Abstract
Objective:
Suicidal ideation (SI) is common in patients with depressive symptoms, who are the most common recipients of electroconvulsive therapy (ECT). We sought to quantify changes in self-reported SI occurring during treatment with ECT, and to identify factors associated with persistence of SI in patients beginning treatment with SI.
Methods:
Retrospective, single-center cohort study of patients receiving ECT and who self-reported symptoms using Quick Inventory of Depressive Symptomatology (QIDS) prior to ECT and after treatment #5 or #10. Changes in QIDS-reported SI over the course of ECT were calculated, and logistic regression models were performed to assess factors associated with reporting SI at the end of treatment.
Results:
2,554 provided baseline and follow-up SI scores, of whom, 1,931 (75.6%) endorsed SI at baseline. There was a reduction in SI with ECT treatment (McNemar’s test; df=1, Χ2=803.7; p<0.001), and in adjusted models 64.0% of individuals with baseline SI reported resolution of SI with ECT treatment, while 3.3% without baseline SI reported SI at the end of treatment. Higher baseline SI severity and outpatient treatment were associated with a higher odds of persistent SI among individuals beginning treatment with SI.
Conclusion:
ECT treatment was associated with reductions in self-reported SI. These results support the use of ECT in the treatment of patients with SI, but further research is needed to determine the effects of ECT on suicidal behavior.
Keywords: Suicidal ideation, Suicide, Cohort studies, Electroconvulsive therapy, Real World Evidence
Introduction:
Suicide is a leading cause of death worldwide, with an estimated 1.3% of overall global deaths in 2019 attributable to suicide 1. In the United States, suicides in 2021 are near record-peak in number, with disparate rates depending on age, sex, and race 2. While many factors influence suicide risk, meta-analysis has indicated that prior suicidal ideation (SI) is one risk factor for suicidal behavior 3–5, and so reduction in SI is one important therapeutic goal. Electroconvulsive therapy (ECT) is an effective treatment for depression across the age span 6, and is associated with a reduction in SI 7–10, suicide attempts 11,12, completed suicide 13, and all-cause mortality 14–16. While some study results indicate increased risk of suicide death in ECT patients even if all-cause mortality decreased 14,15, there is great heterogeneity between studies. Moreover, access to ECT17,18 as well as treatment efficacy may vary based on patient demographics including age19 and race.20 Given the complex nature of SI, further data on the effects of ECT on SI using real-world data can help provide guidance around changes on SI that may occur during ECT during routine clinical practice.
Aims of the Study
This study explores changes in self-reported SI over the course of ECT using a large single-center clinical cohort. We sought to quantify changes in self-reported SI occurring during treatment with ECT, and to identify factors associated with persistence of SI in patients beginning treatment with SI.
Methods
Patient Population
This was a single center retrospective cohort study of patients aged 16 or older receiving ECT at a freestanding psychiatric hospital from May 2011 through March 2020. All patients self-reporting baseline symptom severity and at least one follow-up severity measure (see below) were included in the sample. Patients were followed through discontinuation of ECT or through treatment #10. This retrospective chart review study was approved by the Mass General Brigham Institutional Review Board with a waiver of informed consent.
Scales and Measurements
Treatment was monitored using patient self-report scales. These include the Quick Inventory of Depressive Symptomatology Self-Report 16-item scale (QIDS) 21, the Behavior and Symptom Identification Scale-24 (BASIS-24) 22, and the Montreal Cognitive Assessment (MoCA) 23. By default, patients reported symptom severity using these scales at baseline and following treatment #5 and treatment #10. Demographic information, including race, is based on self-report from the baseline BASIS-24, while diagnosis was determined from the clinical diagnosis recorded at the time of first ECT treatment.
For the primary endpoint, self-reported SI was assessed based on item 12 of the QIDS, which asks about “thoughts of death or suicide” during the past 7 days on a 4-point scale of: 0 “I do not think of suicide or death”; 1 “I feel that life is empty or wonder if it’s worth living”; 2 “I think of suicide or death several times a week for several minutes”; 3 “I think of suicide or death several times a day in some detail, or I have made specific plans for suicide or have actually tried to take my life.” Scores >0 were defined as the presence of SI, with a score of 0 indicating a lack of SI.
ECT Treatment
ECT was provided using a Mecta Spectrum 5000Q instrument (Tualatin, OR). Individualized seizure threshold was determined at the time of first treatment, as previously reported 24,25. Subsequent treatments were delivered initially at 6x seizure threshold for right unilateral treatments, typically three times weekly, with electrode placement and dose adjusted clinically by the treating psychiatrist based on response 26–28. Methohexital was the default anesthetic agent with succinylcholine muscle relaxant, although etomidate, propofol, or ketamine anesthetic could be used at the discretion of the treating psychiatrist or anesthesiologist. Consistent with the MECTA titration tables, ultrabrief pulse ECT was defined as a pulse width of 0.3 ms or 0.37 ms, while pulse widths of ≥0.37 ms were defined as brief pulse.
Statistical Analysis
The demographic characteristics of the sample are reported through descriptive statistics. Suicidal ideation was determined using the QIDS SI question. Participants who scored a ‘0’ on the item prior to treatment were reported as having no SI and participants who had scores greater than ‘0’ were reported as having SI at baseline. For the follow-up assessment, SI was based on the QIDS SI question at the 5th or 10th ECT treatment, whichever was the last assessment. As some patients did not have assessments precisely at treatment #5 or treatment #10, results were included if the assessment was performed within 2 treatments of this, so follow-up values could occur between treatments 3 and 7 or between treatments 8 and 12.
Due to small cell sizes for some racial categories, race was dichotomized to “Not White” or “White” and ECT pulse width was dichotomized to “0.37 milliseconds or less” or “Greater than 0.37 milliseconds”. For the primary statistical analysis, SI scores at baseline and following ECT were compared using McNemar’s test. We also obtained unadjusted and adjusted odds ratios from logistic models with persistence of SI (i.e. SI at last assessment) as dependent variable and baseline SI based on baseline QIDS score as the independent variable of interest. The basic model was adjusted for confounders (variables that differed at baseline and were independently related to the outcome). These confounders included age, inpatient (vs outpatient), baseline BASIS-24 total score, baseline MOCA total score, perceived health (excellent/very good vs poor/very poor and good vs poor/very poor), marital status (with partner vs no partner), race (White vs not White), and pulse width (≤0.37 vs >0.37). To address missing data on variables of interest, multiple imputation was conducted on the missing persistence of SI scores across 10 imputations, with age, sex, baseline QIDS, partner status, education, living status, MOCA category (cognitively impaired yes/no), diagnosis, general health, inpatient status electrode placement, and thoughts of death at baseline used to impute missing values. Logistic regression modeling was repeated with the imputed data; results of both analyses were similar, therefore only unimputed results are reported.
As a subgroup analysis, an additional logistic model was used to investigate clinical and demographic factors associated with persistence of SI among individuals with baseline SI. For this model, the presence of SI at the time of last treatment was the dependent variable, with age, sex, admission status (inpatient vs. outpatient), diagnosis, baseline overall QIDS, baseline QIDS SI score (1 vs. 2 vs. 3), final treatment number (5 vs. 10), initial electrode placement (unilateral vs. bilateral) and whether electrode placement was switched during treatment (yes vs. no) as independent variables. All analyses were implemented using SAS statistical software Version 9.4 or SPSS Version 29. An alpha level of 0.05 or less was used to determine statistical significance.
Results
During the study period, 3,062 patients provided symptom severity scores prior to ECT, of whom 2,554 provided at least one follow-up SI value and were included in the primary analysis. Of these 2,554 patients, 1,931 (75.6%) endorsed SI at baseline while 623 (24.4%) reported no SI. Overall, 1,065 patients were male (41.7%) and 2,313 (90.6%) were white. Primary clinical diagnoses were major depressive disorder (1,869; 73.2%) and bipolar disorder (548; 21.5%). Full demographic information is provided in Table 1 and Table S1. Patients were initially treated with predominantly right unilateral (2,445; 95.6%) and ultrabrief pulse (2,293; 89.8%) ECT parameters, and at the time of last treatment 2,247 (88.0%) utilized right unilateral electrode placement and 1,695 (66.4%) ultrabrief pulse width.
Table 1:
baseline demographics of the sample
| Analysis sample (n=2554) |
|||
|---|---|---|---|
| Overall | No suicidal ideation at baseline | Any suicidal ideation at baseline | |
| N | 2554 | 623 | 1931 |
| Age (mean (SD)), years | 46.7 (16.7) | 51.4 (16.7) | 45.1 (16.3) |
| Sex | |||
| Male | 1065 (41.7) | 264 (42.4) | 801 (41.5) |
| Female | 1489 (58.3) | 359 (57.6) | 1130 (58.5) |
| Race | |||
| American Indian or Alaskan Native | 27 (1.1) | 5 (0.8) | 22 (1.1) |
| Asian | 63 (2.5) | 15 (2.4) | 48 (2.5) |
| African American or Black | 42 (1.6) | 8 (1.3) | 34 (1.8) |
| White | 2313 (90.6) | 570 (91.5) | 1743 (90.3) |
| Other | 12 (0.5) | 5 (0.8) | 7 (0.4) |
| Unknown | 97 (3.8) | 20 (3.2) | 77 (3.9) |
| Subjective Physical Health | |||
| Very poor | 39 (1.5) | 6 (0.9) | 33 (1.7) |
| Poor | 331 (12.9) | 70 (11.2) | 261 (13.5) |
| Good | 1427 (55.9) | 326 (52.3) | 1101 (57.0) |
| Very good | 584 (22.9) | 163 (26.2) | 421 (21.8) |
| Excellent | 155 (6.1) | 54 (8.7) | 101 (5.3) |
| Unknown | 18 (0.7) | 4 (0.6) | 14 (0.7) |
| Clinical Diagnosis | |||
| Major depressive disorder | 1869 (73.2) | 422 (67.7) | 1447 (74.9) |
| Bipolar affective disorder | 548 (21.5) | 149 (23.9) | 399 (20.7) |
| Other | 56 (2.2) | 18 (2.9) | 38 (1.9) |
| Unknown | 81 (3.2) | 34 (5.5) | 47 (2.4) |
| Baseline QIDS (mean (SD)) | 17.04 (4.9) | 12.8 (4.9) | 18.4 (4.1) |
| Baseline QIDS SI | |||
| 0 | 623 (24.4) | 623 (100) | 0 (0.0) |
| 1 | 836 (32.7) | 0 (0.0) | 836 (43.3) |
| 2 | 618 (24.2) | 0 (0.0) | 618 (32.0) |
| 3 | 477 (18.7) | 0 (0.0) | 477 (24.7) |
| Baseline MoCA (mean (SD)) | 27.2 (10.4) | 27.2 (12.5) | 27.2 (9.6) |
| ECT pulse width | |||
| 0.3 or 0.37 | 2293 (89.8) | 525 (84.3) | 1768 (91.6) |
| 0.5 | 65 (2.6) | 21 (3.4) | 44 (2.3) |
| 1.0 | 196 (7.7) | 77 (12.4) | 119 (6.2) |
| ECT electrode placement | |||
| Unilateral | 2442 (95.6) | 579 (92.9) | 1863 (96.5) |
| Bilateral | 112 (4.4) | 44 (7.1) | 68 (3.5) |
At baseline, mean QIDS was 17.0±4.9 overall, indicating severe-range depression. The mean QIDS score was 12.8±4.9 for patients without baseline SI and 18.4±4.1 for patients with baseline SI. Baseline MoCA was a mean of 27.2 in both groups, indicating normal-range cognition. Among the 1,931 individuals reporting baseline SI, 991 (43.5%) reported a score of 1, 724 (31.8%) reported a score of 2, and 561 (24.7%) reported a score of 3, the highest level of SI on the QIDS (Figure 1). At the time of final ECT (5 or 10 treatments), a total of 1,049 individuals reported SI, including 40 of the 623 without baseline SI (6.4%) and 1,009 of the 1,931 with baseline SI (52.3%). There was a higher proportion of patients expressing lower values of SI, and the null hypothesis that there was no change in SI was rejected. (McNemar’s test; df=1, Χ2=803.7; p<0.001). At time of last observation, 591 patients reported an SI score of 1 (56.3% of those with SI), 371 reported an SI score of 2 (35.8% of those with SI), and 82 reported an SI score of 3 (7.8% of those with SI).
Figure 1:
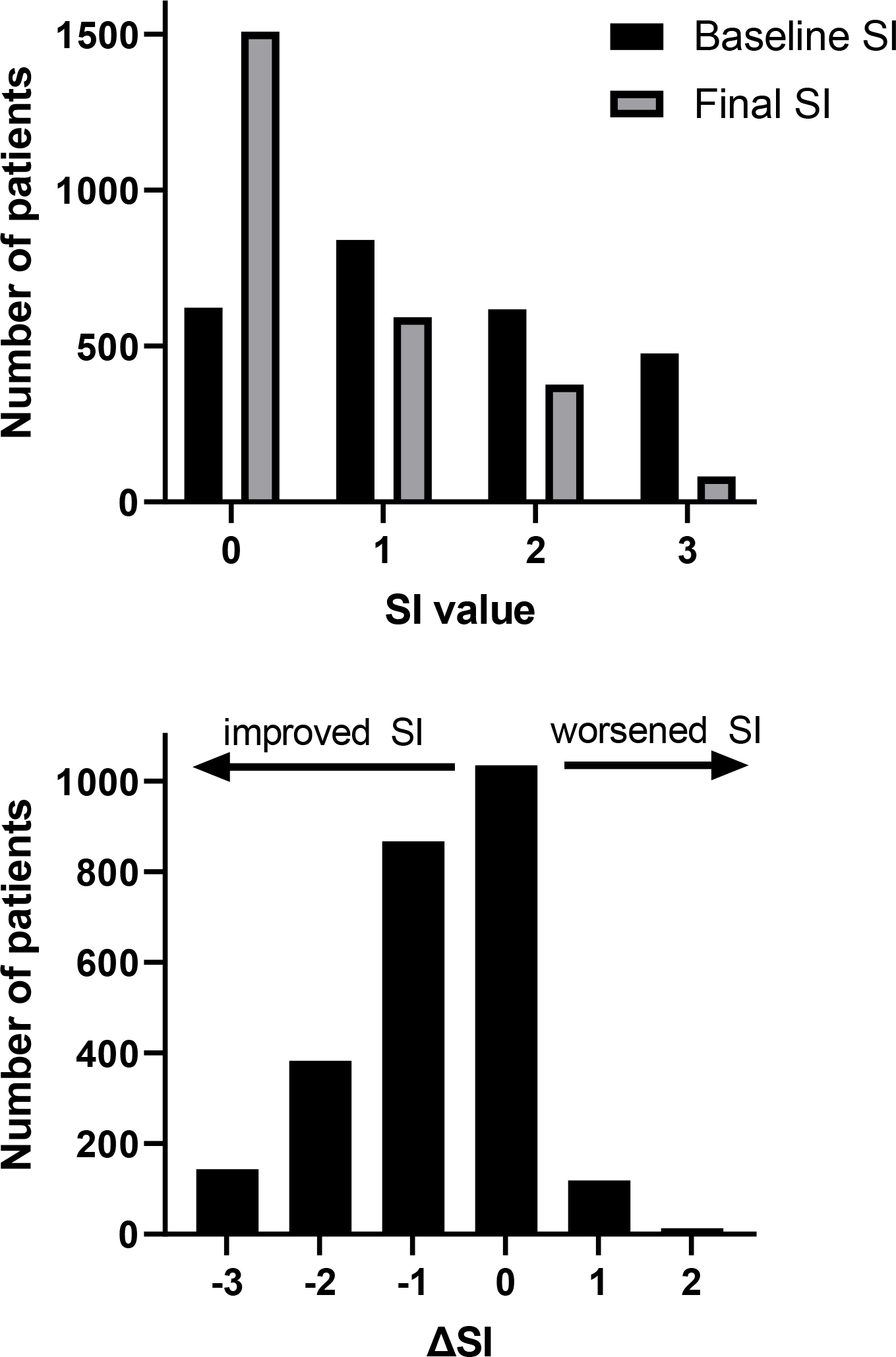
top: self-reported SI scores at baseline (black) and following ECT treatment (gray). bottom: change in self-reported SI scores among individual patients from baseline to following treatment #5 or #10. Negative numbers representing improvement in SI, and positive numbers representing worsening of SI.
In order to explore clinical and demographic factors associated with report of SI at the time of last treatment, a logistic model was conducted on the outcome of QIDS-reported SI (vs. no SI). In this model, baseline SI was associated with a higher odds of SI at the end of treatment OR= 15.77 (95% CI: 11.3, 21.9; p<0.001). This relationship was maintained when the model was adjusted for confounders with ORadj=16.56 (95% CI: 11.7, 23.4; p<0.001). Based on this adjusted model, 96.7% of patients without SI at baseline remained free of SI at the time of last observation, while 64.0% of patients with baseline SI had resolution of SI at time of last observation once confounders were adjusted for (Table 2).
Table 2:
proportions of patients with and without baseline SI who do or do not have SI at the time of last treatment. Presented are unadjusted proportions and proportions adjusted for age, inpatient (vs outpatient), baseline BASIS-24 total score, baseline MOCA total score, perceived health (excellent/very good vs poor/very poor and good vs poor/very poor), marital status (with partner vs no partner), race (White vs not White), and pulse width (≤0.37 vs >0.37).
| Group | Unadjusted Proportion | Adjusted Proportion |
|---|---|---|
| No baseline SI → developing SI at final treatment: | 6.5% | 3.3% |
| No baseline SI → no SI at final treatment: | 93.5% | 96.7% |
| Baseline SI → persistent SI at final treatment | 52.2% | 36.0% |
| Baseline SI → resolved SI at final treatment | 47.8% | 64.0% |
Finally, as a subgroup analysis, a logistic regression was performed to explore features associated with persistence of SI at the end of treatment among patients with baseline SI (Table 3). In this model, outpatient treatment (aOR 1.64; 95% CI: 1.33, 2.01; p<0.001), a change in electrode placement during treatment (aOR 2.11; 95% CI: 1.49, 3.00; p<0.001), and baseline SI score of 2 (aOR 2.17; 95% CI: 1.74, 2.70; p<0.001) or baseline SI score of 3 (aOR 3.92; 95% CI: 3.01, 5.12; p<0.001) were associated with higher odds of persistent SI at the time of last treatment, while other variables were not significantly associated with persistent SI.
Table 3:
multivariate logistic regression on the outcome of persistent SI (compared to resolution of SI) among 1,931 patients with baseline SI.
| Exp(B) | 95% C.I. | P Value | ||
|---|---|---|---|---|
| Lower | Upper | |||
|
| ||||
| Age | 1.00 | 1.00 | 1.00 | 0.51 |
| Sex | ||||
| Female | ref | . | . | |
| Male | 1.01 | 0.84 | 1.23 | 0.89 |
| Admission Status | ||||
| Inpatient | ref | . | . | |
| Outpatient | 1.64 | 1.33 | 2.01 | <.001 |
| Diagnosis | 0.23 | |||
| Other | ref | . | . | |
| Major depressive disorder | 0.84 | 0.52 | 1.34 | 0.46 |
| Bipolar disorder | 0.70 | 0.43 | 1.16 | 0.17 |
| Baseline QIDS | 1.01 | 0.99 | 1.04 | 0.37 |
| Baseline SI Score | <.001 | |||
| 1 | ref | . | . | |
| 2 | 2.17 | 1.74 | 2.70 | <.001 |
| 3 | 3.92 | 3.01 | 5.12 | <.001 |
| Initial Electrode Placement | ||||
| Unilateral | ref | . | . | |
| Bilateral | 0.90 | 0.54 | 1.51 | 0.70 |
| Change in Electrode Placement | ||||
| No | ref | . | . | |
| Yes | 2.11 | 1.49 | 3.00 | <.001 |
| Final Treatment Number | ||||
| 5 | ref | . | . | |
| 10 | 0.88 | 0.71 | 1.09 | 0.23 |
Discussion
In this sample of 2,554 patients receiving ECT, of whom 1,931 expressed SI at baseline, ECT was associated with a decrease in self-reported SI over the course of treatment. In an adjusted model, 96.7% of patients without SI at baseline remained free of SI at the time of last observation, while 64.0% of patients with baseline SI had resolution of SI at time of last observation. Among patients with persistent SI at the end of ECT, there was a reduction in the severity of SI, with a lower proportion of patients expressing the most severe levels of SI. Overall, these results support a robust improvement in self-reported SI with treatment with ECT. As this occurred over a period of 5 to 10 ECT treatments, or approximately 2–3 weeks for patients receiving treatments three times per week, these results provide evidence that ECT may provide more rapid relief of suicidal ideation than may be possible with psychopharmacology or psychotherapeutic interventions 29.
Suicidal ideation resolved in 80.9% of patients with baseline SI in a prior randomized trial of bilateral ECT8, and in 75.6% of patients in a registry study of ECT in Sweden10. Fewer patients in this study had resolution of SI (47.8% in an unadjusted model; 64.0% in an adjusted model) which may reflect differences in baseline patient characteristics between study sites or possible true differences in treatment efficacy. The majority of patients in this study were treated initially with ultrabrief pulse unilateral ECT, as opposed to bilateral or unilateral brief pulse treatments. While these techniques have been compared for overall efficacy in depression treatment in multiple studies30–32, potential differences in treatment of suicidal ideation have not been explored. While emergent SI in individuals without baseline SI was uncommon in this sample, it did occur in a minority of patients, which supports ongoing careful monitoring of individuals receiving ECT for new or worsening suicidal symptoms.
In a subgroup analysis, more severe baseline SI was associated with a higher odds of persistent SI despite treatment. Persistent SI was also more common in outpatient ECT recipients. As patients requiring hospitalization might be expected to have more severe baseline disease, this suggests that non-ECT treatments received during hospitalization may be responsible for some of the observed improvements in SI. Alternatively, outpatients and inpatients may differ in the nature or chronicity of SI as well as in comorbidities such as personality disorders, which may affect ECT responsiveness. Additionally, switching ECT electrode placement was associated with a higher odds of persistent SI. As this was a non-randomized trial, treatment switching was made based on clinical discretion, and so the association between treatment switching and persistent SI suggests that clinicians may be switching electrode placement in patients who are not adequately responding to the initial treatment modality. While this is often utilized in practice 28, the possible risks and benefits of this strategy are uncertain and will be explored in an ongoing prospective trial 33. In this sample, age was not associated with a higher odds of persistent SI, which is discordant from prior results indicating greater relief of SI in older individuals8,10.
Strengths of this study include its large sample size, with broad inclusion criteria making the sample more likely to be representative of typical clinical practice. We included patients of all diagnoses in the sample, allowing for greater generalizability of findings to other patients receiving ECT.
Limitations
This study relies on a single question about suicidal ideation from the QIDS. Similar single item suicide scales have demonstrated predictive value for suicide attempts and suicide deaths34,35, but this has not been explored specifically for the QIDS. We are unable to control for the effects of concomitant pharmacologic or psychotherapeutic treatments occurring during ECT treatment, which may confound the influence of ECT on self-reported SI. Additionally, while these results explore self-reported SI, we do not have data regarding suicidal behaviors or suicide attempts among patients, and are unable to assess the durability of improvements in SI following the completion of ECT. Additionally, many patients continued in the acute course beyond treatment #10, and so ECT may have had additional effects beyond the course analyzed in this paper. Analysis of further ECT for these patients and/or further switch to more aggressive forms of ECT, such as bitemporal placement, would be worthy of further investigation. Finally, as results of this study are based on patient self-report, individuals unwilling or unable to complete self-report scales are not included, which may hinder analysis of the most ill patients who may not have been physically or cognitively able to complete baseline or follow-up assessments (for instance due to severe neurovegetative symptoms).
Conclusion
Among 2,554 patients, 1,931 of whom had SI at baseline, treatment with ECT was associated with a reduction in self-reported SI, with a majority of patients with SI reporting resolution of these symptoms in an adjusted model. More severe baseline SI was associated with higher odds of persistent SI at the end of treatment, but age and sex were not associated with SI persistence.
Supplementary Material
Significant Outcomes:
- Among 2,554 patients treated with ECT, 1,931 (75.6%) endorsed SI at baseline
- ECT was associated with resolution of SI over the course of treatment for the majority of patients; emergent SI in individuals without baseline SI was uncommon
- More severe SI at baseline and outpatient treatment were associated with higher odds of persistent SI at the end of treatment
Limitations:
- Single study center from retrospective chart review
- SI evaluated using single item self-report; no information about suicidal behavior or suicide deaths
- Effects of concomitant medication changes cannot be assessed
Funding
This work was supported by the National Institute of Mental Health (T32MH112485, JL) and the National Institute on Aging (5R01AG061100–02; DH, MM) The sponsors had no role in study design, writing of the report, or data collection, analysis, or interpretation.
Footnotes
Conflicts of Interest
JL receives research funding from the National Institute of Mental Health and Harvard Medical School. He holds equity in Revival Therapeutics. THM receives research funding from the Stanley Center at the Broad Institute, the Brain and Behavior Research Foundation, National Institute of Mental Health, National Human Genome Research Institute Home, and Telefonica Alfa. MM receives research funding from the National Institutes of Health (NI of Aging, Nursing Research, Minority Health and Health Disparities, Heart Lung and Blood, Child Health and Human Development) and Agency for Healthcare Research and Quality. DH receives research funding from the National Institutes of Health (NI of Aging, Heart Lung and Blood). The remaining authors have no disclosures to report.
Data Availability Statement:
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- 1.World Health Organization. Suicide Worldwide in 2019: Global Health Estimates. World Health Organization; 2021. Accessed February 14, 2023. https://apps.who.int/iris/handle/10665/341728 [Google Scholar]
- 2.Stone DM, Mack Karen A., Qualters Judith. Notes from the Field: Recent Changes in Suicide Rates, by Race and Ethnicity and Age Group — United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72(6):160–162. doi: 10.15585/mmwr.mm7206a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glenn CR, Nock MK. Improving the Prediction of Suicidal Behavior in Youth. Int J Behav Consult Ther. 2014;9(3):7–10. [PMC free article] [PubMed] [Google Scholar]
- 4.Czyz EK, Glenn CR, Arango A, Koo HJ, King CA. Short-term associations between nonsuicidal and suicidal thoughts and behaviors: A daily diary study with high-risk adolescents. J Affect Disord. 2021;292:337–344. doi: 10.1016/j.jad.2021.05.104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ribeiro JD, Franklin JC, Fox KR, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. 2016;46(2):225–236. doi: 10.1017/S0033291715001804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luccarelli J, McCoy TH Jr, Seiner SJ, Henry ME. Real-world evidence of age-independent electroconvulsive therapy efficacy: A retrospective cohort study. Acta Psychiatr Scand. 2022;145(1):100–108. doi: 10.1111/acps.13378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fink M, Kellner CH, McCall WV. The Role of ECT in Suicide Prevention. J ECT. 2014;30(1):5–9. doi: 10.1097/YCT.0b013e3182a6ad0d [DOI] [PubMed] [Google Scholar]
- 8.Kellner CH, Fink M, Knapp R, et al. Relief of Expressed Suicidal Intent by ECT: A Consortium for Research in ECT Study. Am J Psychiatry. 2005;162(5):977–982. doi: 10.1176/appi.ajp.162.5.977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luccarelli J, McCoy TH, Seiner SJ, Henry ME. Electroconvulsive therapy is associated with a reduction in self-reported suicidal ideation in adolescents. Brain Stimul Basic Transl Clin Res Neuromodulation. 2022;15(5):1181–1183. doi: 10.1016/j.brs.2022.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sienaert P, Brus O, Lambrichts S, et al. Suicidal ideation and ECT, ECT and suicidal ideation: A register study. Acta Psychiatr Scand. 2022;146(1):74–84. doi: 10.1111/acps.13425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Avery D, Winokur G. Suicide, Attempted Suicide, and Relapse Rates in Depression: Occurrence After ECT and Antidepressant Therapy. Arch Gen Psychiatry. 1978;35(6):749–753. doi: 10.1001/archpsyc.1978.01770300091010 [DOI] [PubMed] [Google Scholar]
- 12.Salagre E, Rohde C, Østergaard SD. Self-Harm and Suicide Attempts Preceding and Following Electroconvulsive Therapy: A Population-Based Study. J ECT. 2022;38(1):13. doi: 10.1097/YCT.0000000000000790 [DOI] [PubMed] [Google Scholar]
- 13.Rönnqvist I, Nilsson FK, Nordenskjöld A. Electroconvulsive Therapy and the Risk of Suicide in Hospitalized Patients With Major Depressive Disorder. JAMA Netw Open. 2021;4(7):e2116589–e2116589. doi: 10.1001/jamanetworkopen.2021.16589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munk-Olsen T, Laursen TM, Videbech P, Mortensen PB, Rosenberg R. All-cause mortality among recipients of electroconvulsive therapy: Register-based cohort study. Br J Psychiatry. 2007;190(5):435–439. doi: 10.1192/bjp.bp.106.026740 [DOI] [PubMed] [Google Scholar]
- 15.Jørgensen MB, Rozing MP, Kellner CH, Osler M. Electroconvulsive therapy, depression severity and mortality: Data from the Danish National Patient Registry. J Psychopharmacol (Oxf). 2020;34(3):273–279. doi: 10.1177/0269881119895518 [DOI] [PubMed] [Google Scholar]
- 16.Rhee TG, Sint K, Olfson M, Gerhard T, H. Busch S, Wilkinson ST. Association of ECT With Risks of All-Cause Mortality and Suicide in Older Medicare Patients. Am J Psychiatry. 2021;178(12):1089–1097. doi: 10.1176/appi.ajp.2021.21040351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luccarelli J, Henry ME, McCoy TH. Demographics of Patients Receiving Electroconvulsive Therapy Based on State-Mandated Reporting Data. J ECT. 2020;36(4):229–233. doi: 10.1097/YCT.0000000000000692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaster TS, Blumberger DM, Gomes T, et al. Patient-level Characteristics and Inequitable Access to Inpatient Electroconvulsive Therapy for Depression: A Population-based Cross-sectional Study: Caractéristiques au niveau du patient et accès inéquitable à la thérapie électroconvulsive pour patients hospitalisés. Can J Psychiatry Rev Can Psychiatr. 2021;66(2):147–158. doi: 10.1177/0706743720935647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steinholtz L, Reutfors J, Brandt L, et al. Response rate and subjective memory after electroconvulsive therapy in depressive disorders with psychiatric comorbidity. J Affect Disord. 2021;292:276–283. doi: 10.1016/j.jad.2021.05.078 [DOI] [PubMed] [Google Scholar]
- 20.Williams M, Rummans T, Sampson S, et al. Outcome of ECT by Race in the CORE Multi-Site Study. J ECT. 2008;24(2):117–121. doi: 10.1097/YCT.0b013e31815c6641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8 [DOI] [PubMed] [Google Scholar]
- 22.Eisen SV, Normand SL, Belanger AJ, Spiro AI, Esch D. The Revised Behavior and Symptom Identification Scale (BASIS-R): Reliability and Validity. Med Care. 2004;42(12):1230–1241. [DOI] [PubMed] [Google Scholar]
- 23.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 24.Luccarelli J, McCoy TH, Seiner SJ, Henry ME. Charge required to induce a seizure during initial dose titration using right unilateral brief pulse electroconvulsive therapy. Brain Stimul Basic Transl Clin Res Neuromodulation. 2020;13(6):1504–1506. doi: 10.1016/j.brs.2020.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luccarelli J, McCoy THJ, Seiner SJ, Henry ME. Total Charge Required to Induce a Seizure in a Retrospective Cohort of Patients Undergoing Dose Titration of Right Unilateral Ultrabrief Pulse Electroconvulsive Therapy. J ECT. 2021;37(1):40–45. doi: 10.1097/YCT.0000000000000714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luccarelli J, McCoy TH, Shannon AP, Forester BP, Seiner SJ, Henry ME. Rate of continuing acute course treatment using right unilateral ultrabrief pulse electroconvulsive therapy at a large academic medical center. Eur Arch Psychiatry Clin Neurosci. 2021;271(1):191–197. doi: 10.1007/s00406-020-01202-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Luccarelli J, McCoy THJ, Shannon AP, Forester BP, Seiner SJ, Henry ME. Duration of Treatment in Electroconvulsive Therapy Among Patients Beginning With Acute Course Right Unilateral Brief Pulse Stimuli. J ECT. 2021;37(4):238–242. doi: 10.1097/YCT.0000000000000768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hart KL, McCoy TH Jr., Henry ME, Seiner SJ, Luccarelli J. Factors associated with early and late response to electroconvulsive therapy. Acta Psychiatr Scand. 2023;147(4):322–332. doi: 10.1111/acps.13537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mann JJ, Michel CA, Auerbach RP. Improving Suicide Prevention Through Evidence-Based Strategies: A Systematic Review. Am J Psychiatry. 2021;178(7):611–624. doi: 10.1176/appi.ajp.2020.20060864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loo CK, Sainsbury K, Sheehan P, Lyndon B. A comparison of RUL ultrabrief pulse (0.3 ms) ECT and standard RUL ECT. Int J Neuropsychopharmacol. 2008;11(07). doi: 10.1017/S1461145708009292 [DOI] [PubMed] [Google Scholar]
- 31.McCormick LM, Brumm MC, Benede AK, Lewis JL. Relative ineffectiveness of ultrabrief right unilateral versus bilateral electroconvulsive therapy in depression. J ECT. 2009;25(4):238–242. doi: 10.1097/YCT.0b013e31819fdff7 [DOI] [PubMed] [Google Scholar]
- 32.Semkovska M, Landau S, Dunne R, et al. Bitemporal Versus High-Dose Unilateral Twice-Weekly Electroconvulsive Therapy for Depression (EFFECT-Dep): A Pragmatic, Randomized, Non-Inferiority Trial. Am J Psychiatry. 2016;173(4):408–417. doi: 10.1176/appi.ajp.2015.15030372 [DOI] [PubMed] [Google Scholar]
- 33.Sienaert P, McLoughlin DM. Changing tactics: Does switching improve electroconvulsive therapy outcomes? Acta Psychiatr Scand. 2023;147(4):319–321. doi: 10.1111/acps.13540 [DOI] [PubMed] [Google Scholar]
- 34.Simon GE, Rutter CM, Peterson D, et al. Does Response on the PHQ-9 Depression Questionnaire Predict Subsequent Suicide Attempt or Suicide Death? Psychiatr Serv. 2013;64(12):1195–1202. doi: 10.1176/appi.ps.201200587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Green KL, Brown GK, Jager-Hyman S, Cha J, Steer RA, Beck AT. The Predictive Validity of the Beck Depression Inventory Suicide Item. J Clin Psychiatry. 2015;76(12):1683–1686. doi: 10.4088/JCP.14m09391 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


