department of Surgery, Turku University Central Hospital, Finland Enrolment from January 1994 to June 1995 Source of funding: not stated Ethical issues: not clearly stated Method to establish definitive diagnosis: visual examination of appendix and abdominal cavity in laparoscopic group. Not clearly stated in conventional group |
|
| Participants | Women between 16 and 40 years of age with acute lower right quadrant abdominal pain entered into the study. All participants: normal ovarian function Exclusion criteria: not stated Mean age in laparoscopic group: 26.9 years (range 18 to 35 years); in conventional (open) group: 28.3 years (range 16 to 40 years). All removed appendices examined histologically |
|
| Interventions | Laparoscopic versus open appendicectomy "The laparoscopic operation was performed with the participants in the Trendelenburg position. A three‐trocar method was used; a 10‐mm periumbilical port for the optics, a 12‐mm port in the left fosse, and a 10‐mm port in the midclavicular line in the right upper quadrant of the abdomen for the instruments. A urinary catheter was used routinely in all participants in this group. Diagnostic laparoscopy was first performed" "If the appendix appeared to be normal and another cause for abdominal pain was found, the appendix was left in situ, but it was removed if no other evident cause for lower abdominal pain was found. If the appendix appeared inflamed, the tip of the appendix was grasped with a nontraumatic grasping instrument and the mesoappendix and the appendix itself were divided with an endoscopic stapling instrument. The laparoscopic operations were carried out by surgeons experienced in laparoscopic surgery. Patients were converted from laparoscopic to open appendectomies at the discretion of the surgeon; however, results for the converted patients were calculated in the laparoscopic group" Open appendicectomies performed via classical transverse muscle‐splitting incision. Stump of the appendix inverted into the cecum with a pursestring suture. All open operations performed by the surgical resident on duty. Both inflamed and non‐inflamed appendices removed in this group |
|
| Outcomes | Operative findings: not defined; stated in methods and reported Operative time (from skin incision to skin closure): stated in methods and reported Postoperative complications: not validated; stated in methods and reported Histological findings: not defined; stated in methods and reported Length of hospital stay: stated in methods and reported Number of days to return to work or normal activity: stated in methods and reported |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Text: states randomly assigned. No more description about how randomisation was generated |
| Allocation concealment (selection bias) | Unclear risk | Text: states nothing about how concealment was preserved |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. All randomly assigned participants analysed |
| Selective reporting (reporting bias) | Low risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in both groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | All baseline characteristics not reported |
Larsson 2001.
| Methods | Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Time of follow‐up: not stated 110 participants randomly assigned Two participants excluded after randomisation: one for no adherence to protocol, another because incomplete follow‐up evaluation Participants lost to follow‐up: not clearly stated 108 women analysed Single centre: Department of Surgery, Skaraborgs, Sjukhus, Sweden Enrolment from 1991 to 1995 Source of funding: not stated Ethical issues: protocol approved by regional ethics committee Method to establish definitive diagnosis: visual examination of appendix and abdominal cavity in laparoscopic group. Not clearly stated in conventional group. All removed appendices sent for pathological examination |
|
| Participants | "Women ages 15 to 47 years with clinical signs of acute appendicitis were included in the study. Before randomisation, the patients were examined by the surgeon on call, and also by the gynaecologist. Standard laboratory tests were performed on all patients. The surgeon decided whether the patient should be scheduled for appendectomy." Exclusion criteria: participants with diffuse peritonitis or with suspicion of gynaecologic disease or pregnancy and women with severe adipositas, known intra‐abdominal adhesions and severe cardiovascular disease Mean age (SD): 24.9 (± 8) in laparoscopy group, 25 (± 8) in conventional group Mean temperature (SD): 37.9 °C (± 0.7) in laparoscopy group, 37.7 ºC (± 0.6) in conventional group Mean serum white cell count (DS): 128,000 (± 4200) in laparoscopy group, 13,100 (± 3700) in conventional group Mean days of abdominal pain (SD): 1.7 (± 1.1) in laparoscopy group, 1.9 (± 1.8) in conventional group Mean CRP (SD): 65.9 ± 51.5 in laparoscopy group, 41 ± 35.6 in conventional group |
|
| Interventions | "In the conventional group (open surgery according to current routines), the appendix was removed. In the case of a healthy appendix, the gynaecologist was called, but the laparoscopy was performed by both the gynaecologist and surgeon on call together. If the appendix was considered inflamed, or if it could not be visualized, the surgeon performed the appendectomy by the standard right lower quadrant incision. If the appendix was considered normal, it was left in situ" All participants given preoperative metronidazole 1 suppository rectally All removed appendices sent for pathological examination |
|
| Outcomes | Accuracy in diagnosing appendicitis: not defined or stated in methods, only reported Final diagnosis: not defined or stated in methods, only reported |
|
| User defined 1 | ||
| Notes | No data on adverse events | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random assignment by sealed envelopes in blocks of 10: no further description about how randomisation was generated |
| Allocation concealment (selection bias) | Unclear risk | Paper: states only 'sealed envelopes', nothing about whether they were sequentially numbered or when they were opened |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Not clear whether follow‐up was similar in the two groups. 2/110 lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | All baseline characteristics not reported |
Morino 2006.
| Methods | Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Follow‐up: at one week, three and 12 months 104 participants recruited, 104 randomly assigned 31 participants excluded before random assignment Lost to follow‐up at three months: five in each group; at 12 months: nine in the laparoscopy group and seven in the conventional group 104 women analysed "Single centre: from the Chirurgia Generale II e Centro di Chirurgia Mini Invasiva Department of Surgery, University of Turin, Turin, Italy" Enrolment between January 2001 and February 2004 Source of funding: not stated Ethical issues: specific informed consent form approved by our institution’s ethics committee Method used to establish definitive diagnosis based on visual examination and surgical pathology when the appendix was removed or bacteriological test of abdominal fluid, if present, in laparoscopic group. Not clearly stated in conventional group |
|
| Participants | Women between 13 and 45 years of age with non‐specific abdominal pain (NSAP) defined as abdominal pain lasting longer than six hours and less than seven days with uncertain diagnoses after clinical examination and baseline investigations, including full blood count, blood urea, amylase and bilirubin, serum electrolytes, urinalysis, pregnancy test, abdominal radiograph and abdominal US. Abdominal pain localised or prevalent in right iliac or suprapubic areas, not accompanied by fever, leucocytosis or clinical signs of peritonitis or haemodynamic instability or other obvious clinical presentation requiring urgent intervention "Exclusion criteria: previous appendectomy or major abdominal surgery, pregnancy, diagnosis of malignancy or chronic disease, contraindications to pneumoperitoneum, patient’s refusal to enter the study and precise diagnoses of: acute appendicitis, inflammatory bowel disease, ectopic pregnancy, endometriosis, urinary infection, renal colic, ovarian cyst, uterine fibroma and IUD associated endometritis after baseline investigations" Mean age (SD): 23.7 years (± 7) in laparoscopy group, 23.2 years (± 6) in conventional group Mean temperature (SD) 36.9 °C (± 0.5) in laparoscopy group, 36.8 °C (± 0.6) in conventional group Mean serum white cell count (DS): 8200 (± 1850) in laparoscopy group, 8730 (± 1600) in conventional group Mean body mass index (SD): 22.1 kg/m2 (± 5) in laparoscopy group, 21.5 (± 3) in conventional group |
|
| Interventions | "Laparoscopic diagnosis in the first 12 hours versus active clinical observation during 48 hours" Laparoscopy performed using an open Hasson technique for the first port placement in the umbilical area. Once 12 mmHg CO2 pneumoperitoneum was created, 2 5‐mm trocars inserted into midline suprapubic area and left iliac area. Abdominal cavity accurately explored in all participants, including complete mobilisation of entire small bowel. When no abnormality identified at laparoscopy, appendicectomy performed whenever serous fluid was present in the abdominal cavity; fluid aspirated and sent for microbiological testing. Attempt made to treat laparoscopically all surgical pathologies diagnosed at laparoscopy Participants randomly assigned to active clinical observation admitted to the surgical ward. Complete clinical examination repeated twice a day, baseline tests repeated at 24 and 48 hours from admission and on the basis of participant's clinical evolution. Once diagnosis was made, treatment immediately started. In the presence of persistent or worsening pain at 48 hours from admission, laparoscopic procedure undertaken. Participants in whom clinical symptoms progressively weakened and finally disappeared before a precise diagnosis were dismissed undiagnosed. Nine participants sent to vaginal ultrasound, four to CT scan, three to plain abdominal radiography and one to abdominal RNM Method used to obtain a definitive diagnosis: visual diagnosis and histopathology for appendicitis, microbiology test for abdominal liquid in laparoscopy group. Visual diagnosis in participants with worsening of pain; if pain disappeared, they were dismissed undiagnosed |
|
| Outcomes | Primary outcomes: number of definitive diagnoses Adverse events: stated in methods and reported "Secondary outcomes: hospitalization time prior of laparoscopy in hours, Mean operative time (minutes), Time of follow up time in months, final hospitalization time in days, patient without diagnosis, laparotomy or abdominal cavity visualization required"; stated in methods and reported |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate: randomisation performed by means of sealed opaque envelopes containing computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Paper: states only sealed opaque envelopes. No mention whether sequentially numbered or when opened |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not in cases of participants dismissed undiagnosed. No loss to follow‐up reported |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done using the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as reference standard in the laparoscopic group |
| Other bias | Unclear risk | All baseline characteristics not reported |
Navarra 2002.
| Methods | Design of RCT: parallel clinical trial Power calculation: not stated No blinding used Follow‐up: not stated 148 participants recruited, 148 randomly assigned No participants refused to enter the trial Lost to follow‐up: 12 participants in laparoscopy group and 15 participants in conventional group 148 participants analysed Single centre: l'Istituto di Clinica Chirurgica Generale e Terapia Chirurgica del l'Universita di Ferrara Enrolment between October 1993 and December 1998 Source of funding: not stated Ethical issues: not stated Method used to establish definitive diagnosis: visual examination of appendix and abdominal cavity in laparoscopic group. Not clearly stated in conventional group |
|
| Participants | Women with suspected clinical diagnosis of appendicitis Exclusion criteria: not stated Median age in laparoscopy group: 26.3 years (15 to 77). Median age in conventional group: 29.6 years (15 to 75) |
|
| Interventions | Laparoscopic appendicectomy versus open appendicectomy (conventional) Laparoscopy performed with participant in lithotomy modified position. Verres needle inserted into umbilical area, followed by a a 10‐mm port for placement of the video camera. Complete review of the abdominal cavity performed to confirm the clinical diagnosis or to determine associated cause of the pain. If peritoneal liquid was found, sample of peritoneal liquid was taken. When no abnormality was identified at laparoscopy, appendicectomy was performed Conventional method: McBurney incision performed in open appendicectomy |
|
| Outcomes | Duration of procedure: stated in methods and reported Postoperative pain: stated in methods and reported Duration of hospital stay: stated in methods and reported Intraoperative and postoperative complications: stated in methods and reported Histopathological diagnosis: stated in methods and reported |
|
| User defined 1 | ||
| Notes | A not clearly defined group of the recruited women: older than 50 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned by using a randomisation list |
| Allocation concealment (selection bias) | Unclear risk | No further description provided |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. 12 participants in the laparoscopy group and 15 participants in the control group were lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | Unclear risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | Not all baseline characteristics reported |
Olsen 1993.
| Methods | Design of RCT: parallel‐group clinical trial Power calculation: not stated No blinding used Time of follow‐up: not stated 60 women among 151 patients with diagnosis of appendicitis. 91 not included because of exclusion criteria or because a surgeon with laparoscopic skills was not available No participants excluded after random assignment Participants lost to follow‐up: not clearly stated 60 women analysed Single centre: Department of Surgery, Kolding County Hospital, Kolding, Denmark Enrollment from 1 January 1988 to 26 November 1991 Source of funding: not stated Ethical issues: approved by the local ethics committee Method to establish definitive diagnosis: visual examination of appendix in laparoscopic group. Not clearly stated in conventional group |
|
| Participants | "Women aged 15‐56 years with clinical signs of acute appendicitis were studied" Participants with signs of diffuse peritonitis, with a previous diagnosis of diffuse peritonitis and with more than two previous lower laparotomies excluded Mean age (range), years: 25.3 (15 to 54) in laparoscopy group, 25.8 (15 to 56) in direct operation |
|
| Interventions | Laparoscopy versus direct operation Appendicectomy performed through a transverse incision in the right iliac fossa Laparoscopy performed under general anaesthesia: no other data provided Appendicectomy performed when acute appendicitis was confirmed and when a diagnosis of appendicitis could not be excluded Appendicitis excluded if a normal appendix could be seen throughout its length. If other abnormalities were found, appropriate treatment given |
|
| Outcomes | Postoperative stay: not defined; stated in methods and reported Complications and readmission: not validated; stated in methods and reported Final diagnosis: only reported |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Text: trial performed in a randomised fashion. No other description provided about how randomisation was generated |
| Allocation concealment (selection bias) | Unclear risk | Text: nothing stated about how concealment was achieved |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. All randomly assigned participants analysed |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in both groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | All baseline characteristics not reported |
van Dalen 2003.
| Methods | Randomisation by closed envelope system Design of RCT: parallel clinical trial Power calculation: not stated No blinding used "Time of follow up: only in patients in whom an appendectomy was not performed was undertaken in September 2001" 63 women of 163 participants with appendicitis diagnosis No participants excluded after random assignment Participants lost to follow‐up: not clearly stated 60 women analysed Single centre: Department of Surgery, Christchurch Hospital, Christchurch, New Zealand Enrolment from July 1991 to July 1992 Source of funding: not stated Ethical issues: ethical approval obtained from the Canterbury Ethics Committee Method used to establish definitive diagnosis: visual examination of appendix and abdominal cavity and histopathological examination of appendix when removed in laparoscopic group. Not clearly stated in conventional group, but in all participants, appendix removed and sent for histopathological study |
|
| Participants | "Female patients aged between 16 and 45 years with a clinical diagnosis of acute appendicitis were eligible for inclusion in the study. Suitable patients in whom a decision had been made to proceed to appendectomy were asked to participate in the study. They were excluded if informed consent was not obtained, or if laparoscopy was contraindicated" Mean age (range): 24 years (16 to 45) in laparoscopy group, 22 years (16 to 51) in conventional group Mean temperature (range): 37.3 °C (36 to 38.4) in laparoscopy group, 37 °C (35.2 to 39.5) in conventional group Mean serum white cell count (range): 13,000 (4200 to 21,500) in laparoscopy group, 13,100 (7100 to 22,000) in conventional group Duration of pain (range): 35.5 days (five to 120) in laparoscopy group and 43.3 days (six to 168) in conventional group |
|
| Interventions | Laparoscopy first or open appendicectomy performed directly If appendix clearly seen and looking normal, no appendicectomy carried out. If other pathology seen, this was dealt with appropriately. If inflamed appendix seen or evidence thereof, or if appendix could not be seen, open appendicectomy carried out Those assigned to appendicectomy group: routine open appendicectomy and other pathology dealt with as necessary |
|
| Outcomes | Mean operating time: not defined or stated in methods, only reported Total days of stay: not defined or stated in methods, only reported Median postoperative stay: not defined or stated in methods, only reported Diagnostic accuracy: not defined or stated in methods, only reported |
|
| User defined 1 | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only mentioned the word "randomised". No further description provided |
| Allocation concealment (selection bias) | Unclear risk | Publication: states that sealed envelopes were used |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open RCT |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clear whether follow‐up was similar in the two groups. Three of 63 lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study not available |
| Free of differential verification bias | Unclear risk | Definitive diagnosis not done with the same reference standard in the two groups |
| Free of partial verification bias | Unclear risk | Non‐random set of participants not undergoing the reference standard |
| Free of Incorporation Bias | High risk | Index test incorporated as the reference standard in the laparoscopic group |
| Other bias | Unclear risk | All baseline characteristics not reported |
Abbreviations
CT = computed tomography.
GSRS = Gastrointestinal Symptom Rating Scale.
IUD = intrauterine device.
NSAP = non‐specific abdominal pain.
NSLAP = non‐specific lower abdominal pain.
PGWB = Psychological General Well Being Index.
PID = pelvic inflammatory disease.
RCT = randomized controlled trial.
SD = standard deviation.
STD = sexually transmitted disease.
US = ultrasonography.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Attwood 1992 | No data about gender were given |
| Bauwens 1998 | Only 56% of the sample were women |
| Cho 2011 | is not a RCT |
| Clarke 2011 | No data about gender were given; obese participants |
| Cox 1996 | No women were included |
| de Wilde 1991 | Only patients with histopathological and clinical diagnosis of appendicitis were included. The outcome was adhesion formation after open or laparoscopic appendectomy |
| Eichen 1994 | Only 63% of the sample were women |
| Frazee 1994 | Only 52% of the sample were women |
| Goudar 2011 | No data about gender were given for analysis |
| Hansen 1996 | Only 65% of the sample were women |
| Hart 1996 | Only 38% of the sample were women |
| Hebebrand 1994 | Only 53% of the sample were women |
| Heikkinen 1998 | Only 48% of the sample were women |
| Hellberg 1999 | No data about gender |
| Helmy 2001 | Only males were included |
| Henle 1996 | Only 51% of the sample were women |
| Huang 2001 | Only 45% of the sample were women |
| Ignacio 2004 | Only males were included |
| Kald 1999 | Only 50% of the sample were women |
| Kaplan 2009 | No data about gender were given |
| Karadayi 2003 | Only 43% of the sample were women |
| Kargar 2011 | No data about gender in the analysis |
| Kazemier 1997 | Only 45% of the sample were women |
| Khalil 2013 | No data about gender in the analysis |
| Koluh 2010 | No data about gender in the analysis |
| Kouhia 2010 | Only patients with confirmed appendicitis |
| Kum 1993 | Only 69% of the sample were women |
| Lavonius 2001 | Only children were included |
| Lejus 1996 | Only children were included |
| Lintula 2004 | Only children were included |
| Little 2002 | Only children were included |
| Long 2001 | No data about gender given |
| Macarulla 1997a | 57% of the sample were women |
| Martin 1995 | Only 41% of the sample were women |
| McAnena 1992 | Only 57% of the sample were women |
| Meynaud‐Kraemer 1999 | This is a meta‐analysis of RCTs in order to evaluate wound infection after open or laparoscopic appendectomy |
| Minne 1997 | Only 38% of the sample were women |
| Moirangthem 2008 | No data about gender given for analysis |
| Mutter 1996 | Only men were included |
| Nordentoft 2000 | No data about gender given |
| Ortega 1995 | Only 29% of the sample were women |
| Ozmen 1999 | Only 54% od the sample were women |
| Pedersen 2001 | Only 53% of the sample were women |
| Perner 1999 | Only 73% of the sample were women, no clinical outcomes |
| Reiertsen 1997 | Only 32% of the sample were women |
| Schietroma 2007 | Only 56% of patients were women. An unstated percentage of patients were older than 45 years old |
| Schippers 1994 | 58% of the sample were women |
| Settmacher 1995 | 56% of the sample were women |
| Sezeur 1997 | Only 31% of the sample were women |
| Shirazi 2010 | Alternate randomization; no gender analysis |
| St Peter 2011 | children < 18 with perforated appendictis |
| Stare 1998 | 53% of the sample were women |
| Tate 1993 | Only 39% of the sample were women |
| Tzovaras 2010 | Only in men |
| Vallribera 2003 | 34% of the sample were women |
| Wei 2010 | Only patients with confirmed appendicitis were included |
| Williams 1996 | Only 24% of the sample were women |
| Witten 1998 | 41% of the sample were women |
| Yeung 1997 | No data about gender given |
| Zaninotto 1995 | It is a non‐randomised clinical trial. Patients were allocated according to the ability of surgeon on duty to perform laparoscopy |
| Zhang 1998 | 41% of the sample were women |
Characteristics of ongoing studies [ordered by study ID]
ISRCTN42332281.
| Trial name or title | Laparoscopic excision versus open appendectomy: multi‐centre, randomised, double‐blind, controlled trial |
| Methods | Allocation: random, no further details Blindness: double‐blind, no further details Duration: six years Design: parallel |
| Participants | Diagnosis: suspected acute appendicitis N = 386, participant age: 18 years and older Sex: unclear |
| Interventions | Conventional open appendicectomy versus laparoscopic appendicectomy |
| Outcomes | Postoperative pain (cm visual analogue scale (VAS), number of analgesic doses) Secondary outcomes:
|
| Starting date | 01/01/2006 |
| Contact information | Dr Luca Ansaloni Unit of Emergency Surgery, Sant'Orsola‐Malpighi Hospital Via Massarenti 9. lansaloni@orsola‐malpighi.med.unibo.it |
| Notes | Accessed 10 May 2014 |
Differences between protocol and review
At full review stage in 2011 the primary outcome was changed from the number of definitive diagnoses (the number of cases in which a final diagnosis was reached for each strategy studied) to the number of specific diagnoses made before discharge. One secondary outcome was removed from those in the published protocol: time from admission to diagnosis. Three secondary outcomes were added: mean operating time, return to normal activities, and normal appendix removed.
Changes made to the published protocol also included replacement of the conventional strategy by 'wait and see' or by open appendicectomy and inclusion of women with suspected appendicitis.
At the 2014 update of this review the secondary outcome 'normal appendix removed' was moved to be included in the primary outcome 'adverse events', and the included studies now specify inclusion of trials where at least 75% of the participants were women of premenopausal age.
Contributions of authors
HGG: participated in conceiving of and designing the study, drafting the review and commenting on it critically for intellectual content and providing final approval of the document to be updated.
LR: participated in drafting the review and commenting on it critically for intellectual content and providing final approval of the document to be updated.
CF: participated in conceiving of and designing the study, drafting the review and commenting on it critically for intellectual content and providing final approval of the document to be updated.
VME: participated in preparing this update of the review, evaluating all titles and abstracts that were found, assessing the full text of studies and reviewing the manuscript.
Sources of support
Internal sources
Cochrane Menstrual Disorders and Subfertility Group (MDSG), Not specified.
External sources
Universidad Nacional de Colombia, Not specified.
Declarations of interest
One of the review authors (Gaitán H) was a principal investigator in an included study (Gaitan 2002). This study was financed by the Colombian Institute for Development of Science and Technology Colciencias (http://zulia.colciencias.gov.co:8098/protocol/index.jsp) (Grant No: 075‐97).
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Al‐Mulhim 2002 {published data only}
- Al‐Mulhim AS, Al‐Mulhim FM, Al‐Suwaiygh AA, Al‐Masaud NA. Laparoscopic versus open appendectomy in females with a clinical diagnosis of appendicitis. Saudi Medical Journal 2002;23(11):1339‐42. [PUBMED: 12506292] [PubMed] [Google Scholar]
Bruwer 2003 {published data only}
- Bruwer F, Coetzer M, Warren BL. Laparoscopic versus open surgical exploration in premenopausal women with suspected acute appendicitis. South African Journal of Surgery. Suid‐Afrikaanse Tydskrif vir Chirurgie 2003;41(4):82‐5. [PUBMED: 14768141] [PubMed] [Google Scholar]
Champault 1993 {published data only}
- Champault G, Rizk N, Lauroy J, Olivares P, Belhassen A, Boutelier P. Right iliac fossa pain in women. Conventional diagnostic approach versus primary laparoscopy. A controlled study (65 cases) [Douleurs iliaques droites de la femme. Approche diagnostique conventionnelle versus laparoscopie pre,iere. Etude controlee (65 cas)]. Annales de Chirugie 1993;47(4):316‐9. [PubMed] [Google Scholar]
Decadt 1999 {published data only}
- Decadt B, Sussman L, Lewis MP, Secker A, Cohen L, Rogers C, et al. Randomized clinical trial of early laparoscopy in the management of acute non‐specific abdominal pain. The British Journal of Surgery 1999;86(11):1383‐6. [DOI] [PubMed] [Google Scholar]
Gaitan 2002 {published data only}
- Gaitán H, Angel E, Sánchez J, Gómez I, Sánchez L, Agudelo C. Laparoscopic diagnosis of acute lower abdominal pain in women of reproductive age. International Journal of Gynaecology and Obstetrics 2002;76(2):149‐58. [DOI] [PubMed] [Google Scholar]
Jadallah 1994 {published data only}
- Jadallah FA, Abdul‐Ghani AA, Tibblin S. Diagnostic laparoscopy reduces unnecessary appendicectomy in fertile women. The European Journal of Surgery = Acta Chirurgica 1994;160(1):41‐5. [PUBMED: 8186313] [PubMed] [Google Scholar]
Laine 1997 {published data only}
- Laine S, Rantala A, Gullichsen R, Ovaska J. Laparoscopic appendectomy—is it worthwhile? A prospective, randomized study in young women. Surgical Endoscopy 1997;11(2):95‐7. [DOI] [PubMed] [Google Scholar]
Larsson 2001 {published data only}
- Larsson PG, Henriksson G, Olsson M, Boris J, Ströberg P, Tronstad SE, et al. Laparoscopy reduces unnecessary appendicectomies and improves diagnosis in fertile women. A randomized study. Surgical Endoscopy 2001;15(2):200‐2. [DOI] [PubMed] [Google Scholar]
Morino 2006 {published data only}
- Morino M, Pellegrino L, Castagna E, Farinella E, Mao P. Acute nonspecific abdominal pain: a randomized, controlled trial comparing early laparoscopy versus clinical observation. Annals of Surgery 2006;244(6):881‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Navarra 2002 {published data only}
- Navarra G, Ascanelli S Turini A, Carcoforo P, Tonini G, Pozza E. Laparoscopic appendectomy versus open appendectomy in suspected acute appendicitis in female patients [Appendicectomia laparoscopica versus appendicectomia aperta nel sospetto di appendicite acuta in pazienti di sesso femminile]. Annali Italiani di Chirurgia 2002;73:59‐64. [PubMed] [Google Scholar]
Olsen 1993 {published data only}
- Olsen JB, Myrén CJ, Haahr PE. Randomized study of the value of laparoscopy before appendicectomy. The British Journal of Surgery 1993;80(7):922‐3. [DOI] [PubMed] [Google Scholar]
van Dalen 2003 {published data only}
- Dalen R, Bagshaw PF, Dobbs BR, Robertson GM, Lynch AC, Frizelle FA. The utility of laparoscopy in the diagnosis of acute appendicitis in women of reproductive age. Surgical Endoscopy 2003;17(8):1311‐3. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Attwood 1992 {published data only}
- Attwood SE, Hill AD, Murphy PG, Thornton J, Stephens RB. A prospective randomized trial of laparoscopic versus open appendectomy. Surgery 1992;112(3):497‐501. [PUBMED: 1387739] [PubMed] [Google Scholar]
Bauwens 1998 {published data only}
- Bauwens K, Schwenk W, Bohm B, Hasart O, Neudecker J, Muller JM. Recovery and duration of work disability after laparoscopic and conventional appendectomy. A prospective randomized study [Rekonvaleszenz und Arbeitsunfahigkeitsdauer nach laparoskopischer und konventioneller Appendektomie. Eine prospektiv‐randomisierte Studie.]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 1998;69(5):541‐5. [PUBMED: 9653559] [DOI] [PubMed] [Google Scholar]
Cho 2011 {published data only}
- Cho MS, Min BS, Hong YK, Lee WJ. Single‐site versus conventional laparoscopic appendectomy: comparison of short‐term operative outcomes.. Surgical Endoscopy 2011;25(1):36‐40. [DOI] [PubMed] [Google Scholar]
Clarke 2011 {published data only}
- Clarke T, Katkhouda N, Mason RJ, Cheng BC, Olasky J, Sohn HJ, et al. Laparoscopic versus open appendectomy for the obese patient: a subset analysis from a prospective, randomized, double‐blind study. Surgical Endoscopy 2011;25(4):1276‐80. [DOI] [PubMed] [Google Scholar]
Cox 1996 {published data only}
- Cox MR, McCall JL, Toouli J, Padbury RT, Wilson TG, Wattchow DA, et al. Prospective randomized comparison of open versus laparoscopic appendectomy in men. World Journal of Surgery 1996;20(3):263‐6. [PUBMED: 8661828] [DOI] [PubMed] [Google Scholar]
de Wilde 1991 {published data only}
Eichen 1994 {published data only}
- Eichen R, Heuser H, Nitschke B. Laparoscopic or conventional appendectomy: a prospective study. Langenbecks Archiv fur Chirurgie. Supplement. Kongressband 1994;111:223‐5. [Google Scholar]
Frazee 1994 {published data only}
- Frazee RC, Roberts JW, Symmonds RE, Snyder SK, Hendricks JC, Smith RW, et al. A prospective randomized trial comparing open versus laparoscopic appendectomy. Annals of Surgery 1994;219(6):725‐8; discussion 728‐31. [PUBMED: 8203983] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goudar 2011 {published data only}
- Goudar BV, Telkar S, Lamani YP, Shirbir SH, Shailesh ME. Laparoscopic versus open appendectomy: a comparison of primary outcome studies from Southern India. Journal of Clinical and Diagnostic Research 2011;5(8):1606‐9. [Google Scholar]
Hansen 1996 {published data only}
- Hansen JB, Smithers BM, Schache D, Wall DR, Miller BJ, Menzies BL. Laparoscopic versus open appendectomy: prospective randomized trial. World Journal of Surgery 1996;20(1):17‐20; discussion 21. [PUBMED: 8588406] [DOI] [PubMed] [Google Scholar]
Hart 1996 {published data only}
- Hart R, Rajgopal C, Plewes A, Sweeney J, Davies W, Gray D, et al. Laparoscopic versus open appendectomy: a prospective randomized trial of 81 patients. Canadian Journal of Surgery. Journal Canadien de Chirurgie 1996;39(6):457‐62. [PUBMED: 8956810] [PMC free article] [PubMed] [Google Scholar]
Hebebrand 1994 {published data only}
- Hebebrand D, Troidl H, Spangenberger W, Neugebauer E, Schwalm T, Gunther MW. Laparoscopic or classical appendectomy? A prospective randomized study [Laparoskopische oder klassische Appendektomie? Eine prospektiv randomisierte Studie.]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 1994;65(2):112‐20. [PUBMED: 8162812] [PubMed] [Google Scholar]
Heikkinen 1998 {published data only}
- Heikkinen TJ, Haukipuro K, Hulkko A. Cost‐effective appendectomy. Open or laparoscopic? A prospective randomized study. Surgical Endoscopy 1998;12(10):1204‐8. [PUBMED: 9745057] [DOI] [PubMed] [Google Scholar]
Hellberg 1999 {published data only}
- Hellberg A, Rudberg C, Kullman E, Enochsson L, Fenyo G, Graffner H, et al. Prospective randomized multicentre study of laparoscopic versus open appendicectomy. The British Journal of Surgery 1999;86(1):48‐53. [PUBMED: 10027359] [DOI] [PubMed] [Google Scholar]
Helmy 2001 {published data only}
- Helmy MA. A comparative study between laparoscopic versus open appendicectomy in men. Journal of the Egyptian Society of Parasitology 2001;31(2):555‐62. [PUBMED: 11478454] [PubMed] [Google Scholar]
Henle 1996 {published data only}
- Henle KP, Beller S, Rechner J, Zerz A, Szinicz G, Klingler A. Laparoscopic versus conventional appendectomy: a prospective randomized study [Laparoskopische versus konventionelle Appendektomie: eine prospektive, randomisierte Studie.]. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 1996;67(5):526‐30; discussion 522. [PUBMED: 8777883] [PubMed] [Google Scholar]
Huang 2001 {published data only}
- Huang MT, Wei PL, Wu CC, Lai IR, Chen RJ, Lee WJ. Needlescopic, laparoscopic, and open appendectomy: a comparative study. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2001;11(5):306‐12. [PUBMED: 11668227] [DOI] [PubMed] [Google Scholar]
Ignacio 2004 {published data only}
- Ignacio RC, Burke R, Spencer D, Bissell C, Dorsainvil C, Lucha PA. Laparoscopic versus open appendectomy: what is the real difference? Results of a prospective randomized double‐blinded trial. Surgical Endoscopy 2004;18(2):334‐7. [PUBMED: 14691696] [DOI] [PubMed] [Google Scholar]
Kald 1999 {published data only}
- Kald A, Kullman E, Anderberg B, Wiren M, Carlsson P, Ringqvist I, et al. Cost‐minimisation analysis of laparoscopic and open appendicectomy. The European Journal of Surgery = Acta Chirurgica 1999;165(6):579‐82. [PUBMED: 10433143] [DOI] [PubMed] [Google Scholar]
Kaplan 2009 {published data only}
- Kaplan M, Salman B, Yilmaz TU, Oguz M. A quality of life comparison of laparoscopic and open approaches in acute appendicitis: a randomised prospective study. Acta Chirurgica Belgica 2009;109(3):356‐63. [DOI] [PubMed] [Google Scholar]
Karadayi 2003 {published data only}
- Karadayi K, Turan M, Canbay E, Topcu O, Sen M. Laparoscopic versus open appendectomy: analysis of systemic acute‐phase responses in a prospective randomized study. Chirurgische Gastroenterologie 2003;19:396‐400. [Google Scholar]
Kargar 2011 {published data only}
- Kargar S, Mirshamsi MH, Zare M, Arefanian S, Shadman Yazdi E, Aref A. Laparoscopic versus open appendectomy; which method to choose? A prospective randomized comparison. Acta Med Iran 2011;49(6):352‐6. [PubMed] [Google Scholar]
Kazemier 1997 {published data only}
- Kazemier G, Zeeuw GR, Lange JF, Hop WC, Bonjer HJ. Laparoscopic vs open appendectomy. A randomized clinical trial. Surgical Endoscopy 1997;11(4):336‐40. [PUBMED: 9094272] [DOI] [PubMed] [Google Scholar]
Khalil 2013 {published data only}
- Khalil J, Muqim R, Rafique M, Khan M. Laparoscopic versus open appendectomy: a comparison of primary outcome measures. Saudi Journal of Gastroenterology 2011;17(4):236‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Koluh 2010 {published data only}
- Koluh A, Delibegovic S, Hasukic S, Valjan V, Latic F. Laparoscopic appendectomy in the treatment of acute appendicitis. Medicinski Archive 2010;64(3):147‐50. [PubMed] [Google Scholar]
Kouhia 2010 {published data only}
- Kouhia ST, Heiskanen JT, Huttunen R, Ahtola HI, Kiviniemi VV, Hakala T. Long‐term follow‐up of a randomized clinical trial of open versus laparoscopic appendicectomy.. British Journal Surgery 2010;97(9):1395‐400. [DOI] [PubMed] [Google Scholar]
Kum 1993 {published data only}
- Kum CK, Ngoi SS, Goh PM, Tekant Y, Isaac JR. Randomized controlled trial comparing laparoscopic and open appendicectomy. The British Journal of Surgery 1993;80(12):1599‐600. [PUBMED: 8298936] [DOI] [PubMed] [Google Scholar]
Lavonius 2001 {published data only}
- Lavonius MI, Liesjarvi S, Ovaska J, Pajulo O, Ristkari S, Alanen M. Laparoscopic versus open appendectomy in children: a prospective randomised study. European Journal of Pediatric Surgery = Zeitschrift fur Kinderchirurgie 2001;11(4):235‐8. [PUBMED: 11558012] [DOI] [PubMed] [Google Scholar]
Lejus 1996 {published data only}
- Lejus C, Delile L, Plattner V, Baron M, Guillou S, Heloury Y, et al. Randomized, single‐blinded trial of laparoscopic versus open appendectomy in children: effects on postoperative analgesia. Anesthesiology 1996;84(4):801‐6. [PUBMED: 8638833] [DOI] [PubMed] [Google Scholar]
Lintula 2004 {published data only}
- Lintula H, Kokki H, Vanamo K, Valtonen H, Mattila M, Eskelinen M. The costs and effects of laparoscopic appendectomy in children. Archives of Pediatrics & Adolescent Medicine 2004;158(1):34‐7. [PUBMED: 14706955] [DOI] [PubMed] [Google Scholar]
Little 2002 {published data only}
- Little DC, Custer MD, May BH, Blalock SE, Cooney DR. Laparoscopic appendectomy: an unnecessary and expensive procedure in children?. Journal of Pediatric Surgery 2002;37(3):310‐7. [PUBMED: 11877640] [DOI] [PubMed] [Google Scholar]
Long 2001 {published data only}
- Long KH, Bannon MP, Zietlow SP, Helgeson ER, Harmsen WS, Smith CD, et al. A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: clinical and economic analyses. Surgery 2001;129(4):390‐400. [PUBMED: 11283528] [DOI] [PubMed] [Google Scholar]
Macarulla 1997a {published data only}
- Macarulla E, Vallet J, Abad JM, Hussein H, Fernandez E, Nieto B. Laparoscopic versus open appendectomy: a prospective randomized trial. Surgical Laparoscopy & Endoscopy 1997;7(4):335‐9. [PUBMED: 9282768] [PubMed] [Google Scholar]
Martin 1995 {published data only}
- Martin LC, Puente I, Sosa JL, Bassin A, Breslaw R, McKenney MG, et al. Open versus laparoscopic appendectomy. A prospective randomized comparison. Annals of Surgery 1995;222(3):256‐61; discussion 261‐2. [PUBMED: 7677456] [DOI] [PMC free article] [PubMed] [Google Scholar]
McAnena 1992 {published data only}
- McAnena OJ, Austin O, O'Connell PR, Hederman WP, Gorey TF, Fitzpatrick J. Laparoscopic versus open appendicectomy: a prospective evaluation. The British Journal of Surgery 1992;79(8):818‐20. [PUBMED: 1393483] [DOI] [PubMed] [Google Scholar]
Meynaud‐Kraemer 1999 {published data only}
- Meynaud‐Kraemer L, Colin C, Vergnon P, Barth X. Wound infection in open versus laparoscopic appendectomy. A meta‐analysis. International Journal of Technology Assessment in Health Care 1999;15(2):380‐91. [PUBMED: 10507196] [PubMed] [Google Scholar]
Minne 1997 {published data only}
- Minne L, Varner D, Burnell A, Ratzer E, Clark J, Haun W. Laparoscopic vs open appendectomy. Prospective randomized study of outcomes. Archives of Surgery 1997;132(7):708‐11; discussion 712. [PUBMED: 9230853] [DOI] [PubMed] [Google Scholar]
Moirangthem 2008 {published data only}
- Moirangthem GS, Arunkumar Ch, Marak AB, Lokendra K, Singh LD. A comparative study between laparoscopic versus open appendicectomy. Journal of Medical Society 2008;22(2):58‐62. [Google Scholar]
Mutter 1996 {published data only}
- Mutter D, Vix M, Bui A, Evrard S, Tassetti V, Breton JF, et al. Laparoscopy not recommended for routine appendectomy in men: results of a prospective randomized study. Surgery 1996;120(1):71‐4. [PUBMED: 8693426] [DOI] [PubMed] [Google Scholar]
Nordentoft 2000 {published data only}
- Nordentoft T, Bringstrup FA, Bremmelgaard A, Stage JG. Effect of laparoscopy on bacteremia in acute appendicitis: a randomized controlled study. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2000;10(5):302‐4. [PUBMED: 11083213] [PubMed] [Google Scholar]
Ortega 1995 {published data only}
- Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy. Laparoscopic Appendectomy Study Group. American Journal of Surgery 1995;169(2):208‐12; discussion 212‐3. [PUBMED: 7840381] [DOI] [PubMed] [Google Scholar]
Ozmen 1999 {published data only}
- Ozmen MM, Zulfikaroglu B, Tanik A, Kale IT. Laparoscopic versus open appendectomy: prospective randomized trial. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 1999;9(3):187‐9. [PUBMED: 10803997] [PubMed] [Google Scholar]
Pedersen 2001 {published data only}
- Pedersen AG, Petersen OB, Wara P, Ronning H, Qvist N, Laurberg S. Randomized clinical trial of laparoscopic versus open appendicectomy. The British Journal of Surgery 2001;88(2):200‐5. [PUBMED: 11167866] [DOI] [PubMed] [Google Scholar]
Perner 1999 {published data only}
- Perner A, Bugge K, Lyng KM, Schulze S, Kristensen PA, Bendtsen A. Changes in plasma potassium concentration during carbon dioxide pneumoperitoneum. British Journal of Anaesthesia 1999;82(1):137‐9. [PUBMED: 10325852] [DOI] [PubMed] [Google Scholar]
Reiertsen 1997 {published data only}
- Reiertsen O, Larsen S, Trondsen E, Edwin B, Faerden AE, Rosseland AR. Randomized controlled trial with sequential design of laparoscopic versus conventional appendicectomy. The British Journal of Surgery 1997;84(6):842‐7. [PUBMED: 9189105] [PubMed] [Google Scholar]
Schietroma 2007 {published data only}
- Schietroma M, Cappelli S, Carlei F, Pescosolido A, Lygidakis NJ, Amicucci G. "Acute abdomen": early laparoscopy or active laparotomic‐laparoscopic observation?. Hepatogastroenterology 2007;54:1137‐41. [PubMed] [Google Scholar]
Schippers 1994 {published data only}
- Schippers E, Pier A, May P, Schumpelick V. Laparoscopic vs open appendectomy—a comparison of postoperative pain and respiratory function [abstract]. Surgical Endoscopy 1994;8:561. [Google Scholar]
Settmacher 1995 {published data only}
- Settmacher U, Manger T, Liebenthal C, Neuhaus K, Volk HD. Immunological modifications after open and laparoscopic surgery. Minimal Invasive Chirurgie 1995;4:95‐102. [Google Scholar]
Sezeur 1997 {published data only}
- Sezeur A, Bure‐Rossier AM, Rio D, Savigny B, Tricot C, Martel P, et al. Does laparoscopy increase the bacteriological risk of appendectomy? Results of a randomized prospective study [La coelioscopie augmente‐t‐elle le risque bacteriologique de l'appendicectomie? Resultats d'une etude prospective randomisee.]. Annales de Chirurgie 1997;51(3):243‐7. [PUBMED: 9297886] [PubMed] [Google Scholar]
Shirazi 2010 {published data only}
- Shirazi B, Ali N, Shamim MS. Laparoscopic versus open appendectomy: a comparative study. Journal of Pakistan Medical Association 2010;60(11):901‐4. [PubMed] [Google Scholar]
Stare 1998 {published data only}
- Stare R, Kocman I, Povsic Cevra Z. Results of a prospective randomised study of laparoscopic appendectomy in community hospital [abstract]. Surgical Endoscopy 1998;12:573. [Google Scholar]
St Peter 2011 {published data only}
- Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, et al. Single incision versus standard 3‐port laparoscopic appendectomy: a prospective randomized trial. Annals of Surgery 2011;254(4):586‐90. [DOI] [PubMed] [Google Scholar]
Tate 1993 {published data only}
- Tate JJ, Dawson JW, Chung SC, Lau WY, Li AK. Laparoscopic versus open appendicectomy: prospective randomised trial. Lancet 1993;342(8872):633‐7. [PUBMED: 8103144] [DOI] [PubMed] [Google Scholar]
Tzovaras 2010 {published data only}
- Tzovaras G, Baloyiannis I, Kouritas V, Symeonidis D, Spyridakis M, Poultsidi A, et al. Laparoscopic versus open appendectomy in men: a prospective randomized trial. Surgical Endoscopy 2010;24(12):2987‐92. [DOI] [PubMed] [Google Scholar]
Vallribera 2003 {published data only}
- Vallribera Valls F, Sala Pedros J, Aguilar Teixedor F, Espin Bassany E. Influence of laparoscopic surgery on perception of quality of life after appendectomy [Influencia de la cirugia laparoscopica en la percepcion de la claidad de vida tras apendicectomia]. Cirugia Espanola 2003;73:88‐94. [Google Scholar]
Wei 2010 {published data only}
- Wei HB, Huang JL, Zheng ZH, Wei B, Zheng F, Qiu WS, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surgical Endoscopy 2010;24(2):266‐9. [DOI] [PubMed] [Google Scholar]
Williams 1996 {published data only}
- Williams MD, Collins JN, Wright TF, Fenoglio ME. Laparoscopic versus open appendectomy. Southern Medical Journal 1996;89(7):668‐74. [PUBMED: 8685751] [DOI] [PubMed] [Google Scholar]
Witten 1998 {published data only}
- Birth M, Witten I, Gadzepko E, Weiser HF. Laparoscopic vs open appendectomy for acute appendicitis: a prospective randomized trial [abstract]. The British Journal of Surgery 1998;85 Suppl 2:39. [Google Scholar]
Yeung 1997 {published data only}
- Yeung CK, Yip KF, Lee KH, Lau WY. The role of minimally invasive surgery in the management of acute appendicitis in children: a prospective randomized trial of laparoscopic vs conventional appendectomy [abstract]. Asian Journal of Surgery 1997;20 Suppl:55. [Google Scholar]
Zaninotto 1995 {published data only}
- Zaninotto G, Rossi M, Anselmino M, Costantini M, Pianalto S, Baldan N, et al. Laparoscopic versus conventional surgery for suspected appendicitis in women. Surgical Endoscopy 1995;9(3):337‐40. [DOI] [PubMed] [Google Scholar]
Zhang 1998 {published data only}
- Zhang WF, Xu CX, Liu YH, Huang GJ. A randomized control study on the appendectomy of 103 cases with laparoscope or mini‐incision. Modern Journal of Physicians 1998;3:8‐9. [Google Scholar]
References to ongoing studies
ISRCTN42332281 {published data only}
- Sant'Orsola‐Malpighi University Hospital Bologna (sponsor). Multicentre randomised, double‐blind, controlled trial of laparoscopic versus open surgery for suspected appendicitis in adults. ISRCTN identifier: ISRCTN42332281 2005; Vol. http://isrctn.org/ISRCTN42332281.
Additional references
Althoubaity 2006
- Althoubaity FK. Suspected acute appendicitis in female patients: trends in diagnosis in emergency department in a university hospital in Western Region of Saudi Arabia. Saudi Medical Journal 2006;27:1667‐73. [PubMed] [Google Scholar]
Bennett 2007
- Bennett J, Boddy A, Rhodes M. Choice of approach for appendicectomy: a meta‐analysis of open versus laparoscopic appendicectomy. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 2007;17(4):245‐55. [PUBMED: 17710043] [DOI] [PubMed] [Google Scholar]
Beyan 2003
- Bevan CD, Ridgway GL, Rothermel CD. Efficacy and safety of azithromycin as monotherapy or combined with metronidazole compared with two standard multidrug regimens for the treatment of acute pelvic inflammatory disease. The Journal of International Medical Research 2003;31(1):45‐54. [DOI] [PubMed] [Google Scholar]
Bijnen 2003
- Bijnen CL, Broek WT, Bijnen AB, Ruiter P, Gouma DJ. Implications of removing a normal appendix. Digestive Surgery 2003;20(3):215‐9. [DOI] [PubMed] [Google Scholar]
Borgstein 1997
- Borgstein PJ, Gordijn RV, Eijsbouts QA, Cuesta MA. Acute appendicitis—a clear‐cut case in men, a guessing game in young women. A prospective study on the role of laparoscopy. Surgical Endoscopy 1997;11(9):923‐7. [DOI] [PubMed] [Google Scholar]
CDC 2003 [Computer program]
- Centers for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. http://www.cdc.gov.ezproxy.auckland.ac.nz/nchs/data/ad/ad358.pdf (accessed 7 July 2013), 2003.
Flum 2002
- Flum DR, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Archives of Surgery 2002;137(7):799‐804. [DOI] [PubMed] [Google Scholar]
Gaitan 2011
- Gaitán HG, Reveiz L, Farquhar C. Laparoscopy for the management of acute lower abdominal pain in women of childbearing age. Cochrane Database of Systematic Reviews 2011, (1):CD007683. [DOI] [PubMed] [Google Scholar]
Golash 2005
- Golash V, Willson PD. Early laparoscopy as a routine procedure in the management of acute abdominal pain: a review of 1,320 patients. Surgical Endoscopy 2005;19(7):882‐5. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Irvin 1989
- Irvin TT. Abdominal pain: a surgical audit of 1190 emergency admissions. The British Journal of Surgery 1989;76(11):1121‐5. [DOI] [PubMed] [Google Scholar]
Kapischke 2006
- Kapischke M, Caliebe A, Tepel J, Schulz T, Hedderich J. Open versus laparoscopic appendicectomy: a critical review. Surgical Endoscopy 2006;20(7):1060‐8. [PUBMED: 16703441] [DOI] [PubMed] [Google Scholar]
Koch 2002
- Koch A, Marusch F, Schmidt U, Gastinger I, Lippert H. Appendicitis in the last decade of the 20th century—analysis of two prospective multicenter clinical observational studies. Zentralblatt fur Chirurgie 2002;127(4):290‐6. [DOI] [PubMed] [Google Scholar]
Li 2010
- Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X, Liu Y. Laparoscopic versus conventional appendectomy—a meta‐analysis of randomized controlled trials. BMC Gastroenterology 2010;10:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maggio 2008
- Maggio AQ, Reece‐Smith AM, Tang TY, Sadat U, Walsh SR. Early laparoscopy versus active observation in acute abdominal pain: systematic review and meta‐analysis. International Journal of Surgery (London, England) 2008;6(5):400‐3. [PUBMED: 18760983] [DOI] [PubMed] [Google Scholar]
Moberg 1998
- Moberg AC, Ahlberg G, Leijonmarck CE, Montgomery A, Reiertsen O, Rosseland AR, Stoerksson R. Diagnostic laparoscopy in 1043 patients with suspected acute appendicitis. The European Journal of Surgery 1998;164(11):833‐40. [DOI] [PubMed] [Google Scholar]
Navez 1995
- Navez B, d'Udekem Y, Cambier E, Richir C, Pierpont B, Guiot P. Laparoscopy for management of nontraumatic acute abdomen. World Journal of Surgery 1995;19(3):382‐6. [DOI] [PubMed] [Google Scholar]
Ou 2000
- Ou CS, Rowbotham R. Laparoscopic diagnosis and treatment of nontraumatic acute abdominal pain in women. Journal of Laparoendoscopic & Advanced Surgical Techniques. Part A 2000;10(1):41‐5. [DOI] [PubMed] [Google Scholar]
Poulin 2000
- Poulin EC, Schlachta CM, Mamazza J. Early laparoscopy to help diagnose acute non‐specific abdominal pain. Lancet 2000;355(9207):861‐3. [DOI] [PubMed] [Google Scholar]
Roper 1988
- Roper W, Winkenwerder W, Hackbarth G, Krakauer H. Effectiveness in health care. An initiative to evaluate and improve medical practice. New England Journal of Medicine 1988;319(18):1197‐202. [DOI] [PubMed] [Google Scholar]
Sala 2007
- Sala E, Watson CJ, Beadsmoore C, Groot‐Wassink T, Fanshawe TR, Smith JC, et al. A randomized, controlled trial of routine early abdominal computed tomography in patients presenting with non‐specific acute abdominal pain. Clinical Radiology 2007;62(10):961‐9. [DOI] [PubMed] [Google Scholar]
Salky 1998
- Salky BA, Edye MB. The role of laparoscopy in the diagnosis and treatment of abdominal pain syndromes. Surgical Endoscopy 1998;12(7):911‐4. [DOI] [PubMed] [Google Scholar]
Sanders 2006
- Sanders DS, Azmy IA, Hurlstone DP. A new insight into non‐specific abdominal pain. Annals of the Royal College of Surgeons of England 2006;88(2):92‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sauerland 2010
- Sauerland S, Jaschinski T, Neugebauer EAM. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database of Systematic Reviews 2010, (10):CD001546. [DOI] [PubMed] [Google Scholar]
Sellors 1991
- Sellors J, Mahony J, Goldsmith C, Rath D, Mander R, Hunter B, et al. The accuracy of clinical findings and laparoscopy in pelvic inflammatory disease. American Journal of Obstetrics and Gynecology 1991;164(1):113‐20. [DOI] [PubMed] [Google Scholar]
Spirtos 1987
- Spirtos NM, Eisenkop SM, Spirtos TW, Poliakin RI, Hibbard LT. Laparoscopy. A diagnosis aid in cases of suspected appendicitis. Its use in women of reproductive age. American Journal of Obstetrics and Gynecology 1987;156(1):90‐4. [DOI] [PubMed] [Google Scholar]
Strömberg 2007
- Strömberg C, Johansson G, Adolfsson A. Acute abdominal pain: diagnostic impact of immediate CT scanning. World Journal of Surgery 2007;31(12):1347‐57. [DOI] [PubMed] [Google Scholar]
Tzovaras 2007
- Tzovaras G, Liakou P, Baloyiannis I, Spyridakis M, Mantzos F, Tepetes K, et al. Laparoscopic appendectomy: differences between male and female patients with suspected acute appendicitis. World Journal of Surgery 2007;31(2):409‐13. [DOI] [PubMed] [Google Scholar]
Whitworth 1988
- Whitworth CM, Whitworth PW, Sanfillipo J, Polk HC. Value of diagnostic laparoscopy in young women with possible appendicitis. Surgery, Gynecology & Obstetrics 1988;167(3):187‐90. [PubMed] [Google Scholar]


