Abstract
Background:
Selectively prioritizing some emotion regulation (ER) strategies over others has been shown to predict well-being; however, it is unclear what mechanisms underlie this process. Impulsivity, which captures both top-down control of and bottom-up reactivity to emotions, is one potential mechanism of interest.
Methods:
Using multilevel mediation modeling, we investigated whether lower ER strategy prioritization (i.e., lower between-strategy variability) mediates the relationship between greater momentary impulsivity and lower ER success in 82 individuals with remitted depression or no history of a mental disorder (1558 observations). To determine the specific effect of impulsivity, we covaried for mean regulatory effort and negative affect.
Results:
The indirect effect of impulsivity on ER success was significant at the within-person, but not between-person, level. Specifically, in moments when individuals endorsed more impulsivity than usual, they showed less ER strategy prioritization than usual, which predicted less successful ER. Individuals who, on average, reported more impulsivity indicated lower ER strategy prioritization, but no difference in ER success.
Conclusion:
ER strategy prioritization mediated the within-person relationship between greater impulsivity and lower ER success. Interventions focused on training individuals to selectively prioritize ER strategies may improve ER success, particularly when individuals are feeling more impulsive than usual.
Keywords: emotion regulation, impulsivity, multilevel modeling, ecological momentary assessment, depression
Emotion regulation (ER) refers to a process in which individuals attempt to influence their affective state. ER has been thought to encompass three stages: (1) the identification stage, in which individuals identify their emotions and decide whether to regulate them; (2) the selection stage, in which individuals select which ER strategies to use; and (3) the implementation stage, in which individuals determine how to implement the selected strategies (Gross, 2015). Particularly, in the selection stage, individuals must decide whether to selectively prioritize using some ER strategies over others. The degree to which individuals selectively prioritize some strategies over others has been operationalized as between-strategy variability (measured as the standard deviation across ER strategies; Double et al., 2022). Specifically, higher between-strategy variability has been thought to indicate that an individual is prioritizing use of one, or a few, ER strategies to a greater extent than other ER strategies (Blanke et al., 2020; Double et al., 2022). On the contrary, lower-between strategy variability has been suggested to indicate that an individual is not selectively prioritizing using some ER strategies to a greater degree than others, but is instead using all ER strategies to a similar degree (Blanke et al., 2020; Double et al., 2022). For example, an individual who reports using one, or several, ER strategies to a much greater degree than all other ER strategies would demonstrate high between-strategy variability (i.e., high standard deviation across ER strategies), and thus high ER strategy prioritization. On the other hand, an individual who reports not using any ER strategies, or using all ER strategies to a similar degree, would demonstrate low between-strategy variability (i.e., low standard deviation across ER strategies), and thus low ER strategy prioritization. In summary, the more that an individual varies their ER strategy use by using one, or a few, ER strategies to a greater extent than others, the more that individual displays higher ER strategy prioritization at any given observation.
Measuring variation in ER strategy use, such as with between-strategy ER variability, contrasts with traditional approaches to examining emotion regulation, which focus on average levels of ER strategy use. Traditionally, the literature on emotion regulation has conceptualized particular ER strategies as either adaptive or maladaptive. However, more recently, there has been a shift towards focusing on variability in ER strategy use, as recent studies have begun to suggest that whether an ER strategy is adaptive or maladaptive may depend on how effectively its use is varied in accordance with situational demands, rather than the inherent nature of the strategy itself (Aldao, 2013; Aldao et al., 2015; Gross, 2015). For instance, reappraisal, which has traditionally been considered an adaptive ER strategy, can either be helpful (e.g., when an individual cannot control the source of their stress and can only regulate their emotions) or unhelpful (e.g., when an individual can control not only their emotions, but also the source of their stress through problem-solving), depending on the context in which it is used (Ford & Troy, 2019; Haines et al., 2016; Troy et al., 2013). Similarly, rumination, which has often been thought of as a maladaptive ER strategy, has been shown to have adaptive qualities as well, such as its potential to contribute to effective problem-solving (Arditte & Joormann, 2011; Joormann et al., 2006).
Recent work has found that greater ER strategy prioritization (i.e., greater between-strategy variability) predicts positive outcomes, such as more successful regulation and greater affective well-being (Blanke et al., 2020; Wang et al., 2021; Wenzel et al., 2021a; Wenzel et al., 2021b). Due to limitations on how frequently ER can be sampled in everyday life (further elaborated on in the Discussion; Ebner-Priemer & Trull, 2009), we observe individual’s overall use of emotion regulation strategies over approximately 30-minute windows. During these 30-minute windows, greater ER strategy prioritization might be advantageous, in that it may indicate that an individual is selectively choosing which ER strategies to use to a greater degree than other ER strategies, and persisting in their use of the selected strategies throughout the entire 30minute period to meet contextual demands (Aldao et al., 2015). On the contrary, lower ER strategy prioritization might be disadvantageous, in that it may indicate that an individual is not carefully determining which ER strategies to prioritize. Instead, an individual showing low ER strategy prioritization might quickly switch between (rather than persist in their use of) certain ER strategies throughout the 30-minute period. For example, an individual may use reappraisal for the first 2 minutes, but then ruminate for the next 2 minutes, and then use distraction for the 2 minutes after that. Such an individual might end up using many ER strategies to a similar extent throughout the entire 30 minutes, but no single strategy long enough to lead to successful regulation. Thus, such an individual might show little variation in the overall degree to which they use different ER strategies relative to one another across the entire 30-minute period, and thus show low ER strategy prioritization.
Despite the beneficial outcomes associated with greater strategy prioritization, it remains unclear what mechanisms contribute to strategy prioritization in daily life. Thus far, one study has found support that emotional intelligence may contribute to strategy prioritization (Double et al., 2022), and two studies have suggested that self-control may also be implicated in strategy prioritization (Wenzel et al., 2021a; Wenzel et al., 2021b). In contrast with emotional intelligence and self-control, here we aim to investigate whether impulsivity might interfere with strategy prioritization.
Whereas self-control encompasses top-down aspects of self-regulation such as response inhibition, impulsivity has been theorized to reflect the interaction of top-down processes (e.g., response inhibition) with bottom-up processes (e.g., delay discounting; Nigg, 2017). In other words, when individuals act impulsively, they are not only acting in an uninhibited way, but also weighting immediate rewards more highly than delayed rewards. Deficits in inhibition (Joormann & Vanderlind, 2014) and greater delay discounting (i.e., greater weighting of immediate rewards over delayed rewards; Malesza, 2021) both have been associated with difficulties with effective ER and with depression. Thus, examining impulsivity, which encompasses aspects of both response inhibition and delay discounting, may be particularly relevant to understanding what contributes to (or interferes with) ER strategy prioritization, and thus ultimately impacts successful ER. Specifically, impulsivity could prevent individuals from thoughtfully selecting a strategy to regulate their emotions based on contextual demands, and instead lead them to regulate their emotions in whatever way is easiest and requires the least cognitive effort. It is also possible that impulsivity could lead individuals to switch from one ER strategy to another, without persisting in using a single strategy long enough to effectively regulate their emotions.
Though impulsivity has typically been measured at the trait level, prior work has demonstrated that behavioral manifestations of impulsivity vary within individuals across time (Tomko et al., 2014). These within-person fluctuations in impulsive behavior may indicate important information about an individual’s momentary cognitive capacity, and thus could be relevant to understanding ER processes, which also fluctuate across the day.
Recent research on ER strategy prioritization primarily has involved non-clinical samples consisting of undergraduate students (Blanke et al., 2020; Wang et al., 2021; Wenzel et al., 2021a; Wenzel et al., 2021b). However, one prior study found that individuals who showed lower ER strategy prioritization reported greater depressive symptoms (Wang et al., 2021), suggesting that clinical characteristics, such as a history of depression, might influence the degree to which individuals selectively prioritize some ER strategies over others. For example, individuals with a history of depression tend to differ in their spontaneous use of ER strategies (Ehring et al., 2010; Liu & Thompson, 2017), and tend to experience less successful ER (Joormann et al., 2007), than healthy individuals. Yet, it is not known whether individuals with a history of depression differ in ER strategy prioritization compared to healthy individuals.
In the present study, we examined evidence from a clinical sample, which included individuals with remitted depression and healthy comparison participants. Examining individuals who have remitted from depression, and are not currently depressed, allows us to specifically investigate state-independent mechanisms of depression that may contribute to risk for recurrence. For example, if individuals with remitted depression show less ER strategy prioritization than healthy individuals, this could suggest that lower ER strategy prioritization may be a trait-like vulnerability factor (or psychological scar) of depression. Utilizing a clinical sample including both individuals with remitted depression and healthy volunteers thus serves as an important extension to existing ER literature, which has largely focused on non-clinical samples, by elucidating how mechanisms of depression may relate to alterations in ER in daily life.
Given that research on ER strategy prioritization is still fairly nascent (Blanke et al., 2020; Double et al., 2022; Wang et al., 2021; Wenzel et al., 2021a; Wenzel et al., 2021b), it also remains unclear how this process unfolds over time. Prior work has suggested that, when an individual shows greater ER strategy prioritization, they may simply be successfully selecting and implementing certain ER strategies off the bat, such that using other ER strategies is not necessitated (Blanke et al., 2020). To test this hypothesis, we examined whether the particular types of ER strategies used predicted strategy prioritization. If particular types of ER strategies that have previously shown to contribute to successful ER (e.g., reappraisal: Lennarz et al., 2019) predict greater strategy prioritization, this could indicate that the relationship between strategy prioritization and ER success may be a reciprocal process (Blanke et al., 2022; Colombo et al., 2021). Specifically, successful ER may allow for greater strategy prioritization, which then may further facilitate ER success. Examining whether the particular types of ER strategies used impact strategy prioritization is an important first step in understanding how strategies are being used when certain strategies are being prioritized over others. This also serves as an important step in integrating existing literature on average levels of ER strategy use, with more recent literature on variability in strategy use.
Here, we examined strategy prioritization with respect to six ER strategies in daily life (i.e., acceptance, decentering, distraction, mind-wandering, reappraisal, and rumination). These six ER strategies map onto different stages of the process model of ER (e.g., attentional deployment: distraction, mind-wandering, and rumination; cognitive change: reappraisal; response modulation: acceptance and decentering; Gross, 2015) and thus each capture unique information about ER strategy use. The present study first investigated whether, at the between-person level, people who tended to endorse more impulsivity showed lower ER strategy prioritization, and thus lower ER success, to better understand what interventions would be most useful for helping people who need it most (Fisher et al., 2018). Then, we investigated whether, at the within-person level, when individuals tended to endorse more impulsivity compared to usual, they showed lower ER strategy prioritization than usual, and thus lower ER success, to elucidate what interventions would be most useful for helping in moments when it is needed most (Fisher et al., 2018).
Next, we examined, at the between-person level, whether individuals with remitted depression tended to show lower strategy prioritization than healthy individuals. We also explored whether depression history moderated relationships between examined variables (i.e., momentary impulsivity, ER strategy prioritization, ER success). Lastly, we determined, at both the between-person and within-person levels, how the types of emotion regulation strategies used impacted strategy prioritization, to help clarify which ER strategies are used when some ER strategies are prioritized to a greater degree than others. We hypothesized that, at both the between-person and within-person levels, putatively adaptive ER strategies (e.g., reappraisal; Lennarz et al., 2019; Wylie et al., 2023) would result in greater strategy prioritization, whereas putatively maladaptive ER strategies (e.g., rumination; Lennarz et al., 2019; Wylie et al., 2023) would result in lower strategy prioritization. Despite our hypotheses, these analyses were partly exploratory in nature, given the dearth of existing literature in this area.
Method
Participants and Procedure
The University of Illinois at Chicago (UIC) and University of Southern California (USC) Institutional Review Boards approved this study. Participants were recruited via online advertisements and university mailing lists and provided written informed consent. The sample consisted of 44 individuals with remitted depression and 38 healthy comparisons, who were all between the ages of 18 and 30 years old. Individuals with remitted depression were considered eligible for the study if they: (1) met criteria for lifetime major depressive disorder (MDD; American Psychiatric Association, 2013), (2) had remitted from a depressive episode for at least 2 months, and (3) scored lower than 8 on the 17-item Hamilton Depression Rating Scale (HDRS-17; Hamilton, 1960). Healthy individuals were considered eligible for the study if they: (1) did not meet criteria for lifetime history of any psychiatric disorders, and (2) scored lower than 8 on the HDRS-17. Diagnostic history was determined using the Diagnostic Interview for Genetic Studies (DIGS; Nurnberger et al., 1994), which was administered by a trained research coordinator or graduate student, along with the HDRS-17.
Once participants provided consent to participate in the study, we trained participants on the ecological momentary assessment (EMA) portion of our study, to ensure that participants understood the meaning of each of the EMA items in our study. For EMA, we sent participants six surveys each day, over the course of a week. Surveys were sent in pairs, with a “pre” and “post” survey, once in the morning, afternoon, and evening. Each “post” survey was sent 30 minutes after its respective “pre” survey was completed. Participants chose to either receive surveys via email or text, from either 8:00am to 7:00pm or from 10:00am to 9:00pm each day. Participants were given an hour to complete each survey, and reminders were sent every 20 minutes over the course of the hour until each survey was completed. The present study consisted of secondary analyses of existing data and utilized measures of negative affect collected at each “pre” survey and measures of ER strategy use, momentary impulsivity, and ER success collected at each “post” survey. On average, participants completed 19 out of the total 21 pre-post survey pairs (90.48% completion rate). The final sample included 82 participants with a total of 1558 pre-post survey pairs used in all analyses, with data collected from 2018 to 2022. More detailed information about the sample’s demographic and clinical characteristics can be found in Table 1.
Table 1.
Demographic and clinical characteristics of the sample
| Healthy Volunteers (N=38) | Individuals with Remitted MDD (N=44) | |
|---|---|---|
| Age, mean (SD) | 25.48 (3.95) | 26.88 (3.72) |
| Female (%) | 63.16 | 65.91 |
| Race | ||
| White (%) | 31.58 | 52.27 |
| Black (%) | 13.16 | 15.91 |
| Latinx (%) | 10.53 | 11.36 |
| Asian (%) | 31.58a | 11.36b |
| Multiracial (%) | 13.16 | 6.82 |
| Other (%) | 0.00 | 2.27 |
| Education Level | 7.75 | 7.95 |
| Strategy Prioritization, mean (SD) | 2.23 (.74) | 1.98 (.61) |
| Momentary Impulsivity, mean (SD) | 1.79 (.91) | 1.95 (.80) |
| Regulatory Success, mean (SD) | 7.51 (1.89)a | 6.24 (1.72)b |
| Average Negative Affect, mean (SD) | 1.99 (0.96)a | 2.56 (0.96)b |
| Average Regulatory Effort, mean (SD) | 4.45 (1.03) | 4.18 (1.09) |
| Acceptance, mean (SD) | 5.04 (1.84) | 4.71 (1.78) |
| Brooding, mean (SD) | 2.11 (1.21) | 2.32 (1.20) |
| Decentering, mean (SD) | 6.05 (2.31)a | 4.58 (1.77)b |
| Distraction, mean (SD) | 3.78 (1.95) | 3.78 (1.57) |
| Mind-Wandering, mean (SD) | 2.94 (1.53)a | 3.81 (1.63)b |
| Reappraisal, mean (SD) | 5.27 (1.84) | 4.59 (1.57) |
Abbreviations: MDD, major depressive disorder; SD, standard deviation.
Note: For education level, a score of 7 is equivalent to an Associate’s degree and a score of 8 is equivalent to a Bachelor’s degree.
Different superscripts within rows indicate significant pairwise comparisons between groups (p<.05).
Measures
Emotion Regulation Strategies (Level 1)
ER strategy use was assessed using items from the Spontaneous Affect Regulation Scale (SARS; Egloff et al., 2006; Gruber et al., 2012; Stange et al., 2017). In each “post” survey, participants reported their use of acceptance (2 items; ωbetween = .89, ωwithin = .64), decentering (2 items; ωbetween = .97, ωwithin = .70), distraction (2 items; ωbetween = .80, ωwithin = .43), mind-wandering (3 items; ωbetween = .90, ωwithin = .63), reappraisal (3 items; ωbetween = .90, ωwithin = .69), and rumination (3 items; ωbetween = .89, ωwithin = .68) since the “pre” survey about 30 minutes ago (Geldhof et al., 2014; Hayes & Coutts, 2020). The specific EMA items used to assess each ER strategy are included in the Supplementary Methods. Participants were told to rate their use of each strategy on a scale of 1 (not at all) to 10 (very much). To create a subscale score for each of the six ER strategies, we averaged the item responses for each ER strategy in each “post” survey.
For acceptance, decentering, distraction, and reappraisal, participants were asked to rate their use of each strategy specifically in response to any negative thoughts or feelings. Participants could respond with a “not applicable” option, if they had not experienced any negative thoughts or feelings to regulate. The “not applicable” option was added to avoid ambiguity in low ratings, so that low ratings would represent when ER strategies were not used in the presence of negative thoughts or feelings (rather than when ER strategies were not used due to the absence of negative thoughts or feelings). We did not provide a “not applicable” option for mind-wandering or rumination, given that these ER strategies were assessed more broadly and not just in response to negative thoughts or feelings. “Not applicable” responses were considered missing data. Of the 1558 survey pairs, the number of “post” surveys that were missing data on each respective ER strategy was as follows: 999 (64.12%) for acceptance, 1004 (64.44%) for decentering, 1107 (71.05%) for distraction, 19 (1.22%) for mind-wandering, 1054 (67.65%) for reappraisal, and 17 (1.09%) for rumination.
Emotion Regulation Strategy Prioritization (Level 1)
Emotion regulation strategy prioritization was operationalized as between-strategy variability. We computed between-strategy variability by calculating the standard deviation of the six ER strategy subscale scores in each “post” survey, which is consistent with prior work (Bahlinger et al., 2022; Battaglini et al., 2022; Blanke et al., 2020; Double et al., 2022; Wang et al., 2021). As a sensitivity analysis, we included mean regulatory effort (measured at Level 1 as the mean of the six ER strategy subscale scores in each “post” survey) as a covariate in several analyses, to capture variability in ER strategy use above and beyond what could be attributed to mean ER strategy use. This was consistent with the approach taken in with prior work (Blanke et al., 2020; Ebner-Priemer et al., 2009; Koval et al., 2013).
Emotion Regulation Success (Level 1)
Perceived ER success was assessed at each “post” survey, with the item “I was successful at regulating my emotions” from the SARS (Egloff et al., 2006; Gruber et al., 2012). This item specifically was asked with respect to the period since the “pre” survey about 30 minutes ago. Responses were rated on a scale of 1 (not at all) to 10 (very much), with a “not applicable” option, to be chosen if participants had not engaged in emotion regulation since the “pre” survey. Of the 1558 survey pairs, 860 (55.20%) “post” surveys were missing data on emotion regulation success.
Momentary Impulsivity (Level 1)
Momentary impulsivity was assessed using four items from the Momentary Impulsivity Scale (MIS; Tomko et al., 2014). These items were: (1) I said things without thinking, (2) I spent more money than I meant to, (3) I have felt impatient, and (4) I made a “spur of the moment” decision (ωbetween = .86, ωwithin = .48; Geldhof et al., 2014; Hayes & Coutts, 2020). Participants rated these items on a scale of 1 (not at all) to 10 (very much). Mean momentary impulsivity was computed by averaging across all four item responses at each observation. These items were asked in each “post” survey, with respect to the period since the last “post” survey around four hours ago. Of the 1558 survey pairs, 34 (2.18%) “post” surveys were missing data on impulsivity.
Negative Affect (Level 1)
Current negative affect (NA) was assessed in each “pre” survey using five items from a modified, brief version of the Positive and Negative Affect Scale (PANAS; ωbetween = .93, ωwithin = .82; Mackinnon et al., 1999; Watson et al., 1988). Participants rated these items on a scale of 1 (not at all) to 10 (very much) based on how they were feeling immediately prior to receiving the survey. Of the 1558 survey pairs, no “pre” surveys were missing data on any of the five NA items. Mean NA was computed by averaging all five items for each survey observation. As a sensitivity analysis, we included mean NA at Level 1 as a covariate in the mediation analysis, to capture how impulsivity impacted ER strategy prioritization and ER success above and beyond what could be attributed to affective distress.
Statistical Analyses
All analyses were conducted using R version 4.1.1. Independent samples t-tests were used to compare healthy individuals to individuals with remitted MDD on demographic and clinical characteristics. With 1558 observations nested within 82 participants, we performed a series of multilevel models using the lme function in the nlme package in R (Pinheiro et al., 2017) with a restricted maximum likelihood method of estimation (REML). First, we fitted a level 1–1-1 mediation model predicting ER success with momentary impulsivity as a predictor and between-strategy variability as a mediator. As a sensitivity analysis, we also fit this level 1–1-1 mediation model including mean regulatory effort and mean negative affect as Level 1 covariates. Second, we fitted a multilevel model predicting between-strategy variability (Level 1 outcome variable), using depression history (Level 2 predictor). As a sensitivity analysis, we also fit this multilevel modeling including mean regulatory effort as a Level 1 covariate. As an exploratory analysis, we also fitted a multilevel model determining whether depression history (Level 2 predictor) moderated paths tested in the 1–1-1 mediation model, such as associations between (1) momentary impulsivity (Level 1 predictor) and ER strategy prioritization (Level 1 outcome variable), (2) momentary impulsivity (Level 1 predictor) and regulatory success (Level 1 outcome variable) covarying for ER strategy prioritization (Level 1 covariate), and (3) ER strategy prioritization (Level 1 predictor) and regulatory success (Level 1 outcome variable) covarying for momentary impulsivity (Level 1 covariate). Lastly, we fitted a multilevel model predicting ER strategy prioritization (Level 1 outcome variable), using each distinct ER strategy (e.g., acceptance, decentering, distraction, mind-wandering, reappraisal, and rumination) separately as a predictor (Level 1 predictors). In this multilevel model, we did not include mean regulatory effort as a covariate, given that mean regulatory effort was calculated by taking the mean of acceptance, decentering, distraction, mind-wandering, reappraisal, and rumination in each “post” survey at Level 1.
To disentangle between-person and within-person effects, the mean of each Level 1 predictor was included in all models. We also specified random slopes for each model, to account for individual differences in effects of each Level 1 predictor (Snijders & Bosker, 2011). Given unequal time intervals between surveys, we specified a continuous autoregressive error structure (Snijders & Bosker, 2011). Accounting for the multilevel data structure, we imputed missing data for each item using the predictive mean matching algorithm in the mice package in R (Eekhout et al., 2014; Enders, 2017; Gottschall et al., 2012; Van Buuren & Groothuis-Oudshoorn, 2011). We generated 100 imputed datasets and reported findings from multilevel models based on pooled analyses of these datasets. We used multiple imputation to account for missing data, given that using complete case analysis can bias findings if the complete cases are not representative of the entire sample (Pedersen et al., 2017). Using multiple imputation allowed us to utilize all available information in the dataset to account for missing data and preserve relationships between variables (Pedersen et al., 2017).
We reported all coefficient estimates, 95% confidence intervals (CIs), and effect sizes (marginal R2) of the multilevel models. Coefficient estimates were interpreted to be significant if the probability was below an alpha value of .05. The 95% CI of the indirect effect in the multilevel mediation model was determined using Monte Carlo simulation, with 20000 simulations, which has been shown to not only perform as well as other methods (e.g., bootstrap), but also be less computationally intensive (Preacher & Selig, 2012; Selig & Preacher, 2008; Tofighi & MacKinnon, 2016).
Transparency and Openness
This was the largest available sample size. We performed no manipulations to the data, other than those described in the analysis section. We follow the Journal Article Reporting Standards (JARS; Kazak, 2018). Materials and analysis code for this study are available upon request. This was a secondary analysis of data from a study whose design and analysis were not pre-registered.
Results
Descriptive Statistics
We reported descriptive statistics of the sample’s demographic and clinical characteristics in Table 1. Compared to healthy individuals, individuals with remitted MDD, on average, showed lower average regulatory success, greater average negative affect, lower average use of decentering, and greater average use of mind-wandering (Table 1). The percentage of Asians included in the sample of healthy volunteers was also significantly higher than the percentage of Asians included in the sample of individuals with remitted depression (Table 1). Otherwise, the groups did not differ on demographic and clinical characteristics (Table 1). We also reported correlations between Level 2 ecological momentary assessment measures in Supplementary Table S1. We found that greater ER strategy prioritization at Level 2 was related to greater average regulatory effort; lower average negative affect; greater regulatory success; lower momentary impulsivity; and greater use of acceptance, decentering, and reappraisal at Level 2 (Supplementary Table S1).
Intraclass correlations ranged across imputed datasets, indicating that variability at the person-level accounted for at least 38% and up to 68% of the total variability in ER strategy prioritization, and at least 34% and up to 35% of the total variability in regulatory success, thus justifying the use of a multilevel modeling approach in subsequent analyses.
Level 2 Mediation Findings
At the between-person level, do people who tend to report more impulsivity on average show lower strategy prioritization, and in turn, lower success with emotion regulation?
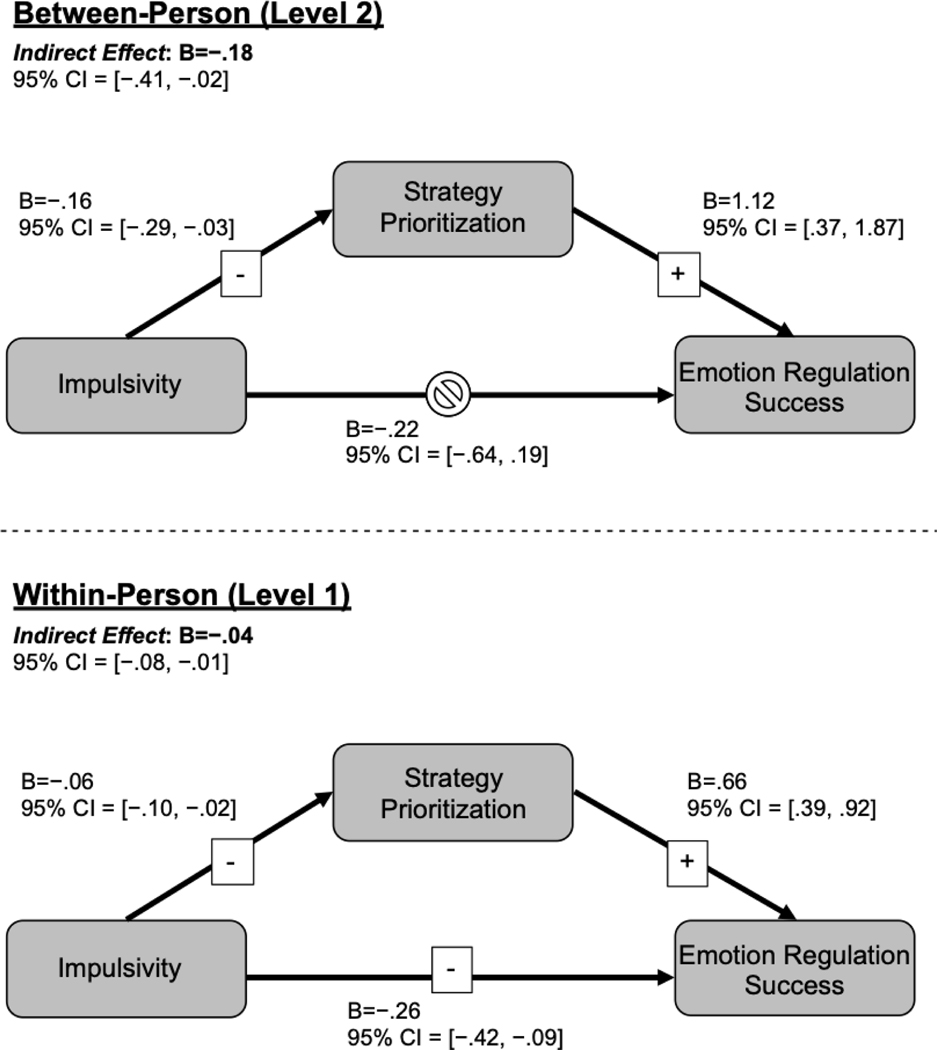
The indirect effect of impulsivity on ER success was significant at the between-person level (B=−.18, 95% CI = [−.41, −.02]; Figure 1). Specifically, individuals who, on average, endorsed more impulsivity showed lower ER strategy prioritization (B=−.16, SE=.07, 95% CI = [−.29, −.03], p<.02; Supplementary Table S2, Figure 1). Further, individuals who showed lower ER strategy prioritization, on average, showed lower ER success (B=1.12, SE=.38, 95% CI = [.37, 1.87], p<.004; Supplementary Table S2, Figure 1). The direct effect of impulsivity on ER success was not significant at the between-person level, suggesting that ER strategy prioritization fully mediated the relationship between impulsivity and regulatory success at Level 2. Specifically, individuals who, on average, reported more impulsivity showed no difference in ER success (p=.292; Supplementary Table S2, Figure 1), after covarying ER strategy prioritization.
Figure 1. Multilevel mediation model.
Abbreviations: 95% CI, 95% confidence interval.
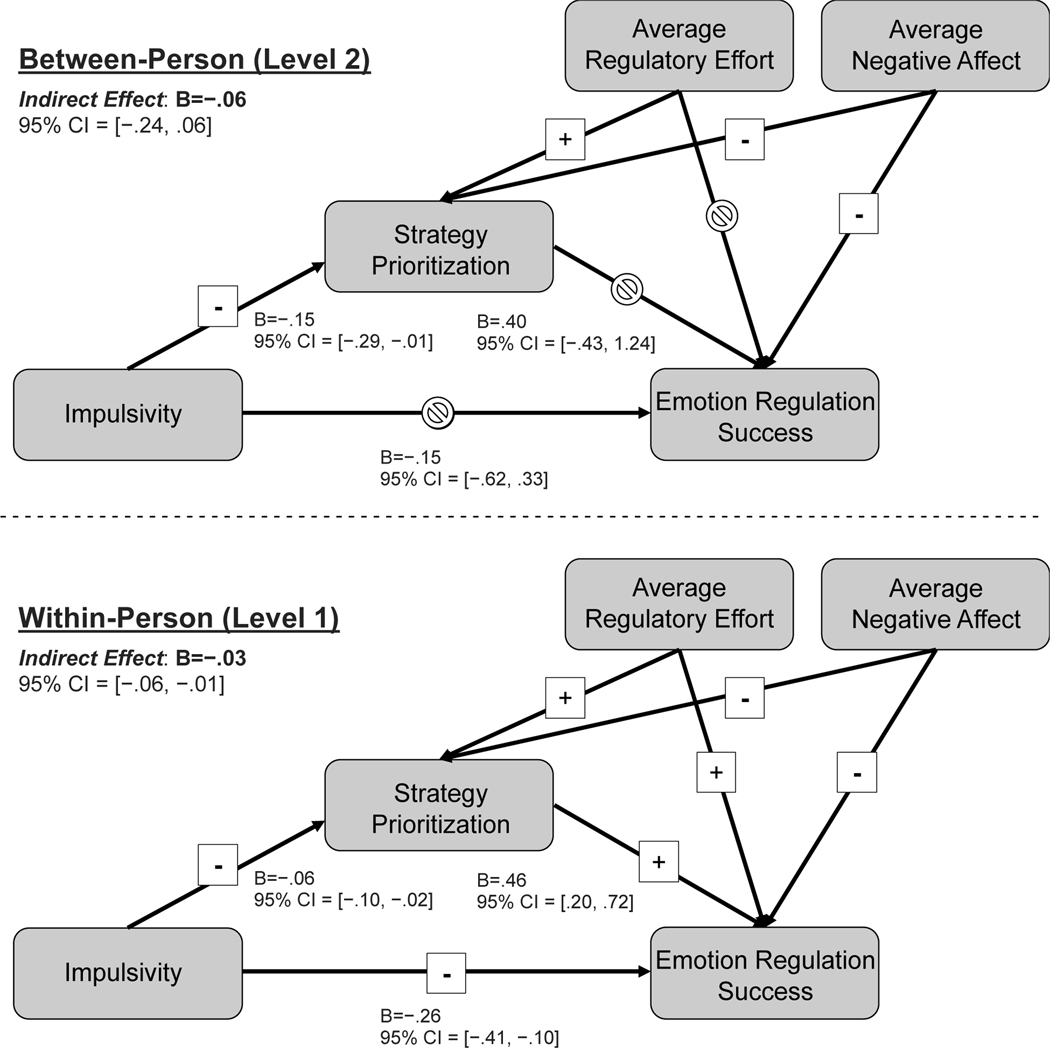
After covarying average regulatory effort and average NA, the indirect effect of impulsivity on ER success was no longer significant at the between-person level (B=−.06, 95% CI = [−.24, .06]; Figure 2). At the between-person level, the effect of impulsivity on ER strategy prioritization (B=−.15, SE=.07, 95% CI = [−.29, −.01], p<.05; Supplementary Table S3, Figure 2) remained significant; however, the effect of ER strategy prioritization on ER success (p=.344; Supplementary Table S3, Figure 2) was no longer significant. With respect to average regulatory effort, we found that individuals who showed lower average regulatory effort showed lower strategy prioritization (B=.37, SE=.07, 95% CI = [.24, .51], p<.001; Supplementary Table S3, Figure 2), but not less ER success, on average (p=.073; Supplementary Table S3, Figure 2). With respect to average NA, we found that individuals who showed greater NA, on average, showed less strategy prioritization (B=−.15, SE=.06, 95% CI = [−.26, −.04], p<.007; Supplementary Table S3, Figure 2) and less ER success (B=−.65, SE=.21, 95% CI = [−1.06, −.24], p<.003; Supplementary Table S3, Figure 2). The estimated marginal R2 of these multilevel models are reported in Supplementary Table S2 and Supplementary Table S3.
Figure 2. Multilevel mediation model with sensitivity analysis.
Abbreviations: 95% CI, 95% confidence interval.
Notes: The paths for the covariates are not included in the figure for clarity. For more details regarding the estimates for these paths, see Supplementary Table S3.
Level 1 Mediation Findings
At the within-person level, in moments when individuals report more impulsivity compared to usual, do they show lower strategy prioritization, and in turn, lower success with emotion regulation than usual?
The indirect effect of impulsivity on ER success was significant at the within-person level (B=−.04, 95% CI = [−.08, −.01]; Figure 1). Specifically, in moments when people endorsed more impulsivity compared to usual, they showed lower ER strategy prioritization than usual (B=−.06, SE=.02, 95% CI = [−.10, −.02], p<.007; Supplementary Table S2, Figure 1), which was associated with lower ER success than usual (B=.66, SE=.14, 95% CI = [.39, .92], p<.001; Supplementary Table S2, Figure 1). The direct effect of impulsivity on ER success was also significant at the within-person level, given that in moments when individuals reported more impulsivity, they showed lower ER success (B=−.26, SE=.08, 95% CI = [−.42, −.09], p<.003; Supplementary Table S2, Figure 1).
After covarying average regulatory effort and average NA, the indirect effect of impulsivity on ER success remained significant at the within-person level (B=−.03, 95% CI = [−.06, −.01]; Figure 2). The effect of impulsivity on ER strategy prioritization (B=−.06, SE=.02, 95% CI = [−.10, −.02], p<.004; Supplementary Table S3, Figure 2), and the effect of ER strategy prioritization on ER success (B=.46, SE=.13, 95% CI = [.20, .72], p<.002; Supplementary Table S3, Figure 2), both also remained significant at the within-person level. Additionally, the direct effect of impulsivity on ER success remained significant (B=−.26, SE=.08, 95% CI = [−.41, −.10], p<.002; Supplementary Table S3, Figure 2). In terms of average regulatory effort, we found that, in moments when individuals showed lower average regulatory effort than usual, they also indicated less ER strategy prioritization than usual (B=.28, SE=.04, 95% CI = [.21, .35], p<.001; Supplementary Table S3, Figure 2) and less success with emotion regulation compared to usual (B=.44, SE=.12, 95% CI = [.10, .22], p<.001; Supplementary Table S3, Figure 2). In terms of average NA, we found that in moments when individuals showed greater NA than usual, they also indicated less ER strategy prioritization than usual (B=−.07, SE=.02, 95% CI = [−.11, −.03], p<.002; Supplementary Table S3, Figure 2) and less ER success compared to usual (B=−.23, SE=.06, 95% CI = [−.35, −.10], p<.001; Supplementary Table S3, Figure 2).
Group Differences in Strategy Prioritization
Do individuals with a history of depression show lower strategy prioritization than healthy individuals?
Individuals with remitted depression showed lower ER strategy prioritization compared to healthy individuals (B=−.24, SE=.11, 95% CI = [−.46, −.02], p<.04, R2= .03; Supplementary Table S4). After covarying average regulatory effort, the effect of depression history on ER strategy prioritization remained significant (B=−.20, SE=.10, 95% CI = [−.40, −.01], p<.05, R2= .20; Supplementary Table S5).
Does depression history moderate associations between examined variables?
Depression history moderated the association between momentary impulsivity at Level 2 and ER strategy prioritization at Level 1 (B=.33, SE=.12, 95% CI = [.09, .57], p<.008; Supplementary Figure S1). For individuals with remitted MDD, the effect of momentary impulsivity at Level 2 on ER strategy prioritization at Level 1 was not significant (B=.02, SE=.10, 95% CI = [−.18, .23], p=.82). For healthy individuals, the effect of momentary impulsivity at Level 2 on ER strategy prioritization at Level 1 was significant (B=−.31, SE=.09, 95% CI = [−.47, −.14], p<.001). Depression history did not moderate any other paths in the 1–1-1 mediation model (all ps>.05).
Emotion Regulation Strategy Type as a Predictor of Strategy Prioritization
How does the type of emotion regulation strategy used relate to strategy prioritization?
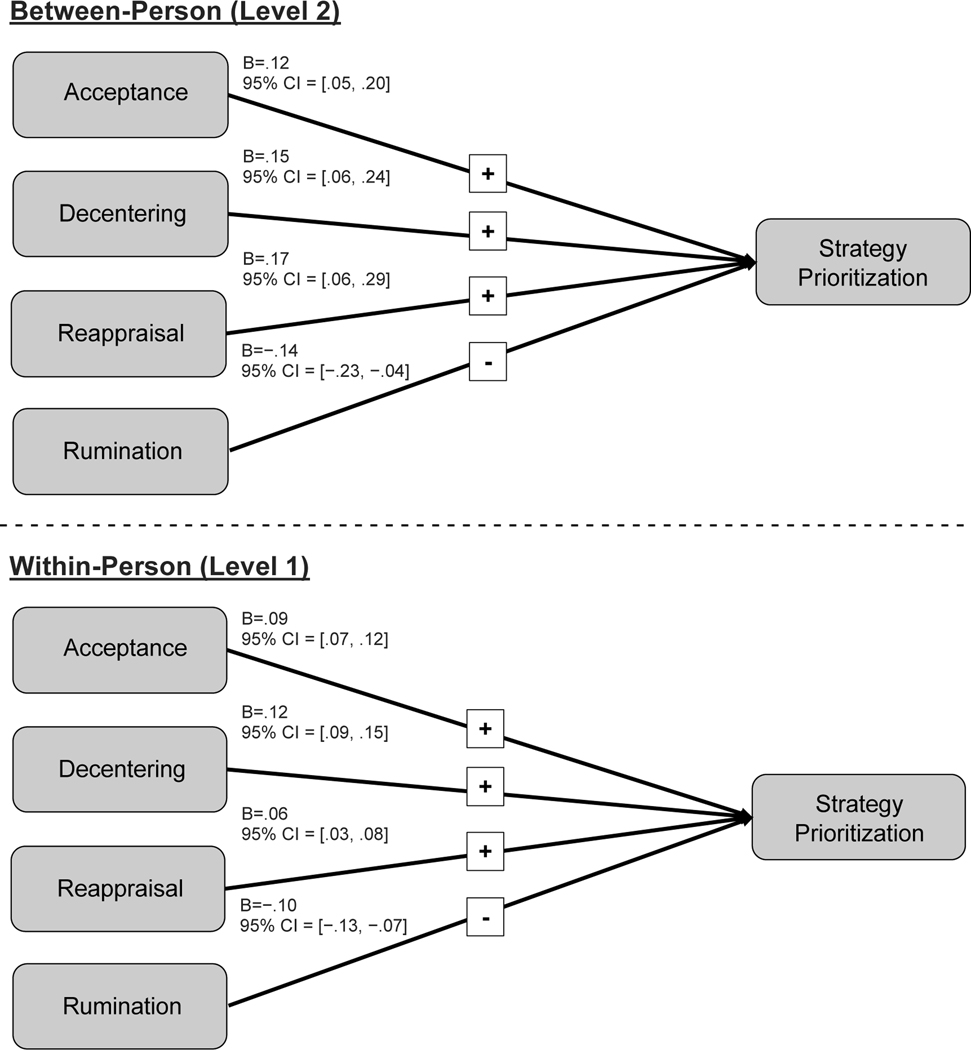
At the between-person level, individuals who, on average, used more acceptance (B=.12, SE=.04, 95% CI = [.05, .20], p<.002; Supplementary Table S6, Figure 3), decentering (B=.15, SE=.05, 95% CI = [.06, .24], p<.002; Supplementary Table S6, Figure 3), or reappraisal (B=.17, SE=.06, 95% CI = [.06, .29], p<.005; Supplementary Table S6, Figure 3) to regulate their emotions showed greater ER strategy prioritization. In contrast, individuals who, on average, used more rumination to regulate their emotions showed lower ER strategy prioritization (B=−.14, SE=.05, 95% CI = [−.23, −.04], p<.005; Supplementary Table S6, Figure 3). There were no differences in ER strategy prioritization between individuals based on their average use of distraction (p=.162; Supplementary Table S6) and mind-wandering (p=.652; Supplementary Table S6).
Figure 3. Multilevel model with emotion regulation strategy type predicting emotion regulation strategy prioritization.
Abbreviations: 95% CI, 95% confidence interval.
Note: Non-significant predictors of strategy prioritization (i.e., distraction, mind-wandering) are not included in the figure; however, these predictors are included in the model. For details regarding the estimates for these paths, see Supplementary Table S6.
At the within-person level, in moments when individuals used more acceptance (B=.09, SE=.01, 95% CI = [.07, .12], p<.001; Supplementary Table S6, Figure 3), decentering (B=.12, SE=.01, 95% CI = [.09, .15], p<.001; Supplementary Table S6, Figure 3), or reappraisal (B=.06, SE=.01, 95% CI = [.03, .08], p<.001; Supplementary Table S6, Figure 3) compared to usual, they tended to show greater ER strategy prioritization compared to usual. On the contrary, in moments when people used more rumination (B=−.10, SE=.02, 95% CI = [−.13, −.07], p<.001; Supplementary Table S6, Figure 3) than usual, they tended to show less ER strategy prioritization compared to usual. In moments when individuals engaged in distraction (p=.054; Supplementary Table S6) or mind-wandering (p=.381; Supplementary Table S6) more than usual, they did not show any difference in ER strategy prioritization compared to usual. The marginal R2 of this multilevel model was estimated to be 0.47 (Supplementary Table S6).
Discussion
The present study found that, at both the between- and within-person levels, momentary impulsivity was associated with emotion regulation strategy prioritization. At the within-person level, emotion regulation strategy prioritization was also related to emotion regulation success. We extended prior work, which showed that deficits in top-down processes (e.g., self-control) relate to strategy prioritization (Wenzel et al., 2021a; Wenzel et al., 2021b), by illustrating that impulsivity in everyday life predicted less strategy prioritization. Impulsivity has been thought to capture both top-down (e.g., response inhibition) and bottom-up (e.g., delay discounting) processes (Nigg, 2017). Given that impulsivity predicted lower strategy prioritization, the present findings could suggest that lower strategy prioritization might be driven by both (1) weakened top-down control (e.g., difficulties with inhibiting attention to irrelevant stimuli and focusing on regulatory strategy use), and (2) heightened bottom-up reactivity to emotions (e.g., highly valuing an immediate reduction in negative affect, and possibly switching quickly from one regulatory strategy to the next).
Not only was momentary impulsivity associated with lower regulatory strategy prioritization, but lower regulatory strategy prioritization was associated with lower regulatory success at the within-person level. Whereas previous studies found that lower ER strategy prioritization predicted negative clinical outcomes (Blanke et al., 2020; Wang et al., 2021; Wenzel et al., 2021a; Wenzel et al., 2021b), our data indicate that ER strategy prioritization may also be a mechanism by which greater momentary impulsivity confers risk for negative clinical outcomes (Carver & Johnson, 2018). This suggests the possibility that interventions focused on training individuals to prioritize using some ER strategies to a greater degree than others may improve regulatory success, and may be particularly needed during moments when people are acting more impulsively than usual. Additionally, cognitive training interventions that target response inhibition and working memory have been shown to decrease impulsivity (Peckham & Johnson, 2018) – it is possible that such interventions may also increase ER strategy prioritization, by providing individuals with the skills to more effectively focus on the ER strategy at hand, as well as more effectively use ER strategies that may rely on working memory (e.g., reappraisal; McRae et al., 2012; Pe et al., 2013).
Cognitive training interventions may be particularly important to deliver in moments when individuals are reporting greater momentary impulsivity than usual, as ER strategy prioritization significantly mediated the relationship between greater momentary impulsivity and lower ER success at the within-person level. The lack of a significant mediation effect at the between-person level suggests that cognitive training interventions may not necessarily benefit ER success in certain people (e.g., individuals who score high on average momentary impulsivity) more than others (e.g., individuals who score low on average momentary impulsivity), but rather may serve to improve ER success in all individuals when delivered in moments of need (e.g., moments when individuals report higher momentary impulsivity compared to usual). The significance of effects at the within-person level, but not at the between-person level, also further highlights the importance of examining relationships between variables at both levels, given that these relationships do not necessarily generalize across levels (Fisher et al., 2018).
Individuals with remitted depression showed lower ER strategy prioritization compared to healthy individuals, which suggests that lowered ER strategy prioritization may either be a vulnerability factor for depression, or a psychological “scar” of depression (Just et al., 2001). Future studies should elucidate whether lowered ER strategy prioritization may confer vulnerability to depression, by exploring whether individuals who are at risk for depression (e.g., first-degree relatives of individuals with depression) show lower strategy prioritization compared to healthy individuals. If individuals who are at risk of depression show lower ER strategy prioritization, this may suggest that lowered strategy prioritization could be a vulnerability factor for depression. If individuals at risk do not show lower ER strategy prioritization, this may suggest that lowered strategy prioritization may not be a vulnerability factor for depression, and instead might be a psychological consequence of depression, which could be evaluated further with prospective studies across stages of illness. Much of the literature on ER strategy prioritization has been limited to non-clinical samples thus far (Blanke et al., 2020; Wang et al., 2021; Wenzel et al., 2021a; Wenzel et al., 2021b). Given that emotion dysregulation is relevant to many forms of psychopathology (Aldao et al., 2010; Joormann & Stanton, 2016; McLaughlin et al., 2011), it remains important to elucidate the role that lowered strategy prioritization may play in the development of psychopathology, using clinical and at-risk samples.
Here, we found that acceptance, decentering, and reappraisal were associated with greater ER strategy prioritization, whereas rumination was associated with lower ER strategy prioritization. As suggested in prior work (Blanke et al., 2020), it is possible that greater ER strategy prioritization may indicate the successful selection and implementation of certain ER strategies, which sufficiently meet contextual demands without necessitating the use of other additional ER strategies. In particular, because acceptance, decentering, and reappraisal tend to relate to successful ER (Lennarz et al., 2019; Webb et al., 2012; Wu et al., 2022; Wylie et al., 2023), additional ER strategies may not be needed, allowing these selective few strategies to be prioritized. In contrast, rumination may tend to lead to unsuccessful ER (Aldao et al., 2010; Lennarz et al., 2019; Wylie et al., 2023), necessitating additional ER strategies, thus contributing to less selective prioritization in ER strategy use. Given that strategy prioritization and regulatory success could have a reciprocal relationship, future studies should sample these constructs on a more intensive timescale, to better understand how these processes contribute to one another.
One limitation of the present study is that our EMA protocol captured overall ER strategy use within an approximately 30-minute timeframe – thus, we were not able to conduct a more fine-grained analysis on how ER strategies were used within this timeframe. It is possible that individuals who showed low ER strategy prioritization could have either (1) quickly switched from using one ER strategy to the next, (2) simultaneously used many ER strategies all at once throughout this timeframe, or (3) refrained from using any ER strategies during this timeframe. Thus, it remains unclear the mechanism by which reduced ER strategy prioritization relates to lower regulatory success. We asked participants to report their ER strategy use in 21 surveys (three surveys each day for seven days) and did not collect data on ER strategy use on a smaller timescale to limit participant burden (Ebner-Priemer & Trull, 2009). Future studies could examine ER strategy prioritization more intensively (on a smaller timescale), to capture how strategy prioritization unfolds over time in more nuance, and to better understand the directionality of the relationship between strategy prioritization and regulatory success. One way that future studies could achieve this is by asking participants to complete more surveys on a single day about ER strategy use and ER success, but for fewer days. Future studies could also ask participants to report not only the degree to which they engaged in using ER strategies, but also how long they persisted in ER strategy use before switching strategies.
A second limitation of this study is the use of self-report data. Given that participants were asked to report their ER strategy use primarily in response to unpleasant thoughts or feelings, participants would have only endorsed using ER strategies if they perceived a need to regulate their emotions. Individuals with depression may differ in their emotion preferences (Vanderlind et al., 2020), which might impact the circumstances in which individuals with depression determine that there is a need to regulate their emotions. This possibility should be examined in future work, which could measure participants’ ER strategy use in response to a lab-based stressor. Future work also is needed to determine whether higher self-reported momentary impulsivity is related to lower ER strategy prioritization in the context of a stressor that is standardized across participants (e.g., in the lab), to complement our results that occurred during moments when individuals perceived a need to regulate their emotions in everyday life. A third limitation of the study is its focus on examining ER in response to negative affect. Research has suggested the importance of also examining ER in response to positive affect (Nelis et al., 2015; Werner-Seidler et al., 2013). For example, individuals with remitted depression have been shown to attempt to dampen positive affect more frequently than healthy individuals (Nelis et al., 2015; Werner-Seidler et al., 2013). Thus, future work could test the generalizability (vs. specificity) of lowered strategy prioritization in response to positive and negative affect as a potential trait-vulnerability factor, or psychological consequence, of depression.
Lastly, the effect sizes found in this study are fairly small. Impulsivity predicted approximately 4% of the variance in ER strategy prioritization, and together, impulsivity and ER strategy prioritization predicted around 17% of the variance in regulation success (Supplementary Table S2). Though these individual effects were small, small effect sizes could still be important to predicting regulatory behavior and outcomes. Future work can build on these findings and account for more of the variance in these constructs by investigating how situational factors might shape ER strategy prioritization and regulation success. This would be important to further capturing how context impacts ER processes (Aldao, 2013). Future work should also aim to utilize larger samples that may be better powered to detect very small effect sizes (Pan et al., 2018), which may be important to accounting for more variance in clinically-relevant outcomes.
Conclusion
This study is the first to document relationships between impulsivity and ER strategy prioritization. Examining the process of ER repeatedly over time allowed us to detect these relationships between and within individuals in everyday life. Individuals who tended to endorse more impulsivity showed less ER strategy prioritization. Further, during moments when individuals reported more impulsivity than usual, they showed lower ER strategy prioritization, which was associated with less ER success. Interventions focused on training people to selectively prioritize using some ER strategies to a greater degree than other strategies may improve regulation success particularly during moments when people are endorsing acting more impulsively than usual.
Supplementary Material
HIGHLIGHTS.
Impulsivity interferes with regulatory strategy prioritization in daily life
Lower regulatory strategy prioritization contributes to lower regulation success
Training individuals to prioritize some strategies over others may improve success
Interventions may be particularly necessary during moments of increased impulsivity
Acknowledgments
Ellie Xu was supported by the National Science Foundation Graduate Research Fellowship Program (DGE-1842487). This work was supported by grants to Jonathan P. Stange from the National Institute of Mental Health (K23MH112769), the Portes Foundation and Institute of Medicine of Chicago, and the American Psychological Foundation. REDCap was supported by the University of Illinois at Chicago (UIC) Center for Clinical and Translational Science and the Southern California Clinical and Translational Science Institute, which are supported by the National Center for Advancing Translational Sciences of the National Institutes of Health, through Grant Award Number UL1TR002003 (UIC) and UL1TR001855 and UL1TR000130 (USC).
The funding sources had no involvement in study design; in the collection, analysis, and interpretation of data; the writing of the report; and in the decision to submit the article for publication.
Footnotes
Conflicts of Interest
The authors declare that there were no conflicts of interest with respect to the authorship or publication of this article.
Declarations of interest: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aldao A. (2013). The Future of Emotion Regulation Research: Capturing Context. Perspectives on Psychological Science, 8(2), 155–172. 10.1177/1745691612459518 [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Aldao A, Sheppes G, & Gross JJ (2015). Emotion Regulation Flexibility. Cognitive Therapy and Research, 39(3), 263–278. 10.1007/s10608-014-9662-4 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Arditte KA, & Joormann J. (2011). Emotion Regulation in Depression: Reflection Predicts Recovery from a Major Depressive Episode. Cognitive Therapy and Research, 35(6), 536–543. 10.1007/s10608-011-9389-4 [DOI] [Google Scholar]
- Bahlinger K, Lincoln TM, & Clamor A. (2022). Are Acute Increases and Variability in Emotion Regulation Strategies Related to Negative Affect and Paranoid Thoughts in Daily Life? Cognitive Therapy and Research, 46(1), 62–72. 10.1007/s10608-021-10253-1 [DOI] [Google Scholar]
- Battaglini AM, Rnic K, Jameson T, Jopling E, Albert AY, & LeMoult J. (2022). The Association of Emotion Regulation Flexibility and Negative and Positive Affect in Daily Life. Affective Science, 3(3), 673–685. 10.1007/s42761-022-00132-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanke ES, Brose A, Kalokerinos EK, Erbas Y, Riediger M, & Kuppens P. (2020). Mix it to fix it: Emotion regulation variability in daily life. Emotion, 20(3), 473–485. 10.1037/emo0000566 [DOI] [PubMed] [Google Scholar]
- Blanke ES, Neubauer AB, Houben M, Erbas Y, & Brose A. (2022). Why do my thoughts feel so bad? Getting at the reciprocal effects of rumination and negative affect using dynamic structural equation modeling. Emotion, 22, 1773–1786. 10.1037/emo0000946 [DOI] [PubMed] [Google Scholar]
- Bonanno GA, & Burton CL (2013). Regulatory Flexibility: An Individual Differences Perspective on Coping and Emotion Regulation. Perspectives on Psychological Science, 8(6), 591–612. 10.1177/1745691613504116 [DOI] [PubMed] [Google Scholar]
- Carver CS, & Johnson SL (2018). Impulsive reactivity to emotion and vulnerability to psychopathology. American Psychologist, 73(9), 1067–1078. 10.1037/amp0000387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo D, Pavani J-B, Fernandez-Alvarez J, Garcia-Palacios A, & Botella C. (2021). Savoring the present: The reciprocal influence between positive emotions and positive emotion regulation in everyday life. PLOS ONE, 16(5), e0251561. 10.1371/journal.pone.0251561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Double KS, Pinkus RT, & MacCann C. (2022). Emotionally intelligent people show more flexible regulation of emotions in daily life. Emotion, 22, 397–402. 10.1037/emo0001069 [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Eid M, Kleindienst N, Stabenow S, & Trull TJ (2009). Analytic strategies for understanding affective (in) stability and other dynamic processes in psychopathology. Journal of Abnormal Psychology, 118(1), 195. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, & Trull TJ (2009). Ecological momentary assessment of mood disorders and mood dysregulation. Psychological Assessment, 21(4), 463–475. 10.1037/a0017075 [DOI] [PubMed] [Google Scholar]
- Eekhout I, de Vet HCW, Twisk JWR, Brand JPL, de Boer MR, & Heymans MW (2014). Missing data in a multi-item instrument were best handled by multiple imputation at the item score level. Journal of Clinical Epidemiology, 67(3), 335–342. 10.1016/j.jclinepi.2013.09.009 [DOI] [PubMed] [Google Scholar]
- Egloff B, Schmukle SC, Burns LR, & Schwerdtfeger A. (2006). Spontaneous emotion regulation during evaluated speaking tasks: Associations with negative affect, anxiety expression, memory, and physiological responding. Emotion, 6(3), 356–366. 10.1037/1528-3542.6.3.356 [DOI] [PubMed] [Google Scholar]
- Ehring T, Tuschen-Caffier B, Schnülle J, Fischer S, & Gross JJ (2010). Emotion regulation and vulnerability to depression: Spontaneous versus instructed use of emotion suppression and reappraisal. Emotion, 10, 563–572. 10.1037/a0019010 [DOI] [PubMed] [Google Scholar]
- Enders CK (2017). Multiple imputation as a flexible tool for missing data handling in clinical research. Behaviour Research and Therapy, 98, 4–18. 10.1016/j.brat.2016.11.008 [DOI] [PubMed] [Google Scholar]
- Fisher AJ, Medaglia JD, & Jeronimus BF (2018). Lack of group-to-individual generalizability is a threat to human subjects research. Proceedings of the National Academy of Sciences, 115(27), E6106–E6115. 10.1073/pnas.1711978115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford BQ, & Troy AS (2019). Reappraisal Reconsidered: A Closer Look at the Costs of an Acclaimed Emotion-Regulation Strategy. Current Directions in Psychological Science, 28(2), 195–203. 10.1177/0963721419827526 [DOI] [Google Scholar]
- Geldhof GJ, Preacher KJ, & Zyphur MJ (2014). Reliability estimation in a multilevel confirmatory factor analysis framework. Psychological Methods, 19(1), 72–91. 10.1037/a0032138 [DOI] [PubMed] [Google Scholar]
- Gottschall AC, West SG, & Enders CK (2012). A Comparison of Item-Level and Scale-Level Multiple Imputation for Questionnaire Batteries. Multivariate Behavioral Research, 47(1), 1–25. 10.1080/00273171.2012.640589 [DOI] [Google Scholar]
- Gross JJ (2015). Emotion Regulation: Current Status and Future Prospects. Psychological Inquiry, 26(1), 1–26. 10.1080/1047840X.2014.940781 [DOI] [Google Scholar]
- Gruber J, Harvey AG, & Gross JJ (2012). When trying is not enough: Emotion regulation and the effort–success gap in bipolar disorder. Emotion, 12(5), 997–1003. 10.1037/a0026822 [DOI] [PubMed] [Google Scholar]
- Haines SJ, Gleeson J, Kuppens P, Hollenstein T, Ciarrochi J, Labuschagne I, Grace C, & Koval P. (2016). The Wisdom to Know the Difference: Strategy-Situation Fit in Emotion Regulation in Daily Life Is Associated With Well-Being. Psychological Science, 27(12), 1651–1659. 10.1177/0956797616669086 [DOI] [PubMed] [Google Scholar]
- Hamilton M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56–62. 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, & Coutts JJ (2020). Use omega rather than Cronbach’s alpha for estimating reliability. But…. Communication Methods and Measures, 14(1), 1–24. 10.1080/19312458.2020.1718629 [DOI] [Google Scholar]
- Joormann J, Dkane M, & Gotlib IH (2006). Adaptive and Maladaptive Components of Rumination? Diagnostic Specificity and Relation to Depressive Biases. Behavior Therapy, 37(3), 269–280. 10.1016/j.beth.2006.01.002 [DOI] [PubMed] [Google Scholar]
- Joormann J, Siemer M, & Gotlib IH (20070813). Mood regulation in depression: Differential effects of distraction and recall of happy memories on sad mood. Journal of Abnormal Psychology, 116(3), 484. 10.1037/0021-843X.116.3.484 [DOI] [PubMed] [Google Scholar]
- Joormann J, & Stanton CH (2016). Examining emotion regulation in depression: A review and future directions. Behaviour research and therapy, 86, 35–49. 10.1016/j.brat.2016.07.007 [DOI] [PubMed] [Google Scholar]
- Joormann J, & Vanderlind WM (2014). Emotion Regulation in Depression: The Role of Biased Cognition and Reduced Cognitive Control. Clinical Psychological Science, 2(4), 402–421. 10.1177/2167702614536163 [DOI] [Google Scholar]
- Just N, Abramson LY, & Alloy LB (2001). Remitted depression studies as tests of the cognitive vulnerability hypotheses of depression onset: A critique and conceptual analysis. Clinical Psychology Review, 21(1), 63–83. [DOI] [PubMed] [Google Scholar]
- Kazak AE (2018). Journal article reporting standards. [DOI] [PubMed] [Google Scholar]
- Koval P, Pe ML, Meers K, & Kuppens P. (2013). Affect dynamics in relation to depressive symptoms: Variable, unstable or inert? Emotion, 13(6), 1132. [DOI] [PubMed] [Google Scholar]
- Lennarz HK, Hollenstein T, Lichtwarck-Aschoff A, Kuntsche E, & Granic I. (2019). Emotion regulation in action: Use, selection, and success of emotion regulation in adolescents’ daily lives. International Journal of Behavioral Development, 43(1), 1–11. 10.1177/0165025418755540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levens SM, Muhtadie L, & Gotlib IH (2009). Rumination and impaired resource allocation in depression. Journal of Abnormal Psychology, 118, 757–766. 10.1037/a0017206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu DY, & Thompson RJ (2017). Selection and implementation of emotion regulation strategies in major depressive disorder: An integrative review. Clinical Psychology Review, 57, 183–194. 10.1016/j.cpr.2017.07.004 [DOI] [PubMed] [Google Scholar]
- Mackinnon A, Jorm AF, Christensen H, Korten AE, Jacomb PA, & Rodgers B. (1999). A short form of the Positive and Negative Affect Schedule: Evaluation of factorial validity and invariance across demographic variables in a community sample. Personality and Individual Differences, 27(3), 405–416. 10.1016/S0191-8869(98)00251-7 [DOI] [Google Scholar]
- Malesza M. (2021). Relationship between emotion regulation, negative affect, gender and delay discounting. Current Psychology, 40(8), 4031–4039. 10.1007/s12144-019-00366-y [DOI] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Mennin DS, & Nolen-Hoeksema S. (2011). Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy, 49(9), 544–554. 10.1016/j.brat.2011.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRae K, Jacobs SE, Ray RD, John OP, & Gross JJ (2012). Individual differences in reappraisal ability: Links to reappraisal frequency, well-being, and cognitive control. Journal of Research in Personality, 46(1), 2–7. 10.1016/j.jrp.2011.10.003 [DOI] [Google Scholar]
- Nelis S, Holmes EA, & Raes F. (2015). Response styles to positive affect and depression: Concurrent and prospective associations in a community sample. Cognitive therapy and research, 39, 480–491. 10.1007/s10608-015-9671-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT (2017). Annual Research Review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. Journal of Child Psychology and Psychiatry, 58(4), 361–383. 10.1111/jcpp.12675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurnberger JI, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, Severe JB, Malaspina D, & Reich T. (1994). Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Archives of General Psychiatry, 51(11), 849–864. 10.1001/archpsyc.1994.03950110009002 [DOI] [PubMed] [Google Scholar]
- Pan H, Liu S, Miao D, & Yuan Y. (2018). Sample size determination for mediation analysis of longitudinal data. BMC Medical Research Methodology, 18(1), 1–11. 10.1186/s12874-018-0473-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pe ML, Raes F, & Kuppens P. (2013). The Cognitive Building Blocks of Emotion Regulation: Ability to Update Working Memory Moderates the Efficacy of Rumination and Reappraisal on Emotion. PLOS ONE, 8(7), e69071. 10.1371/journal.pone.0069071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peckham AD, & Johnson SL (2018). Cognitive control training for emotion-related impulsivity. Behaviour Research and Therapy, 105, 17–26. 10.1016/j.brat.2018.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen AB, Mikkelsen EM, Cronin-Fenton D, Kristensen NR, Pham TM, Pedersen L, & Petersen I. (2017). Missing data and multiple imputation in clinical epidemiological research. Clinical epidemiology, 157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, DebRoy S, Sarkar D, Heisterkamp S, Van Willigen B, & Maintainer R. (2017). Package ‘nlme’. Linear and nonlinear mixed effects models, 3(1), 274. [Google Scholar]
- Preacher KJ, & Selig JP (2012). Advantages of Monte Carlo Confidence Intervals for Indirect Effects. Communication Methods and Measures, 6(2), 77–98. 10.1080/19312458.2012.679848 [DOI] [Google Scholar]
- Selig JP, & Preacher KJ (2008). Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects [Computer software]. [Google Scholar]
- Snijders TA, & Bosker RJ (2011). Multilevel analysis: An introduction to basic and advanced multilevel modeling, Multilevel analysis, 1–368. [Google Scholar]
- Stange JP, Hamilton JL, Fresco DM, & Alloy LB (2017). Flexible parasympathetic responses to sadness facilitate spontaneous affect regulation. Psychophysiology, 54(7), 1054–1069. 10.1111/psyp.12856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi D, & MacKinnon DP (2016). Monte Carlo Confidence Intervals for Complex Functions of Indirect Effects. Structural Equation Modeling: A Multidisciplinary Journal, 23(2), 194–205. 10.1080/10705511.2015.1057284 [DOI] [Google Scholar]
- Tomko RL, Solhan MB, Carpenter RW, Brown WC, Jahng S, Wood PK, & Trull TJ (2014). Measuring impulsivity in daily life: The Momentary Impulsivity Scale. Psychological Assessment, 26(2), 339–349. 10.1037/a0035083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troy AS, Shallcross AJ, & Mauss IB (2013). A Person-by-Situation Approach to Emotion Regulation: Cognitive Reappraisal Can Either Help or Hurt, Depending on the Context. Psychological Science, 24(12), 2505–2514. 10.1177/0956797613496434 [DOI] [PubMed] [Google Scholar]
- Van Buuren S, & Groothuis-Oudshoorn K. (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3), 1–67. 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- Vanderlind WM, Millgram Y, Baskin-Sommers AR, Clark MS, & Joormann J. (2020). Understanding positive emotion deficits in depression: From emotion preferences to emotion regulation. Clinical psychology review, 76, 101826. 10.1016/j.cpr.2020.101826 [DOI] [PubMed] [Google Scholar]
- Wang X, Blain SD, Meng J, Liu Y, & Qiu J. (2021). Variability in emotion regulation strategy use is negatively associated with depressive symptoms. Cognition and Emotion, 35(2), 324–340. 10.1080/02699931.2020.1840337 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Webb TL, Miles E, & Sheeran P. (2012). Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychological Bulletin, 138(4), 775–808. 10.1037/a0027600 [DOI] [PubMed] [Google Scholar]
- Wenzel M, Bürgler S, Rowland Z, & Hennecke M. (2023). Self-control dynamics in daily life: The importance of variability between self-regulatory strategies and strategy differentiation. European Journal of Personality, 37(1), 33–56. 10.1177/08902070211043023 [DOI] [Google Scholar]
- Wenzel M, Rowland Z, & Kubiak T. (2021). Examining five pathways on how selfcontrol is associated with emotion regulation and affective well-being in daily life. Journal of Personality, 89(3), 451–467. 10.1111/jopy.12590 [DOI] [PubMed] [Google Scholar]
- Werner-Seidler A, Banks R, Dunn BD, & Moulds ML (2013). An investigation of the relationship between positive affect regulation and depression. Behaviour research and therapy, 51(1), 46–56. 10.1016/j.brat.2012.11.001 [DOI] [PubMed] [Google Scholar]
- Wu JL, Hamilton JL, Fresco DM, Alloy LB, & Stange JP (2022). Decentering predicts attenuated perseverative thought and internalizing symptoms following stress exposure: A multi-level, multi-wave study. Behaviour Research and Therapy, 152, 104017. 10.1016/j.brat.2021.104017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wylie MS, Colasante T, De France K, Lin L, & Hollenstein T. (2023). Momentary emotion regulation strategy use and success: Testing the influences of emotion intensity and habitual strategy use. Emotion, 23, 375–386. 10.1037/emo0001074 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.