Abstract
Introduction:
The overall impact of social connectedness on health outcomes in older adults living in nursing homes and assisted living settings is unknown. The purpose of this paper was to synthesize the literature regarding the health impact of social connectedness among older adults living in nursing homes or assisted living settings.
Methods:
Using PRISMA guidelines, we identified eligible studies from Scopus, MEDLINE, PsycINFO, CINAHL, and Cochrane databases (1990 - 2021). Bias and quality reporting assessment was performed using standardized criteria for cohort, cross-sectional, and qualitative studies. At each stage, ≥ 2 researchers conducted independent evaluations.
Results:
Of the 7,350 articles identified, 25 cohort (follow-up range: one month - 11 years; with 2 also contributing to cross-sectional), 86 cross-sectional, 8 qualitative, and 2 mixed methods were eligible. Despite different instruments used, many residents living in nursing homes and assisted living settings had reduced social engagement. Quantitative evidence supports a link between higher social engagement and health outcomes most studied (e.g., depression, quality of life). Few studies evaluated important health outcomes (e.g., cognitive and functional decline). Most cohort studies showed that lack of social connectedness accelerated time to death.
Conclusions:
Social connectedness may be an important modifiable risk factor for adverse health outcomes for older adults living in nursing homes and assisted living facilities. Most studies were cross-sectional and focused on quality of life and mental health outcomes. Longitudinal studies suggest that higher social engagement delays time to death. Evidence regarding other health outcomes important to older adults was scant and requires further longitudinal studies.
Keywords: social connectedness, social engagement, nursing homes, assisted living, mental health, mortality
1. Introduction
The overall impact of social connectedness on health outcomes in older adults living in nursing homes and assisted living settings around the world is unknown. Social connectedness has been described as belonging to a web of key relationships, community, and engagement in purposeful activities in support of a valued current state (Herzog, 2002; Holt-Lundstad, 2022; "Social Connectedness: Evaluating the Healthy People 2020 Framework: The Minnesota Project," 2010). Dimensions of social connectedness are categorized into three domains: structural (e.g., social networks, integration, and affiliation), functional (e.g., perceived and received social support), and quality (e.g., social inclusion or exclusion) (Holt-Lundstad, 2022). In long-term care settings (i.e., nursing homes, assisted living), connectedness to others is key to quality of life (QOL) as social ties with peer residents can lead to a sense of belonging and being valued by others (Bradshaw, 2012; Kang et al., 2021). In nursing homes, deficits in social connectedness may be felt most acutely among residents who are cognitively impaired (Bova et al., 2021; Cahill, 2011).
Health outcomes are individual or group health status changes ascribed to interventions (Lee & Leung, 2014). They are measured either by the decline or gain in physical functioning (e.g., activities of daily living and mobility) and psychological functioning (e.g., depression and life satisfaction) in long-term care settings (Edvardsson et al., 2019). Although QOL is used interchangeably as an outcome or construct in the literature (Costa et al., 2021), it is often measured as a health-related outcome in long-term care settings (Aspen et al., 2014; Edvardsson et al., 2019). Given the unclear health impact of social connectedness for older adults in congregate long-term care settings worldwide, a comprehensive systematic review is required to evaluate the overall relationship between social connectedness and health outcomes for them. This is because there is great heterogeneity with respect to the size of long-term care facilities, the populations of older adults they serve, organizational structures (e.g., staffing types, staff-to-resident ratios, turnover), and available community-based resources, and these characteristics can either promote or discourage social connectedness (Clemens et al, 2022). For instance, a smaller number of beds, a home-like environment, a higher staffing level, and a location in an urban area are associated with greater social connectedness (Castle & Fogel, 1998; Clemens et al., 2022; Garre-Olmo et al., 2012; Yoon et al., 2016).
The overall goal of this in-depth review of literature is to synthesize the qualitative and quantitative evidence about this relationship among older adults living in congregate settings (i.e., nursing homes and assisted living) in various countries. In performing this systematic review, we aim to identify consistencies in the evidence, highlight opportunities for improving the evidence base, and identify research gaps in need of further study.
2. Methods
This study was the second of two planned systematic reviews. The first focused on social isolation and loneliness (Lapane, 2022). The current systematic review includes quantitative and qualitative studies on social connectedness and engagement. The systematic review followed the guidance of the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) (Moher, 2009; Shamseer, 2015). Because this was a systematic review of published research, it was not considered human subjects research. For this reason, we did not seek study approval from the University Institutional Review Board.
2.1. Inclusion and Exclusion Study Criteria
Our inclusion criteria for the review were as follows: peer-reviewed, published in English between January 1, 1990, and August 31, 2021, used human subjects and qualitative and quantitative studies that examined social connectedness in congregate long-term care settings for older adults with health conditions as outcomes.
Conversely, our exclusion criteria for this review were studies that were not published in English (due to the lack of translation resources) and between January 1, 1990, and August 31, 2021, did not use human subjects and were not peer-reviewed. We also excluded articles of the following conditions:
Pilot studies, feasibility studies, study protocols, case studies, review articles, intervention studies, and conference papers.
Studies focused on young adults living in congregate long-term care settings as our focus was on older adults.
Studies examined social connectedness as an outcome.
Studies that did not include information on social connectedness.
Studies examined either older adults in the community settings or did not differentiate older adults living in the community or congregate settings as we are interested only in congregate long-term care settings.
2.2. Search Strategy
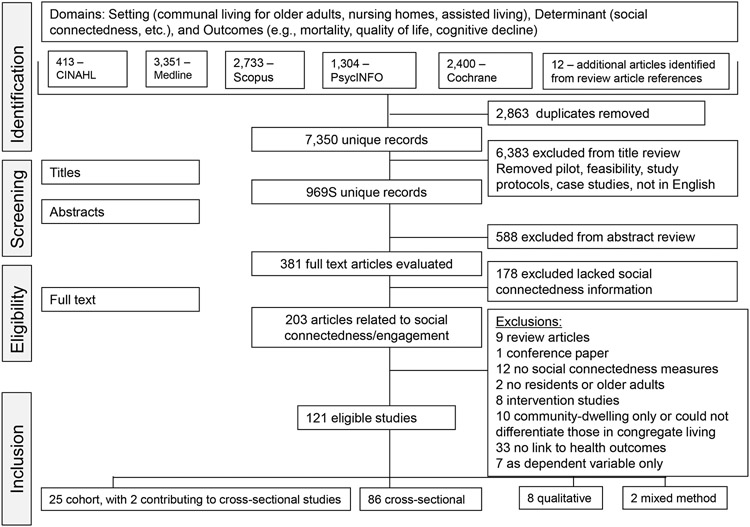
We worked with a research librarian to develop a search strategy to meet the needs of the systematic review. We shaped the search strategy in relation to three broad concepts: 1) social engagement and social connectedness, 2) health outcomes, and 3) setting (e.g., assisted living and nursing homes). The research team first developed keywords relevant to each concept. The research librarian next helped the team refine key words and develop search algorithms aligned with the domains of interest. The research librarian suggested we search five databases to cast a very wide net: PsycINFO, MEDLINE, CINAHL, Scopus, and Cochrane Reviews. The search algorithms used in these five databases consist of medical subject headings (MeSH) terms and text words in three aspects: 1) setting – congregate long-term care for older adults (e.g., nursing homes and assisted living); 2) determinants – factors associated with social connectedness; and 3) outcomes – health outcomes associated with older adults (e.g., mortality, cognitive decline, depression, and quality of life). Based on our inclusion and exclusion criteria, we limited our search in each database to include studies published between January 1, 1990, and August 31, 2021. We excluded studies that were not published in English or lacked human subjects. Articles contributing to our understanding of the association between measures of social connectedness and health outcomes were identified. A search of PROSPERO (Page, 2018) and Cochrane Reviews revealed no review on this topic (by C.E.D.) however, in the intervening time, a scoping review has been published (Lem et al, 2021). Figure 1 (see Appendix) provides the search strategy applied for the broader study.
Figure 1.
PRISMA Diagram
2.3. Review Process
Because of the vast number of articles meeting the search criteria (see Appendix), two reviewers first screened the titles to determine relevance. If either of these reviewers selected the article for further consideration, the article went on to the abstract review. For those articles proceeding to abstract review, two reviewers independently read each abstract. If both reviewers selected the abstract as eligible for full-text review, it proceeded in the process. If only one reviewer indicated it might be relevant for inclusion, a senior researcher (K.L.L.) made the final determination. We then obtained the full article for the articles deemed potentially eligible based on their title and abstract. In the last step of the eligibility determination phase, two reviewers independently evaluated each potential article for inclusion. Again, if both agreed it should move forward for further consideration, it did. If only one of the reviewers suggested it continue to be considered, a senior researcher (K.L.L.) made the final determination after re-reading and consulting with the reviewers’ notes. After this process, we identified a preliminary list of eligible studies. Additional studies may have been determined to be ineligible during the detailed abstraction process because, with detailed examination, new information was revealed that did not meet our inclusion criteria, such as ineligible study types (e.g., review articles or conference papers) or respondents’ characteristics (e.g., young adults or community-dwelling). We described these reasons for exclusion in Figure 1. Some of these articles described older adults as “elderly” and we do not endorse this ageist term. However, we retained these articles in our review so that our results would accurately reflect the extant literature in this area.
2.4. Quality Assessment
For quantitative studies, modified Downs and Black criteria (Downs, 1998) was used for cohort studies, and the Appraisal Tool for Cross-Sectional Studies (AXIS) (Downes, 2016) guided the evaluations for cross-sectional studies. For cross-sectional studies, areas of methodological quality reviewed included: 1) reporting of objectives; 2) sample selection; 3) threats to the internal validity of the study (e.g., confounding, misclassification, selection bias); 4) issues related to statistics (e.g., appropriate method, reporting of precision, power); and 5) generalizability of the study. Two or more reviewers completed the quality evaluation for each article. In the event of discordant ratings, the reviewers discussed until consensus was achieved.
Different criteria were used to evaluate the quality and bias in the qualitative studies. Using a modified version of the consolidated criteria for reporting qualitative research COREQ (Tong & Craig, 2007), two reviewers independently evaluated elements within three domains for each article: four items under the research team and reflexivity domain, eleven items under the study design domain, and eight items concerning the conduct and reporting of the analysis. Discrepancies were resolved through discussion between the two reviewers and consensus was easily achieved.
2.5. Data Extraction of Key Elements and Result Synthesis
Given the heterogeneity between quantitative and qualitative studies included, we employed a segregated design to synthesize them separately (Pearson et al., 2015; Sandelowski et al., 2006). Using a descriptive synthesis approach (Dixon-Wood et al., 2005; Xiao & Watson, 2019), we created tables to present the key elements to facilitate the organization and understanding of the studies included in the review. Identification of elements to extract flowed from our specific study question. For example, policies or resources surrounding nursing home operations and the timing of nursing home admissions can encourage or limit social connectedness among older adults, which vary as a function of geography and time (Lapane et al., 2022; Veiga-Seijo et al., 2022); thus we felt it was important to provide information on the location and time frame of the study. Further, in the United States, the quality of resident information in nursing homes appears to vary by residents’ race/ethnicity. Thus, we extracted information on the race/ethnicity of the study participants (if available). Regardless of the study design, we also extracted the study purpose and key sample characteristics. For qualitative and mixed method studies, we differentiated the study type, objective, methods used, and analytic technique applied. We also summarized key findings relevant to social connectedness and its impact on residents’ lives. For quantitative studies, we did not plan to perform a meta-analysis due to the likely heterogeneity of measures, and thus a descriptive approach was employed. First, we extracted the study objective. This was important because, for some, evaluating social connectedness was not the primary reason for the study. Such studies examined social connectedness as either a mediator, moderator, or risk factor (Y. Chen, Lin, K., Wu, C., Chen, C., & Hsieh, Y, 2020; Y. M Chen et al., 2009; Cuijpers & Van Lammeren, 1999; L. W. Guse, & Masesar, M. A., 1999; Kasser & Ryan, 1999; Papi, Karimi, Amini Harooni, Nazarpour, & Shahry, 2019) and are still included in our study. We also extracted information about the operational definitions of social connectedness, the operational definitions of the outcomes under study, and key findings (e.g., the extent of social connectedness and the association between social connectedness and the health outcome). For cohort studies, we also extracted the length of follow-up. To better understand the findings of the quantitative studies, we grouped them based on their study design and tabulated their findings on health impacts of social connectedness into three categories: positive, negative, or no impact, as presented in Table 5 (see Appendix). Overall, data extraction was accomplished by one member of the research team and a second member did a quality review check, verifying that the data extracted was accurate. Any differences were discussed until consensus was achieved. The agency funding for each study was not extracted as we did not believe there would be undue influence on the study findings.
Table 5.
Synthesis of quantitative evidence by study design
| Social connectedness | ||||
|---|---|---|---|---|
| Positive impact | Negative or no impact | |||
| Health outcomes | Cohort | Cross-sectional | Cohort | Cross-sectional |
| Death or hospital admission | 6 | 2 | ||
| Functional decline (cohort), physical function, cognitive decline | 2 | 2 | 1 | |
| Mental health: anxiety, depression, depressive symptoms, psychological well-being | 7 | 35 | 1 | 7 |
| Quality of life satisfaction with life, positive affect, self-esteem, morale, meaning in life, successful aging | 2 | 33 | 1 | 8 |
| Self-rated health | 1 | 6 | 2 | |
| Vitality, thriving | 3 | |||
| Underweight, malnutrition, insufficient energy intake, self-feeding dependence, weight loss | 1 | 2 | 3 | |
| CNS medication use: antipsychotic use or hypnotics | 1 (women) | 1 | 1 (men) | 1 |
| Symptoms: pain, dyspnea, fatigue, anomia, sleep | 1 | 5 | 1 | 2 |
| Aggressive behaviors, positive behaviors | 1 | 3 | 1 | |
| Urinary incontinence, pressure ulcers | 1 | 1 | 1 | |
The number of studies does not equal the total number of cohort and cross-sectional studies because some studies evaluated multiple health outcomes and some studies evaluated multiple dimensions of social connectedness.
2.6. Quality Assurance of Systematic Review
Multiple steps were taken to ensure the quality of this systematic review. The research team consulted with a research librarian and searched multiple databases, casting a wide net when developing search terms. Dual review was applied at all phases of the determination for eligibility, data extraction, and quality assessment. Discrepancies were resolved through discussion until consensus was achieved.
3. Results
3.1. Search Results
We identified 381 articles potentially eligible for the current study (Figure 1). From these articles, 178 did not include information on social connectedness or engagement and thus were excluded from further review. Of the remaining 203 articles, we excluded: nine review articles, one conference paper, 12 that did not include measures of social connectedness or engagement; two studies that did not include resident participants or older adults; eight intervention studies; 10 studies that included only those who were community-dwelling or living independently or that included older adults living either in the community or in congregate living settings, but did not stratify analysis by living setting; 33 studies that did not attempt to link social connectedness to a health outcome; and 7 that considered social connectedness as the dependent variable of interest. Of the remaining 121 eligible studies, 25 were cohort, 86 cross-sectional, eight were qualitative, and two were mixed methods. Two of the eligible cohort studies also had a cross-sectional component which were included in the synthesis of the cross-sectional analyses.
3.2. Qualitative and Mixed Methods Studies
Characteristics
Table 1 shows the characteristics of the eight qualitative studies and two mixed-methods studies that met the eligibility criteria. Of the 10 studies with a qualitative component, all were descriptive or exploratory in nature. The number of participants in the qualitative studies ranged from 12 (Moyle, Fetherstonhaugh, Greben, Beattie, & group, 2015) to 56 (Kaelen et al., 2021) residents. Two studies used focus groups (with residents [Leung, Wu, Lue, & Tang, 2004], with direct care staff along with interviews conducted with residents [Kaelen et al., 2021]) and the rest used interviews (with two studies [Bergland & Kirkevold, 2006, 2007] using open-ended interviews with a subset of field observations rather than a semi-structured interview format). In addition to residents, some studies included direct care staff (Kaelen et al., 2021), caregivers, and family members (Adra, Hopton, & Keady, 2015) as participants. In all studies, at least half of the participants were women (range: 50.0% [Leung et al., 2004] to 85.7% [E. Cho et al., 2017]), and all included older adults. In studies reporting participants’ marital status (Baldacchino & Bonello, 2013; Moyle et al., 2011), most were separated, widowed, or single. No studies reported the race/ethnicity of the participants. One of the two mixed methods studies included a cross-sectional study (Baldacchino & Bonello, 2013) and the other a cohort study (Potter, Sheehan, Cain, Griffin, & Jennings, 2018) to complement the exploratory qualitative research.
Table 1.
Characteristics of eligible qualitative studies or mixed-methods studies on the association between social connectedness and health outcomes among older adults living in nursing homes or assisted living facilities
| (Author, Year) Method Location (Year data collected) |
Objective | # of Residents and Description |
Sample Description % Female Age (years) % Race/Ethnicity % Marital status |
Main Findings |
|---|---|---|---|---|
| Qualitative studies | ||||
| (Adra et al., 2015) Descriptive, exploratory Lebanon (2010 to 2011) |
Explore the perspectives of quality of life for older residents, care staff, and family |
Design: Semi-structured interviews Participants: 20 residents living in 2 nursing homes, 11 caregivers, and 8 family members |
Residents: Female: 55.0% Age (Range: 65-91): 73.7 Race/ethnicity not reported. Marital status not reported. |
Findings from residents: Maintaining family connectedness and maintaining and developing significant relationships contributed to quality of life. Conversations with family/friends were meaningful. Close bonds with others in the home created a feeling of continuity between past and present circumstances. Inadequate staffing/workload prevented more meaningful interactions between residents and staff. |
| (Bergland & Kirkevold, 2006) Descriptive, exploratory Norway (Dates of data collection not reported.) |
Investigate mentally lucid residents’ perspective on what contributes to thriving in a nursing home |
Design: Open-ended interviews and field observations Participants: 26 residents living in 2 nursing homes 16 residents included in the field observation |
Female: 76.9% Women Age: 89.5 (Range: 74 to 103) Men Age: 89.0 (Range: 81 to 99) Race/ethnicity not reported. Marital status not reported. |
The innermost core aspect was mental attitude towards living in a nursing home. Essential to thriving was the quality of care and caregivers. Two of the five additional aspects contributing to thriving were positive relationships with peers and family but were not considered to be the core aspect contributing to thriving. |
| (Bergland & Kirkevold, 2007) Descriptive, exploratory Norway (Dates of data collection not reported.) |
Describe nursing home residents’ perceptions of the significance of relationships with peer residents to thriving |
Design: Open-ended interviews and field observations Participants: 26 residents living in 2 nursing homes 16 residents field observation |
Female: 76.9% Age: 89.4 (Range: 74 to 103) Race/ethnicity not reported. Marital status not reported. |
Personal relationships with peer residents were not essential to thriving. The expectations, wishes, and capacity to interact with other residents varied, as did the importance of these relationships to thriving. Caregivers have a major impact on whether and how social encounters and interactions develop into positive relationships that contributed to thriving. Participating in activities did not help them form relationships that contributed to thriving. |
| (E. Cho et al., 2017) Descriptive with thematic analysis South Korea (2015) |
Explore older adults’ perceptions of daily lives in nursing homes |
Design: Semi-structured interviews Participants: 21 older adults with normal cognitive function living in 5 nursing homes |
Women: 85.7% Age: 83.6±7.1 Race/ethnicity not reported. Marital status not reported. |
One of five themes that emerged related to residents’ desire for meaningful interpersonal relationships was to improve their quality of life. Some reported that difficulty ambulating and living with others who have cognitive impairment made it difficult to develop personal relationships. |
| (Kaelen et al., 2021) Thematic content analysis Belgium (2020) |
Understand psychosocial and mental health needs of nursing home residents during COVID-19 |
Design: Semi-structured interviews with residents Focus groups with direct care staff Participants: 56 residents living in 8 nursing homes without severe cognitive impairment |
Women: 62.5% Age (Range: 58 to 101): <79: 34.0% 80-89: 37.5% >90: 28.6% Race/ethnicity not reported. Marital status not reported. |
Residents reported losing their social connections both inside and outside of the nursing homes, with uncertainty about when their social life could resume. Some residents reported cognitive and physical decline, symptoms of depression, and suicidal ideation as a result. |
| (Leung et al., 2004) Exploratory Taiwan (Dates of data collection not reported.) |
Compare components of quality of life among older nursing home residents to those living in the community |
Design: 4 focus groups (2 groups of men from nursing homes, 2 groups of women from nursing homes) 2 focus groups from community (1 with men only, 1 with women only) Participants: 28 older nursing home residents 16 community-dwelling older adults |
Women: 50.0% Age: 75.4±5.7 Race/ethnicity not reported. Marital status not reported. |
Of six dimensions identified, one was related to social function. Within the social function domain, domains included: connectedness, exercise and leisure activities, social activities, and services. Regardless of setting, older adults noted that social connections with people (especially spouse, children, grandchildren) and society is important and that social activities are sources of self-efficacy. For those living in nursing homes, friendship and kinship were emphasized, as was self-needs whereas for community-dwelling older adults, relationships with family and family needs were emphasized. |
| (Moyle et al., 2011) Exploratory New South Wales and Queensland Australia (Dates of data collection not reported.) |
Understand factors that influence quality of life for people living with dementia in long-term care |
Design: Semi-structured interviews Participants: 32 residents living in 4 long-term care facilities, aged ≥65 years with dementia |
Women: 68.8% Age group: 70-79: 9.4% 80-89: 78.1% ≥ 90: 12.5% Race/ethnicity not reported. Married: 37.5% Widowed: 56.3% Single/Divorced: 6.2% |
Connections to family: Residents noted the importance of being with family and the opportunities this provided for meaningful conversations (e.g., recall previous memories, link them to the community). Family involvement improved their quality of life. Connections to staff: When family and friends no longer visited, some residents looked towards staff for companionship. But staff did not fulfil residents’ emotional needs and were too busy doing their jobs. Connections with other people (residents): Connections with other residents were important for quality of life. Limited relationships were blamed on others not reaching out (rather than under the control of the residents themselves). Forming of relationships was a challenge for some residents. |
| (Moyle et al., 2015) Descriptive with thematic analysis Brisbane and Melbourne, Australia (Date of data collection not reported.) |
Understand what influences quality of life and strategies to improve quality of life of older people with dementia living in long-term care |
Design: Semi-structured interviews Participants: 12 residents living in 4 long-term care facilities (3 from each) with early-stage dementia |
People with dementia: Women: 75.0% Age: 89.0±8.3 Race/ethnicity not reported. Marital status not reported. |
Social interactions and satisfaction were key factors improving quality of life. Residents commented on interactions with family, friends, and residents/staff (at times not being able to differentiate staff from residents). Family: For many, quality of life was about family as they provided meaning, enjoyment, and support. Friends: Most did not mention friends from outside the facility. Memory loss affected ability to maintain friendships. Residents and staff: Being in a facility provides company. Half thought the residents provided an important source of social interactions. One participant didn’t feel he could have good conversations in the facility. Others suggested they can’t walk around to have conversations. Staff lacked time to have meaningful conversations. |
| Mixed method studies | ||||
| (Baldacchino & Bonello, 2013) Descriptive, exploratory and a cross-sectional study Malta and Australia (Dates of data collection not reported.) |
Evaluate factors related to anxiety and depression |
Design: Semi-structured interviews Participants: Older adults living in 6 nursing homes participated in the quantitative (137 residents) and qualitative study (42 residents) |
Quantitative sample: Female: 75.2% Age: 72.8 Married: 13.1% Separated/Widowed: 53.3% Single: 33.6% Qualitative sample: Female: 73.8% Age: 71.9 Race/ethnicity not reported. Married: 14.3% Separated/Widowed: 61.9% Single: 23.8% |
Three contributing factors to anxiety and depression included adaptation to institutional living, physical functioning, and personal outlook towards the future. Within the adaptation to institutional living theme, social support, social activities, and positive relationships with family, roommates, and pets were important factors to control anxiety and depression. |
| (Potter et al., 2018) Exploratory study using thematic framework and a prospective cohort study United Kingdom |
Explore the relationship between the physical environment and depressive symptoms |
Qualitative: Semi-structured interviews 15 residents in 4 care homes Quantitative: 510 residents in 50 care homes |
Qualitative sample: Female: 80% Age (range: 68-95): 85 Quantitative sample: Female: 77.0% Age: 86.4±7.3 Race/ethnicity not reported. Marital status not reported. |
The mean MDS 2.0 based index of social engagement was 4.6±1.8. The association between the index of social engagement and the geriatric depression scale (GDS-15) (adjusted for resident characteristics) did not hold when residential environmental characteristics were added to the model (β= −0.11; 95% confidence interval: −0.25 to 0.02). |
Determined from lead author via email correspondence.
Mean Age±SD (years)
Described like assisted living homes.
Findings
Most qualitative studies highlighted the importance of social connectedness on health outcomes, including QOL (Adra et al., 2015; E. Cho et al., 2017; Moyle et al., 2015; Moyle et al., 2011), cognitive and physical decline (Kaelen et al., 2021), symptoms of depression (Baldacchino & Bonello, 2013; Kaelen et al., 2021), and suicidal ideation (Kaelen et al., 2021). Two studies (Bergland & Kirkevold, 2006, 2007) suggested that positive peer relationships contributed to (but were not essential to) thriving in the nursing home setting. Barriers to developing social relationships included difficulty ambulating and living with others who have cognitive impairment (E. Cho et al., 2017; Moyle et al., 2015). Barriers to developing meaningful interactions with staff included staff shortages and heavy workloads (Adra et al., 2015; Moyle et al., 2015; Moyle et al., 2011). One mixed methods study (Baldacchino & Bonello, 2013) found that social connectedness was an important factor in controlling anxiety and depression, while another study (Potter et al., 2018) found that the association between social engagement and depression was explained by residential environmental characteristics.
3.3. Cross-sectional Studies
Characteristics
Table 2 shows that 27 of the eligible cross-sectional studies were conducted in the United States, thirteen in China, and twelve in Taiwan. Eight studies were a secondary analysis of data from a previous study (J. Cho et al., 2012; Choi, Jung, & Kim, 2018; Hsiao & Chen, 2018; H. Lee, Park, Kwon, & Cho, 2017; M. McCabe et al., 2021; Morrison-Koechl et al., 2021; Randall et al., 2011; Smit, de Lange, Willemse, Twisk, & Pot, 2016). Nine studies (Beck & Ovesen, 2003; Y. M. Chen, Hwang, Chen, Chen, & Lan, 2009; Degenholtz, Kane, Kane, Bershadsky, & Kling, 2006; Hjaltadóttir, Ekwall, Nyberg, & Hallberg, 2012; Kang, 2012; Li, Chang, & Porock, 2015; Saleh et al., 2017; Smit et al., 2016; Vanbeek, Frijters, Wagner, Groenewegen, & Ribbe, 2011) used the Minimum Data Set data and administrative data. For the studies collecting primary data, most had trained members of the research team to conduct structured interviews (face-to-face) or distribute self-administered surveys and six studies (Björk et al., 2017; Y. Chen, Ryden, M. B., Feldt, K., & Savik, K, 2000; Cohen-Mansfield & Marx, 1992; Damian, Pastor-Barriuso, & Valderrama-Gama, 2008; Fernández-Mayoralas, 2015; Marventano et al., 2015) relied on nursing home staff to collect information on the residents. Among the studies reporting the duration of the interviews, the study with the shortest interview reported 25 minutes duration (Yeung, Kwok, & Chung, 2012); the studies with the longest interview time (Bitzan, 1998; Maenhout et al., 2020) had interviews that were at least 2 hours over two sessions. One study (Beerens et al., 2016) performed an ecological momentary assessment of residents, and two studies (Jao, Loken, MacAndrew, Van Haitsma, & Kolanowski, 2018; H. Lee et al., 2017) involved video recordings. Although not all studies mentioned the sampling strategy employed, many studies noted the use of convenience samples. The study with the smallest sample size (Wahyuni, Shahdana, & Armini, 2019) included 20 residents, and the study (Björk et al., 2017) with the largest sample size included 4,831 residents. Four studies (Carpenter, 2002; H. T. Chang, Liu, L. F., Chen, C. K., Hwang, S. J., Chen, L. K., & Lu, F. H, 2010; Y. M. Chen et al., 2009; Ghusn, Hyde, Stevens, Hyde, & Teasdale, 1996) were conducted in nursing homes serving veterans that included no women, and one study had all women (Wahyuni et al., 2019). The study (Randall et al., 2011) with the oldest participants (mean age: 99.8±1.7) was specifically targeting centenarians. Marital status was not reported in 26 studies. In the studies that did report marital status, there was heterogeneity in the proportion of married (range: 3.9% [Tosangwarn, Clissett, & Blake, 2017] to 61.6% [Onunkwor et al., 2016]). Race/ethnicity was not reported in 65 studies.
Table 2.
Characteristics of cross-sectional studies on the association between social connectedness/engagement and health outcomes among older adults living in congregate long-term care settings
| (Author, Year) Location |
Objective | Data Source (Years of data) |
# of Residents and Description |
Sample Description % Female Age (years) % Marital status indicators % Race/Ethnicity |
|---|---|---|---|---|
| (Beck & Ovesen, 2003) Denmark |
Estimate the influence of social engagement and dining location on dietary intake | Minimum Data Set (MDS) 2.0 data collected by registered dietician and cross-checked with nurses and medical records Energy intake derived from 4-day estimated dietary records (Not reported) |
40 residents in 2 nursing homes | Female: 82% Mean age: 83 (Range: 80-85) Marital status not reported. Race/ethnicity not reported. |
| (Beerens et al., 2016) Netherlands |
Investigate which aspects of daily life are related to quality of life | Ecological momentary assessment of residents (Not reported) |
115 residents with dementia living in 18 long-term care facilities | Female: 75.0% Mean age: 83.8±7.8 Widowed: 66% Race/ethnicity not reported. |
| (Bitzan, 1998) Wisconsin, USA |
Examine the association between nursing home roommate relationships and subjective well-being | Structured questionnaires administered by research staff to residents, face-to-face (Duration on average 2 hours held over 2 sessions) Convenience sample (Not reported) |
31 residents sharing rooms with non-relatives for a ≥ 2 months | Female: 93.5% Mean age: 83 (range: 51-99) Marital status not reported. All were white; most were of German and Polish descent. |
| (Björk et al., 2017) Sweden |
Estimate the extent to which engagement in everyday activities is associated with thriving | Structured questionnaires administered to care staff who knew the residents best (2013-2014) |
4,831 residents in 172 nursing homes | Female: 67.8% Mean age: 85.5±7.8 Marital status not reported. Race/ethnicity not reported. |
| (Carpenter, 2002) Louisiana, USA |
Evaluate associations between dimensions of social support on psychological well-being | Structured questionnaires administered to patients; staff reported ADL assessment (Not reported) |
32 newly admitted to a Transitional Care Unit at a Veterans Affairs Medical Center | Female: 0% Mean age: 67.8±8.5 Married/Partnered: 41.0% Widowed: 19.0% Divorced/separated/never: 40.0% African American: 63.0% Euro-American: 37.0% |
| (H. T. Chang, Liu, L. F., Chen, C. K., Hwang, S. J., Chen, L. K., & Lu, F. H, 2010) Taiwan |
Evaluate quality of life and related factors of senior veterans | Structured questionnaires administered by investigator to residents, face-to-face (Not reported) |
260 residents aged ≥65 years without cognitive and hearing impairments, and living in 4 veterans’ homes for >3 months | Female: 0% Mean age: 82.9±4.7 Married: 18.8% Widowed: 18.8% Divorced/never: 59.2% Others: 3.1% Race/ethnicity not reported. |
| (L. Chang, 2015) Taiwan |
Examine whether leisure self-determination and social support were related to acute and chronic stress | Structured questionnaires administered by research staff to residents, face-to-face (2012) |
141 residents living in 2 nursing homes who were aged ≥65 years, no mental health conditions, and able to participate in leisure activities | Female: 62.4% Mean age: 79.4±7.1 Married: 7.8% Widowed: 72.4% Divorced: 8.5% Unmarried: 11.3% Race/ethnicity not reported. |
| (L. C. Chang, 2018) Taiwan |
Examine association between leisure self-determination and social support types on stress | Structured questionnaires administered by research staff to residents, face-to-face (Duration on average 35 minutes) (Not reported) |
139 residents living in 2 nursing homes who were aged ≥65 years, no mental health conditions, and able to participate in leisure activities | Female: 63.3% Mean age: 79.4±7.1 Married: 7.9% Widowed: 72.7% Divorced/never: 19.4% Race/ethnicity not reported. |
| (Chao, 2019) Taiwan |
Determine the association between activity participation and mental health | Structured questionnaires administered by research staff to residents, face-to-face Stratified probability sample (2014) |
634 residents living in 155 long-term care facilities >3 months, aged ≥60 years, able to understand and respond | Female: 60.0% Mean age: 78.3±9.1 Married: 23.7% Race/ethnicity not reported. |
| (Y. Chen, Ryden, M. B., Feldt, K., & Savik, K, 2000) Minnesota, USA |
Examine social interaction and physical, verbal, and sexual aggression | Research staff retrieved demographic and case mix information from medical records and administered several questionnaires to residents. Research staff guided nurses and nurses’ aides who completed key instruments based on observations of residents over a 3-week period. (Not reported) |
129 residents living in 3 nursing homes and expected to stay >6 months who were cognitively impaired with Mini-Mental Status Exam scores ≤24 and consistently aggressive | Female to male ratio: 2.5 to 1 Mean age: 85.6±7.8 Married: 29.5% Widowed: 58.9% Never: 11.6% Race/ethnicity not reported. |
| (Y. M. Chen et al., 2009) Taiwan |
Explore the relationship of urinary incontinence and physical function, cognitive status, depressive symptoms and quality of life | MDS 2.0 and structured questionnaires administered by trained nurse to residents, face-to-face (2006) |
594 residents living in 1 veterans nursing home aged ≥65 years | Female: 0% Mean age: 80.9±5.3 Marital status not reported. Race/ethnicity not reported. |
| (Y. Chen, Lin, L., Chuang, L., & Chen, M, 2017) Taiwan |
Examine the extent to which perceived social support and depression mediate the association between functional ability and spiritual well-being | Structured questionnaires administered by research staff to residents, face-to-face (2014-2015) |
377 residents living in 11 long-term care facilities ≥1 month, aged ≥65 years, with no hearing, visual, or cognitive impairments | Female: 61% Mean age: 79.1±10.4 Married: 25.7% Widowed: 56.0% Divorced/never: 17.0% Others: 1.3% Race/ethnicity not reported. |
| (Y. Chen, Lin, K., Wu, C., Chen, C., & Hsieh, Y, 2020) Taiwan |
Identify determinants of quality of life | Self-administered questionnaires with researchers’ guidance when needed Convenience sample (2016-2017) |
210 residents living in 1 long-term care facility ≥ 6 months, aged ≥65 years, able to answer questions, and scored ≥ 24 on Mini-Mental State Examination | Female: 58.1% Mean age: 80.3±9.74 Married: 37.1% Widowed: 51.4% Divorced/never: 11.4% Min Nan: 85.7% Hakka: 4.8% Aborigines: 1.0% Mainland Chinese: 8.6% |
| (Y. Chen et al., 2020) Wuhan, Yichang, Huanggang, Hangzhou, Jinhua, Haikou, Sanya, Xi’an, Xianyang, Shenzhen, Beijing, Chengdu, Chongqing, China |
Investigate the extent to which perceived social support and self-rated health mediate the relationship between pain and depression | Structured questionnaires administered by research staff to residents, face-to-face Convenience sample (2017-2018) |
2,154 residents living in 38 nursing homes aged ≥60 years, spoke Mandarin, without cognitive and severe hearing impairments | Female: 64.2% Mean age: 82.0±7.0 Married: 34.8% Divorced/widowed/never: 65.2% Race/ethnicity not reported. |
| (Cheng, Lee, & Chow, 2010) Hong Kong, China |
Investigate the extent to which structural and functional social support promote psychological well-being | Structured questionnaires administered by research staff to residents, face-to-face (Duration on average 30 minutes) (Not reported) |
71 residents living in 7 nursing homes with any activity of daily living limitation and Mini-Mental State Exam score ≥18 | Female: 80.3% Mean age: 80.9±6.14 Marital status not reported. Race/ethnicity not reported. |
| (Chipps & Jarvis, 2015) South Africa |
Investigate the association between social capital and mental well-being | Structured questionnaires administered by research staff to residents, face-to-face Purposeful sampling by management of residents who may be socially isolated (2013) |
75 residents living in 1 residential care facility, aged ≥60 years and cognitively intact | Female: 77.3% 60 – 75 years: 41.3% 76-100 years: 58.7% Widowed: 60.0% Divorced/never: 40.0% White: 77.3% Indian: 22.7% |
| (J. Cho et al., 2012) Georgia, USA |
Examine the relationship of functional indicators, psychological and situational factors and fatigue | Secondary analysis of data from The Georgia Centenarian Study (Poon, 2007) Structured questionnaires administered by research staff to residents, face-to-face (Not reported) |
62 residents living in long-term care facilities aged ≥ 98 years and cognitively intact | Characteristics of residents living in long-term care not provided separately from community dwelling participants. |
| (Choi et al., 2018) South Korea |
Identify contributing factors of aggressive behaviors | Secondary data analysis of a random sample of participants of a nationally representative sample Trained nurses and social workers working in the nursing homes completed the assessment form (2013) |
1,447 residents living in 91 nursing homes ≥ 1 month, aged ≥65 years | Female: 77.4% Mean age: 82.8 ± 7.5 Married: 18.8% Race/ethnicity not reported. |
| (Cohen-Louck & Aviad, 2020) Israel |
Examine the relationship between family support and social engagement and suicidal tendency levels and meaning in life | Structured questionnaires administered by research staff to residents, face-to-face (Not reported) |
92 independently functioning residents of 7 nursing homes and assisted living facilities | Female: 63.0% Mean age: 81.8 ± 7.4 Married: 19.6% Widowed: 60.8% Race/ethnicity not reported. |
| (Cohen-Mansfield & Marx, 1992) Maryland, USA |
Examine the relationship between social network characteristics and dimensions of agitation | Charge nurses and social workers completed the questionnaires (Not reported) |
408 residents living in 1 large nursing home | Female: 77.5% Mean age: 85 (range: 70-99) Married: 19.1% Race/ethnicity not reported. |
| (Commerford & Reznikoff, 1996) New York, USA |
Examine the relationship of perceived social support on depression and self-esteem | Structured questionnaires administered by the investigator to residents, face-to-face (Not reported) |
83 residents living in 4 nursing homes with ≤ 2 errors on the Mental Status Questionnaire | Female: 77.1% Mean age: 80.7±10.5 Marital status not reported. White: 84.3% African American:14.5% Hispanic: 1.2% |
| (Creighton, Davison, & Kissane, 2019) Australia |
Identify biopsychosocial factors associated with anxiety | Structured questionnaires administered by research staff to residents, face-to-face; research staff abstracted items from charts, and interviewed nursing staff using structured questionnaires (2015-2016) |
178 residents living in 12 nursing homes ≥3 months, aged ≥65 years, Mini-Mental State Exam score ≥18, with no/mild cognitive impairment, and no schizophrenia or bipolar affective disorder | Female: 66.3% Mean age: 85.4±7.4 Married: 19.1% Widowed: 52.8% Divorced/separated/never: 27.0% Race/ethnicity not reported. |
| (Cuijpers & Van Lammeren, 1999) Netherlands |
Explore the relationship between chronic illness and depression | Structured questionnaires administered by trained interviewers to residents, face-to-face; research staff interviewed nursing staff about resident’s chronic illnesses (nurses could refer to medical records) (Duration on average 1 hour) (Not reported) |
424 residents living in 10 residential homes who scored ≥ 18 on Mini-Mental State Examination | Female: 78.5% Age groups: <70: 2.1% 70-80: 23.7% 81-90: 57.8% >90: 16.4% Married: 10.5% Widowed: 74.3% Divorced: 3.8% Never: 11.3% Race/ethnicity not reported. |
| (Cummings, 2002) Southeastern USA |
Examine the effect of functional impairment and social support on well-being | Structured questionnaires administered by trained interviewers to residents, face-to-face (Duration on average 20 minutes) (Not reported) |
57 residents in an assisted-living facility who were without cognitive impairment or communication problems | Female: 78.6% Mean age: 83.7±7.4 Married: 19.6% White: 100% |
| (Cummings & Cockerham, 2004) Southeastern USA |
Explore factors associated with depression and life satisfaction | Structured questionnaires administered by trained interviewers to residents, face-to-face (Duration on average 30 minutes) (Not reported) |
145 residents of 2 assisted living facilities able to communicate, and no cognitive impairment | Female: 77.4% Mean age: 84.4±7.2 Married: 16.9% Caucasian: 100% |
| (Damian et al., 2008) Spain |
Describe the physical, mental, and social factors associated with self-rated health | Structured questionnaires administered by trained geriatricians to residents, their main caregivers, and their physician (or nurse), face-to-face Multistage cluster sampling (1998-1999) |
669 residents living in 49 nursing homes | Female: 75.0% Mean age: 83.4±7.3 Marital status not reported. Race/ethnicity not reported. |
| (Degenholtz et al., 2006) California, New York, New Jersey, Minnesota, Florida, Maryland, USA |
Determine the association between resident and facility level factors and quality of life | Interviews with residents to collect quality of life, linked with data from MDS and Online Survey and Certification Automated Record (1999-2000; 2001) |
2,829 residents living in 101 nursing facilities, aged ≥65 years, able to communicate, and in English | Female: 74.0% Mean age: 84.0±8.1 Marital status not reported. White: 89.0% |
| (Doyle, 1995) Australia |
Examine the effect of nursing staff turnover, frequency of visitors, and the presence or absence of close friends on depressive symptoms | Self-administered questionnaires reported by residents and nursing staff (director of nursing) (Not reported) |
165 residents living in 24 nursing homes, Mini-Mental State Exam score >18 | Female: 75.0% Mean age: 82.0±8.6 Married: 19.0% Widowed: 59.0% Race/ethnicity not reported. |
| (Drageset et al., 2008) Norway |
Quantify the relationship between social support and health-related quality of life | Structured questionnaires administered by the principal investigator to residents, face-to-face (2004-2005) |
227 residents living in 30 nursing homes > 6 months, aged ≥ 65 years, cognitively intact, and capable of carrying out a conversation | Female: 72.2% Age groups: 65-74: 8.8% 75-84: 34.4% 85-94: 45.8% ≥95: 11.0% Married or cohabitating: 16.7% Widowed: 63.4% Divorced, unmarried: 19.8% Race/ethnicity not reported. |
| (Duncan, Killian, & Lucier-Greer, 2017) Arkansas, USA |
Explore the extent to which perceived social support mediates the association between leisure activity engagement and ill-being | Structured questionnaires administered by research staff to residents, face-to-face (Duration between 45-60 minutes) (Not reported) |
110 older adults living in 13 long-term care facilities, Mini-Mental State Exam scores ≥25 | Female: 68.1% Mean age: 80.6±9.5 Married/Partnered: 17.3% Widowed: 44.5% Divorced/separated/never: 20.9% White: 95.5% |
| (El Zoghbi, 2014) Lebanon |
Description of nutritional status and its correlates | Structured questionnaires administered by research staff to residents, face-to-face (2012) |
111 residents living in 3 long stay institutions longer than 4 weeks and aged ≥65 years | Female: 50.5% Mean age: Woman: 78.1 ± 1.02 Men: 74.5 ± 1.09 Married: 27.0% Widow: 24.3% Divorced: 12.6% Single: 24.3% Race/ethnicity not reported. |
| (Fernández-Mayoralas, 2015) Spain |
Evaluate the association between leisure activity profiles and quality of life | Structured questionnaires administered to residents by health professionals working at the nursing homes who were supervised by researchers (2008 and 2010) |
759 residents living in 14 nursing homes aged ≥60 years | Female: 77.3% Mean age: 84.2±7.2 Married/Partnered: 16.2% Widowed: 60.5% Divorced/separated/never: 22.8% Race/ethnicity not reported. |
| (Ghusn et al., 1996) Texas, USA |
Identify factors that enhance later life satisfaction | Structured questionnaires administered by research staff to residents, face-to-face (1993) |
78 residents living in 2 Veterans Affairs nursing homes | Female: 0% Age groups: 44-54: 6.4% 55-64: 28.2% 65-74: 41.0% 75-84: 20.5% > 85: 3.8% Married/Partnered: 30.8% Widowed: 15.4% Divorced/separated/never: 53.8% African American: 30.8% Caucasian: 64.1% Hispanic: 5.1% |
| (Guse, 1999) Manitoba, Canada |
Explore factors related to quality of life | Structured questionnaires (with 3 open-ended questions) administered by research staff to residents, face-to-face (1997) |
32 permanent residents aged ≥55 years from 1 long-term care facility | Female: 34.0% Age groups: 65-74: 28.0% 75-84: 59.0% >84: 13.0% Married/Partnered: 34.4% Widowed: 46.9% Divorced/separated/never: 18.8% Race/ethnicity not reported. |
| (Haugan, Moksnes, & Løhre, 2016) Norway |
Investigate the association between perceived nurse-patient interaction and quality of life | Structured questionnaires administered by research staff to residents, face-to-face (2008 and 2009) |
202 residents living in 44 nursing homes > 6 months and cognitively intact | Female: 72.3% Mean age: 85.6 Marital status not reported. Race/ethnicity not reported. |
| (Hjaltadóttir et al., 2012) Iceland |
Investigate association between residents’ health status and functional profile and quality indicators | MDS (no admission assessments) (2003-2009) |
3,694 residents living in nursing homes | Female: 66.2% Mean age: 84.3±8.2 Marital status not reported. Race/ethnicity not reported |
| (Hollinger-Smith & Buschmann, 2000) Illinois, USA |
Examine factors associated with failure to thrive syndrome | Structured questionnaires administered by research staff to residents and medical records (Not reported) |
130 residents living in 2 nursing homes for ≥2 weeks, aged ≥65 years, able to read and write in English | Female: 58.5% Mean age: 76.6±8.7 Widowed: 53.1% Single: 23.1% Caucasian: 83.8% |
| (Hsiao & Chen, 2018) Taiwan |
Investigate the associations among individual, family, and extrafamilial factors and depression | Secondary analysis of Vulnerability and Social Exclusion among Different Groups of Disadvantaged Elderly in an Aging Society: Phenomena and Strategies Project Structured questionnaires administered by research staff, face-to-face (2007) |
327 residents living in 39 care institutions, aged ≥65 years, cognitively intact with mild to no physical impairment | Female: 48.3% Mean age: 82.1±7.5 No spouse: 74.6% Race/ethnicity not reported. |
| (Hsu & Wright, 2014) Taiwan |
Examine the association between frequency, meaningfulness, and enjoyment of social activities and depressive symptoms |
Structured questionnaires, research staff read the questions to participants needing assistance, face-to-face (Not reported) |
174 residents living in 13 long-term care facilities, aged ≥65 years, cognitively intact, able to speak Mandarin or Taiwanese, not bedridden, no severe speech/hearing impairment, no dementia or psychiatric disorder | Female: 54.0% Mean age: 78.6±7.8 Married/Partnered: 24.7% Widowed: 63.2% Divorced/separated/never: 12.1% Race/ethnicity not reported. |
| (Jang, Park, Dominguez, & Molinari, 2014) Florida, USA |
Explore how social engagement interacts with functional disability in predicting depressive symptoms | Structured questionnaires administered by research staff to residents, face-to-face (2004) |
150 residents living in 17 assisted living facilities, aged ≥60 years, without severe cognitive impairment | Female: 77.3% Mean age: 82.8±9.4 Married: 10.7% Race/ethnicity not reported. |
| (Jao et al., 2018) Pennsylvania, USA |
Examine the association between social interactions and affect | Research staff extract information from medical charts, video recorded residents for 20 minutes in morning and afternoon over 5 consecutive days, and interviewed them (2005-2008) |
126 residents living in 12 nursing homes, aged ≥65 years with dementia (Mini-Mental State Exam score 7-24), who spoke English, unstable medical illness | Female: 77.0% Mean age: 86.1±6.0 Married/Partnered: 17.6% Widowed: 72.8% Divorced/separated/never: 9.5% Caucasian: 88.1% African American: 11.9% |
| (Kang, 2012) Iowa, USA |
Evaluate the association between social depression and functional and behavioral variables | MDS 2.0 Research staff extracted medications from medical charts (2008-2009) |
153 residents living in 17 nursing homes aged ≥ 60 years with a diagnosis of Alzheimer’s disease or related dementias in their medical chart | Female: 64.7% Mean age: 85.0±7.3 Married: 35.3% Widowed: 55.6% Divorced/separated: 3.3% Never: 5.9% White: 100% |
| (Kasser & Ryan, 1999) New York, USA |
Investigate the effects of autonomy support and relatedness on well-being | Structured questionnaires, research staff aided residents if needed, face-to-face (Duration on average 34 minutes) (Not reported) |
50 residents living in 1 nursing home, aged >60 years, competent to give informed consent | Female: 78.0% Mean age: 83 (range: 70-99) Marital status not reported. Race/ethnicity not reported. |
| (Kehyayan, Hirdes, Tyas, & Stolee, 2016) Alberta, British Columbia, Manitoba, Nova Scotia, Ontario, Saskatchewan, Canada |
Identify predictors of long-term care facility residents self-reported quality of life | Structured quality of life questionnaires administered by trained surveyors to residents (face-to-face) linked to MDS 2.0 (2010) |
928 residents in 48 long-term care facilities, without severe cognitive impairment, who spoke English | Female: 65.5% Age groups: <65: 10.6% 65-84: 46.1% ≥85: 43.3% Married: 21.0% Race/ethnicity not reported. |
| (Keister, 2006) Midwestern USA |
Determine if person and situation factors were associated with health outcomes during the first week in nursing home | Structured questionnaires to residents (face-to-face) Convenience sample (1999-2000) |
114 residents who moved into 11 nursing homes in the last week and were expected to live there at least 8 weeks, aged ≥65 years, who understood and spoke English and had not been diagnosed with major depression in past 4 months | Female: 74% Mean age: 82.3±7.7 Widowed: 61.4% White: 92% |
| (Kroemeke & Gruszczynska, 2016) Poland |
Examine the association between social support and subjective well-being | Self-administered questionnaires distributed by research staff (Not reported) |
180 nursing home residents aged ≥60 years, cognitively intact, and no acute illness | Female: 67.5% Mean age: 79.1±9.1 Married: 17% Divorced/widowed/never: 83% Race/ethnicity not reported. |
| (Kwok, Yeung, & Chung, 2011) Hong Kong, China |
Examine the moderating role of social support on the relationship between physical functional impairment and depressive symptoms | Structured questionnaires administered by research staff to residents, face-to-face (Duration on average 25 minute) Convenience sample (Not reported) |
187 residents living in 2 nursing homes, aged ≥65 years, with Mini-Mental Exam scores ≥ 18 | Female: 71.1% Age groups: 65-75: 23.0% 76-85: 40.1% >85: 36.9% Marital status not reported. Race/ethnicity not reported. |
| (G. E. Lee, 2010) South Korea |
Identify predictors of nursing home life adjustment | Structured questionnaires administered by research staff to residents, face-to-face (2007) |
156 residents living in 7 nursing homes aged >65 years, cognitively intact and healthy enough to participate | Female: 80.1% Mean age: 79.1±6.0 Marital status not reported. Race/ethnicity not reported. |
| (H. Lee et al., 2017) Michigan and Pennsylvania, USA |
Examined the relationship between staff–resident interactions and resident psychological well-being | Secondary analysis from a multisite study on wandering (Algase, 2008) Videotaped residents 12 20-minute observation periods on 2 non-consecutive days, between 8:00 A.M. and 8:00 P.M. Random cluster sampling (Not reported) |
110 residents living in 17 nursing homes and 6 assisted living facilities, ≥ 65 years with dementia (Mini-Mental State Exam score <24, English-speaking, not wheelchair-bound, and adequate vision/hearing | Female: 72.7% Mean age: 84±6.9 Marital status not reported. Caucasian: 70.0% |
| (Leedahl, Chapin, & Little, 2015) Kansas, USA |
Examine relationships between social integration and mental and functional health | Structured questionnaires administered by research staff to residents, face-to-face (Duration not longer than 1 hour) Two-stage multilevel sampling (Not reported) |
140 long-stay residents living in 30 nursing homes, ≥ 65 years, long-term stay, able to consent, Mini-Mental Exam Score >12, and Cognitive Performance Scale <3 | Female: 74.3% Mean age: 83.1±9.0 Married: 15.0% Widowed: 55.0% White: 92.7% |
| (Li et al., 2015) New York, USA |
Examine factors associated with daytime sleep | MDS 2.0 (2005 to 2010) |
300 residents living in 1 nursing home for more than 3 months | Female: 72% Mean age: 86.9±7.0 Marital status not reported. White: 99% Hispanic or Black: 1% |
| (Lin, Wang, & Huang, 2006) Taiwan |
Examine the relationship between depressive symptoms and length of residency, health status and social support | Structured questionnaires administered by research staff to residents, face-to-face Convenience sampling (Not reported) |
138 residents living in 8 nursing homes at least 6 months, aged ≥ 65 years, and cognitively intact | Female: 53.6% Mean age: 78.0±7.1 Married: 25.4% Race/ethnicity not reported. |
| (Liu, Xue, Xue, & Hou, 2018) Xinjiang, China |
Evaluate the relationship between health literacy, self-care agency, social support and health status | Structured questionnaires administered by research staff to residents, face-to-face (2011-2012) |
1,452 participants aged between 60 and 99 years from 44 nursing homes | None reported |
| (Maenhout et al., 2020) Belgium |
Investigate the relationship between personal, organizational, activity-related factors, and social satisfaction on quality of life | Structured questionnaires administered by research staff to residents, face-to-face (Duration 2-4 hours to complete, 2 sessions in a week) Stratified random sample (Not reported) |
171 residents living in 73 nursing homes for > 1 month, aged ≥ 75 years, cognitively healthy, able to understand and answer questions | Female: 73.1% Mean age: 85.4±5.9 Married: 15.8% Widowed: 71.3% Divorced/separate/never: 11.7% Race/ethnicity not reported. |
| (Martin et al., 2006) California, USA |
Evaluate factors associated with excessive daytime sleeping | Structured behavioral observations were performed for one minute every 15 minutes from 9:00 am–5:00 pm for 2 days (1999-2002) |
492 residents from 4 nursing homes | Female: 80.5% Mean age not reported. Marital status not reported. Race/ethnicity not reported. |
| (Marventano et al., 2015) Spain |
Evaluate the association between characteristics of residents with dementia and quality of life and residential care centers characteristics with quality of life | Nurses, occupational therapists, directors of nursing care, medical staff, caregivers, and proxies completed different components of the survey and chart review (2010) |
429 residents living in 14 nursing care homes aged ≥60 years with dementia | Female: 82.1% Mean age: 85.8±6.7 Married: 17.5% Race/ethnicity not reported. |
| (M. McCabe et al., 2021) Australia |
Evaluate the contribution of resident choice and the staff–resident relationship on resident quality of life | Secondary analysis from a randomized trial on consumer directed care (M. P. McCabe, Beattie, E., Karantzas, G., Mellor, D., Sanders, K., Busija, L., Goodenough, B., Bennett, M., Von Treuer, K., & Byers, J, 2018) Structured questionnaires administered by research staff to residents, face-to-face (Duration on average 30-45 minutes) (2018-2020) |
604 residents living in 33 nursing homes ≥2 months, possessed adequate English communication skills, without severe cognitive impairment | Female: 64.4% Mean age: 85.4±7.7 Marital status not reported. Race/ethnicity not reported. |
| (Mitchell & Kemp, 2000) California, USA |
Examine effects of health status and social involvement on quality of life | Structured questionnaires administered by research staff to residents, face-to-face (Duration on average 1 hour) Stratified random sample (Not reported) |
201 residents living in 55 assisted living facilities, alert without cognitive impairment | Female: 74.0% Mean age: 81±9.6 Widowed: 69.0% Non-Hispanic White: 96.0% |
| (Morrison-Koechl et al., 2021) Canada |
Explores the effects of psychosocial factors on energy intake | Secondary analysis of data from the Making the Most of Mealtimes study (Keller et al., 2017) Direct observations of mealtime experience, structured interviews with care partners, resident chart reviews, and measures of nutritional care Convenience sampling (Not reported) |
604 residents from 32 long-term care homes | Female: 68.2% Mean age: 86.8±7.8 Marital status not reported. Race/ethnicity not reported. |
| (Nie, Hu, Zhu, & Xu, 2020) Hunan, China |
Explore risk factors for suicidal ideation | Structured questionnaire Multistage cluster random sample (2018) |
817 residents living in 24 nursing homes > 1 year, aged ≥60 years, physically and mentally able to participate, no severe hearing impairment, severe cognitive deficits, language barrier, or terminal illness | Female: 54.0% Mean age: 79.1±8.7 Divorced/loss of a partner/never married: 63.0% Race/ethnicity not reported. |
| (Onunkwor et al., 2016) Malaysia |
Determine the quality of life and its associated factors | Structured questionnaires administered by research staff to residents, face-to-face Stratified random sampling (2014) |
203 residents living in 8 elderly homes, aged ≥60 years, able to understand English, Malay, or Chinese, no communication problem or cognitive impairment | Female: 35.5% Mean age: 71.5±6.8 Married: 61.6% Malay: 3.0% India: 8.4% Chinese: 87.1% Others: 1.5% |
| (Papi, Karimi, Amini Harooni, Nazarpour, & Shahry, 2019) Iran |
Determine predictors of sleep disorder | Structured questionnaires, unclear if self-administered or administered by research team Convenience sample (2017) |
130 residents from 4 nursing homes aged > 60 years, no cognitive disorders | Female: reported as 66.2% in abstract and 33.8% in results Mean age: 68±7.8 Marital status not reported. Race/ethnicity not reported. |
| (N. S. Park, 2009) Alabama, USA |
Explore the association between social engagement and psychological well-being | Structured questionnaires administered by research staff to residents, face-to-face (Duration on average 60-90 minutes) (2006) |
82 residents living in 8 assisted living facilities, aged ≥ 65 years without dementia, capable of understanding and answering questions | Female: 74.4% Mean age: 84.0±6.1 Marital status not reported. Race/ethnicity not reported. |
| (S. Park & Sok, 2020) South Korea |
Examine the relationship between the factors influencing the adaptation ability and life satisfaction | Structured questionnaires distributed by research staff to residents, assistance provided by research staff if needed Random sample (2017) |
229 residents living in an elderly care facility for >6 months aged ≥ 65 years, with cognitive ability to respond, with < 2 pharmacological treatments | Female: 67.2% Age groups: 65–74: 14.8% 75–85: 41.5% ≥85: 43.7% Married: 30.1% Race/ethnicity not reported. |
| (Patra et al., 2017) Greece |
Explore the association between social support and depression | Self-administered questionnaires distributed by research staff (2016) |
170 residents living in nursing homes aged >60 years, able to read and write in Greek, no psychiatric illness | Female: 66.5% Mean age: 79.5±7.4 Married: 11.8% Race/ethnicity not reported. |
| (Pramesona & Taneepanichskul, 2018) Indonesia |
Investigate risk factors of depression | Structured questionnaires administered by research staff to residents, face-to-face (Duration between 30–45 minutes) (2017) |
181 residents living in 3 homes ≥ 1 month, aged ≥60 years, no chronic diseases | Female: 65.7% Mean age: 74.4±7.6 Married: 12.2% Widowed: 56.3% Divorced/separate/never: 31.5% Race/ethnicity not reported. |
| (Randall et al., 2011) Georgia, USA |
Investigate the influence of social relations on health outcomes | Secondary analysis of data from The Georgia Centenarian Study (Poon, 2007) Structured questionnaires administered by research staff to residents, face-to-face (4 sessions, each <2 hours) (2002 – 2005) |
105 nursing home residents and 55 assisted living residents, aged ≥ 98 years and cognitively intact | Female: 78.5% Mean age: 99.8±1.7 Married: 6.0% Widowed: 85.0% White: 85.0% African American: 15.0% |
| (Rozzini et al., 1996) Italy |
Describe the association between depression and its factors | Residents were assessed by three geriatricians (Not reported) |
56 residents without severe dementia and without neurological conditions | Female: 76.8% Mean age: 81.1±8.6 Marital status not reported. Race/ethnicity not reported. |
| (Saleh et al., 2017) British Columbia, Canada |
Explore the association between social engagement and use of antipsychotics | MDS 2.0 and the Continuing Care Information Management System (2008 – 2011) |
2,639 newly admitted long-stay residents aged ≥65 years with Alzheimer’s disease or other dementias | Female: 65.8% Mean age: 83.9±6.8 Married: 35.9% Widowed: 47.9% Divorced/separate/never: 11.8% Race/ethnicity not reported. |
| (Segal, 2005) Colorado, USA |
Assess the relationship of assertiveness, depression, and social support | Anonymous self-administered questionnaires (Not reported) |
50 residents of several nursing homes, older adults were free of cognitive impairment | Female: 75.0% Mean age: 74.9±11.9 Marital status not reported. Caucasian: 92.0% |
| (Smit et al., 2016) Netherlands |
Evaluate activity involvement and quality of life | Secondary analysis of data from the Living Arrangements for people with Dementia (LAD) study (Willemse & 11 (11), 2011) MDS 2.0 merged with informal caregiver and nursing home staff surveys (2010-2011) |
1,144 residents living in 144 long-term care facilities providing care for people with moderate-to very severe dementia | Female: 75.2% Mean age: 84.2±7.6 Marital status not reported. Race/ethnicity not reported. |
| (Street, Burge, Quadagno, & Barrett, 2007) Florida, USA |
Examine how organizational characteristics, transition experiences, and social relationships impact quality of life | Structured questionnaires administered by research staff to residents, face-to-face (2004-2005) |
384 residents living in assisted living facilities, aged ≥65 years, and who were cognitively intact | Female: 73.9% Mean age: 84.2±7.6 Marital status not reported. Race/ethnicity not reported. |
| (Sun et al., 2017) Shandong, China |
Explore the roles of self-esteem, depression, and social support on quality of life | Structured questionnaires administered by investigators to residents, face-to-face (2015) |
205 residents living in 5 nursing homes aged ≥60 years, without terminal illnesses, able to communicate, and cognitively intact | Female: 53.7% Mean age: 77.3±7.9 Married: 29.8% Widowed/divorced: 54.6% Single: 15.6% Race/ethnicity not reported. |
| (Tosangwarn et al., 2017) Thailand |
Explore the association between internalized stigma, self-esteem, social support, and coping strategies and depressive symptoms | Structured questionnaires administered by nurse researcher to residents, face-to-face (Duration on average 1 hour) (2015) |
128 residents living in 2 care homes, aged ≥60 years who can speak Thai and without severe cognitive impairment or psychological disturbance | Female: 62.5% Mean age: 76.9±7.8 Married/partnered: 3.9% Widowed: 48.5% Divorced/separated: 26.6% Single: 21.1% Race/ethnicity not reported. |
| (Tseng & Wang, 2001) Taiwan |
Explore the role of social support, health status, and family interactions on quality of life | Structured questionnaires distributed by research staff to residents, assistance provided by research staff if needed (Duration on average 30-45 minutes) Convenience sample (Not reported) |
161 residents living in 10 nursing homes for > 6 months, aged ≥65 years, with good cognitive function and ability to complete the questionnaire | Female: 40.4% Mean age: 76-74±7.1 Married: 34.1% Widowed: 46.6% Unmarried: 19.3% Race/ethnicity not reported. |
| (Tu, Lai, Shin, Chang, & Li, 2011) Taiwan |
Explore the relationship between health status, social support, and leisure activities with depression | Interviews using structured questionnaires (2007) |
309 residents living in 6 long-term care facilities, aged ≥65 years, and capable of answering questions clearly | Female: 61.2% Mean age: 81.6 Spouseless: 80.6% Race/ethnicity not reported. |
| (Vanbeek et al., 2011) Netherlands |
Investigate the relationship between social engagement and depressive symptoms | MDS 2.0, collected over 3 days (2002-2003) |
502 residents living in 37 long-term care dementia units | Female: 79.7% Mean age: 85.1±7.1 Married/ partner: 26.7% Race/ethnicity not reported. |
| (Wahyuni et al., 2019) Indonesia |
Evaluate the relationship of social support with depression | Primary data collected with a self-administered questionnaire (Not reported) |
20 residents living in 1 nursing home who could read, write, communicate verbally, and cooperate, but who did not have a serious illness | Female: 100% Age group: 60-74: 35.0% 79-90: 60.0% >90: 5.0% Widowed: 95.0% Not married: 5.0% Race/ethnicity not reported. |
| (J. Wang, Wang, Cao, Jia, & Wu, 2018) Shanghai, China |
Examine the association between social support and perceived empowerment and quality of life | Structured questionnaires administered by investigator or research assistant to residents, face-to-face (Duration ~ 45 to 125 minutes) Convenience and purposive sampling (2011-2012) |
515 residents living in 9 long term care facilities > 1 month, age ≥60 years, speak Mandarin or Shanghai dialect | Female: 60.4% Mean age: 84.0±5.2 Married: 6.2% Race/ethnicity not reported. |
| (Wiesmann, Becker, & Hannich, 2017) Germany |
Explore association between age, social network, sense of coherence and positive aging | Structured questionnaires administered by investigator or research assistant to residents, face-to-face (Duration on average 42 minutes) (Not reported) |
190 residents living in 20 nursing homes ≥ 3 months, aged ≥65 years | Female: 81.6% Mean age: 84.3±7.6 Widowed: 66.7% Race/ethnicity not reported. |
| (Wu et al., 2017) Shandong, China |
Identify factors related to successful aging | Structured questionnaires administered by investigator or research assistant to residents, face-to-face Convenience sample (2015) |
205 resident living in 5 nursing homes, aged ≥60 years | Female: 53.7% Mean age: 77.3±7.9 Married: 29.8% Race/ethnicity not reported. |
| (Wu et al., 2018) Shandong, China |
Quantify the relationship between social support and health-related quality of life | Structured questionnaires administered by investigator or research assistant to residents, face-to-face Convenience sample (2015) |
205 residents living in 5 nursing homes aged ≥60 years, without terminal illnesses, able to communicate, and cognitively intact | Female: 53.7% Mean age: 77.3±7.9 Married: 29.8% Race/ethnicity not reported. |
| (Xu et al., 2019) Shandong, China |
Investigate the role of child visit frequency and family support in the relationship between the number of children and quality of life | Structured questionnaires administered by investigator or research assistant to residents, face-to-face Convenience sample (2016) |
371 residents living in 33 nursing homes for ≥1 month, aged ≥60 years, with Mini-Mental State Exam score≥10, with no sensory impairments affecting participation | Female: 59.3% Mean age: 77.5±8.7 Married and lived together: 8.1% Married and separated: 11.9% Han: 98.1% |
| (Yeung et al., 2012) Hong Kong, China |
Evaluate the mediating effect of institutional peer support on the relationship between physical decline and depressive symptoms | Structured questionnaires administered by research assistant to residents, face-to-face (Duration on average 25 minutes) Convenience sample (2009) |
187 residents living in 2 nursing homes without stroke, dementia, or Parkinson’s disease | Female: 71.1% Age group: 65-75: 23% 76-85: 40.1% 85+: 36.9% Married: 38.0% Widowed: 40.0% Single: 22.0% Race/ethnicity not reported. |
| (Ysseldyk, Haslam Sa Fau - Haslam, & Haslam, 2013) Ontario, Canada |
Examine relationships between religion and well-being among older adults | Semi-structured interviews conducted by research staff to residents, face-to-face (Duration ~60 minutes) (2002 & 2008) |
42 older adults from 3 care homes | Female: 59.5% Mean age: 86.3±5.8 Marital status not reported. Race/ethnicity not reported. |
| (Zhang et al., 2018) Shandong, China |
Investigate the relationship among social support, physical health, and suicidal thoughts | Structured questionnaires administered by investigator or research assistant to residents, face-to-face Convenience sample (2015) |
205 residents living in 5 nursing homes aged ≥60 years, without terminal illnesses, able to communicate, and cognitively intact | Female: 53.7% Mean age: 77.3±7.9 Married: 29.8% Widowed: 53.7% Divorced: 1.0% Single: 15.6% Race/ethnicity not reported. |
| (Zhu et al., 2020) Hunan, China |
Explore risk factors for poor sleep quality | Structured questionnaires administered by trained research staff to residents, face-to-face (Duration 30 to 60 minutes) (2018) |
817 residents living in 24 nursing homes for > 1 year and aged > 60 years | Female: 54.0% Age group: 60~69: 16.5% 70~79: 28.4% ≥80: 55.1% Marital Status Stable: 37.0% Race/ethnicity not reported. |
| (Zurakowski, 2000) USA |
Investigate the effects of social support on anomia and self-reported health | Structured questionnaires administered by trained graduate students in nursing to residents, face-to-face Convenience sample |
91 residents living in 4 nursing homes | Female: 79.1% Mean age: 79.4±16.2 Married: 8.8% Widowed: 59.3% Divorced: 4.4% Single: 27.5% White: 100% |
Determined from lead author via email correspondence.
Mean Age±SD (years)
Described like assisted living homes.
Findings
The Supplemental Table 1 shows a summary of the analyses derived from the eligible cross-sectional studies. There was great heterogeneity with respect to the measures of social connectedness used. The concepts measured included network size, social support from inside and outside of the facility, relationship to resident (family, friends, peer resident, staff), and type of support provided. Many measures captured elements of perceived social support. The most common measure of social connectedness was a version of the Index of Social Engagement (Gerritsen, 2008; Mor et al., 1995). The majority of cross-sectional studies evaluated mental health outcomes or QOL outcomes. The most common depressive symptom scale used was a version of the Geriatric Depression Scale (n=21 studies). A particular measure did not dominate studies with QOL and life satisfaction as outcomes. Most studies (but not all) attempted to adjust for various confounders. Most studies demonstrated a favorable association between social connectedness and the health outcomes studied. Across the studies, size of social network was not consistently associated with health outcomes, and the relationships with peer residents within the facilities appeared to be positively associated with health outcomes.
3.4. Cohort Studies
Characteristics
Table 3 shows the characteristics of the 25 eligible cohort studies. Seven studies were retrospective (Fehnel et al., 2015; Foebel et al., 2015; Freeman, Spirgiene, Martin-Khan, & Hirdes, 2016; Hjaltadottir, Hallberg, Ekwall, & Nyberg, 2011; Kiely & Flacker, 2003; Kiely, Simon, Jones, & Morris, 2000; Palese et al., 2019). The duration of follow-up ranged from one month (Fehnel et al., 2015; Kroemeke & Gruszczynska, 2016) to eleven years (Cohen-Mansfield, Marx, Lipson, & Werner, 1999), with most having an average duration being 1 year (Chau, 2021; Foster & Cataldo, 1993; Kiely & Flacker, 2003; Maxwell et al., 2015; Rozzini, Boffelli, Franzoni, Frisoni, & Trarucchi, 1996; Yamada et al., 2016). Most studies reporting the number of facilities included residents from multiple long-term care facilities, with few exceptions (Cohen-Mansfield et al., 1999; Foster & Cataldo, 1993; Kiely et al., 2000; Rozzini et al., 1996). There was great variation in the number of residents included in the studies (range: 56 residents [Rozzini et al., 1996] to 125,496 [E. Neufeld, Freeman, Spirgiene, & Horwath, 2019]). In all but three studies (Foster & Cataldo, 1993; Weiner, Peterson, Logue, & Keefe, 1998; K.-P. Yeh et al., 2014), most residents were women. The average age ranged from 49.3 years (Foster & Cataldo, 1993) to 87.0 years (Kiely et al., 2000). Race/ethnicity was reported in four studies (89.4% white [Grabowski & Mitchell, 2010], “mostly white sample” [Inventor et al., 2018], 85% White [Fehnel et al., 2015], 84% White [Kiely & Flacker, 2003], 16.5% African-American [Weiner et al., 1998]). Marital status was reported in fourteen studies (range of % married: 1.9% [Mao & Han, 2018] to 33% [Weiner et al., 1998]).
Table 3.
Characteristics of included cohort studies on the association between social connectedness/engagement and health outcomes among older adults living in congregate long term care settings
| (Author, Year) Location |
Study Design / Data Source (Years of data) |
# of Residents and Description | Sample Description % Female Age (years) % Marital status % Race/Ethnicity |
|---|---|---|---|
| (Chau, 2021) Australia |
Prospective Primary data collection ~1 year of follow-up (Range: 0.40-1.87 years) (2015 to 2018) |
15 long term care facilities 147 residents with no or mild cognitive impairment recruited at baseline, with 81 who completed the study |
Completers: Female: 69.1% Mean age: 85.0±9.0 Married/partnered: 23.5% Never married/partnered:7.4% Widowed: 53.1% Race/ethnicity not reported. |
| (Cohen-Mansfield et al., 1999) Maryland, USA |
Prospective Chart reviews, questionnaires 11 years of follow-up (1985-1986) |
1 nursing home 399 residents |
Female: 77.7% Mean age: 85.7±6.6 Marital status not reported. Race/ethnicity not reported. |
| (Fehnel et al., 2015) USA |
Retrospective Minimum Data Set 2.0 at admission 30 days (2008) |
39,178 people aged ≥65 year directly admitted to nursing home after a new-onset ischemic stroke | Female: 65.1% Mean age: 83±7.7 85% White, 9.9% Black, 3.2% Hispanic, 0.3% American Indian, 1.6% Asian |
| (Foebel et al., 2015) Ontario, Canada |
Retrospective Minimum Data Set 2.0 3-6 months (2003-2011) |
47,768 long term care or complex continuing care residents not at end of life who were either not using antipsychotics or who newly initiated antipsychotics | Female: 67.3% Mean age: 83.2±9.5 Marital status not reported. Race/ethnicity not reported. |
| (Foster & Cataldo, 1993) New York, USA |
Prospective Primary data collection 1 year of follow-up, monthly re-examinations (Dates of data collection not reported.) |
1 long term care facility 104 newly admitted residents without depression recruited, with 62 completed the study |
Completers: Female: 33.9% Mean age: 49.3±17.6 Marital status not reported. Race/ethnicity not reported. |
| (Freeman et al., 2016) Ontario, Canada |
Retrospective Minimum Data Set 2.0 at admission and first follow up assessment (90 days) (2005-2011) |
111,052 newly admitted long term care residents | Female: 68.9% Mean age: 82.9±9.8 Married/Partnered: 26.6% Not married/no partner: 73.4% Race/ethnicity not reported. |
| (Grabowski & Mitchell, 2010) Massachusetts, USA |
Prospective Longitudinal data from Choices, Attitudes, Strategies, and Care for Advanced Dementia at the End-of-Life (CASCADE) study. (2003-2006) |
22 nursing homes Dyadic data from 323 health care proxies and residents with advanced dementia aged ≥60 years, with ≥30 days or longer stay, cognitive impairment due to dementia, Global Deterioration Scale score of 7, an appointed health care proxy who could communicate in English, no cognitive impairment due to stroke, traumatic brain injury, tumor, or a chronic psychiatric condition, not comatose |
Female: 85.4% Mean age: 85.3±7.5 Marital status not reported. White: 89.4% |
| (Hjaltadottir et al., 2011) Iceland |
Retrospective Minimum Data Set 2.0 within 90 days of admission 36 months of follow-up (1996-2006) |
62 nursing homes 2,206 residents |
Female: 59.8% Mean age: 82.5±7.6 Marital status not reported. Race/ethnicity not reported. |
| (Inventor et al., 2018) Midwestern USA |
Prospective Secondary analysis of data from a previous study Data collected at baseline, 12 and 24 months (1990 to 1992) |
2 nursing homes At baseline: 87 residents in dementia unit 90 in traditional care |
Female: 79.1% Mean age: 85.0±5.7 Married/partnered: 18.6% “mostly white sample” |
| (Kiely et al., 2000) Massachusetts, USA |
Retrospective Minimum Data Set 2.0 data Partial assessments every 2 months, full annual assessments over 4.5 years (1994 to 1998) |
1 long term care facility 927 residents without serious communication difficulties |
Female: 75.0% Mean age: 87.0±6.3 Marital status not reported. Race/ethnicity not reported. |
| (Kiely & Flacker, 2003) New York, USA |
Retrospective Minimum Data Set 2.0 data cross-linked to the National Death Index 1 year of follow-up (1994 to 1997) |
653 nursing homes 30,070 long-stay residents without a serious communication problem |
Female: 73.0% Age≥ 65: 100% Marital status not reported. 84% White, 9% Black, 3% Hispanic, 3% American Indian, 1% Asian |
| (Kloos et al., 2019) Netherlands |
Prospective Primary data collection 5-8 months of follow-up (Dates of data collection not reported.) |
4 nursing homes 128 residents completed baseline, 91 completed follow-up |
Female: 72.7% Mean age: 85.0±6.9 Married/partnered: 20.3% Widowed: 75% |
| (Kroemeke & Gruszczynska, 2016) Poland* |
Prospective Primary data collection, self-administered questionnaires 1 month of follow-up (2013) |
212 completed follow-up, 138 were nursing home residents >60 years of age, no cognitive impairment, no acute illness |
Total sample: Female: 67.5% Mean age: 79.1±9.1 Married/partnered: 17% Widowed/unmarried/divorced: 83% Race/ethnicity not reported. |
| (Lou et al., 2012) Hong Kong |
Prospective Minimum Data Set 2.0 Follow-up through 2010 (2005) |
10 long term care facilities 1,184 residents without psychotic disorders or psychosocial interventions |
Female: 65.6% Mean age: 81.7±8.8 Married/partnered: 27.3% Widowed: 57.4% Race/ethnicity not reported. |
| (Mao & Han, 2018) China |
Prospective Chinese Longitudinal Health Longevity Survey 7 years of follow-up (First interviewed: 1998, 2000, 2002; Interviewed again in 2005 and 2008) |
133 residents of nursing homes in urban areas 53 residents of nursing homes in rural areas |
Urban (Rural): Female: 62.4% (37.7%) Mean age: 84.2±6.5 (81.9±7.0) Married/partnered: 7.5% (1.9%) Widowed: 70.7% (73.6%) Race/ethnicity not reported. |
| (Maxwell et al., 2015) Alberta, Canada |
Prospective Primary data (Standardized comprehensive assessment of residents and interviewed family caregivers) 1 year follow-up (2006 to 2008) |
59 assisted living facilities 609 residents with dementia 54 long term care facilities 691 residents with dementia |
Assisted living (Long term care): Female: 78.0% (67.2%) Mean age: 85.7±6.6 (86.4±6.9) Married/partnered: 15.6% (25.2%) Widowed: 73.2% (61.7%) Race/ethnicity not reported. |
| (E. Neufeld et al., 2019) Ontario, Canada |
Prospective Minimum Data Set 2.0 data ~90-day follow-up (2011 to 2014) |
125,496 nursing home residents at baseline 86,974 had a follow-up assessment |
Baseline (follow-up): Female: 64.8% (65.6%) Mean age: 83.3±8.3 (83.7±8.1) Married/partnered: 31.8% (30.5%) Widowed: 52.5% (53.4%) Race/ethnicity not reported. |
| (Palese et al., 2019) Italy |
Retrospective Information collected every six months (2008 to 2013) |
105 nursing homes 13,175 newly admitted residents > 65 years |
Female: 74.7% Mean age: 83.5±9.5 Marital status not reported. Race/ethnicity not reported. |
| (Pastor-Barriuso et al., 2020) Spain |
Prospective Primary data collection at baseline linked to Spanish National Death Index 10 years of follow-up (through 2013) (1998 to 1999) |
55 nursing homes 382 residents without severe physical and cognitive impairments 14% of residents had primary caregivers complete the baseline survey |
Female: 74.4% Age group: 65-79: 32.1% 80-84: 25.6% 85-89: 23.8% ≥ 90: 18.5% Married/partnered: 14.2% Widowed/divorced: 52.1% Race/ethnicity not reported. |
| (Rozzini et al., 1996) Italy |
Prospective Primary data collection 1 year follow-up (Dates of data collection not reported.) |
1 nursing home 56 residents without severe dementia and without neurological conditions |
Female: 76.8% Mean age: 81.1±8.6 Marital status not reported. Race/ethnicity not reported. |
| (Vetrano et al., 2018) Czech Republic, England, Finland, France, Germany, Israel, Italy, Netherlands |
Prospective Primary data collection 12 months of follow-up (Dates of data collection not reported.) |
57 nursing homes 3,036 residents participating in the Services and Health for Elderly in Long TERm care (SHELTER) study |
Female: 74% Mean age: 84.6±7.7 Marital status not reported. Race/ethnicity not reported. |
| (Y. H. Wang, Liu, Chang, & Yeh, 2019) Taiwan |
Secondary data collected from a Non-Profit Organization foundation in central Taiwan A single group pre- and post-test design was used with measurements taken at the baseline and 6 months after implementation of the restorative care intervention (2017-2019) |
24 nursing homes 310 residents aged ≥65 years with life expectancy >6 months and met at least one: constrained, used diapers, intubated with endotracheal tube/Foley catheter/nasogastric tube, unable to move around without wheelchair, or stand for 5 seconds |
Female: 59.4% Mean age: 81.3±7.4 Marital status not reported. Race/ethnicity not reported. |
| (Weiner et al., 1998) North Carolina, USA |
Prospective Primary data collection 4 weeks of follow-up |
2 nursing homes 115 nursing home residents |
Female: 44.0% Age quartiles: 73/81/87 (range 32-99) Married: 33.0% Divorced, widowed, separated: 49.1% Never married: 21.9% African-American: 16.5% |
| (Yamada et al., 2016) Czech Republic, England, Finland, France, Germany, Israel, Italy, Netherlands |
Prospective interRAI instrument for Long Term Care Facilities Data collected at baseline, 6, and 12 months (2009 to 2011) |
59 nursing homes 1,989 residents without severe cognitive impairment or unstable health |
Female: 71.8% Mean age: 83.3±11.1 Marital status not reported. Race/ethnicity not reported. |
| (K.-P. Yeh et al., 2014) Taiwan |
Prospective Minimum Data Set, Chinese version 2.1 12 months of follow-up (2006-2010) |
2 veterans’ nursing homes 1,125 residents aged ≥ 65 years in the home for ≥ 18 months |
Female: 0% Mean age: 83.3±5.1 Marital status not reported. Race/ethnicity not reported. |
Determined from lead author via email correspondence.
Mean Age±SD (years)
Described like assisted living homes.
Findings
Table 4 shows that in the eligible cohort studies, there was heterogeneity in the proportion of participants with no or low social engagement (range of % no social engagement: 6.6% [Kiely & Flacker, 2003] to 33% [Vetrano et al., 2018], range of % no or low social engagement: 18.2% [Freeman et al., 2016] to 36.0% [Pastor-Barriuso, Padrón-Monedero, Parra-Ramírez, García López, & Damián, 2020], 61.2% with reduced social engagement [Foebel et al., 2015]). Findings from included cohort studies are also summarized in Table 5. Although the outcomes under study differed, as did the operational definitions of social connectedness, studies reported that social connectedness was associated with favorable outcomes including psychological well-being (Mao & Han, 2018), delayed cognitive decline (Freeman et al., 2016; Yamada et al., 2016), positive behaviors (Inventor et al., 2018), self-feeding independence (Palese et al., 2019), positive affect (Kroemeke & Gruszczynska, 2016), decreased depression or depressive symptoms (Chau, 2021; Kloos, Trompetter, Bohlmeijer, & Westerhof, 2019; Lou, Chi, Kwan, & Leung, 2012; E. Neufeld et al., 2019), and delayed time to death (Fehnel et al., 2015; Hjaltadottir et al., 2011; Kiely & Flacker, 2003; Kiely et al., 2000; Maxwell et al., 2015; Pastor-Barriuso et al., 2020). Three studies suggested that social connectedness measures may have opposite effects. One study (Grabowski & Mitchell, 2010) compared residents at the end of life with > 7 hours of visits to residents with 1-7 hours/week of visits on 8 different quality measures. The quality metrics were worse for residents receiving >7 hours of visits/week compared to residents receiving 1-7 hours/week across 5 of the 8 quality measures. Residents with recent (≤ 3 days) or visits > 3 days died at a rate more quickly than those without family visits (Vetrano et al., 2018). Another study (Foebel et al., 2015) showed that reduced social engagement was associated with lower risk of initiating an antipsychotic in women, but not men. No association between measures of social connectedness were observed with pain (Weiner et al., 1998), changes in the Geriatric Depression Scale (Rozzini et al., 1996), functional decline (K.-P. Yeh et al., 2014), or time to death (Cohen-Mansfield et al., 1999).
Table 4.
Findings from included cohort studies on the association between social connectedness/engagement and health outcomes among older adults living in congregate long term care settings
| (Author, Year) |
Study purpose | Measure of social connectedness |
Measures of health outcomes |
Covariates | Major findings |
|---|---|---|---|---|---|
| (Chau, 2021) | Examine key risk factors for depression among older adults in long-term care | Multidimensional scale of perceived social support (MSPSP) (Zimet, Dahlem, Zimet, & Farley, 1988; Zimet, Powell, Farley, Werkman, & Berkoff, 1990) | Geriatric Depression Scale (GDS-15) (Yesavage et al., 1982) M.I.N.I. International Neuropsychiatric Interview (D. Sheehan, 2015; D. V. Sheehan et al., 1997) |
Age, gender, education, marital status, and other risk factors (pain, sleep, cognitive impairment, physical function, person-environment fit) | As social support score increased depression score decreased. |
| (Cohen-Mansfield et al., 1999) | Examine factors associated with mortality | Hebrew Home Social Network Rating Scale (Cohen-Mansfield & Marx, 1992) | Date and cause of death abstracted from death certificates | Age, gender, hearing, surgery in past 2 years, number of medical diagnoses, cognitive function, activities of daily living, appetite, falls, incontinence, sleep aggressive behaviors, screaming | Size and quality of social network were not associated with time to death. |
| (Fehnel et al., 2015) | Identify factors that predict hospital readmission and mortality after ischemic stroke | Minimum Data Set (MDS) Index of Social Engagement (Mor et al., 1995) | Date of death (whether from Medicare files or MDS not specified) Hospital re-admissions from Medicare Part A |
Age, race, sex, education level, non-native English speaker, active tobacco use, do not resuscitate order, do not hospitalize order, hospice care, guardianship status, hospital length of stay, bowel and bladder incontinence, urinary catheter, body mass index, marital status, co-morbid conditions, gastric feeding tube, tracheostomy, activities of daily living, cognitive impairment, communication scale, pressure ulcer, CHESS (changes in health, end-stage disease, symptoms, and signs score) index, Elixhauser score. | Relative to residents with a social engagement score of zero (not engaged), each social engagement score from 1 to 6 (very engaged) was inversely associated with 30-day readmission or death. |
| (Foebel et al., 2015) | Estimate factors associated with new antipsychotic use in residents newly admitted to long term care | Reduced social engagement measure derived from MDS 2.0 items | Initiation of an antipsychotic as documented on the MDS 2.0 | Age, cognitive impairment, physical function, communication, delirium, comorbid conditions, hearing, vision, pain, delusions, motor agitation, depressive symptoms, urinary tract infection, # of medications, other psychoactive medications, restraints, hospital stay, emergency room visits, days between assessments Stratified by sex |
61.2% had reduced social engagement. In women, reduced social engagement was associated with initiation of an antipsychotic, but not in men. |
| (Foster & Cataldo, 1993) | Evaluate the extent to which the onset of depression can be predicted in a long-term care facility | ‘How many friends do you have here at the hospital? By friend, I mean someone who you talk to regularly, not just a casual acquaintance.’ (self-reported each month) | Monthly evaluations by a research psychiatrist (≥15 on 21-item Hamilton Depression Rating Scale [Hamilton, 1960] and ≥10 on GDS-15 [Yesavage et al., 1982]) or using DSM-III criteria for affective disorders |
At admission: coping, GDS-15, Life satisfaction scale, non-affective psychiatric symptoms, activities of daily living Monthly after admission: Health status, Zung Self-Rating Depression Scale, activities of daily living, non-affective psychiatric symptoms |
Mean monthly number of friends for non-depressed patients: 2.4±2.5 Mean monthly number of friends for depressed patients: 1.6±1.3 Number of friends included in the final model and considered an important factor in predicting depression onset. |
| (Freeman et al., 2016) | Examine the role of physical restraint use, use of antipsychotic medications, and engagement in social activities and cognitive decline | MDS 2.0 Index of Social Engagement (Mor et al., 1995) | Cognitive Performance Scale (John N. Morris et al., 1994) (range: 0 [intact] – 6 [severe impairment]) | Sex, age group (years), dementia, physical restraint use, prescribed antipsychotic medication | 18.2% had no-low social engagement among those with cognitive decline at follow-up. Moderate-high social engagement scores reduced risk of cognitive decline at follow up. |
| (Grabowski & Mitchell, 2010) | Examine the association between private oversight and the quality of end-of-life care for residents with advanced dementia | # of hours per week residents had visits by their health care proxies (HCP) (no visit, 1-7 hours/week of visits, >7 hours/week of visits) | Pressure ulcer, pain, dyspnea, hospice use, hospital transfer, do-not-hospitalize (DNH) order, satisfaction with care at the end-of-life in dementia, antipsychotic use |
Characteristics of residents: Sex, age, ethnicity, general health and disease severity by Bedford Alzheimer Nursing Scale Characteristics of proxy: Sex, child of nursing home resident or not, age (years), education |
Mean number of residents without weekly HCP visitation: 0.12±0.32 Residents with >7 hours/week of visits had increased risk of pressure ulcer, pain, dyspnea, and less likely to have a DNH order. |
| (Hjaltadottir et al., 2011) | Identify factors associated with 3-year mortality | MDS 2.0 Index of Social Engagement (Mor et al., 1995) | National death registry | Age, gender, activities of daily living, changes in health scale, location admitted to nursing home from | Relative to residents with the highest level of social engagement, each other level of social engagement was associated with a faster time to death. |
| (Inventor et al., 2018) | Examine which factors influence positive and negative behaviors among people with Alzheimer’s disease |
Resident activities: solitary, care-related, family/friend visits, structured, unstructured, large and small (2-5 people) |
Positive behaviors: smiling, positive physical expressions, engaging in conversation Negative behaviors: grimacing, verbal aggression, physical aggression, physical non-aggression, repetitive behaviors |
Age, gender, race, cognitive function, physical function, special care dementia unit, # of psychotropic medications and measure of social environment | Solitary activities were associated with fewer episodes of positive behaviors. |
| Derived from 60 direct 5-minute observations of each resident over 12 consecutive weekdays from 9 am to 9 pm | |||||
| (Kiely et al., 2000) | Examine the effect of social engagement on mortality in long term care | MDS 2.0 Index of Social Engagement (Mor et al., 1995) | Time to death based on facility records or last available MDS assessment | Age, gender, limitations in activities of daily living, body mass index, weight loss, heart failure, shortness of breath | 23.1% lacked any social engagement. Residents with higher social engagement had delayed time to death. Residents with no social engagement died faster than residents with maximum social engagement scores. |
| (Kiely & Flacker, 2003) | Examine the effect of social engagement on mortality in long term care | MDS 2.0 Index of Social Engagement (Mor et al., 1995) | Survival time was time between baseline MDS assessment and date of death (from the National Death Index) | Age, gender, activities of daily living, body mass index, recent weight loss, unstable condition, shortness of breath, asthma/ emphysema/chronic obstructive pulmonary disease, diabetes, heart failure, pressure ulcer, cancer, leaves food uneaten, swallowing problem | Among long-stay residents, 6.6% lacked any social engagement and 9.9% had the maximum score on the social engagement index. Residents with higher social engagement had delayed time to death and those without died faster than those with highest social engagement scores. |
| (Kloos et al., 2019) | Quantify the association between the satisfaction of autonomy, relatedness, and competence with depression and well-being among nursing home residents | 8-item relatedness subscale embedded within the 21-item Basic Need Satisfaction in Life Scale (Gagné, 2003) | Measured 5-8 months after baseline: 8-item Dutch version of the GDS (Jongenelis et al., 2007) Dutch version (Custers, Westerhof, Kuin, & Riksen-Walraven, 2010) of the 5-item Satisfaction With Life Scale (Diener, Emmons, Larsen, & Griffin, 1985) |
Autonomy and competence subscales of the Basic Need Satisfaction in Life Scale | The mean relatedness score at baseline was 4.27± 0.58. Relatedness was associated with GDS, but not Satisfaction With Life Scale. |
| (Kroemeke & Gruszczynska, 2016) | Examine the moderating effect of institutional care on the association between support and subjective well-being | Berlin Social Support Scales (Schulz & Schwarzer, 2003) (Received and provided support) | Center for Epidemiological Studies Depression Scale (CES-D) (Radloff, 1977) 3 items from the PANAS (Watson, Clark, & Tellegen, 1988) |
Baseline level of CES-D and positive affect, instrumental activities of daily living, and subjective health | Received support was associated with positive affect. Providing and receiving support was not associated with positive affect. |
| (Lou et al., 2012) | Examine the association between social engagement and depressive symptoms | MDS 2.0 Index of Social Engagement (Mor et al., 1995) | 7-item Depression Rating Scale (J.N. Morris, Murphy, & Nonemaker, 1995) | Age, gender, education, marital status, familial financial support, activities of daily living, cognition, pain | At baseline, the mean index of social engagement was 2.13±1.81. A 1-point increase on the social engagement scale over 1 year resulted in a 0.11-point decrease in the depressive symptoms score with the effect of the quadratic change following a similar pattern. |
| (Mao & Han, 2018) | Examine the associations between living arrangements and psychological well-being and life satisfaction, and the mediating role of social support | Types of social support (financial, instrumental, emotional) and sources of social support (spouse, children, informal (non-family), formal) Living arrangement |
7-item psychological well-being score (higher scores better) Life satisfaction: “How do you rate your life at present?” Range: 1 (very good) to 5 (very bad); categorized as good/very good versus other |
Age, gender, education, marital status, number of children, number children living nearby, and physical and cognitive functions Stratified by rural/urban |
Urban: Compared with living with children, living in nursing homes had small positive direct (and total) effects on life satisfaction, with higher life satisfaction through formal financial support and lower life satisfaction due to not receiving instrumental support from a spouse. Rural: Compared with living with children, nursing homes residents received more financial, instrumental, and emotional support from formal sources and formal financial support (rather than from children) which was associated with better psychological well-being. |
| (Maxwell et al., 2015) | Determine factors associated with hospitalization over 1 year for residents with dementia living in long term care or assisted living | Summary score of strength of social relationships (0-2-low/none, 3-5 moderate/high) Average time in activities when awake |
Time to first event (i.e., hospitalization, admission to long term care, death, transfer to other setting) or 1-year | Age, gender, cognitive impairment, health instability, fatigue, number of medications, previous hospitalizations <1 year, bowel incontinence, rural/urban | Among those in assisted living, 20.5% scored low/none on social relationship strength. Residents with no social relationships were hospitalized/died more quickly than those with moderate/high social relationships. Among those in long term care, 38.2% scored low/none on strength of social relationships. No estimates of hazard ratios provided. |
| (E. Neufeld et al., 2019) | Investigate factors associated with symptoms of depression | MDS 2.0 items Social connectedness /support (binary) Involved in social activities (binary) |
7-item Depression Rating Scale (≥3 probable depression) (Burrows, Morris, Simon, Hirdes, & Phillips, 2000; Eva Neufeld, Hirdes, Perlman, & Rabinowitz, 2015) | Age, gender, marital status, limitations in activities of daily living, cognitive impairment, pain, falls, baseline depression | 23.5% had social activities at baseline. Residents with social connectedness were less likely to develop indicators of probable depression. |
| (Palese et al., 2019) | Identify predictors of self-feeding dependence | Social Engagement Scale and Relationship with Others Scale (Pascazio, 2009) | Self-feeding dependence progression over time measured on an ordinal scale | Age, sex, activities of daily living, cognitive performance scale, depression, pain, behaviors, clinical instability, comorbidities, pressure sores, time order, and facility factors | Social engagement deprivation increased the risk of self-feeding dependence. Engagement with family, health-care workers, or volunteers was protective against the progression of self-feeding dependence. |
| (Pastor-Barriuso et al., 2020) | Estimate the effect of social engagement on long-term all-cause mortality | To what extent do you/does the resident interact with other residents in the institution? | Date of death from facilities and the Spanish National Death Index | Age, gender, education, marital status, number of chronic conditions, functional dependency, length of stay, assigned caregiver, frequency of external visits, facility ownership, facility size | 36.0% of residents had low/no social engagement. No differences between those with moderate levels of social engagement and low/no social engagement at 2, 5, or 10 years of follow up. Standardized mortality risk differences at 5 years were lower for those with high social engagement, but not at 2 or 10 years. |
| (Rozzini et al., 1996) | Identify predictors of mood changes over a 12-month period | Nursing home activities scale (scores 0 [none] to 32 [high level]) (McCaffree & Harkins, 1975) based on observed behaviors | 30-item GDS (Brink et al., 1982) | Age, gender, baseline GDS, baseline measures and changes in: cognitive function, satisfaction with the nursing home environment, Barthel index, chronic symptoms, pain, diseases, disabling diseases, drugs, and self-evaluation score | The mean activity score was 5.0 ± 5.4. Neither baseline activities score or changes in activities score was associated with changes in GDS score. |
| (Vetrano et al., 2018) | Investigate the association between determinants of health and survival | InterRAI LTCF Social participation and family visits (never, ≤3 days, >3 days ago) | InterRAI LTCF death from any cause and date of death | Age, sex, cognitive impairment, functional impairment, body mass index, physical activity, vaccines, and number of diseases | Involvement in social activities and family visits were associated with delayed time to death. |
| (Y. H. Wang et al., 2019) | Evaluate factors associated with resident outcomes | Interview Schedule for Social Interaction (C. Yeh, L, 1999) Frequency of family visits |
GDS-15 (0–5 good, 6–9 melancholy, ≥10 depression) (Luo, Kuo, & Tang, 2012) EuroQol-5D self-reported health status |
Gender, age, baseline data collection, mobility, cognitive function, comorbidities, intervention type and facilities random effects | The frequency of family visits was high (42%) and social support from facility staff was also high (24.66 ± 4.64). Support from facility staff was associated with an increase in utility of quality of life, an increase in self-reported health, and a decrease in depression. |
| (Weiner et al., 1998) | Examine factors associated with pain scales | Quality of residents’ proximate social network (Cohen-Mansfield & Marx, 1992) | Pain scale Pain thermometer |
Age, gender, race, education, marital status, analgesics, cognitive impairment, comorbidity, depression, physical function, self-rated health | Quality of residents’ proximate social network was not associated with pain measures. |
| (Yamada et al., 2016) | Examine whether dual sensory impairment is associated with greater cognitive decline | 7 MDS items comparable to Index of Social Engagement (Mor et al., 1995) | Cognitive Performance Scale (John N. Morris et al., 1994) Changes in CPS over time (baseline, 6 months, 12 months) |
Age, gender, facility, baseline information on primary diagnosis of Alzheimer’s disease, other dementia, and psychiatric diseases, depressive symptoms, cognitive and functional state, communication problem, and use of sensory assistive device | 15.7% had no behaviors indicative of social engagement. Fewer numbers of behaviors indicating social engagement observed were associated with a greater decrease in cognitive function. Concurrent vision and hearing impairment was not associated with a greater cognitive decline when > one behavior indicating social engagement was present. |
| (K.-P. Yeh et al., 2014) | Evaluate factors associated with rapid functional decline and 12-month mortality | MDS 2.0 Index of Social Engagement (Mor et al., 1995) | Recent activities of daily living decline defined as a 1-point increase in RUG-III activities of daily living score in the past 6 months and 1-year mortality | Age, education, body mass index, comorbidities, pain, cognitive impairment, baseline activities of daily living, RAP triggers | Social engagement was not associated with recent functional decline. |
3.5. Synthesis of Quantitative Studies
Table 5 shows that most analyses conducted within the eligible studies focused on mental health outcomes (including anxiety, depressive symptoms, suicidality, and psychological well-being) and quality of life (including satisfaction with life, positive affect, morale, successful aging, self-esteem, and meaning in life). In cross-sectional and cohort analyses, the number of cohorts and cross-sectional studies supporting a positive impact of social connectedness on mental health outcomes (42 versus 8 analyses) and quality of life (35 versus 9 analyses) was higher than those with no association or a negative impact, albeit the number of cohort studies was small. Few studies evaluated physical and cognitive functioning as a health outcome (five analyses), but of those that did, four studies had a positive association between social connectedness and these health outcomes. Few studies evaluated the association between symptoms that older adults often experience (e.g., pain, fatigue) and behavioral problems and social connectedness. Of the eight studies quantifying the effect of social connectedness on death, all but two supported that lack of social connectedness accelerates time to death.
3.6. Quality assessment
Supplemental Tables 2, Supplemental Table 3, and Supplemental Table 4 show the results of the quality review, with a synthesis of each provided below each table.
4. Discussion
With this systematic review of literature, we synthesized the qualitative and quantitative evidence on the relationship between social connectedness and health-related outcomes among older adults living in nursing homes and assisted living settings. We found that across many different countries, many older adults living in these facilities experienced a lack of social connectedness. Evidence supporting the association between social connectedness and physical and mental health outcomes was predominantly from cross-sectional studies. Longitudinal studies were far fewer. Results derived from the cohort studies quantifying the association between social connectedness and the development of depression were mixed. In the four studies evaluating mortality, lack of social connectedness appeared to hasten time to death. Further, many studies excluded residents with cognitive impairment, even though residents with cognitive impairment may feel the deficits in social connectedness most acutely (Bova et al., 2021; Cahill, 2011).
The absence of social connectedness has been portrayed as social disengagement, isolation, or the subjective feeling of loneliness (Berkman, 2000; Bethell, 2021b). Similar to studies of older adults living in the community, our study found that a lack of social engagement or social connectedness still occurred in nursing homes and assisted living settings. Among community-dwelling older adults, risk factors for social isolation include being male, unmarried, low income, and low educational attainment (Cudjoe, 2020). Twenty-four percent of community-dwelling older adults experience social isolation, with 4% classified as severely isolated (Cudjoe, 2020). In long-term care settings, psychiatric disorders, male gender (Chamberlain, 2020), and residing in a facility in socially isolated neighborhoods also contribute to the problem (C. Park, Kim, D., & Briesacher, B. A, 2021). These findings on risk factors for social isolation in the community and long-term care settings demonstrate that the lack of social connectedness may persist as older adults transition from living in the community and are admitted to congregate long-term care settings. Therefore, research to identify newly admitted residents at risk for social isolation may be useful to target residents in need of additional assistance in forming satisfying relationships with peers in their facilities.
Our findings are comparable but distinct from other studies. Two recent scoping reviews, one focused on the mental health impacts of social connection during the COVID-19 pandemic and the other on the physical health impacts of social connection, provided evidence that better social connection is linked to better mood and emotional health (Bethell, 2021b), reduced mortality risk, and better sleep (Lem et al., 2021). However, there are limits to the generalizability of their findings as the quality of their evidence was not assessed (Arksey & O’Malley, 2005). To the best of our knowledge, our study extends the literature as the first systematic review that evaluates both physical and psychological health impacts of social connectedness for older adults in congregate long-term care settings. Our systematic review findings (published predominantly before the COVID-19 pandemic) were less definitive, with stronger associations in cross-sectional than cohort studies, but showed consistent evidence linking lower social connectedness to hastened mortality. Several physical and mental conditions, such as dementia, cognitive decline, obesity, anxiety, depression, suicide, alcoholism, aggression, impulsivity, hypertension, stroke, and heart disease, have been linked to loneliness and social isolation (Bethell, 2021a; Cacioppo, 2015; Shankar, 2013; "Social isolation, loneliness in older people pose health risks," 2019). Engaging with others in meaningful activities may ultimately lead to both improved mood and longevity (Cornwell, 2008; "Social isolation, loneliness in older people pose health risks," 2019). Indeed, stronger social relationships may improve longevity as much as quitting smoking, increasing physical activity, or reducing obesity with a 50% increased likelihood of survival among those with stronger social ties (Holt-Lunstad, 2010).
4.1. Practice Implications
Our study revealed that lack of or reduced social connectedness commonly occurred among older adults living in congregate long-term care settings. Social connectedness is a modifiable risk factor for adverse health outcomes in these older adults. A recent systematic review and meta-analysis of randomized trials has shown that interventions to improve social connectedness are effective (Zagic, 2022). The extent to which such interventions may be feasible in long-term care settings remains unknown. Long-term care facilities attempt to promote social connectedness using a variety of strategies such as communal dining, group activities, shared rooming, and involvement of family members. Key strategies for enhancing social connections include phone calls and visits with family and friends, having personal objects available to residents that bridge their past and present, promoting relationships among fellow residents and staff to build a sense of community, and providing both structure and meaning by offering appropriate organized recreational activities (Naik P, 2020). To be effective, however, social engagement needs to be authentic and responsive to personal choice within an environment that promotes comfort and privacy (Callahan, n.d). Active counseling for long-term care residents to increase social connections and prescribing opportunities for connection have also been suggested (Hicks, 2000; Martino, 2015). Yet, promoting authentic engagement in these settings can be challenging due to factors including short-staffing, resource limitations, and an overall orientation that focuses more on medical care and less on practices related to quality of life (Kane, 2001).
4.2. Research Implications
Most studies eligible for our systematic review used cross-sectional study designs. Among these cross-sectional studies, most linked higher social connectedness to reduced depression, albeit the temporal sequence is unclear owing to the nature of the study design. Additional longitudinal studies are needed to further understand the extent to which social connectedness impacts health outcomes in older adults in congregate living situations.
How social connectedness may affect other health outcomes is not well understood. Negative cognitive effects of social isolation are thought to be related to 1) lack of social stimulation on the brain thereby reducing cognitive reserve and brain resilience (Evans, 2018; Read, 2020) or 2) induction of prolonged stress that may reduce cognitive functioning (Read, 2020; Seeman, 2001). Social connection may have a positive effect on health by reducing inflammation and enhancing antiviral responses (Leschak, 2019). The mechanism for these improved outcomes may be the promotion of adaptive responses to acute or chronic stressors which then lessen their negative effects on health (Holt-Lunstad, 2010). We found that most studies focused on depression as the health outcome of interest. Quantifying the impact of social connectedness on a variety of health outcomes may provide evidence to support (or refute) various hypothesized mechanisms relating social connectedness to health outcomes.
4.3. Strengths and Limitations
There are several strengths to our study. We used the PRISMA guidelines to guide our systematic review (Moher, 2009; Shamseer, 2015). We also consulted a research librarian to produce search terms that were defined as broadly as possible to enable us to capture as many relevant articles as possible across five different databases. Further, our team conducted dual checks and reviews of the quality and bias assessment of the studies to ensure the accuracy of this systematic review.
There are limitations as well. Despite our best effort to include all possible articles in our search, we may have missed relevant articles in our study. We also did not include articles reported in other languages. Thus, there is a publication bias toward articles written in English. Last, we cannot perform a meta-analysis due to the heterogeneity in methodologies used in the different studies included in our systematic review.
5. Conclusions
Across all studies, a lack of social connectedness was shown to affect older adults living in nursing homes and assisted living facilities. We found fairly consistent findings from cross-sectional studies showing an association between social connectedness and depressive symptoms. Our systematic review highlights the need for additional longitudinal studies to further understand the extent to which social connectedness impacts health outcomes in older adults in congregate living situations. Qualitative studies included in our review provided insights on how to enhance social connectedness for older adults transitioning to congregate living settings. With these findings in hand, interventions need to be developed and studied to provide a robust evidence-base for a population often neglected by the evidence. Without such evidence, administrators of nursing homes and assisted living facilities will be left guessing about how best to promote social connectedness as older adults acclimate to their new homes.
Supplementary Material
SUMMARY STATEMENT OF IMPLICATIONS FOR PRACTICE.
What does this research add to existing knowledge in gerontology?
Our research is the first systematic review that demonstrates the health impacts of social connectedness among older adults living in congregate long-term care settings.
This research identifies significant research gaps which call for more longitudinal studies of the health impacts of social connectedness among older adults living in congregate long-term care settings.
What are the implications of this new knowledge for nursing care with older people?
Nursing homes and assisted living settings must determine how best to promote social connectedness among residents given its association with health outcomes.
Care staff should be trained to understand the need for and importance of social connectedness in congregate long-term care settings.
How could the findings be used to influence policy or practice or research or education?
Care policies to address ways to maintain older adults’ social needs in congregate long-term care settings in the event of another pandemic are necessary.
Policies to emphasize the significance of social connectedness as an essential component of staff training curriculum.
There is a need for more longitudinal research on the effectiveness of interventions to promote social connectedness in long-term care settings.
Acknowledgments:
We acknowledge the assistance of Becky Baltich Nelson, research librarian at the University of Massachusetts Chan Medical School. The work was funded by a grant to Dr. Lapane from the National Institutes of Health (R01AG071692).
Appendix Search Strategy
Note: One search strategy was used to address the needs of two systematic reviews: 1) focused on loneliness; and 2) (the current study) focused on social connectedness. The comprehensive search strategy is shown below.
Databases and limits
We searched the following five databases with limits shown in parentheses and number of records: CINAHL (limited to Jan 1990 – August 2021, English language, Peer-reviewed, Human; n=416), Scopus (limited to 1990 – 2021, English, Humans; n=2,733), Cochrane Library (limited to Cochrane reviews only, Jan 1990 – August 2021; n=2,400), MEDLINE Complete = 3,351 (limited to 1990-2021, English, Humans; n=3,351), and PsycINFO (limited to 1990-2021, English, Humans, Peer-reviewed journals; n=1,304).
Search Algorithms
The search algorithms combine three domains: Setting, Determinant, and Outcomes
The syntax for CINAHL as shown:
Setting:
(Assisted Living Facilities [MH] OR (assisted adj3 living) OR (MH "Housing for the Elderly") OR Homes for the Aged [MH] OR ( ((home* adj3 aged) or (old adj3 age adj3 home*) or (housing adj3 elderly) or (retirement adj3 (home* or center* or centre*)))) OR (MH "Long Term Care") OR (long adj3 term adj3 care) OR
(MH "Nursing Homes+") OR (((nursing adj3 home*) or (intermediate adj3 care adj3 facility*) or (skilled adj3 nursing adj3 facility*) or (extended adj3 (care or nursing) adj3 facilit*))) OR (MH "Rehabilitation Centers") OR (((rehab* adj3 (center* or centre*)) or (inpatient adj3 rehabilitation))) OR (MH "Residential Facilities") OR (residential adj3 facilit*) OR
(MH "Subacute Care") OR (((subacute or sub-acute or postacute or post-acute) adj3 care)))
AND
Determinant:
(Friends [MH] OR ((friend* or companion* or acquaintance*)) OR Group Structure [MH] OR (((group adj3 structure*) or (informal adj3 network*) or (network adj3 composition*))) OR (MH "Interpersonal Relations") OR (((interpersonal or social*) adj3 relation*)) OR (MH "Patient Isolation") OR ((patient adj3 (exclu* or isolat* or seclu*))) OR (MH "Peer Group") OR ((peer adj3 (group* or relation*))) OR ((MH "Recreational Therapy") OR (MH "Recreation Therapy (Iowa NIC)")) OR (recreation* adj3 therap*) OR (MH "Social Inclusion") OR (social* adj3 inclu*) OR (MH "Social Isolation") OR (MH "Social Isolation (Saba CCC)") OR (MH "Social Isolation (NANDA)") OR
((MH "Social Isolation") OR (MH "Social Isolation (Saba CCC)") OR (MH "Social Isolation (NANDA)")) OR (((social* adj3 (alienat* or breakdown* or depriv* or exclu* or isolat*)) or ostraci* or lonel*)) OR (MH "Social Participation") OR ((social* adj3 (activit* or citizenship or engag* or participat*))) OR (MH "Social Skills") OR (((interpersonal or social*) adj3 (ability* or competenc* or skill*))) OR (MH "Social Support (Iowa NOC)") OR (((social* adj3 (care or connect* or support*)) or (psychosocial adj3 support*))))
AND
Outcomes:
(MH "Anhedonia") OR (MH "Anxiety") OR (MH "Anxiety (Saba CCC)") OR (MH "Behavioral Symptoms") OR
(MH "Cognitive Therapy") OR ( (((cognitive or mental) adj3 (dysfunction* or impair* or declin* or deteriorat*)) or (neurocognitive adj3 disorder*))) OR (MH "Confusion (Saba CCC)") OR (MH "Confusion") OR (MH "Death") OR
Frailty [MH] OR ((frail* or debilit*)) OR (MH "Functional Status") OR ((functional adj3 (declin* or dependence* or status*))) OR (MH "Hospitalization") OR Illness Behavior [MH] OR (((illness or sickness) adj3 behavior*)) OR
(Lethargy [MH] OR lethargy) OR (MH "Mental Health") OR (((mental or psychological) adj3 (health or well-being or wellbeing))) OR ((MH "Morbidity") OR morbidit) OR (MH "Mortality") OR (Patient Readmission [MH] OR readmission*) OR (MH "Quality of Life") OR (MH "Quality of Life") OR (((quality adj3 life) or HRQOL or (life adj3 satisfaction))) OR
( "Sleep Initiation and Maintenance Disorders" [MH] ) OR (((sleep adj5 (disorder* or dysfunction*)) or DIMS or (early adj3 awakening) or insomnia* or sleeplessness))
The syntax for MEDLINE and PsycINFO as shown:
Setting:
((Assisted Living Facilities/ or (assisted adj3 living).ti,ab.) OR (Homes for the Aged/ or Housing for the Elderly/ or ((home* adj3 aged) or (old adj3 age adj3 home*) or (housing adj3 elderly) or (retirement adj3 (home* or center* or centre*))).ti,ab.) OR (Long-Term Care/ or (long adj3 term adj3 care).ti,ab.) OR (exp Nursing Homes/ or ((nursing adj3 home*) or (intermediate adj3 care adj3 facility*) or (skilled adj3 nursing adj3 facility*) or (extended adj3 (care or nursing) adj3 facilit*)).ti,ab.) OR (Rehabilitation Centers/ or ((rehab* adj3 (center* or centre*)) or (inpatient adj3 rehabilitation)).ti,ab.) OR (Residential Facilities/ or (residential adj3 facilit*).ti,ab.) OR (Subacute Care/ or ((subacute or sub-acute or postacute or post-acute) adj3 care).ti,ab.))
AND
Determinant:
((Friends/ or (friend* or companion* or acquaintance*).ti,ab.) OR (Group Structure/ or ((group adj3 structure*) or (informal adj3 network*) or (network adj3 composition*)).ti,ab.) OR (Interpersonal Relations/ or ((interpersonal or social*) adj3 relation*).ti,ab.) OR (Patient Isolation/ or (patient adj3 (exclu* or isolat* or seclu*)).ti,ab.) OR (Peer Group/ or (peer adj3 (group* or relation*)).ti,ab.) OR (Recreation Therapy/ or (recreation* adj3 therap*).ti,ab.) OR (Social Inclusion/ or (social* adj3 inclu*).ti,ab.) OR (Social Isolation/ or ((social* adj3 (alienat* or breakdown* or depriv* or exclu* or isolat*)) or ostraci* or lonel*).ti,ab.) OR (Social Participation/ or (social* adj3 (activit* or citizenship or engag* or participat*)).ti,ab.) OR (Social Skills/ or ((interpersonal or social*) adj3 (ability* or competenc* or skill*)).ti,ab.) OR (exp Social Support/ or ((social* adj3 (care or connect* or support*)) or (psychosocial adj3 support*)).ti,ab.))
AND
Outcomes:
((Anhedonia/ or anhedonia*.ti,ab.) OR (Anxiety/ or (anxiet* or angst or hypervigilan* or nervousness).ti,ab.) OR (exp Behavioral Symptoms/ or (((affective or behavior*) adj3 symptom*) or alexithymia* or (emotion* adj3 disturbance*) or aggressi* or catatoni* or delusion* or depersonalization* or depressi* or encopresis or enuresis or (urinary adj3 incontinence) or (daytime adj3 wetting) or bedwetting or ((functional or nonorganic or psychogenic) adj3 hearing adj3 loss*) or malingering or (mental adj3 fatigue*) or (neuropsychiatric adj3 symptom*) or obsessi* or paranoi* or ((primary or psychogenic) adj3 polydipsia*) or (problem adj3 behavior*) or (self adj3 (destructive or harm* or injur* or mutilat*)) or NSSH or NSSI or suicid* or ((life or psychological) adj3 stress*) or wandering).ti,ab.) OR (Cognitive Dysfunction/ or (((cognitive or mental) adj3 (dysfunction* or impair* or declin* or deteriorat*)) or (neurocognitive adj3 disorder*)).ti,ab.) OR (exp Confusion/ or (confusion* or disorientation* or bewilderment or delirium*).ti,ab.) OR (Death/ or (death or (end adj3 life)).ti,ab.) OR (Diagnostic Self Evaluation/ or ((self adj3 (appraisal* or evaluation*)) or (self adj3 report* adj3 health) or (subjective adj3 health)).ti,ab.) OR (Frailty/ or (frail* or debilit*).ti,ab.) OR (Functional Status/ or (functional adj3 (declin* or dependence* or status*)).ti,ab.) OR (Hospitalization/ or hospitalization*.ti,ab.) OR (Illness Behavior/ or ((illness or sickness) adj3 behavior*).ti,ab.) OR (Lethargy/ or lethargy.ti,ab.) OR (Mental Health/ or ((mental or psychological) adj3 (health or well-being or wellbeing)).ti,ab.) OR (Morbidity/ or morbidit.ti,ab.) OR (Mortality/ or (mortalit* or ((death or fatalit*) adj3 rate*)).ti,ab.) OR (Patient Readmission/ or readmission*.ti,ab.) OR (Quality of Life/ or ((quality adj3 life) or HRQOL or (life adj3 satisfaction)).ti,ab.) OR ("Sleep Initiation and Maintenance Disorders"/ or ((sleep adj5 (disorder* or dysfunction*)) or DIMS or (early adj3 awakening) or insomnia* or sleeplessness).ti,ab.)
The syntax for Scopus as shown:
Setting:
((TITLE-ABS((assisted W/3 living))) OR (TITLE-ABS(((home* w/3 aged) or (old w/3 age w/3 home*) or (housing w/3 elderly) or (retirement w/3 (home* or center* or centre*))))) OR (TITLE-ABS((long w/3 term w/3 care))) OR (TITLE-ABS(((nursing w/3 home*) or (intermediate w/3 care w/3 facility*) or (skilled w/3 nursing w/3 facility*) or (extended w/3 (care or nursing) w/3 facilit*)))) OR (TITLE-ABS(((rehab* w/3 (center* or centre*)) or (inpatient w/3 rehabilitation)))) OR (TITLE-ABS((residential w/3 facilit*))) OR (TITLE-ABS(((subacute or sub-acute or postacute or post-acute) w/3 care))))
AND
Determinant:
((TITLE-ABS(friend* or companion* or acquaintance*)) OR (TITLE-ABS((interpersonal or social*) w/3 relation*)) OR (TITLE-ABS(((group w/3 structure*) or (informal w/3 network*) or (network w/3 composition*)))) OR (TITLE-ABS((patient w/3 (exclu* or isolat* or seclu*)))) OR (TITLE-ABS((peer w/3 (group* or relation*)))) OR (TITLE-ABS((recreation* w/3 therap*))) OR (TITLE-ABS((social* w/3 inclu*))) OR (TITLE-ABS(((social* w/3 (alienat* or breakdown* or depriv* or exclu* or isolat*)) or ostraci* or lonel*))) OR (TITLE-ABS((social* w/3 (activit* or citizenship or engag* or participat*)))) OR (TITLE-ABS(((interpersonal or social*) w/3 (ability* or competenc* or skill*)))) OR (TITLE-ABS(((social* w/3 (care or connect* or support*)) or (psychosocial w/3 support*)))))
AND
Outcomes:
((TITLE-ABS(anhedonia*)) OR (TITLE-ABS((anxiet* or angst or hypervigilan* or nervousness))) OR (TITLE-ABS((((affective or behavior*) w/3 symptom*) or alexithymia* or (emotion* w/3 disturbance*) or aggressi* or catatoni* or delusion* or depersonalization* or depressi* or encopresis or enuresis or (urinary w/3 incontinence) or (daytime w/3 wetting) or bedwetting or ((functional or nonorganic or psychogenic) w/3 hearing w/3 loss*) or malingering or (mental w/3 fatigue*) or (neuropsychiatric w/3 symptom*) or obsessi* or paranoi* or ((primary or psychogenic) w/3 polydipsia*) or (problem w/3 behavior*) or (self w/3 (destructive or harm* or injur* or mutilat*)) or NSSH or NSSI or suicid* or ((life or psychological) w/3 stress*) or wandering))) OR (TITLE-ABS((((cognitive or mental) w/3 (dysfunction* or impair* or declin* or deteriorat*)) or (neurocognitive w/3 disorder*)))) OR (TITLE-ABS((confusion* or disorientation* or bewilderment or delirium*))) OR (TITLE-ABS((death or (end w/3 life)))) OR (TITLE-ABS(((self w/3 (appraisal* or evaluation*)) or (self w/3 report* w/3 health) or (subjective w/3 health)))) OR (TITLE-ABS((frail* or debilit*))) OR (TITLE-ABS((functional w/3 (declin* or dependence* or status*)))) OR (TITLE-ABS(hospitalization*)) OR (TITLE-ABS(((illness or sickness) w/3 behavior*))) OR (TITLE-ABS(lethargy)) OR (TITLE-ABS(((mental or psychological) w/3 (health or well-being or wellbeing)))) OR (TITLE-ABS(morbidity)) OR (TITLE-ABS((mortalit* or ((death or fatalit*) w/3 rate*)))) OR (TITLE-ABS(readmission*)) OR (TITLE-ABS(((quality w/3 life) or HRQOL or (life w/3 satisfaction)))) OR (TITLE-ABS(((sleep w/5 (disorder* or dysfunction*)) or DIMS or (early w/3 awakening) or insomnia* or sleeplessness))))
The syntax for Cochrane Library as shown:
Setting:
(MeSH descriptor: [Assisted Living Facilities] this term only OR (assisted near/3 living) OR MeSH descriptor: [Homes for the Aged] this term only OR MeSH descriptor: [Housing for the Elderly] this term only OR ((home* near/3 aged) or (old near/3 age near/3 home*) or (housing near/3 elderly) or (retirement near/3 (home* or center* or centre*))) OR MeSH descriptor: [Long-Term Care] this term only OR (long near/3 term near/3 care) OR MeSH descriptor: [Nursing Homes] explode all trees OR ((nursing near/3 home*) or (intermediate near/3 care near/3 facility*) or (skilled near/3 nursing near/3 facility*) or (extended near/3 (care or nursing) near/3 facilit*)) OR MeSH descriptor: [Rehabilitation Centers] this term only OR ((rehab* near/3 (center* or centre*)) or (inpatient near/3 rehabilitation)) OR MeSH descriptor: [Residential Facilities] this term only OR (residential near/3 facilit*) OR MeSH descriptor: [Subacute Care] this term only OR ((subacute or sub-acute or postacute or post-acute) near/3 care))
AND
Determinant:
(MeSH descriptor: [Friends] this term only OR (friend* or companion* or acquaintance*) OR MeSH descriptor: [Group Structure] this term only OR ((group near/3 structure*) or (informal near/3 network*) or (network near/3 composition*)) OR MeSH descriptor: [Interpersonal Relations] this term only OR ((interpersonal or social*) near/3 relation*) OR MeSH descriptor: [Patient Isolation] explode all trees OR (patient near/3 (exclu* or isolat* or seclu*)) OR MeSH descriptor: [Peer Group] this term only OR (peer near/3 (group* or relation*)) OR MeSH descriptor: [Recreation Therapy] this term only OR (recreation* near/3 therap*) OR MeSH descriptor: [Social Inclusion] this term only OR (social* near/3 inclu*) OR MeSH descriptor: [Social Isolation] this term only OR ((social* near/3 (alienat* or breakdown* or depriv* or exclu* or isolat*)) or ostraci* or lonel*) OR MeSH descriptor: [Social Participation] this term only OR (social* near/3 (activit* or citizenship or engag* or participat*)) OR MeSH descriptor: [Social Skills] this term only OR ((interpersonal or social*) near/3 (ability* or competenc* or skill*)) OR MeSH descriptor: [Social Support] explode all trees OR ((social* near/3 (care or connect* or support*)) or (psychosocial near/3 support*)))
AND
Outcomes:
(MeSH descriptor: [Anhedonia] this term only OR anhedonia* OR MeSH descriptor: [Anxiety] this term only OR (anxiet* or angst or hypervigilan* or nervousness) OR MeSH descriptor: [Behavioral Symptoms] explode all trees OR (((affective or behavior*) near/3 symptom*) or alexithymia* or (emotion* near/3 disturbance*) or aggressi* or catatoni* or delusion* or depersonalization* or depressi* or encopresis or enuresis or (urinary near/3 incontinence) or (daytime near/3 wetting) or bedwetting or ((functional or nonorganic or psychogenic) near/3 hearing near/3 loss*) or malingering or (mental near/3 fatigue*) or (neuropsychiatric near/3 symptom*) or obsessi* or paranoi* or ((primary or psychogenic) near/3 polydipsia*) or (problem near/3 behavior*) or (self near/3 (destructive or harm* or injur* or mutilat*)) or NSSH or NSSI or suicid* or ((life or psychological) near/3 stress*) or wandering) OR MeSH descriptor: [Cognitive Dysfunction] this term only OR (((cognitive or mental) near/3 (dysfunction* or impair* or declin* or deteriorat*)) or (neurocognitive near/3 disorder*)) OR MeSH descriptor: [Confusion] explode all trees OR (confusion* or disorientation* or bewilderment or delirium*) OR MeSH descriptor: [Death] this term only OR (death or (end near/3 life)) OR MeSH descriptor: [Diagnostic Self Evaluation] this term only OR ((self near/3 (appraisal* or evaluation*)) or (self near/3 report* near/3 health) or (subjective near/3 health)) OR MeSH descriptor: [Frailty] this term only OR (frail* or debilit*) OR MeSH descriptor: [Functional Status] this term only OR (functional near/3 (declin* or dependence* or status*)) OR MeSH descriptor: [Hospitalization] explode all trees OR hospitalization* OR MeSH descriptor: [Illness Behavior] this term only OR ((illness or sickness) near/3 behavior*) OR MeSH descriptor: [Lethargy] this term only OR lethargy OR MeSH descriptor: [Mental Health] this term only OR ((mental or psychological) near/3 (health or well-being or wellbeing)) OR MeSH descriptor: [Morbidity] this term only OR morbidity OR MeSH descriptor: [Mortality] this term only OR (mortalit* or ((death or fatalit*) near/3 rate*)) OR MeSH descriptor: [Patient Readmission] this term only OR readmission* OR MeSH descriptor: [Quality of Life] this term only OR ((quality near/3 life) or HRQOL or (life near/3 satisfaction)) OR MeSH descriptor: [Sleep Initiation and Maintenance Disorders] this term only OR ((sleep near/5 (disorder* or dysfunction*)) or DIMS or (early near/3 awakening) or insomnia* or sleeplessness))
Footnotes
Conflicts of interest: The authors have no conflicts of interest.
Data availability:
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
REFERENCES
- Adra MG, Hopton J, & Keady J (2015). Constructing the meaning of quality of life for residents in care homes in the Lebanon: perspectives of residents, staff and family. Int J Older People Nurs, 10(4), 306–318. doi: 10.1111/opn.12094 [DOI] [PubMed] [Google Scholar]
- Algase DL, Antonakos C, Yao L, Beattie ER, Hong GR, & Beel-Bates CA (2008). Are wandering and physically nonaggressive agitation equivalent? Am J Geriatr Psychiatry, 16(4), 293–299. [DOI] [PubMed] [Google Scholar]
- Arksey H, O'Malley L (2005). Scoping studies: towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- Baldacchino DR, & Bonello L (2013). Anxiety and depression in care homes in Malta and Australia: part 2. Br J Nurs, 22(13), 780–785. doi: 10.12968/bjon.2013.22.13.780 [DOI] [PubMed] [Google Scholar]
- Beck AM, & Ovesen L (2003). Influence of Social Engagement and Dining Location on Nutritional Intake and Body Mass Index of Old Nursing Home Residents. Journal of Nutrition For the Elderly, 22(4), 1–11. doi: 10.1300/J052v22n04_01 [DOI] [Google Scholar]
- Beerens HC, de Boer B, Zwakhalen SMG, Tan FES, Ruwaard D, Hamers JPH, & Verbeek H (2016). The association between aspects of daily life and quality of life of people with dementia living in long-term care facilities: a momentary assessment study. International Psychogeriatrics, 28(8), 1323–1331. doi: 10.1017/S1041610216000466 [DOI] [PubMed] [Google Scholar]
- Bergland A, & Kirkevold M (2006). Thriving in nursing homes in Norway: contributing aspects described by residents. Int J Nurs Stud, 43(6), 681–691. doi: 10.1016/j.ijnurstu.2005.09.006 [DOI] [PubMed] [Google Scholar]
- Bergland A, & Kirkevold M (2007). The significance of peer relationships to thriving in nursing homes. J Clin Nurs, 17(10), 1295–1302. doi: 10.1111/j.1365-2702.2007.02069.x [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, & Seeman TE (2000). From social integration to health: Durkheim in the new millennium. Soc Sci Med, 51(6), 843–857. [DOI] [PubMed] [Google Scholar]
- Bethell J, Aelick K, Babineau J, Bretzlaff M, Edwards C, Gibson J, Hewitt C, Iaboni A, Lender D, Schon D, & McGilton KS (2021a). Social connection and physical health outcomes among long-term care home residents: a scoping review. BMC Geriatr, 722(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethell J, Aelick K, Babineau J, Bretzlaff M, Edwards C, Gibson J, Hewitt C, Iaboni A, Lender D, Schon D, & McGilton KS (2021b). Social Connection in Long-Term Care Homes: A Scoping Review of Published Research on the Mental Health Impacts and Potential Strategies During COVID-19. J Am Med Dir Assoc, 22(2), 228–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitzan JE (1998). EMOTIONAL BONDEDNESS AND SUBJECTIVE WELL-BEING: Between Nursing Home Roommates. Journal of Gerontological Nursing, 24(9), 8–9. doi: 10.3928/0098-9134-19980901-08 [DOI] [PubMed] [Google Scholar]
- Björk S, Lindkvist M, Wimo A, Juthberg C, Bergland Å, & Edvardsson D (2017). Residents’ engagement in everyday activities and its association with thriving in nursing homes. Journal of Advanced Nursing, 73(8), 1884–1895. doi: 10.1111/jan.13275 [DOI] [PubMed] [Google Scholar]
- Bova C, Jesdale B, Mbrah A, Botelho L, Lapane K (2021). Development and psychometric evaluation of the Social Connectedness Index in nursing home residents with Alzheimer’s disease and dementia using the Minimum Data Set 3.0. Geriatric Psychiatry, 36(7), 1110–1119. 10.1002/gps.5516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradshaw SA, Playford ED, & Riazi A (2012). Living well in care homes: a systematic review of qualitative studies. Age Ageing, 41(4), 429–440. [DOI] [PubMed] [Google Scholar]
- Brink TL, Yesavage JA, Lum O, Heersema PH, Adey M, & Rose TL (1982). Screening Tests for Geriatric Depression. Clinical Gerontologist, 1(1), 37–43. doi: 10.1300/J018v01n01_06 [DOI] [Google Scholar]
- Burrows AB, Morris JN, Simon SE, Hirdes JP, & Phillips C (2000). Development of a Minimum Data Set-based depression rating scale for use in nursing homes. Age and Ageing, 29, 165–172. doi: 10.1093/ageing/29.2.165 [DOI] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT (2015). Loneliness: clinical import and interventions. Perspect Psychol Sci, 10(2), 238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill S, & Diaz-Ponce AM (2011). 'I hate having nobody here. I'd like to know where they all are': Can qualitative research detect differences in quality of life among nursing home residents with different levels of cognitive impairment? Aging Ment Health, 15(5), 562–572. [DOI] [PubMed] [Google Scholar]
- Callahan A, & Kartupelis J (n.d). Meaningful Relationships in Long Term Care — Helping Residents Make Their House a Home. Social Work Today. [Google Scholar]
- Carpenter BD (2002). Family, Peer, and Staff Social Support in Nursing Home Patients: Contributions to Psychological Well-Being. Journal of Applied Gerontology, 21(3), 275–293. doi: 10.1177/073346480202100301 [DOI] [Google Scholar]
- Chamberlain SA, Duggleby W, Teaster PB, & Estabrooks CA (2020). Characteristics of Socially Isolated Residents in Long-Term Care: A Retrospective Cohort Study. Gerontol Geriatr Med., 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang HT, Liu LF, Chen CK, Hwang SJ, Chen LK, & Lu FH (2010). Correlates of institutionalized senior veterans' quality of life in Taiwan. Health and Quality of Life Outcomes, 8(1), 70. doi: 10.1186/1477-7525-8-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L. (2015). Reexamining the Relationship Between Leisure and Stress Among Older Adults. Journal of Leisure Research, 47(3), 358–372. doi: 10.1080/00222216.2015.11950365 [DOI] [Google Scholar]
- Chang LC (2018). Is Social Support Always Related to Stress Reduction in Nursing Home Residents? A Study in Leisure Contexts. Research in Gerontological Nursing, 11(4), 174–180. doi: 10.3928/19404921-20180502-02 [DOI] [PubMed] [Google Scholar]
- Chao S, & Chen Y (2019). Environment patterns and mental health of older adults in long-term care facilities: the role of activity profiles. Aging & Mental Health, 23(10), 1307–1316. doi: 10.1080/13607863.2018.1484889 [DOI] [PubMed] [Google Scholar]
- Chau R, Kissane DW, & Davison TE (2021). Risk Factors for Depression in Long-term Care: A Prospective Observational Cohort Study. Clin Gerontol, 44(2), 112–125. doi: 10.1080/07317115.2019.1635548 [DOI] [PubMed] [Google Scholar]
- Chen Y, Lin K, Wu C, Chen C, & Hsieh Y (2020). Determinants of quality of life in the older residents of long-term care facilities using the World Health Organization International Classification of Functioning, Disability and Health framework in Taiwan. Disability and Rehabilitation, 42(16), 2325–2333. doi: 10.1080/09638288.2018.1559888 [DOI] [PubMed] [Google Scholar]
- Chen Y, Lin L, Chuang L, & Chen M (2017). The Relationship of Physiopsychosocial Factors and Spiritual Well-Being in Elderly Residents: Implications for Evidence-Based Practice. Worldviews on Evidence-Based Nursing, 14(6), 484–491. doi: 10.1111/wvn.12243 [DOI] [PubMed] [Google Scholar]
- Chen Y, Ryden MB, Feldt K, & Savik K (2000). The relationship between social interaction and characteristics of aggressive, cognitively impaired nursing home residents. American Journal of Alzheimer's Disease, 15(1), 10–17. doi: 10.1177/153331750001500108 [DOI] [Google Scholar]
- Chen Y, Wu M, Zeng T, Peng C, Zhao M, Xiao Q, … Wang X (2020). Effect of pain on depression among nursing home residents: Serial mediation of perceived social support and self-rated health. A cross-sectional study. Geriatrics & Gerontology International, 20(12), 1234–1240. doi: 10.1111/ggi.14067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YM, Hwang SJ, Chen LK, Chen DY, & Lan CF (2009). Urinary incontinence among institutionalized oldest old Chinese men in Taiwan. Neurourol Urodyn, 28(4), 335–338. doi: 10.1002/nau.20628 [DOI] [PubMed] [Google Scholar]
- Cheng S-T, Lee CKL, & Chow PK-Y (2010). Social support and psychological well-being of nursing home residents in Hong Kong. International Psychogeriatrics, 22(7), 1185–1190. doi: 10.1017/S1041610210000220 [DOI] [PubMed] [Google Scholar]
- Chipps J, & Jarvis MA (2015). Social capital and mental well-being of older people residing in a residential care facility in Durban, South Africa. Aging & Mental Health, 20(12), 1264–1270. doi: 10.1080/13607863.2015.1105196 [DOI] [PubMed] [Google Scholar]
- Cho E, Kim H, Kim J, Lee K, Meghani SH, & Chang SJ (2017). Older Adult Residents' Perceptions of Daily Lives in Nursing Homes. J Nurs Scholarsh, 49(5), 495–503. doi: 10.1111/jnu.12314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho J, Martin P, Margrett J, MacDonald M, Johnson MA, Poon LW, … Davey A (2012). Multidimensional predictors of fatigue among octogenarians and centenarians. Gerontology, 58(3), 249–257. doi: 10.1159/000332214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi H, Jung Y-I, & Kim H (2018). Factors related to aggressive behaviors among older adults in nursing homes of Korea: A cross-sectional survey study. International Journal of Nursing Studies, 88, 9–15. doi: 10.1016/j.ijnurstu.2018.07.014 [DOI] [PubMed] [Google Scholar]
- Cohen-Louck K, & Aviad Y (2020). Suicidal Tendencies, Meaning in Life, Family Support, and Social Engagement of the Elderly Residing in the Community and in Institutional Settings. The Israel journal of psychiatry and related sciences, 57, 13–22. [Google Scholar]
- Cohen-Mansfield J, & Marx MS (1992). The Social Network of the Agitated Nursing Home Resident. Research on Aging, 14(1), 110–123. doi: 10.1177/0164027592141006 [DOI] [Google Scholar]
- Cohen-Mansfield J, Marx MS, Lipson S, & Werner P (1999). Predictors of Mortality in Nursing Home Residents. Journal of Clinical Epidemiology, 52(4), 273–280. doi: 10.1016/S0895-4356(98)00156-5 [DOI] [PubMed] [Google Scholar]
- Commerford MC, & Reznikoff M (1996). Relationship of Religion and Perceived Social Support to Self-Esteem and Depression in Nursing Home Residents. The Journal of Psychology, 130(1), 35–50. doi: 10.1080/00223980.1996.9914986 [DOI] [PubMed] [Google Scholar]
- Cornwell B, Laumann EO, & Schumm LP (2008). The Social Connectedness of Older Adults: A National Profile. Am Sociol Rev, 73(2), 185–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa D, Mercieca-Bebber R, Rutherford C, Tait MA, King MT (2021, Aug). How is quality of life defined and assessed in published research? Qual Life Res, 30(8), 2109–2121. 10.1007/s11136-021-02826-0 [DOI] [PubMed] [Google Scholar]
- Creighton AS, Davison TE, & Kissane DW (2019). The Factors Associated With Anxiety Symptom Severity in Older Adults Living in Nursing Homes and Other Residential Aged Care Facilities. Journal of Aging and Health, 31(7), 1235–1258. doi: 10.1177/0898264318767781 [DOI] [PubMed] [Google Scholar]
- Cudjoe TKM, Roth DL, Szanton SL, Wolff JL, Boyd CM, & Thorpe RJ (2020). The Epidemiology of Social Isolation: National Health and Aging Trends Study. J Gerontol B Psychol Sci Soc Sci, 75(1), 107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, & Van Lammeren P (1999). Depressive symptoms in chronically ill elderly people in residential homes. Aging & Mental Health, 3(3), 221–226. doi: 10.1080/13607869956172 [DOI] [Google Scholar]
- Cummings SM (2002). Predictors of Psychological Well-being among Assisted-Living Residents. Health & Social Work, 27(4), 293–302. doi: 10.1093/hsw/27.4.293 [DOI] [PubMed] [Google Scholar]
- Cummings SM, & Cockerham C (2004). Depression and Life Satisfaction in Assisted Living Residents. Clinical Gerontologist, 27(1-2), 25–42. doi: 10.1300/J018v27n01_04 [DOI] [Google Scholar]
- Custers AFJ, Westerhof GJ, Kuin Y, & Riksen-Walraven M (2010). Need fulfillment in caring relationships: Its relation with well-being of residents in somatic nursing homes. Aging & Mental Health, 14, 731–739. doi: 10.1080/13607861003713133 [DOI] [PubMed] [Google Scholar]
- Damian J, Pastor-Barriuso R, & Valderrama-Gama E (2008). Factors associated with self-rated health in older people living in institutions. BMC Geriatr, 8, 5. doi: 10.1186/1471-2318-8-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenholtz HB, Kane RA, Kane RL, Bershadsky B, & Kling KC (2006). Predicting Nursing Facility Residents' Quality of Life Using External Indicators. Health Services Research, 41(2), 335–356. doi: 10.1111/j.1475-6773.2005.00494.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E, Emmons R, Larsen R, & Griffin S (1985). The Satisfaction With Life Scale. Journal of Personality Assessment, 49, 71–75. doi: 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A (2005). Synthesising qualitative and quantitative evidence - a review of possible methods. Journal of Health Services Research & Policy, 10(1), 45–53. [DOI] [PubMed] [Google Scholar]
- Downes MJ, Brennan ML, Williams HC, & Dean RS (2016). Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downs SH, & Black N (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52, 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle CJ (1995). Effect of Staff Turnover and the Social Environment on Depressive Symptoms in Nursing Home Residents. International Psychogeriatrics, 7(1), 51–61. doi: 10.1017/S1041610295001840 [DOI] [PubMed] [Google Scholar]
- Drageset J, Eide G, Nygaard H, Bondevik M, Nortvedt M, & Natvig GK (2008). The impact of social support and sense of coherence on health-related quality of life among nursing home residents-A questionnaire survey in Bergen, Norway. International journal of nursing studies, 46, 65–75. doi: 10.1016/j.ijnurstu.2008.07.005 [DOI] [PubMed] [Google Scholar]
- Duncan JM, Killian TS, & Lucier-Greer M (2017). Leisure, relatedness, and ill-being among older adults in long-term care. Activities, Adaptation & Aging, 41, 273–290. doi: 10.1080/01924788.2017.1326764 [DOI] [Google Scholar]
- El Zoghbi M, Boulos C, Awada S, Rachidi S, Al-Hajje A, Bawab W, Saleh N, & Salameh P (2014). Prevalence of Malnutrition and Its Correlates in Older Adults Living in Long Stay Institutions Situated in Beirut, Lebanon. Journal of research in health sciences, 14, 11–17. [PubMed] [Google Scholar]
- Evans IEM, Llewellyn DJ, Matthews FE, Woods RT, Brayne C, Clare L, & CFAS-Wales research team. (2018). Social isolation, cognitive reserve, and cognition in healthy older people. PLoS One, 13(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehnel CR, Lee Y, Wendell LC, Thompson BB, Potter NS, & Mor V (2015). Post-Acute Care Data for Predicting Readmission After Ischemic Stroke: A Nationwide Cohort Analysis Using the Minimum Data Set. J Am Heart Assoc, 4(9), e002145. doi: 10.1161/JAHA.115.002145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Mayoralas G, Rojo-Pérez F, Martínez-Martín P, Prieto-Flores M, Rodríguez-Blázquez C, Martín-García S, Rojo-Abuín J, & Forjaz M (2015). Active ageing and quality of life: factors associated with participation in leisure activities among institutionalized older adults, with and without dementia. Aging & Mental Health, 19(11), 1031–1041. doi: 10.1080/13607863.2014.996734 [DOI] [PubMed] [Google Scholar]
- Foebel A, Ballokova A, Wellens NI, Fialova D, Milisen K, Liperoti R, & Hirdes JP (2015). A retrospective, longitudinal study of factors associated with new antipsychotic medication use among recently admitted long-term care residents. BMC Geriatr, 15, 128. doi: 10.1186/s12877-015-0127-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster JR, & Cataldo JK (1993). Prediction of first episode of clinical depression in patients newly admitted to a medical long-term care facility: Findings from a prospective study. International Journal of Geriatric Psychiatry, 8, 297–304. doi: 10.1002/gps.930080404 [DOI] [Google Scholar]
- Freeman S, Spirgiene L, Martin-Khan M, & Hirdes JP (2016). Relationship between restraint use, engagement in social activity, and decline in cognitive status among residents newly admitted to long-term care facilities. Geriatrics & Gerontology International, 17(2), 246–255. doi: 10.1111/ggi.12707 [DOI] [PubMed] [Google Scholar]
- Gagné M. (2003). The role of autonomy support and autonomy orientation in prosocial behavior engagement. Motivation and Emotion, 27, 199–223. doi: 10.1023/A:1025007614869 [DOI] [Google Scholar]
- Gerritsen DL, Steverink N, Frijters DHM, Hirdes JP, Ooms ME, & Ribbe MW (2008). A Revised Index for Social Engagement for Long-Term Care. Journal of Gerontological Nursing, 34(4), 40–48. doi: 10.3928/00989134-20080401-04 [DOI] [PubMed] [Google Scholar]
- Ghusn HF, Hyde D, Stevens ES, Hyde M, & Teasdale TA (1996). Enhancing Satisfaction in Later Life. Journal of Gerontological Social Work, 26(1-2), 27–47. doi: 10.1300/J083V26N01_03 [DOI] [Google Scholar]
- Grabowski DC, & Mitchell SL (2010). Family oversight and the quality of nursing home care for residents with advanced dementia. (1537-1948 (Electronic)). doi: 10.1097/MLR.0b013e318195fce7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guse LW, & Masesar MA (1999). Quality of life and successful aging in long-term care: perceptions of residents. Issues in Mental Health Nursing, 20(6), 527–539. doi: 10.1080/016128499248349 [DOI] [PubMed] [Google Scholar]
- Hamilton M. (1960). A RATING SCALE FOR DEPRESSION. Journal of Neurology, Neurosurgery & Psychiatry, 23(1), 56. doi: 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haugan G, Moksnes UK, & Løhre A (2016). Intrapersonal self-transcendence, meaning-in-life and nurse–patient interaction: powerful assets for quality of life in cognitively intact nursing-home patients. Scandinavian Journal of Caring Sciences, 30(4), 790–801. doi: 10.1111/scs.12307 [DOI] [PubMed] [Google Scholar]
- Herzog AR, Ofstedal MB, & Wheeler LM (2002). Social engagement and its relationship to health. Clin Geriatr Med. , 3(18), 593–609. [DOI] [PubMed] [Google Scholar]
- Hicks TJ (2000). What is your life like now? Loneliness and elderly individuals residing in nursing homes. J Gerontol Nurs, 26(8), 15–19. [DOI] [PubMed] [Google Scholar]
- Hjaltadóttir I, Ekwall AK, Nyberg P, & Hallberg IR (2012). Quality of care in Icelandic nursing homes measured with Minimum Data Set quality indicators: Retrospective analysis of nursing home data over 7 years. International Journal of Nursing Studies, 49(11), 1342–1353. doi: 10.1016/j.ijnurstu.2012.06.004 [DOI] [PubMed] [Google Scholar]
- Hjaltadottir I, Hallberg IR, Ekwall AK, & Nyberg P (2011). Predicting mortality of residents at admission to nursing home: a longitudinal cohort study. BMC Health Serv Res, 11, 86. doi: 10.1186/1472-6963-11-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollinger-Smith L, & Buschmann M (2000). Failure to Thrive Syndrome. Clinical Gerontologist, 20(4), 65–88. doi: 10.1300/J018v20n04_06 [DOI] [Google Scholar]
- Holt-Lunstad J, Smith TB, & Layton JB (2010). Social relationships and mortality risk: a meta-analytic review. PLoS Med, 7(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J. (2022, Apr 5). Social Connection as a Public Health Issue: The Evidence and a Systemic Framework for Prioritizing the "Social" in Social Determinants of Health. Annu Rev Public Health, 43, 193–213. 10.1146/annurev-publhealth-052020-110732 [DOI] [PubMed] [Google Scholar]
- Hsiao Y-C, & Chen C-Y (2018). Exploring Individual, Family, and Extrafamilial Factors Associated With Depression Among Elderly Residents of Care Settings. The International Journal of Aging and Human Development, 86(3), 219–241. doi: 10.1177/0091415017699938 [DOI] [PubMed] [Google Scholar]
- Hsu Y-C, & Wright CL (2014). The association between participation in social activity and depressive symptoms in institutionalized elders in Taiwan. Geriatric Nursing, 35(1), 31–36. doi: 10.1016/j.gerinurse.2013.09.004 [DOI] [PubMed] [Google Scholar]
- Inventor R, Farran J, Paun O, Cothran F, Rajan K, Swantek S, & McCann J (2018). Longitudinal Effects of Activities, Social Environment, and Psychotropic Medication Use on Behavioral Symptoms of Individuals With Alzheimer's Disease in Nursing Homes. Journal of Psychosocial Nursing and Mental Health Services, 56(11), 18–26. doi: 10.3928/02793695-20180503-04 [DOI] [PubMed] [Google Scholar]
- Jang Y, Park NS, Dominguez DD, & Molinari V (2014). Social engagement in older residents of assisted living facilities. Aging & Mental Health, 18(5), 642–647. doi: 10.1080/13607863.2013.866634 [DOI] [PubMed] [Google Scholar]
- Jao Y-L, Loken E, MacAndrew M, Van Haitsma K, & Kolanowski A (2018). Association between social interaction and affect in nursing home residents with dementia. Aging & Mental Health, 22(6), 778–783. doi: 10.1080/13607863.2017.1304526 [DOI] [PubMed] [Google Scholar]
- Jongenelis K, Gerritsen DL, Pot AM, Beekman ATF, Eisses AMH, Kluiter H, & Ribbe MW (2007). Construction and validation of a patient- and user-friendly nursing home version of the Geriatric Depression Scale. International Journal of Geriatric Psychiatry, 22(9), 837–842. doi: 10.1002/gps.1748 [DOI] [PubMed] [Google Scholar]
- Kaelen S, van den Boogaard W, Pellecchia U, Spiers S, De Cramer C, Demaegd G, … Draguez B (2021). How to bring residents’ psychosocial wellbeing to the heart of the fight against Covid19 in Belgian nursing homes—A qualitative study. PLOS ONE, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane RA (2001). Long-term care and a good quality of life: bringing them closer together. Gerontologist, 41(3), 293–304. [DOI] [PubMed] [Google Scholar]
- Kang H. (2012). Correlates of Social Engagement in Nursing Home Residents with Dementia. Asian Nursing Research, 6(2), 75–81. doi: 10.1016/j.anr.2012.05.006 [DOI] [PubMed] [Google Scholar]
- Kang B, Scales K, McConnell ES, Song Y, Lepore M, Corazzini K (2020, Apr). Nursing home residents' perspectives on their social relationships. J Clin Nurs, 29(7-8), 1162–1174. 10.1111/jocn.15174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasser VG, & Ryan RM (1999). The Relation of Psychological Needs for Autonomy and Relatedness to Vitality, Well-Being, and Mortality in a Nursing Home1. Journal of Applied Social Psychology, 29(5), 935–954. doi: 10.1111/j.1559-1816.1999.tb00133.x [DOI] [Google Scholar]
- Kehyayan V, Hirdes JP, Tyas SL, & Stolee P (2016). Predictors of Long-Term Care Facility Residents’ Self-Reported Quality of Life With Individual and Facility Characteristics in Canada. Journal of Aging and Health, 28(3), 503–529. doi: 10.1177/0898264315594138 [DOI] [PubMed] [Google Scholar]
- Keister KJ (2006). Predictors of self-assessed health, anxiety, and depressive symptoms in nursing home residents at week 1 postrelocation. J Aging Health, 18(5), 722–742. doi: 10.1177/0898264306293265 [DOI] [PubMed] [Google Scholar]
- Keller HH, Carrier N, Slaughter S, Lengyel C, Steele CM, Duizer L, … Villalon L (2017). Making the Most of Mealtimes (M3): protocol of a multi-centre cross-sectional study of food intake and its determinants in older adults living in long term care homes. BMC Geriatrics, 17(1), 15. doi: 10.1186/s12877-016-0401-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiely DK, & Flacker JM (2003). The protective effect of social engagement on 1-year mortality in a long-stay nursing home population. J Clin Epidemiol, 56(5), 472–478. doi: 10.1016/s0895-4356(03)00030-1 [DOI] [PubMed] [Google Scholar]
- Kiely DK, Simon SE, Jones RN, & Morris JN (2000). The protective effect of social engagement on mortality in long-term care. J Am Geriatr Soc, 48(11), 1367–1372. doi: 10.1111/j.1532-5415.2000.tb02624.x [DOI] [PubMed] [Google Scholar]
- Kloos N, Trompetter HR, Bohlmeijer ET, & Westerhof GJ (2019). Longitudinal Associations of Autonomy, Relatedness, and Competence With the Well-being of Nursing Home Residents. Gerontologist, 59(4), 635–643. doi: 10.1093/geront/gny005 [DOI] [PubMed] [Google Scholar]
- Kroemeke A, & Gruszczynska E (2016). Well-Being and Institutional Care in Older Adults: Cross-Sectional and Time Effects of Provided and Received Support. PLoS One, 11(8), e0161328. doi: 10.1371/journal.pone.0161328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok SYCL, Yeung DYL, & Chung A (2011). The Moderating Role of Perceived Social Support on the Relationship between Physical Functional Impairment and Depressive Symptoms among Chinese Nursing Home Elderly in Hong Kong. TheScientificWorldJOURNAL, 11, 469895. doi: 10.1100/tsw.2011.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapane KL, Dube CE, Jesdale BM, Bova C (2022). Social Connectedness among Long-Stay Nursing Home Residents with Alzheimer's and Dementia: Exploring Individual and Facility-Level Variation. Dement Geriatr Cogn Disord, 51(3), 249–261. 10.1159/000525343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapane KL, Lim E, McPhillips E, Barooah A, Yuan Y, & Dube CE (2022). Health effects of loneliness and social isolation in older adults living in congregate long term care settings: A systematic review of quantitative and qualitative evidence. Arch Gerontol Geriatr, 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee GE (2010). Predictors of adjustment to nursing home life of elderly residents: A cross-sectional survey. International Journal of Nursing Studies, 47(8), 957–964. doi: 10.1016/j.ijnurstu.2009.12.020 [DOI] [PubMed] [Google Scholar]
- Lee H, Park S, Kwon E, & Cho J (2017). Socioeconomic Disparity in Later-Year Group Trajectories of Depressive Symptoms: Role of Health and Social Engagement Change. Int J Environ Res Public Health, 14(6). doi: 10.3390/ijerph14060588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leedahl SN, Chapin RK, & Little TD (2015). Multilevel Examination of Facility Characteristics, Social Integration, and Health for Older Adults Living in Nursing Homes. The Journals of Gerontology: Series B, 70(1), 111–122. doi: 10.1093/geronb/gbu112 [DOI] [PubMed] [Google Scholar]
- Lem K, McGilton KS, & Aelick K (2021). Social connection and physical health outcomes among long-term care home residents: a scoping review. BMC Geriatr, 21. doi: 10.1186/s12877-021-02638-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leschak CJ, & Eisenberger NI (2019). Two Distinct Immune Pathways Linking Social Relationships With Health: Inflammatory and Antiviral Processes. Psychosom Med, 81(8), 711–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung KK, Wu EC, Lue BH, & Tang LY (2004). The use of focus groups in evaluating quality of life components among elderly Chinese people. Qual Life Res, 13(1), 179–190. doi: 10.1023/B:QURE.0000015291.79826.a8 [DOI] [PubMed] [Google Scholar]
- Li J, Chang YP, & Porock D (2015). Factors associated with daytime sleep in nursing home residents. Res Aging, 37(1), 103–117. doi: 10.1177/0164027514537081 [DOI] [PubMed] [Google Scholar]
- Lin P-C, Wang H-H, & Huang H-T (2006). Depressive symptoms among older residents at nursing homes in Taiwan. Journal of Clinical Nursing, 16(9), 1719–1725. doi: 10.1111/j.1365-2702.2007.01743.x [DOI] [PubMed] [Google Scholar]
- Liu Y, Xue L, Xue H, & Hou P (2018). Health literacy, self-care agency, health status and social support among elderly Chinese nursing home residents. Health Education Journal, 77(3), 303–311. doi: 10.1177/0017896917739777 [DOI] [Google Scholar]
- Lou VW, Chi I, Kwan CW, & Leung AY (2012). Trajectories of social engagement and depressive symptoms among long-term care facility residents in Hong Kong. Age Ageing, 42(2), 215–222. doi: 10.1093/ageing/afs159 [DOI] [PubMed] [Google Scholar]
- Luo T, Kuo L, & Tang Y (2012). The effectiveness of intermediate care for hip-fracture patients. J. Taiwan Geriatr. Gerontol, 7, 20–36. [Google Scholar]
- Maenhout A, Cornelis E, Van de Velde D, Desmet V, Gorus E, Van Malderen L, … De Vriendt P (2020). The relationship between quality of life in a nursing home and personal, organizational, activity-related factors and social satisfaction: a cross-sectional study with multiple linear regression analyses. Aging & Mental Health, 24(4), 649–658. doi: 10.1080/13607863.2019.1571014 [DOI] [PubMed] [Google Scholar]
- Mao X, & Han W (2018). Living Arrangements and Older Adults' Psychological Well-Being and Life Satisfaction in China: Does Social Support Matter? Family Relations, 67(4), 567–584. doi: 10.1111/fare.12326 [DOI] [Google Scholar]
- Martin JL, Webber AP, Alam T, Harker JO, Josephson KR, & Alessi CA (2006). Daytime sleeping, sleep disturbance, and circadian rhythms in the nursing home. Am J Geriatr Psychiatry, 14(2), 121–129. doi: 10.1097/01.JGP.0000192483.35555.a3 [DOI] [PubMed] [Google Scholar]
- Martino J, Pegg J, & Frates EP (2015). The Connection Prescription: Using the Power of Social Interactions and the Deep Desire for Connectedness to Empower Health and Wellness. Am J Lifestyle Med, 11(6), 466–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marventano S, Prieto-Flores M-E, Sanz-Barbero B, Martín-García S, Fernandez-Mayoralas G, Rojo-Perez F, … Forjaz MJ (2015). Quality of life in older people with dementia: A multilevel study of individual attributes and residential care center characteristics. Geriatrics & Gerontology International, 15(1), 104–110. doi: 10.1111/ggi.12238 [DOI] [PubMed] [Google Scholar]
- Maxwell CJ, Amuah JE, Hogan DB, Cepoiu-Martin M, Gruneir A, Patten SB, … Strain LA (2015). Elevated Hospitalization Risk of Assisted Living Residents With Dementia in Alberta, Canada. J Am Med Dir Assoc, 16(7), 568–577. doi: 10.1016/j.jamda.2015.01.079 [DOI] [PubMed] [Google Scholar]
- McCabe M, Byers J, Busija L, Mellor D, Bennett M, & Beattie E (2021). How Important Are Choice, Autonomy, and Relationships in Predicting the Quality of Life of Nursing Home Residents? Journal of Applied Gerontology, 40(12), 1743–1750. doi: 10.1177/0733464820983972 [DOI] [PubMed] [Google Scholar]
- McCabe MP, Beattie E, Karantzas G, Mellor D, Sanders K, Busija L, Goodenough B, Bennett M, Von Treuer K, & Byers J (2018). A randomized controlled trial to evaluate the effectiveness of a staff training program to implement consumer directed care on resident quality of life in residential aged care. BMC Geriatrics, 18(1), 287. doi: 10.1186/s12877-018-0966-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffree KM, & Harkins EB (1975). Final report for evaluation of the outcomes of nursing home care. Washington, DC: Health Care Study Center, Battelle Human Affairs Research Centers. [Google Scholar]
- Mitchell JM, & Kemp BJ (2000). Quality of Life in Assisted Living Homes: A Multidimensional Analysis. The Journals of Gerontology: Series B, 55(2), P117–P127. doi: 10.1093/geronb/55.2.P117 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, & PRISMA Group. (2009). Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. BMJ 21(339). [PMC free article] [PubMed] [Google Scholar]
- Mor V, Branco K, Fleishman J, Hawes C, Phillips C, Morris J, & Fries B (1995). The structure of social engagement among nursing home residents. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 50, P1–P8. doi: 10.1093/geronb/50B.1.P1 [DOI] [PubMed] [Google Scholar]
- Morris JN, Fries BE, Mehr DR, Hawes C, Phillips C, Mor V, & Lipsitz LA (1994). MDS Cognitive Performance Scale. Journal of Gerontology, 49, M174–M182. doi: 10.1093/geronj/49.4.M174 [DOI] [PubMed] [Google Scholar]
- Morris JN, Murphy K, & Nonemaker S (1995). Long Term Care Facility Resident Assessment Instrument (RAI) User’s Manual. Version 2.0. Health Care Financing Administration. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS20rai1202toc.pdf [Google Scholar]
- Morrison-Koechl J, Wu SA, Slaughter SE, Lengyel CO, Carrier N, & Keller HH (2021). Hungry for more: Low resident social engagement is indirectly associated with poor energy intake and mealtime experience in long-term care homes. Appetite, 159, 105044. doi: 10.1016/j.appet.2020.105044 [DOI] [PubMed] [Google Scholar]
- Moyle W, Fetherstonhaugh D, Greben M, Beattie E, & group A (2015). Influencers on quality of life as reported by people living with dementia in long-term care: a descriptive exploratory approach. BMC Geriatr, 15, 50. doi: 10.1186/s12877-015-0050-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyle W, Venturto L, Griffiths S, Grimbeek P, McAllister M, Oxlade D, & Murfield J (2011). Factors influencing quality of life for people with dementia: a qualitative perspective. Aging Ment Health, 15(8), 970–977. doi: 10.1080/13607863.2011.583620 [DOI] [PubMed] [Google Scholar]
- Naik P, U. V (2020). How Elderly Residents in Nursing Homes Handle Loneliness-From the Nurses' Perspective. SAGE Open Nurs, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neufeld E, Freeman S, Spirgiene L, & Horwath U (2019). A Cross-Sectoral Comparison of Prevalence and Predictors of Symptoms of Depression Over Time Among Older Adults in Ontario, Canada. J Geriatr Psychiatry Neurol, 34(1), 11–20. doi: 10.1177/0891988720901790 [DOI] [PubMed] [Google Scholar]
- Neufeld E, Hirdes JP, Perlman CM, & Rabinowitz T (2015). Risk and protective factors associated with intentional self-harm among older community-residing home care clients in Ontario, Canada. International Journal of Geriatric Psychiatry, 30(10), 1032–1040. doi: 10.1002/gps.4259 [DOI] [PubMed] [Google Scholar]
- Nie Y, Hu Z, Zhu T, & Xu H (2020). A Cross-Sectional Study of the Prevalence of and Risk Factors for Suicidal Ideation Among the Elderly in Nursing Homes in Hunan Province, China. Frontiers in Psychiatry, 11. Retrieved from https://www.frontiersin.org/articles/10.3389/fpsyt.2020.00339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onunkwor OF, Al-Dubai SAR, George PP, Arokiasamy J, Yadav H, Barua A, & Shuaibu HO (2016). A cross-sectional study on quality of life among the elderly in non-governmental organizations’ elderly homes in Kuala Lumpur. Health and Quality of Life Outcomes, 14(1), 6. doi: 10.1186/s12955-016-0408-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page MJ, Shamseer L, & Tricco AC (2018). Registration of systematic reviews in PROSPERO: 30,000 records and counting. Systematic Reviews, 7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palese A, Grassetti L, Zuttion R, Ferrario B, Ponta S, Achil I, … Watson R (2019). Self-feeding dependence incidence and predictors among nursing home residents: Findings from a 5 year retrospective regional study. Nurs Health Sci, 21(3), 297–306. doi: 10.1111/nhs.12596 [DOI] [PubMed] [Google Scholar]
- Papi S, Karimi Z, Amini Harooni GG, Nazarpour A, & Shahry P (2019). Determining the Prevalence of Sleep Disorder and Its Predictors Among Elderly Residents of Nursing Homes of Ahvaz City in 2017. Salmand, 576–587. doi: 10.32598/SIJA.13.Special-Issue.576 [DOI] [Google Scholar]
- Park C, Kim D, & Briesacher BA (2021). Association of Social Isolation of Long-term Care Facilities in the United States With 30-Day Mortality. JAMA Netw Open, 4(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park NS (2009). The Relationship of Social Engagement to Psychological Well-Being of Older Adults in Assisted Living Facilities. Journal of Applied Gerontology, 28(4), 461–481. doi: 10.1177/0733464808328606 [DOI] [Google Scholar]
- Park S, & Sok SR (2020). Relation Modeling of Factors Influencing Life Satisfaction and Adaptation of Korean Older Adults in Long-Term Care Facilities. International journal of environmental research and public health, 17(1). doi: 10.3390/ijerph17010317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascazio L, Morosini P, Bembich S, Nardone I, Clarici A, Barbina L, Zuttion R, & Gigantesco A (2009). Description and validation of a geriatric multidimensional graphical instrument for promoting longitudinal evaluation. Archives of Gerontology and Geriatrics, 48, 317–324. [DOI] [PubMed] [Google Scholar]
- Pastor-Barriuso R, Padrón-Monedero A, Parra-Ramírez L, García López F, & Damián J (2020). Social engagement within the facility increased life expectancy in nursing home residents: a follow-up study. BMC Geriatrics, 20(1), 480. doi: 10.1186/s12877-020-01876-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patra P, Alikari V, Fradelos EC, Sachlas A, Kourakos M, Rojas Gil AP, … Zyga S (2017, 2017). Assessment of Depression in Elderly. Is Perceived Social Support Related? A Nursing Home Study. Paper presented at the GeNeDis 2016, Cham. [DOI] [PubMed] [Google Scholar]
- Poon LW, Jazwinski M, Green RC, Woodard JL, Martin P, Rodgers WL, Johnson MA, Hausman D, Arnold J, Davey A, Batzer MA, Markesbery WR, Gearing M, Siegler IC, Reynolds S, & Dai J (2007). Methodological Considerations in Studying Centenarians: Lessons Learned From the Georgia Centenarian Studies. Annu Rev Gerontol Geriatr, 27(1), 231–264. [PMC free article] [PubMed] [Google Scholar]
- Potter R, Sheehan B, Cain R, Griffin J, & Jennings PA (2018). The Impact of the Physical Environment on Depressive Symptoms of Older Residents Living in Care Homes: A Mixed Methods Study. Gerontologist, 58(3), 438–447. doi: 10.1093/geront/gnx041 [DOI] [PubMed] [Google Scholar]
- Pramesona BA, & Taneepanichskul S (2018). Prevalence and risk factors of depression among Indonesian elderly: A nursing home-based cross-sectional study. Neurology, Psychiatry and Brain Research, 30, 22–27. doi: 10.1016/j.npbr.2018.04.004 [DOI] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Randall GK, Martin P, MacDonald M, Margrett J, Bishop AJ, & Poon LW (2011). Comparing the Support-Efficacy Model among Centenarians Living in Private Homes, Assisted Living Facilities, and Nursing Homes. Journal of Aging Research, 2011, 280727. doi: 10.4061/2011/280727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read S, Comas-Herrera A, & Grundy E (2020). Social Isolation and Memory Decline in Later-life. J Gerontol B Psychol Sci Soc Sci, 75(2), 367–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozzini R, Boffelli S, Franzoni S, Frisoni GB, & Trarucchi M (1996). Prevalence and predictors of depressive symptoms in a nursing home. International Journal of Geriatric Psychiatry, 11(7), 629–634. doi: [DOI] [Google Scholar]
- Saleh N, Penning M, Cloutier D, Mallidou A, Nuernberger K, & Taylor D (2017). Social Engagement and Antipsychotic Use in Addressing the Behavioral and Psychological Symptoms of Dementia in Long-Term Care Facilities. Canadian Journal of Nursing Research, 49(4), 144–152. doi: 10.1177/0844562117726253 [DOI] [PubMed] [Google Scholar]
- Sandelowski M, Voils C, Barroso J (2006). Defining and designing mixed research synthesis studies.pdf>. Res Sch., 13(1), 29. [PMC free article] [PubMed] [Google Scholar]
- Schulz U, & Schwarzer R (2003). Soziale Unterstützung bei der Krankheitsbewältigung: Die Berliner Social Support Skalen (BSSS). [Social Support in Coping with Illness: The Berlin Social Support Scales (BSSS).]. Diagnostica, 49, 73–82. doi: 10.1026/0012-1924.49.2.73 [DOI] [Google Scholar]
- Seeman TE, Lusignolo TM, Albert M, & Berkman L (2001). Social relationships, social support, and patterns of cognitive aging in healthy, high-functioning older adults: MacArthur studies of successful aging. Health Psychol, 20(4), 243–255. [DOI] [PubMed] [Google Scholar]
- Segal DL (2005). Relationships of Assertiveness, Depression, and Social Support Among Older Nursing Home Residents. Behavior Modification, 29(4), 689–695. doi: 10.1177/0145445503259391 [DOI] [PubMed] [Google Scholar]
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, & PRISMA-P Group. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ, 350, g7647. [DOI] [PubMed] [Google Scholar]
- Shankar A, Hamer M, McMunn A, & Steptoe A (2013). Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English Longitudinal Study of Ageing. Psychosom Med, 75(2), 161–170. [DOI] [PubMed] [Google Scholar]
- Sheehan D. (2015). M.I.N.I International Neuropsychiatric Interview (English Version 7.0.0 for DSM-V) [Measure]. [Google Scholar]
- Sheehan DV, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A, … Dunbar GC (1997). The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry, 12(5), 232–241. doi: 10.1016/S0924-9338(97)83297-X [DOI] [Google Scholar]
- Smit D, de Lange J, Willemse B, Twisk J, & Pot AM (2016). Activity involvement and quality of life of people at different stages of dementia in long term care facilities. Aging & Mental Health, 20(1), 100–109. doi: 10.1080/13607863.2015.1049116 [DOI] [PubMed] [Google Scholar]
- Social Connectedness: Evaluating the Healthy People 2020 Framework: The Minnesota Project,. (2010). Retrieved from https://www.health.state.mn.us/communities/practice/resources/publications/docs/1007socialconnectedness_report.pdf [Google Scholar]
- Social isolation, loneliness in older people pose health risks. (2019). Retrieved from https://www.nia.nih.gov/news/social-isolation-loneliness-older-people-pose-health-risks [Google Scholar]
- Street D, Burge S, Quadagno J, & Barrett A (2007). The Salience of Social Relationships for Resident Well-Being in Assisted Living. The Journals of Gerontology: Series B, 62(2), S129–S134. doi: 10.1093/geronb/62.2.S129 [DOI] [PubMed] [Google Scholar]
- Sun Y, Zhang D, Yang Y, Wu M, Xie H, Zhang J, … Su Y (2017). Social Support Moderates the Effects of Self-esteem and Depression on Quality of Life Among Chinese Rural Elderly in Nursing Homes. Archives of Psychiatric Nursing, 31(2), 197–204. doi: 10.1016/j.apnu.2016.09.015 [DOI] [PubMed] [Google Scholar]
- Tong A, & Craig J (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care, 19(1353-4505 (Print)), 349–357. [DOI] [PubMed] [Google Scholar]
- Tosangwarn S, Clissett P, & Blake H (2017). Predictors of depressive symptoms in older adults living in care homes in Thailand. Archives of Psychiatric Nursing, 32(1), 51–56. doi: 10.1016/j.apnu.2017.09.010 [DOI] [PubMed] [Google Scholar]
- Tseng SZ, & Wang RH (2001). Quality of Life and Related Factors among Elderly Nursing Home Residents in Southern Taiwan. Public Health Nursing, 18(5), 304–311. doi: 10.1046/j.1525-1446.2001.00304.x [DOI] [PubMed] [Google Scholar]
- Tu Y-Y, Lai Y-L, Shin S-C, Chang H-J, & Li L (2011). Factors Associated with Depressive Mood in the Elderly Residing at the Long-Term Care Facilities. International Journal of Gerontology, 6(1), 5–10. doi: 10.1016/j.ijge.2011.12.004 [DOI] [Google Scholar]
- Vanbeek APA, Frijters DHM, Wagner C, Groenewegen PP, & Ribbe MW (2011). Social engagement and depressive symptoms of elderly residents with dementia: a cross-sectional study of 37 long-term care units. International Psychogeriatrics, 23(4), 625–633. doi: 10.1017/S1041610210002061 [DOI] [PubMed] [Google Scholar]
- Veiga-Seijo R, Miranda-Duro MDC, Veiga-Seijo S (2022, Jan-Feb). Strategies and actions to enable meaningful family connections in nursing homes during the COVID-19: A Scoping Review. Clin Gerontol, 45(1), 20–30. 10.1080/07317115.2021.1937424 [DOI] [PubMed] [Google Scholar]
- Vetrano DL, Collamati A, Magnavita N, Sowa A, Topinkova E, Finne-Soveri H, … Poscia A (2018). Health determinants and survival in nursing home residents in Europe: Results from the SHELTER study. Maturitas, 107, 19–25. doi: 10.1016/j.maturitas.2017.09.014 [DOI] [PubMed] [Google Scholar]
- Wahyuni S, Shahdana S, & Armini NK (2019). The Relationship of Social Support with Older Adult Depression in Hargo Dedali Nursing Home, Surabaya. Indian Journal of Public Health Research & Development, 10 doi: 10.5958/0976-5506.2019.02258.7 [DOI] [Google Scholar]
- Wang N, Hailey D, Yu P (2011, Sep). Quality of nursing documentation and approaches to its evaluation: a mixed-method systematic review. J Adv Nurs, 67(9), 1858–1875. 10.1111/j.1365-2648.2011.05634.x [DOI] [PubMed] [Google Scholar]
- Wang J, Wang J, Cao Y, Jia S, & Wu B (2018). Perceived Empowerment, Social Support, and Quality of Life Among Chinese Older Residents in Long-Term Care Facilities. Journal of Aging and Health, 30(10), 1595–1619. doi: 10.1177/0898264318795724 [DOI] [PubMed] [Google Scholar]
- Wang YH, Liu LF, Chang LH, & Yeh CH (2019). The Implementation of Restorative Care and Factors Associated with Resident Outcomes in Long-Term Care Facilities in Taiwan. Int J Environ Res Public Health, 16(20). doi: 10.3390/ijerph16203860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. doi: 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Weiner DK, Peterson BL, Logue P, & Keefe FJ (1998). Predictors of pain self-report in nursing home residents. Aging Clinical and Experimental Research, 10(5), 411–420. doi: 10.1007/BF03339888 [DOI] [PubMed] [Google Scholar]
- Wiesmann U, Becker M-L, & Hannich H-J (2017). Positive aging in nursing home residents: A salutogenic analysis. GeroPsych: The Journal of Gerontopsychology and Geriatric Psychiatry, 30, 71–78. doi: 10.1024/1662-9647/a000166 [DOI] [Google Scholar]
- Willemse B, Smit D, De Lange J, & Pot AM, & 11 (11). (2011). Nursing home care for people with dementia and residents’quality of life, quality of care and staff well-being: Design of the Living Arrangements for people with Dementia (LAD) study. BMC Geriatrics, 11(11), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu M, Yang Y, Zhang D, Sun Y, Xie H, Zhang J, … Su Y (2017). Prevalence and related factors of successful aging among Chinese rural elders living in nursing homes. European Journal of Ageing, 14(4), 419–428. doi: 10.1007/s10433-017-0423-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu M, Yang Y, Zhang D, Zhao X, Sun Y, Xie H, … Li Y (2018). Association between social support and health-related quality of life among Chinese rural elders in nursing homes: the mediating role of resilience. Quality of Life Research, 27(3), 783–792. doi: 10.1007/s11136-017-1730-2 [DOI] [PubMed] [Google Scholar]
- Xiao Y, Watson M (2017). Guidance on Conducting a Systematic Literature Review. Journal of Planning Education and Research, 39(1), 93–112. 10.1177/0739456x17723971 [DOI] [Google Scholar]
- Xu D, Mou H, Gao J, Zhu S, Wang X, Ling J, & Wang K (2019). Quality of life of nursing home residents in mainland China: The role of children and family support. Archives of Gerontology and Geriatrics, 83, 303–308. doi: 10.1016/j.archger.2019.04.009 [DOI] [PubMed] [Google Scholar]
- Yamada Y, Denkinger MD, Onder G, Henrard JC, van der Roest HG, Finne-Soveri H, … Topinkova E (2016). Dual Sensory Impairment and Cognitive Decline: The Results From the Shelter Study. J Gerontol A Biol Sci Med Sci, 71(1), 117–123. doi: 10.1093/gerona/glv036 [DOI] [PubMed] [Google Scholar]
- Yeh CL (1999). Relationship between Social Support and Physical Health, Depression in Self-Paid Care Homes. Master’s Thesis, Degree-Chung Shan Medical University, Taichung, China. [Google Scholar]
- Yeh K-P, Lin M-H, Liu L-K, Chen L-Y, Peng L-N, & Chen L-K (2014). Functional decline and mortality in long-term care settings: Static and dynamic approach. Journal of Clinical Gerontology and Geriatrics, 5(1), 13–17. doi: 10.1016/j.jcgg.2013.08.001 [DOI] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, & Leirer VO (1982). Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research, 17(1), 37–49. doi: 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- Yeung DY, Kwok SYC, & Chung A (2012). Institutional peer support mediates the impact of physical declines on depressive symptoms of nursing home residents. Journal of Advanced Nursing, 69(4), 875–885. doi: 10.1111/j.1365-2648.2012.06076.x [DOI] [PubMed] [Google Scholar]
- Yoon JY, Kim H, Jung YI, Ha JH (2016, Dec). Impact of the nursing home scale on residents' social engagement in South Korea. Int Psychogeriatr, 28(12), 1965–1973. 10.1017/S1041610216001198 [DOI] [PubMed] [Google Scholar]
- Ysseldyk R, Haslam Sa Fau - Haslam C, & Haslam C (2013). Abide with me: religious group identification among older adults promotes health and well-being by maintaining multiple group memberships. Aging Ment Health(1364-6915 (Electronic)). doi: 10.1080/13607863.2013.799120 [DOI] [PubMed] [Google Scholar]
- Zagic D, Wuthrich VM, Rapee RM, & Wolters N (2022). Interventions to improve social connections: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol, 57(5), 885–906. [DOI] [PubMed] [Google Scholar]
- Zhang D, Yang Y, Wu M, Zhao X, Sun Y, Xie H, … Su Y (2018). The moderating effect of social support on the relationship between physical health and suicidal thoughts among Chinese rural elderly: A nursing home sample. International Journal of Mental Health Nursing, 27(5), 1371–1382. doi: 10.1111/inm.12436 [DOI] [PubMed] [Google Scholar]
- Zhu X, Hu Z, Nie Y, Zhu T, Chiwanda Kaminga A, Yu Y, & Xu H (2020). The prevalence of poor sleep quality and associated risk factors among Chinese elderly adults in nursing homes: A cross-sectional study. PLoS One, 15(5), e0232834. doi: 10.1371/journal.pone.0232834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment, 52, 30–41. doi: 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, & Berkoff KA (1990). Psychometric Characteristics of the Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment, 55(3-4), 610–617. doi: 10.1080/00223891.1990.9674095 [DOI] [PubMed] [Google Scholar]
- Zurakowski TL (2000). The Social Environment of Nursing Homes and the Health of Older Residents. Holistic Nursing Practice, 14(4). Retrieved from https://journals.lww.com/hnpjournal/Fulltext/2000/07000/The_Social_Environment_of_Nursing_Homes_and_the.5.aspx [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.